Although there has been a significant decline in overall stroke mortality rates since the 1950s, age-adjusted stroke death rates have remained higher in blacks than in whites through 2008.1 The Table shows the 2009 stroke death rates per 100 000 according to age and sex for blacks and whites. The relative excess in deaths from stroke among blacks compared with whites is most marked in the population aged <65 years, in which, for example, there is a black/white mortality ratio of 3.7 among men aged 45 to 54 years. The black/white mortality ratio decreases with age in both sexes until ages ≥85 years, when death rates in blacks are lower than in whites. Differences between whites and other racial and ethnic groups in the United States are important but less marked. In 2008, stroke death rates were lowest in American Indians/Alaska natives (24.0 in women and 24.5 in men per 100 000.)1 Stroke death rates were similar in Hispanic and Asian/Pacific Islanders, both with rates lower than those in whites.1 Complicating the discussion of racial and ethnic differences in stroke mortality is that the race groups of whites, blacks, Asian/Pacific Islander, and American Indian/Alaska Native include persons of Hispanic and non-Hispanic origin, and the Hispanic category includes persons across all race groups. Also, death rates are known to be underestimated for Hispanics, Asian/Pacific Islanders, and American Indians/Alaska Natives for whom data are likely less reliable.2
Table.
Death Rates Per 100 000 Population for Stroke According to Age and Sex for Blacks and Whites and Black/White Mortality Ratio, 2009
| Age, y | Men
|
Women
|
||||
|---|---|---|---|---|---|---|
| Black Death Rate | White Death Rate | Black/White Mortality Ratio | Black Death Rate | White Death Rate | Black/White Mortality Ratio | |
| 45–54 | 45.5 | 12.2 | 3.7 | 34.8 | 9.9 | 3.5 |
| 55–64 | 106.9 | 32.3 | 3.3 | 66.7 | 24.7 | 2.7 |
| 65–74 | 240.4 | 110.1 | 2.2 | 166.0 | 88.9 | 1.9 |
| 75–84 | 544.0 | 394.5 | 1.4 | 471.3 | 370.9 | 1.3 |
| ≥85 | 1103.5 | 1142.3 | 1.0 | 1268.6 | 1325.4 | 1.0 |
Rates provided for non-Hispanic whites and non-Hispanic blacks.
Data taken from Centers for Disease Control and Prevention, National Center for Health Statistics. CDC WONDER Online Database, compiled from Compressed Mortality File 1999–2009 Series 20 No. 20, 2012. Accessed October 28, 2012 at http://wonder.cdc.gov/cmf-icd10.html.
The initial concerns about black–white disparities in stroke were recognized in the 1970s based on mortality statistics.3,4 These concerns were reinforced by 3 population-based cohort studies of stroke incidence reporting rates observed during the 1960s that also showed similar black–white disparities in incident stroke risk.5–7
There are several more current epidemiological studies that provide insights to black–white differences in stroke incidence across a broad age spectrum and in different regions of the United States, with some also providing insights to the risk factors potentially contributing to the excess stroke risk in blacks compared with whites.8–17 The higher prevalence of risk factors in blacks, particularly hypertension and diabetes mellitus, are perhaps the most widely recognized contributing factors.8,18,19 Data from 13-year follow-up (through 1987) of the first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study showed that the risk factors of age, sex, education, blood pressure treatment group (normotensive, controlled hypertensive, hypertensives receiving medication, and hypertensives not receiving medication), systolic blood pressure, diabetes mellitus, history of heart disease, Quetelet index (ie, body mass index), hemoglobin, and magnesium explained approximately one-third of the excess stroke risk among blacks aged 35 to 74 years at baseline.9 Blacks especially had higher prevalence of diabetes mellitus, hypertension, and lower educational level. Consistent with the previous Evans County, Georgia study,5 there was also an interaction with age, suggesting that even after adjustment for these risk factors, blacks aged 35 to 44 years remained at substantially increased risk for stroke, but racial differences for those aged >64 years were smaller or nonexistent. Some limitations of this report include the use of administrative data (medical records, death certificates) codes rather than physician adjudication of stroke events, lack of smoking status, and less complete follow-up for blacks.9
Incidence data for comparing rates for blacks and whites from the studies that included physician review of stroke cases have been recently summarized.17 Data from the Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS), one of the largest population-based surveillance studies of black–white differences in clinically reviewed stroke incidence cases, used the community socioeconomic status (SES) measure of percentage below poverty to examine the contribution of SES to the black–nonblack differences in incident stroke.13 Lower (poorer) community SES was found to be significantly associated with higher stroke incidence, and this effect was similar for blacks and nonblacks (largely whites). The contribution of community SES to excess black stroke incidence was estimated to be 39%, leaving 61% unaccounted for, but they were unable to adjust for individual-level risk factors, including diabetes mellitus and hypertension, that may overlap with SES.13 The Atherosclerosis Risk in Communities (ARIC) study that included 4 geographical areas of the United States (only 2 had sufficient numbers of blacks) showed that the addition of educational status (a surrogate measure of SES) to the model adjusting for age, sex, hypertension, and diabetes mellitus decreased the black/white ischemic stroke incidence rate ratio from 1.57 (95% confidence interval, 1.18–2.09) to 1.38 (95% confidence interval, 1.01–1.89), a reduction of one-third, although the potential for differential effects by age was not examined.10
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study is a population-based national cohort study of 30 239 community-dwelling individuals aged ≥45 years at enrollment in 2003–2007 that was designed to investigate factors associated with the excess stroke mortality of residents of the stroke belt region and that of blacks compared with whites.16 Follow-up is ongoing with physician adjudication of suspected stroke events. On the basis of follow-up through May 2010, data from REGARDS have shown that black–white patterns in stroke incidence are similar to national patterns of stroke mortality, suggesting that black–white disparities in stroke incidence play a role in black–white stroke mortality disparities.17 However, the magnitude of the disparities in stroke incidence is only approximately half of the mortality disparity, suggesting that stroke incidence only partially explains the black–white mortality disparities and that racial disparities in case fatality also may be contributing to disparities in mortality. However, data from the GCNKSS show a higher stroke incidence in blacks than in whites but a similar case fatality.11,19
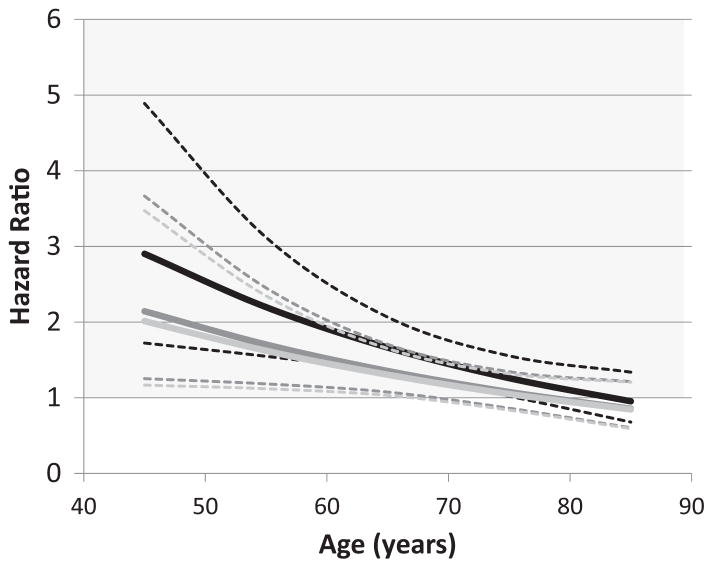
Using an approach similar to the work by Giles et al9 reporting the National Health and Nutrition Examination Survey follow-up data, further analyses of REGARDS data were conducted to determine whether blacks were still at higher risk for stroke than whites after adjusting for the traditional stroke risk factors (ie, variables in the Framingham Stroke Risk Score: age, sex, systolic blood pressure, use of antihypertensive medications, current smoking status, history of heart disease, diabetes mellitus, left ventricular hypertrophy, and atrial fibrillation)20,21 and SES, defined by annual household income and education. Of the analytic sample of 25 714 participants, 40% were black. Blacks were younger and had higher prevalence of antihypertensive medication use, diabetes mellitus, left ventricular hypertrophy, smoking, and lower SES than whites. Similar to findings from National Health and Nutrition Examination Survey follow-up, after adjustment for the Framingham risk factors, there was substantial attenuation of the black excess risk and it was further attenuated after adjustment for SES factors. The hazard ratio for incident stroke in blacks compared with whites at different ages is shown in the Figure. At ages <65 years, in which the black–white disparities in stroke risk are the greatest, the Framingham risk factors accounted for ≈40% of the excess risk in blacks; with the addition of SES factors, this was increased to ≈50%. Of the individual risk factors, systolic blood pressure had the most powerful effect on the black–white stroke risk, accounting for ≈50% of the combined Framingham risk factor effect. The next largest contributing factors were use of antihypertensive medications and diabetes mellitus, each accounting for ≈25% to 33% of the combined risk factor effect.22 Although the risk factor and SES adjustment accounted for approximately one-half of the disparity in the REGARDS cohort, the other half of the excess stroke incidence in the cohort must be attributable to other sources or factors. This same report suggested that the other potential contributors to the black–white disparity in stroke risk could potentially be arising from (1) a racial difference in the impact of risk factors, with the presence of risk factors having a larger impact on blacks than whites; (2) residual confounding from incomplete assessment of these traditional risk factors, in which, for example, characterizing hypertension with systolic blood pressure and medication use fails to capture other aspects such as the duration of the condition or diurnal variations in blood pressure; (3) novel risk factors such as inflammation, psychosocial factors, and others; and (4) measurement error in the predictive factors in the model.22 Very promising efforts are underway investigating these potential pathways, in which, for example, there seems to be a differential impact of elevated blood pressure on blacks, with a 3-times larger increase in stroke risk among blacks than whites for the same magnitude difference in systolic blood pressure.23
Figure.
Estimated black/white hazard ratio as a function of age and covariate adjustment. Black lines show hazard ratio and 95% confidence limits after adjustment for sex; dark gray lines show hazard ratio and 95% confidence limits after further adjustment for Framingham stroke risk factors; and light gray lines show hazard ratio and 95% confidence limits after further adjustment for socioeconomic status factors.
Although the black–white disparities in stroke have been known for at least a half century, only recently has the pace of scientific investigations increased. Understanding the causes of these immense disparities is the first step to design and implement interventions to reduce the unequal distribution of the public health burden of stroke.
Acknowledgments
Sources of Funding
The REGARDS study was supported by cooperative agreement NS 041588 from the National Institute of Neurological Disorders and Stroke.
Footnotes
Disclosures
None.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics—2012 Update: A Report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. Health, United States. With Special Features on Socioeconomic Status and Health. Hyattesville, MD: National Center for Health Statistics; 2012. 2011. [Google Scholar]
- 3.Wylie CM. Death statistics for cerebrovascular disease: a review of recent findings. Stroke. 1970;1:184–193. doi: 10.1161/01.str.1.3.184. [DOI] [PubMed] [Google Scholar]
- 4.Oh SJ. Cerebrovascular diseases in Negroes. J Natl Med Assoc. 1971;63:93–98. [PMC free article] [PubMed] [Google Scholar]
- 5.Heyman A, Karp HR, Heyden S, Bartel A, Cassel JC, Tyroler HA, et al. Cerebrovascular disease in the biracial population of Evans County, Georgia. Stroke. 1971;2:509–518. doi: 10.1161/01.str.2.6.509. [DOI] [PubMed] [Google Scholar]
- 6.Ostfeld AM. Heart disease and stroke in an elderly welfare population. Bull N Y Acad Med. 1973;49:458–466. [PMC free article] [PubMed] [Google Scholar]
- 7.Stallones RA, Dyken ML, Fang HCH, Heyman A, Seltser R, Stamler J. Report of the Joint Committee for Stroke Facilities. I. Epidemiology for stroke facilities planning. Stroke. 1972;3:359–371. [PubMed] [Google Scholar]
- 8.Kittner SJ, White LR, Losonczy KG, Wolf PA, Hebel JR. Black-white differences in stroke incidence in a national sample. The contribution of hypertension and diabetes mellitus. JAMA. 1990;264:1267–1270. [PubMed] [Google Scholar]
- 9.Giles WH, Kittner SJ, Hebel JR, Losonczy KG, Sherwin RW. Determinants of black-white differences in the risk of cerebral infarction. The National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Arch Intern Med. 1995;155:1319–1324. [PubMed] [Google Scholar]
- 10.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 11.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, et al. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 12.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleindorfer DO, Lindsell C, Broderick J, Flaherty ML, Woo D, Alwell K, et al. Impact of socioeconomic status on stroke incidence: a population-based study. Ann Neurol. 2006;60:480–484. doi: 10.1002/ana.20974. [DOI] [PubMed] [Google Scholar]
- 14.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 15.Sacco RL, Boden-Albala B, Abel G, Lin IF, Elkind M, Hauser WA, et al. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke. 2001;32:1725–1731. doi: 10.1161/01.str.32.8.1725. [DOI] [PubMed] [Google Scholar]
- 16.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 17.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillum RF. Risk factors for stroke in blacks: a critical review. Am J Epidemiol. 1999;150:1266–1274. doi: 10.1093/oxfordjournals.aje.a009957. [DOI] [PubMed] [Google Scholar]
- 19.Kleindorfer D. Sociodemographic groups at risk: race/ethnicity. Stroke. 2009;40(3 Suppl):S75–S78. doi: 10.1161/STROKEAHA.108.534909. [DOI] [PubMed] [Google Scholar]
- 20.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 21.D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25:40–43. doi: 10.1161/01.str.25.1.40. [DOI] [PubMed] [Google Scholar]
- 22.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half full (empty?) glass. Stroke. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med 2012. 2013;173:46–51. doi: 10.1001/2013.jamainternmed.857. [DOI] [PMC free article] [PubMed] [Google Scholar]