Abstract
Objective
Obesity is a major public health problem that increases risk for a broad spectrum of co-morbid conditions. Despite evidence for a strong genetic contribution to susceptibility to obesity, previous efforts to discover the relevant genes using positional cloning have failed to account for most of the apparent genetic risk variance.
Design and Methods
Deploying a strategy combining analysis of exome sequencing data in extremely obese members of four consanguineous families with segregation analysis, we screened for causal genetic variants. Filter-based analysis and homozygosity mapping were used to identify and prioritize putative functional variants.
Results
We identified two novel frameshift mutations in the Leptin Receptor (LEPR) in two of the families.
Conclusions
These results provide proof-of-principle that whole-exome sequencing of families segregating for extreme obesity can identify causal pathogenic mutations. The methods described here can be extended to additional families segregating for extreme obesity and should enable the identification of mutations in novel genes that predispose to obesity.
Keywords: genetics of obesity, leptin receptor
Introduction
Obesity is a common and increasingly prevalent risk factor for many diseases including type 2 diabetes, atherosclerosis, and some forms of cancer, as well as all-cause mortality (1, 2). Heritability estimates for body mass index (BMI) indicate a substantial genetic contribution (h2~0.4–0.7) (3, 4), but efforts to account for this variance have had limited success. Monogenic forms of obesity are rare, and common genetic variants account for only 2–4% of the familial risk (5). Rare variants with large effect sizes that may account for some of the unexplained heritability in obesity have not been systematically investigated in previous studies of human obesity (6). The search for such variants could identify novel genes in body weight regulation.
In this study we utilized whole-exome sequencing (WES) of extremely obese individuals from four consanguineous families to examine the role of rare coding variations in the pathogenesis of obesity. Sampling at the phenotypic extremes increases the probability of identifying highly penetrant risk alleles (7) and enriches for monogenic forms of common complex traits (8). Moreover, focusing on early onset extreme obesity can reduce etiological heterogeneity, as there is less time for environmental factors to contribute to extreme obesity in children (9). Homozygosity mapping can further improve the efficiency of disease mutation identification in consanguineous cases by focusing on regions of homozygosity originating from a recent common ancestor of both parents, which comprise approximately 10% of the exome in offspring of first cousins (10).
Here we report the identification of two novel Leptin Receptor (LEPR) frameshift mutations (p.H160LfsX9 and p.C186AfsX27) in severely obese children from two consanguineous families. Our findings demonstrate that WES coupled with extreme sampling in consanguineous families is an effective method for identifying pathogenic mutations that cause obesity and, potentially, other heritable disorders.
Methods and Procedures
Subjects
Four consanguineous families were recruited and provided informed consent and assent when appropriate as part of our ongoing study of the molecular genetic basis of human obesity, using protocols approved by the Institutional Review Boards at Columbia University Medical Center (New York, NY), The Rockefeller University (New York, NY), and the Intramural NIH Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Bethesda, MD). Genomic DNA was extracted from whole blood or saliva using a DNA extraction kit (Gentra DNA Isolation Kit; Qiagen, Valencia, CA) or Oragene DNA (DNA Genotek, Ontario, CA). Circulating leptin concentration was measured in serum samples using human leptin immunoassay kits (Linco Research, St. Charles, MO; Mayo Medical Laboratories New England, Wilmington, MA)
Study Design
We sequenced the probands from four consanguineous unions and an affected sibling from one family (Table 1) to identify rare recessive variants within regions of homozygosity. Affymetrix 6.0 microarrays were used to genotype affected individuals to rule out structural variations that cosegregated with obesity and to identify regions of homozygosity using Homozygosity Mapper (11).
Table 1.
Anthropometric measurements at time of enrollment and endocrine measurements at age(s) indicated for individuals with whole-exome sequence. − indicates a mutation + indicates wild type sequence. N/A indicates not available.
| Family ID |
Subject ID |
LEPR Mutation Status |
Gender | Age at Enrollment |
Weight (kg) |
Height (cm) |
BMI (kg/m2) |
BMI Percentile |
Circulating [Leptin] (ng/mL) |
Fasting [Insulin] (µIU/mL) |
Pubertal Status |
Acanthosis Nigricans |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 283 | 1511 | −/− | M | 1 year 3 months |
22.5 | 80 | 35.2 | >98 | Age 1 36.1 |
Age 11 53.0 |
Age 13 Tanner I |
+ |
| 466 | 2150 | −/− | F | 12 years | 107 | 138.5 | 55.8 | 99.7 | Age 14 57.1 |
Age 12 41.3 Age 14 23.0 |
Age 14 Breasts Tanner V Public hair Tanner III |
+ |
| 466 | 2239 | −/− | M | 14 years 11 months |
110 | 159.6 | 43.2 | 99.9 | Age 13 62.0 |
Age 13 29.5 |
Age 13 Tanner I Testes 2.5 mL Tanner II |
+ |
| 475 | 2173 | +/+ | F | 11 years | 135.5 | 149 | 61.0 | 99.9 | Age 14 years 5 months 73.3 |
Age 13 69.1 |
Age 13 Breasts Tanner IV Genitals Tanner V |
+ |
| 489 | 2206 | +/+ | M | 9 years | 115 | 135 | 63.0 | 99.6 | Age 9 50.5 |
N/A | N/A | N/A |
Genomic DNA (3 µg) was fragmented and exons were captured using the Agilent SureSelect™ Human All Exon kit. Libraries were sequenced with 100 bp paired-end reads on an Illumina HiSeq 2000 according to the manufacturer’s protocol. High quality sequencing reads were aligned to the human reference genome sequence human assembly hg19 using the Burrows-Wheeler Aligner v0.5.9 (12), allowing up to five mismatched, inserted or deleted bases per 100 bp read. The Genome Analysis Toolkit (GATK) Unified Genotyper v1.0 was used to refine local alignment of reads, recalibrate base quality scores, and call variants (single nucleotide variants [SNVs] and insertions/deletions [indels]) within targeted regions (13). In addition to the default GATK filters (12), variants were further filtered to have a minimum genotype quality of 30, a minimum quality depth of 5, a minimum strand bias of −0.10, and a maximum fraction of reads with mapping quality of zero at 10%.
Analysis of WES Data
To identify potentially damaging rare variants, we first identified variants that were functional (non-synonymous, frameshift, and splice site) and rare (minor allele frequency <1% in the 1000 Genomes Project (www.1000genomes.org), dbSNP (www.ncbi.nlm.nih.gov/projects/SNP/), and the NHLBI Exome Variant Server (EVS; http://evs.gs.washington.edu/EVS/) databases). We then computationally analyzed SNVs and indels using algorithms that accounted for biochemical, evolutionary, and structural information (14). GenomeBrowse (http://www.goldenhelix.com/GenomeBrowse/; Golden Helix, Bozeman, MT) was used to visualize sequences for all homozygous rare variants to exclude calls due to shallow sequence depth and misalignment of short reads. Our analyses were restricted to homozygous SNVs and indels, and variants mapping to regions of homozygosity were prioritized. Variants with high composite pathogenicity scores (>5) were prioritized for confirmatory dideoxy sequencing and segregation analysis in all available family members.
Results
Clinical Descriptions
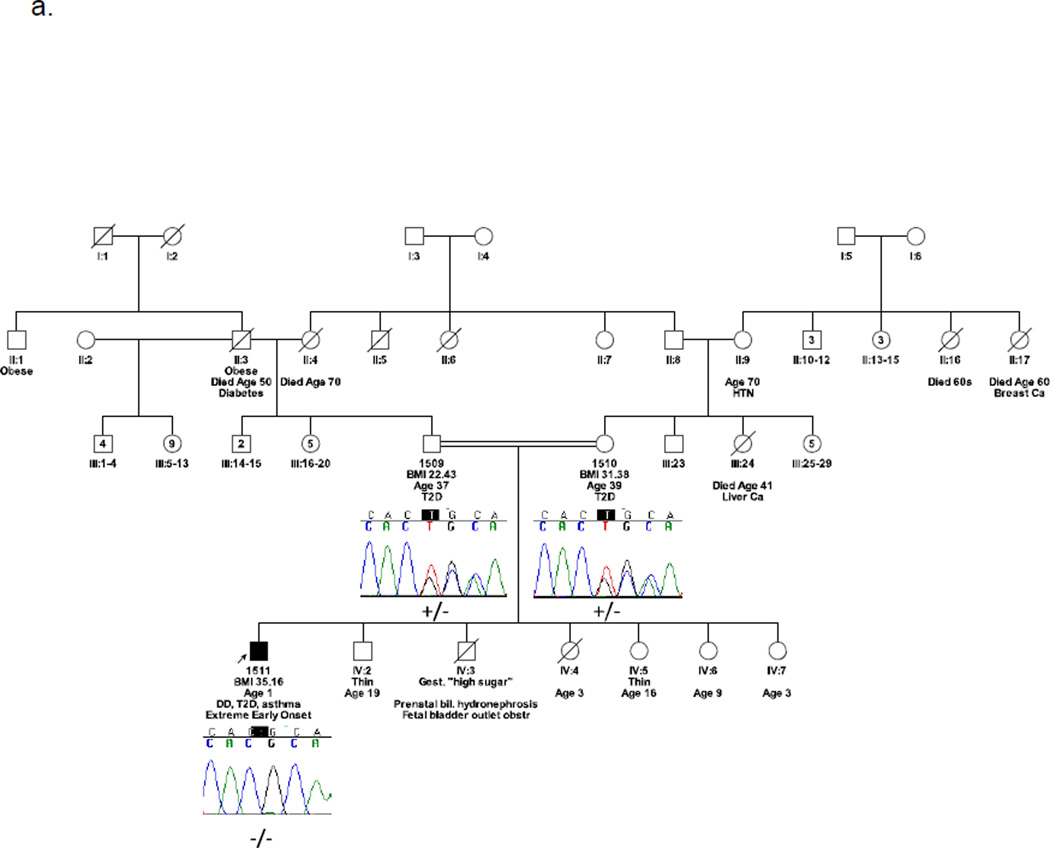
Family 283
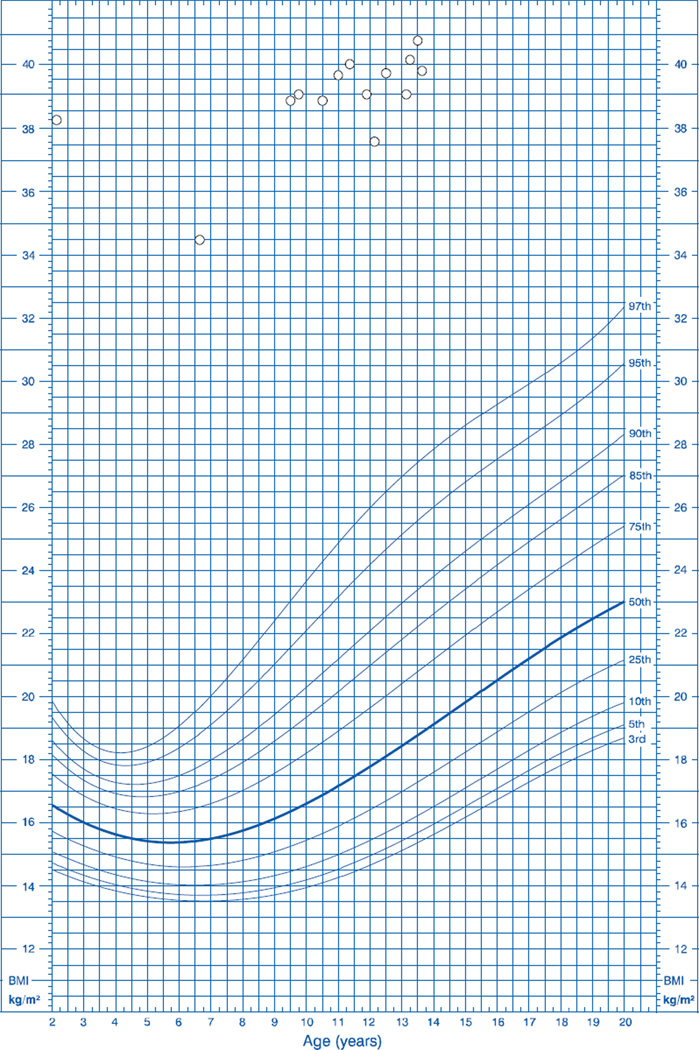
The proband (1511) from Family 283 is the son of first cousins originating from Guinea (Figure 1a). During infancy he displayed an insatiable appetite and required frequent feeding, gaining approximately one pound per week. He reached 8.5 kg (above 97th percentile) at 2 months of age. At age 1 year and 3 months, he weighed 22.5 kg (above 97th percentile) and his length was 80 cm (above 50th percentile), with a BMI (35.2 kg/m2) and weight-for-length percentile above 97%. At this age his circulating leptin concentration was 36.1 ng/mL, almost double the average level in obese adult males (~20 ng/mL) (15). He has continued to exhibit excessive weight gain, and his BMI has remained consistently above the 99th percentile (Figure 2) despite efforts to limit his caloric intake.
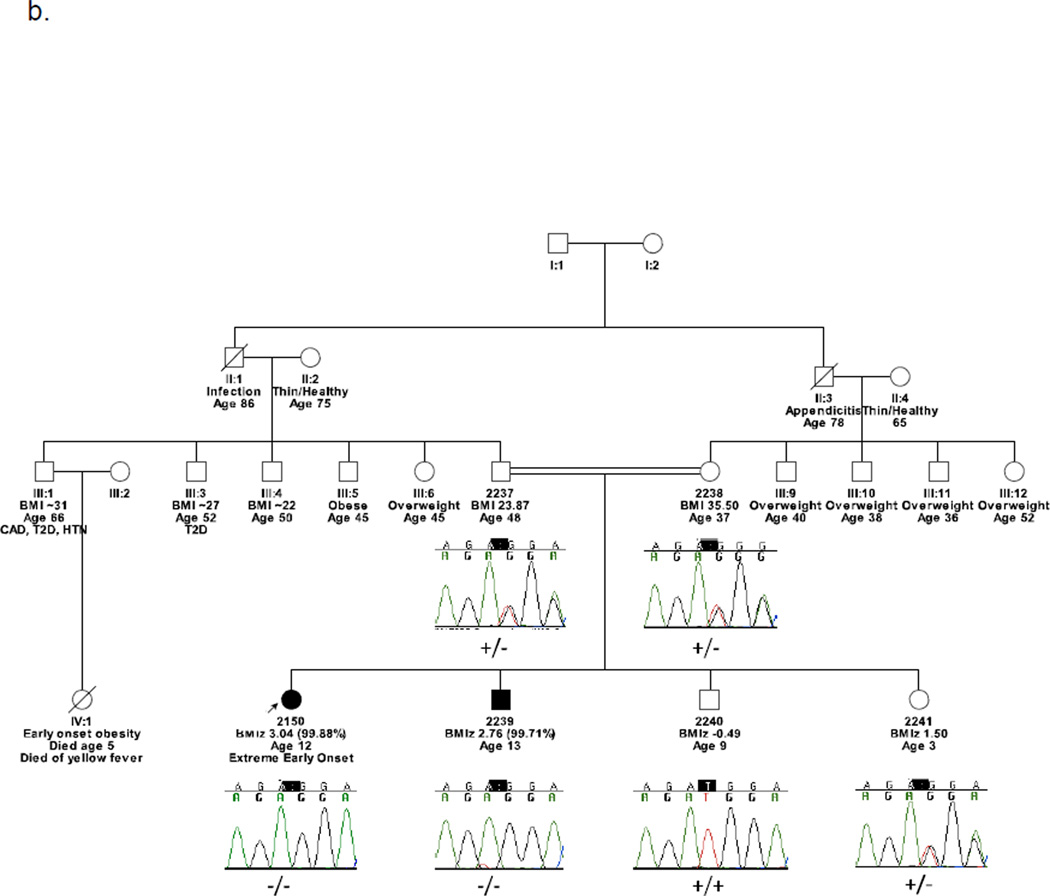
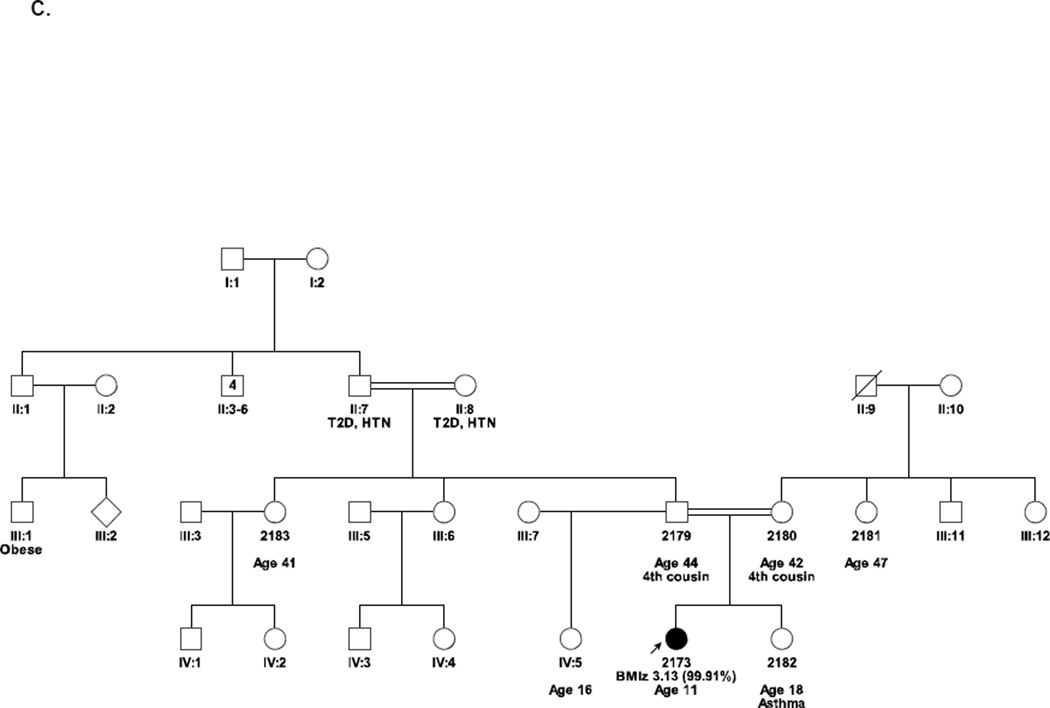
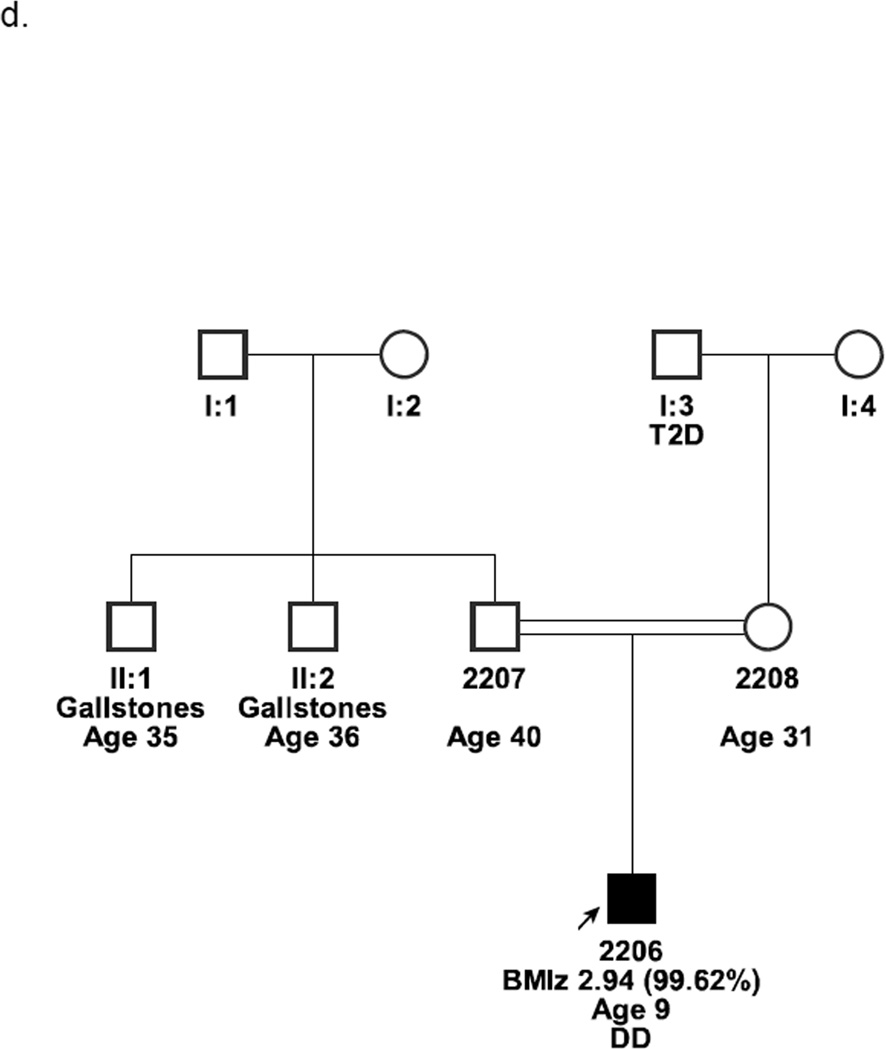
Figure 1.
Pedigrees from families of all individuals sequenced. Chromatograms depict results of confirmatory dideoxy sequencing.
Abbreviations: DD: developmental delay; T2D: type 2 diabetes; HTN: hypertension.
Figure 1a. Family 283: Guinean family segregating a p.C186AfsX27 (c.556delT) mutation in LEPR. WES was performed on individual 1511.
Figure 1b. Family 466: Sudanese family segregating a p.H160LfsX9 (c.479delA) frameshift mutation in LEPR. WES was performed on individuals 2150 and 2239.
Figure 1c. Family 475. Dominican family. Parents are fourth cousins. WES was performed on individual 2173.
Figure 1d. Family 489. Jordanian family. Parents are related but the extent of consanguinity is uncertain. WES was performed on individual 2206.
Figure 2.
Growth chart with body mass index-for-age percentiles for the proband (1511) from family 283. Modified from the Center for Disease Control’s individual growth charts for boys in 2000.
Clinical genetic testing included karyotype, fluorescent in-situ hybridization (FISH) and methylation analysis for Prader-Willi Syndrome and Melanocortin 4 Receptor (MC4R), and Cohen Syndrome molecular testing that were all normal. His bone age at a chronological age of 6 was advanced at 13 years. Endocrine evaluation at age 11 years demonstrated normal prepubertal cortisol and an elevated fasting serum insulin concentration (53 µIU/mL).
In addition to having excessive weight gain and hyperphagia, the patient is mildly developmentally delayed and did not speak until age 2 years. He is currently receiving special education. He also has asthma and was diagnosed with type 2 diabetes at age 12 years. At age 13 an abdominal ultrasound showed diffusely increased hepatic echogenicity, indicative of hepatic steatosis.
Currently he continues to struggle with hyperphagia, never feeling satiated after meals. At age 13, he weighed 121.7 kg and was 175 cm tall (above 97th percentile), with a BMI of 39.7 kg/m2 (99.6th percentile). He is Tanner Stage I. Acanthosis nigricans was present on the neck and axillae.
Family 466
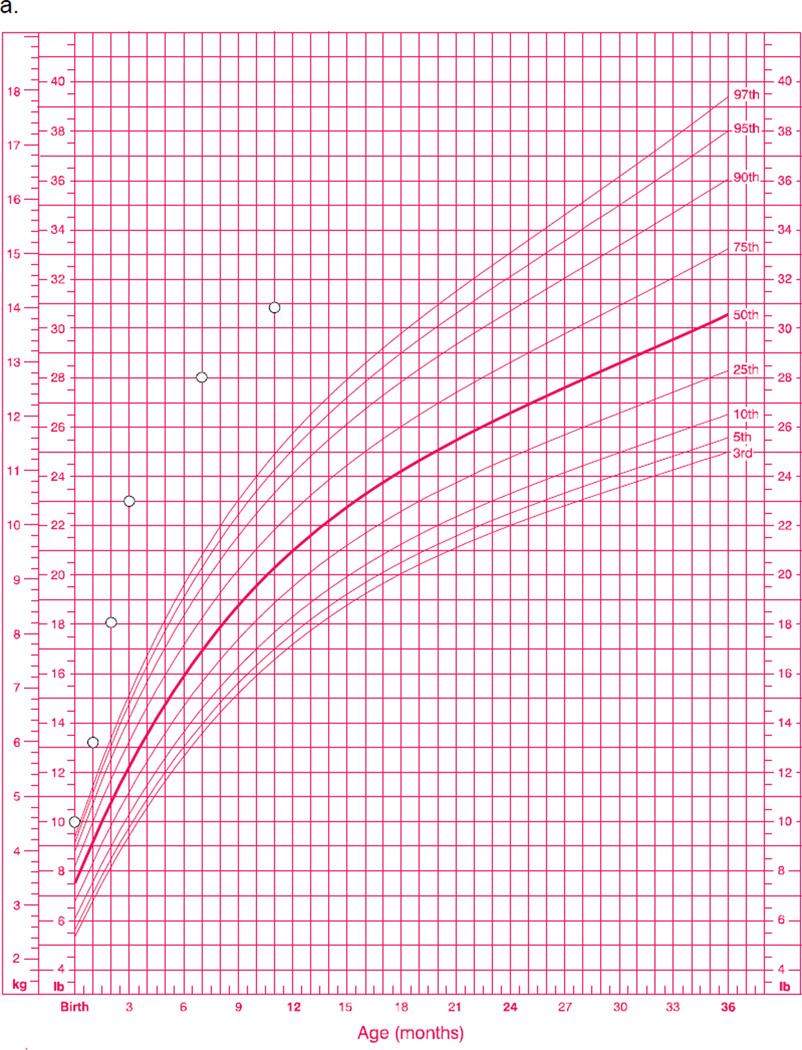
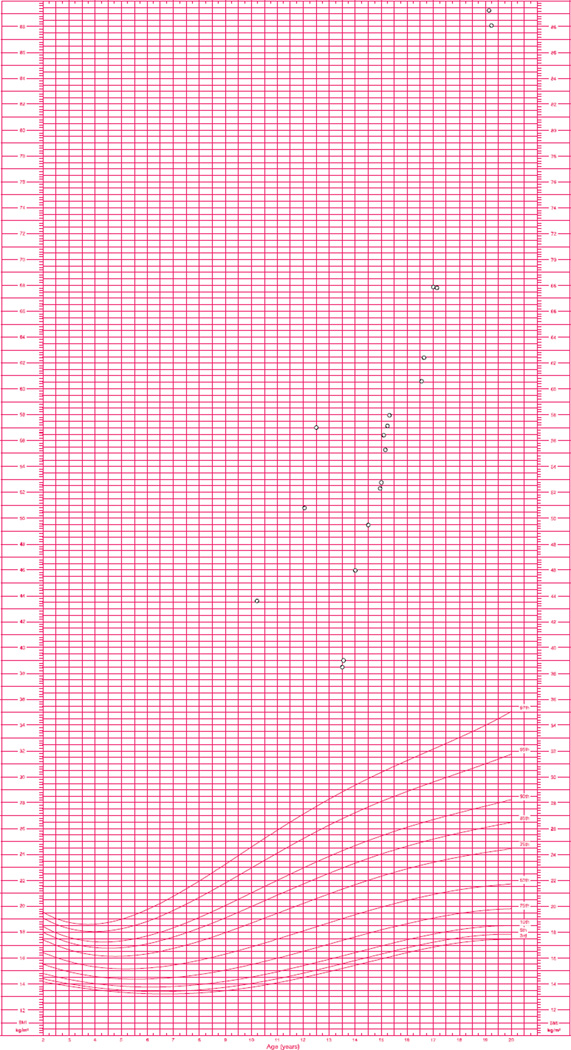
Family 466 is Sudanese with two affected children (2150 and 2239) of a first cousin marriage (Figure 1b). The proband (2150) began rapidly gaining weight at 1 month of age (Figure 3a). At age 12 years, she was 138.5 cm tall (~5th percentile) and weighed 107 kg (BMI of 55.8 kg/m2 [99.9th percentile]), with an abdominal circumference of 132.9 cm (above 90th percentile (16)). Her BMI has consistently remained above the 99th percentile (Figure 3b). Her circulating leptin concentration at this age was 57.1 ng/mL, which was above the average level in obese females (~40 ng/mL) (15). She had sleep apnea and impaired glucose tolerance. Her fasting serum insulin was elevated at 41.3 µIU/mL although her HbA1c level of 5.2% was normal (normal < 5.7%). Thyroid and adrenal function were normal. At age 14 years and 11 months she was premenarchal, and her bone age was 13 years and 3 months. Acanthosis nigricans was present over multiple skin regions.
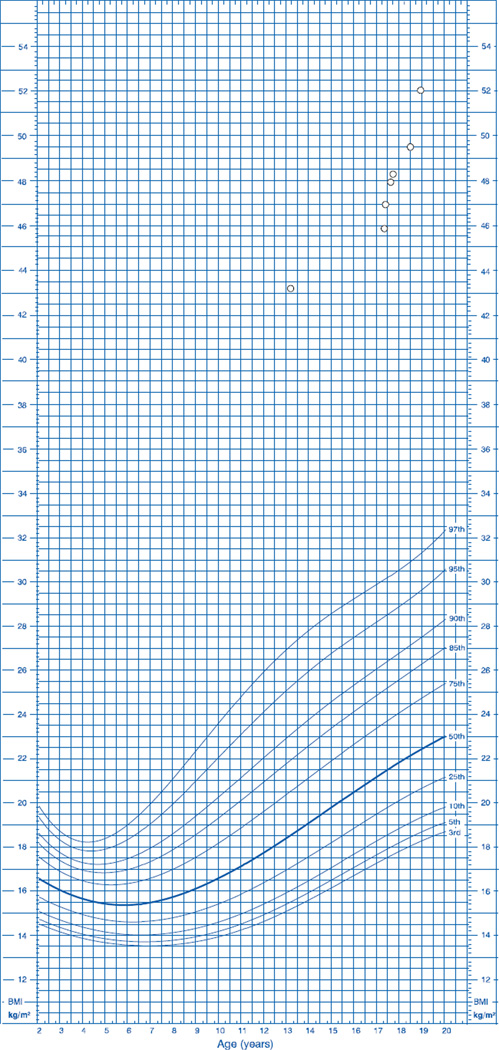
Figure 3.
Growth charts for the affected individuals (proband 2150 and brother 2239) from family 466. Modified from the Center for Disease Control’s individual growth charts in 2000.
Figure 3a. Growth chart with weight-for-age percentiles for subject 2150.
Figure 3b. Growth chart with body mass index-for-age percentiles for subject 2150. Between ages 13–14, 2150 was able to lose 60 pounds under close supervision. However, following discharge, she regained all of the weight.
Figure 3c. Growth chart with body mass index-for-age percentiles for the subject 2239.
Subject 2150 is also developmentally delayed; she began speaking at age 12 months, but could not walk until age 3 years. Around age 14 she had an IQ of 75. She received mostly failing grades in mainstream grade 9 classes.
The proband’s affected brother (2239) did not have rapid weight gain until after age 2 years. At age 13 years and 3 months, he had a height of 159.6 cm (60th percentile), weight of 110 kg (BMI of 43.2 kg/m2 [99.7th percentile]), and an abdominal circumference of 127.4 cm (above 90th percentile (16)). At this age his bone age was 12 years. His circulating leptin concentration was 62.0 ng/mL, triple the average level in obese adult males (~20 ng/mL) (15). His BMI has remained consistently above the 99th percentile (Figure 3c). Acanthosis nigricans was present on the neck, inguinal folds, and axillae.
Family 475
Family 475 is from the Dominican Republic with two children (2173 and 2182) of fourth cousins (Figure 1c). The proband (2173) had a BMI of 61.0 kg/m2 (99.9th percentile) at age 11 years. At this age she lost 60 pounds, but regained all of the weight. At age 13, her fasting serum insulin (69.1 µIU/mL) and her HbA1c (6.1%) were slightly elevated, but her fasting blood glucose (87 mg/dL) was normal. Her leptin concentration at age 14 years and 5 months was 73.7 ng/mL, almost double the average level in obese females (~40 ng/mL) (15). Clinical molecular genetic tests for MC4R and POMC mutations were negative. Acanthosis nigricans was present over multiple skin regions.
Family 489
The proband (2206) from Family 489 is Jordanian and the son of related parents, but of uncertain extent of consanguinity (Figure 1d). As an infant he was hyperphagic and began gaining excessive weight at 2½ years of age. At age 7 years, he developed sleep apnea. By age 9 years, he was 135 cm tall and weighed 115 kg (BMI of 63.1 kg/m2 [99.8th percentile]). His circulating leptin concentration was 50.5 ng/mL, more than double the average level in obese males (~20 ng/mL) (15).
2206 is developmentally delayed, and started to speak at age 3. He has almond shaped eyes and small hands and feet. His karyotype was normal, and methylation and FISH results for Prader-Willi Syndrome were normal. A brain MRI and the following tests at age 9½ years were all normal: free thyroxine (T4), thyroid stimulating hormone, insulin-like growth factor 1, cortisol, and adrenocorticotropic hormone.
Filter-based analysis and homozygosity mapping of exome data
On average, we generated 16.17 Gb of exonic sequence per person from five individuals in the four consanguineous families (4 probands and 1 affected sibling). On average 60% of reads mapped to the human reference exome (hg19) with a mean coverage of over 150X. Over 92% of the targeted exons were covered by more than 15 reads for all cases sequenced.
Family 283
Subject 1511 had a total of 32,654 called SNVs, of which 1,502 were rare and non-synonymous. He also had 4,142 called indels, 295 of which were both rare and functional (frameshift, amino acid insertion or deletion, or splice site). Filter-based analysis of SNVs and indels based on pathogenicity and sequence conservation yielded 32 variants (22 SNVs and 12 indels) that were homozygous and potentially pathogenic in 1511 (Table 2).
Table 2.
Number of variants at each stage of the filtering process
| Family ID | 283 | 466 | 475 | 489 | ||||
|---|---|---|---|---|---|---|---|---|
| Subject ID | 1511 | 2150/2239 Shared |
2173 | 2206 | ||||
| Total SNVs | 32654 | 36100 | 28469 | 25777 | ||||
| Non-synonymous SNVs | 8795 | 9951 | 7747 | 7099 | ||||
| Rare SNVs | 1502 | 1536 | 929 | 691 | ||||
| Damaging SNVs | 696 | 732 | 454 | 377 | ||||
| Homozygous SNVs | 22 | 10 | 8 | 12 | ||||
| SNVs in Regions of Homozygosity | 12 (4) | 6 (2) | 3 (2) | 3 (2) | ||||
| Other Homozygous SNVs | 9 (1) | 4 (0) | 5 (0) | 9 (1) | ||||
| Total Indels | 4142 | 4702 | 3919 | 3698 | ||||
| Functional (Frameshift, AA Insertion/Deletion, Splice Site) Indels | 1086 | 1213 | 1061 | 1053 | ||||
| Rare Indels | 295 | 361 | 273 | 263 | ||||
| Homozygous Indels | 12 | 5 | 12 | 8 | ||||
| Indels in Regions of Homozygosity | 2 (1) | 3 (1) | 4 (2) | 3 (0) | ||||
| Other Homozygous Indels | 10 (0) | 2 (0) | 8 (0) | 8 (0) | ||||
| Total Confirmed Recessive SNVs and Indels | 5 | 4 | 4 | 3 | ||||
| Confirmed Recessive SNVs |
DAK p.A474V CD248 p.R42H IFI44L p.G232E MRGPRD p.R206W |
DLG1 p.V717L ZNF77 p.C144F GBP7 p.M368I |
TMEM63A p.N190H MTMR11 p.T421I |
MMP2 p.K4299N XKR9 p.F275Y ZNF696 p.R36W |
||||
| Confirmed Recessive Indels |
LEPR p.C186AfsX27 |
LEPR p.H160LfsX9 |
ACOT4 p.A189Q;Y190S |
|||||
Numbers in parentheses denote the number of damaging recessive SNVs/indels confirmed by dideoxy sequencing and segregation analysis. SNV: single nucleotide variant; indel: insertion/deletion.
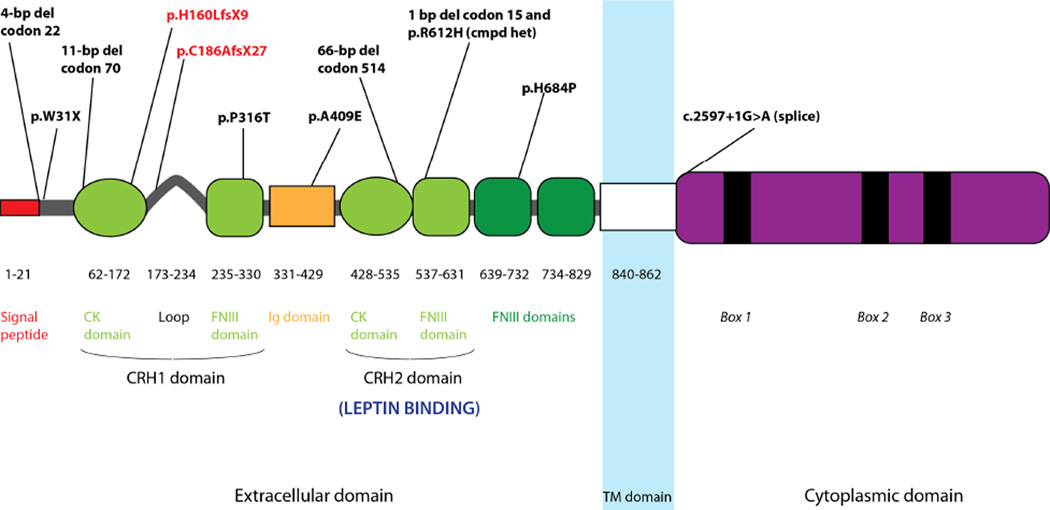
1511 inherited two copies of a p.C186AfsX27 (c.556delT) frameshift mutation in the Leptin Receptor (LEPR) gene (Supplemental Table S3). His unaffected parents were confirmed as carriers using dideoxy sequencing (Figure 1a). The mutation occurs in the loop connecting the cytokine (CK) and fibronectin type III (FIII) domains of the cytokine receptor homology 1 (CRH1) domain in LEPR and introduces a premature stop codon after insertion of 27 novel amino acids (Figure 4).
Figure 4.
Schematic of pathogenic LEPR mutations. Novel mutations identified in families 283 and 466 are denoted by red bolded text. Mutations were identified from the Human Gene Mutation Database (32) and Farooqi et al. (29).
1511 had 22 additional rare homozygous SNVs, including 12 in regions of homozygosity (Table 2). Of the 5 SNVs with composite pathogenicity scores above 5, all but two, in DAK (Dihydroxyacetone Kinase 2 Homolog) and CD248 (CD248 molecule, endosialin), had consistently poor sequence conservation and/or pathogenicity scores, or minor allele frequency above 1% in Africans in the EVS database (Supplemental Tables S1 and S2). Both variants were considered “tolerated” with SIFT scores of 0.09 and 0.08, respectively, and therefore likely benign.
In addition to the LEPR frameshift mutation, 1511 had 11 rare homozygous indels, including one in a region of homozygosity. However, all were found to be of low read depth, were poorly conserved, or were in an Olfactory Receptor.
Family 466
In an analysis restricted to recessive variants common to both 2150 and 2239, the affected siblings had 36,100 SNVs, and 1537 were rare and non-synonymous. The affected siblings also shared 4,702 recessive indels, and 1,213 were both rare and functional (frameshift, amino acid insertion or deletion, or splice site). Further filtering by pathogenicity and conservation showed that 2150 and 2239 were both homozygous for 15 potentially damaging variants (10 SNVs and 5 indels) (Table 2).
Subjects 2150 and 2239 inherited two copies of a p.H160LfsX9 (c.479delA) frameshift mutation in LEPR (Supplemental Table S3). Results were independently confirmed by dideoxy sequencing, and both unaffected parents and an unaffected sister were confirmed to be carriers, while a second unaffected brother was homozygous for the wild type allele (Figure 1b). The mutation occurs in the CK domain of the CRH1 domain in LEPR, and introduces a premature stop codon after insertion of 9 novel amino acids (Figure 4).
2150 and 2239 also shared 10 SNVs, six of which were in regions of homozygosity (Table 2). Of the five variants with combined pathogenicity scores above 5, the variants in ZNF77 (Zinc Finger Protein 77) and GBP7 (Guanylate Binding Protein 7) and were found to have a minor allele frequency above 1% in Africans from the EVS database, one variant in VPS13C (Vacuolar Protein Sorting 13 Homolog C) was homozygous in both parents and an unaffected sibling, and a second variant in VPS13C was homozygous in all family members. The remaining c.2149G>T (p.V717L) variant in DLG1 (Discs, Large Homolog 1), annotated as rs148283553, was confirmed to segregate with obesity in the family (Supplemental Tables S1 and S2), but was predicted to be “tolerated” by SIFT.
Aside from the frameshift mutation in LEPR, 2150 and 2239 shared an additional 4 homozygous indels, including one in a region of homozygosity. Only the indel in FAM18B2 (Protein FAM18B2) was confirmed by Sanger sequencing to be homozygous in 2150 and 2239, but was also homozygous in the unaffected father 2237. Upon visual inspection the other two indels were not robust variant calls and were not confirmed.
Family 475
Subject 2173 had 28,469 called SNVs, and 7,747 were rare and non-synonymous. She also had 3,920 called indels, of which 1,062 were rare and functional (frameshift, amino acid insertion or deletion, or splice site). Filter-based analysis found that 2173 was homozygous for 8 SNVs and 12 indels that were potentially pathogenic (Table 2). We used Sanger sequencing to confirm 2 recessive SNVs and 2 indels. Within a region of homozygosity on chromosome 1, we identified a c.568A>C (p.N190H) variant in TMEM63A (Transmembrane Protein 63A) (rs115347439) and a c.1262G>A (p.T421I) variant in MTMR11 (Myotubularin Related Protein 11) (rs114842926) (Supplemental Tables S1 and S2). For both variants, dideoxy sequencing confirmed the proband's sister 2182 to be homozygous for the rare variant, and both parents to be heterozygous. 2173 was also homozygous for a complex indel: a 4 bp insertion (c.563_564insTCAA) and a 4 bp deletion (c.566_569delCTTA) separated by 2 nucleotides, resulting in two amino acid substitutions (p.A189Q;Y190S) in ACOT4 (Acyl-CoA Thioesterase 4) (Supplemental Table S3). Sister 2182 and parents 2179 and 2180 were confirmed to be heterozygous for both variants in ACOT4. The remaining SNVs and indels were not robust variant calls, and none were at strongly conserved loci. There were no obvious candidate pathogenic mutations from Family 475.
Family 489
Individual 2206 had 25,777 called SNVs, of which 7,099 were rare and non-synonymous. He also had 3,698 indels and 1,053 were functional (frameshift, amino acid insertion or deletion, or splice site). Further filtering by pathogenicity and sequence conservation resulted in 20 potentially damaging homozygous variants (12 SNVs and 8 indels) (Table 2). All three SNVs with composite pathogenicity scores above 5 were confirmed to be homozygous recessive in 2206 using dideoxy sequencing and segregation analysis: a c.1287G>T (p.K429N) variant in MMP2 (Matrix Metalloproteinase-2) (rs201083413), a c.818T>A (p.F275Y) variant in XKR9 (XK, Kell Blood Group Complex Subunit-Related Family, Member 9) (rs74941166), and a c.106C>T (p.R36W) variant in ZNF696 (Zinc Finger Protein 696) (rs140398403) (Supplemental Tables S1 and S2). In addition, 8 homozygous recessive indels were called in 2206 (Table II). Two were weakly conserved and 6 were not robust calls+. We were unable to identify a clear candidate pathogenic mutation in Family 489.
Discussion
Leptin is an adipocyte-derived hormone that regulates energy homeostasis via hypothalamic neurons expressing the leptin receptor (LEPR). Leptin circulates at concentrations proportional to fat mass (17) and both induces anorexigenic signals and inhibits orexigenic signals, leading to decreased food intake and increased energy expenditure. Leptin signaling also plays a permissive role in the initiation of puberty and subsequent maintenance of gonadal axis integrity (17, 18). LEPR belongs to the interleukin 6 family of class I cytokine receptors, which consist of extracellular ligand-binding, transmembrane, and cytoplasmic signaling domains (19). Alternative splicing generates six LEPR isoforms (LEPRa-f), which can be classified as secreted (LEPRe), short (LEPRa, LEPRc, LEPRd, and LEPRf), or long (LEPRb). All isoforms share the same extracellular domain comprised of two cytokine receptor homology domains (CRH1 and CRH2) separated by an Ig-like domain and adjacent to two fibronectin III (FNIII) domains (20). LEPRe contains only extracellular domains and is hypothesized to bind and regulate the physiology of circulating leptin (21). Leptin signaling related to energy homeostasis is mediated primarily by LEPRb (22). Leptin induces the formation of LEPRb homodimers, triggering downstream signaling via phosphorylation of Janus Kinase 2 (JAK2), recruitment of Signal Transducer and Activator of Transcription 3 (STAT3), and ultimately transcription of target genes in the nucleus. The short forms of LEPR have truncated intracellular domains, which lack the ‘Box 2’ region and STAT binding sites. However, both long and short forms of LEPR have a ‘Box 1’ motif necessary for JAK2 activation, and can initiate signaling events apart from STAT3 activation via leptin-dependent phosphorylation of JAK2 in vitro. This additional signaling capacity may allow different isoforms to perform distinct functions within contexts in which they are differentially expressed (23).
Congenital deficiency of leptin or LEPR disrupts leptin signaling in both mice and humans, leading to severe obesity, hyperphagia, altered immune function, and delayed puberty due to hypogonadotropic hypogonadism (24–26). We identified two novel p.C186AfsX27 and p.H160LfsX9 frameshift mutations that truncate the LEPR protein (Figure 4), resulting in protein products that lack the leptin binding (CRH2) domain necessary for leptin signal transduction for all LEPR isoforms. Both mutations affect the extracellular N-terminus of the LEPR protein, thereby impacting all isoforms, and are predicted to result in nonsense-mediated decay due to the introduction of a premature stop codon. In subjects 1511, 2150, and 2239 the elevated circulating leptin concentrations appear to be increased above those attributable to increased adiposity per se, although direct measurements of body fat were not made. Such elevations have been previously described in individuals with hypomorphic mutations of LEPR and have been attributed to “leptin resistance” (27). The delayed onset of puberty and secondary sex characteristics observed (Table 1) are due to hypogonadotropic hypogonadism secondary to hypothalamic unresponsiveness to leptin (25, 28). The highly deleterious nature of these frameshift mutations is also consistent with the hyperphagia, resultant rapid weight gain, and extreme obesity observed in individuals 1511, 2150, and 2239.
Both families segregating for deleterious LEPR frameshift mutations had additional potentially damaging SNVs that segregated with extreme obesity. Family 283 segregated a c.1421C>T (p.A474V) missense variant in DAK with a pathogenicity score of 9.49 as well as a c.125C>T (p.R42H) missense variant with a combined score of 7.33. In Family 466, a c.2149G>T (p.V717L) variant in DLG1 with a pathogenicity score of 7.27 segregated with extreme obesity. We do not believe that these missense variants are strong contributors to the obesity phenotype in families 283 and 466 given the strong evidence that disruptive mutations in LEPR can completely account for the obesity and gonadal axis phenotypes. However, recessive rare variants besides the LEPR mutations could account for the cognitive disabilities in 1511 and 2150.
Given the low prevalence (~3%) of pathogenic LEPR mutations in previous studies of extreme obesity in consanguineous families (29), it is perhaps surprising that half of the consanguineous families reported here have obesity attributable to LEPR mutations. However, the probands from families 283 and 466 represent the most severely affected individuals from our database of over 150 families with obesity. Our focus on families with consanguinity increased the likelihood of identifying private mutations that cause autosomal recessive forms of obesity. Both families 283 (from Guinea) and 466 (from Sudan) originate from Africa, and their source populations have distinct genetic origins (30) and independently gave rise to private ancestral LEPR mutations that are unlikely to be found in other populations.
Our findings suggest that sampling at phenotypic extremes can enrich for families with Mendelian forms of obesity, and demonstrate that WES can identify pathogenic mutations that cause severe, early onset obesity. Although the current study was focused on consanguineous families, we believe that extension of this approach to non-consanguineous families with apparently dominant and recessive inheritance of extreme obesity should lead to the identification of mutations in novel pathogenic genes (and pathways), as families with a strong history of disease are likely to be enriched for rare pathogenic alleles (31). More common variants in such genes may also contribute to the pathogenesis of less severe forms of obesity.
Supplementary Material
Acknowledgements
RG and WKC conceived the experiments.
RG carried out the experiments and analyzed the data.
YHC and YS processed the data.
RLL, WKC, PL, NMM, ST, JCH, JAY, NKM, and RM oversaw data collection.
WKC and RLL designed the study.
RG, RLL, and WKC wrote the paper.
All authors had final approval of the submitted version of the paper.
We gratefully acknowledge the contributions of the patients and their families to these studies. We thank Florence Chu for her contribution to DNA extraction and database maintenance. This work was supported by NIH DK52431-19, DK26687-31, UL1 RR024156, the Russell Berrie Foundation, and the Intramural Research Program of NICHD, NIH, Z1A-HD-00641. RG is supported by funding from CIHR DFSA-113549.
Footnotes
Conflicts of Interest
The authors report no conflicts of interest.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 3.Stunkard AJ, Foch TT, Hrubec Z. A twin study of human obesity. JAMA. 1986;256:51–54. [PubMed] [Google Scholar]
- 4.Stunkard AJ, Sorensen TI, Hanis C, et al. An adoption study of human obesity. N Engl J Med. 1986;314:193–198. doi: 10.1056/NEJM198601233140401. [DOI] [PubMed] [Google Scholar]
- 5.Speliotes EK, Willer CJ, Berndt SI, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42:937–948. doi: 10.1038/ng.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manolio TA, Collins FS, Cox NJ, et al. Finding the missing heritability of complex diseases. Nature. 2009;461:747–753. doi: 10.1038/nature08494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guey LT, Kravic J, Melander O, et al. Power in the phenotypic extremes: a simulation study of power in discovery and replication of rare variants. Genet Epidemiol. 2011 doi: 10.1002/gepi.20572. [DOI] [PubMed] [Google Scholar]
- 8.Gilissen C, Hoischen A, Brunner HG, Veltman JA. Unlocking Mendelian disease using exome sequencing. Genome biology. 2011;12:228. doi: 10.1186/gb-2011-12-9-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell CG, Walley AJ, Froguel P. The genetics of human obesity. Nat Rev Genet. 2005;6:221–234. doi: 10.1038/nrg1556. [DOI] [PubMed] [Google Scholar]
- 10.Choi M, Scholl UI, Ji W, et al. Genetic diagnosis by whole exome capture and massively parallel DNA sequencing. Proc Natl Acad Sci U S A. 2009;106:19096–19101. doi: 10.1073/pnas.0910672106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seelow D, Schuelke M, Hildebrandt F, Nurnberg P. HomozygosityMapper--an interactive approach to homozygosity mapping. Nucleic Acids Res. 2009;37:W593–W599. doi: 10.1093/nar/gkp369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DePristo MA, Banks E, Poplin R, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nature genetics. 2011;43:491–498. doi: 10.1038/ng.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenna A, Hanna M, Banks E, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome research. 2010;20:1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sinha VK, Vaarties K, De Buck SS, et al. Towards a better prediction of peak concentration, volume of distribution and half-life after oral drug administration in man, using allometry. Clin Pharmacokinet. 2011;50:307–318. doi: 10.2165/11539250-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Van Gaal LF, Wauters MA, Mertens IL, Considine RV, De Leeuw IH. Clinical endocrinology of human leptin. Int J Obes Relat Metab Disord. 1999;23(Suppl 1):29–36. doi: 10.1038/sj.ijo.0800792. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum M, Nicolson M, Hirsch J, et al. Effects of gender, body composition, and menopause on plasma concentrations of leptin. The Journal of clinical endocrinology and metabolism. 1996;81:3424–3427. doi: 10.1210/jcem.81.9.8784109. [DOI] [PubMed] [Google Scholar]
- 18.Rosenbaum M, Leibel RL. Leptin: a molecule integrating somatic energy stores, energy expenditure and fertility. Trends Endocrinol Metab. 1998;9:117–124. doi: 10.1016/s1043-2760(98)00028-9. [DOI] [PubMed] [Google Scholar]
- 19.Tartaglia LA. The leptin receptor. The Journal of biological chemistry. 1997;272:6093–6096. doi: 10.1074/jbc.272.10.6093. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz MW, Woods SC, Porte D, Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 21.Ge H, Huang L, Pourbahrami T, Li C. Generation of soluble leptin receptor by ectodomain shedding of membrane-spanning receptors in vitro and in vivo. The Journal of biological chemistry. 2002;277:45898–45903. doi: 10.1074/jbc.M205825200. [DOI] [PubMed] [Google Scholar]
- 22.Bates SH, Myers MG., Jr The role of leptin receptor signaling in feeding and neuroendocrine function. Trends Endocrinol Metab. 2003;14:447–452. doi: 10.1016/j.tem.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Bjorbaek C, Uotani S, da Silva B, Flier JS. Divergent signaling capacities of the long and short isoforms of the leptin receptor. The Journal of biological chemistry. 1997;272:32686–32695. doi: 10.1074/jbc.272.51.32686. [DOI] [PubMed] [Google Scholar]
- 24.Montague CT, Farooqi IS, Whitehead JP, et al. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387:903–908. doi: 10.1038/43185. [DOI] [PubMed] [Google Scholar]
- 25.Clement K, Vaisse C, Lahlou N, et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature. 1998;392:398–401. doi: 10.1038/32911. [DOI] [PubMed] [Google Scholar]
- 26.Strobel A, Issad T, Camoin L, Ozata M, Strosberg AD. A leptin missense mutation associated with hypogonadism and morbid obesity. Nat Genet. 1998;18:213–215. doi: 10.1038/ng0398-213. [DOI] [PubMed] [Google Scholar]
- 27.Farooqi IS, Jebb SA, Langmack G, et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. The New England journal of medicine. 1999;341:879–884. doi: 10.1056/NEJM199909163411204. [DOI] [PubMed] [Google Scholar]
- 28.Lahlou N, Clement K, Carel JC, et al. Soluble leptin receptor in serum of subjects with complete resistance to leptin: relation to fat mass. Diabetes. 2000;49:1347–1352. doi: 10.2337/diabetes.49.8.1347. [DOI] [PubMed] [Google Scholar]
- 29.Farooqi IS, Wangensteen T, Collins S, et al. Clinical and molecular genetic spectrum of congenital deficiency of the leptin receptor. The New England journal of medicine. 2007;356:237–247. doi: 10.1056/NEJMoa063988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tishkoff SA, Reed FA, Friedlaender FR, et al. The genetic structure and history of Africans and African Americans. Science. 2009;324:1035–1044. doi: 10.1126/science.1172257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng B, Li B, Han Y, Amos CI. Power analysis for case-control association studies of samples with known family histories. Hum Genet. 2010;127:699–704. doi: 10.1007/s00439-010-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenson PD, Ball EV, Mort M, et al. Human Gene Mutation Database (HGMD): 2003 update. Hum Mutat. 2003;21:577–581. doi: 10.1002/humu.10212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.