Editor’s note:
The gut-brain axis—an imaginary line between the brain and the gut—is one of the new frontiers of neuroscience. Microbiota in our gut, sometimes referred to as the “second genome” or the “second brain,” may influence our mood in ways that scientists are just now beginning to understand. Unlike with inherited genes, it may be possible to reshape, or even to cultivate, this second genome. As research evolves from mice to people, further understanding of microbiota’s relationship to the human brain could have significant mental health implications.
As a scientist, I often find myself chatting with friends and neighbors about the latest advances in neuroscience. In the past few years I have found more and more people asking about microbiota—the microorganisms that typically inhabit a bodily organ. In the last 10 years, I’ve been one of many neuroscientists advancing new ideas about how microbiota in the gut affects brain function. The media has taken notice as well. Recent stories on the gut-brain axis—among the most exciting new frontiers in neuroscience—include “Some of My Best Friends Are Germs” in the New York Times Magazine and “Gut Microbes Contribute to Mysterious Malnutrition” in National Geographic. In 2012, the editors of Science thought the research important enough to devote a special issue to the topic.
Why is the issue so fascinating? For one thing, it’s heightened consciousness of how diet and nutrition impact our health. For another, it’s sheer numbers. Our brains contain billions of neurons, but we less often talk about the fact that trillions of “good” bacteria are alive and well in our intestinal tracts. Remarkably, these naturally occurring, ever-present commensal bacteria may be instrumental in how our brain develops, how we behave, react to stress, and respond to treatment for depression and anxiety.
With such serious mental health implications to consider, there is substantial buzz among neuroscientists about the bidirectional nature of these seemingly infinite relationships. I am continually impressed by the creative ways that my colleagues are making discoveries, especially in how microbiota may influence the brain and the immune system during early life. And just last week researchers at UCLA found that regularly eating yogurt with probiotics, which contain “good” bacteria, seems to affect brain functioning in women.
Ups and Downs
Scientists have recognized communication between the brain and the gut for more than 100 years, with studies in the early 19th and 20th centuries showing that a person’s emotional state can alter the function of the gastrointestinal (GI) tract.1–3 One of the best examples is the work of William Beaumont, an army surgeon, who became known as the “Father of Gastric Physiology.” In the 1830s, Beaumont, who was able to monitor gastric secretions through a fistula (a permanent opening in the stomach wall), noted an association between changing moods and gastric secretions. In the mid-to-late 1900s, research examining stress biology and its impact on human health uncovered clear connections between an individual’s stress response and gut function. This classical view of top-down control—that is, the brain’s ability to control gut function—is supported by evidence revealing that the brain influences body systems, including the GI tract, through neural connections of the autonomic nervous system and through humoral systems in the bloodstream. Both of these communication pathways are activated in stressful situations and influence gut function. What is exciting and new is the consideration of bottom-up control—that is, how the gut, or more precisely the microbiota in the GI tract, can influence brain function. Researchers have recently shown that the presence of gut microbiota during early development influences the brain’s neural connectivity related to anxiety and depression. Gut microbiota has been linked to behavior, to stress, and to stress-related diseases. Changes in gut microbiota may influence risk of disease, and manipulating microbiota may provide novel ways to intervene in clinical situations related to mood and anxiety disorders.
The Inside Story
Normal commensal microbiota colonizes the mammalian gut and other body surfaces shortly after birth and remains there throughout an individual’s lifetime. In humans, the lower intestine contains 1014 to 1015 bacteria; that is, there are 10 to 100 times more bacteria in the gut than there are somatic cells in the human body.4 The interactions between commensal microbiota and its host are for the most part beneficial. In particular, the presence of commensal organisms is critical to immune function, nutrient processing, and other aspects of healthy physiology.5, 6 Using the latest molecular and genetic tools, researchers have shown that several bacterial phyla are represented in the gut and that commensal populations show considerable diversity, with as many as 1,000 distinct bacterial species involved.7 In addition, factors such as genetics, age, sex, and diet continually influence the composition and profile of an individual’s microbiota. 8, 9 In healthy people, there is considerable variability in gut bacterial composition, and yet if the same person’s gut bacteria are examined at different times (a few months or more apart), they hardly change.4, 10, 12 But in stressful situations, or in response to physiological or diet changes, the microbiota profile may itself change, creating an imbalance in host-microbiota interactions. Such changes can affect the person’s health.
Seeing the Light
Gut microbiota are important to healthy brain development. In particular, microbiota may influence the development of brain regions involved in our response to stress and control stress-related conditions such as anxiety and depression. In an attempt to understand these relationships, scientists manipulate gut bacteria in mice by raising germ-free mice in sterile isolators and then measuring the presence of gut bacteria. The isolator eliminates any exposure to outside air, contaminants, and commensal bacteria. Much of this work draws upon standard animal behavioral tests that measure activity, approach, and avoidance. Mice have a natural tendency to explore their environment while avoiding open and brightly lit areas. The elevated-plus maze, a behavioral apparatus that is elevated aboveground (Fig. 1), contains an area (with two closed and two open arms) for a mouse to explore. When a normal control mouse is placed in the maze, it tends to explore both arms but to spend most of its time in the closed one. When a germ-free mouse is removed from its sterile housing conditions and placed in the maze, it tends to spend significantly more time in the open arm. This suggests that mice without gut bacteria have low levels of anxiety-like behavior, since they spend more time in the aversive area of the testing apparatus.13, 14
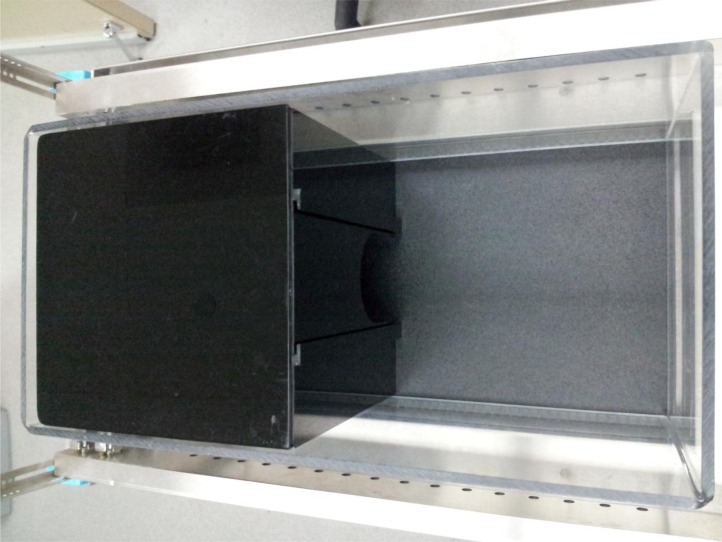
Figure 1:
The Elevated Plus Maze. This apparatus is elevated off the ground and consists of four black plexiglas arms in the shape of a plus. Two of the four arms are considered closed arms as they contain black plexiglas sides. The two open arms have small raised ledges situated along the perimeter. A test mouse is placed in the center of the apparatus and left to explore for five minutes. Infrared beams detect the placement and movement of the mouse. The elevated plus maze was connected to a computer that collected behavioral data using MotorMonitor software.
Another behavioral test uses the light-dark box, which has a dark, closed area connected to a light open area (Fig. 2). A normal control mouse explores both the light and the dark chambers with a preference for the darker one. However, germ-free mice spend more time in the light side of the apparatus, again demonstrating that mice without gut bacteria have low levels of anxiety-like behavior because the light chamber is considered the aversive region in this test, and germ-free mice spend more time in the light chamber.13, 15
Figure 2:
Light/dark Box. This apparatus—an automated infrared system containing clear a plexiglas activity chamber with a dark enclosed insert—is connected to a computer that records activity, also using MotorMonitor software. A test mouse is placed in the light side and left to explore for ten minutes. The small opening between the chambers allows access to both the light and dark chambers for the duration of the test.
Germ-free mice have helped researchers explore whether there are particular times over a mouse’s lifespan when microbiota-brain interactions are most important. Germ-free mice have been exposed to normal housing conditions at different times though their development. Exposure to normal housing conditions has revealed colonization of the sterile GI tract of germ-free mice with normal populations of gut bacteria. This also results in normalization of the undeveloped immune system that is present in germ-free mice. When adult germ-free mice were colonized with normal bacteria, they continued to show reduced anxiety-like behaviors, suggesting that the absence of gut bacteria early in development has a permanent effect on the brain wiring related to anxiety and exploratory behavior.14, 16 In contrast, when germ-free mice were colonized early in life as pups or during adolescence and then tested in adulthood, normal anxiety-like behavior was observed,13, 15 suggesting that microbiota influence the way the brain is wired early in development.17
In addition to studying mice, researchers have used antibiotic treatment to manipulate gut bacteria. Exposure to antibiotics in drinking water has been shown to lead to reduced numbers of gut bacteria in mice and to a reduction in the diversity of the bacterial population.18 Consistent with work in germ-free mice, mice exposed to antibiotics for a single week showed increased exploratory behavior and reduced anxiety-like behavior, an observation that was linked to changes in the bacterial profile.19 Two weeks following the end of the antibiotic treatment, both the bacterial profile and the behavior returned to normal, suggesting that transient changes in gut microbiota can influence behavior.19
On the Right Paths
Having established connections among gut bacteria, the brain, and behavior, it is intriguing to consider the ways that microbiota may communicate with the brain. Certainly, classical thinking tells us that there are neural connections from the body to the brain through peripheral nerves, and, in particular, the vagus nerve, which provides information from the gut to the brain. Evidence that bacteria in the GI tract can activate the vagus connection to the brain comes from work showing that administering food-borne pathogens, such as Citrobacter rodentium and Campylobacter jejuni, to mice activated vagal pathways and related brain regions.20, 21 This neural activation occurred in the absence of a peripheral immune response, suggesting the presence of a direct link between the bacteria in the gut and the nervous system. In a recent study, feeding healthy mice probiotics, or “good bacteria,” decreased anxiety-like and depressive-like behaviors compared to control mice,22 while a related study showed that feeding mice probiotics activates neurons in the hypothalamus, a brain region known to play a role in stress reactivity.23 In the latter study, the activation of neurons in the hypothalamus was greater when mice were fed infectious bacteria leading to a robust peripheral immune response. This suggests that both peripheral nerves and blood-borne immune signaling molecules can contribute to gut-brain communication.23 At the level of the hypothalamus, the brain’s autonomic nervous system control center, there is considerable evidence that psychological, physiological, and pathological challenges can activate the hypothalamus and turn on the body’s stress response. It is fascinating that the communication pathways from gut microbiota to the brain also lead to activation of this key brain region.
While the above-noted work establishes a neural pathway from the gut to the brain, a second important pathway for communication is the immune system. The immune system has two components, the innate immune system and the adaptive immune system. In germ-free mice, the adaptive immune system is undeveloped. Since gut microbiota are essential for immune system development, germ-free mice can be considered to have a low level of inflammation. When we consider the link between inflammation and anxiety-like behavior, we observe that a low inflammatory state is associated with low anxiety-like behavior, whereas higher levels of inflammation lead to increased anxiety-like behavior.17 For example, infection with the parasite Trichuris muris in mice results in gut inflammation and increased anxiety-like behavior.24 In addition, chemically induced gut inflammation in an animal model of colitis also results in gut inflammation and increased anxiety-like behavior.24 Evidence that the microbiota acts as a modulator of this immune-related increase in anxiety-like behavior is provided in the same reports stating that treatment with probiotic Bifidobacterium longum alleviated the anxiety-like behavior.24,25 These observations suggest that probiotic treatment may have potential for treatment of inflammation and related anxiety symptoms.
Commensal bacteria play an important role in maintaining the integrity of the intestinal tract, and in situations of stress or disease, increased intestinal permeability can contribute to increased inflammation.26, 27 Increased intestinal permeability, sometimes referred to as “leaky gut,” can lead to translocation of bacteria out of the lumen of the GI tract across the intestinal layer. This is an additional pathway that microbiota and pathogenic bacteria use to communicate with the brain via the immune system or through activation of local neurons in the enteric nervous system (ENS). The ENS is a part of the autonomic nervous system that is housed in the gut and is responsible for gut motility and other normal gut functions.28 It is a vast network of neurons that are the first points of contact for microbiota in the intestinal lumen and are an important component of the brain-gut axis.
The Stress Factor
One of the most common clinical features of depression is dysregulation of the stress response system, the hypothalamic-pituitary-adrenal (HPA) axis.29 As was previously noted, in response to psychological, physiological, and pathological challenges, neurons in the hypothalamus are activated and signal the pituitary to release adrenocorticotrophic hormone into the bloodstream, which in turn activates the adrenal gland to release the stress hormone cortisol. The stress response, or HPA activation, is part of our normal homeostatic processes, and yet, in depression, it is often overactive or, in some cases, underactive.29 One of the first studies considering stress and microbiota demonstrated that germ-free mice have an overactive stress response.23 A more recent study has shown that stress exposure during early life in rats disrupts the microbiota profile and leads to increased stress reactivity in adulthood.30 Importantly, in this study, treatment of rat pups with probiotic Lactobacillus sp. normalized stress hormone levels.30 Early-life stress also leads to increased depressive-like behavior in adult rats, and a similar study showed that treatment of rats exposed to stress during early life with the probiotic Bifiodo infantis reduced the depressive-like symptoms in adulthood.31 Overall these recent studies imply a link among microbiota imbalance, stress-related behaviors, and stress reactivity, and also suggest that probiotic treatment may be a good approach to treating stress-related symptoms.
To date, researchers have done little work related to stress and microbiota in humans, and in particular, there have been no studies that directly link microbiota to depression or anxiety. The most promising of the clinically related work shows that probiotic administration in people may have antidepressant or anxiety-reducing effects. In one study, healthy subjects were given probiotics for 30 days. Researchers used several questionnaires to test the effects of probiotics on stress, anxiety, depression, and coping. Their results showed that the probiotics group had less psychological stress than the control group did.32 In a separate study, researchers were able to show that healthy people with low mood at the beginning of the study showed improvement in mood following probiotic administration for three weeks.33 Finally, in a clinical study on individuals with chronic fatigue syndrome, administration of probiotics over a two-month trial resulted in fewer anxiety-related symptoms.34 These studies show that clinical trials to date support a role for microbiota in anxiety and depression, and also demonstrate the potential for treatment with probiotics.
Moving Forward
There is no doubt that research in the last decade has established a link between gut microbiota and brain function in mice. We have learned several things: (1) gut microbiota are a large population that is important to healthy metabolism and brain function, (2) gut-brain communication pathways include neural connections, (3) gut microbiota are significant during early development and can influence the wiring of stress circuitry in the brain, and (4) probiotics, or “good bacteria,” have been shown in animal and human studies to have a beneficial impact on mood symptoms. While these findings are both exciting and promising, we should not make the mistake of thinking that we have found the answers to all clinical situations related to mood. Microbiota—certainly an important modulator of health—must be considered as one component of a complex, multifaceted communication system needed to establish a healthy balance for brain development and function. The research is flourishing across the world as scientists strive to learn more. Stay tuned.
References
- 1.Barden N. Implication of the hypothalamic-pituitary-adrenal axis in the physiopathology of depression. J Psychiatry Neurosci. 2004;29:185–193. [PMC free article] [PubMed] [Google Scholar]
- 2.Beaumont W. Experiments and observations on the gastric juice and the physiology of digestion. Plattsburg: F.P. Allen; 1833. [DOI] [PubMed] [Google Scholar]
- 3.Bech-Nielsen GV, Hansen CH, Hufeldt MR, Nielsen DS, Aasted B, Vogensen FK, Midtvedt T, Hansen AK. Manipulation of the gut microbiota in C57BL/6 mice changes glucose tolerance without affecting weight development and gut mucosal immunity. Res Vet Sci. 2011 doi: 10.1016/j.rvsc.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Benton D, Williams C, Brown A. Impact of consuming a milk drink containing a probiotic on mood and cognition. European journal of clinical nutrition. 2007;61:355–361. doi: 10.1038/sj.ejcn.1602546. [DOI] [PubMed] [Google Scholar]
- 5.Bercik P, Denou E, Collins J, Jackson W, Lu J, Jury J, Deng Y, Blennerhassett P, Macri J, McCoy KD, et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011a;141:599–609. 609, e591–593. doi: 10.1053/j.gastro.2011.04.052. [DOI] [PubMed] [Google Scholar]
- 6.Bercik P, Park AJ, Sinclair D, Khoshdel A, Lu J, Huang X, Deng Y, Blennerhassett PA, Fahnestock M, Moine D, et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol Motil. 2011b;23:1132–1139. doi: 10.1111/j.1365-2982.2011.01796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bercik P, Verdu EF, Foster JA, Macri J, Potter M, Huang X, Malinowski P, Jackson W, Blennerhassett P, Neufeld KA, et al. Chronic gastrointestinal inflammation induces anxiety-like behavior and alters central nervous system biochemistry in mice. Gastroenterology. 2010;139:2102–2112. e2101. doi: 10.1053/j.gastro.2010.06.063. [DOI] [PubMed] [Google Scholar]
- 8.Bravo JA, Forsythe P, Chew MV, Escaravage E, Savignac HM, Dinan TG, Bienenstock J, Cryan JF. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A. 2011;108:16050–16055. doi: 10.1073/pnas.1102999108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cannon WB. The influence of emotional states on the functions of the alimentary canal. Am J Med Sci. 1909;137:480–487. [Google Scholar]
- 10.Clarke G, Grenham S, Scully P, Fitzgerald P, Moloney RD, Shanahan F, Dinan TG, Cryan JF. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2012 doi: 10.1038/mp.2012.77. [DOI] [PubMed] [Google Scholar]
- 11.Costello EK, Lauber CL, Hamady M, Fierer N, Gordon JI, Knight R. Bacterial community variation in human body habitats across space and time. Science. 2009;326:1694–1697. doi: 10.1126/science.1177486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desbonnet L, Garrett L, Clarke G, Kiely B, Cryan JF, Dinan TG. Effects of the probiotic Bifidobacterium infantis in the maternal separation model of depression. Neuroscience. 2010;170:1179–1188. doi: 10.1016/j.neuroscience.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305–312. doi: 10.1016/j.tins.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Furness JB. The enteric nervous system and neurogastroenterology. Nature reviews Gastroenterology & hepatology. 2012;9:286–294. doi: 10.1038/nrgastro.2012.32. [DOI] [PubMed] [Google Scholar]
- 15.Gareau MG, Jury J, MacQueen G, Sherman PM, Perdue MH. Probiotic treatment of rat pups normalises corticosterone release and ameliorates colonic dysfunction induced by maternal separation. Gut. 2007;56:1522–1528. doi: 10.1136/gut.2006.117176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gareau MG, Silva MA, Perdue MH. Pathophysiological mechanisms of stress-induced intestinal damage. Current molecular medicine. 2008;8:274–281. doi: 10.2174/156652408784533760. [DOI] [PubMed] [Google Scholar]
- 17.Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, Gordon JI, Relman DA, Fraser-Liggett CM, Nelson KE. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312:1355–1359. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goehler LE, Park SM, Opitz N, Lyte M, Gaykema RP. Campylobacter jejuni infection increases anxiety-like behavior in the holeboard: possible anatomical substrates for viscerosensory modulation of exploratory behavior. Brain Behav Immun. 2008;22:354–366. doi: 10.1016/j.bbi.2007.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heijtz RD, Wang S, Anuar F, Qian Y, Bjorkholm B, Samuelsson A, Hibberd ML, Forssberg H, Pettersson S. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci U S A. 2011;108:3047–3052. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hooper LV, Wong MH, Thelin A, Hansson L, Falk PG, Gordon JI. Molecular analysis of commensal host-microbial relationships in the intestine. Science. 2001;291:881–884. doi: 10.1126/science.291.5505.881. [DOI] [PubMed] [Google Scholar]
- 21.Jumpertz R, Le DS, Turnbaugh PJ, Trinidad C, Bogardus C, Gordon JI, Krakoff J. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am J Clin Nutr. 2011;94:58–65. doi: 10.3945/ajcn.110.010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474:327–336. doi: 10.1038/nature10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyte M, Li W, Opitz N, Gaykema RP, Goehler LE. Induction of anxiety-like behavior in mice during the initial stages of infection with the agent of murine colonic hyperplasia Citrobacter rodentium. Physiol Behav. 2006;89:350–357. doi: 10.1016/j.physbeh.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 24.Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol. 2004;4:478–485. doi: 10.1038/nri1373. [DOI] [PubMed] [Google Scholar]
- 25.Messaoudi M, Violle N, Bisson JF, Desor D, Javelot H, Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut microbes. 2011;2:256–261. doi: 10.4161/gmic.2.4.16108. [DOI] [PubMed] [Google Scholar]
- 26.Neufeld KA, Kang N, Bienenstock J, Foster JA. Effects of intestinal microbiota on anxiety-like behavior. Commun Integr Biol. 2011a;4:492–494. doi: 10.4161/cib.4.4.15702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neufeld KM, Kang N, Bienenstock J, Foster JA. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol Motil. 2011b;23:255–264. e119. doi: 10.1111/j.1365-2982.2010.01620.x. [DOI] [PubMed] [Google Scholar]
- 28.Pavlov I. The work of digestive glands. London: Griffen; 1910. [English translation from Russian by W. H. Thompson.] [Google Scholar]
- 29.Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, Nielsen T, Pons N, Levenez F, Yamada T, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rao AV, Bested AC, Beaulne TM, Katzman MA, Iorio C, Berardi JM, Logan AC. A randomized, double-blind, placebo-controlled pilot study of a probiotic in emotional symptoms of chronic fatigue syndrome. Gut Pathog. 2009;1:6. doi: 10.1186/1757-4749-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schloissnig S, Arumugam M, Sunagawa S, Mitreva M, Tap J, Zhu A, Waller A, Mende DR, Kultima JR, Martin J, et al. Genomic variation landscape of the human gut microbiome. Nature. 2013;493:45–50. doi: 10.1038/nature11711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serino M, Chabo C, Burcelin R. Intestinal MicrobiOMICS to define health and disease in human and mice. Current pharmaceutical biotechnology. 2012;13:746–758. doi: 10.2174/138920112799857567. [DOI] [PubMed] [Google Scholar]
- 33.Sudo N, Chida Y, Aiba Y, Sonoda J, Oyama N, Yu XN, Kubo C, Koga Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol. 2004;558:263–275. doi: 10.1113/jphysiol.2004.063388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teitelbaum AA, Gareau MG, Jury J, Yang PC, Perdue MH. Chronic peripheral administration of corticotropin-releasing factor causes colonic barrier dysfunction similar to psychological stress. Am J Physiol Gastrointest Liver Physiol. 2008;295:G452–459. doi: 10.1152/ajpgi.90210.2008. [DOI] [PubMed] [Google Scholar]