Abstract
Objective
Cognitive problems are commonly reported by hematopoietic stem cell transplant (HSCT) survivors, and are associated with poorer physical and mental well-being. It was hypothesized that adverse effects of subjective cognitive impairment occur because cognitive difficulties reduce survivors’ confidence that they can manage HSCT-related symptoms—that is, self-efficacy for symptom management.
Methods
HSCT survivors (n = 245) 9-months to 3-years post-HSCT completed measures of subjective cognitive functioning, self-efficacy for symptom management, and clinically important outcomes: depressed mood, anxiety, and quality of life. Mediation analyses using bootstrapping were conducted to investigate whether effects of subjective cognitive impairment on these outcomes were mediated by self-efficacy for cognitive (SE-Cognitive), emotional (SE-Emotional), social (SE-Social), and physical (SE-Physical) symptom management.
Results
Self-efficacy mediated relations between subjective cognitive impairment and depressed mood (total indirect effect = −.0064 and 95% confidence interval [CI] −.0097 to −.0036), anxiety (total indirect effect = −.0045, CI −.0072 to −.0021), and quality of life (total indirect effect = .0952, CI .0901 to .2642). SE-Emotional was a unique mediator when the outcome was depressed mood and anxiety. SE-Social, SE-Physical and SE-Emotional were specific mediators when outcome was quality of life.
Conclusions
Findings support the conclusion that subjective cognitive impairment reduces HSCT survivors’ confidence in their ability to manage common post-HSCT symptoms, with implications for physical and mental well-being. Interventions that help enhance survivors’ self-efficacy are likely to benefit HSCT survivors who report subjective cognitive impairment.
Keywords: cancer, oncology, cognitive functioning, self-efficacy, quality of life, distress
Hematopoietic stem cell transplant (HSCT; also commonly known as bone marrow transplant) is an aggressive treatment for hematological malignancies that causes numerous physical and psychological difficulties, including significant distress and poor quality of life [1, 2]. Although previously a treatment of last resort, HSCTs are now indicated early in the course of many diseases. This shift in treatment strategy has resulted in improved survival rates [3, 4], but has also led to a greater focus on lingering side effects found among survivors.
Researchers have recently begun to examine the potential neurotoxic effects of HSCT as well as the deleterious neurological impact of the cancers it treats. There are two ways in which such cognitive impairments have been measured: neuropsychological assessment (objective) and self-report measures of cognitive functioning (subjective). HSCT patients have impaired cognitive function using both forms of measurement [5–7]. However, in general, objective neuropsychological test results are not correlated with subjective cognitive functioning [7, 8]. Thus, patients may demonstrate deficits on neuropsychological tests but perceive little impairment in daily functioning, or they may demonstrate relatively normal neuropsychological test results despite perceiving considerable daily impairment. Despite the fact that subjective cognitive functioning is often not correlated with objective neuropsychological impairment, it is associated with poorer psychological adjustment and quality of life. For instance, Booth-Jones and colleagues [7] investigated HSCT patients who were 6-months post-discharge and found that poorer subjective cognitive functioning was associated with greater depressive symptomatology as well as poorer physical and mental quality of life. Similar associations have also been found in women receiving adjuvant therapy for breast cancer for whom self-reports of memory and concentration difficulties were associated with psychological distress and poorer quality of life [9].
Mechanisms through which subjective cognitive impairment affects distress and quality of life are not currently well-defined, but they are worth clarifying because they may be good targets for psychosocial interventions. One possible mechanism is suggested by Bandura’s social cognitive theory and its emphasis on self-efficacy, or “belief in one’s capabilities to organize and execute the courses of action required to manage prospective situations” [10]. HSCT survivors’ self-efficacy for managing symptoms is particularly likely to have implications for their well-being because of their high physical and psychosocial symptom burden after treatment [1]. Indeed, low self-efficacy has been associated with elevated psychological distress and poorer quality of life in other cancer patients [e.g., 11–13]. Thus, experiencing difficulties such as memory problems and poor concentration may cause survivors to doubt their ability to manage symptoms, which in turn may adversely affect their psychological adjustment and quality of life. Evidence from other patient populations supports the plausibility of such a mechanism. For example, in chronic pain patients, self-efficacy has been shown to mediate the relationship between self-reported pain intensity and outcomes such as disability and depression [14]. Self-efficacy for managing cognitive symptoms has also been found to mediate the relationship between community integration and global life satisfaction in patients with traumatic brain injury [15]. If self-efficacy were similarly conceptualized as a mediator among HSCT survivors suffering from subjective cognitive impairment, it might explain the link between subjective cognitive impairment and distress and poor quality of life.
Thus, the purpose of the present study was to examine whether self-efficacy for symptom management mediates relations between subjective cognitive functioning and the following outcomes: psychological adjustment (i.e., depressed mood and anxiety), and health-related quality of life. We hypothesized that among HSCT survivors, poorer subjective cognitive functioning would be associated with lower levels of self-efficacy for symptom management, which would in turn be associated with poorer adjustment and quality of life.
Method
Participants and Procedures
Data for this study come from a randomized controlled trial of a psychosocial intervention for HSCT survivors with at least moderate distress. All study procedures were approved by the institutional review boards at both study sites. Participants were recruited in two ways. The first was through direct recruitment from two medical centers in the Northeastern United States (one urban and one suburban). Potentially eligible participants were identified by clinical database staff and mailed introductory materials describing the study, followed by a recruitment phone call from a trained staff member. The second way participants entered the study was through community recruitment. Specifically, participants were informed about the study through advertisements in newsletters and on the internet, through mailings coordinated with advocacy organizations, and in newspapers. Interested individuals then contacted the study team for more information.
A screening interview was conducted to establish that participants met the following eligibility requirements: history of HSCT 9 months to 3 years prior to assessment; ≥ age 18 (and at least 16 at time of HSCT); English speaking; had telephone service; alive with their disease or free of disease after successful HSCT; and had at least moderate psychological distress or other survivorship difficulties in one or more of the following domains: cancer-specific distress (Impact of Events Scale) [16]; generalized distress (Brief Symptom Inventory – Global Severity Index) [17]; depressed mood (BSI Depression subscale) [17]; anxiety (BSI Anxiety subscale) [17]; health-related quality of life (Functional Assessment of Cancer Therapy–Bone Marrow Transplant full scale or one or more subscales) [18]; and sense of purpose in life (Life Engagement Test) [19].1 Eligible participants completed an initial assessment that included a mailed questionnaire and telephone interview. Data for the present report were obtained during this initial assessment, prior to administration of the psychosocial intervention being tested.
Participant characteristics appear in Table 1. The sample consisted of 245 men (42%) and women (58%) who had undergone HSCT. Their average age was 54.20 years (SD = 12.12 years). Most were White (85.31%) and married (76.73%). Two-thirds had completed a college education. The median annual household income was between $80,000 and $95,000, with a range of less than $20,000 to over $110,000. Diagnosis had occurred on average 4 years, 2 months prior to HSCT (SD = 3 years, 8 months), and the transplant had occurred on average 1 year, 8 months prior to the assessment (SD = 8 months). Type of transplant was evenly split between allogeneic (using stem cells from a donor, including umbilical cord blood; n = 123) and autologous (using stem cells from the patients’ own cells; n = 122) transplants. The majority of HSCTs were performed for malignances such as leukemia, lymphoma, or myeloma (95.51%).When refusers (n = 70) were compared with participants on sociodemographic and medical variables for which data were available, some differences were noted. Chi-square analyses indicated that refusers were more likely to be female (χ2[1, n = 314] = 13.09, p < .001) and non-White (χ2[1, n = 302] = 7.32, p < .001). The refuser group was also more likely to consist of autologous transplant survivors than the participant group (χ2[1, n = 307] = 5.30, p < .05). In addition, t-test analyses indicated that refusers (M = 58.03, SD = 13.28) were significantly older, on average, than participants (M = 54.20, SD = 12.12; t[304] = 2.17, p < .05).
Table 1.
Participant characteristics (n=245)
| Characteristic | n | % |
|---|---|---|
| Gender (female) | 142 | 58.0 |
| Ethnicitya | ||
| White/non-Hispanic | 209 | 85.3 |
| Black/African American | 11 | 4.5 |
| Spanish/Latino/Hispanic | 8 | 3.3 |
| Asian/Pacific Islander | 6 | 2.4 |
| Caribbean/West Indian | 3 | 1.2 |
| Other | 8 | 3.3 |
| Marital statusb | ||
| Married/marriage-like relationship | 188 | 76.7 |
| Single/Never married | 28 | 11.4 |
| Divorced/Separated | 23 | 9.4 |
| Widowed | 6 | 2.4 |
| Educational levelc | ||
| Less than high school | 1 | 0.4 |
| High school | 27 | 11.0 |
| Partial college/trade school | 54 | 22.0 |
| College degree | 85 | 34.7 |
| Graduate degree | 76 | 31.0 |
| Missing | 2 | 0.8 |
| Annual household incomed | ||
| Less than $20,000 | 22 | 9.0 |
| $20,000–$34,999 | 18 | 7.3 |
| $35,000–$49,999 | 24 | 9.8 |
| $50,000–$64,999 | 18 | 7.3 |
| $65,000–$79,999 | 27 | 11.0 |
| $80,000–$94,999 | 26 | 10.6 |
| $95,000–$110,000 | 20 | 8.2 |
| Over $110,000 | 74 | 30.2 |
| Missing | 16 | 6.5 |
| Transplant type | ||
| Allogeneic | 123 | 50.2 |
| Autologous | 122 | 49.8 |
| Transplant due to malignancy | 234 | 95.5 |
Due to variable frequencies, for analyses ethnicity was recoded as 0=White/non-Hispanic, 1=non-White.
Due to variable frequencies, for analyses marital status was recoded as 0=married/marriage-like relationship, 1=single/never married, divorced/separated, or widowed.
Due to variable frequencies, for analyses educational level was recoded as 0=less than college degree, 1=college degree or higher
Due to variable frequencies, for analyses income level was recoded as 0= < $50,000, 1 ≥ $50,000
Measures
Subjective cognitive functioning was measured using a brief version of the Functional Assessment of Cancer Therapy–Cognitive Scale (FACT-Cog) [20], a self-report measure of cognitive functioning in cancer patients. We used 28 items from the 50-item scale, choosing items that had been endorsed most frequently in our earlier research with HSCT survivors or that corresponded with complaints we have observed in this population, including “My thinking has been slow,” “I have had trouble remembering whether I did things I was supposed to do, like taking a medicine or buying something I needed,” and “These problems have interfered with my ability to work.” Participants rate on a five-point Likert scale (0 = never to 4 = several times a day) the frequency with which each cognitive symptom occurred in the past 7 days. Negatively worded items are reverse scored and then all scores are summed so that higher scores reflect fewer cognitive problems and better quality of life. This 28-item scale demonstrated excellent internal consistency in our sample (Cronbach α = .98).
Self-efficacy for symptom management was assessed with a measure originally developed for use with people with chronic medical disability [21] and adapted for use with people suffering from cognitive impairment due to traumatic brain injury (TBI; the TBI Self-Efficacy Questionnaire) [15] . This adapted scale retains the factor structure of the original instrument and has good internal reliability (Cronbach α = .93) [15]. For each of 13 items, respondents rate how confident they are that they can manage tasks, including, “How confident are you that you can get help with your daily tasks (like house cleaning, yard work, shopping) from resources other than family or friends, if needed?” and “How confident are you that you can compensate for any cognitive difficulties caused by your illness so that they don’t interfere with the things that you want to do?” Responses are made on a ten-point scale (1=not at all confident to 10=totally confident), and are typically summed to create a total score (total self-efficacy). Cicerone and Azulay [15] recommended that the assessment of self-efficacy be linked to specific domains of functioning to increase sensitivity and predictive utility. Bandura [22] also noted that domain-specific measures predicted changes in functioning better than general measures. Therefore, we used the subscales created by Cicerone and Azulay [15]: 4 items assessed perceived ability to obtain assistance (Self-Efficacy - Social), 4 items assessed self-management of cognitive symptoms (Self-Efficacy - Cognitive), 4 items assessed self-management of emotional symptoms (Self-Efficacy - Emotional), and a single item assessed self-management of physical symptoms (Self-Efficacy - Physical). In the current study, the total scale demonstrated excellent internal consistency (Cronbach α = .91), as did the Self-Efficacy – Emotional subscale (Cronbach α = .90) and the Self-Efficacy – Cognitive subscale (Cronbach α = .95). Internal consistency was acceptable for the Self-Efficacy – Social subscale (Cronbach α = .78).
Depressed mood and anxiety were measured using subscales of the Brief Symptom Inventory (BSI) [17]. The BSI is a 53-item measure of psychological distress and symptoms that is appropriate for use with medical patients. It is a brief version of the 90-item Symptom Checklist-90-Revised [17]. The depression and anxiety subscales assess symptomatology (e.g. “feeling no interest in things” and “suddenly scared for no reason”) over the past month on a scale ranging from 1= not at all to 4=extremely. Internal consistency in the current study was good (Cronbach α = .84 for both subscales).
Quality of life was assessed with the Functional Assessment of Cancer Therapy – Bone Marrow Transplant version 4 scale (FACT-BMT) [18, 23] . This scale is a commonly used and well-validated measure of the functional status of cancer patients who have undergone HSCT. It measures four primary quality of life domains using the 27 items of the FACT-G: physical well-being (e.g. “I am bothered by side effects of treatment”), social/family well-being (e.g. “I get emotional support from my family”), emotional well-being (e.g. “I worry that my condition will get worse”) and functional well-being (e.g. “I am able to work [include work at home”. It also measures specific HSCT-related concerns using the FACT-BMT which consists of 10 items (e.g. “The effects of treatment are worse than I had imagined”) [24]. A total quality of life score was used in the present study by summing all subscale and FACT-BMT scores. In the present study, internal reliability was good (Cronbach α = .89).
Medical information was gathered from medical chart review and self-report, and included the number of days since transplant, the number of days since diagnosis, and type of transplant (allogeneic or autologous).
Sociodemographic information was self-reported and included age, gender, race (White or other), marital status (married or other), and years of education.
Statistical Analyses
Bivariate correlations (or point biserial correlations for dichotomous variables) were used to determine the sociodemographic and medical covariates that were significantly related to each outcome variable (i.e., depressed mood, anxiety, and quality of life). All mediation analyses were conducted while adjusting for sociodemographic and medical variables that were significantly correlated with the outcome being predicted. We predicted that self-efficacy for symptom management would mediate relations between subjective cognitive functioning and the three outcome variables. To test mediation effects, we conducted mediation analyses using bootstrapping. Bootstrapping is a statistical method that involves repeatedly sampling from the data set, which allows repeated estimates of the indirect effect (i.e., the effect of subjective cognitive functioning on the outcome variable through the mediators). Using this method, we were able to generate 5,000 bootstrapped samples. Point estimates and 95% bias corrected and accelerated confidence intervals for indirect and total effects were generated. A point estimate is a single value used to estimate a population parameter. Advantages to using this statistical approach to testing mediation effects compared to Baron and Kenny’s approach include: i) bootstrapping of the sampling distribution does not rely on the assumption of normal sampling distributions of the indirect effects; ii) type II error is reduced because it requires fewer inferential tests; and iii) multiple mediators can be tested at the same time [25]. Whereas inferential testing bases significant findings typically on p values of less than .05, bootstrapping bases significant findings upon confidence intervals that do not contain zero.
Results
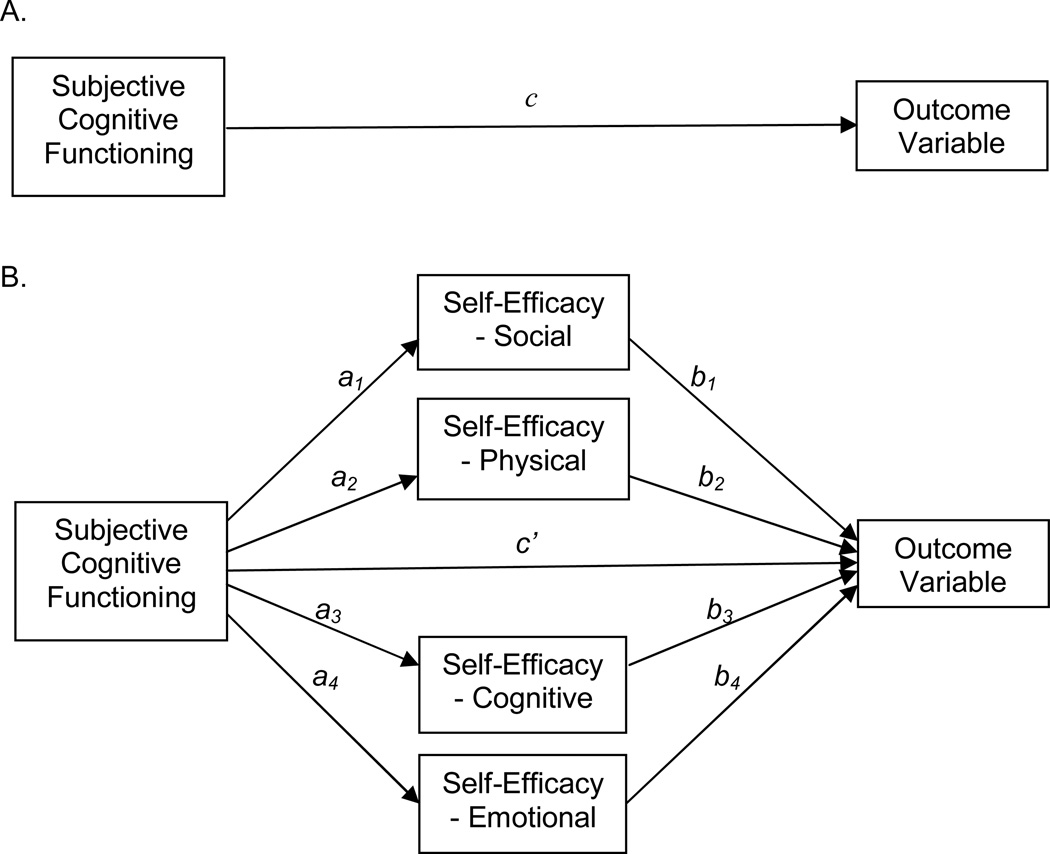
Bivariate correlations and descriptive data for study variables are shown in Table 2. Figure 1 illustrates the multiple mediation design tested in the present study and is based on analogous figures presented by Preacher and Hayes [26]. Note that paths a1–4 represent the effects of subjective cognitive functioning on the proposed self-efficacy mediators, and paths b1–4 represent the effects of the mediators on the outcome variable. The total effect of subjective cognitive functioning on outcome is represented by path c, and path c’ is the direct effect of subjective cognitive functioning on outcome controlling for the self-efficacy mediators. The indirect effects are exerted on an outcome through the proposed mediators. The direct paths from subjective cognitive functioning to the mediators and from the mediators to the outcome variables are presented in Table 3and the results of the bootstrapped tests of simultaneous multiple indirect effects are presented in Table 4.
Table 2.
Correlations among study variables (n=245)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depressed mood | — | .68*** | −.76*** | −.38*** | −.49*** | −.74*** | −.49*** | −.45*** | −.13* | −.07 |
| 2. Anxiety | — | −.64*** | −.18** | −.47*** | −.61*** | −.42*** | −.56*** | −.15* | −.08 | |
| 3. Quality of life | — | .46*** | .54*** | .71*** | .66*** | .55*** | .06 | .03 | ||
| 4. Self-efficacy – Social | — | .34*** | .48*** | .43*** | .14* | .09 | .08 | |||
| 5. Self-efficacy – Cognitive | — | .61*** | .53*** | .62*** | .18** | .13* | ||||
| 6. Self-efficacy – Emotional | — | .58*** | .48*** | .25*** | .12 | |||||
| 7. Self-efficacy – Physical | — | .34*** | .07 | .00 | ||||||
| 8. Subjective cognitive functioning | — | .14* | .03 | |||||||
| 9. Age | — | .04 | ||||||||
| 10. Ethnicity (non–White) | — | |||||||||
| 11. Gender (female) | ||||||||||
| 12. Education, years | ||||||||||
| 13. Income (high) | ||||||||||
| 14. Marital status (married) | ||||||||||
| 15. Transplant type (allogeneic) | ||||||||||
| 16. Days since diagnosis | ||||||||||
| 17. Days since transplant | ||||||||||
| M | .50 | .60 | 111.83 | 30.11 | 30.64 | 30.07 | 7.00 | 79.13 | 54.20 | .85 |
| SD | .58 | .61 | 19.30 | 8.10 | 8.25 | 7.94 | 2.44 | 25.27 | 12.12 | .35 |
| Range | .01–3.17 | .01–3.17 | 59–146 | 4–40 | 4–40 | 5–40 | 1–10 | 6–112 | 20–78 | — |
| 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|
| 1. Depressed mood | −.04 | .02 | −.16* | −.19** | .09 | −.09 | −.14* |
| 2. Anxiety | .08 | −.08 | −.12 | −.05 | .16* | −.06 | −.21** |
| 3. Quality of life | −.08 | −.05 | .15* | .10 | −.14* | .08 | .13* |
| 4. Self-efficacy – Social | −.02 | .05 | .18** | .12 | .01 | −.02 | .02 |
| 5. Self-efficacy – Cognitive | −.04 | .05 | .07 | .03 | −.08 | −.04 | .15* |
| 6. Self--efficacy – Emotional | −.00 | −.08 | .14* | .10 | −.10 | .07 | .15* |
| 7. Self-efficacy – Physical | −.05 | −.01 | .10 | .06 | −.12 | .01 | .11 |
| 8. Subjective Cognitive Functioning | −.14* | .02 | .14* | .02 | −.09 | −.01 | .04 |
| 9. Age | −.10 | −.01 | .11 | .14* | −.14* | .01 | .07 |
| 10. Ethnicity (non-White) | −.05 | .01 | .11 | .07 | .05 | .09 | .10 |
| 11. Gender (female) | — | −.13* | −.19** | −.20** | .05 | .03 | .03 |
| 12. Education, years | — | .25*** | .07 | .14* | −.03 | −.06 | |
| 13. Income (high) | — | .46*** | .02 | .04 | −.01 | ||
| 14. Marital status (married) | — | .00 | .04 | −.03 | |||
| 15. Transplant type (allogeneic) | — | .07 | −.05 | ||||
| 16. Days since diagnosis | — | .23*** | |||||
| 17. Days since transplant | — | ||||||
| M | .58 | 16.02 | .72 | .76 | .50 | 1523.63 | 611.36 |
| SD | .49 | 2.40 | .45 | .43 | .50 | 1342.44 | 236.27 |
| Range | — | 11–24 | — | — | — | 245–8140 | 230–1153 |
=p≤.05;
=p≤.01;
=p≤.001
Figure 1.
Mediation design with self-efficacy domains as mediators. (A) Subjective cognitive functioning affects the outcome variable. (B) Subjective cognitive functioning is hypothesized to exert indirect effects on the outcome variable through the four self-efficacy mediators.
Table 3.
Direct paths from subjective cognitive functioning to mediators and from mediators to outcome variables
| Mediators | Direct paths from subjective cognitive functioning to mediators |
Direct paths from mediators to outcome variables |
||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | t | p | B | SE | t | p | |
| Outcome variable is depressed mood | ||||||||
| Social SE | 0.0421 | 0.0214 | 1.9671 | 0.0504 | −0.0018 | 0.0038 | −0.4856 | 0.6277 |
| Physical SE | 0.0349 | 0.0061 | 5.6882 | <0.0001 | −0.0153 | 0.0142 | −1.0811 | 0.2809 |
| Cognitive SE | 0.2065 | 0.0167 | 12.3287 | <0.0001 | 0.0039 | 0.0048 | 0.8284 | 0.4083 |
| Emotional SE | 0.1387 | 0.0183 | 7.5726 | <0.0001 | −0.0476 | 0.0048 | −9.9255 | <0.0001 |
| Outcome variable is anxiety | ||||||||
| Social SE | 0.0440 | 0.0206 | 2.1393 | 0.0334 | 0.0084 | 0.0041 | 2.0475 | 0.0417 |
| Physical SE | 0.0313 | 0.0058 | 5.3534 | <0.0001 | −0.0257 | 0.0150 | −1.7144 | 0.0878 |
| Cognitive SE | 0.1995 | 0.0164 | 12.1746 | <0.0001 | 0.0056 | 0.0051 | 1.0936 | 0.2753 |
| Emotional SE | 0.1465 | 0.0177 | 8.2982 | <0.0001 | −0.0351 | 0.0052 | −6.8128 | <0.0001 |
| Outcome variable is quality of life | ||||||||
| Social SE | 0.0443 | 0.0214 | 2.0708 | 0.0395 | 0.3170 | 0.1137 | 2.7883 | 0.0058 |
| Physical SE | 0.0342 | 0.0061 | 5.6255 | <0.0001 | 2.7808 | 0.4233 | 6.5693 | <0.0001 |
| Cognitive SE | 0.2098 | 0.0168 | 12.4910 | <0.0001 | −0.2553 | 0.1430 | −1.7858 | 0.0755 |
| Emotional SE | 0.1437 | 0.0187 | 7.7009 | <0.0001 | 0.8335 | 0.1407 | 5.9246 | <0.0001 |
Note
SE = self-efficacy
Table 4.
Mediation of the indirect effects of subjective cognitive functioning on outcome variables through the self-efficacy domains
| BCa 95% CI |
|||
|---|---|---|---|
| Mediator | Point estimate |
Lower | Upper |
| Outcome variable is depressed mood | |||
| Self-efficacy total indirect effect | −0.0064* | −0.0097 | −0.0036 |
| Social self-efficacy | −0.0001 | −0.0006 | 0.0003 |
| Physical self-efficacy | −0.0005 | −0.0020 | 0.0005 |
| Cognitive self-efficacy | 0.0008 | −0.0019 | 0.0032 |
| Emotional self-efficacy | −0.0066* | −0.0093 | −0.0039 |
| Outcome variable is anxiety | |||
| Self-efficacy total indirect effect | −0.0045* | −0.0072 | −0.0021 |
| Social self-efficacy | 0.0004 | 0.0000 | 0.0012 |
| Physical self-efficacy | −0.0008 | −0.0022 | 0.0002 |
| Cognitive self-efficacy | 0.0011 | −0.0009 | 0.0034 |
| Emotional self-efficacy | −0.0051* | −0.0079 | −0.0029 |
| Outcome variable is quality of life | |||
| Self-efficacy total indirect effect | 0.1755* | 0.0901 | 0.2642 |
| Social self-efficacy | 0.0140* | 0.0003 | 0.0398 |
| Physical self-efficacy | 0.0952* | 0.0527 | 0.1516 |
| Cognitive self-efficacy | −0.0536 | −0.1220 | 0.0128 |
| Emotional self-efficacy | 0.1198* | 0.0602 | 0.1815 |
Note. BCa = bias corrected and accelerated confidence intervals.
Confidence intervals that do not contain zero are deemed to be significant.
Mediation Analyses Predicting Depressed Mood
After controlling for age, marital status, income level, and days since transplant, results indicated that, taken as a set, social, physical, cognitive and emotional self-efficacy mediated the effect of subjective cognitive functioning on depressed mood. The total and direct effects of subjective cognitive functioning on depressed mood were −.0102, p < .0001, and −.0038, p < .01 respectively. The difference between the total and direct effects was the total indirect effect through the four mediators, with a point estimate of −.0064 and a 95% bias corrected and accelerated bootstrap confidence interval (BCa CI) of −.0097 to −.0036. When the total indirect effect was examined, the directions of the a and b paths were consistent with the interpretation that reporting better subjective cognitive functioning was associated with greater self-efficacy for symptom management (for each of the four self-efficacy domains), which in turn was associated with less depressed mood. When specific indirect effects were examined, only Self-Efficacy – Emotional remained significant after controlling for all other potential mediators (i.e., its 95% BCa CI did not include zero). As shown in Table 4, its point estimate was −.0066 and BCa CI was −.0093 to −.0039. Additionally, participants who were married reported less depressed mood than those who were unmarried, single, widowed or divorced (p < .05).
Mediation Analyses Predicting Anxiety
After controlling for days since transplant and type of transplant (allogeneic vs. autologous), results indicated that, taken as a set, social, physical, cognitive, and emotional self-efficacy mediated the effect of subjective cognitive functioning on anxiety. The total and direct effects of subjective cognitive functioning on anxiety were −.0132, p <.0001, and −.0088, p < .0001 respectively. The total indirect effect through the four mediators had a point estimate of −.0045 and a 95% BCa CI of −.0072 to −.0021. When the total indirect effect was examined, the directions of the a and b paths indicated that better subjective cognitive functioning was associated with greater self-efficacy for symptom management (for the four domains), which in turn was associated with reduced anxiety. When specific indirect effects were examined, again, only Self-Efficacy – Emotional was a unique mediator after controlling for the other potential mediators (i.e., point estimate was −.0051, and BCa CI was −.0079 to −.0029; see Table 4). Upon examination of the covariates, the number of days since transplant was found to be negatively associated with anxiety (p < .01).
Mediation Analyses Predicting Health-Related Quality of Life
After controlling for age, days since transplant, and type of transplant, results indicated that, taken as a set, social, physical, cognitive, and emotional self-efficacy mediated the effect of subjective cognitive functioning on quality of life. The total and direct effects of subjective cognitive functioning on quality of life were .3981, p <.0001, and .2226, p < .0001 respectively. The total indirect effect through the four mediators had a point estimate of .1755 and a 95% BCa CI of .0901 to .2642. When the total indirect effect was examined, the a and b paths indicated that better subjective cognitive functioning was associated with greater self-efficacy for symptom management (for the four domains), which in turn was associated with better quality of life. When specific indirect effects were examined, Self-Efficacy – Social (point estimate of .0140, BCa CI of .0003 to .0398), Self-Efficacy – Physical (point estimate of .0952, BCa CI of .0527 to .1516), and Self-Efficacy – Emotional (point estimate of .1198, BCa CI of .0602 to .1815) were unique mediators of the relation between subjective cognitive functioning and quality of life (see Table 4).
Discussion
There is convincing evidence that subjective cognitive impairment is associated with adjustment and quality of life difficulties in HSCT survivors [5, 7]. Our results replicate these findings, and also suggest that these poor outcomes occur in part because of the adverse effects of subjective cognitive impairment on self-efficacy. That is, experiencing subjective cognitive impairment appears to reduce HSCT survivors’ confidence in their ability to manage their symptoms effectively. We found that self-efficacy for emotional symptom management was a unique mediator when depressed mood and anxiety were the outcomes, and that self-efficacy for obtaining assistance, and for physical and emotional symptom management were mediators when quality of life was the outcome. Surprisingly, self-efficacy for management of cognitive symptoms was not a significant mediator of associations between subjective cognitive functioning and any of the outcome variables, even though it seemed a likely candidate to be related to subjective cognitive functioning. These findings illustrate the multi-faceted nature of the relationship between subjective cognitive functioning and survivors’ well-being. They also highlight the importance of targeting specific domains of self-efficacy, particularly self-efficacy for emotional symptom management, in treatment efforts. Additional findings from the present study indicated that those who were married were less depressed than those who were not. This is consistent with a large body of research indicating that married individuals tend to have higher levels of subjective well-being and less depression than unmarried persons [27–29], including married individuals with medical illnesses [30]. This association may be due to the higher level of social support potentially available to married HSCT survivors [31]. Not surprisingly, longer time since transplant was associated with less anxiety, consistent with research indicating that psychological functioning tends to improve during the years following transplantation [1].
Although it has been noted that subjective cognitive functioning is often not correlated with objective measures of cognitive functioning in HSCT survivors [7, 32], our findings confirm that survivors’ subjective cognitive functioning was associated with their mental and physical well-being. It may be that more intensive and comprehensive objective testing would detect subtle cognitive problems that contribute to survivors’ subjective experiences or that objective assessments of cognitive functioning are not fully capturing the impairments that patients experience in their daily lives. Clearly additional research in this area is warranted. Moreover, the mechanism we have described through which subjective cognitive impairment reduces adjustment and quality of life has the potential to inform both clinical care and interventions for these individuals. Our findings suggest that focusing on enhancing survivors’ self-efficacy, particularly for the management of emotional symptoms, may reduce the negative impact of subjective cognitive impairment upon adjustment and quality of life.
A potential intervention for bolstering self-efficacy for emotional symptom management in HSCT survivors is the expressive-writing protocol that requires individuals to write about an emotional topic for 20–30 minutes per day for 3–5 days spread over a relatively brief period of time [33]. Findings show that such interventions can lead to improved outcomes for people writing about a variety of life stressors including surviving cancer [34] and has been shown to improve self-efficacy for managing emotional symptoms in a non-cancer population [35]. Note that upon completion of the randomized controlled trial that is the parent study for the current sub-study, we will be able to evaluate the efficacy of expressive-writing interventions in HSCT survivors and will also be able to determine the potential efficacy of the interventions in HSCT survivors with subjective cognitive impairment.
Cognitive-behavioral therapy may also be helpful in improving emotional self-efficacy in HSCT survivors as it can include techniques that focus on improving emotional self-regulation (of which self-efficacy is a key motivational component). Such techniques include relaxation training, self-monitoring and alteration of maladaptive beliefs. Indeed, cognitive-behavioral therapy has already been shown to improve the management of distress in HSCT survivors [36].
Cognitive rehabilitation approaches that include components that promote self-efficacy in multiple domains may also be effective in helping HSCT survivors with subjective cognitive impairment. For example, Ferguson and colleagues [37] investigated the potential benefits of a brief treatment for breast cancer survivors reporting memory and attention problems after chemotherapy. The intervention, called ‘Memory and Attention Adaptation Training’ (MAAT), involved the use of a participant workbook, monthly visits, and phone contacts. The content of MAAT included education on memory and attention; self-awareness training; self-regulation through the use of relaxation training, activity scheduling and pacing; and cognitive compensatory strategies training. Self-reported cognitive functioning, neuropsychological test performance (verbal memory and executive functioning domains), and health-related quality of life all improved after treatment and were maintained for 6 months. It seems likely that an intervention such as MAAT which involves careful monitoring of behavioral change through homework and feedback from the trained professional would help to boost self-efficacy (e.g., by helping patients experience, recognize, and benefit from mastery experiences, as well as helping them to recognize that errors will occur as part of the learning process). It could also increase adherence to daily life activities that had previously been challenging by providing patients with objective information about their functioning.
Due to the similarity between self-efficacy for one’s perceived ability to obtain assistance and the concept of perceived social support, potential treatment approaches may also be derived from the extensive perceived social support literature in other populations dealing with medical illness. For example, Barrera and colleagues [38] tested an online social support intervention in 160 individuals with Type 2 diabetes that involved providing participants with access to internet forums that facilitated social interactions with other participants. Participants were encouraged to discuss concerns, successes, frustrations and coping strategies with each other. Individuals in the support conditions reported significant increases in their perceived social support as measured by the Diabetes Support Scale and a general support scale. Hence, drawing from the perceived social support literature may be important in designing an intervention that provides opportunities for survivors to feel efficacious in accessing support that they need.
Finally, holistic approaches to cognitive rehabilitation that have been found to be efficacious for those with brain injury [39, 40], may also be helpful for HSCT survivors reporting cognitive impairment. Such approaches typically provide individual- and group-based therapies in an integrated, therapeutic environment and are focused on remediating cognitive impairments, functional skills, and interpersonal functions [41] among those with moderate to severe traumatic brain injury [40]. Although HSCT survivors’ cognitive issues are generally less severe than those in brain injury patients who are typically treated in holistic programs, components of the holistic approach are likely to be useful for HSCT survivors due to its emphasis on improving self-efficacy [39, 42].
Limitations
Although we found that self-efficacy for symptom management partially mediated relations between subjective cognitive impairment and depressed mood, anxiety, and quality of life, there were still significant direct relations between subjective cognitive impairment and these outcomes, suggesting that the mechanism by which those relations occur is more complex than has been examined here. Additional possible mediators include (a lack of) perceived social support (e.g., due to a belief that cognitive issues are being disregarded by others or if cognitive difficulties strain potentially supportive relationships) and reduced self-esteem associated with perceived decline in functioning.
There are also limitations due to the cross-sectional nature of the data. Although we hypothesized that subjective cognitive impairment leads to reduced self-efficacy, which in turn leads to poorer outcomes, future longitudinal work is required in order to determine true temporal causality. However, the current data still provides an important foundation to support future work in this area. Additional limitations arise from the significant sociodemographic and medical treatment differences between those who refused or were excluded from the study (e.g., due to relapse) and those who chose to participate and were included in this study. The current sample was also mostly well-educated, white, and high income individuals. This is, unfortunately, consistent with the lack of diversity found in other studies investigating HSCT survivors and highlights the need to specifically capture a more diverse population when undertaking survivorship studies in the future. Indeed, there is evidence from research with other cancer populations that having lower socioeconomic status may be associated with greater distress and worse quality of life [43]. In addition, researchers have noted racial/ethnic differences in other cancer populations with respect to health-related quality of life. For example, Penedo and colleagues [44] found that African American and Hispanic men living with prostate cancer reported lower quality of life than non-Hispanic white men living with prostate cancer. A study of breast cancer survivors also found that African American women reported worse physical functioning and general health compared with white survivors [45]. Hence, caution should be exercised when generalizing these findings to other samples of HSCT survivors until findings are replicated in a more diverse sample.
Conclusion
These results suggest that self-efficacy may be an important therapeutic target for clinical interventions when patients report cognitive difficulties following HSCT. Interventions that focus on bolstering specific domains of self-efficacy, particularly self-efficacy for the management of emotional symptoms, may be useful in reducing the negative impact of subjective cognitive impairment upon adjustment and quality of life.
Acknowledgements
We wish to thank Katie Basmajian, M.A., AnnaMarie Vu, B.A., and Jennifer Chee-Chait, B.A. for their assistance in data collection for this project. This research was supported by funding from the American Cancer Society (PI: Rini; grant #RSGPB-07-285-01-CPPB) and the National Cancer Institute (grant #2R25CA081137-11A1).
Footnotes
The authors have no financial interests to disclose.
Exact cut-offs are available from the authors.
References
- 1.Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: A review of the literature. Psycho-Oncol. 2009;18:113–127. doi: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers ME, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- 3.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–1826. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- 4.Karanes C, Nelson GO, Chitphakdithai P, Agura E, Ballen KK, Bolan CD, et al. Twenty years of unrelated donor hematopoietic cell transplantation for adult recipients facilitated by the national marrow donor program. Biol Blood Marrow Transplant. 2008;14(9 Suppl):8–15. doi: 10.1016/j.bbmt.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Harder H, Cornelissen JJ, Van Gool AR, Duivenvoorden HJ, Eijkenboom WM, van den Bent MJ. Cognitive functioning and quality of life in long-term adult survivors of bone marrow transplantation. Cancer. 2002;95:183–192. doi: 10.1002/cncr.10627. [DOI] [PubMed] [Google Scholar]
- 6.Syrjala KL, Dikmen S, Langer SL, Roth-Roemer S, Abrams JR. Neuropsychologic changes from before transplantation to 1 year in patients receiving myeloablative allogeneic hematopoietic cell transplant. Blood. 2004;104:3386–3392. doi: 10.1182/blood-2004-03-1155. [DOI] [PubMed] [Google Scholar]
- 7.Booth-Jones M, Jacobsen PB, Ransom S, Soety E. Characteristics and correlates of cognitive functioning following bone marrow transplantation. Bone Marrow Transplant. 2005;36:695–702. doi: 10.1038/sj.bmt.1705108. [DOI] [PubMed] [Google Scholar]
- 8.Poppelreuter M, Weis J, Mumm A, Orth HB, Bartsch HH. Rehabilitation of therapy-related cognitive deficits in patients after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41:79–90. doi: 10.1038/sj.bmt.1705884. [DOI] [PubMed] [Google Scholar]
- 9.Shilling V, Jenkins V. Self-reported cognitive problems in women receiving adjuvant therapy for breast cancer. Eur J Oncol Nurs. 2007;11:6–15. doi: 10.1016/j.ejon.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Self-efficacy in changing societies. Cambridge: Cambridge University Press; 1995. [Google Scholar]
- 11.Beckham JC, Burker EJ, Lytle BL, Feldman ME, Costakis MJ. Self-efficacy and adjustment in cancer patients: A preliminary report. Behav Med. 1997;23:138–142. doi: 10.1080/08964289709596370. [DOI] [PubMed] [Google Scholar]
- 12.Kreitler S, Peleg D, Ehrenfeld M. Stress, self-efficacy and quality of life in cancer patients. Psycho-Oncol. 2007;16:329–341. doi: 10.1002/pon.1063. [DOI] [PubMed] [Google Scholar]
- 13.Lev EL, Paul D, Owen SV. Age, self-efficacy, and change in patients' adjustment to cancer. Cancer Practice. 1999;7:170–176. doi: 10.1046/j.1523-5394.1999.74004.x. [DOI] [PubMed] [Google Scholar]
- 14.Arnstein P, Caudill M, Mandle CL, Norris A, Beasley R. Self efficacy as a mediator of the relationship between pain intensity, disability and depression in chronic pain patients. Pain. 1999;80:483–491. doi: 10.1016/S0304-3959(98)00220-6. [DOI] [PubMed] [Google Scholar]
- 15.Cicerone KD, Azulay J. Perceived self-efficacy and life satisfaction after traumatic brain injury. J Head Trauma Rehabil. 2007;22:257–266. doi: 10.1097/01.HTR.0000290970.56130.81. [DOI] [PubMed] [Google Scholar]
- 16.Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Derogatis LR. BSI brief symptom inventory: Administration, scoring, and procedures manual. 4th ed. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 18.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 19.Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, et al. The life engagement test: Assessing purpose in life. J Behav Med. 2006;29:291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs SR, Jacobsen PB, Booth-Jones M, Wagner LI, Anasetti C. Evaluation of the functional assessment of cancer therapy cognitive scale with hematopoietic stem cell transplant patients. J Pain Symptom Manage. 2007;33:13–23. doi: 10.1016/j.jpainsymman.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome measures for health education and other health care interventions. Thousand Oaks, CA: SAGE Publications; 1996. [Google Scholar]
- 22.Bandura A. Regulation of cognitive processes through perceived self-efficacy. Developmental Psychology. 1989;25:729–735. [Google Scholar]
- 23.McQuellon RP, Russell GB, Cella DF, Craven BL, Brady M, Bonomi A, et al. Quality of life measurement in bone marrow transplantation: Development of the functional assessment of cancer therapy-bone marrow transplant (FACT-BMT) scale. Bone Marrow Transplant. 1997;19:357–368. doi: 10.1038/sj.bmt.1700672. [DOI] [PubMed] [Google Scholar]
- 24.Cella D. Manual of the functional assessment of chronic illness therapy (FACIT) scales. Evanston Northwestern Healthcare and Northwestern University: Center on outcomes, research and education (CORE) 1997 [Google Scholar]
- 25.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 26.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 27.Diener E. Subjective well-being. Psychol Bull. 1984;95:542–575. [PubMed] [Google Scholar]
- 28.Kessler RC, Essex M. Marital status and depression: The importance of coping resources. Social Forces. 1982;61:484–507. [Google Scholar]
- 29.Ross CE, Mirowsky J. Explaining the social patterns of depression: Control and problem solving--or support and talking? J Health Soc Behav. 1989;30:206–219. [PubMed] [Google Scholar]
- 30.Chandra V, Szklo M, Goldberg R, Tonascia J. The impact of marital status on survival after an acute myocardial infarction: A population-based study. Am J Epidemiol. 1983;117:320–325. doi: 10.1093/oxfordjournals.aje.a113544. [DOI] [PubMed] [Google Scholar]
- 31.Sherbourne CD, Hays RD. Marital status, social support, and health transitions in chronic disease patients. J Health Soc Behav. 1990;31:328–343. [PubMed] [Google Scholar]
- 32.Poppelreuter M, Weis J, Kulz AK, Tucha O, Lange KW, Bartsch HH. Cognitive dysfunction and subjective complaints of cancer patients. a cross-sectional study in a cancer rehabilitation centre. Eur J Cancer. 2004;40:43–49. doi: 10.1016/j.ejca.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Pennebaker JW, Mayne TJ, Francis ME. Linguistic predictors of adaptive bereavement. J Pers Soc Psychol. 1997;72:863–871. doi: 10.1037//0022-3514.72.4.863. [DOI] [PubMed] [Google Scholar]
- 34.Lepore SJ, Smyth JM, editors. The writing cure: How expressive writing promotes health and emotional well-being. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- 35.Kirk BA, Schutte NS, Hine DW. The effect of an expressive-writing intervention for employees on emotional self-efficacy, emotional intelligence, affect, and workplace incivility. J Appl Soc Psychol. 2011;41:179–195. [Google Scholar]
- 36.DuHamel KN, Mosher CE, Winkel G, Labay LE, Rini C, Meschian YM, et al. Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J Clin Oncol. 2010;28:3754–3761. doi: 10.1200/JCO.2009.26.8722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferguson RJ, Ahles TA, Saykin AJ, McDonald BC, Furstenberg CT, Cole BF, et al. Cognitive-behavioral management of chemotherapy-related cognitive change. Psycho-Oncol. 2007;16:772–777. doi: 10.1002/pon.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barrera M, Jr, Glasgow RE, McKay HG, Boles SM, Feil EG. Do internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. Am J Community Psychol. 2002;30:637–654. doi: 10.1023/A:1016369114780. [DOI] [PubMed] [Google Scholar]
- 39.Cicerone KD, Mott T, Azulay J, Friel JC. Community integration and satisfaction with functioning after intensive cognitive rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2004;85:943–950. doi: 10.1016/j.apmr.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 40.Cicerone KD, Mott T, Azulay J, Sharlow-Galella MA, Ellmo WJ, Paradise S, et al. A randomized controlled trial of holistic neuropsychologic rehabilitation after traumatic brain injury. Arch Phys Med Rehabil. 2008;89:2239–2249. doi: 10.1016/j.apmr.2008.06.017. [DOI] [PubMed] [Google Scholar]
- 41.Ben-Yishay Y, Gold J. Therapeutic milieu approach to neuropsychological rehabilitation. In: Woods RL, editor. Neurobehavioral Sequelae of Traumatic Brain Injury. New York: Taylor & Francis; 1990. pp. 194–218. [Google Scholar]
- 42.Ben-Yishay Y, Diller L. Cognitive remediation in traumatic brain injury: Update and issues. Arch Phys Med Rehabil. 1993;74:204–213. [PubMed] [Google Scholar]
- 43.Simon AE, Wardle J. Socioeconomic disparities in psychosocial wellbeing in cancer patients. Eur J Cancer. 2008;44:572–578. doi: 10.1016/j.ejca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 44.Penedo FJ, Dahn JR, Shen BJ, Schneiderman N, Antoni MH. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67:1022–1027. doi: 10.1016/j.urology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 45.Paskett ED, Alfano CM, Davidson MA, Andersen BL, Naughton MJ, Sherman A, et al. Breast cancer survivors' health-related quality of life : Racial differences and comparisons with noncancer controls. Cancer. 2008;113:3222–3230. doi: 10.1002/cncr.23891. [DOI] [PMC free article] [PubMed] [Google Scholar]