Abstract
BACKGROUND
Facial appearance transfer (FAT) from donor to recipient in face transplantation is a concern. Previous studies of FAT and Facial Appearance Persistence (FAP, preservation of Recipient’s facial likeness) in face transplants simulated using two-dimensional photograph manipulations found low FAT (2.6%) and high FAP (66%). Three-dimensional computer simulation of complex facial transplant patterns may improve the accuracy of FAT and FAP estimations.
METHODS
Three-dimensional virtual models of human faces were generated from de-identified CT angiographs and used as “Donors” or “Recipients” for virtual face transplantation (VFT). Surgical planning software was used to perform 73 VFTs by creating specific facial defects (Mandibular, Midface or Large) in the Recipient models and restoring them with allografts extracted from the Donor models. Twenty independent reviewers evaluated the resemblance of each resulting Post-transplant model to the Donor (FAT) and Recipient (FAP). The results were analyzed using tests for equal results with one-sample and pairwise Rao-Scott Pearson chi-square testing, correcting for clustering and multiple testing.
RESULTS
Overall rates of FAP and FAT were high (69.2%) and low (32.4%), respectively. The Mandibular pattern had the highest rates of FAP and lowest rates of FAT. FAP and FAT were similar across genders.
CONCLUSIONS
FAP is high whereas FAT is low after VFT. Appearance transfer and persistence after VFT are more dependant on the anatomy than on the size of transplanted facial aesthetic units. This information may reassure recipients of partial face transplants as well as donor families.
LEVEL OF EVIDENCE
not ratable
INTRODUCTION
Facial transplantation (FT) enables superior aesthetic and functional restoration of complex facial defects compared with conventional reconstruction.1 There have been 25 clinical cases worldwide.2,3*
Potential recipients and families of donors of FT have expressed concern about the transfer of donor’s facial appearance to the recipient. For recipients, a new facial appearance may introduce additional psychological stress,4,5 and for relatives of donors, potential recognition of their loved one’s face on another individual may discourage donation. Understanding the extent of facial appearance transfer following FT will allow enhancement of the informed consent processes for patients and donor families alike.
Facial regions with similar composition, thickness and texture are naturally demarcated by folds or creases into different aesthetic units.6 Conventional reconstruction of facial deformity spanning across more than one aesthetic unit has unsatisfactory outcomes.7 The degree to which facial units alone or in combination contribute to overall facial appearance is unclear. Humans assess appearance and identity through central processing of the face, perceiving it as a whole unit rather than as a combination of individual features.8–10 Humans can accurately identify features in context of the whole face, but not when presented in isolation or in a changed configuration.9,10 Thus, in partial FT, donor features should not transfer the donor’s appearance to the recipient.11
Given the small number of FT cases and the relatively short follow-up, there is insufficient information to address the issue of appearance transfer from donor to recipient, and furthermore, these types of studies cannot be conducted in real FTs because the donors’ identities are confidential. Fortunately, computer simulations, or virtual FTs (VFTs), can help address these challenges.12
Facial appearance transfer (FAT) and persistence (FAP) are, respectively, the transfer of facial likeness from Donor to Recipient and the preservation of Recipient’s facial likeness after facial transplantation. Previously, multiple FTs were performed between 4 cadaveric heads and the post-transplant faces more closely resembled the Recipients than the Donors.13 Also previously, FAT and FAP were low (2.6%) and high (66%),11 respectively, and the aesthetic match was optimal for Donors aged between 2 decades below and 1 decade above the Recipients in a two-dimensional computer simulation model of central facial transplants.14
A three-dimensional (3D) computer simulation model of FT was developed to include both skeletal and soft-tissue anatomy and provide a more accurate testing medium for FAT and FAP. The hypothesis was that FAT would be low and FAP would be high using this model.
METHODS
Scan retrieval and matching
Under Partners Human Research Committee protocol #2010P001335, high-resolution de-identified CT angiographs were retrospectively collected from a clinical radiology database at Brigham and Women’s Hospital (BWH). Age and gender information was retained. The scans were obtained using a standard head and neck protocol: 16-cm wide-area detector with 0.5-mm slices, 80mAs and 80 kVp, as DICOM files. Scans were reviewed to exclude abnormal findings or memorable expressions.
One-hundred-and-forty-three normal CT angiographs evenly distributed across genders and age groups were collected. Within each age-gender group, scans were randomly and equally divided into Donors and Recipients. Each Recipient was paired with a gender-matched, 10 years younger to 20 years older Donor (Table 1).
Table 1.
Age and gender distribution of matched Donor-Recipient pairs
| RECIPIENTS | |||||||
|---|---|---|---|---|---|---|---|
| DONORS | Females | Age (years) | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 |
| 20–29 | 3 | 4 | |||||
| 30–39 | 3 | 2 | 3 | ||||
| 40–49 | 1 | 1 | 3 | 3 | |||
| 50–59 | 1 | 1 | 2 | 3 | |||
| 60–69 | 1 | 2 | 4 | ||||
| Males | 20–29 | 2 | 4 | ||||
| 30–39 | 3 | 2 | 3 | ||||
| 40–49 | 1 | 1 | 3 | 3 | |||
| 50–59 | 1 | 1 | 2 | 3 | |||
| 60–69 | 1 | 2 | 4 | ||||
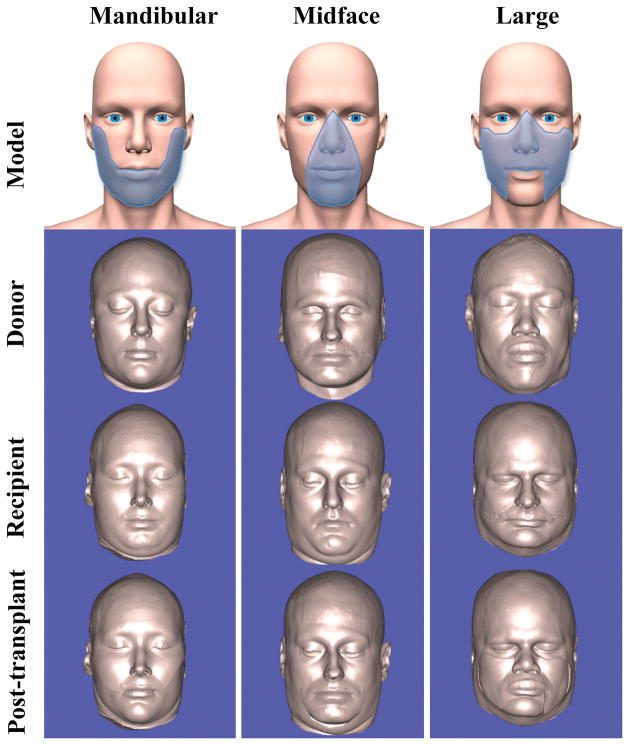
Based on facial defects observed in patients screened at BWH for FT,15 three donor allograft patterns were designed (Mandibular, Midface, and Large) (Figure 1) that simulated clinical scenarios of facial transplantation and involved various aesthetic units. The Mandibular, Midface, and Large patterns mimicked defects involving the entire mandible, the central face, and the structures transplanted in the first clinical case at BWH,16 respectively. The Mandibular pattern extended from the soft tissue overlying the top of the mandibular condyle in a beard-like distribution to the oral commissure bilaterally, including the lower lip and chin. The Midface pattern included central features (units 2, 5, 6, and 7) bilaterally, in addition to a small portion of the cheek just lateral to the nasolabial folds to mimic clinical operative plans for similar defects. The Large pattern included the central features and most of the cheek bilaterally (units 2, 4, and 5), excluding the chin and lower lip (units 6 and 7). The Midface and Large patterns included most aesthetic units whereas the Mandibular pattern only included the chin. The Mandibular and Large patterns covered a large area of the face, in contrast to the Midface pattern. Transplant patterns were assigned randomly such that each gender group had an approximately equal pattern distribution (Table 2).
Figure 1. Facial defect patterns simulated in the VFTs.
Three patterns (Mandibular, Midface, and Large, top row, shaded areas) were used to create defects in Recipient models [third row] and extract allografts from Donor models [second row] to perform VFTs [bottom row]. For purposes of illustration, examples of individual VFTs for each pattern type are presented in the bottom three rows. The example Mandibular pattern Post-transplant VFT model [bottom row, left column] involved a 31-year-old female donor [second row, left column] and a 22-year-old female recipient [third row, left column]. The Midface pattern Post-transplant VFT model example [bottom row, center column] involved a 38-year-old male donor [second row, center column] and a 29-year-old male recipient [third row, center column]. Lastly, the example of a Large pattern Post-transplant VFT model [bottom row, right column] involved a 54-year-old male donor [second row, right column] and a 43-year-old male recipient [third row, right column].
Table 2.
Distribution of virtual face transplant patterns by gender
| Pattern | Male (n) | Female (n) |
|---|---|---|
| Mandibular | 11 | 13 |
| Midface | 13 | 12 |
| Large | 12 | 12 |
Virtual face transplantation
Scans imported into surgical planning software (Surgicase CMF, Materialise, Leuven, Belgium) were converted into 3D models comprising all structures above the neck except hair. Separate reconstructions of bone and soft tissue were extracted from the CT data using specific threshold parameters. The spatial relationships between soft tissue and bone were maintained for each scan. Most models were used only once either as Donor or Recipient, but 3 were reused in one new role.
In real FTs, tissues are dissected from and attached in the planes of the donor and recipient bone, respectively. Here, however, Recipient and Donor models were superimposed in 3D virtual space and defects were created simultaneously using the same cut to obtain the most realistic virtual alignment. Three bony landmarks were used as reference points: nasion, menton, and sella turcica (see Figure, Supplemental Digital Content 1). Because of differences in skull size and shape, best efforts were made to fit these three points. For the Midface and Large patterns, priority was given to the nasion for anterior-posterior and superior-inferior positioning and to the line between the nasion and the base of the sella turcica for lateral positioning. For the Mandibular pattern, priority was given to the menton for anterior-posterior and superior-inferior positioning and to the line between the nasion and the base of the sella turcica for lateral positioning, as in reality surgical adjustment of the mandible to create a proper fit is clinically easier.
After Recipient and Donor alignment, a specific facial defect was created in the Recipient soft tissue model and “filled” with matching tissues extracted from the Donor soft tissue model. Briefly, two identical cuts were made in the soft tissue of each Recipient and Donor using the osteotomy tool of SurgiCase: one in the shape of the transplant pattern and perpendicular to the surface of the face (“cookie-cutter”) and the other perpendicular to and completely intersecting the “cookie cutter” plane within the soft tissue to create a “cup”. The Post-transplant model was generated by visualizing the superposition of the Recipient with its defect and the Donor allograft without moving any of the pieces in the virtual space (see PowerPoint presentation, Supplemental Digital Content 2).
Seventy-three VFTs were thus completed (Tables 1 and 2). All soft tissue models were displayed in Caucasian skin tone. Thirty-second videos were generated for each model showing the rotating sequence: front-facing, 90° to the right, front-facing, 90° to the left, front-facing, 45° up, front-facing, 45° down, and front-facing. Post-transplant model videos were labeled “IMAGE A”, while Recipient and Donor model videos were randomly labeled “IMAGE B” or “IMAGE C”.
Reviews
Two male and two female layperson reviewers with a minimum of high school diploma from each of five age groups (20–29, 30–39, 40–49, 50–59, and 60–69) were recruited; they were not involved in the medical field, and received compensation. Reviewers observed each of 73 sets of matched IMAGES A, B and C. IMAGE A was shown first by itself for 30 seconds, then IMAGES B and C were shown together for 30 seconds, and then the reviewer answered Questions 1 and 2 (Box 1) by assessing facial appearance based on facial features, their relation to each other on the face and overall appearance, and refraining from judging computer-generated scars or poorly fitting allografts.
Box 1.
Question 1
The person in IMAGE A:
Looks a lot like the person in IMAGE B
Looks a little like the person in IMAGE B
Does not look like the person in IMAGE B
I am not sure if it looks like the person in IMAGE B
Question 2
The person in IMAGE A:
Looks a lot like the person in IMAGE C
Looks a little like the person in IMAGE C
Does not look like the person in IMAGE C
I am not sure if it looks like the person in IMAGE C
Reviewers took a short break after every 15 tasks. The order of appearance for the sets was randomized with respect to surgical pattern and VFT gender. Reviewers recorded their responses on paper; these were transcribed into Excel (Microsoft, Redmond, WA, USA) and the transcription was verified. Questions 1 and 2 randomly assessed FAP or FAT because Images B and C were randomly assigned as Donor or Recipient to prevent reviewer identification. Randomization was unmasked during data transcription.
Statistical methods
Results were calculated using proportions, means with standard deviations, and medians with interquartile ranges. Confidence intervals for FAT and FAP were calculated adjusting for clustering of the 20 reviews within each of the 73 matched sets. For each Recipient and Donor Question, the proportions of (a) and (b) answers were combined to a positive assessment category: “Looks like”. The proportion of “Looks like” to “c) Does not look like” was compared against a neutral null hypothesis of 50%/50%, using a one-sample Rao-Scott Pearson chi-square test, adjusting for clustering of the 20 reviews within each of the 73 matched sets.
FAT and FAP were determined for each transplant pattern, for genders and for age groups within genders. Similar confidence estimates and one-sample tests against a neutral null hypothesis of 50%/50% were used. Additionally, for each pattern, tests for equal results between pairs of groups were calculated using Rao-Scott Pearson chi-square tests, adjusting for clustering of the 20 reviews within each of the 73 matched sets. P-values were 2-sided and considered statistically significant if P < 0.05. Bonferroni corrections were used to adjust p-values for multiple testing. All analyses were performed with SAS version 9.2 (SAS Institute Inc, Cary, NC).
For each comparison between pairs of groups, the study design provided at least 80% power to detect an odds ratio of at least 1.5 (after dichotomizing outcomes FAT and FAP) using a Rao-Scott Pearson chi-square test statistic with a significance level of 0.05.
RESULTS
Reviewer response characterization
Reviewer tasks generated 1437 responses, and 23 missing observations.
Overall FAP/FAT
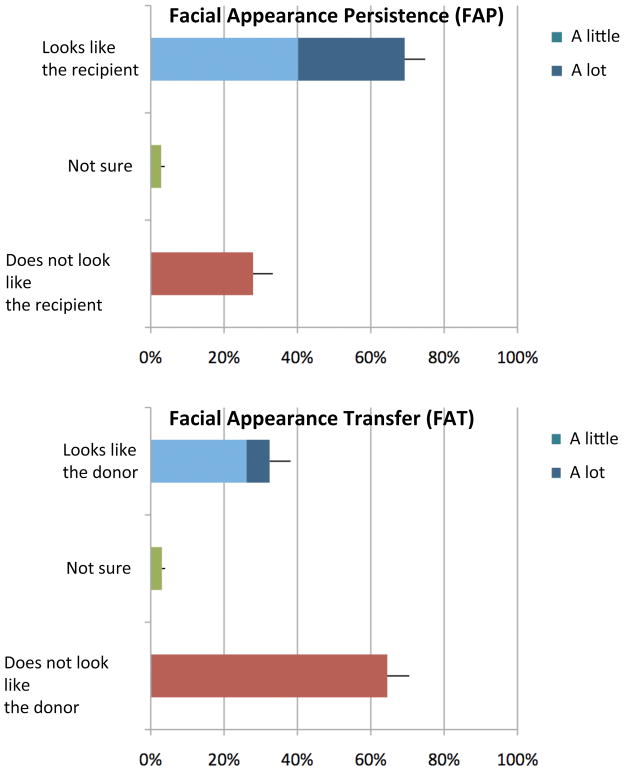
Of the significantly more reviewers who thought the post-transplant face looked like the recipient (69.2%, p<0.001) than not (27.9%) (Figure 2, upper graph), 42.0% felt it “looked a lot” like the recipient.
Figure 2. Overall rates of FAP [upper graph] and FAT [lower graph].
The proportion of reviewer responses to the Recipient Question [upper graph] and Donor Question [lower graph] is displayed. [Upper Graph] FAP (the Post-transplant model looks like the Recipient) is significantly high (p < 0.001) and [lower graph] FAT (the Post-transplant model looks like the Donor) is significantly low (p < 0.001) when tested against a 50%/50% null hypothesis. The error bars represent the 95% confidence interval for the each of the fields.
Of the significantly fewer reviewers who thought the post-transplant face looked like the donor (32.4%, p<0.001) than not (64.5%) (Figure 2, lower graph), 19.5% felt it “looked a lot” like the donor.
Effect of transplant pattern
FAP was significantly high (p < 0.001, p < 0.01, p < 0.05) for each transplant pattern (Mandibular, Midface, Large, respectively) (Figure 3, upper graph). FAP was higher for the Mandibular pattern than for the Midface (p < 0.001) or Large patterns (p < 0.001). Of those that positively identified FAP, 50.3%, 33.5%, and 40.0% reported strong FAP with the Mandibular, Midface, and Large patterns, respectively.
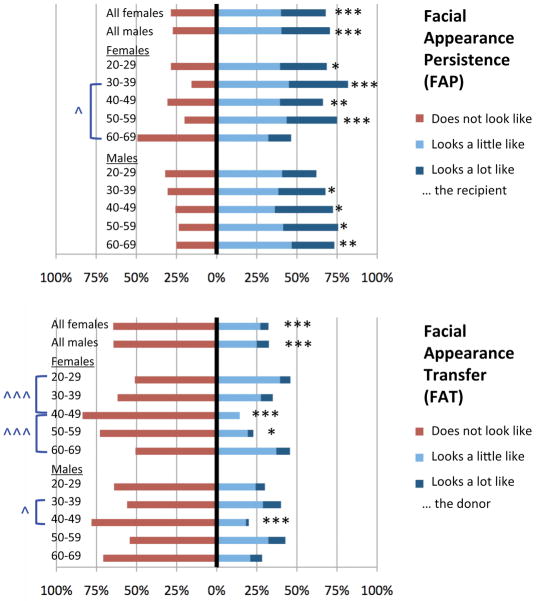
Figure 3. Rates of FAP [upper graph] and FAT [lower graph] for three VFT patterns.
The proportion of reviewer responses to the Recipient Question [upper graph] and Donor Question [lower graph] for three facial transplant patterns (Mandibular, Midface, Large) are displayed. The asterisks represent the p-values from a one-sample chi-squared test of the “Looks like”/”Does not look like” ratio against a null hypothesis of a 50%/50% split. The wedges (^) represent the p-values from the pair-wise test for equal FAP or FAT between patterns. */^ = p < 0.05; **/^^ = p < 0.01; ***/^^^ = p < 0.001; N.S. = not significant at α = 0.05. The Mandibular pattern has significantly higher rates of FAP than the Midface or Large patterns [upper graph] and significantly lower rates of FAT than the Midface or Large patterns [lower graph].
FAT was low for the Mandibular (p < 0.001) and Large (p < 0.01) patterns, but not for the Midface pattern (Figure 3, lower graph). FAT was lower in the Mandibular pattern than in the Midface (p < 0.001) and Large patterns (p < 0.05). Of those that positively identified FAT, only 17.6%, 19.3%, and 20.9% reported strong FAT with the Mandibular, Midface, and Large patterns, respectively.
Effect of Recipient Gender and Age
No significant effect of recipient gender in overall FAT or FAP was detected (Figure 4). All age-gender recipient groups had significantly high FAP (except females 60–69 years and males 20–29 years). Only three of the age-gender recipient groups had significantly low FAT (females 40–59 years and males 40–49 years). FAP was significantly higher for females aged 30–39 than for those aged 60–69 (p < 0.05) and FAT was significantly lower for females aged 40–49 vs. 20–29 (p < 0.001), for females aged 40–49 vs. 60–69 (p < 0.001), and for males aged 40–49 vs. 30–39 (p < 0.05).
Figure 4. Rates of FAP [upper graph] and FAT [lower graph] for various Recipient age-gender groups.
The proportion of reviewer responses to the Recipient Question [upper graph] and Donor Question [lower graph] for all females, all males, and all subsets of age groups within each gender (20–29, 30–39, 40–49, 50–59, and 60–69 years). Each stacked graph includes the positive assessment of FAP [upper graph] or FAT [lower graph] (“looks like the Recipient” and “looks like the Donor”, respectively) on the right of the 0% line (light and dark blue) and the negative assessment of FAP [lower graph] or FAT [upper graph] (“does not look like the Recipient” or “does not look like the Donor”, respectively) on the left of the 0% line (red). “Not sure” responses are not shown in the interest of simplicity. The two topmost stacked bars in the upper and lower graph show overall rates of FAP and FAT, respectively, for each gender. The black asterisks represent the p-values from a one-sample chi-squared test of the “Looks like”/”Does not look like” ratio against a null hypothesis of a 50%/50% split. The blue asterisks represent the p-values from the pair-wise test for equal FAP or FAT between patterns. */^ = p < 0.05; **/^^ = p < 0.01; ***/^^^ = p < 0.001. Lack of an asterisk or wedge indicates not significant at α = 0.05.
DISCUSSION
This study used three-dimensional VFTs to address limited knowledge regarding facial appearance transfer and persistence after facial transplantation, and evaluated the effect of transplantation of different facial units and the effect of recipient age and gender on FAP and FAT.
Study-independent reviewers evaluated FAP and FAT without bias. Reviewers were blinded as to which of IMAGE A or B were the donor or recipient of the VFT, and one half of the reviewers were shown the sequences of VFTs in reverse order, to rule out bias due to exhaustion or familiarity.
While FAP results were similar to an earlier two-dimensional study,11 FAT was higher, likely due to the increased complexity and realism of the model. The percentage of reviewers who felt strongly about positive FAP (42.0%) was higher than that of reviewers who felt strongly about positive FAT (19.5%). Although this was not statistically tested, the strength of the reviewers’ perception of FAP and FAT suggests that, when positively identified, FAP is a more dominant perception than FAT. Evaluative comparison between the findings of this and the earlier study is not possible, as the methodologies differed in more than just the use of two dimensional versus three-dimensional images. In the prior study, FAP was assessed using an unfamiliar donor and a familiar recipient, whereas FAT was assessed using familiar donors and unfamiliar recipients. Here, all donors and recipients were unfamiliar.
VFTs were performed by creating a facial defect in the soft tissues of the Recipient and transplanting a soft tissue allograft from the Donor after aligning bony landmarks. Although the models were realistic, they lacked hair, had variations in skin texture, and were static 3D captures with a single neutral expression (Figure 1). Additionally, there were some defects due to artifacts of metal (e.g. dental fillings) and/or from unnatural osteotomy cuts. In reality, postoperative soft tissue scarring, fat or muscle atrophy, multiple planned revisions, and weight gain or loss also contribute to final facial appearance. However, this is unavoidable in any potential simulation as no computer model can predict those specific, and often unique, changes to a patient post-operative. We believe that these drawbacks are outweighed by the ability of simulation to conduct such an investigation logistically and ethically.
Real allograft design occurs on a case-by-case basis, depending on the severity of the Recipient’s defect. While the number of potential designs we can test for are limitless, we used three clinically relevant patterns based on patient screening at BWH. Although these designs are unlikely to exactly match the specific unique injuries of future patients, this and other future studies will allow us to better prognosticate this information for general classes of injury.
The appearance of the soft tissue is determined in part by the underlying bone. Some clinical cases require that bone be transplanted with the allograft, whereas others only require transplant of soft tissues. In the latter cases, the underlying recipient’s bone helps shape the donor tissue to the recipient’s bony structure, maximizing FAP. In this study, the shape of the donor allograft includes all underlying donor muscle, cartilage, and bone. Therefore, these VFTs mimicked the “worst case scenario” of FAT. Even in this worst-case scenario, overall FAT and FAP rates were low and high, respectively (Figure 2).
High FAP was observed for all facial defect patterns (Mandibular, Midface, and Large), and low FAT was observed for the Mandibular and Large patterns (Figure 3). The Mandibular pattern had the highest FAP and lowest FAT likely because it included the least number of central aesthetic units. The Midface and Large patterns both included the same number of central facial units, but the Large pattern covered a larger area. There was no significant difference in FAP or FAT between these two, suggesting that the specific aesthetic units included with the allograft, and not the size of the allograft contributes most to FAP and FAT.
This study followed the guidelines of donor’s age between 20 years younger and 10 years older than the recipient.14 High FAP and low FAT were found regardless of gender. Further breakdown into age-gender groups showed mostly high FAP, but fewer groups showed low FAT. However, because each group only had 7 or 8 VFTs with a random distribution of patterns, significance testing is unreliable and pairwise testing provides limited information. Interestingly, the 40–49 age group for both genders had significantly lower FAT than other groups. This may result from having a large potential donor age range (Table 1), although if that were the case similar findings would be expected in the 50–59 decade. Reviewers may have been most familiar with the 40–49 age group as that is the largest age group in the U.S. population for both genders.17 Most real cases of FTs to date involved adult males. Only adult age ranges were included in this study because FT has not been performed in children likely due to the inadequacy of informed consent in minors. With improved immunosuppressive therapy in the future, FT may become available to the pediatric population.18 Appearance transfer in this population must also be studied.
CONCLUSIONS
This study’s findings can enrich informed consent for potential recipients of FTs by providing information regarding the likelihood of appearance persistence after transplantation, and for families of potential donors by showing that the appearance of their loved one has a low likelihood to transfer to the recipient. Appearance transfer and persistence are more dependent on the specific aesthetic units included with the facial allograft than on the size of the allograft. Further research can determine how facial units individually and in combinations and underlying bone affect appearance transfer after facial transplantation. Computer simulations of VFT can also help optimize aesthetic matching between donors and recipients by comparing cephalometric measurements of bone and soft tissue. Software that enables soft tissue simulation will facilitate these studies.
Although evaluation of actual FTs would provide the most realistic information about appearance persistence and transfer, the methodology is hampered by the right to anonymity of patients and donors. Virtual face transplantation, therefore, remains the best to obtain statistically significant information about appearance after FT.
Supplementary Material
Donor tissues are shown in green and recipient tissues are shown in red. A three-dimensional cutting plane is used to cut pieces from the donor and recipient and superimpose the donor allograft on the recipient defect.
Superimposed outlines of bone features from CT scans of the Donor (green) and Recipient (red) are shown in (A) coronal, (B) axial, and (C) sagittal sections on a background of the Recipient’s scan. The Donor’s bone and soft tissue are repositioned to match up bony landmarks: sella turcica (long arrows in A and C), menton (short arrow in C), and nasion (arrowhead in C). Note that the pterygoid plates are also aligned (double-headed arrow in B). The three-dimensional rendering of the superimposed bone structures is shown in (D).
Acknowledgments
The authors thank the Greenwall Foundation and National Institutes of Health for funding for this project. The authors also wish to convey their gratitude to the donor families and the New England Organ Bank for their roles in procuring for their patients the gift of a facial allograft.
Funding for this work was received from a National Institutes of Health (NIH) R21 grant and the Greenwall Foundation.
Footnotes
Based on information gathered from scientific meeting presentations and media releases, as well as recently published reviews.
DISCLOSURE
None of the authors have any financial interests or commercial associations that might pose or create a conflict of interest with information presented in this article.
Author contributions:
Chandawarkar: study design, data collection, survey administration, data analysis, drafting of manuscript, figure creation
Diaz-Siso: study design, data collection, manuscript review
Bueno: study design, manuscript review
Jania: data collection
Hevelone and Lipsitz: data analysis
Caterson and Mukundan: study design, data collection
Pomahac: principal investigator, study design, manuscript review and finalization
References
- 1.Pomahac B, Nowinski D, Diaz-Siso JR, et al. Face transplantation. Curr Probl Surg. 2011;48:293–357. doi: 10.1067/j.cpsurg.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Siemionow M, Ozturk C. Face transplantation: outcomes, concerns, controversies, and future directions. J Craniofac Surg. 2012;23:254–259. doi: 10.1097/SCS.0b013e318241b920. [DOI] [PubMed] [Google Scholar]
- 3.Lantieri L. Face transplant: a paradigm change in facial reconstruction. J Craniofac Surg. 2012;23:250–253. doi: 10.1097/SCS.0b013e318241c10b. [DOI] [PubMed] [Google Scholar]
- 4.Goering S. Facing the consequences of facial transplantation: individual choices, social effects. Am J Bioeth. 2004;4:37–39. doi: 10.1080/15265160490496714. [DOI] [PubMed] [Google Scholar]
- 5.Rumsey N. Psychological aspects of face transplantation: read the small print carefully. Am J Bioeth. 2004;4:22–25. doi: 10.1080/15265160490496903. [DOI] [PubMed] [Google Scholar]
- 6.Fattahi T. An overview of facial aesthetic units. J Oral Maxillofac Surg. 2003;61:1207–1211. doi: 10.1016/s0278-2391(03)00684-0. [DOI] [PubMed] [Google Scholar]
- 7.Arno A, Barret JP, Harrison RA, et al. Face allotransplantation and burns: a review. J Burn Care Res. 2012 Sep-Oct;33:561–576. doi: 10.1097/BCR.0b013e318247eb06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maurer D, Grand RL, Mondloch CJ. The many faces of configural processing. Trends Cogn Sci. 2002;6:255–260. doi: 10.1016/s1364-6613(02)01903-4. [DOI] [PubMed] [Google Scholar]
- 9.Young AW, Hellawell D, Hay DC. Configurational information in face perception. Perception. 1987;16:747–759. doi: 10.1068/p160747. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka JW, Farah MJ. Parts and wholes in face recognition. Q J Exp Psychol A. 1993;46:225–245. doi: 10.1080/14640749308401045. [DOI] [PubMed] [Google Scholar]
- 11.Pomahac B, Aflaki P, Nelson C, et al. Evaluation of appearance transfer and persistence in central face transplantation: a computer simulation analysis. J Plast Reconstr Aesthet Surg. 2010;63:733–738. doi: 10.1016/j.bjps.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 12.Xia JJ, Phillips CV, Gateno J, et al. Cost-effectiveness analysis for computer-aided surgical simulation in complex cranio-maxillofacial surgery. J Oral Maxillofac Surg. 2006;64:1780–1784. doi: 10.1016/j.joms.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 13.Baccarani A, Follmar KE, Das RR, et al. A pilot study in sub-SMAS face transplantation: defining donor compatibility and assessing outcomes in a cadaver model. Plast Reconstr Surg. 2007;119:121–129. doi: 10.1097/01.prs.0000245078.66513.c0. [DOI] [PubMed] [Google Scholar]
- 14.Aflaki P, Nelson C, Balas B, et al. Simulated central face transplantation: age consideration in matching donors and recipients. J Plast Reconstr Aesthet Surg. 2010;63:e283–285. doi: 10.1016/j.bjps.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Pomahac B, Diaz-Siso JR, Bueno EM. Evolution of indications for facial transplantation. J Plast Reconstr Aesthet Surg. 2011 Nov;64:1410–1416. doi: 10.1016/j.bjps.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 16.Pomahac B, Pribaz J, Eriksson E, et al. Restoration of facial form and function after severe disfigurement from burn injury by a composite facial allograft. Am J Transplant. 2011;11:386–393. doi: 10.1111/j.1600-6143.2010.03368.x. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Census Bureau. US Census. 2007. [Google Scholar]
- 18.Washington KM, Zanoun RR, Cadogan KA, et al. Composite tissue allotransplantation for the reconstruction of congenital craniofacial defects. Transplant Proc. 2009;41:523–527. doi: 10.1016/j.transproceed.2009.01.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Donor tissues are shown in green and recipient tissues are shown in red. A three-dimensional cutting plane is used to cut pieces from the donor and recipient and superimpose the donor allograft on the recipient defect.
Superimposed outlines of bone features from CT scans of the Donor (green) and Recipient (red) are shown in (A) coronal, (B) axial, and (C) sagittal sections on a background of the Recipient’s scan. The Donor’s bone and soft tissue are repositioned to match up bony landmarks: sella turcica (long arrows in A and C), menton (short arrow in C), and nasion (arrowhead in C). Note that the pterygoid plates are also aligned (double-headed arrow in B). The three-dimensional rendering of the superimposed bone structures is shown in (D).