Abstract
BACKGROUND
Most traumatic brain injuries among older persons in the U.S. are attributed to falls. Efforts to prevent falls may also plausibly reduce the incidence of TBIs and resultant costs.
OBJECTIVES
To evaluate the association between the treatment or usual care region of the Connecticut Collaboration for Fall Prevention (CCFP), a clinical intervention for prevention of falls, and the rate of hospitalization for fall-related traumatic brain injury (FR-TBI) among persons ≥ 70 years. The Medicare charges of FR-TBI hospitalizations are also described.
DESIGN
Using a quasi-experimental design, rates of hospitalization for FR-TBI were recorded over an eight year period (2000–2007) in two distinct geographic regions (treatment and usual care) chosen for their similarity in characteristics associated with occurrence of falls.
SETTING/PARTICIPANTS
Over 200,000 persons, 70 years and older, residing in two geographical regions in Connecticut.
INTERVENTION
Clinicians in the treatment region translated research protocols from Yale FICSIT, a successful fall prevention randomized clinical trial, into discipline- and site-specific fall prevention procedures for integration into their clinical practices.
MEASUREMENTS
The rate of hospitalization for fall-related traumatic brain injury among persons 70 years and older
RESULTS
Relative to the usual care region, CCFP’s treatment region exhibited lower rates of hospitalization for FR-TBI; RR= 0.84 with 95% credible interval (0.72 – 0.99).
CONCLUSION
The significantly lower rate of hospitalization for FR-TBI in CCFP’s treatment region suggests that the engagement of practicing clinicians in the implementation of evidence-based fall-prevention practices may reduce hospitalizations for FR-TBI.
Keywords: Connecticut Collaboration for Fall Prevention, fall-related traumatic brain injury, hospitalization, Bayesian, spatial model
INTRODUCTION
Relative to other age groups, adults aged 75 years and older have the highest incidence of hospitalization for traumatic brain injury (TBI).1,2 Although there is a paucity of information regarding prevention of TBI among older persons, 3 it is generally acknowledged that falls are responsible for most TBI among older persons. 4,5 For this reason fall prevention may offer a viable option for averting some proportion of these expensive and potentially life-altering injuries in the burgeoning geriatric population.
Many randomized controlled trials have demonstrated the efficacy of various fall-prevention efforts among older persons.6,7 One of these, the Yale FICSIT trial8, reduced falls among older adults by 30% among community dwelling older adults. It was followed by a successful translational fall prevention dissemination and implementation effort, that was carried out in a defined region of CT. 9
In this article we report the association between the treatment region (TR) or usual care region (UCR) and the rate of hospitalization for fall related traumatic brain injury (FR-TBI) among persons of age ≥ 70 years. Secondary objectives were the reporting of related Medicare charges for both study regions and the frequency distribution of the aggregated diagnoses documenting these hospitalizations.
METHODS
Study Design
The Connecticut Collaboration for Fall Prevention (CCFP) used a non-randomized quasi-experimental design to compare the rates of emergency room and hospital services for fall related injury among community-dwelling persons age 70 and older in two geographically distinct regions of CT.10 Previous CCFP reports detail efforts in the treatment region (TR) to embed evidence-based fall prevention screenings and interventions into clinical practice in emergency departments, home care agencies 11 primary care practices,12 rehabilitation facilities,13 and senior centers.14 Briefly, workgroups comprised of rehabilitation therapists, nurses, physicians, and pharmacists were tasked with translating research protocols into site-and discipline-specific assessment and intervention protocols and integrating them into their practices.15 The interventions targeted impairments in balance, gait, transfers, medications, postural hypotension, sensory deficits, and environmental hazards, including unsafe use of footwear or assistive devices.16
To evaluate the effectiveness of CCFP, the TR was compared with a matched usual care region (UCR). Obtaining individual informed consent was not feasible in this community-based intervention. Therefore zip code tabulation regions (ZCTAs), i.e., bounded regions corresponding to zip codes, were defined to comprise the TR and UCR. Each study region consisted of groupings of ZCTAs based on participating hospital catchment areas. There was no known contamination between the regions, either from formally networked health systems or otherwise, that might have influenced the uptake of the intervention. Selected aggregate characteristics of the two regions were compared with a chi-square test. These characteristics included proportional makeup by gender, education, race/ethnicity, income, medical resources, and living in an institution. The TR consisted of 58 ZCTAs in the greater Hartford region while the UCR was a discontinuous stretch of 53 ZCTAs along the southern coastline.9 As has been described elsewhere,15 data were collected over eight years; 2 years of pre-intervention, 3 years of intervention, and 3 years of evaluation. The CCFP study was approved by the Human Investigation Committee at the Yale University School of Medicine, and dissemination activities are ongoing.15 In comparing the outcome rates of the TR relative to the UCR, and temporally referencing the evaluation period to the intervention period, the following adjusted rate ratios (RR) and 95% Bayesian credible intervals were reported: emergency department and hospital admissions for serious fall-related injury RR=0.91 (0.88–0.94) and fall-related injury RR=0.89 (0.86–0.92).9
This article documents a secondary analysis of the CCFP data that is restricted to hospitalizations resulting from fall-related traumatic brain injury (FR-TBI) and includes annual Medicare charges for FR-TBI hospitalizations.
Outcome Data
Hospital related outcome data were obtained from the Connecticut Health Information Management (CHIME) database, 17 managed by the Connecticut Hospital Association (CHA),18 and indexed by E-codes from the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). 19 CHIME is the most comprehensive hospital database in Connecticut, with over 31 million patient encounters. Outcome data regarding discharge diagnoses and hospital charges were obtained for the 14 acute care hospitals in the TR and UCR. These data were believed to be representative of the state FR-TBI data in that they include both of CT’s Level 1 trauma centers and seven of the 13 state trauma centers. Because residential street addresses are confidential, CHIME ensured that hospital data were provided only for residential zip codes corresponding to ZCTAs in the TR and UCR. Hospitalization for fall-related TBI was defined as any assigned a fall-related E-code by CHIME (817, 824, 880–888, or 927) and at least one of the following ICD-9-CM codes specific to TBI (800 – 801, 803–804, 850–854, or 959.01). These ICD-9-CM codes are the same used by members of the Traumatic Brain Injury Surveillance Working Group of the Centers for Disease Control and Prevention (CDC).20
Population Data
The study population consisted of all persons 70 years and older residing within the treatment or usual care geographic regions. Data were obtained from Medicare denominator files 21 and all charges are reported in U.S. dollars from 2007. The covariate data for each ZCTA are for persons 65 years or older and were obtained from the weighted 2000 U.S. Census Sample Tables,22 in which the closest cutoff to 70 years or older was 65 years or older.
Statistical Analysis
The observed, annual rates of hospitalization for FR-TBI in each study region were plotted across the eight year period. Because the analytical units are bounded areas (ZCTAs) rather than persons, the association between the CCFP intervention and rate of hospitalization for FR-TBI was evaluated with a spatial model. A spatial model adjusts for spatial correlation between neighboring ZCTAs because those adjacent to each other tend to be more similar than those further away. A spatial model is also adjusted for characteristics that are aggregate of the entire ZCTA and which are obtained from U.S. census data. This spatial analysis used a Bayesian Poisson model that included ZCTA-specific random effects for spatial and non-spatial correlation, adjustment for study period (evaluation versus intervention), an interaction between treatment type and study period, time in years, and covariates. The covariates included ZCTA-based proportional estimates of the following characteristics among residents ≥ 65 years of age: nonwhite race, institutional residents, community-residing with disability, income < $15,000, and income > $75,000. Finally, the model included the following ZCTA-based adjustments for the important confounders of age and sex: proportion of males ≥ 65 years of age and proportion of persons of age ≥ 80 years in the population ≥ 65 years of age. The evaluation model included two levels of comparison. The first was geographic, i.e., the TR relative to the UCR, whereas the second was temporal, i.e., evaluation period relative to intervention period. We used WinBUGS Version 1.4 and statistical significance was interpreted as a 95% credible interval for a risk ratio that excluded zero.23 Length of stay and Medicare charges (in 2007 U.S. dollars) were tabulated by year. The ICD-9-CM codes used to define FR-TBI were also aggregated over the 8 years and examined for relative frequency.
RESULTS
The demographic characteristics of the study regions are presented as the mean proportion across the ZCTAs within each study region (Table 1) and are similar for both regions with few exceptions. The proportion of black residents in the UCR is significantly higher whereas the TR has a significantly higher proportion of residents living in institutions, emphasizing the need to adjust for these covariates in the evaluation model.
Table 1.
Baseline Aggregate Characteristics of the Treatment and Usual Care Regions in the Connecticut Collaboration for Fall Prevention (2000 – 2007)
| Population Characteristics a | Treatment Region (53 ZCTAs) N = 95,433 persons age ≥ 70 years |
Usual Care Region (58 ZCTAs) N = 109,413 age ≥ 70 years |
|---|---|---|
| Percent of Regional Population | ||
| Female | 61.3 | 61.4 |
| Race | ||
| White | 91.8 | 92.3 |
| Blackb | 5.2 | 5.8 |
| Other | 2.5 | 2.4 |
| Hispanic or Latino | 2.2 | 2.2 |
| Education level c | ||
| High school graduate or less | 66.9 | 63.8 |
| Some college or more | 33.1 | 36.2 |
| Annual Household income c | ||
| <$15,000 | 23.3 | 22.9 |
| >$75,000 | 14.3 | 18.2 |
| Below Poverty Level | 7.6 | 7.2 |
| Living in an institutionb,c | 7.4 | 5.3 |
| Non-institutionalized persons with physical disability† | 24.0 | 24.0 |
| Data on Hospitals and Emergency departments d | ||
| Number of hospitals (number of beds) | 7 (2303) | 7 (2505) |
| Mean number of beds/hospital | 329 | 358 |
| Total adult discharges, 2003 | 70,084 | 77,230 |
| Mean number of discharges/hospital | 10,012 | 11,033 |
| Total adult ED visits, 2000 | 351,515 | 356,847 |
| Mean number of ED visits/hospital | 50,216 | 50,978 |
ZCTA = zip code tabulation area
Population data were obtained from the 2000 U.S. Census. Unless stated otherwise, the data refer to the persons who were 70 years of age or older
Values are significantly different for P-value ≤ 0.05 based on a chi-square test
Data are for persons 65 years of age or older and were obtained from the weighted 2000 Census Sample Tables, in which the closest age cutoff to 70 years or older was 65 years or older
Hospital and emergency department data and counts of fall-related healthcare utilization are from CHIME (Connecticut Health Information Management database)
The observed rates of hospitalization for FR-TBI in each of the study regions over the eight year period, which account for the number of admissions as well as the population at risk, are similar and fairly static in the first five years when the intervention was being developed and implemented (Figure 1). Although rates subsequently rise in both regions during the three year evaluation period, rates in the UCR rise more quickly.
Figure 1.
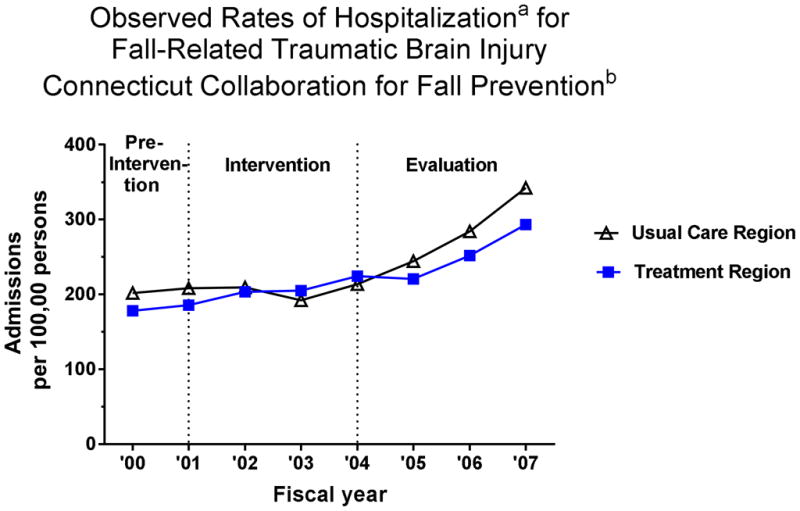
Observed Annual Rates of Hospitalization per 100,000 Persons by Study Region for Fall Related Traumatic Brain Injury a in the Connecticut Collaboration for Fall Preventionb ( 2000 –2007)
Footnotes:
a hospitalization for fall-related traumatic brain injury defined as admissions assigned a fall-related E-code by CHIME (817, 824, 880–888, or 927) and at least one of the following ICD-9-CM codes specific to traumatic brain injury (800 – 801, 803–804, 850–854, or 959.01).
b national data indicate that between 2002 and 2006 the rate of hospitalization for FR-TBI rose by 34%. Because rates adjust for population growth, this reflects an increasing trend in the occurrence of FR-TBI among older persons. (Faul M, Xu L, Wald MM, VG C. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Centers for Disease Control and Prevention. 2010; National Center for Injury Prevention and Control 43.)
As calculated from the Bayesian Poisson model, the rate ratio (RR) and 95% credible interval for the CCFP treatment region were RR = 0.84 (0.72 – 0.99).
Because our model evaluated only the rate of hospitalization for FR-TBI, it did not incorporate information from the hospital stays in each region. In Table 2 several important characteristics of the hospital stays in each study region are presented for the eight year period. These include median length of stay (LOS) in days, median charges per day and per hospital stay, and total charges from all hospital stays attributed to FR-TBI. All charges were filed to Medicare and are reported in U.S. dollars from 2007. While it is beyond the scope of this brief report to analyze the regional differences of the hospital stays, this table provides broad estimates of the expenditures related to FR-TBI hospitalizations among older persons in CT (Table 2). The UCR consistently exhibits a higher number of admissions, due in part to its larger population. Rows 3 and 4 present a median LOS that is longitudinally stable in both regions with stays in the UCR that are typically one day longer. The median charges per day in the UCR are higher except for FY07 when charges in the TR increased abruptly. The median charge per stay in the UCR is higher, reflecting its longer LOS and typically greater cost per day. Overall charges for all hospital stays attributed to FR-TBI are substantially higher in the UCR than in the TR.
Table 2.
Characteristics of Hospital Admissions for Fall Related Traumatic Brain Injury (FR-TBI) in the Connecticut Collaboration for Fall Prevention (2000 – 2007)
| Characteristics of Hospitalizations for FR-TBI | Pre-Intervention | Intervention | Evaluation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| FY00 | FY01 | FY02 | FY03 | FY04 | FY05 | FY06 | FY07 | ||
| Number of Admissions | UCR | 214 | 227 | 227 | 208 | 230 | 262 | 302 | 363 |
| TR | 166 | 175 | 191 | 193 | 210 | 205 | 232 | 269 | |
| Median Length of Stay (Days) | UCR | 6 | 5 | 5 | 5 | 5 | 5 | 4 | 5 |
| TR | 5 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | |
| Median Charge per Day (USD) a | UCR | 2,822 | 2903 | 3,717 | 4,077 | 3,924 | 4,650 | 4,997 | 5,273 |
| TR | 2,513 | 2,667 | 2,863 | 3,002 | 3,475 | 3,775 | 4,505 | 5,644 | |
| Median Charge per Stay (USD) a | UCR | 16,832 | 14,824 | 16,642 | 18,485 | 17,188 | 18,655 | 21,027 | 24,046 |
| TR | 10,349 | 11,215 | 11,704 | 12,743 | 13,276 | 16,497 | 18,495 | 21,166 | |
| Total Charges for All Stays in Millions (USD) a | UCR | 6.34 | 6.24 | 6.18 | 6.40 | 6.60 | 8.85 | 10.08 | 14.83 |
| TR | 2.85 | 3.50 | 3.29 | 3.78 | 4.56 | 5.09 | 7.04 | 8.89 | |
FR-TBI = fall-related traumatic brain injury
FY00 = fiscal year 2000 where fiscal year runs from October of calendar year 1999 through September of 2000
UCR = usual care region
TR = treatment region
2007 U.S. Dollars
The last results reported describe the frequency distribution of the ICD-9-CM codes aggregated by region over the eight years. For the UCR, the most frequent ICD-9-CM code reported for FR-TBI over the eight years was code 852 (intracranial hemorrhage; subarachnoid, subdural, and extradural) accounting for 45.5% of admissions. Other codes were: 851 (cerebral laceration and contusion); 959.01 (head injury not otherwise specified); 850 (concussion); 801 (fracture of base of skull); and 853 (other and unspecified intracranial hemorrhage). These codes accounted for 13.2%, 11.5%, 9.2%, 8.5%, and 8.1% respectively, totaling 96% of all FR-TBI codes. Similarly in the TR, code 852 accounted for 44.9% of all FR-TBI codes and the other codes, listed in the same order as for the UCR, accounted for the following percentages: 14.6%, 10.6%, 10.5%, 7.6%, and 8.2%, respectively. As observed above for the UCR, these codes accounted for a total of 96% of all FR-TBI codes in the TR.
DISCUSSION
The significantly lower rate of hospitalization for FR-TBI in CCFP’s treatment region suggests that the engagement of practicing clinicians in the implementation of evidence-based fall-prevention practices may reduce hospitalizations for FR-TBI. The rates of hospitalization for FR-TBI were similar in both study regions prior to the evaluation period (Figure 1), at which time rates rose in both regions, with the UCR outpacing the TR. No specific explanation has been uncovered for this temporal change in rates in both regions of Connecticut. However national data indicate that between 2002 and 2006 the rate of hospitalization for FR-TBI rose by 34%.24 Between 2002 and 2006, the number of admissions in our reference group (UCR) rose by 33%, closely reflecting the national trend.
The compelling public health challenge is to identify the driving force behind the rising rate and health care expenditures for hospitalization for FR-TBI among older persons. A recent study from Australia concluded that the increase in national rates of TBI (8% per year over 13 years) was due to an increase in the number of adults living beyond age 85 and a higher rate of falls among this age group.5 They further noted that falls among this age group increasingly result in the serious injury of intra-cranial hemorrhage.5 To explore the plausibility of this hypothetical explanation, we examined the U.S. census data for CT from 2000 and 2010. These data revealed the state’s population of age ≥ 85 years had grown by 32.1%. This rate of growth contrasted sharply with that of the state population of age ≥ 65 years, which only grew by 7.7%.25 Other studies speculate whether the widespread use of anti-coagulant therapies among older persons raises the risk of intracranial hemorrhage among those who do fall.3,26,27 The Australian study posits that, given the high incidence of FR-TBI among the oldest old, risk-benefit analysis of anti-coagulant therapy is warranted. 5 Consistent with the conjecture of the Australian investigators, the CCFP data showed that ICD-9-CM codes for intracranial hemorrhage accounted for more than half of all codes reported over the study period.
There are several limitations to our study that warrant mention. Because of the small number of FR-TBI outcome events, we were not able to stratify the analysis on age and sex as was done in earlier analyses of CCFP outcomes.28 We subsequently used ZCTA-based measures representing the proportions of persons of age ≥ 80 years and of males to adjust for the two confounding factors of age and sex. The other ZCTA-specific covariates provided similar, limited adjustment for the outcome and, owing to limitations of census data, do not adjust for comorbidity, functional impairment, or impairments of vision or hearing. Because CCFP is based on a non-randomized design, the authors make no claims of causality.
There are, however, two reasons why CCFP may have accounted for the observed change in rates during the evaluation period. First, we could identify no secular trends that might account for the observed differences. Second, the divergence in rates transpired, as would be expected, during the evaluation period. This divergence in rates suggests that clinical interventions designed to prevent falls among older persons may prevent some FR-TBI events. The 632 FR-TBI admissions to the 14 participating CT hospitals in 2007 potentially cost the Medicare program $23 million for acute care only. Acute care is only the first stage of caring for an older adult who sustains a TBI. Additional costs are incurred from rehabilitation and long term care. To prevent suffering and reduce healthcare costs, it is essential to examine every potential means of prevention.
Acknowledgments
Funding
Supported by a grant from the Aging Services Division of the State of Connecticut Department of Social Services to the Connecticut Collaboration for Fall Prevention (CCFP) at Yale University School of Medicine (PI – Baker) and by a grant from the National Institute on Aging (1R21AG033130-01A2, PI-Murphy). The views and opinions expressed are those of the authors. The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342, PI-Tinetti). The original CCFP efforts were supported by the Donaghue Medical Research Foundation (DF#00-206, PIs-Tinetti and Baker). This publication was also made possible in part by CTSA Grant Number UL1 RR024139 (PI-Murphy) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical research. Its contents are solely the views and opinions of the authors and not those of the CT Department of Social Services, the State of Connecticut, the NCRR or the NIH.
Sponsor’s Role: The funding agencies had no role in the conduct of the research.
Footnotes
Author Contributions: Study concept and design: DIB, HGA, MET. Acquisition of participants or data: DIB, LSL Analysis and Interpretation of Data: TEM, DIB, HGA, MET. Preparation of the manuscript: TEM, DIB, LSL, HGA, MET.
Conflicts of Interest: The authors have no conflicts relevant to this research. Supported by a grant from the Aging Services Division of the State of Connecticut Department of Social Services to the Connecticut Collaboration for Fall Prevention (CCFP) at Yale University School of Medicine (PI – Baker) and by a grant from the National Institute on Aging (1R21AG033130-01A2, PI-Murphy). The views and opinions expressed are those of the authors. The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342, PI-Tinetti). The original CCFP efforts were supported by the Donaghue Medical Research Foundation (DF#00-206, PIs-Tinetti and Baker). This publication was also made possible in part by CTSA Grant Number UL1 RR024139 (PI-Murphy) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical research. Its contents are solely the views and opinions of the authors and not those of the CT Department of Social Services, the State of Connecticut, the NCRR or the NIH.
References
- 1.Centers for Disease Control and Prevention. Incidence rates of hospitalization related to traumatic brain injury --- 12 states, 2002. MMWR. 2006;55:201–204. [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Thompson HK, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54:1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruns J, Hauser WA. The epidemiology of taumatic brain injury: A review. Epilepsia. 2003;44(Suppl 10):2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 5.Harvey LA, Close JCT. Traumatic brain injury in older adults: Characteristics, causes and consequences. Injury. 2012:1–6. doi: 10.1016/j.injury.2012.07.188. In Press. [DOI] [PubMed] [Google Scholar]
- 6.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60A:187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 7.Liu-Ambrose T, Khan KM, Eng JJ, et al. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: A 6-month randmized, controlled trial. J Am Geriatr Soc. 2004;52:657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tinetti ME, Baker DI, Garrett PA, et al. Yale FICSIT: Risk Factor abatement strategy for fall prevention. J Am Geriatr Soc. 1993;41:315–320. doi: 10.1111/j.1532-5415.1993.tb06710.x. [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359:252–261. doi: 10.1056/NEJMoa0801748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy TE, Allore HG, Leo-Summers L, et al. Bayesian hierarchical modeling for a non-randomized, longitudinal fall prevention trial with spatially correlated observations. Stat Med. 2011;30:522–530. doi: 10.1002/sim.3912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortinsky RH, Iannuzzi-Sucich M, Baker DI, et al. Fall-risk assessment and management in clinical practice: Views from healthcare providers. J Am Geriatr Soc. 2004;52:1522–1526. doi: 10.1111/j.1532-5415.2004.52416.x. [DOI] [PubMed] [Google Scholar]
- 12.Chou WC, Tinetti ME, King MB, et al. Perceptions of physicians on the barriers and facilitators to integrating fall risk evaluation and management into practice. J Gen Intern Med. 2006;21:117–122. doi: 10.1111/j.1525-1497.2005.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown CJ, Gottschalk M, Van Ness PV, et al. Changes in physical therapy providers’ use of fall prevention strategies following a multicomponent behavioral change intervention. Phys Ther. 2005;85:394–403. [PubMed] [Google Scholar]
- 14.Baker DI, Gottschalk M, Bianco L. Step by step: integrating evidence-based fall risk management into senior centers. Gerontologist. 2007;47:548–554. doi: 10.1093/geront/47.4.548. [DOI] [PubMed] [Google Scholar]
- 15.Murphy TE, Baker DI, Leo-Summers L, et al. Integration of fall prevention into state policy in Connecticut. Gerontologist. 2013;53:508–515. doi: 10.1093/geront/gns122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker DI, King MB, Fortinsky RH, et al. Dissemination of an evidence-based multicomponent fall risk-assessment and management strategy throughout a geographic area. J Am Geriatr Soc. 2005;53:675–680. doi: 10.1111/j.1532-5415.2005.53218.x. [DOI] [PubMed] [Google Scholar]
- 17.CHIME. [Accessed March 5, 2013];Chime Data. 2013 www.cthosp.org/member-services/data-services/chimedata/
- 18.CHIME. [Accessed March 5, 2013];About-CHA. 2013 www.chime.org/about-cha/
- 19.National Center for Health Statistics. [Accessed October 11, 2007];Classification of diseases, functioning and disability. www.cdc.gov/nchs/icd9.htm.
- 20.Coronado VG, Thomas KE, Sattin RW, et al. The CDC traumatic brain injury surveillance system: Characteristics of persons aged 65 years and older hospitalized with a TBI. J Head Trauma Rehabil. 2005;20:215–228. doi: 10.1097/00001199-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services (CMS ) [Accessed March 5, 2013];Denominator file from CMS. www.cms.hhs.gov/Research-Statistics-Data-and-Systems/Files-for-Order/IdentifiableDataFiles/DenominatorFile.html.
- 22.US Census. [Accessed September 15, 2007];Factfinder. 2000 http/factfinder.census.gov/home/saff/main.html.
- 23.Lunn DJ, Thomas A, Best N, et al. WinBUGS - a Bayesian modelling framework: Concepts, structure, and extensibility. Stat Comp. 2000;10:325–337. [Google Scholar]
- 24.Faul M, Xu L, Wald MM, VGC . Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Centers for Disease Control and Prevention; National Center for Injury Prevention and Control; 2010. p. 43. [Google Scholar]
- 25.US Census Bureau. Census 2000 Summary File 1 and Census 2010 Summary File 1. 2010. Population 65 years and older and population 85 years and older for the United States, Regions, and states, and for Puerto Rico: 2000 and 2010. Table 2. [Google Scholar]
- 26.Cohen DB, Rinker C, Wilberger JE. Traumatic brain injury in anticoagulated patients. J Trauma. 2006;60:553–557. doi: 10.1097/01.ta.0000196542.54344.05. [DOI] [PubMed] [Google Scholar]
- 27.Lavoie A, Ratte S, Clas D, et al. Preinjury warfarin use among elderly patients with closed head injuries in a trauma center. J Trauma. 2004;56:802–807. doi: 10.1097/01.ta.0000066183.02177.af. [DOI] [PubMed] [Google Scholar]
- 28.Murphy TE, Tinetti ME, Allore HG. Hierarchical models to evaluate translational research: Connecticut collaboration for fall prevention. Contemp Clin Trials. 2008;29:343–350. doi: 10.1016/j.cct.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


