Abstract
Background and Purpose
Regular physical activity is an important recommendation for stroke prevention. We compared the associations of self-reported physical activity (PA) with incident stroke in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study.
Methods
REGARDS recruited 30,239 US blacks (42%) and whites, aged ≥45 with follow-up every six months for stroke events. Excluding those with prior stroke, analysis involved27,348participants who reported their frequency of moderate-vigorous intensity PA at baseline according to three categories: none (physical inactivity), 1–3 times/week and ≥ 4 times/week. Stroke and TIA cases were identified during an average of 5.7 years of follow-up. Cox proportional hazards models were constructed to examine whether self-reported PA was associated with risk of incident stroke.
Results
Physical inactivity was reported by 33% of participants and was associated with a hazard ratio (HR) of 1.20 ([95% confidence intervals 1.02–1.42], p = 0.035). Adjustment for demographic and socioeconomic factors did not affect HR, but further adjustment for traditional stroke risk factors (diabetes, hypertension, body mass index, alcohol use and smoking) partially attenuated this risk (HR 1.14 [0.95–1.37], p = 0.17). There was no significant association between PA frequency and risk of stroke by sex groups although there was a trend towards increased risk for men reporting PA 0–3 times a week compared to 4 or more times a week.
Conclusions
Self-reported low PA frequency is associated with increased risk of incident stroke. Any effect of PA is likely to be mediated through reducing traditional risk factors.
Keywords: stroke, physical exercise, stroke prevention
Stroke is a leading cause of disability in the United States and the fourth leading cause of mortality1 with total incidence expected to escalate in the coming decades with the rapidly ageing population2. Adults who make healthy lifestyle choices have an 80% lower risk of stroke when compared to those who do not3, indicating that advances can still be made in primary prevention of stroke. An important component of a healthy lifestyle is regular physical activity (PA), as recommended by the “Physical Activity Guidelines for Americans”4, which is associated with lower risk of stroke5, 6. Recent data from the 2010 National Health Interview Survey revealed that 49% of Americans do not meet these Physical Activity Guidelines7. There is considerable evidence from prospective and case-controlled studies that higher self-reported PA levels are associated with a reduced risk of stroke1, 8.
Physical inactivity has been identified as the second leading risk factor for stroke following hypertension in a multinational case-control study (INTERSTROKE), finding a population-attributable risk of 28.5%9. Although the precise amounts and type of exercise required to prevent stroke are unclear, meta-analyses conclude that “regular” PA reduces the risk of stroke by 25–30% when compared with the least active people8, 10. Recent evidence is emerging that there may be differences between sexes with vigorous PA associated with decreased risk of stroke in men11 but not women12. Many large prospective studies investigating the association between PA and stroke have involved only women or men, and often only in limited locations or professions13–16. The aim of this study was to investigate the potential for PA to reduce incident stroke in a large, national multi-racial prospective cohort study of men and women.
Materials and Methods
The REasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national, population based, longitudinal study of 30 239 Americans, was designed to determine the causes for the excess stroke mortality in African Americans and those living in the Southeastern US17. Participants aged 45 years and over were recruited by mail and telephone between 2003 and 2007 from a commercially available list of residents with over sampling of blacks and residents of the southeastern Stroke Belt, an area with higher stroke mortality rates than the remaining United States18. Within the Stroke Belt, there is a region along the coastal plain of North Carolina, South Carolina and Georgia that has even higher stroke mortality than the remainder of the Stroke Belt, and this area is identified as the Stroke Buckle19. Demographic information and medical history were obtained by telephone interview followed by an in-home visit to obtain physical measurements. Cerebrovascular disease risk factors were body mass index, smoking status (never versus past versus current use of cigarettes), alcohol use (heavy: ≥ 7 drinks/week for women, ≥14 per week for men; moderate:1–7 for women, 1–14 for men; and none), diabetes (fasting glucose >126 ml/dL or non-fasting glucose >200 ml/dL, or self-reported use of oral hypoglycemic medications or insulin) and hypertension (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or self-reported use of antihypertensive medications). Participants are contacted every 6 months by telephone to assess potential stroke, with retrieval and central physician adjudication of medical charts of suspected strokes. Consent was obtained verbally and later in writing. All involved Institutional Review Boards approved the study methods.
Of the 30 239 REGARDS participants, follow up data were available for 29 643. Of these, we excluded 1 854 participants due to prevalent stroke, and 441 who had not answered the PA question.
Assessment of physical activity
At enrollment, participants reported their usual PA frequency using the following question: “How many times per week do you engage in intense physical activity, enough to work up a sweat?” Physical activity, in this context, could involve leisure time, commuting and occupational PA. Responses were categorized into 3 groups: 1 = no times per week, 2 = 1 to 3 times per week, 3 = 4 or more times per week. Although geographic region and season may influence the intensity of PA required to work up a sweat, this widely used measure of PA is well validated20, 21, can include either aerobic or resistance training and has been used in similar studies such as the National Health And Nutrition Examination Survey22 and similar questions have been used in other longitudinal cohort studies13, 23. The “sweat question” has been shown to correlate with measures of physical fitness, such as maximal oxygen uptake and treadmill time during a maximal exercise fitness test24, 25.This categorization of PA is appropriate because the effects of PA on stroke risk are more pronounced with moderate-vigorous rather than light PA8, 11 and allows analysis of the dose-response relationship between PA frequency and risk of stroke.
Stroke events
Incidence of stroke is confirmed in a three-stage process which has been described previously26. Briefly, reports of possible stroke during follow-up result in the retrieval of medical records that are centrally adjudicated by at least 2 physician members of a committee of stroke experts to confirm that the case meets the WHO definition27. Events not meeting this definition due to a duration of symptoms <24 hours and neuroimaging consistent with acute ischemia or hemorrhage were classified as “clinical strokes”, or “probable strokes” if adjudicators agreed that event was likely a stroke or death related to stroke but information was incomplete for WHO or clinical classification. Strokes were further classified as ischemic or hemorrhagic. Participants who reported a diagnosis of TIA were also included in this analysis as a stroke-event.
Statistical analysis
Cox proportional hazards analysis was used to determine the hazard ratios (HR) and 95% confidence intervals (CIs) for the association between PA and incident stroke/TIA. Models were initially adjusted for age, sex, race and age-race interaction, then for socioeconomic factors (income and education). An additional model was adjusted for stroke risk factors (diabetes, hypertension, body mass index, alcohol use and smoking status). A final model took into account the effect of physical health limitations on incident stroke for those people who answered yes to either one or both of the following questions: “Does your health limit moderate activities such as moving a table, pushing a vacuum cleaner, bowling or playing golf?”, “Does your health limit you climbing several flights of stairs?”
The protective level of PA was defined as taking part in exercise 4 times or more per week, in accordance with the INTERSTROKE study9.
Results
Table 1 shows the baseline characteristics of the REGARDS participants by PA category. Participants who were more physically active tended to be male, white, have higher levels of education, higher income and had lower BMI and prevalence of diabetes.
Table 1.
Baseline Characteristics of Study Participants by Physical Activity Frequency
| All N=27348 |
≥ 4x/wk n=8187 |
1–3x/wk n=10003 |
None n=9158 |
p- value* |
||
|---|---|---|---|---|---|---|
| Age, mean (SD) | 64.6(9.39) | 64.8(9.13) | 63.6(9.22) | 65.6(9.71) | <0.0001 | |
| Black, % | 40.4 | 36.1 | 40.5 | 44.2 | <0.0001 | |
| Female, % | 55.5 | 46.1 | 55.0 | 64.3 | <0.0001 | |
| Region, % | ||||||
| Belt | 34.7 | 34.9 | 34.5 | 34.7 | 0.3899 | |
| Buckle | 21.0 | 21.6 | 21.0 | 20.6 | ||
| Nonbelt | 44.3 | 43.5 | 44.5 | 44.7 | ||
| Urban Group, % | ||||||
| Urban | 78.1 | 75.1 | 78.7 | 80.1 | <0.0001 | |
| Mixed | 11.0 | 12.2 | 10.8 | 10.2 | ||
| Rural | 10.9 | 12.7 | 10.5 | 9.7 | ||
| Annual Income, % | ||||||
| Less than 20K | 17.1 | 15.2 | 14.2 | 22.1 | <0.0001 | |
| 20–34K | 23.9 | 23.2 | 23.1 | 25.4 | ||
| 35–74K | 30.5 | 31.3 | 32.6 | 27.3 | ||
| 75K and above | 16.5 | 18.2 | 19.2 | 12.1 | ||
| Refused | 12.0 | 12.1 | 10.9 | 13.1 | ||
| Highest Education, % | ||||||
| Less than HS | 11.6 | 11.0 | 9.5 | 14.6 | <0.0001 | |
| HS graduate | 25.7 | 25.5 | 23.4 | 28.3 | ||
| Some college | 26.9 | 25.9 | 27.1 | 27.5 | ||
| College Grad and above | 35.8 | 37.6 | 40.0 | 29.6 | ||
| BMI kg/m2, mean(SD) | 29.3(6.18) | 28.2(5.44) | 29.3(5.95) | 30.3(6.86) | <0.0001 | |
| Smoke, % | ||||||
| Current | 14.2 | 12.7 | 13.0 | 16.7 | <0.0001 | |
| Never | 45.8 | 44.4 | 48.4 | 44.2 | ||
| Past | 40.0 | 42.9 | 38.6 | 39.1 | ||
| Alcohol Use, % | ||||||
| Heavy | 4.1 | 5.2 | 3.7 | 3.6 | <0.0001 | |
| Moderate | 34.1 | 36.8 | 36.6 | 28.8 | ||
| None | 61.8 | 58.0 | 59.7 | 67.6 | ||
| Diabetes, % | 21.0 | 17.5 | 19.7 | 25.4 | <0.0001 | |
| Hypertension, % | 57.8 | 53.2 | 56.1 | 63.9 | <0.0001 | |
HS = high school, BMI = body mass index.
p-values based on ANOVA tests for mean differences and Chi-square tests for differences in proportions
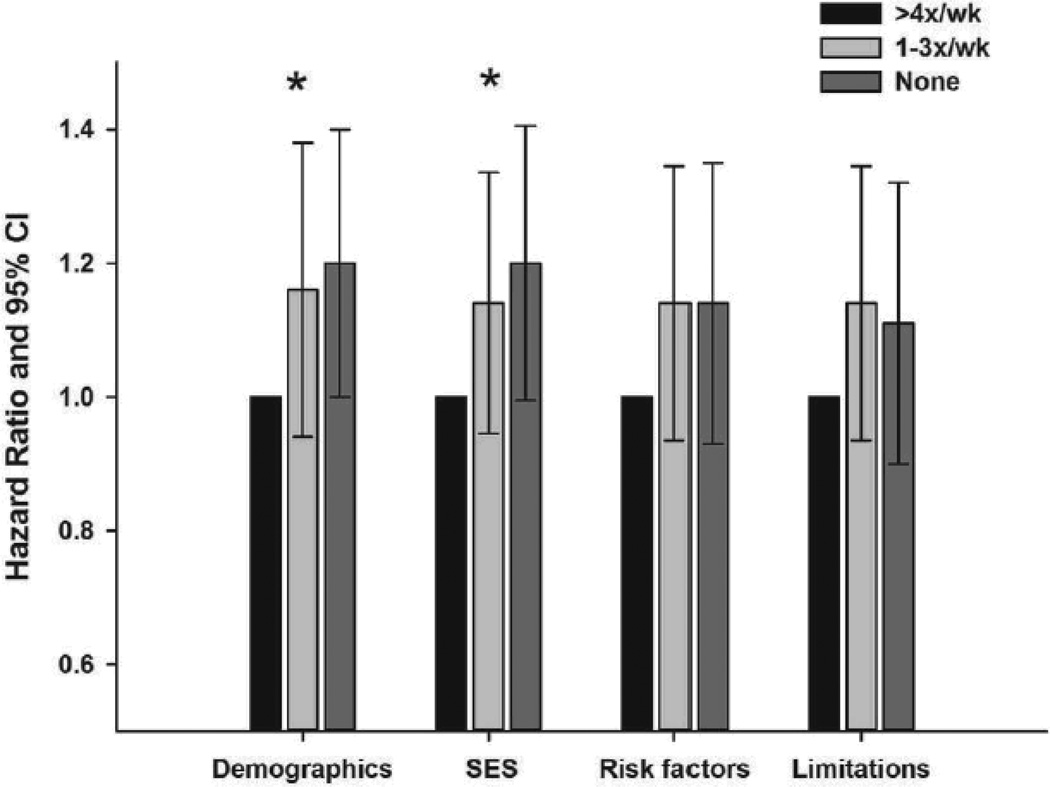
Participants were followed for a mean of 5.7 years, and there were 918 confirmed incident stroke and TIA cases. There was a significant association between PA and incident stroke/TIA as demonstrated in Figure 1. After adjustment for age, sex, race and age-race interaction, the HR for stroke/TIA for those undertaking no PA was 1.20 (95% confidence interval [CI]: 1.02 to 1.42) and for PA1-3x/wk, the HR was 1.16 (95% CI: 0.98 to 1.42). After adjustment for region, urban/rural residence and socioeconomic status (SES), the significant association remained with similar HR of 1.20(95% CI: 1.01 to 1.42) for no PA and 1.14 (95% CI: 0.96 to 1.35) for 1–3x/wk. There was a dose dependent relationship, with PA 1–3x/wk offering less protection against stroke than ≥4x/wk. Further adjustment for stroke risk factors attenuated the effect by 30% to 1.14 (95% CI: 0.95 to 1.37), making the association statistically insignificant. The final adjustment for physical limitations did not change the HRs further.
Figure 1.
PA frequency and risk of incident stroke/TIA. The initial regression model included adjustment for demographics (age, sex, race and age-race interaction) and then further adjustments were performed for 3 additional models: SES (including region, urban/rural residence); stroke risk factors (diabetes, hypertension, BMI, alcohol use, smoking); presence of physical limitations (unable to climb stairs, perform moderate physical activities). * denotes significant association between PA and stroke (Ptrend < 0.05).
The association between PA frequency and incident stroke/TIA was further investigated by comparing the risk of incident stroke in those who report being physically active≥4x/wk to those reporting PA 0–3x/wk. After adjustment for age, sex, race and age-race interaction, the HR for stroke/TIA was 1.18 (95% CI: 1.01, 1.36). This was partially attenuated after adjustment for region, urban/rural residence and SES (HR 1.17;95% CI (0.99, 1.36) and the associations were statistically insignificant after further adjustment.
Analyses were repeated separately for stroke type (ischemic versus haemorrhagic), with no difference in the results obtained [data not shown].
The protective effect of PA has been reported to differ between men and women28 but the interaction between sex and PA was not significant in this analysis (p = 0.22), perhaps due to insufficient power. To investigate this further we stratified our results by sex to investigate whether this revealed a difference in risk of incident stroke in our cohort (see Table 2). Men who took part in PA 1–3x/wk compared with ≥4x/wk had greater incidence of stroke. This relationship was significant for the demographic model with a hazard ratio of 1.30 (95% CI: 1.05 to 1.61) and also for the SES model with a hazard ratio of 1.26 (95% CI: 1.00 to 1.59). Further adjustment for stroke risk factors and physical limitations did not attenuate the effect for men (adjustment for physical limitations not shown, results are identical to the risk factor model for men).These findings contrast with those observed in women, with no significant association between PA and incident stroke although there was a trend towards a similar reduction in risk for PA 1–3 times/week and 4 or more times a week compared to none. Additional analysis was performed combining both 1–3 and ≥ 4x/wk categories to compare any PA to none. This demonstrated a lack of association between PA frequency and incident stroke, with the demographic model demonstrating no effect of PA on stroke (women, hazard ratio 1.15 (95% CI: 0.95 to 1.39); men, hazard ratio 1.05 (95% CI: 0.86 to 1.29).
Table 2.
Association between PA frequency and incident stroke/TIA in women and men
| No. of cases | Demographic model | SES model | Risk factor model | |
|---|---|---|---|---|
| Women | ||||
| ≥ 4x/wk (n = 3777) | 105 | 1 | 1 | 1 |
| 1–3x/wk (n = 5498) | 146 | 1.00 (0.78–1.28) | 0.99 (0.76–1.29) | 0.99 (0.75–1.30) |
| None (n = 5890) | 198 | 1.15 (0.91–1.46) | 1.19 (0.93–1.52) | 1.10 (0.85–1.43) |
| p-value for trend | 0.20 | 0.12 | 0.40 | |
| Men | ||||
| ≥ 4x/wk (n = 4410) | 149 | 1 | 1 | 1 |
| 1–3x/wk (n = 4505) | 188 | 1.30 (1.05–1.61) | 1.26 (1.00–1.59) | 1.29 (1.02–1.64) |
| None (n = 3268) | 132 | 1.21 (0.95–1.53) | 1.16 (0.90–1.49) | 1.13 (0.87–1.47) |
| p-value for trend | 0.09 | 0.21 | 0.35 |
There was no significant interaction between race and physical activity therefore results were not stratified for race.
Discussion
The results of this large, population-based prospective cohort study confirm that regular PA is associated with a decreased risk of incident stroke and TIA. This effect was seen for ≥4x/wk compared to no PA, with 1–3x/wk showing a trend toward being less protective than ≥4x/wk although not significantly different. This confirms previous reports suggesting that exercising four times a week is associated with a reduced risk of stroke9 and other meta-analyses which suggest that moderate intensity PA reduces the risk of stroke8, 11.To the best of our knowledge, this is the first study to quantify the protective effect of PA on incident stroke in such a large multiracial cohort with equal representation of men and women in the US.
The association between PA and incident stroke was present after adjustment for demographic and SES factors, but further adjustment for stroke risk factors attenuated the relationship somewhat. This suggests that PA interacts with stroke risk factors, such as diabetes, hypertension, body mass index, alcohol use and smoking status. In our cohort, there was an unexpected finding in the prevalence of risk factors amongst the groups: those who regularly participated in PA were more likely to be moderate or heavy consumers of alcohol. Both PA groups were, however, less likely to smoke, have hypertension or have a high BMI, and had significantly less diabetes than the non-exercisers. Thus, reduced stroke risk in the exercisers is likely to be explained for the most part by the positive effect that PA has on BMI, hypertension and diabetes, although PA also has the potential to reduce stroke risk due to other biological actions (e.g. improving endothelial function29 and reducing platelet activity30).
Consistent with a previous report28, we found a difference between PA and risk reduction when results were stratified according to sex. There was no protective effect of 1–3x/wk or ≥4x/wk on incident stroke/TIA in women, which was confirmed by collapsing both activity categories and still finding no association. The opposite was true for men, with increased hazard ratios for 1–3x/wk (but not 0 times per week) compared with ≥4x/wk, although this trend was not significant (p = 0.09). Combining both PA categories for men attenuated the association completely, confirming that PA ≥4x/wk is required to reduce the risk of incident stroke in men.
Our PA measure enabled us to classify participants based on the frequency of moderate to vigorous PA rather than duration. Nevertheless, there was a significant difference in stroke risk between those individuals reporting PA1–3 or ≥4 times per week, confirming that regular moderate to heavy intensity PA is protective against stroke and TIA11. This was further substantiated with subsequent analysis which compared PA≥ 4x/wk to 0–3 x/wk and found a significant association with a HR of 1.18; exercising “intensely” at least four times a week was required for PA have a protective effect in this cohort, as previously reported11. Separate analyses by stroke subtype showed similar results. This is consistent with other reports that have considered risk of stroke separately for all stroke, as well as haemorrhagic and ischaemic strokes with similar findings8, 9, 12, 31.
An important consideration in the interpretation of these results is the potential limitation of our measurement of PA. Although the “sweat question” is a valid tool to assess PA in large cohort studies such as REGARDS, it does not include certain key elements to consider when quantifying PA. Firstly, asking specifically about intense PA which works up a sweat may prevent participants from including activities with a light or moderate intensity such as walking or cycling, which may underestimate the amounts of PA actually performed. Secondly, our measure of PA does not quantify the duration or type of PA, nor the precise number of sessions: responses for those who reported exercising once per week were included in the same category as those exercising three times per week. It is possible that the inability to find an association between PA and incident stroke in women in our sample is due to the limitation of our PA measure to capture walking and other low intensity PA; it has previously been reported that walking, but not vigorous PA, is associated with reduced stroke risk in women12. Future large-scale cohort studies should consider incorporating measures of PA that allow quantification of intensity, duration and frequency, such as the International Physical Activity Questionnaire32 or accelerometry.
Another limitation of the study was that the classification of PA category was performed at entry into the study, with stroke events occurring several years later. While participants may have changed their PA habits during this time, the advantage of this method is that responses are not influenced by recall bias if they were asked to report their usual PA habits soon after diagnosis of stroke, which frequently leads to overestimating of PA5. Another potential limitation is that stroke cases could have been missed if participants did not seek medical care or report a suspected stroke. However, medical records were obtained for 89% of potential stroke events, including those instances where participants sought medical attention for stroke-like symptoms. It is possible that incident stroke may have been under-reported, but few stroke events are likely to have been missed. The strengths of this study include the rigorous confirmation of stroke incidence with review of medical records with stroke experts, and participation in follow up interviews was very high. Furthermore, other strengths include the large sample size representative of blacks and whites, with greater representation of those in areas of high stroke mortality.
In conclusion, regular moderately-vigorous self-reported PA is associated with a reduced risk of stroke and TIA in this large multi-racial prospective cohort study. When considering men, exercising at an intensity sufficient to work up a sweat at least 4 times a week is more protective than exercising 1–3 times per week. Any effect of PA is likely to be mediated through reduction of traditional risk factors such as body mass index and diabetes.
Acknowledgments
MN McDonnell is supported by a National Health and Medical Research Council of Australia Fellowship. The authors thank the investigators, staff, and participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org
Sources of Funding
This research project was supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institute of Health, Department of Health and Human Services.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howard G, Goff DC. Population shifts and the future of stroke: forecasts of the future burden of stroke. Ann N Y Acad Sci. 2012;1268:14–20. doi: 10.1111/j.1749-6632.2012.06665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation. 2008;118:947–954. doi: 10.1161/CIRCULATIONAHA.108.781062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 5.Stroud N, Mazwi TM, Case LD, Brown RD, Jr, Brott TG, Worrall BB, et al. Prestroke physical activity and early functional status after stroke. J Neurol Neurosurg Psychiatry. 2009;80:1019–1022. doi: 10.1136/jnnp.2008.170027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Win S, Parakh K, Eze-Nliam CM, Gottdiener JS, Kop WJ, Ziegelstein RC. Depressive symptoms, physical inactivity and risk of cardiovascular mortality in older adults: the Cardiovascular Health Study. Heart. 2011;97:500–505. doi: 10.1136/hrt.2010.209767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10:1–207. [PubMed] [Google Scholar]
- 8.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke. 2003;34:2475–2481. doi: 10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- 9.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 11.Willey JZ, Moon YP, Paik MC, Boden-Albala B, Sacco RL, Elkind MS. Physical activity and risk of ischemic stroke in the Northern Manhattan Study. Neurology. 2009;73:1774–1779. doi: 10.1212/WNL.0b013e3181c34b58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sattelmair JR, Kurth T, Buring JE, Lee IM. Physical activity and risk of stroke in women. Stroke. 2010;41:1243–1250. doi: 10.1161/STROKEAHA.110.584300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu FB, Stampfer MJ, Colditz GA, Ascherio A, Rexrode KM, Willett WC, et al. Physical activity and risk of stroke in women. JAMA. 2000;283:2961–2967. doi: 10.1001/jama.283.22.2961. [DOI] [PubMed] [Google Scholar]
- 14.Kiely DK, Wolf PA, Cupples LA, Beiser AS, Kannel WB. Physical activity and stroke risk: the Framingham Study. Am J Epidemiol. 1994;140:608–620. doi: 10.1093/oxfordjournals.aje.a117298. [DOI] [PubMed] [Google Scholar]
- 15.Lee IM, Hennekens CH, Berger K, Buring JE, Manson JE. Exercise and risk of stroke in male physicians. Stroke. 1999;30:1–6. doi: 10.1161/01.str.30.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke. 1990;21:701–706. doi: 10.1161/01.str.21.5.701. [DOI] [PubMed] [Google Scholar]
- 17.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 18.Borhani NO. Changes and Geographic Distribution of Mortality from Cerebrovascular Disease. Am J Public Health Nations Health. 1965;55:673–681. doi: 10.2105/ajph.55.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt region of the United States. Stroke. 1997;28:936–940. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 20.Washburn RA, Adams LL, Haile GT. Physical activity assessment for epidemiologic research: the utility of two simplified approaches. Prev Med. 1987;16:636–646. doi: 10.1016/0091-7435(87)90047-8. [DOI] [PubMed] [Google Scholar]
- 21.Washburn RA, Goldfield SR, Smith KW, McKinlay JB. The validity of self-reported exercise-induced sweating as a measure of physical activity. Am J Epidemiol. 1990;132:107–113. doi: 10.1093/oxfordjournals.aje.a115622. [DOI] [PubMed] [Google Scholar]
- 22.Prevention CfDCa. National Health and Nutrition Examination Survey Questionnaire: physical activity and physical fitness - PAQ. 2007 - 2008 Data Documentation, Codebook, and Frequencies. Centers for Disease Control and Prevention; http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/PAQ_E.htm#PAQ620 20 June 2012 2009. [Google Scholar]
- 23.Duvernoy CS, Martin JW, Briesmiester K, Muzik O, Mosca L. Self-reported physical activity and myocardial flow reserve in postmenopausal women at risk for cardiovascular disease. J Womens Health (Larchmt) 2006;15:45–50. doi: 10.1089/jwh.2006.15.45. [DOI] [PubMed] [Google Scholar]
- 24.Siconolfi SF, Lasater TM, Snow RC, Carleton RA. Self-reported physical activity compared with maximal oxygen uptake. Am J Epidemiol. 1985;122:101–105. doi: 10.1093/oxfordjournals.aje.a114068. [DOI] [PubMed] [Google Scholar]
- 25.Kohl HW, Blair SN, Paffenbarger RS, Jr, Macera CA, Kronenfeld JJ. A mail survey of physical activity habits as related to measured physical fitness. Am J Epidemiol. 1988;127:1228–1239. doi: 10.1093/oxfordjournals.aje.a114915. [DOI] [PubMed] [Google Scholar]
- 26.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980;58:113–130. [PMC free article] [PubMed] [Google Scholar]
- 28.Diep L, Kwagyan J, Kurantsin-Mills J, Weir R, Jayam-Trouth A. Association of physical activity level and stroke outcomes in men and women: a meta-analysis. J Womens Health (Larchmt) 2010;19:1815–1822. doi: 10.1089/jwh.2009.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sherman DL. Exercise and endothelial function. Coron Artery Dis. 2000;11:117–122. doi: 10.1097/00019501-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Rauramaa R, Salonen JT, Seppanen K, Salonen R, Venalainen JM, Ihanainen M, et al. Inhibition of platelet aggregability by moderate-intensity physical exercise: a randomized clinical trial in overweight men. Circulation. 1986;74:939–944. doi: 10.1161/01.cir.74.5.939. [DOI] [PubMed] [Google Scholar]
- 31.Wendel-Vos GC, Schuit AJ, Feskens EJ, Boshuizen HC, Verschuren WM, Saris WH, et al. Physical activity and stroke. A meta-analysis of observational data. Int J Epidemiol. 2004;33:787–798. doi: 10.1093/ije/dyh168. [DOI] [PubMed] [Google Scholar]
- 32.Hagstromer M, Oja P, Sjostrom M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9:755–762. doi: 10.1079/phn2005898. [DOI] [PubMed] [Google Scholar]