Abstract
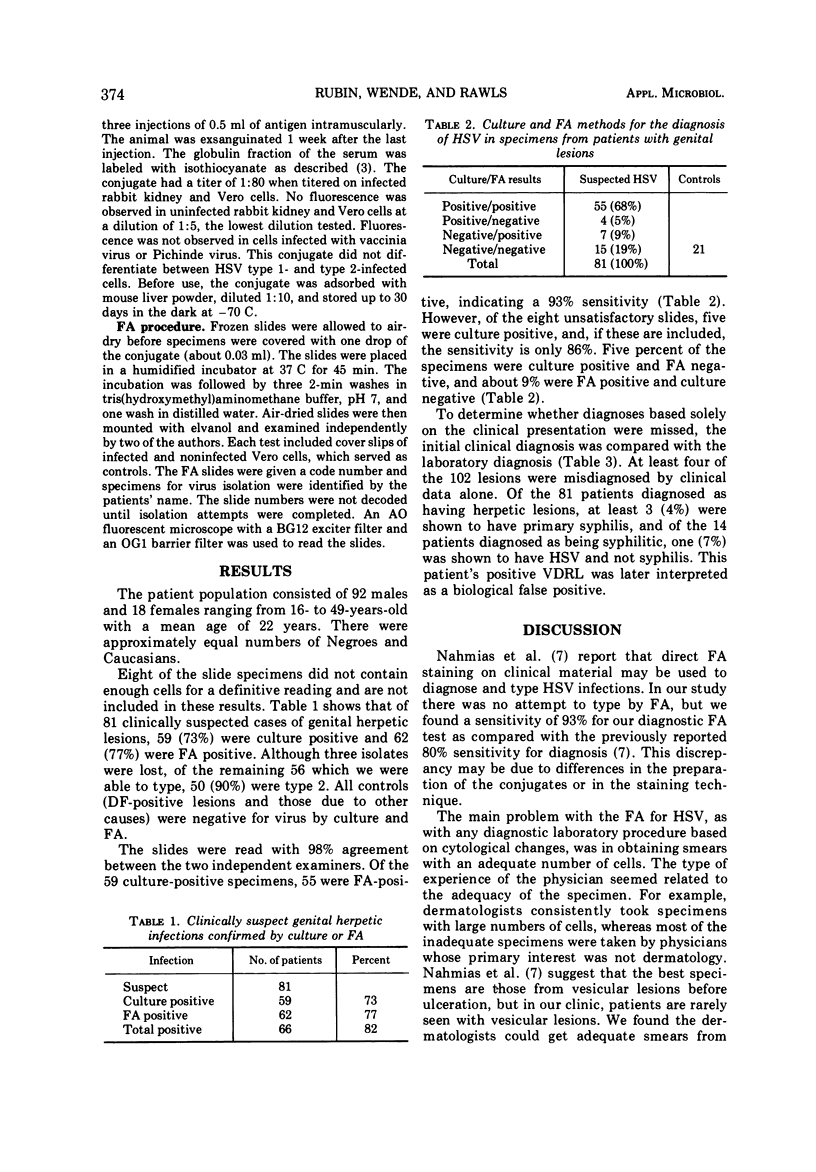
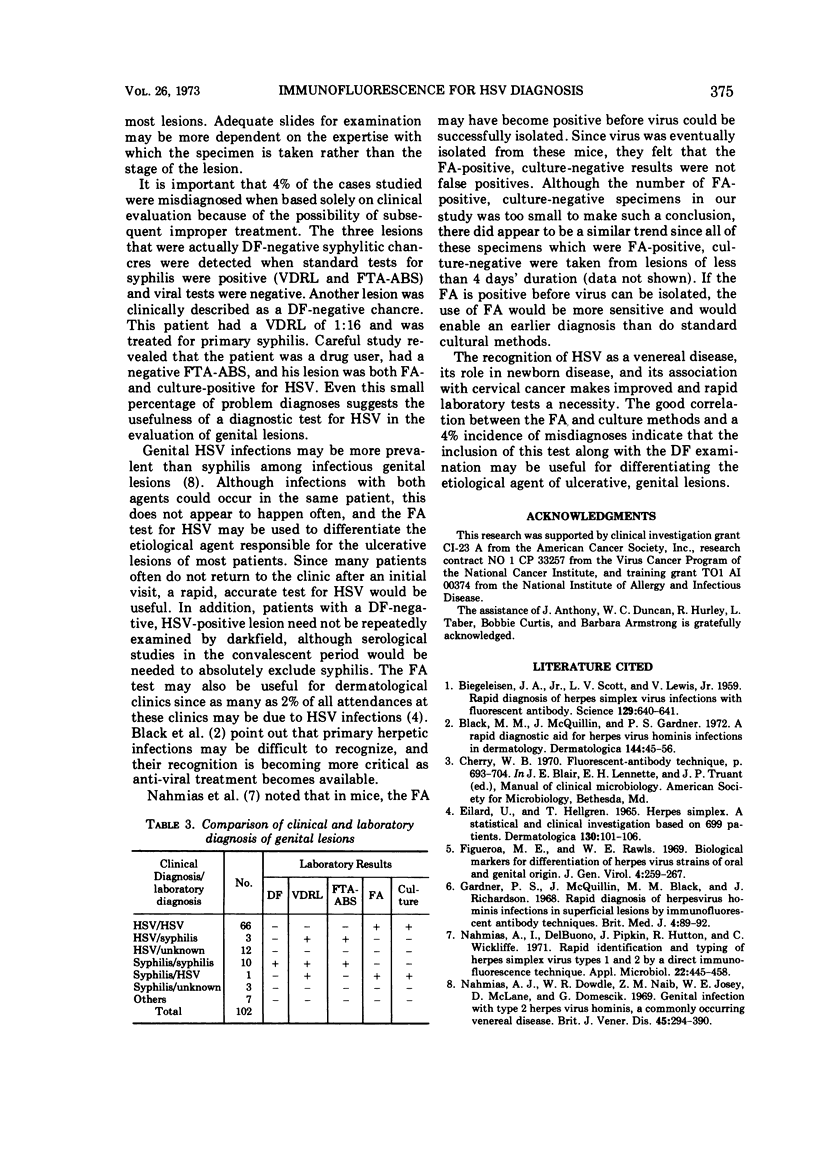
Herpetic lesions of the genitalia may be confused clinically with other ulcerative, genital lesions. Direct immunofluorescence (FA) provides a rapid method of diagnosis, and the utility of this method for the diagnosis of genital ulcers was examined. One hundred and ten patients with genital lesions were examined by darkfield for syphilis and by FA and culture for herpes simplex virus (HSV) infections. Satisfactory samples were obtained from 102 patients, of which 81 were clinically suspected cases of HSV. Acetone-fixed slides of scrapings of ulcerative lesions were stained with conjugated antiserum prepared in rabbits against HSV type 2. HSV was isolated from 73% of specimens of suspected herpetic lesions, and 77% of these specimens were positive by FA. Nine percent were positive by FA only and these were not thought to represent false positives. Five percent were positive by culture only. A comparison of clinical diagnoses with laboratory findings revealed that 4% of the cases were misdiagnosed when only the clinical evaluation was considered. The data suggest that the inclusion of a diagnostic FA test for HSV along with the darkfield examination may be useful for differentiating the etiological agents of ulcerative, genital lesions.
Full text
PDF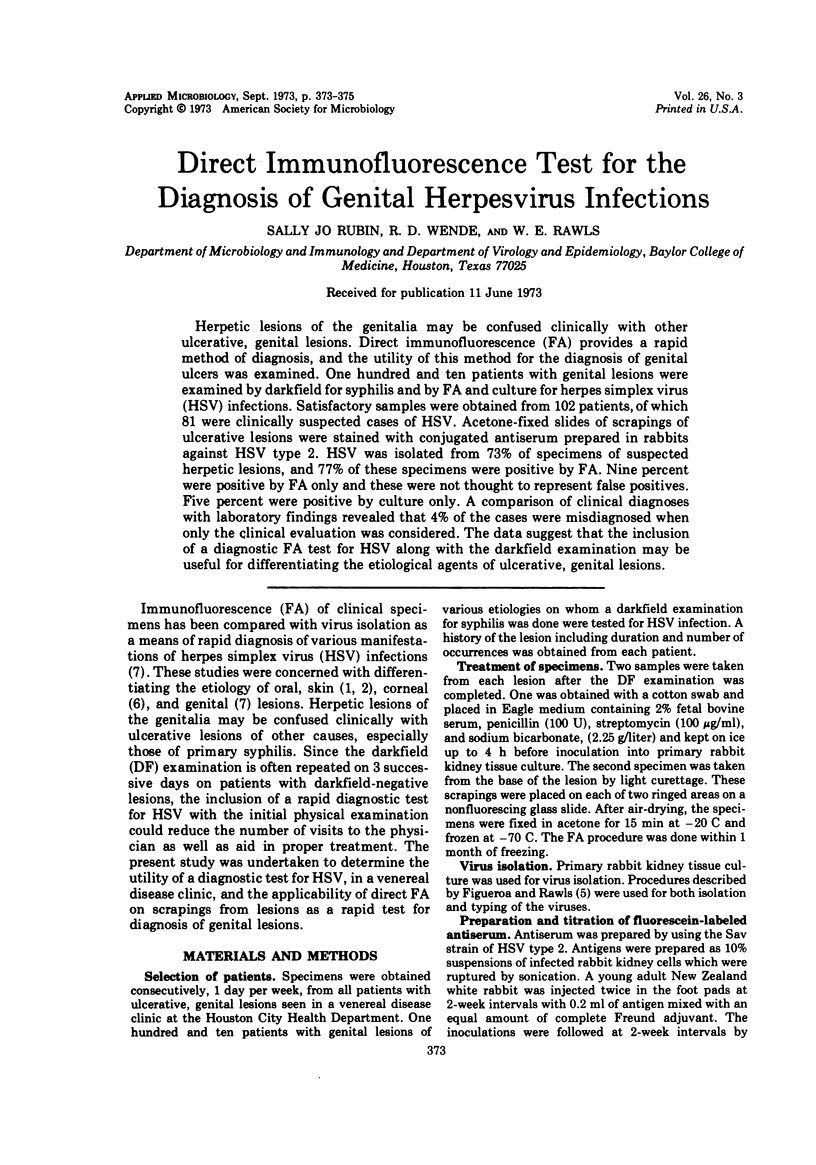
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BIEGELEISEN J. Z., Jr, SCOTT L. V., LEWIS V., Jr Rapid diagnosis of herpes simplex virus infections with fluorescent antibody. Science. 1959 Mar 6;129(3349):640–641. doi: 10.1126/science.129.3349.640. [DOI] [PubMed] [Google Scholar]
- Black M. M., McQuillin J., Gardner P. S. A rapid diagnostic aid for herpesvirus hominis infections in dermatology. Dermatologica. 1972;144(1):45–56. doi: 10.1159/000252095. [DOI] [PubMed] [Google Scholar]
- EILARD U., HELLGREN L. HERPES SIMPLEX. A STATISTICAL AND CLINICAL INVESTIGATION BASED ON 669 PATIENTS. Dermatologica. 1965;130:101–106. [PubMed] [Google Scholar]
- Figueroa M. E., Rawls W. E. Biological markers for differentiation of herpes-virus strains of oral and genital origin. J Gen Virol. 1969 Mar;4(2):259–267. doi: 10.1099/0022-1317-4-2-259. [DOI] [PubMed] [Google Scholar]
- Gardner P. S., McQuillin J., Black M. M., Richardson J. Rapid diagnosis of herpesvirus hominis infections in superficial lesions by immunofluorescent antibody technics. Br Med J. 1968 Oct 12;4(5623):89–92. doi: 10.1136/bmj.4.5623.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahmias A. J., Dowdle W. R., Naib Z. M., Josey W. E., McLone D., Domescik G. Genital infection with type 2 Herpes virus hominis. A commonly occurring venereal disease. Br J Vener Dis. 1969 Dec;45(4):294–298. doi: 10.1136/sti.45.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahmias A., DelBuono I., Pipkin J., Hutton R., Wickliffe C. Rapid identification and typing of herpes simplex virus types 1 and 2 by a direct immunofluorescence technique. Appl Microbiol. 1971 Sep;22(3):455–458. doi: 10.1128/am.22.3.455-458.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]


