Abstract
Background
Rates of screening mammography and the number of mammography facilities have declined in the past decade. We assessed changes over time and geographic disparities in the availability of mammography services.
Methods
Using information from the US Food and Drug Administration and the US Census, county-level mammography capacity was defined as the number of mammography machines per 10,000 women age 40 and older. We examined trends in capacity between 2000 and 2010 and county characteristics associated with declines in capacity.
Results
Between 2000 and 2010, the number of mammography facilities declined 10% from 9,434 to 8,469; the number of mammography machines declined 10% from 13,100 to 11,762; and median county mammography capacity dropped almost 20% from 1.77 to 1.42 machines per 10,000 women age 40 and older. In cross-sectional analysis, counties with greater proportions of uninsured residents, less educated residents, greater population density and higher managed care penetration had lower mammography capacity. Conversely, counties with more hospital beds per 100,000 had higher capacity. High initial mammography capacity, growth in the proportion of the population age 65 and older and proportion living in poverty, and increased managed care penetration were all associated with a decrease in capacity between 2000 and 2010. Only the proportion of rural residents was associated with an increase in capacity.
Conclusions
Geographic variation in mammography capacity and declines in capacity over time are associated with demographic, socioeconomic and health care market characteristics. Maldistribution of mammography resources may explain geographic disparities in breast cancer screening rates.
BACKGROUND
Screening mammography reduces breast cancer mortality by about 15% in women age 40 and older.1-3 Although rates of screening mammography have increased substantially in the past three decades, one-quarter of US women age 40 and older report having no recent screening mammogram, and this proportion varies widely from state to state.4, 5 In addition to its use as a screening and diagnostic tool, mammography is also a fundamental part of post-treatment surveillance among breast cancer survivors. About 20% of women with a history of breast cancer do not adhere to guidelines for follow-up mammography.6-10
The availability and accessibility of mammography depend on a number of factors, including the supply and location of mammography equipment and personnel. Although prior reports suggested that overall mammography capacity in the US was large enough to meet existing needs,11, 12, it is not clear whether resources are currently distributed proportionally to the population across local areas or sufficient to meet national targets for breast cancer screening.13
In light of reported declines in rates of screening mammography and financial pressures facing many mammography facilities,14-16 it is especially critical to understand how the availability and accessibility of mammography resources affect mammography utilization and outcomes. The goals of this study were to evaluate trends in the number and distribution of mammography resources in the US and to assess the impact of socioeconomic and health care market characteristics on changes in the availability of mammography capacity.
METHODS
Data
Information on the number, location and characteristics of mammography facilities was obtained from the US Food and Drug Administration (FDA). In accordance with the Mammography Quality Standards Act (MQSA), the FDA has maintained administrative records on all certified mammography facilities in the US since 1994.17 Facilities are inspected annually, and data obtained from inspection reports include the number of mammography machines at each facility. County-level demographic, economic and health care market characteristics were obtained from the US Census Bureau, the Area Resource File, and the Centers for Medicare and Medicaid Services.
Mammography Capacity
For every county in the US (n=3,141), we estimated mammography capacity as the number of mammography machines per 10,000 women age 40 years and older. Women in this age group constitute the population eligible for annual screening mammography.18 Annual mammography capacity was estimated from 2000 through 2010, and each year's estimate included only machines at facilities whose FDA certification was effective for the entire calendar year. Age-specific estimates of the female population in each county in each year were obtained from the 2000 and 2010 Census surveys and from intercensal population estimates produced by the US Census Bureau.
County Characteristics
Mammography capacity was assessed in relation to county-level demographic, socioeconomic and health care resource characteristics (Table 1). Information obtained from the 2000 and 2010 US Census surveys included percent of the population that identified their race as Black, percent of the population age 65 and older, percent living below the federal poverty level, percent who did not graduate high school, percent living in rural areas, and population density (total population per square mile of land area). From the Area Resource File we identified the numbers of primary care physicians and radiologists per 100,000 residents in 2002 and 2010, and the number of short-term hospital beds per 100,000 in 2000 and 2008, based on information from the American Medical Association and the American Hospital Association. The percent of residents lacking health insurance was based on Small Area Health Insurance Estimates (SAHIE) produced by the US Census Bureau. Medicare managed care penetration in 2000 and 2009, reported by CMS, was used as a proxy for managed care penetration by all insurers in each county.
Table 1.
Characteristics of US counties, 2000-2010
| Characteristic | 2000 | 2010 | Change, 2000-2010 | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Proportion of county population | |||||
| Age 65 and older | 0.147 | 0.042 | 0.159 | 0.042 | 0.012 |
| Black | 0.088 | 0.145 | 0.090 | 0.146 | 0.002 |
| At or below federal poverty level | 0.142 | 0.066 | 0.168 | 0.062 | 0.026 |
| Adults without high school diploma | 0.226 | 0.088 | 0.169 | 0.074 | −0.057 |
| In rural areas | 0.599 | 0.310 | 0.586 | 0.315 | −0.013 |
| Uninsured | 0.148 | 0.050 | 0.184 | 0.058 | 0.036 |
| Medicare managed care penetration | 0.050 | 0.094 | 0.160 | 0.118 | 0.110 |
| Population density (residents per square mile) | 243 | 1,667 | 259 | 1,725 | 16 |
| Primary care physicians per 100,000 | 19.8 | 20.4 | 14.6 | 19.8 | −5.2 |
| Radiologists per 100,000 | 4.6 | 7.9 | 6.6 | 14.1 | 2.0 |
| Hospital beds per 100,000 | 340 | 433 | 307 | 425 | −33 |
N=3,141 counties
SD: standard deviation
Analysis
We evaluated the impact of demographic, socioeconomic and health care resource characteristics on mammography capacity using multivariable linear regression. In separate cross-sectional analyses we assessed the impact of these characteristics on capacity in 2000 and in 2010. In each model the dependent variable was the natural log of county mammography capacity, therefore estimated coefficients can be interpreted as the percentage difference in capacity associated with each predictor. Predictors in each model corresponded with the year in which capacity was defined. We used natural log transformations for population density and the numbers of primary care physicians, radiologists and hospital beds per population; other independent variables were already described as percentages, and therefore not log-transformed to facilitate interpretation of results.
For each county we estimated the net change in mammography capacity as the difference between capacity in 2010 and capacity in 2000. We also estimated the slope of a regression line fit through the estimates of capacity in each year for each county, and used t-tests to assess whether the estimated slope was statistically significantly different from zero at α<0.05. Based on these estimates, we classified each county as having had an increase, decrease or no change in mammography capacity during the study period.
We evaluated the impact of county characteristics on change in capacity, using the natural log of change in county mammography capacity between 2000 and 2010 as the dependent variable. By using the natural log of capacity change, the estimated coefficients for each predictor in this regression model can be interpreted as impacts on the rate of change in county mammography capacity. Predictors included county demographic characteristics defined in 2000 and the change from 2000 to 2010 in the proportions of the county population who were age 65 and older, black, lived below the poverty level, did not graduate high school, lived in rural areas, and lacked health insurance. We included log-transformed values of population density and the number of hospital beds in 2000, the number of primary care physicians and radiologists in 2002, and the changes in these four characteristics. Mammography capacity in 2000 was also included as a predictor.
RESULTS
Correlates of Capacity
In both 2000 and 2010, counties with greater proportions of uninsured residents and higher managed care penetration had fewer mammography machines per 10,000 adult women. Population density and the proportion of residents without a high school diploma were also negatively associated with mammography capacity, while the number of hospital beds per 100,000 was associated with greater capacity (Table 2). In 2000, counties with more residents living in rural areas had lower mammography capacity, while counties with a greater proportion of the population at or below poverty had higher capacity. In 2010, counties with more primary care physicians per population had lower mammography capacity, while counties with a greater proportion of residents age 65 and older had higher capacity.
Table 2.
Predictors of county-level mammography capacity
| Characteristic | 2000 | 2010 | ||
|---|---|---|---|---|
| Coefficient | p | Coefficient | p | |
| Proportion age 65+ | 0.384 | NS | 0.486 | <0.05 |
| Proportion black | −0.020 | NS | 0.054 | NS |
| Proportion at or below poverty | 1.076 | <0.0001 | 0.200 | NS |
| Proportion without high school diploma | −0.596 | 0.0003 | −0.543 | <0.01 |
| Proportion rural | −0.193 | <0.0001 | −0.033 | NS |
| Proportion uninsured | −1.121 | 0.0005 | −1.074 | <0.0001 |
| Medicare managed care penetration | −0.384 | <0.0001 | −0.432 | <0.0001 |
| Population density | −0.079 | <0.0001 | −0.090 | <0.0001 |
| Primary care physicians per 100,000 | 0.017 | NS | −0.023 | <0.05 |
| Radiologists per 100,000 | 0.010 | NS | 0.010 | NS |
| Hospital beds per 100,000 | 0.079 | <0.0001 | 0.081 | <0.0001 |
Notes:
The adjusted impact of each characteristic on county-level mammography capacity was estimated in separate multivariable linear regression models, where the dependent variable was the natural of mammography capacity in the respective year. All characteristics shown were included in each model, and county characteristics corresponded with the year in which capacity was defined. Population density and the numbers of primary care physicians, radiologists and hospital beds per population were included as log-transformed variables.
NS: not statistically significant at p<0.05.
Changes in Mammography Capacity
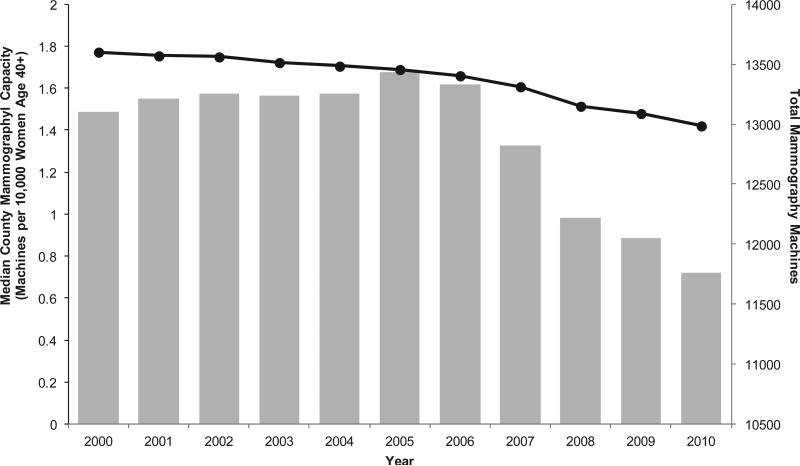
In 2000 there were 13,100 mammography machines in 9,434 FDA-certified facilities, and median county-level mammography capacity was 1.77 machines per 10,000 women age 40 and older. By 2010 there were 11,762 mammography machines in 8,469 FDA-certified facilities, and median county-level mammography capacity was 1.42 machines per 10,000 women age 40 and older. These changes represent a 10% decrease in the total number of machines, a 10% decrease in the number of facilities, and almost a 20% decrease in median capacity (Figure 1).
Figure 1. County mammography capacity and total mammography machines in the US, 2000-2010.
Black circles indicate median county-level mammography capacity; gray bars indicate total number of mammography machines in all FDA-certified mammography facilities in each year.
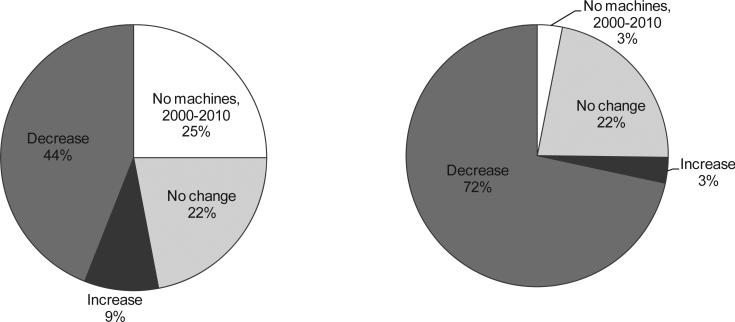
Of the 3,141 counties, 789 (25%) never had a mammography machine in any year between 2000 and 2010 (Figure 2). In an additional 686 counties that had at least one machine (22% of all counties), the regression slope for capacity over the study period was not statistically different from zero, suggesting no change in capacity during this time. In 283 counties (9%) the slope was positive and significantly different from zero, reflecting an increase in capacity, and in 1,383 counties (44%) the slope was negative and significantly different from zero, reflecting a decrease in capacity.
Figure 2. Change in mammography capacity in all US counties, 2000-2010.
The panel on the left shows the unweighted distribution of counties by change in mammography capacity over the study period. The panel on the right shows the distribution of counties by change in capacity weighted by county share of women age 40 and older. Change in capacity was estimated from the slope of a regression line for each county fit through capacity estimates in each year, 2000-2010. Counties with an increase (decrease) in capacity were defined by a positive (negative) estimated slope that was significantly different from 0 by t-test at a<0.05.
Weighted by the adult female population distribution in each county, the 44% of counties that saw decreases in mammography capacity represented almost three-quarters of all US women age 40 and older. These results were the same whether counties were weighted by their 2000 or 2010 population estimates.
Impact of County Characteristics on Changes in Capacity
We found a negative association between mammography capacity in 2000 and the change in capacity from 2000 through 2010, implying a greater rate of decrease in capacity among counties with higher initial capacity (Table 3). The proportion of residents without a high school diploma and the change between 2000 and 2010 in the proportion age 65 and older and the proportion at or below the poverty level were also negatively associated with change in capacity over that time period. The proportion living in rural areas in 2000 was positively associated with change in capacity. Both Medicare managed care penetration in 2000 and the change in penetration over the study period were negatively associated with change in capacity. Similar relationships were observed for population density and change in population density and the number of hospital beds and change in number of hospital beds.
Table 3.
Predictors of change in county-level mammography capacity, 2000-2010
| Characteristic | Coefficient | p |
|---|---|---|
| Mammography capacity, 2000 | −0.630 | <0.0001 |
| Proportion age 65+, 2000 | 0.372 | NS |
| Change in proportion age 65+ | −3.709 | <0.0001 |
| Proportion black, 2000 | −0.046 | NS |
| Change in proportion black | 0.830 | NS |
| Proportion at or below poverty, 2000 | 0.119 | NS |
| Change in proportion in poverty | −1.108 | 0.0007 |
| Proportion without high school diploma, 2000 | −0.777 | <0.0001 |
| Change in proportion without diploma | −0.185 | <0.01 |
| Proportion rural, 2000 | 0.139 | 0.0027 |
| Change in proportion rural | −0.060 | NS |
| Proportion uninsured, 2000 | −0.046 | NS |
| Change in proportion uninsured | −0.350 | NS |
| Medicare managed care penetration, 2000 | −0.273 | <0.01 |
| Change in managed care penetration | −0.161 | <0.05 |
| Population density, 2000 | −0.038 | <0.0001 |
| Change in population density | −0.557 | <0.0001 |
| Primary care physicians per 100,000, 2000 | −0.012 | NS |
| Change in primary care physicians per 100,000 | −0.002 | NS |
| Radiologists per 100,000, 2000 | −0.001 | NS |
| Change in radiologists per 100,000 | 0.007 | NS |
| Hospital beds per 100,000, 2000 | 0.040 | <0.0001 |
| Change in hospital beds per 100,000 | 0.046 | <0.0001 |
Notes:
The adjusted impact of each county characteristic on change in county mammography capacity was estimated in a linear regression model where the dependent variable was the natural log of change in capacity between 2000 and 2010. All characteristics shown here were included in the model. The estimated coefficients for each predictor in can be interpreted as impacts on the rate of change in county mammography capacity.
NS: not statistically significant at p<0.05.
DISCUSSION
Mammography remains the only recommended modality of population-based screening for breast cancer.19-21 In this analysis we observed declines in the availability of mammography facilities and machines between 2000 and 2010, as well as a decrease in county-level mammography capacity. The counties affected by significant declines in mammography capacity represented more than 70% of the female population age 40 and older.
A number of population characteristics were associated with cross-sectional variation in mammography capacity as well as changes in capacity over time. While the proportion of rural residents in 2000 was positively associated with an increase in capacity between 2000 and 2010, counties with more rural residents had lower capacity relative to other counties in each year. Our results suggest that counties whose populations had lower educational attainment, increasing poverty rates and a growing proportion of elderly residents were particularly vulnerable to declines in capacity.
One quarter of all US counties had no mammography facilities in any year. This proportion was stable over time and similar to prior estimates.22 However, when weighted for the population distribution, these areas represented only 3% of US women age 40 and older. Lack of resource capacity is likely a barrier to breast cancer screening in these areas, and initiatives that establish or expand mobile mammography programs in neighboring counties may improve access for women who reside in zero-capacity counties.
Several health care market factors were correlated with mammography capacity. Counties with more uninsured residents or higher managed care penetration had lower capacity and were more likely to experience a decline in capacity. Both low health insurance coverage rates and high managed care penetration could potentially limit the profitability of health care services, especially preventive services, which may not be not be generously reimbursed by insurers and may be viewed as unnecessary by uninsured women who would have to pay for them out of pocket. Although some studies have found better adherence with breast cancer screening recommendations among managed care enrollees compared with their peers covered by traditional fee-for-service insurance policies,23-25 lower mammography capacity may be a barrier to breast cancer screening for women living in areas with high managed care penetration.
Mammography capacity was not significantly influenced by the number of radiologists per population. This is not surprising given the relatively low reimbursement of mammography and other real or perceived negative attributes of mammography, such as job stress and fear of malpractice, relative to other types of imaging services.26 Even though the mean number of radiologists per 100,000 county residents increased between 2000 and 2010, this change did not improve the availability of screening mammography for women in most counties, perhaps because new radiologists chose more lucrative and technologically interesting practice areas. Thus, policies aimed at the radiology workforce may not be the most effective levers for improving access to screening mammography.
Access to mammography has been a particular concern in the US since the passage of the Mammography Quality Standards Act (MQSA), enacted in 1992, which established national uniform quality standards for mammography.17, 27, 28 The MQSA has been credited with substantial improvements in mammography quality, and in earlier reports federal analysts concluded that the law has not impaired access to mammography services.29-31 From 1994 to 1997, facility closures were nearly offset by new facility openings or re-openings, and almost all facilities that closed were located within 25 miles of another certified mammography facility.30, 31 Between 1998 and 2001, the number of certified facilities declined by about 5%, but the total number of mammography machines increased 11%.12 The declines we observed in mammography facilities, machines and capacity per population between 2000 and 2010 were not likely related to federal legislation, but they renew earlier concerns about access to breast cancer screening services.
Our results also reinforce earlier anecdotal and empirical evidence that some areas may be disproportionately impacted by mammography facility closures. A prior survey of selected counties found that in some metropolitan areas, demand for mammography has grown while capacity has declined, leading to long waiting times and temporary interruptions in mammography availability.12 Our surveys of mammography facilities in six states in 2008 and 2011 suggest that wait times for the next available screening mammogram appointment are longer at facilities in counties with lower capacity.32, 33
In the current study we assumed that the imaging capacity of every machine is identical, while in fact, newer mammography machines may be more efficient than older machines, producing more scans per unit over a unit's lifetime. Notably, our study period coincides with widespread dissemination of digital mammography, which was approved for clinical use in January 2000. In 2008, 54% of mammography facilities in six states reported that they offered digital mammography or were in the process of acquiring digital mammography equipment.33 By 2011, 78% of facilities in the same six states reported that they offered digital mammography.32 Compared with screen-film mammography, digital mammography is associated with a significantly shorter image acquisition time.34 We were not able to account for variability across facilities in their average throughput or hours of operation.
Similarly, we addressed neither the availability of radiologic technologists nor the quality of services provided. The credentials and minimum number of personnel at each facility are regulated by the MQSA to some extent, and machine condition and image quality are monitored in mandatory annual facility inspections. However, some facilities may exceed the minimum standards, contributing to heterogeneity in service quality and capacity between facilities.
Ultimately, we are concerned with the impact of mammography capacity on the likelihood of screening. National surveys have routinely documented geographic variation in rates of screening mammography utilization, and our prior work suggests that women in counties with inadequate mammography capacity are less likely to have screening mammograms.35 It is not clear whether interventions for improving geographic access to screening should involve direct operation or relocation of resources by public health authorities, incentives for radiologists to offer screening mammography in low-capacity areas or other strategies. However, by identifying county-level demographic and health care market characteristics associated with lower capacity and declines in capacity, interventions can target the areas in greatest need of enhanced resource availability and the areas at greatest risk of further declines in mammography capacity.
Condensed abstract.
Geographic variation in mammography capacity and declines in capacity over time are associated with demographic, socioeconomic and health care market characteristics. Maldistribution of mammography resources may explain geographic disparities in breast cancer screening rates.
Acknowledgments
Funding:
This work was funded by grants from Susan G. Komen for the Cure (POP107806, PI: Elkin), the American Cancer Society (MRSG-06-127-01-CPHPS, PI: Elkin) and the National Cancer Institute (K07-CA118189, PI: Elkin).
Footnotes
Financial disclosures and conflicts of interest:
The authors have no financial disclosures or conflicts of interest to report.
REFERENCES
- 1.Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2002;137:347–360. doi: 10.7326/0003-4819-137-5_part_1-200209030-00012. [DOI] [PubMed] [Google Scholar]
- 2.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2009;151:727–737. W237–742. doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gotzsche PC, Nielsen M. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2011:CD001877. doi: 10.1002/14651858.CD001877.pub4. [DOI] [PubMed] [Google Scholar]
- 4.Ryerson AB, Miller JW, Eheman CR, Leadbetter S, White MC. Recent trends in U.S. mammography use from 2000-2006: a population-based analysis. Preventive Medicine. 2008;47:477–482. doi: 10.1016/j.ypmed.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Miller JW, King JB, Joseph DA, Richardson LC, Centers for Disease C, Prevention Breast cancer screening among adult women--Behavioral Risk Factor Surveillance System, United States, 2010. MMWR Morbidity and Mortality Weekly Report. 2012;61(Suppl):46–50. [PubMed] [Google Scholar]
- 6.Andersen MR, Urban N. The use of mammography by survivors of breast cancer. American Journal of Public Health. 1998;88:1713–1714. doi: 10.2105/ajph.88.11.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geller BM, Kerlikowske K, Carney PA, et al. Mammography surveillance following breast cancer. Breast Cancer Research and Treatment. 2003;81:107–115. doi: 10.1023/A:1025794629878. [DOI] [PubMed] [Google Scholar]
- 8.Hillner BE, McDonald K, Penerthy L, et al. Measuring standards of care for early breast cancer in an insured population. Journal of Clinical Oncology. 1997;15:1401–1408. doi: 10.1200/JCO.1997.15.4.1401. [DOI] [PubMed] [Google Scholar]
- 9.Keating NL, Landrum MB, Guadagnoli E, Winer EP, Ayanian JZ. Factors related to underuse of surveillance mammography among breast cancer survivors. Journal of Clinical Oncology. 2006;24:85–94. doi: 10.1200/JCO.2005.02.4174. [DOI] [PubMed] [Google Scholar]
- 10.Schapira M, McAuliffe T, Nattinger AB. Underutilization of mammography in older breast cancer survivors. Medical Care. 2000;38:281–289. doi: 10.1097/00005650-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Government Accountability Office . Mammography: Current Nationwide Capacity is Adequate, But Access Problems May Exist in Certain Locations. U.S. General Accounting Office; Washington, DC: 2006. [Google Scholar]
- 12.U.S. Government Accountability Office . Mammography: Capacity Generally Exists to Deliver Services. U.S. General Accounting Office; Washington, DC: 2002. [Google Scholar]
- 13.U.S. Department of Health and Human Services [January 10, 2013];Office of Disease Prevention and Health Promotion. Healthy People 2020. Available from URL: http://www.healthypeople.gov/2020/default.aspx.
- 14.Use of mammograms among women aged >/= 40 years--United States, 2000-2005. MMWR Morbidity and Mortality Weekly Report. 2007;56:49–51. [PubMed] [Google Scholar]
- 15.Breen N, A.K. C, Meissner HI, et al. Reported drop in mammography : is this cause for concern? Cancer. 2007;109:2405–2409. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 16.Farria DM, Schmidt ME, Monsees BS, et al. Professional and economic factors affecting access to mammography: a crisis today, or tomorrow? Results from a national survey. Cancer. 2005;104:491–498. doi: 10.1002/cncr.21304. [DOI] [PubMed] [Google Scholar]
- 17.Mammography Quality Standards Act. 1992.
- 18.U.S. Preventive Services Task Force Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 19.Allen SS, Pruthi S. The mammography controversy: when should you screen? J Fam Pract. 2011;60:524–531. [PubMed] [Google Scholar]
- 20.Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer Journal for Clinicians. 2010;60:99–119. doi: 10.3322/caac.20063. [DOI] [PubMed] [Google Scholar]
- 21.Smith RA, Duffy SW, Tabar L. Breast cancer screening: the evolving evidence. Oncology (Williston Park) 2012;26:471–475. 479–481, 485–476. [PubMed] [Google Scholar]
- 22.Peipins LA, Miller J, Richards TB, et al. Characteristics of US counties with no mammography capacity. J Community Health. 2012;37:1239–1248. doi: 10.1007/s10900-012-9562-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haggstrom DA, Phillips KA, Liang SY, Haas JS, Tye S, Kerlikowske K. Variation in screening mammography and Papanicolaou smear by primary care physician specialty and gatekeeper plan (United States). Cancer Causes and Control. 2004;15:883–892. doi: 10.1007/s10552-004-1138-5. [DOI] [PubMed] [Google Scholar]
- 24.Makuc DM, Freid VM, Parsons PE. Health insurance and cancer screening among women. Advance Data from Vital and Health Statistics. National Center for Health Statistics; Hyattsville, MD: 1994. pp. 1–12. [PubMed] [Google Scholar]
- 25.Phillips KA, Haas JS, Liang SY, et al. Are gatekeeper requirements associated with cancer screening utilization? Health Services Research. 2004;39:153–178. doi: 10.1111/j.1475-6773.2004.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baxi SS, Snow JG, Liberman L, Elkin EB. The future of mammography: radiology residents’ experiences, attitudes, and opinions. AJR Am J Roentgenol. 2010;194:1680–1686. doi: 10.2214/AJR.09.3735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mammography Quality Standards Reauthorization Act of 1998. 1998.
- 28.Mammography Quality Standards Reauthorization Act of 2004. 2004.
- 29.U.S. General Accounting Office . FDA's Mammography Inspections: While Some Problems Need Attention, Facility Compliance is Growing. U.S. General Accounting Office; Washington, DC: 1997. [Google Scholar]
- 30.U.S. General Accounting Office . Mammography Services: Impact of Federal Legislation on Quality, Access and Health Outcomes. U.S. General Accounting Office; Washington, DC: 1997. [Google Scholar]
- 31.U.S. General Accounting Office . Mammography Quality Standards Act: X-ray Quality Improved, Access Unaffected, but Impact on Health Outcomes Unknown. U.S. General Accounting Office; Washington, DC: 1998. [Google Scholar]
- 32.Elkin EB, Nobles JP, Pinheiro LC, Atoria CL, Schrag D. Changes in access to screening mammography, 2008-2011. Cancer Causes Control. 2013;24:1057–1059. doi: 10.1007/s10552-013-0180-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elkin EB, Snow JG, Leoce NM, Atoria CL, Schrag D. Mammography capacity and appointment wait times: barriers to breast cancer screening. Cancer Causes Control. 2012;23:45–50. doi: 10.1007/s10552-011-9853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berns EA, Hendrick RE, Solari M, et al. Digital and screen-film mammography: comparison of image acquisition and interpretation times. AJR Am J Roentgenol. 2006;187:38–41. doi: 10.2214/AJR.05.1397. [DOI] [PubMed] [Google Scholar]
- 35.Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Medical Care. 2010;48:349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]