Abstract
Mesenchymal stem cells (MSCs) were first isolated more than 50 years ago from the bone marrow. Currently MSCs may also be isolated from several alternative sources and they have been used in more than a hundred clinical trials worldwide to treat a wide variety of diseases. The MSCs mechanism of action is undefined and currently under investigation. For in vivo purposes MSCs must be produced in compliance with good manufacturing practices and this has stimulated research on MSCs characterization and safety. The objective of this review is to describe recent developments regarding MSCs properties, physiological effects, delivery, clinical applications and possible side effects.
Keywords: Mesenchymal stem/stromal cells, cell therapy, graft versus host disease, immunomodulatory properties, regenerative medicine, advanced therapy medicinal product, transplantation, MSCs sources.
1. INTRODUCTION
The presence of non-hematopoietic stem cells in bone marrow as observed by Cohnheim more than 140 years ago [1] has been then confirmed by other studies that clearly showed that bone marrow (BM) contains cells that can differentiate into fibroblasts, as well as into other cells of mesodermal origin [2].
In post-natal tissue, it has been shown that mesenchymal stem cells (MSCs) are localized in a “vascular niche” in the wall of large or in medium-size vessels of every organ and tissue of the body [3]. Their localization in the vascular wall probably originates during embryogenesis. In fact, immature vascular progenitor cells, i.e. angioblasts migrate from somites to the embryonic dorsal aorta [4]. It is possible that during the process of vessels maturation, some of these vascular mesenchymal cell progenitors remain entrapped within the vessel wall [5]. Their persistence in the vascular system, even after birth, may suggest a role for these cells in controlling vessel integrity; they could also compensate for the continuous post-natal mechanical forces and shear stress on vassels. Further-more, vascular damage is induced by many human disorders
(cancer, atherosclerosis, inflammation, aneurysmal dilatation, vascular stenosis and others) and the in situ presence of MSCs may contribute to the vascular regenerative process.
Since 2001, when the European Directive 2001/83/CE relating to medicinal products for human use was approved, products for advanced medicinal therapy (AMT), used for gene therapy, somatic cell therapy and for tissue engineering, have been considered as drugs. Each of these products has specific pharmacologic, metabolic and immunologic activities and the potential for treating a variety of disorders. For these reasons cellular products for AMT must meet the same stringent conditions required for drugs before they are placed on the market, in particular their activity, efficacy, safety and required dose must be defined. Furthermore they must be manipulated according to Good Manufacturing Practices (GMP) and they require testing in approved clinical trials before being commercialized.
In the last decade, MSCs have attracted great interest due to the numerous applications proposed for their use. However, as AMT products, they must satisfy all the above mentioned requirements. Details concerning the European regulatory directives are reported in chapter 9.
The term “mesenchymal stem cells” initially referred to multi-lineage progenitor cells isolated and culture-expanded from human adult BM. However, in order to better describe and define the direction of MSCs research, recent findings on MSCs cell features call for an adaptation of the nomenclature. The first issue is that this class of cells can be isolated from almost every vascularized tissue; this is related to the fact that every blood vessel in the body has mesenchymal cells in abluminal locations that are summarily called pericytes. This observation led to the suggestion that MSCs are pericytes [6]. Moreover, it has been clearly demonstrated that MSCs home to sites of inflammation or tissue injury and secrete considerable levels of both immunomodulatory and trophic agents. This indicates that their therapeutic capacities are not associated with the ability of MSCs to differentiate into different end-stage mesenchymal cell types and thus the term “stem” is not essential to describe these cells. Together with evidence that MSCs are highly heterogeneous and consist of several subpopulations with varying differentiation potentials [7], the term “mesenchymal stromal cells”, was proposed with reference to their stromal origin. Very recently Caplan, followed by other notable researchers, proposed a further adjustment in the term MSCs. Considering that MSCs multipotency is not the key aspect of their current therapeutic use, MSCs should be an acronym for “medicinal signaling cells” [6], focusing on their secretive paracrine activities.
For the purposes of this review and for the sake of simplification, the acronym MSCs is generically used to identify this class of cells. Indeed, although the powerful immunomodulatory and trophic functions of MSCs deserve further investigation to improve their therapeutic use, in our opinion the MSCs multipotency is still an important aspect for tissue engineering strategies.
Herein, we provide background in order to direct future studies on MSCs, considering them as drugs and thus discussing their physiological effects, delivery, clinical applications and possible side effects.
2. IDENTITY DOCUMENT OF MSCs
Despite the exhaustive number of studies conducted to characterize MSCs by their surface antigen expression profile, variability still exists within MSCs populations. Markers are useful can be of help to establish the homogeneity of a population of mature cells, whereas they may be less informative to study a stem cell population. The International Society for Cellular Therapy (ISCT) proposed three minimal criteria to identify MSCs: 1) adherence to plastic; 2) specific surface antigen expression (positivity for CD105, CD73,CD90 and negative for CD45, CD34, CD14 or CD11b, CD79a or CD19 and HLA class II); 3) multipotent capacity to differentiate into osteoblasts, adipocytes or chondroblasts under standard in vitro differentiating conditions [8]. However, in addition to these minimal criteria and to have a more precise, although complicated, picture, we should assume that adult human MSCs are also positive for several other markers as reported in (Table 1) [8-7].
Table 1.
Markers for the Identification of BMSCs
| Positive selection | Negative selection | |
|---|---|---|
| CD9 | CD119 | CD11a |
| CD10 | CD120a | CD14 |
| CD13 | CD120b | CD15 |
| CD29 | CD121 | CD18 |
| CD44 | CD123 | CD19 |
| CD49a | CD124 | CD25 |
| CD49b | CD126 | CD31 |
| CD49c | CD127 | CD34 |
| CD49d | CD140a | CD40 |
| CD49e | CD166 (ALCAM) | CD45 |
| CD51 | CD271 | CD50 |
| CD54 (ICAM-1) | CCR1 | CD56 |
| CD58 | CCR4 | CD62E |
| CD61 | CCR7 | CD62P |
| CD62L | CXCR5 | CD80 |
| CD71 | CCR10 | CD86 |
| CD73 | F9- 3C2F1, | CD117 |
| CD90 | HEK-3D6 | HLA-II |
| CD102 | STRO-1 | |
| CD104 | HER-2/erbB2 | |
| CD105 | Frizzled 9 | |
| CD106 (V-CAM1) | GD2 | |
According to some authors, MSCs should also express embryonic stem cell markers, such as Oct-4, Rex-1, and Sox-2, for at least 10 passages [18]. Based on the above markers, many techniques for the isolation of MSCs using antibody selection have been recently developed. Some methods use negative selection to enrich the MSCs cell population (by removing cells from the hematopoietic lineage); other methods positively select MSCs by using specific antibodies [14, 15].
The main reason for the marker expression variability are due to the source of MSCs (see chapter 3 - Source of isolation) and/or the different stages of culture [19].
MSCs surface marker expression may also be influenced by the method of isolation. Furthermore, a very important cause of differences in marker expression is due to stimulation by cytokines or growth factors secreted by contaminant cell populations present at the first stage of culture. This indicates that in vitro expression of MSCs markers may not correlate with their expression patterns in vivo.
All the above considerations indicate that mesenchymal precursor cells are phenotypically very heterogeneous. This is a very crucial point because, as also stated by Boheler [20], it involves the survival and homing capacity of the cells to host tissues following transplantation, and the differentiation potential of these cells in vivo. In a recent study, it has been shown that also fibroblasts possess multi-lineage differentiation capacity, albeit less than MSCs [21]. This confirms previous data on the fibroblast differentiation potential [22] and underlines the necessity to find additional functional features to better characterize MSCs. In the same study, it was also observed that MSCs retained strong angiogenic properties, whereas fibroblasts were much less angiogenic. Thus it has been proposed that additional and more distinctive MSCs markers, namely those indicating capacity to affect angiogenesis should be included [21]. The property of MSCs to induce angiogenesis is well-known, suggesting that their therapeutic efficacy in several diseases, including ischemia, can be attributed mostly to their angiogenic potential [23, 24]. For these reasons, the evaluation of MSCs angiogenic capacity is not only important for a better functional characterization of these cells, but it could also be useful to predict their effectiveness in clinical applications in tissue regenerative therapies.
3. SOURCES OF ISOLATION
Although BM is still the most common source of MSCs, in the last two decades there has been a continuous effort to identify alternative sources of MSCs, mainly driven by a constant quest for a “more convenient” source. Therefore, MSCs have been found particularly in tissues that are discarded, such as fat from liposuction, deciduous teeth, or placenta and umbilical cord. A second driving force for an alternative source to BM has been the quest for a “superior” source of MSCs. However, MSCs isolated from BM, adipose tissue and fetal annexes using standardized isolation and culture protocols, seem to show comparable features [25]. Thus today, it is still unclear which tissue source for MSCs recovery is optimal for a given clinical situation.
The question whether MSCs obtained from different sources are the same cells has long been debated and opinions are still conflicting. Several studies have investigated MSCs isolated from different sources in order to compare their morphology, frequency of colony formation, expansion characteristics, multilineage differentiation capacity, immunophenotype, and success rate of isolating the cells. It has been demonstrated that all cells isolated from adipose tissue, bone marrow and umbilical cord blood exhibit a similar fibroblastoid morphology, formation of CFU-F, multi-potential differentiation capability and expression of a typical set of surface proteins, with the exception of CD105 and CD106, described to be associated with hematopoiesis and cell migration, which were differently expressed: a significant reduction was observed in umbilical cord cells and in adipose tissue, respectively [26]. In the same study the authors demonstrated that umbilical cord blood MSCs were not able to differentiate toward the adipogenic lineage. The debate on the differentiation ability of these types of MSCs continues and very conflicting data are published in the literature. [27-29]. Some studies show that adipose-derived MSCs are more angiogenic than bone marrow-derived cells (BMSCs) [30], display their proliferative capacity for long period [26, 31] and retain for longer time their adipogenic capacity [18, 32]. The immu-nosuppressive properties of ASCs seem to be superior to BMSCs [33, 34]. Although the underlying mechanisms of all these differences are not known, several studies have shown that MSCs and ASCs exhibit differences in their proteomic and transcriptomic profile [18, 35, 36] that might justify the differences between MSC and ASC.
However, it is really difficult to make a comparison since there are several variables that may strongly influence MSCs in culture.
3.1. Bone Marrow-derived MSCs
To date most knowledge on MSCs derives from studies performed on bone marrow-derived MSCs (BMSCs). For this reason, very often BMSCs serve as a “positive control” for MSCs isolated from other tissues.
The number of MSCs that can be isolated from a tissue is variable. From a clinical perspective it is relevant that a large number of cells are collected, in particular when unexpanded MSCs are utilized [37, 38]. A limited number of MSCs are contained in BM: according to Muschler [39] in humans an average of 1/18,000 mononuclear cells are MSCs, therefore considering that there are about 65x106 mononuclear cells (MNCs) for every ml of BM, in whole bone marrow there are only 3555 MSCs/ml. Obviously, this is an approximate number: indeed, in addition to the large inter-donor variability, the technique used to harvest BM and technique used to isolate the mononuclear fraction can greatly influence the number of MSCs that can be isolated from a sample. The aspiration technique and volume of BM harvested must be taken into account in order to reduce peripheral blood contamination. Several authors have evaluated the influence of BM volume aspiration on MNCs and BMSCs yield. It was already shown that the concentration of MNCs in peripheral blood is much lower than that in BM [40]. For this reason, some authors recommended collecting just 2 ml of BM before changing the harvest site in order to avoid dilution of BM with peripheral blood. Several methods have been described for isolating MSCs from BM, including immune-magnetic beads, density gradient separation and direct BM plating. Currently, the standard method for isolating BMSCs is based on density gradient centrifugation. Several studies report comparisons between different density gradient media and demonstrate conflicting results. While some authors found no influence on composition and quality of the isolated BMSCs [41], others demonstrated that the choice of different protocols affects cell yield and quality [42, 43]. In general, a valid cell separation process should guarantee a pure, highly viable population of MNCs with minimal contamination with red blood cells and granulocytes, while maintaining optimum functional capacity.
3.2. Adipose-Tissue Derived MSCs
Like BM, adipose tissue derives from the mesenchyme and consists of a highly complex system containing different cell populations, including mature adipocytes, pre-adipocytes, fibroblasts, vascular smooth muscle cells, endothelial cells and adipose-derived stem cells (ASCs). Lipoaspirates from aesthetic surgery are usually discarded and for this reason, together with their large availability, accessibility, and ease of procurement with minimal discomfort for the patient under local anesthesia, adipose tissue could represent an ideal source of progenitor cells. ASCs are adult mesenchymal stromal/stem cells that can be easily isolated by a simple collagenase I-based isolation procedure which is able to digest the matrix and yields the so-called stromal vascular fraction (SVF) [44, 45]. It contains several cell populations, including ASCs, which are then usually further purified by plastic adherence. ASCs are similar to BMSCs regarding morphology, immunophenotype and colony frequency [26]. Indeed they possess the ability to self-renew, express a very similar immunophenotypic pattern and are able to differentiate into several cell lineages of mesodermal origin, i.e. adipocytes, chondrocytes and osteoblasts [11, 44, 46, 47]. Moreover, it has been also shown that they are able to trans-differentiate into cells of endodermic and ectodermic origins, such as neuronal-like cells, endocrine pancreatic cells, hepatocytes, epithelial cells and cardiomyocytes [48-53]. However, ASCs and BMSCs show slight differences in their expression of particular markers: CD49d and CD34 are expressed on ASCs but not on BMSCs, whereas CD106 is expressed on BMSCs but not on ASCs. In BM, CD106 expression may be functionally associated with hematopoiesis, stem cell homing and proliferation, whereas adipose tissue-derived cells do not need this molecule since they belong to non hematopoietic tissue.
3.3. Placenta-derived MSCs
Besides its fundamental functions in nutrition and protection of the developing fetus in the womb and its role in fetomaternal tolerance, human placenta has recently attracted wide attention also as a valuable source of stem/progenitor cells. A significant advantage of placenta as stem/progenitor cell source is its readly availability. Indeed this organ is easily procured without invasive procedures at delivery and its use is free of ethical concerns, considering that it would normally be discarded as biological waste.
The placenta is an organ consisting of a fetal (fetal membranes, chorionic plate and umbilical cord) and a maternal component (decidua). MSCs have been isolated from both fetal and maternal tissues, and in particular: i) from amnio chorionic fetal membranes [54-57]; ii) from the chorionic villous stroma of first-trimester placenta [58] and term placenta [55, 59], although isolation of these cells might be affected by contamination with maternal cells [60], so that the fetal origin has to be demonstrated with methods sensitive enough to detect less than 1% maternal cells [57]; iii) from at least five compartments of the umbilical cord: the umbilical cord blood, the umbilical vein subendothelium, and three regions of Wharton’s jelly, i.e. the perivascular zone, the intervascular zone, and the subamnion [61]; iv) from different regions of the decidua [55]. Placental MSCs meet all the ISCT basic criteria, since they are plastic adherent, they show a specific MSCs pattern of surface antigens [57, 58, 61, 62], and under specific culture conditions in vitro, placental MSCs exhibit multilineage differentiation capacity [58, 59, 63].
Placental MSCs have been reported to grow faster and more robustly, and have greater long-term growth ability than BMSCs [64]. Some differences between placental MSCs and BMSCs were also found in the expression of chemokine receptors and other surface molecules. Brooke and colleagues [65] revealed that although these cells display a similar pattern for these molecules, the placental cells express a much higher level of VCAM-1 ligand VLA-4 (CD49d) and a lower level of CCR1 and CXCR6. Other molecules such as CD56, CD10 and CD49d have been shown to be more highly expressed on placental MSCs [66].
MSCs from placental regions, like human BMSCs, are poor antigen-presenting cells due to their low or limited expression of MHC class II and costimulatory molecules [57]. It has been demonstrated that placenta-derived MSCs fail to induce an allogeneic T-cell response and inhibit lymphocyte proliferation induced by allo-antigens or via T cell receptor cross-linking, likely through mechanisms based on secretion of soluble factors [54, 67] and in a dose-dependent way [68].
Furthermore, amniotic membrane MSCs block differentiation and maturation of monocytes into dendritic cells, with a reduction in the production of inflammatory cytokines and production of high levels of Th2-related cytokines [69].With the same mechanism of cell cycle arrest in the G0/G1 phase, amniotic membrane-derived MSCs also exert an anti-proliferative effect on cancer cell lines [69].
3.4. Synovial Fluid-derived MSCs
Synovium-derived mesenchymal stem cells (SMSCs) are a good candidate for a cell-based product particularly intended to treat cartilage defects because they have superior chondrogenic differentiation properties compared with other cell types [70,71]. SMSCs can be easily harvested by arthroscopy with minimal pain and complication; in addition synovial tissue and synovial fluid can be easily regenerated because the synovial membrane possesses a high regenerative capability [72].
In particular, synovial fluid contains a population of MSCs that are consistently more chondrogenic in vitro, in comparison to BM- and adipose tissue-derived MSCs [73]. Although their exact role in homeostasis and repair of joint structures needs to be established, these cells have been demonstrated to contribute to the healing of ligament injury in a rabbit experimental model [74].
In general several joint structures (subchondral bone, synovium, cartilage, infrapatellar fat pad) have been shown to host resident MSCs [70, 73, 75].
3.5. Other MSCs Sources
Several other sources of MSCs have been identified in the last two decades. Although some of these sources seem promising for obtaining MSCs for clinical use, most, due to the low MSC yield and/or invasiveness of the harvesting procedure, do not encourage further investigation (Table 2).
Table 2.
Other Human MSCs Tissue Sources
| Tissue | Reference |
|---|---|
| Periostium | [76] |
| Pericytes | [77] |
| Dental pulp | [10] |
| Peripheral blood | [78] |
| Dermis | [79] |
| Trabecular bone | [80] |
| Infrapatellar pad | [75] |
| Muscle | [81] |
| Pancreas | [82] |
| Peridontal ligaments | [83] |
| Mestrual blood | [84] |
| Milk | [85] |
| Urinary tract | [86] |
4. IN VITRO MSCs EXPANSION: ALTERNATIVE METHODS
Due to the low frequency of mesenchymal progenitors in human tissues, MSCs in vivo use requires that the cells be extensively ex vivo manipulated to achieve numbers that are necessary for their clinical application [87]. MSCs are generally cultured, both under experimental and clinical grade conditions, in the presence of fetal.
calf serum (FCS) [88]. Nonetheless, the use of FCS raises concerns when utilized in clinical grade preparations, because of the theoretical risk of transmission of prions and agents responsible for still unidentified zoonoses, as well as the risk in causing immune reactions in the host with consequent rejection of the transplanted cells [89].
In view of these considerations, animal serum-free media have been investigated. Both autologous and allogeneic human serum have been tested for in vitro expansion of MSCs, and one group showed that autologous serum was superior to both FCS and allogeneic human serum in terms of proliferative capacity [90]. To reduce the amount of bovine antigens, a final 48-hour incubation with medium supplemented with 20% human serum, has been evaluated [89]. Several serum-free media, based on the use of cytokines and growth factors, such as basic fibroblast growth factor (b-FGF) and transforming growth factor beta (TGF-β), have also been tested under experimental conditions [91].
Platelet lysate (PL) has been demonstrated to be a powerful substitute for FCS in MSCs expansion, thanks to its high concentration of natural growth factors (GFs) [92, 93]. Lucarelli et al. and Doucet et al. first demonstrated that growth factors contained in PL are able to promote MSCs expansion in a dose-dependent manner [92, 94]. Bernardo et al. showed that a culture medium supplemented with 5% PL is superior to 10% FCS in terms of clonogenic efficiency and proliferative capacity of MSCs, therefore providing more efficient expansion, together with significant time savings [95]. Moreover, the in vitro immune regulatory properties of PL-expanded MSCs resulted to be comparable with those of MSCs cultured in the presence of FCS in terms of capacity to decrease alloantigen-induced cytotoxic activity, to promote differentiation of CD4+ T cell subsets expressing a Treg (regulatory T cells) phenotype, and to increase IL-6 production in culture supernatant [95]. Gene expression changes in long-term cultured PL-expanded MSCs resulted similar to those of MSCs expanded in the presence of FCS, suggesting that replicative senescence modifications develop in both cases, in the absence of malignant transformation [96]. Although PL seems to be a suitable substitute for FCS in the expansion of MSCs, further studies are needed to better understand the biological and functional properties, in vitro and in vivo, of PL-expanded MSCs, as compared with those cultured in the presence of FCS. Once these studies are successfully completed, PL might be introduced in routine preparation of MSCs to be employed for clinical application.
In the context of clinical use of MSCs, further issues related to the isolation/expansion protocols for cells to be utilized in different clinical situations should be taken into account. For example, recently, the importance of host factors, which seem to be capable of activating MSCs in order to mediate their immunomodulatory effects, has been underlined [97]. Along these lines, MSCs would not be constitutively inhibitory, but they could acquire their immunosuppressive functions after being exposed to an inflammatory environment [97]. The culture of cells in the presence of IFN-γ and/or other inflammatory cytokines, such as TNF-( and IL-1ß, could therefore be of value in some clinical contexts where a potent immunosuppressive effect of MSCs is desirable [98, 99].
MSCs also express a large number of toll-like receptors (TLRs) and their stimulation has been shown to affect MSCs immunomodulatory properties [100]. Analogously with the functional status of monocytes/macrophages, two functionally different MSCs populations have been identified: the TLR4-primed MSCs population which exhibits a pro-inflammatory profile (MSC1) and the TLR3-primed MSCs population which delivers immunosuppressive signals (MSC2). In accordance with this theory, T cell inhibition or activation could be obtained in different clinical situations thanks to the stimulation of specific TLR during ex vivo culture [101].
5. EVALUATION OF THE RISK OF MALIGNANT TRANSFORMATION OF IN VITRO EXPANDED MSCs
Cells propagated in vitro are in a proliferative state under non-physiologic conditions; this may cause accumulation of DNA damage, resulting in an increased risk for malignant transformation [102]. Moreover, after a variable number of cell divisions, in vitro expanded MSCs, like every normal somatic cell, enter a senescent state and ultimately stop proliferating. Several molecular pathways have been implicated in senescence, including DNA damage and progressive shortening of telomeres. It is well known that somatic cells may activate molecular mechanisms in an attempt to circumvent senescence. Remarkably, it has been hypothesized that escape from senescence, for instance by means of telomerase activity that counteracts telomere shortening, is a crucial step in malignant transformation [102].
In vitro and in vivo experimental studies have documented that murine MSCs are prone to malignant transformation [103]; moreover they may support tumor growth and metastatic spread [104]. On the contrary, spontaneous malignant transformation appears to be a rather exceptional event for human MSCs [105, 106]. Indeed, Rubio and co-workers [107] and Rosland and co-workers [108] have documented spontaneous malignant transformation in human MSCs expanded in vitro, but the results reported by both groups have subsequently been withdrawn, since it was demonstrated that spontaneous transformation reflected cross-contamination with established human immortalized cell lines [109, 110].
So far, tumor formation has not been reported in ongoing clinical trials using MSCs; however, it is worth considering that for many therapeutic applications, the use of allogeneic MSCs might promote effective elimination of transformed cells by the immune system, while an autologous setting might increase the risk of tumor formation [102]. It is also worth considering that a very recent systematic review of current clinical trials documented that MSCs therapy appears safe [111]. Nonetheless, the authors emphasize that further larger scale controlled clinical trials with rigorous reporting of adverse events are required to further define the safety profile of MSCs [111]. Consequently, MSCs expanded in vitro for clinical use have to be rigorously evaluated for the risk of malignant transformation. In our opinion, the appropriate quality control procedure to investigate this important issue should at least include: (i) release of MSCs expanded in a low number of passages (≤ 4), in an attempt to minimize the administration of senescent cells, (ii) careful evaluation of the morphology and proliferation pattern at each culture passage, and the phenotype of the final product (iii), demonstration of absence of genetic instability by molecular and conventional karyotyping, (iv) assessment of telomerase activity on the final product, considering that it has been documented that non-malignant human MSCs display a low/undetectable level of this enzymatic activity [112], (v) DNA fingerprinting by analysis of short tandem repeats to assess the donor identity of the final product, (vi) whenever feasible, expansion of a sizable aliquot of the MSCs lot cryopreserved for release for further 4-5 passages, in order to demonstrate the absence of transformed MSCs which could have been present at undetectable levels in earlier passages.
6. INSIGHTS INTO TISSUE REGENERATION MEDIATED BY MSCs
One of the features that makes the use of MSCs interesting in the clinical setting, is their ability to migrate to the damaged tissue or toward inflammatory sites after intravenous administration. Although the mechanism by which MSCs are able to migrate and home to sites of injury has not yet been elucidated, it is reasonable to assume that an increase in inflammatory chemokine concentration at the site of inflammation is the first key mediator of MSCs trafficking to the injury site. Since chemokine receptors and essential molecules for the transmigration of leukocytes from blood to tissue, such as integrins and selectins, are strongly expressed by MSCs, this could explain the MSCs mechanism of transport, homing, adhesion and transmigration across the endothelium [17, 113].
Although traditionally the MSCs regenerative capacity was associated with their presumptive plasticity, their therapeutic effects seem to be particularly due to their paracrine function through the secretion of a broad range of bioactive molecules. Their potential has been exploited in immunomodulation, angiogenesis, support of growth and differentiation of local stem and progenitor cells, chemo-attraction and anti-scarring and anti-apoptosis effects [16]. This points to MSCs as therapeutic agents even if they do not engraft or differentiate into tissue-specific cells, thus significantly increasing the range of MSCs therapeutic applications.
The number of molecules known to mediate the paracrine action of cultured MSCs is very high and new molecules involved in these processes are discovered every day. Anti-apoptosis is the first expected effect when MSCs are used to treat acute lesions; the principal bioactive molecules responsible for the anti-apoptotic effect are VEGF, HGF, IGF-I, stanniocalcin-1, TGFβ and GM-CSF [114]. The same molecules, in addition to PIGF, MCP-1, bFGF and IL-6 also stimulate local angiogenesis, which is particularly relevant during tissue re-organization [115]. Mitosis of tissue-intrinsic progenitors or resident stem cells has been demonstrated to be activated by the secretion of SCF, LIF, M-CSF, SDF-1 and angiopoietin-1 [116].
Adult human MSCs express intermediate levels of major histo-compatibility complex (MHC) class I and are negative for human leukocyte antigen (HLA) class II antigens, although its expression can be induced by treating cells with interferon-γ. The expression of HLA class I on human fetal MSCs is lower than that on adult cells [117-119]. For these reasons, for several years, MSCs have been considered immune privileged cells, unable to induce alloreactivity in humans. However, more recently it has been demonstrated that donor-derived MSCs are immunogenic in an allogeneic host and stimulate donor graft rejection in a murine model of submyeloablative allogeneic BM transplantation [120]. Moreover, it has been documented that both autologous and allogeneic activated natural killer (NK) lymphocytes are able to mediate MSCs cytolysis, even though MSCs can inhibit interleukin-2 (IL-2)-induced NK-cell proliferation and effector functions [121].
MSCs modulate different aspects of both innate and adaptive immunity, exerting immune regulatory functions, both in in vivo and in vitro, in a wide range of immunocompetent cells, including antigen presenting cells, T, B and NK lymphocytes [122, 123]. In particular, it has been recently demonstrated that MSCs suppress dendritic cell activation in vivo, resulting in the inhibition of cytokine secretion, down-regulation of molecules involved in lymphoid organ homing with subsequent impairment of T-cell priming. MSCs may also affect neutrophil and macrophage functions, by inhibiting apoptosis of resting and activated cells [124]. The capacity of MSCs to modulate T cell responses is well documented; in particular they may inhibit T cell proliferation induced by different stimuli or direct T cells towards regulatory patterns [123, 125]. Controversial results have been described on the immomodulatory role of MSCs on B lymphocyte function, with some studies documenting MSCs inhibitory effect on B cell proliferation, differentiation and immunoglobulin secretion, and other studies demonstrating that under certain experimental conditions MSCs exert a stimulatory effects on B lymphocytes [126, 127].
The immunomodulatory properties of MSCs require cell-to-cell contact, as well as release of soluble factors, including IL-6, IL10, TGFβ, prostaglandin (PGE)-2, indolamine 2,3 dioxygenase (IDO) and soluble HLA-G [93, 123]. Recently it has also been demonstrated that MSCs may release microvesicles transporting functional mRNA and microRNA, a newly described mechanism of cell communication with tissue-injured cells [128], opening a new perspective on the MSCs action during the regenerative process.
All these properties and characteristics underscore the remarkable therapeutic options MSCs offer in several clinical settings.
7. MSCs AND AGING
The relation between aging and MSCs is complex because it includes the effect of aging on MSCs themselves and the contribution of MSCs to the aging of the organism [129]. However aging affects MSCs potential and consequently impairs homeostasis and organ function. In particular, over time, in rodents, monkeys and human BMSCs show a decline in terms of differentiation properties, and the same impairment was demonstrated also for ASCs [130]. Even though debate continues, it is accepted that the difference in MSCs during aging is due to both extrinsic and intrinsic factors, such as genetic background and epigenetic changes [131]. Mansilla et al. [132] proposed that some clinical situations like lipodystrophic syndromes, progeria, and more generally aging could be the consequence of a progressive and persistent stem cell exhaustion syndrome. The main consequence of this syndrome is an irreversible loss of the effective regenerative MSCs pool and thus a new strategy for the treatment of aging and age-related disorders could be the use of “younger” allogeneic mesenchymal progenitor cells.
Moreover, in older age and in the presence of osteoporosis, mesenchymal precursors tend to follow the adipogenic pathway instead of the osteogenic one [131]. Furthermore the reduction in BMSCs with aging leads to impaired osteogenesis and bone formation. In order to fight this situation, Guan et al. [133] used MSCs on the bone surface, where osteogenic differentiation could take place. The method applied was based on the attachment of a synthetic high-affinity peptidomimetic ligand on the MSCc surface. The results open the way to the use of this strategy for new bone formation and bone strength increase in elderly patients [133].
Regardings cardiovascular diseases, aging is now considered to be a risk factor. BMSCs play a role both in cardiac cell maintenance [134] and in cardiac repair, thanks to their ability to home to injured myocardium [135]. Phase-II clinical trials are ongoing to test the long-term safety and efficacy of allogeneic MSC-based therapies for cardiac repair [136].
Aging also affects wound healing. In particular the incidence of chronic wounds increases over 60 years of age [137]. In this case an impaired macrophage function is noted and MSCs are able to restore macrophage phagocytic properties in aged mouse [137].
All together these first results encourage the employment of MSCs in aging-related diseases. In particular, MSCs from young donors could be administered to elderly patients to supplement their MSCs deficiency.
8. CLINICAL APPLICATIONS
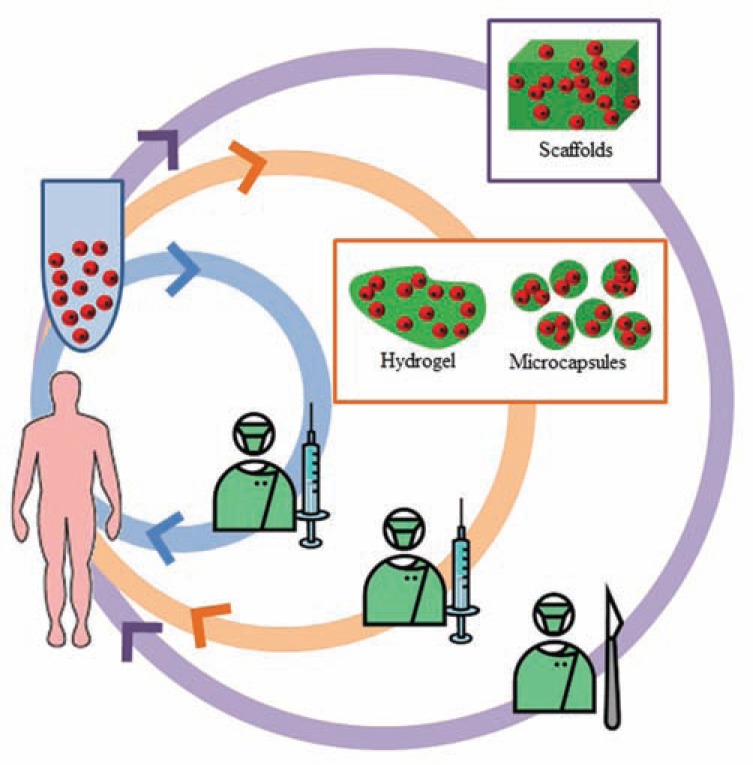
Although MSCs were discovered in the ’60s, their widespread use in clinical applications is recent and is due to the discovery of their properties of self-renewal and differentiation into different cell types when placed in culture [138]. The basic clinical characteristic of MSCs depends on their differentiation towards cells of mesodermal origin, like bone, cartilage and adipose tissue, cells of ectodermal origin, like neurons, or finally cells of endodermal origin, like kidney, liver and colon [139] as well as their strong immunomodulatory properties, which results in the inhibition of proliferation and function of T, B and natural killer cells, and that can be successfully employed to facilitate BM and solid-organ transplantation, preventing rejection and improving the function of the graft. These observations are the starting point for clinical trials that aim to treat several diseases such as myocardial infarction, multiple sclerosis, amyotrophic lateral sclerosis and leukemia [140, 141]. The best administration technique is one that guarantees the highest regenerative benefit with the lowest degree of side effects. Besides tissue engineered products, which requires a MSCs-scaffold construct to be directly implanted at the lesion site, the most studied methods for MSCs transplantation are based on intravenous (i.v.) or intra-arterial infusion and direct injection into the target tissue [142]. (Fig. 1) shows the different vehicles for each way of administration.
Fig. (1).
Schematic representation of the most common strategies for the MSCs administration in clinical settings. Bioptic tissues from donors (allogeneic use) or from the patient (autologous use) are used to isolate MSCs. The cell suspension can be administrated by intravenous or intra-arterial infusion (blue ring), or vehiculated on injectable products, as hydrogels or microcapsules, and injected into the target tissue (orange ring), or loaded on solid implantable scaffolds and transplanted during surgery (purple ring). (The color version of the figure is available in the electronic copy of the article).
Among the different MSCs administration routes, i.v. is the most convenient because it allows for the distribution of MSCs to many organs i.e. lungs, spleen, liver, BM, thymus, kidney, skin and tumor tissues. Dissemination occurs quickly, which could have both positive and negative effects. Among the latter there is the first passage effect with risk of embolism in the lung. On the contrary, entrapment in the spleen or liver is associated with upregulation of CD3 lymphocytes [142]. This route has been employed in animal studies carried out to treat acute kidney injury, infarcted heart, type I diabetes mellitus, GvHD, systemic lupus erythematosus, acute disseminated encephalomyelitis (multiple sclerosis) and pulmonary fibrosis (reviewed in [143]).
Recently, the intraoperative use of MSCs has been proposed. In this type of application, usually bone marrow is either centrifuged or filtered to separate the MNCs population including MSCs. In this way, MSCs do not undergo extensive manipulation under GMP conditions and thus their use can be extended to a larger number of clinical settings.
However, the number of MSCs which are obtained with this technique is low and the population is not homogeneous; for this reason this approach is used for local application of MSCs, with or without a scaffold.
Regarding humans, up to 289 MSCs clinical trials are currently registered (http://clinicaltrials.gov, last access 2012, October 08) [143] and MSCs have already been granted expanded access for use in pediatric steroid-refractory acute GvHD by the United States Food and Drug Administration [144]. In the following subsections the clinical studies in which MSCs are being investigated will be briefly reviewed.
When considering the use of ex vivo expanded MSCs for clinical application, some potential risks should be considered: the immunogenicity of the cells, the biosafety of medium components, the risk of ectopic tissue formation, and the potential in vitro transformation of the cells during expansion.
Concerning the immunogenicity of MSCs, some authors have shown that MSCs are not intrinsically immunoprivileged; indeed the infusion of allogeneic MSCs into immunocompetent and MHC-mismatched mice may induce an immune response, resulting in their rejection [120]. Moreover, when gene-marked MSCs were employed in the treatment of Osteogenesis Imperfecta, the cells were not detected in the treated patients, indicating their potential recognition and rejection by the host immune system [145]. Despite this, the majority of clinical trials for MSCs therapeutic application have reported so far the low immunogenicity of MSCs in humans [88, 146-148]. In view of these considerations, the state of immune competence of the patient at the time of infusion, the number of infusions needed to treat the patient and the donor origin of MSCs (autologous or allogeneic) should be taken into consideration.
The second potential side-effect relates to the use of FCS for ex vivo expansion of MSCs which might be associated with the risk of transmission of zoonoses and with potential immune reactions in the host, resulting in rejection of the cells especially after repeated treatments [89, 149]. For these reasons, animal-free additives are being considered for clinical-grade expansion of MSCs (see chapter 4).
A further potential risk of MSCs treatment involves the formation of mesenchymal tissues at ectopic sites. In a rat myocardial infarction model, it has been reported that MSCs may form bone following local injection into the myocardium [150]. Similarly, formation of adipose tissue in kidneys has been observed in a rat model of experimental glomerulonephritis [151]. Despite these experimental findings, in clinical trials, thus far, no ectopic tissue or tumor formation in vivo has been observed. A strict and long-term follow-up of patients treated with MSCs is recommended. For the potential in vitro transformation of MSCs during ex vivo expansion, see chapter 5.
8.1. MSCs for Treatment of Graft-versus-Host-Disease (GvHD)
The immunomodulatory properties of MSCs have been successfully employed to treat severe, steroid-resistant acute GvHD, developing after either allogeneic hematopoietic stem cell transplantation (HSCT) or donor lymphocyte infusion. Le Blanc et al. [152] first reported on a pediatric patient experiencing grade-IV refractory acute GvHD who was rescued with i.v. infusions of HLA-haploidentical MSCs [152]. Following this study, 55 adult and pediatric patients with steroid-resistant GvHD were enrolled in a multicenter phase I/II study, whose primary endpoints where both safety and efficacy in terms of improvement of survival and decreased trasplanted-related mortality (TRM). Patients were treated with i.v. infusions of allogeneic MSCs. No adverse events were recorded and a clinical response was noted in the majority of patients with a significant advantage in terms of survival for complete responders, as compared with partial/non-responding patients [88], with significantly decreased TRM.
These results were confirmed in a pediatric study including 37 children with grade III-IV aGvHD, showing complete response in 59% of the patients after i.v. MSCs treatment [153]. A significantly better overall survival (OS) was observed in children treated who had received a reduced 2nd line immune suppressive treatment and were given MSCs earlier after GvHD onset. Also in this context, despite very promising preliminary results, the real efficacy of MSCs therapy needs to be further evaluated in prospective, randomized trials.
In the USA the largest, prospective, open-labeled multicentric phase-II study was run in 16 Centers between 2005 and 2006 and the results were published in 2009 [154]. This study randomized 31 adult patients (median age 52 years) with acute grade II-IV GvHD to receive i.v. MSCs infusions at two different concentrations along with corticosteroid as first line treatment. MSCs were isolated from BM aspirates of third party donors, cultured in FBS, and frozen until infusion. All patients received their first MSCs infusion within 48 hours from appearance of signs of GvHD and a second infusion 3 days later. The primary endpoint was evaluation of toxicity. No adverse events were documented. The secondary endpoint was evaluation of efficacy. Response rate was 94% with 77% complete responses and 16% partial response. No differences in terms of efficacy and safety were observed between the high- and low-dose MSCs group. Patients who achieved complete response to treatment had significantly improved survival compared with non-responder patients (88% vs 14%, p = 0.0008). The higher response rate in this study, compared with the European study [88], was thought to be due to a higher percentage of patients exhibiting a milder degree of GvHD when enrolled in the US-trial.
To better understand if the precocious use of MSCs in milder forms of steroid-resistant GvHD was one of the determining factors for an improved response rate, successive trials were aimed at evaluating this issue. After demonstration of feasibility and safety of treatment by Lucchini et al. [155], the same group in a phase I-II study (EudraCT 2008-007869-23) treated, as second-line therapy, both adult and pediatric patients developing acute or chronic GvHD, infusing MSCs immediately after steroid failure, to evaluate if earlier MSCs administration would allow better responses (at least 3 MSCs infusions, 1x106/kg cell dose for each infusion to each patient). The primary endpoint of this study was safety. The secondary endpoints were the response of GvHD (evaluated 28 days after the last MSCs infusion), as well as the overall survival and transplant-related deaths. Preliminary data from 47 analyzed patients [156] support previous findings. No side effects or infusion-related toxicities were observed, no ectopic tissue formation or increased relapse incidence were documented. To reiterate, patients affected by acute GvHD have a greater chance to respond to MSCs administration, and these findings seem to be in line with immunobiological observations which indicate chronic GvHD as a disease in which acute inflammation no longer plays an active role [157]. Moreover, patients affected by grade II-III GvHD seem to respond better than grade IV, thus suggesting a possible limitation in the treatment of very severe cases with this type of immunotherapy. Moreover, pediatric patients respond generally better than adults. Of note, treatment of GvHD with MSCs as the 2nd line therapy after steroid failure helped to avoid additional delivering of immunosuppressive lines in a consistent number of patients, thus allowing a better and more prompt immune reconstitution. In summary, response was significantly more likely in patients exhibiting grade II GvHD versus those exhibiting more severe gradings (87.5% vs. 51.6%, p = 0.02) and in patients receiving MSCs in a time frame of 30 days from the onset of GvHD (75.9% vs. 43.7%, p= 0.05). The current median follow up for this cohort is 250 days (range 30-1066). Responders showed a significantly lower transplant-related mortality (10.0% vs. 88.2%, p <0.05) and a better overall survival probability than non responders (23.3% vs. 88.2%, p <0.05). Moreover, biological and immunological analyses of blood samples collected after infusions demonstrated, for the first time, that clinical response paralleled decreased percentages of proinflammatory Th17 cells and increased T-reg circulating cells, and was accompanied by plasmatic reduction in well-known pro-inflammatory molecules, recognized as specific markers of active GvHD [158].
8.2. MSCs for Crohn’s Disease
Due to the relapsing/refractory nature of the disease, alternative therapeutic strategies are warranted to increase remission and to improve quality of life in Crohn’s Disease (CD) patients [159].
Based on encouraging experimental results obtained in animal models of colitis [160, 161], phase I/II clinical trials have been conducted. Ten patients with refractory luminal CD have been treated with i.v. infusion of autologous BMSCs, demonstrating the feasibility and safety of the approach [147]. Clinical response was observed in three patients, together with an increase in CD4+CD127+ Tregs in mucosal biopsies. With regard to fistulizing CD, five patients were treated with locally administered autologous MSCs, obtaining healing of fistulas [162]. In a subsequent phase I/II study, ten CD patients with refractory complex perianal fistulas were given intrafistular injections of autologous BMSCs; complete fistula healing in seven patients and a partial response in the remaining three were observed [148]. The healing of fistula was accompanied by a decrease in the CD and perianal disease activity index. Also in this study, an increase in the percentage of mucosal, as well as circulating, Tregs was noted after MSCs treatment, suggesting the possible role played by Tregs in MSC-mediated repair of inflamed tissues.
Altogether, these studies demonstrate the feasibility and safety of MSCs treatment in refractory CD, however efficacy needs to be proven in large randomized clinical trials.
8.3. MSCs as Support for Hematopoietic Stem Cell Recovery/Engraftment
MSCs co-infusion was first demonstrated to enhance engraftment of hematopoietic stem cells (HSCs) in NOD/SCID mice [163]. Subsequently, MSCs were employed to accelerate haema-tological recovery in 28 breast cancer patients given a co-infusion of autologous peripheral blood HSCs and MSCs after high-dose chemotherapy. All patients had a rapid hematopoietic recovery in the absence of toxicity [164]. These results were confirmed in a multicenter, phase I/II trial enrolling 46 patients with haematological malignancies who received allogeneic HSCs co-infused with MSCs [165]. In a subsequent phase I/II, multicenter clinical study enrolling 14 children given a T-cell depleted HLA-disparate allograft proved to be safe and all patients showed sustained hematopoietic engraftment, as compared with 20% graft failure rate in historical controls [146]. The safety of co-transplantation of parental MSCs was also demonstrated in 13 pediatric patients given an umbilical cord blood transplantation [166]. While no advantage in terms of engraftment rate and speed of haematological recovery was observed, patients given MSCs had a lower incidence of grade II-IV acute GvHD as compared with historical controls [166].
8.4. MSCs in the Orthopaedic Practice
MSCs therapeutic potential has been observed in bone and cartilage disease, and promising approaches have also been attempted in the repair of meniscus, tendons, muscles and ligaments.
To date, there are approximately 15 clinical trials concerning the use of MSCs in orthopaedic practice [143]. Most of the cell-based approachs are based on autologous MSCs, even if allogeneic MSCs were the first to be investigated. Systemic infusion of allogeneic MSCs was successfully used in the 90’s to treat osteogenesis imperfecta [149], a genetic disorder in which osteoblasts produce defective type I collagen, leading to osteopenia, multiple fractures, severe bone deformities and impaired stature. Allogeneic HSCT led to engraftment of functional mesenchymal progenitor cells, with relevant benefit for children with this disease [167].
In bone diseases, MSCs are usually delivered or applied locally, often in combination with suitable scaffolds when it is necessary to provide mechanical stabilization or support as in osteosynthesized fractures of long bones [168] and in atrophic nonunions. Although controversial, MSCs seeded on hydroxyapatite scaffolds have also been used to heal defects derived from curettage of a bone tumor as an alternative to autologous bone grafting [169]. In an attempt to improve the outcome in total ankle replacement, expanded BMSCs have been applied to ceramic ankle prosthesis [170]; good results have been achived in terms of bone formation around the cell-seeded areas of the prostheses and implant stability. MSCs can also be utilized in bone regeneration as a fresh product, without in vitro expansion. The most common variation of this approach is the use of concentrated BM, which are obtained directly in the operating room by centrifugation or close system filtration resulting in concentrated mononuclear cells, including mesenchymal progenitor cells. Of course this represents a compromise between the cost reduction and time savings and the “quality” of the cell population that is obtained, since the cell population is not homogeneous and also contains hematopoietic cells, platelets and leucocytes, with a lower concentration of progenitor cells. Connolly [171] was the first to demonstrate the efficacy of percutaneous injection of autologous BM in a series of delayed unions, non-unions, arthrodesis and bone defects. Autologous concentrated BM has also been successfully used for the treatment of idiopathic osteonecrosis of the femoral head with very satisfactory results also at medium-long follow up [172, 173] as well as for the treatment of unicameral bone cysts [174].
To date there have been only limited reports on human autologous BMSCs implantation for cartilage repair, but several clinical trials are in progress, thus demonstrating the wide interest in this kind of treatment. Wakitani reported successful results on cultured MSCs embedded in a collagen gel and delivered to the knee joint covered with autologous periosteum in 41 patients. Patients achieved good functional recovery and no adverse reactions, tumors or infections were observed at a mean follow up of about six years [175].
A pilot clinical study recently demonstrated that the combination of MSCs, platelet-rich plasma gel and fibrin was able to induce relevant improvement of chondral defects, with formation of simil-hyaline tissue [176]. Another innovative and promising approach derives from the synergistic effect between expanded chondrocytes and expanded MSCs: chondrocytes seem to be able to induce the chondrogenic differentiation of MSCs, while the latter seem to promote chondrocyte proliferation [177-180].
As well as for bone regeneration, the convenience of using fresh MSCs directly obtained in the operating room has led to a recent significant increase in clinical studies, showing favorable results in the treatment of both knee and ankle chondral or osteochondral lesions [181-183]. Even if still at an experimental stage, TGFβ1, FGF-2 (fibroblast growth factor 2) and CDMP-1 (cartilage-derived morphogenetic protein-1) gene modified MSCs have been demonstrated to enhance the repair of full-thickness articular cartilage defects in allogeneic rabbits [184, 185].
8.5. MSCs for Skin Regeneration and Plastic Surgery
Burns and chronic ulcers are cutaneous wounds that share common problems, i.e. the loss of both superficial epidermis and dermis, abnormal and incorrect wound healing [186]. In adult skin, stem cells are mainly located in the hair follicle bulge. It has been demonstrated that follicular cells can in vitro recreate the epidermis [187] so in vivo they can improve re-epithelization. When there is deep injury, hair follicles are disrupted and skin grafting is recommended [188]. Starting from Rheinwald and Green [189] who in 1975 proposed the first cellular treatment, nowadays researchers affirms that MSCs modulate systemic effects of burn trauma: hypermetabolic response, inflammation and immunosuppression. In particular, the therapeutic effect of MSCs seems to be due more to paracrine mechanisms and growth factor secretion than post-engraftment differentiation and proliferation [188]. At first, MSCs were employed in burns caused by ionizing radiation, because of the lack of a therapeutic alternative for this type of burn: the results suggested that MSCs controlled local inflammation. The rationale of their employment in this setting is provided by the studies on MSCs in chronic wound treatment. Chronic wounds are characterized by an incorrect wound healing process, with a prolonged inflammatory phase which prevents or retards subsequent events [190]. When a skin wound extends to the dermis and is larger than 1cm in diameter, the healing process may be impossible or may lead to extensive scarring and a specialized treatment, such as skin grafting, is required [191]. During the wound healing process stem cells are inactive players particularly during the inflammatory phase. Leucocytes, which migrate to the site of injury in the early inflammatory phase, derive from HSCs; MSCs direct hematopoietic progenitor stem cells to differentiate into dendritic cells; and MSCs are mobilized in the peripheral circulation and engraft near adnexal structures in the skin [192]. MSCs can act as wound healing agents by paracrine communication with resident wound cells, infiltrating inflammatory cells and antigen presenting cells or by their differentiation into resident cells or both mechanisms. MSCs can be admi-nistered topically: cells can be placed directly on the wound, injected into neighboring tissue or included into skin substitutes. Besides the good results obtained by different studies, several issues must be considered, such as their long-term fate [193] and different results due to the age of the subject [192]. When a wound is completely healed, the new tissue results in scar formation, which is characterized by disorganized collagen formation [194]. The use of fat grafting may improve scar formation as recently demonstrated by Guisantes et al. in [195]. In this setting the attention was focused on cells of the stromal vascular fraction (SVF), such as mesenchymal stem cells and progenitors. Coleman, who developed his lipostructure technique in the early 1980s, and, subsequently, other authors [196, 197] suggested that the long-term remodeling effects observed after adipose tissue grafting may be due to the presence of mesenchymal stem cells and progenitors [198].
8.6. Neurodegenerative Disease
Stem-cell-based therapies represent a new approach for neurodegenerative diseases. MSCs have the ability to differentiate into all mature neural cell types. They have been suggested to adopt “astrocytic ” and “neuronal like” cell fates. In particular, in neural progenitor maintenance medium, MSCs acquire new morphological characteristics, neural markers, and electrophysiological properties, which are suggestive of neural differentiation [199]. In animals, MSCs seem to limit damage to, or mediate repair of, CNS tissue via mechanisms other than cell replacement or trans-differentiation, probably via their paracrine functions. Several studies have revealed that the therapeutic action of MSCs is related to the release, even far from the site of injection, of protective factors rather than to replacement of degenerating neurons. Such a therapeutic effect may be provided by different classes of molecules, including trophic factors, anti-inflammatory cytokines and immuno-modulatory chemokines released from transplanted cells. Although the adult brain contains a small number of stem cells in restricted areas, the central nervous system exhibits only a limited capacity for regenerating lost tissue. Therefore, cell replacement therapies of damaged brain have provided the basis for the development of potentially powerful new therapeutic strategies for a broad spectrum of human neurological diseases, such as Parkinson’s disease (PD), Huntington’s disease, Amyotrophic Lateral Sclerosis (ALS), Alzheimer’s disease (AD) [200].
MSCs derived from PD patients are similar to normal MSCs in phenotype, morphology, and differentiation capacity. Moreover, PD-derived MSCs are able to differentiate into neurons in a specific medium with up to 30% of cells exhibiting the characteristics of dopamine cells. PD-derived MSCs could inhibit T-lymphocyte proliferation induced by mitogens. These findings suggest that BMSCs obtained from PD patients may be a promising cell type for cellular therapy and somatic gene therapy applications [201].
MSCs therapy might also represent a promising new therapeutic strategy for ALS that could support or restore motoneuron function. It has been demonstrated that expanded MSCs can survive and migrate after transplantation in the lumbar spinal cord of SOD1G93A mice, where they prevent astrogliosis and microglial activation and delay ALS-related decrease in the number of motoneurons, thus resulting in amelioration of motor performance [202].
BMSCs from ALS patients maintain their peculiar characteristics when expanded in vitro and do not display chromosomal alterations or cellular senescence, while they acquire, under specific conditions, new morphological characteristics and neural markers which are suggestive of neural differentiation like those seen in cells obtained from healthy donors [203].
In two phase I trials, Mazzini et al. showed the feasibility and safety of transplantation with autologous MSCs into the spinal cord of ALS patients. Nineteen patients with ALS were treated with autologous BMSCs implanted into the dorsal spinal cord. Eight patients died after a mean survival time of 31.6 months from surgery for reasons unassociated with the experimental treatment. The most important results were the neuro-radiological demonstration of the lack of tumor formation or abnormal cell growth, the absence of significant effects associated with the procedure and the absence of deterioration in psychosocial status during a follow-up of nearly nine years [204].
Preclinical studies suggested that MSCs represent also an effective therapy in animal models of myelin disease, such as multiple sclerosis, where MSCs might contribute to re-myelination and myelin recovery.
8.7. Future Perspectives for Using MSCs in Cancer Therapy
The best cancer chemotherapy approach is to deliver the drug to the tumor microenvironment in order to kill tumor cells while producing the lowest collateral toxicity. With this aim, many approaches have been proposed including the genetic manipulation of stem cells. Among them, MSCs represent an optimal choice to deliver anti-tumor agents due to their adaptability to culture conditions necessary for in vitro manipulation and their capacity for homing to pathological tissues when systemically administrated in vivo [205-211]. MSCs have been genetically modified to over-express several different anti-tumor molecules including interleukins, interferons, prodrugs, oncolytic viruses, anti-angiogenic agents, pro-apoptotic proteins and growth factor inhibitors, and they have been shown to be effective in killing tumor cells both in vitro and in vivo (reviewed in [212]). However, MSCs genetic manipulation is not free from risks when clinically applied [213].
Besides the possibility of introducing genes into MSCs that may affect tumor growth, it has been shown that MSCs isolated from bone marrow possess drug metabolizing activity. In particular, these cells are able to incorporate anti-cancer drugs, such as doxorubicin, that can be subsequently released affecting the proliferation of neighbouring cells [214, 215]. More recent studies have demonstrated that human MSCs exposed to a very high concentration of paclitaxel in vitro, rapidly incorporated the drug and slowly released it in the culture medium in a time dependent manner. In addition PTX primed MSCs acquired potent anti-tumor and anti-angiogenic activity when co-cultured with cancer cells or endothelial cells respectively. In vivo, the co-injection of PTX primed MSCs with different types of human cancer cells in immunodeficient mice significantly delayed tumor development and inhibited tumor growth [216, 217]. These results highlight a completely novel manner to apply MSCs in cancer therapy. Moreover, since MSCs can be loaded with drugs without any genetic manipulation, this may reduce the risk of cell transformation, thus enhancing the safety for their eventual use in the treatment of some human cancers.
9. REGULATORY DIRECTIVES FOR MSC-BASED THERAPY: “CELLS AS DRUGS”
From a regulatory point of view, since 2001 every product for advanced therapy is considered a drug [218]. Any new drug, before commercialization, must be subjected to pre-clinical and clinical trials. The pre-clinical phase is intended to guarantee the essential characteristics of safety and efficacy of the new drug, and to determine its pharmacokinetic profile. This is a complicated process for a chemical or biotechnological drug, and even more demanding in the case of MSCs for clinical use. As a matter of fact, the main problem is to define which is the real drug: is it the total cell population or its metabolites? Another problem is to determine the required/recommended dose, considering the great variability between cells from different donors and also from the same donor but from different sites of collection. Finally, there are no specific markers to unequivocally identify MSCs [219]. Moreover, preclinical studies for MSCs advanced therapies do not always reflect subsequent activity in humans [220]. Regulatory directives postulate that the clinical phase must start after the pre-clinical phase is completed; however, this sequence has not always been respected. After completion of clinical trials and formal marketing authorization from Authorities for a specific pharmaceutical dosage form, large-scale production is started according to GMP protocols. In the case of MSCs this involves the use of adequate instrumentation and the adoption of appropriate procedures by trained personnel, with a consequent high unitary cost of production. Furthermore, each batch should have the same characteristics and this is not always feasible with MSCs, considering the above-mentioned problems of dose definition and characteristics for the standardization of the product [221]. Cooperation between institutions is essential: regulatory organs and researchers should work together to find an acceptable compromise between the requirements for the marketing authorization of a chemical or biotechnological drug with the those for MSCs advanced therapies.
10. CONCLUSION AND FUTURE PERSPECTIVES
MSCs are among the most promising candidates for future regenerative medicine regimens. They can be obtained from many different adult tissue sources, are easy to isolate readily adapt to culture conditions, and undergo to rapid in vitro expansion. Besides their multipotency, MSCs possess strong paracrine activity; they release a broad spectrum of molecules that affect angiogenesis, inflammation and immunity. Thus they appear to play a central role in controlling tissue homeostasis and in participating in tissue regeneration. For these reasons MSCs offer a large number of possible applications for the treatment of many diseases. Since they have been included among AMT products, they are subjected to the same conditions that govern the production and use of drugs. While further studies will provide new insights into their characteristics, this review is intended as a background source for clinical trials focused on the clinical application of MSCs.
ACKNOWLEDGEMENTS
Authors thank Dr. Theodora Chlapanidas, Dr. Giulia Lucconi, Dr. Sara Perteghella, Dr. Laurine Kelly, Dr. Maddalena Caruso, Dr. Elena Arrigoni, Dr. Giovanna Lucchini and Dr. Erica Dander for their help in editing the manuscript.
DISCLOSURE POLICY
The manuscript was neither prepared nor funded in any part by a commercial organization. The authors of this manuscript have no conflicts of interest to disclose.
ABBREVIATIONS
- AD
= Alzheimer’s disease
- ALS
= Amyotrophic Lateral Sclerosis
- AMSCs
= Amniotic mesenchymal stem/stromal cells
- AMT
= Advance medicinal therapy
- ASCs
= Adipose-derived stem/stromal cells
- BM
= Bone marrow
- BMSCs
= Bone marrow stem/stromal cells
- CMSCs
= Chorionic mesenchymal stem/stromal cells
- FCS
= Fetal calf serum
- GMP
= Good Manufacturing Practice
- GvHD
= Graft versus-host disease
- HSCs
= Hematopoietic stem cells
- HSCT
= Hematopoietic stem cell transplantation
- ISCT
= International Society for Cellular Therapy
- MNCs
= Mononuclear cells
- MSCs
= Mesenchymal stem/stromal cells
- PD
= Parkinson’s disease
- PL
= Platelet lysate
- SMSCs
= Synovium-derived mesenchymal stem/stromal cells
- SVF
= Stromal vascular fraction
- TRegs
= Regulatory T cells
REFERENCES
- 1.Cohnheim J. Ueber entzundung und eiterung. Path Anat Physiol Klin Med. Berlin. 1867:1–79. [Google Scholar]
- 2.Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976;4:267–74. [PubMed] [Google Scholar]
- 3.Zengin E, Chalajour F, Gehling UM, et al. Vascular wall resident progenitor cells: a source for postnatal vasculogenesis. Development. 2006;133:1543–51. doi: 10.1242/dev.02315. [DOI] [PubMed] [Google Scholar]
- 4.Cossu G, Bianco P. Mesoangioblasts - vascular progenitors for extravascular mesodermal tissues. Curr Opin Genet Dev. 2003;13:537–42. doi: 10.1016/j.gde.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Carmeliet P. Angiogenesis in life. disease and medicine. Nature. 2005;438:932–6. doi: 10.1038/nature04478. [DOI] [PubMed] [Google Scholar]
- 6.Caplan AI. What's in a Name?. Tissue Eng. 2010;16:2415–7. doi: 10.1089/ten.TEA.2010.0216. [DOI] [PubMed] [Google Scholar]
- 7.Muraglia A, Cancedda R, Quarto R. Clonal mesenchymal progenitors from human bone marrow differentiate in vitro according to a hierarchical model. J Cell Sci. 2000;113:1161–6. doi: 10.1242/jcs.113.7.1161. [DOI] [PubMed] [Google Scholar]
- 8.Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells.The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- 9.Prockop DJ. Marrow stromal cells as steam cells for nonhematopoietic tissues. Science. 1997;276:71–4. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 10.Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A. 2000;97:13625–30. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quirici N, Scavullo C, de Girolamo L, et al. Anti-L-NGFR and-CD34 monoclonal antibodies identify multipotent mesenchymal stem cells in human adipose tissue. Stem Cells Dev. 2010;19:915–25. doi: 10.1089/scd.2009.0408. [DOI] [PubMed] [Google Scholar]
- 12.Martinez C, Hofmann TJ, Marino R, Dominici M, Horwitz EM. Human bone marrow mesenchymal stromal cells express the neural ganglioside GD2: a novel surface marker for the identification of MSCs. Blood. 2007;109:4245–8. doi: 10.1182/blood-2006-08-039347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buehring HJ, Battula VL, Treml S, Schewe B, Kanz L, Vogel W. Novel markers for the prospective isolation of human MSC. Ann N Y Acad Sci. 2007;1106:262–71. doi: 10.1196/annals.1392.000. [DOI] [PubMed] [Google Scholar]
- 14.Jones EA, Kinsey SE, English A, et al. Isolation and characterization of bone marrow multipotential mesenchymal progenitor cells. Arthritis Rheum. 2002;46:3349–60. doi: 10.1002/art.10696. [DOI] [PubMed] [Google Scholar]
- 15.Gindraux F, Selmani Z, Obert L, et al. Human and rodent bone marrow mesenchymal stem cells that express primitive stem cell markers can be directly enriched by using the CD49a molecule. Cell Tissue Res. 2007;327:471–83. doi: 10.1007/s00441-006-0292-3. [DOI] [PubMed] [Google Scholar]
- 16.da Silva Meirelles L, Fontes AM, Covas DT, Caplan AI. Mechanisms involved in the therapeutic properties of mesenchymal stem cells. Cytokine Growth Factor Rev. 2009;20:419–27. doi: 10.1016/j.cytogfr.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Salem HK, Thiemermann C. Mesenchymal Stromal Cells: Current Understanding and Clinical Status. Stem Cells. 2010;28:585–96. doi: 10.1002/stem.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Izadpanah R, Trygg C, Patel B, et al. Biologic properties of mesenchymal stem cells derived from bone marrow and adipose tissue. J Cell Biochem. 2006;99:1285–97. doi: 10.1002/jcb.20904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mafi P, Hindocha S, Mafi R, Griffin M, Khan WS. Adult mesenchymal stem cells and cell surface characterization - a systematic review of the literature. Open Orthop J. 2011;5:253–60. doi: 10.2174/1874325001105010253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boheler KR. Functional markers and the 'homogeneity' of human mesenchymal stem cells. J Physiol. 2004;554:592. doi: 10.1113/jphysiol.2003.057224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blasi A, Martino C, Balducci L, et al. Dermal fibroblasts display similar phenotypic and differentiation capacity to fat-derived mesenchymal stem cells. but differ in anti-inflammatory and angiogenic potential. Vasc Cell. 2011;3:5. doi: 10.1186/2045-824X-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorenz K, Sicker M, Schmelzer E, et al. Multilineage differentiation potential of human dermal skin-derived fibroblasts. Exp Dermatol. 2008;17:925–32. doi: 10.1111/j.1600-0625.2008.00724.x. [DOI] [PubMed] [Google Scholar]
- 23.Miranville A, Heeschen C, Sengenes C, Curat CA, Busse R, Bouloumie A. Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation. 2004;110:349–55. doi: 10.1161/01.CIR.0000135466.16823.D0. [DOI] [PubMed] [Google Scholar]
- 24.De Siena R, Balducci L, Blasi A, et al. Omentum-derived stromal cells improve myocardial regeneration in pig post-infarcted heart through a potent paracrine mechanism. Exp Cell Res. 2010;316:1804–15. doi: 10.1016/j.yexcr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 25.Cavallo C, Cuomo C, Fantini S, et al. Comparison of alternative mesenchymal stem cell sources for cell banking and musculoskeletal advanced therapies. J Cell Biochem. 2011;112:1418–30. doi: 10.1002/jcb.23058. [DOI] [PubMed] [Google Scholar]
- 26.Kern S, Eichler H, Stoeve J, et al. Comparative analysis of mesenchymal stem cells from bone marrow. umbilical cord bood.or adipose tissue. Stem Cells . 2006; 24:1294–301. doi: 10.1634/stemcells.2005-0342. [DOI] [PubMed] [Google Scholar]
- 27.Lee OK, Kuo TK, Chen W-M, et al. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood. 2004;103:1669 –75. doi: 10.1182/blood-2003-05-1670. [DOI] [PubMed] [Google Scholar]
- 28.Flynn A, Barry F, O'Brien T. UC blood-derived mesenchymal stromal cells: an overview. Cytotherapy. 2007;9:717–26. doi: 10.1080/14653240701584578. [DOI] [PubMed] [Google Scholar]
- 29.Bosch J, Houben AP, Radke TF, et al. Distinct differentiation potential of "MSC" derived from cord blood and umbilical cord: are cord-derived cells true mesenchymal stromal cells?. Stem Cells Dev. 2012;21:1977–88. doi: 10.1089/scd.2011.0414. [DOI] [PubMed] [Google Scholar]
- 30.Kim Y, Kang H, Jang SW, et al. Direct comparison of human mesenchymal stem cells derived from adipose tissues and bone marrow in mediating neovascularization in response to vascular ischemia. Cell Physiol Biochem. 2011;28:175–84. doi: 10.1159/000110447. [DOI] [PubMed] [Google Scholar]
- 31.Bieback K, Kern S, Kocaömer A, et al. Comparing mesenchymal stromal cells from different human tissues: bone marrow. adipose tissue and umbilical cord blood. Biomed Mater Eng. 2008;18:S71–6. [PubMed] [Google Scholar]
- 32.Pachón-Peña G, Yu G, Tucker A, et al. Stromal stem cells from adipose tissue and bone marrow of age-matched female donors display distinct immunophenotypic profiles. J Cell Physiol. 2011;226:843–51. doi: 10.1002/jcp.22408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bochev I, Elmadjian G, Kyurkchiev D, et al. Mesenchymal stem cells from human bone marrow or adipose tissue differently modulate mitogen-stimulated B-cell immunoglobulin production in vitro. Cell Biol Int. 2008;32:384–93. doi: 10.1016/j.cellbi.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 34.Ivanova-Todorova E, Bochev I, Mourdjeva M, et al. Adipose tissue-derived mesenchymal stem cells are more potent suppressors of dendritic cells differentiation compared to bone marrow-derived mesenchymal stem cells. Immunol Lett. 2009;126:37–42. doi: 10.1016/j.imlet.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 35.Noël D, Caton D, Roche S, et al. Cell specific differences between human adipose-derived and mesenchymal-stromal cells despite similar differentiation potentials. Exp Cell Res. 2008;314:1575–84. doi: 10.1016/j.yexcr.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 36.Wagner W, Wein F, Seckinger A, et al. Comparative characteristics of mesenchymal stem cells from human bone marrow adipose tissue and umbilical cord blood. Exp Hematol. 2005;33:1402–16. doi: 10.1016/j.exphem.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Nilsson C, Aboud S, Karlen K, Hejdeman B, Urassa W, Biberfeld G. Optimal blood mononuclear cell isolation procedures for gamma interferon enzyme-linked immunospot testing of healthy Swedish and Tanzanian subjects. Clin Vaccine Immunol. 2008;15:585–9. doi: 10.1128/CVI.00161-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goel RK, Suri V, Suri A, et al. Effect of bone marrow-derived mononuclear cells on nerve regeneration in the transection model of the rat sciatic nerve. J Clin Neurosci. 2009;16:1211–7. doi: 10.1016/j.jocn.2009.01.031. [DOI] [PubMed] [Google Scholar]
- 39.Muschler GF, Nitto H, Boehm CA, Easley KA. Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res. 2001;19:117–25. doi: 10.1016/S0736-0266(00)00010-3. [DOI] [PubMed] [Google Scholar]
- 40.Ganong W. Review of medical physiology. McGraw-Hill New York. 2005 [Google Scholar]
- 41.Yeo C, Saunders N, Locca D, et al. Ficoll-Paque (TM) versus Lymphoprep (TM): a comparative study of two density gradient media for therapeutic bone marrow mononuclear cell preparations. Regen Med. 2009;4:689–96. doi: 10.2217/rme.09.44. [DOI] [PubMed] [Google Scholar]
- 42.Seeger FH, Tonn T, Krzossok N, Zeiher AM, Dimmeler S. Cell isolation procedures matter: a comparison of different isolation protocols of bone marrow mononuclear cells used for cell therapy in patients with acute myocardial infarction. Eur Heart J. 2007;28:766–72. doi: 10.1093/eurheartj/ehl509. [DOI] [PubMed] [Google Scholar]
- 43.Chang Y, Hsieh P-H, Chao CCK. The efficiency of Percoll and Ficoll density gradient media in the isolation of marrow derived human mesenchymal stem cells with osteogenic potential. Chang Gung Med J. 2009;32:264–75. [PubMed] [Google Scholar]
- 44.Zuk PA, Zhu M, Mizuno H, et al. Multilineage cells from human adipose tissue: Implications for cell-based therapies. Tissue Eng. 2001;7:211–28. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- 45.Faustini M, Bucco M, Chlapanidas T, et al. Nonexpanded mesenchymal stem cells for regenerative medicine: Yield in stromal vascular fraction from adipose tissues. Tissue Eng. 2010;16:1515–21. doi: 10.1089/ten.TEC.2010.0214. [DOI] [PubMed] [Google Scholar]
- 46.de Girolamo L, Sartori MF, Arrigoni E, et al. Human adipose-derived stem cells as future tools in tissue regeneration: Osteogenic differentiation and cell-scaffold interaction. Int J Artif Organs. 2008;31:467–79. doi: 10.1177/039139880803100602. [DOI] [PubMed] [Google Scholar]
- 47.de Girolamo L, Lopa S, Arrigoni E, Sartori MF, Preis FWB, Brini AT. Human adipose-derived stem cells isolated from young and elderly women: their differentiation potential and scaffold interaction during in vitro osteoblastic differentiation. Cytotherapy. 2009;11:793–803. doi: 10.3109/14653240903079393. [DOI] [PubMed] [Google Scholar]
- 48.Schaeffler A, Buechler C. Concise review: Adipose tissue-derived stromal cells - Basic and clinical implications for novel cell-based therapies. Stem Cells. 2007;25:818–27. doi: 10.1634/stemcells.2006-0589. [DOI] [PubMed] [Google Scholar]
- 49.Kwon EB, Lee JY, Piao S, Kim IG, Ra JC. Comparison of human muscle-derived stem cells and human adipose-derived stem cells in neurogenic trans-differentiation. Korean J Urol. 2011;52:852–7. doi: 10.4111/kju.2011.52.12.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim SC, Han DJ, Lee JY. Adipose Tissue Derived Stem Cells for Regeneration and Differentiation into Insulin-Producing Cells. Curr Stem Cell Res Ther. 2010;5:190–4. doi: 10.2174/157488810791268717. [DOI] [PubMed] [Google Scholar]
- 51.Al Battah F, De Kock J, Vanhaecke T, Rogiers V. Current status of human adipose-derived stem cells: differentiation into hepatocyte-like cells. ScientificWorldJournal. 2011;11:1568–81. doi: 10.1100/tsw.2011.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baer PC, Döring C, Hansmann M-L, Schubert R, Geiger H. New insights into epithelial differentiation of human adipose-derived stem cells. J Tissue Eng Regen Med. 2011 doi: 10.1002/term.518. [DOI] [PubMed] [Google Scholar]
- 53.Choi YS, Dusting GJ, Stubbs S, et al. Differentiation of human adipose-derived stem cells into beating cardiomyocytes. J Cell Mol Med. 2010;14:878–89. doi: 10.1111/j.1582-4934.2010.01009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bailo M, Soncini M, Vertua E, et al. Engraftment potential of human amnion and chorion cells derived from term placenta. Transplantation. 2004;78:1439–48. doi: 10.1097/01.tp.0000144606.84234.49. [DOI] [PubMed] [Google Scholar]
- 55.In 't Anker PS, Scherjon SA, Kleijburg-van der Keur C, et al. Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells. 2004;22:1338–45. doi: 10.1634/stemcells.2004-0058. [DOI] [PubMed] [Google Scholar]
- 56.Soncini M, Vertua E, Gibelli L, et al. Isolation and characterization of mesenchymal cells from human fetal membranes. J Tissue Eng Reg Med. 2007;1:296–305. doi: 10.1002/term.40. [DOI] [PubMed] [Google Scholar]
- 57.Parolini O, Alviano F, Bagnara GP, et al. Concise review: Isolation and characterization of cells from human term placenta: Outcome of the first international workshop on placenta derived stem cells. Stem Cells. 2008;26:300–11. doi: 10.1634/stemcells.2007-0594. [DOI] [PubMed] [Google Scholar]
- 58.Portmann-Lanz CB, Schoebedein A, Huber A, et al. Placental mesenchymal stem cells as potential autologous graft for pre- and perinatal neuroregeneration. Am J Obstet Gynecol. 2006;194:664–73. doi: 10.1016/j.ajog.2006.01.101. [DOI] [PubMed] [Google Scholar]
- 59.Castrechini NM, Murthi P, Gude NM, et al. Mesenchymal stem cells in human placental chorionic villi reside in a vascular Niche. Placenta. 2010;31:203–12. doi: 10.1016/j.placenta.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 60.Wulf GG, Viereck V, Hemmerlein B, et al. Mesengenic progenitor cells derived from human placenta. Tissue Eng. 2004;10:1136–47. doi: 10.1089/ten.2004.10.1136. [DOI] [PubMed] [Google Scholar]
- 61.Troyer DL, Weiss ML. Concise review: Wharton's jelly-derived cells are a primitive stromal cell population. Stem Cells. 2008;26:591–9. doi: 10.1634/stemcells.2007-0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taghizadeh RR, Cetrulo KJ, Cetrulo CL. Wharton's Jelly stem cells: Future clinical applications. Placenta. 2011;32:311–5. doi: 10.1016/j.placenta.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 63.Alaminos M, Perez-Koehler B, Garzon I, et al. Transdifferentiation potentiality of human Wharton's Jelly stem cells towards vascular endothelial cells. J Cell Physiol. 2010;223:640–7. doi: 10.1002/jcp.22062. [DOI] [PubMed] [Google Scholar]
- 64.Barlow S, Brooke G, Chatterjee K, et al. Comparison of human placenta- and bone marrow-derived multipotent mesenchymal stem cells. Stem Cells Dev. 2008;17:1095–107. doi: 10.1089/scd.2007.0154. [DOI] [PubMed] [Google Scholar]
- 65.Brooke G, Tong H, Levesque J-P, Atkinson K. Molecular trafficking mechanisms of multipotent mesenchymal stem cells derived from human bone marrow and placenta. Stem Cells Dev. 2008;17:929–40. doi: 10.1089/scd.2007.0156. [DOI] [PubMed] [Google Scholar]
- 66.Mariotti E, Mirabelli P, Abate G, et al. Comparative characteristics of mesenchymal stem cells from human bone marrow and placenta: CD10. C49d.and CD56 make a difference. Stem Cells Dev . 2008; 17:1039–41. doi: 10.1089/scd.2008.0212. [DOI] [PubMed] [Google Scholar]
- 67.Rossi D, Pianta S, Magatti M, Sedlmayr P, Parolini O. Characterization of the conditioned medium from amniotic membrane cells: prostaglandins as key effectors of its immunomodulatory activity. PLoS One. 2012;7:e46956. doi: 10.1371/journal.pone.0046956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wolbank S, Peterbauer A, Fahrner M, et al. Dose-dependent immunomodulatory effect of human stem cells from amniotic membrane: a comparison with human mesenchymal stem cells from adipose tissue. Tissue Eng. 2007;13:1173–83. doi: 10.1089/ten.2006.0313. [DOI] [PubMed] [Google Scholar]
- 69.Magatti M, De Munari S, Vertua E, et al. Amniotic mesenchymal tissue cells inhibit dendritic cell differentiation of peripheral blood and amnion resident monocytes. Cell Transplant. 2009;18:899–914. doi: 10.3727/096368909X471314. [DOI] [PubMed] [Google Scholar]
- 70.De Bari C, Dell'Accio F, Tylzanowski P, Luyten FP. Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum. 2001;44:1928–42. doi: 10.1002/1529-0131(200108)44:8<1928::AID-ART331>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 71.Sakaguchi Y, Sekiya I, Yagishita K, Muneta T. Comparison of human stem cells derived from various mesenchymal tissues - Superiority of synovium as a cell source. Arthritis Rheum. 2005;52:2521–9. doi: 10.1002/art.21212. [DOI] [PubMed] [Google Scholar]
- 72.Theoret CL, Barber SM, Moyana T, Townsend HGG, Archer JF. Repair and function of synovium after arthroscopic synovectomy of the dorsal compartment of the equine antebrachiocarpal joint. Vet Surg. 1996;25:142–53. doi: 10.1111/j.1532-950x.1996.tb01390.x. [DOI] [PubMed] [Google Scholar]
- 73.Jones EA, Crawford A, English A, et al. Synovial fluid mesenchymal stem cells in health and early osteoarthritis - Detection and functional evaluation at the single-cell level. Arthritis Rheum. 2008;58:1731–40. doi: 10.1002/art.23485. [DOI] [PubMed] [Google Scholar]
- 74.McGonagle D, Jones E. A potential role for synovial fluid mesenchymal stem cells in ligament regeneration. Rheumatology (Oxford) 2008;47:1114–6. doi: 10.1093/rheumatology/ken236. [DOI] [PubMed] [Google Scholar]
- 75.Wickham MQ, Erickson GR, Gimble JM, Vail TP, Guilak F. Multipotent stromal cells derived from the infrapatellar fat pad of the knee. Clin Orthop Relat Res. 2003:196–212. doi: 10.1097/01.blo.0000072467.53786.ca. [DOI] [PubMed] [Google Scholar]
- 76.Nakahara H, Goldberg VM, Caplan AI. Culture-expanded human periosteal-derived cells exhibit osteochondral potential in vivo. J Orthop Res. 1991;9:465–76. doi: 10.1002/jor.1100090402. [DOI] [PubMed] [Google Scholar]
- 77.Brighton CT, Lorich DG, Kupcha R, Reilly TM, Jones AR, Woodbury RA. The pericyte as a possible osteoblast progenitor-cell. Clin Orthop Relat Res. 1992:287–99. [PubMed] [Google Scholar]
- 78.Zvaifler NJ, Marinova-Mutafchieva L, Adams G, et al. Mesenchymal precursor cells in the blood of normal individuals. Arthritis Res. 2000;2:477–88. doi: 10.1186/ar130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Young HE, Steele TA, Bray RA, et al. Human reserve pluripotent mesenchymal stem cells are present in the connective tissues of skeletal muscle and dermis derived from fetal. ault.and geriatric donors. Anat Rec. 2001; 264:51–62. doi: 10.1002/ar.1128. [DOI] [PubMed] [Google Scholar]
- 80.Osyczka AM, Noth U, Danielson KG, Tuan RS. Different osteochondral potential of clonal cell lines derived from adult human trabecular bone. Ann N Y Acad Sci. 2002;961:73–7. doi: 10.1111/j.1749-6632.2002.tb03054.x. [DOI] [PubMed] [Google Scholar]
- 81.Lu HH, Kofron MD, El-Amin SF, Attawia MA, Laurencin CT. In vitro bone formation using muscle-derived cells: a new paradigm for bone tissue engineering using polymer-bone morphogenetic protein matrices. Biochem Biophys Res Commun. 2003;305:882–9. doi: 10.1016/s0006-291x(03)00858-1. [DOI] [PubMed] [Google Scholar]
- 82.Hu Y, Liao LM, Wang LY, et al. Isolation and identification of mesenchymal stem cells from human fetal pancreas. J Lab Clin Med. 2003;141:342–9. doi: 10.1016/S0022-2143(03)00022-2. [DOI] [PubMed] [Google Scholar]
- 83.Trubiani O, Di Primo R, Traini T, et al. Morphological and cytofluorimetric analysis of adult mesenchymal stem cells expanded ex vivo from periodontal ligament. Int J Immunopathol Pharmacol. 2005;18:213–21. doi: 10.1177/039463200501800204. [DOI] [PubMed] [Google Scholar]
- 84.Patel AN, Park E, Kuzman M, Benetti F, Silva FJ, Allickson JG. Multipotent menstrual blood stromal stem cells: isolation. characterizion.aand differentiation. Cell Transplant. 2008; 17:303–11. doi: 10.3727/096368908784153922. [DOI] [PubMed] [Google Scholar]
- 85.Patki S, Kadam S, Chandra V, Bhonde R. Human breast milk is a rich source of multipotent mesenchymal stem cells. Hum Cell. 2010;23:35–40. doi: 10.1111/j.1749-0774.2010.00083.x. [DOI] [PubMed] [Google Scholar]
- 86.Bharadwaj S, Liu G, Shi Y, et al. Characterization of urine-derived stem cells obtained from upper urinary tract for use in cell-based urological tissue engineering. Tissue Eng. 2011;17:2123–32. doi: 10.1089/ten.tea.2010.0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bernardo ME, Avanzini MA, Ciccocioppo R, et al. Phenotypical/functional characterization of in vitro-expanded mesenchymal stromal cells from patients with Crohn's disease. Cytotherapy. 2009;11:825–36. doi: 10.3109/14653240903121260. [DOI] [PubMed] [Google Scholar]
- 88.Le Blanc K, Frassoni F, Ball L, et al. Mesenchymal stem cells for treatment of steroid-resistant. seere.acute graft-versus-host diseasea phase II study. Lancet . 2008;371 :1579–86. doi: 10.1016/S0140-6736(08)60690-X. [DOI] [PubMed] [Google Scholar]
- 89.Spees JL, Gregory CA, Singh H, et al. Internalized antigens must be removed to prepare hypoimmunogenic mesenchymal stem cells for cell and gene therapy. Mol Ther. 2004;9:747–56. doi: 10.1016/j.ymthe.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 90.Shahdadfar A, Fronsdal K, Haug T, Reinholt FP, Brinchmann JE. In vitro expansion of human mesenchymal stem cells: Choice of serum is a determinant of cell proliferation. differentiaion.gene expression., and transcriptome stability. Stem Cells . 2005;23:1357–66. doi: 10.1634/stemcells.2005-0094. [DOI] [PubMed] [Google Scholar]
- 91.Jung S, Sen A, Rosenberg L, Behie LA. Identification of growth and attachment factors for the serum-free isolation and expansion of human mesenchymal stromal cells. Cytotherapy. 2010;12:637–57. doi: 10.3109/14653249.2010.495113. [DOI] [PubMed] [Google Scholar]
- 92.Doucet C, Ernou I, Zhang YZ, et al. Platelet lysates promote mesenchymal stem cell expansion: A safety substitute for animal serum in cell-based therapy applications. J Cell Physiol. 2005;205:228–36. doi: 10.1002/jcp.20391. [DOI] [PubMed] [Google Scholar]
- 93.Avanzini MA, Bernardo ME, Cometa AM, et al. Generation of mesenchymal stromal cells in the presence of platelet lysate: a phenotypic and functional comparison of umbilical cord blood- and bone marrow-derived progenitors. Haematologica. 2009;94:1649–60. doi: 10.3324/haematol.2009.006171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lucarelli E, Beccheroni A, Donati D, et al. Platelet-derived growth factors enhance proliferation of human stromal stem cells. Biomaterials. 2003;24:3095–100. doi: 10.1016/s0142-9612(03)00114-5. [DOI] [PubMed] [Google Scholar]
- 95.Bernardo ME, Avanzini MA, Perotti C, et al. Optimization of in vitro expansion of human multipotent mesenchymal stromal cells for cell-therapy approaches: further insights in the search for a fetal calf serum substitute. J Cell Physiol. 2007;211:121–30. doi: 10.1002/jcp.20911. [DOI] [PubMed] [Google Scholar]
- 96.Schallmoser K, Bartmann C, Rohde E, et al. Replicative senescence-associated gene expression changes in mesenchymal stromal cells are similar under different culture conditions. Haematologica. 2010;95:867–74. doi: 10.3324/haematol.2009.011692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dazzi F, Krampera M. Mesenchymal stem cells and autoimmune diseases. Best Pract Res Clin Haematol. 2011;24:49–57. doi: 10.1016/j.beha.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 98.Krampera M, Cosmi L, Angeli R, et al. Role for interferon-gamma in the immunomodulatory activity of human bone marrow mesenchymal stem cells. Stem Cells. 2006;24:386–98. doi: 10.1634/stemcells.2005-0008. [DOI] [PubMed] [Google Scholar]
- 99.Ren G, Zhang L, Zhaon X, et al. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell. 2008;2:141–50. doi: 10.1016/j.stem.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 100.Nemeth K, Mayer B, Mezey E. Modulation of bone marrow stromal cell functions in infectious diseases by toll-like receptor ligands. J Mol Med. 2010;88:5–10. doi: 10.1007/s00109-009-0523-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM. A new mesenchymal stem cell (MSC) paradigm: polarization into a pro-inflammatory MSC1 or an Immunosuppressive MSC2 phenotype. PLoS One. 2010;5:e10088. doi: 10.1371/journal.pone.0010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wagner W, Ho AD, Zenke M. Different Facets of Aging in Human Mesenchymal Stem Cells. Tissue Eng. 2010;16:445–53. doi: 10.1089/ten.TEB.2009.0825. [DOI] [PubMed] [Google Scholar]
- 103.Mohseny AB, Szuhai K, Romeo S, et al. Osteosarcoma originates from mesenchymal stem cells in consequence of aneuploidization and genomic loss of Cdkn2. J Pathol. 2009;219:294–305. doi: 10.1002/path.2603. [DOI] [PubMed] [Google Scholar]
- 104.Karnoub AE, Dash AB, Vo AP, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–63. doi: 10.1038/nature06188. [DOI] [PubMed] [Google Scholar]
- 105.Wang Y, Huso DL, Harrington J, et al. Outgrowth of a transformed cell population derived from normal human BM mesenchymal stem cell culture. Cytotherapy. 2005;7:509–19. doi: 10.1080/14653240500363216. [DOI] [PubMed] [Google Scholar]
- 106.Achille V, Mantelli M, Arrigo G, et al. Cell-cycle phases and genetic profile of bone marrow-derived mesenchymal stromal cells expanded in vitro from healthy donors. J Cell Biochem. 2011;112:1817–21. doi: 10.1002/jcb.23100. [DOI] [PubMed] [Google Scholar]
- 107.Rubio D, Garcia-Castro J, Martin MC, et al. Spontaneous human adult stem cell transformation (Retracted article.See vol. 70. pg. 6682. 2010). Cancer Res. 2005;65:3035–9. doi: 10.1158/0008-5472.CAN-04-4194. [DOI] [PubMed] [Google Scholar]
- 108.Rosland GV, Svendsen A, Torsvik A, et al. Long-term cultures of bone marrow-derived human mesenchymal stem cells frequently undergo spontaneous malignant transformation (This article contains errors due to a cross contamination of the cell lines we used.To correct this issue we published a letter in Cancer Res. 2010 Ag 1.0(15).,6393-6). Cancer Res. 2009; 69:5331–9. doi: 10.1158/0008-5472.CAN-08-4630. [DOI] [PubMed] [Google Scholar]
- 109.Garcia S, Bernad A, Martin MC, et al. Pitfalls in spontaneous in vitro transformation of human mesenchymal stem cells. Exp Cell Res. 2010;316:1648–50. doi: 10.1016/j.yexcr.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 110.Torsvik A, Rosland GV, Svendsen A, et al. Spontaneous malignant transformation of human mesenchymal stem cells reflects cross-contamination: putting the research field on track (Correction letter for Cancer Res.20 9Jul 1 69(13) 5331-9). Cancer Res. 2010; 70:6393–6. doi: 10.1158/0008-5472.CAN-10-1305. [DOI] [PubMed] [Google Scholar]
- 111.Lalu MM, McIntyre L, Pugliese C, et al. Safety of Cell Therapy with Mesenchymal Stromal Cells (SafeCell): A Systematic Review and Meta-Analysis of Clinical Trials. PLoS One. 2012;7:e47559. doi: 10.1371/journal.pone.0047559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bernardo ME, Zaffaroni N, Novara F, et al. Human bone marrow-derived mesenchymal stem cells do not undergo transformation after long-term In vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res. 2007;67:9142–9. doi: 10.1158/0008-5472.CAN-06-4690. [DOI] [PubMed] [Google Scholar]
- 113.Krampera M, Pasini A, Pizzolo G, Cosmi L, Romagnani S, Annunziato F. Regenerative and immunomodulatory potential of mesenchymal stem cells. Curr Opin Pharmacol. 2006;6:435–41. doi: 10.1016/j.coph.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 114.Rehman J, Traktuev D, Li JL, Merfeld-Clauss S, et al. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109:1292–8. doi: 10.1161/01.CIR.0000121425.42966.F1. [DOI] [PubMed] [Google Scholar]
- 115.Sorrell JM, Baber MA, Caplan AI. Influence of adult mesenchymal stem cells on in vitro vascular formation. Tissue Eng. 2009;15:1751–61. doi: 10.1089/ten.tea.2008.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Majumdar MK, Thiede MA, Mosca JD, Moorman M, Gerson SL. Phenotypic and functional comparison of cultures of marrow-derived mesenchymal stem cells (MSCs) and stromal cells. J Cell Physiol. 1998;176:57–66. doi: 10.1002/(SICI)1097-4652(199807)176:1<57::AID-JCP7>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 117.Le Blanc K, Tammik C, Rosendahl K, Zetterberg E, Ringden O. HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol. 2003;31:890–6. doi: 10.1016/s0301-472x(03)00110-3. [DOI] [PubMed] [Google Scholar]
- 118.Le Blanc K, Ringden O. Immunobiology of human mesenchymal stem cells and future use in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005;11:321–34. doi: 10.1016/j.bbmt.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 119.Götherström C, Ringdén O, Tammik C, Zetterberg E, Westgren M, Le Blanc K. Immunologic properties of human fetal mesenchymal stem cells. Am J Obstet Gynecol. 2004;190:239–45. doi: 10.1016/j.ajog.2003.07.022. [DOI] [PubMed] [Google Scholar]
- 120.Nauta AJ, Westerhuis G, Kruisselbrink AB, Lurvink EGA, Willemze R, Fibbe WE. Donor-derived mesenchymal stem cells are immunogenic in an allogeneic host and stimulate donor graft rejection in a nonmyeloablative setting. Blood. 2006;108:2114–20. doi: 10.1182/blood-2005-11-011650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Spaggiari GM, Capobianco A, Becchetti S, Mingari MC, Moretta L. Mesenchymal stem cell-natural killer cell interactions: evidence that activated NK cells are capable of killing MSCs. whereas MSCs can inhibit IL-2-induced NK-cell proliferation. . Blood. 2006;107:1484–90. doi: 10.1182/blood-2005-07-2775. [DOI] [PubMed] [Google Scholar]
- 122.Locatelli F, Maccario R, Frassoni F. Mesenchymal stromal cells. from indifferent spectators to principal actors. Are we going to witness a revolution in the scenario of allograft and immune-mediated disorders?. Haematologica. 2007;92:872–7. doi: 10.3324/haematol.11479. [DOI] [PubMed] [Google Scholar]
- 123.Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726–36. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]
- 124.Raffaghello L, Bianchi G, Bertolotto M, et al. Human mesenchymal stem cells inhibit neutrophil apoptosis: A model for neutrophil preservation in the bone marrow niche. Stem Cells. 2008;26:151–62. doi: 10.1634/stemcells.2007-0416. [DOI] [PubMed] [Google Scholar]
- 125.Maccario R, Podesta M, Moretta A, et al. Interaction of human mesenchymal stem cells with cells involved in alloantigen-specific immune response favors the differentiation of CD4(+). T-cell subsets expressing a regulatory/suppressive phenotype. Haematologica. 2005;90:516–25. [PubMed] [Google Scholar]
- 126.Corcione A, Benvenuto F, Ferretti E, et al. Human mesenchymal stem cells modulate B-cell functions. Blood. 2006;107:367–72. doi: 10.1182/blood-2005-07-2657. [DOI] [PubMed] [Google Scholar]
- 127.Comoli P, Ginevri F, Maccario R, et al. Human mesenchymal stem cells inhibit antibody production induced in vitro by allostimulation. Nephrol Dial Transplant. 2008;23:1196–202. doi: 10.1093/ndt/gfm740. [DOI] [PubMed] [Google Scholar]
- 128.Collino F, Deregibus MC, Bruno S, et al. Microvesicles derived from adult human bone marrow and tissue specific mesenchymal stem cells shuttle selected pattern of mirnas. PloS One. 2010;5:e11803. doi: 10.1371/journal.pone.0011803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sethe S, Scutt A, Stolzing A. Aging of mesenchymal stem cells. Ageing Res Rev. 2006;5:91–116. doi: 10.1016/j.arr.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 130.Alt EU, Senst C, Murthy SN, et al. Aging alters tissue resident mesenchymal stem cell properties. Stem Cell Res. 2012;8:215–25. doi: 10.1016/j.scr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 131.Jakob F, Ebert R, Rudert M, et al. In situ guided tissue regeneration in musculoskeletal diseases and aging Implementing pathology into tailored tissue engineering strategies. Cell Tissue Res. 2012;347:725–35. doi: 10.1007/s00441-011-1237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mansilla E, Diaz Aquino V, Zambon D, et al. Could metabolic syndrome. lipodystrphy.and aging be mesenchymal stem cell exhaustion syndromes?. Stem Cells Int. 2011; 2011:1–10. doi: 10.4061/2011/943216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Guan M, Yao W, Liu R, et al. Directing mesenchymal stem cells to bone to augment bone formation and increase bone mass. Nature Med. 2012;18:456–63. doi: 10.1038/nm.2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cai B, Zhu S, Li J, Chen N, Liu Y, Lu Y. Bone marrow-derived mesenchymal stem cells protected rat cardiomyocytes from premature senescence. Int J Cardiol. 2012;154:180–223. doi: 10.1016/j.ijcard.2011.05.032. [DOI] [PubMed] [Google Scholar]
- 135.Fazel S, Cimini M, Chen L, et al. Cardioprotective c-kit+ cells are from the bone marrow and regulate the myocardial balance of angiogenic cytokines. J Clin Invest. 2006;116:1865–77. doi: 10.1172/JCI27019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Vassalli G, Moccetti T. Cardiac repair with allogeneic mesenchymal stem cells after myocardial infarction. Swiss Med Wkly. 2011;141:1–6. doi: 10.4414/smw.2011.13209. [DOI] [PubMed] [Google Scholar]
- 137.Lee S, Szilagyi E, Chen L, et al. Activated mesenchymal stem cells increase wound tensile strength in aged mouse model via macrophages. J Surg Res. 2012 doi: 10.1016/j.jss.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 138.Wong RSY. Mesenchymal Stem Cells: Angels or Demons. J Biomed Biotechnol. 2011;2011 doi: 10.1155/2011/459510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ding DC, Shyu WC, Lin SZ. Mesenchymal Stem Cells. Cell Transplant. 2011;20:5–14. doi: 10.3727/096368910X. [DOI] [PubMed] [Google Scholar]
- 140.Caplan AI. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol. 2007;213:341–7. doi: 10.1002/jcp.21200. [DOI] [PubMed] [Google Scholar]
- 141.Otto WR, Wright NA. Mesenchymal stem cells from experiment to clinic. Fibrogenesis Tissue Repair. 2011;4:20. doi: 10.1186/1755-1536-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kurtz A. Mesenchymal stem cell delivery routes and fate. Int J Stem Cells. 2008;1:1–7. doi: 10.15283/ijsc.2008.1.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.ClinicalTrials.ov [homepage on the Internet]. The U.S. National Institutes of Health [cited 2012 Oct 18]. Available from: http://www.clinicaltrials.gov. [Google Scholar]
- 144.Parekkadan B, Milwid JM. Mesenchymal stem cells as therapeutics. Annu Rev Biomed Eng. 2010;12:87–117. doi: 10.1146/annurev-bioeng-070909-105309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Horwitz EM, Gordon PL, Koo WK, et al. Isolated allogeneic bone marrow-derived mesenchymal cells engraft and stimulate growth in children with osteogenesis imperfecta: implications for cell therapy of bone. Proc Natl Acad Sci USA. 2002;99:8932–37. doi: 10.1073/pnas.132252399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ball LM, Bernardo ME, Roelofs H, et al. Cotransplantation of ex vivo-expanded mesenchymal stem cells accelerates lymphocyte recovery and may reduce the risk of graft failure in haploidentical hematopoietic stem-cell transplantation. Blood. 2007;110:2764–7. doi: 10.1182/blood-2007-04-087056. [DOI] [PubMed] [Google Scholar]
- 147.Duijvenstein M, Vos ACW, Roelofs H, et al. Autologous bone marrow-derived mesenchymal stromal cell treatment for refractory luminal Crohn’s disease: results of a phase I study. Gut. 2010;59:1662–9. doi: 10.1136/gut.2010.215152. [DOI] [PubMed] [Google Scholar]
- 148.Ciccocioppo R, Bernardo ME, Sgarella A, et al. Autologous bone marrow-derived mesenchymal stromal cells in the treatment of fistulising Crohn's disease. Gut. 2011;60:788–98. doi: 10.1136/gut.2010.214841. [DOI] [PubMed] [Google Scholar]
- 149.Horwitz EM, Prockop DJ, Fitzpatrick LA, et al. Transplantability and therapeutic effects of bone marrow-derived mesenchymal cells in children with osteogenesis imperfecta. Nat Med. 1999;5:309–13. doi: 10.1038/6529. [DOI] [PubMed] [Google Scholar]
- 150.Breitbach M, Bostani T, Roell W, et al. Potential risks of bone marrow cell transplantation into infarcted hearts. Blood. 2007;110:1362–9. doi: 10.1182/blood-2006-12-063412. [DOI] [PubMed] [Google Scholar]
- 151.Kunter U, Rong S, Boor P, et al. Mesenchymal stem cells prevent progressive experimental renal failure but maldifferentiate into glomerular adipocytes. J Am Soc Nephrol. 2007;18:1754–64. doi: 10.1681/ASN.2007010044. [DOI] [PubMed] [Google Scholar]
- 152.Le Blanc K, Rasmusson I, Sundberg B, et al. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet. 2004;363:1439–41. doi: 10.1016/S0140-6736(04)16104-7. [DOI] [PubMed] [Google Scholar]
- 153.Ball LM, Bernardo ME, van Tol MJD, et al. Mesenchymal stromal cells are highly effective in steroid-refractory. grade III-IV acute graft-versus-host disease in children. Bone Marrow Transplant. 2011;46:6–7. [Google Scholar]
- 154.Kebriaei P, Isola L, Bahceci E, et al. Adult human mesenchymal stem cells added to corticosteroid therapy for the treatment of acute graft-versus-host disease. Biol Blood and Marrow Transplant. 2009;15:804–11. doi: 10.1016/j.bbmt.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 155.Lucchini G, Dander E, Pavan F, et al. Platelet-lysate-expanded mesenchymal stromal cells for the treatment of steroid resistant GvHD: clinical results and biological readouts in a multicentre study. Bone Marrow Transplant. 2012;47:55–6. [Google Scholar]
- 156.Introna M, Lucchini G, Dander E, et al. Safe and effective treatment of Graft versus Host Disease with platelet lysate-expanded human mesenchymal stromal cells: a phase 1 study on 47 adult and pediatric patients. Blood (ASH Annual Meeting Abstracts). 2012;120:743. [Google Scholar]
- 157.Choi SW, Levine JE, Ferrara JLM. Pathogenesis and management of Graft-versus-Host Disease. Immunol Allergy Clin North Am. 2010;30:75–101. doi: 10.1016/j.iac.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dander E, Lucchini G, Vinci P, et al. Mesenchymal stromal cells for the treatment of Graft-versus-Host Disease: understanding the in vivo biological effect through patient immune monitoring. Leukemia. 2012;26:1681–4. doi: 10.1038/leu.2011.384. [DOI] [PubMed] [Google Scholar]
- 159.Cho JH. The genetics and immunopathogenesis of inflammatory bowel disease. Nat Rev Immunol. 2008;8:458–66. doi: 10.1038/nri2340. [DOI] [PubMed] [Google Scholar]
- 160.Gonzalez MA, Gonzalez-Rey E, Rico L, Buescher D, Delgado M. Adipose-derived mesenchymal stem cells alleviate experimental colitis by inhibiting inflammatory and autoimmune responses. Gastroenterology. 2009;136:978–89. doi: 10.1053/j.gastro.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 161.Zhang Q, Shi S, Liu Y, et al. Mesenchymal stem cells derived from human gingiva are capable of immunomodulatory functions and ameliorate inflammation-related tissue destruction in experimental colitis. J Immunol. 2009;183:7787–98. doi: 10.4049/jimmunol.0902318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Garcia-Olmo D, Garcia-Arranz M, Herreros D, Pascual I, Peiro C, Rodriguez-Montes JA. A phase I clinical trial of the treatment of Crohn's fistula by adipose mesenchymal stem cell transplantation. Dis Colon Rectum. 2005;48:1416–23. doi: 10.1007/s10350-005-0052-6. [DOI] [PubMed] [Google Scholar]
- 163.Almeida-Porada G, Porada CD, Tran N, Zanjani ED. Cotransplantation of human stromal cell progenitors into preimmune fetal sheep results in early appearance of human donor cells in circulation and boosts cell levels in bone marrow at later time points after transplantation. Blood. 2000;95:3620–7. [PubMed] [Google Scholar]
- 164.Koc ON, Gerson SL, Cooper BW, et al. Rapid hematopoietic recovery after coinfusion of autologous-blood stem cells and culture-expanded marrow mesenchymal stem cells in advanced breast cancer patients receiving high-dose chemotherapy. J Clin Oncol. 2000;18:307–16. doi: 10.1200/JCO.2000.18.2.307. [DOI] [PubMed] [Google Scholar]
- 165.Lazarus HM, Koc ON, Devine SM, et al. Cotransplantation of HLA-identical sibling culture-expanded mesenchymal stem cells and hematopoietic stem cells in hematologic malignancy patients. Biol Blood Marrow Transplant. 2005;11:389–98. doi: 10.1016/j.bbmt.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 166.Bernardo ME, Ball LM, Cometa AM, et al. Co-infusion of ex vivo-expanded parental MSCs prevents life-threatening acute .VHD.but does not reduce the risk of graft failure in pediatric patients undergoing allogeneic umbilical cord blood transplantation. Bone Marrow Transplant. 2011; 46:200–7. doi: 10.1038/bmt.2010.87. [DOI] [PubMed] [Google Scholar]
- 167.Otsuru S, Gordon PL, Shimono K, et al. Transplanted bone marrow mononuclear cells and MSCs impart clinical benefit to children with osteogenesis imperfecta through different mechanisms. Blood. 2012;120:1933–41. doi: 10.1182/blood-2011-12-400085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Shekkeris AS, Jaiswal PK, Khan WS. Clinical applications of mesenchymal stem cells in the treatment of fracture non-union and bone defects. Curr Stem Cell Res Ther. 2012;7:127–33. doi: 10.2174/157488812799218956. [DOI] [PubMed] [Google Scholar]
- 169.Morishita T, Honoki K, Ohgushi H, Kotobuki N, Matsushima A, Takakura Y. Tissue engineering approach to the treatment of bone tumors: three cases of cultured bone grafts derived from patients' mesenchymal stem cells. Artif Organs. 2006;30:115–8. doi: 10.1111/j.1525-1594.2006.00190.x. [DOI] [PubMed] [Google Scholar]
- 170.Ohgushi H, Kotobuki N, Funaoka H, et al. Tissue engineered ceramic artificial joint - ex vivo osteogenic differentiation of patient mesenchymal cells on total ankle joints for treatment of osteoarthritis. Biomaterials. 2005;26:4654–61. doi: 10.1016/j.biomaterials.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 171.Connolly JF. Injectable bone-marrow preparations to stimulate osteogenic repair. Clin Orthop Relat Res. 1995:8–18. [PubMed] [Google Scholar]
- 172.Hernigou P, Poignard A, Zilber S, Rouard H. Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop. 2009;43:40–5. doi: 10.4103/0019-5413.45322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gangji V, DeMaertelaer V, Hauzeur JP. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head five year follow-up of a prospective controlled study. Bone. 2011;49:1005–9. doi: 10.1016/j.bone.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 174.DiBella C, Dozza B, Frisoni T, Cevolani L, Donati D. Injection of demineralized bone matrix with bone marrow concentrate improves healing in unicameral bone cyst. Clin Orthop Relat Res. 2010;468:3047–55. doi: 10.1007/s11999-010-1430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wakitani S, Okabe T, Horibe S, et al. Safety of autologous bone marrow-derived mesenchymal stem cell transplantation for cartilage repair in 41 patients with 45 joints followed for up to 11 years and 5 months. J Tissue Eng Regen Med. 2011;5:146–50. doi: 10.1002/term.299. [DOI] [PubMed] [Google Scholar]
- 176.Haleem AM, El Singergy AA, Sabry D, et al. The clinical use of human culture-expanded autologous bone marrow mesenchymal stem cells transplanted on platelet-rich fibrin glue in the treatment of articular cartilage defects: a pilot study and preliminary results. Cartilage. 2010;1:253–61. doi: 10.1177/1947603510366027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Acharya C, Adesida A, Zajac P, et al. Enhanced chondrocyte proliferation and mesenchymal stromal cells chondrogenesis in coculture pellets mediate improved cartilage formation. J Cell Physiol. 2012;227:88–97. doi: 10.1002/jcp.22706. [DOI] [PubMed] [Google Scholar]
- 178.Cooke ME, Allon AA, Cheng T, et al. Structured three-dimensional co-culture of mesenchymal stem cells with chondrocytes promotes chondrogenic differentiation without hypertrophy. Osteoarthritis Cartilage. 2011;19:1210–8. doi: 10.1016/j.joca.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gaetani P, Torre ML, Klinger M, et al. Adipose-derived stem cell therapy for intervertebral disc regeneration: An in vitro reconstructed tissue in alginate capsules. Tissue Eng. 2008;14:1415–23. doi: 10.1089/ten.tea.2007.0330. [DOI] [PubMed] [Google Scholar]
- 180.Chlapanidas T, Farago S, Mingotto F, et al. Regenerated silk fibroin scaffold and infrapatellar adipose stromal vascular fraction as feeder-layer: a new product for cartilage advanced therapy. Tissue Eng. 2011;17:1725–33. doi: 10.1089/ten.TEA.2010.0636. [DOI] [PubMed] [Google Scholar]
- 181.Slynarski K, Deszczynski J, Karpinski J. Fresh bone marrow and periosteum transplantation for cartilage defects of the knee. Transplantat Proc. 2006;38:318–9. doi: 10.1016/j.transproceed.2005.12.075. [DOI] [PubMed] [Google Scholar]
- 182.de Girolamo L, Bertolini G, Cervellin M, Sozzi G, Volpi P. Treatment of chondral defects of the knee with one step matrix-assisted technique enhanced by autologous concentrated bone marrow: In vitro characterisation of mesenchymal stem cells from iliac crest and subchondral bone. Injury. 2010;41:1172–7. doi: 10.1016/j.injury.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 183.Buda R, Vannini F, Cavallo M, Grigolo B, Cenacchi A, Giannini S. Osteochondral lesions of the knee: a new one-step repair technique with bone-marrow-derived cells. J Bone Joint Surg Am. 2010;92A:2–11. doi: 10.2106/JBJS.J.00813. [DOI] [PubMed] [Google Scholar]
- 184.Guo X, Zheng Q, Yang S, et al. Repair of full-thickness articular cartilage defects by cultured mesenchymal stem cells transfected with the transforming growth factor beta(1) gene. Biomed Mater. 2006;1:206–15. doi: 10.1088/1748-6041/1/4/006. [DOI] [PubMed] [Google Scholar]
- 185.Cucchiarini M, Ekici M, Schetting S, Kohn D, Madry H. Metabolic activities and chondrogenic differentiation of human mesenchymal stem cells following recombinant adeno-associated virus-mediated gene transfer and overexpression of fibroblast growth factor 2. Tissue Eng. 2011;17:1921–33. doi: 10.1089/ten.TEA.2011.0018. [DOI] [PubMed] [Google Scholar]
- 186.Price R, Anthony E, Myers S, Navsaria H. Tissue engineering for skin transplantation.In: Van Blitterswijk C eds. Tissue Engineering. Elsevier Inc. 2008: 507–32. [Google Scholar]
- 187.Marazzi M, Crovato F, Bucco M, et al. GMP-compliant culture of human hair follicle cells for encapsulation and transplantation. Cell Transplant. 2012;21:373–8. doi: 10.3727/096368911X565010. [DOI] [PubMed] [Google Scholar]
- 188.Arno A, Smith AH, Blit PH, Al Shehab M, Gauglitz GG, Jeschke MG. Stem cell therapy: A new treatment for burns?. Pharmaceuticals. 2011;4:1355–80. doi: 10.3390/ph4101355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Rheinwald JG, Green H. Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell. 1975;6:331–43. doi: 10.1016/s0092-8674(75)80001-8. [DOI] [PubMed] [Google Scholar]
- 190.Schreml S, Szeimies R-M, Prantl L, Landthaler M, Babilas P. Wound healing in the 21st century. J Am Acad Dermatol. 2010;63:866–81. doi: 10.1016/j.jaad.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 191.Berthiaume F, Maguire TJ, Yarmush ML. Tissue engineering and regenerative medicine: history. progess.and challenges. Ann Rev Chem Biomol Eng. 2011; 2:403–30. doi: 10.1146/annurev-chembioeng-061010-114257. [DOI] [PubMed] [Google Scholar]
- 192.Lau K, Paus R, Tiede S, Day P, Bayat A. Exploring the role of stem cells in cutaneous wound healing. Exp Dermtol. 2009;18:921–33. doi: 10.1111/j.1600-0625.2009.00942.x. [DOI] [PubMed] [Google Scholar]
- 193.Sorrell JM, Caplan AI. Topical delivery of mesenchymal stem cells and their function in wounds. Stem Cell Res Ther. 2010;1:30. doi: 10.1186/scrt30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Nauta A, Gurtner GC, Longaker MT. Wound healing and regenerative strategies. Oral Diseases. 2011;17:541–9. doi: 10.1111/j.1601-0825.2011.01787.x. [DOI] [PubMed] [Google Scholar]
- 195.Guisantes E, Fontdevila J, Rodríguez G. Autologous fat grafting for unaesthetic scars correction. Ann Plast Surg. 2011 doi: 10.1097/SAP.0b013e31821ee386. [DOI] [PubMed] [Google Scholar]
- 196.Klinger M, Marazzi M, Vigo D, Torre M. Fat injection for cases of severe burn outcomes: A new perspective of scar remodeling and reduction. Aesthetic Plast Surg. 2008;32:465–9. doi: 10.1007/s00266-008-9122-1. [DOI] [PubMed] [Google Scholar]
- 197.Kaufman MR, Bradley JP, Dickinson B, et al. Autologous fat transfer national consensus survey: Trends in techniques for harvest. preparaion.and application., and perception of short- and long-term results. . Plast Reconstr Surg. 2007; 119:323–31. doi: 10.1097/01.prs.0000244903.51440.8c. [DOI] [PubMed] [Google Scholar]
- 198.Tremolada C, Palmieri G, Ricordi C. Adipocyte transplantation and stem cells: plastic surgery meets regenerative medicine. Cell Transplant. 2010;19:1217–23. doi: 10.3727/096368910X507187. [DOI] [PubMed] [Google Scholar]
- 199.Mareschi K, Novara M, Rustichelli D, et al. Neural differentiation of human mesenchymal stem cells: evidence for expression of neural markers and eag K+ channel types. Exp Hematol. 2006;34:1563–72. doi: 10.1016/j.exphem.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 200.Wislet-Gendebien S, Laudet E, Neirinckx V, Rogister B. Adult Bone Marrow: Which stem cells for cellular therapy protocols in neurodegenerative disorders?. J Biomed Biotechnol. 2012;2012 doi: 10.1155/2012/601560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Zhang Z, Wang X, Wang S. Isolation and characterization of mesenchymal stem cells derived from bone marrow of patients with Parkinson's disease. In vitro Cell Dev Biol Anim. 2008;44:169–77. doi: 10.1007/s11626-008-9093-1. [DOI] [PubMed] [Google Scholar]
- 202.Vercelli A, Mereuta OM, Garbossa D, et al. Human mesenchymal stem cell transplantation extends survival. improves motor performance and decreases neuroinflammation in mouse model of amyotrophic lateral sclerosis. Neurobiol Dis. 2008;31:395–405. doi: 10.1016/j.nbd.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 203.Ferrero I, Mazzini L, Rustichelli D, et al. Bone marrow mesenchymal stem cells from healthy donors and sporadic amyotrophic lateral sclerosis patients. Cell Transplant. 2008;17:255–66. doi: 10.3727/096368908784153940. [DOI] [PubMed] [Google Scholar]
- 204.Mazzini L, Mareschi K, Ferrero I, et al. Mesenchymal stromal cell transplantation in amyotrophic lateral sclerosis: a long-term safety study. Cytotherapy. 2012;14:56–60. doi: 10.3109/14653249.2011.613929. [DOI] [PubMed] [Google Scholar]
- 205.Loebinger MR, Eddaoudi A, Davies D, Janes SM. Mesenchymal stem cell delivery of trail can eliminate metastatic cancer. Cancer Res. 2009;69:4134–42. doi: 10.1158/0008-5472.CAN-08-4698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Nakamizo A, Marini F, Amano T, et al. Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Res. 2005;65:3307–18. doi: 10.1158/0008-5472.CAN-04-1874. [DOI] [PubMed] [Google Scholar]
- 207.Nakamura K, Ito Y, Kawano Y, et al. Antitumor effect of genetically engineered mesenchymal stem cells in a rat glioma model. Gene Therapy. 2004;11:1155–64. doi: 10.1038/sj.gt.3302276. [DOI] [PubMed] [Google Scholar]
- 208.Menon LG, Shi VJ, Carroll RS, Menon LGSV, Carroll RS, editors. 2008. StemBook: Cambridg MA.: Harvard Stem Cell Institute; Mesenchymal stromal cells as a drug delivery system.In:. . [PubMed] [Google Scholar]
- 209.Stagg J, Lejeune L, Paquin A, Galipeau J. Marrow stromal cells for interleukin-2 delivery in cancer immunotherapy. Human Gene Ther. 2004;15:597–608. doi: 10.1089/104303404323142042. [DOI] [PubMed] [Google Scholar]
- 210.Kucerova L, Altanerova V, Matuskova M, Tyciakova S, Altaner C. Adipose tissue-derived human mesenchymal stem cells mediated prodrug cancer gene therapy. Cancer Res. 2007;67:6304–13. doi: 10.1158/0008-5472.CAN-06-4024. [DOI] [PubMed] [Google Scholar]
- 211.Studeny M, Marini FC, Champlin RE, Zompetta C, Fidler IJ, Andreeff M. Bone marrow-derived mesenchymal stem cells as vehicles for interferon-beta delivery into tumors. Cancer Res. 2002;62:3603–8. [PubMed] [Google Scholar]
- 212.Shah K. Mesenchymal stem cells engineered for cancer therapy. Adv Drug Deliv Rev. 2012;64:739–48. doi: 10.1016/j.addr.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Zhang X-B, Beard BC, Trobridge GD, et al. High incidence of leukemia in large animals after stem cell gene therapy with a HOXB4-expressing retroviral vector. J Clin Invest. 2008;118:1502–10. doi: 10.1172/JCI34371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Cocke KS, Updyke LW, Wierda D. Mouse bone marrow stromal cells can accumulate and release cytotoxic concentrations of doxorubicin into the hematopoietic microenvironment. In vitro Toxicol. 1993;6:243–56. [Google Scholar]
- 215.Pessina A, Piccirillo M, Mineo E, et al. Role of SR-4987 stromal cells in the modulation of doxorubicin toxicity to in vitro granulocyte-macrophage progenitors (CFU-GM). Life Sci. 1999;65:513–23. doi: 10.1016/s0024-3205(99)00272-6. [DOI] [PubMed] [Google Scholar]
- 216.Pessina A, Bonomi A, Cocce V, et al. Mesenchymal stromal cells primed with paclitaxel provide a new approach for cancer therapy. PloS One. 2011;6:e28321. doi: 10.1371/journal.pone.0028321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Pessina A, Cocce V, Bonomi A, et al. Human skin-derived fibroblasts acquire in vitro anti-tumor potential after priming with paclitaxel. Anticancer Agents Med Chem. 2012 [PubMed] [Google Scholar]
- 218.European Parlament. Directive 2001/83/EC of the european parliament and of the council of 6 november 2001 on the community code relating to medicinal products for human use. 2001 [Google Scholar]
- 219.Sensebe L. Clinical grade production of mesenchymal stem cells. Biomed Mater Eng. 2008;18:3–10. [PubMed] [Google Scholar]
- 220.Lowdell MW, Birchall M, Thrasher AJ. Use of compassionate-case ATMP in preclinical data for clinical trial applications. Lancet. 2012;379:2341. doi: 10.1016/S0140-6736(12)61018-6. [DOI] [PubMed] [Google Scholar]
- 221.Belardelli F, Rizza P, Moretti F, Carella C, Galli MC, Migliaccio G. Translational research on advanced therapies. Ann Istit Sup San. 2011;47:72–8. doi: 10.4415/ANN_11_01_15. [DOI] [PubMed] [Google Scholar]