Abstract
The Healthy Eating Index (HEI) is a measure of diet quality in terms of conformance with federal dietary guidance. Publication of the Dietary Guidelines for Americans, 2010 prompted an interagency working group to update the HEI. The HEI-2010 retains several features of the 2005 version: (1) it has 12 components, many unchanged, including 9 adequacy and 3 moderation components; (2) it uses a density approach to set standards, e.g., per 1000 calories or as a percent of calories; and (3) it employs least-restrictive standards, i.e., those that are easiest to achieve among recommendations that vary by energy level, sex, and/or age. Changes to the index include: (1) Greens and Beans replaces Dark Green and Orange Vegetables and Legumes; (2) Seafood and Plant Proteins has been added to capture specific choices from the protein group; (3) Fatty Acids, a ratio of poly- and mono-unsaturated to saturated fatty acids, replaces Oils and Saturated Fat to acknowledge the recommendation to replace saturated fat with mono-and polyunsaturated fatty acids; and (4) a moderation component, Refined Grains, replaces the adequacy component, Total Grains, to assess over-consumption. The HEI-2010 captures the key recommendations of the 2010 Dietary Guidelines and, like earlier versions, will be used to assess the diet quality of the U.S. population and subpopulations, in evaluating interventions, in dietary patterns research, and to evaluate various aspects of the food environment.
Keywords: Healthy Eating Index, diet quality, diet assessment tool
Introduction
The Healthy Eating Index (HEI) is a measure of diet quality in terms of conformance to the Dietary Guidelines for Americans, which are the basis of nutrition policy for the United States government and the foundation of all federal nutrition guidance. The accompanying U.S. Department of Agriculture (USDA) Food Patterns translate key recommendations of the Dietary Guidelines into specific, quantified recommendations for types and amounts of foods to consume at 12 calorie levels with limits on calories from solid fats and added sugars.1 The USDA Food Patterns are used to set the scoring standards for the HEI. In addition to the USDA Food Patterns, the 2005 and the 2010 editions of the Dietary Guidelines included the Dietary Approaches to Stop Hypertension (DASH) Eating Plan as another example of a dietary pattern that illustrates eating according to the Dietary Guidelines. Compared to typical food consumption patterns in the U.S., both the USDA Food Patterns and the DASH Eating Plan include more vegetables, fruits, whole grains, and low-fat dairy products and less refined grains, saturated fatty acids, and added sugars.1, 2
The Dietary Guidelines are issued every 5 years by the USDA and U.S. Department of Health and Human Services. The HEI was last revised to reflect the 2005 edition of the Dietary Guidelines.3,4 The release of the 2010 Dietary Guidelines and revised USDA Food Patterns necessitated an update to the HEI-2005 to capture key changes, such as the addition of recommendations for seafood (fish and shellfish) and limitations on refined grains.1 However, key features of the HEI-2005, described elsewhere,3 were maintained in the HEI-2010: (1) diet quality is assessed from two perspectives: adequacy (dietary components to increase) and moderation (dietary components to decrease); (2) the scoring standards are density-based such that the relative mix of foods is evaluated; and (3) the standards for the maximum scores are the least-restrictive (easiest to achieve) recommendations among those that vary by energy level, sex, and/or age. For the adequacy components, this means that increasing levels of intake receive increasingly higher scores; whereas for the moderation components, increasing levels of intake receive decreasingly lower scores. In other words, for all components, higher scores indicate closer conformance with dietary guidance.
The purpose of this paper is to describe the process and rationale for updating the HEI to reflect the key diet-related recommendations of the 2010 Dietary Guidelines and the resulting components and scoring standards. The evaluation of the HEI-2010 will be described in a separate report.
Process for Updating the HEI
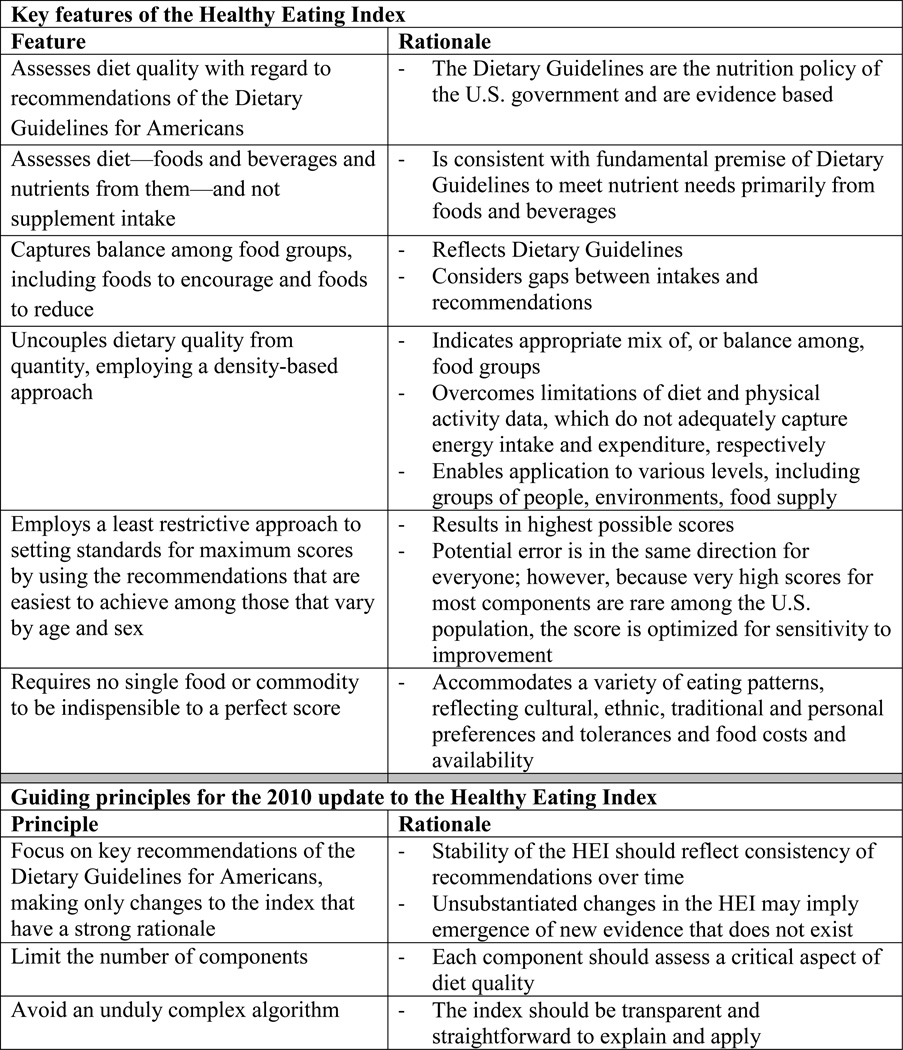
The USDA Center for Nutrition Policy and Promotion (CNPP) convened a group of federal users of the HEI and the Dietary Guidelines to discuss the process and content for the update. This meeting and subsequent discussions of a working group of staff from CNPP and the National Cancer Institute led to the development of guiding principles for the update (Figure 1). Drawing upon these principles, the working group subsequently reviewed the HEI-2005 in relation to the 2010 Dietary Guidelines and the USDA Food Patterns, discussed potential strategies to address key changes in the guidance, and made the decisions presented here. The wider group commented on the changes to the HEI and reviewed this manuscript prior to publication.
Figure 1.
Key features of the Healthy Eating Index and guiding principles for the 2010 update
HEI-2010 Components
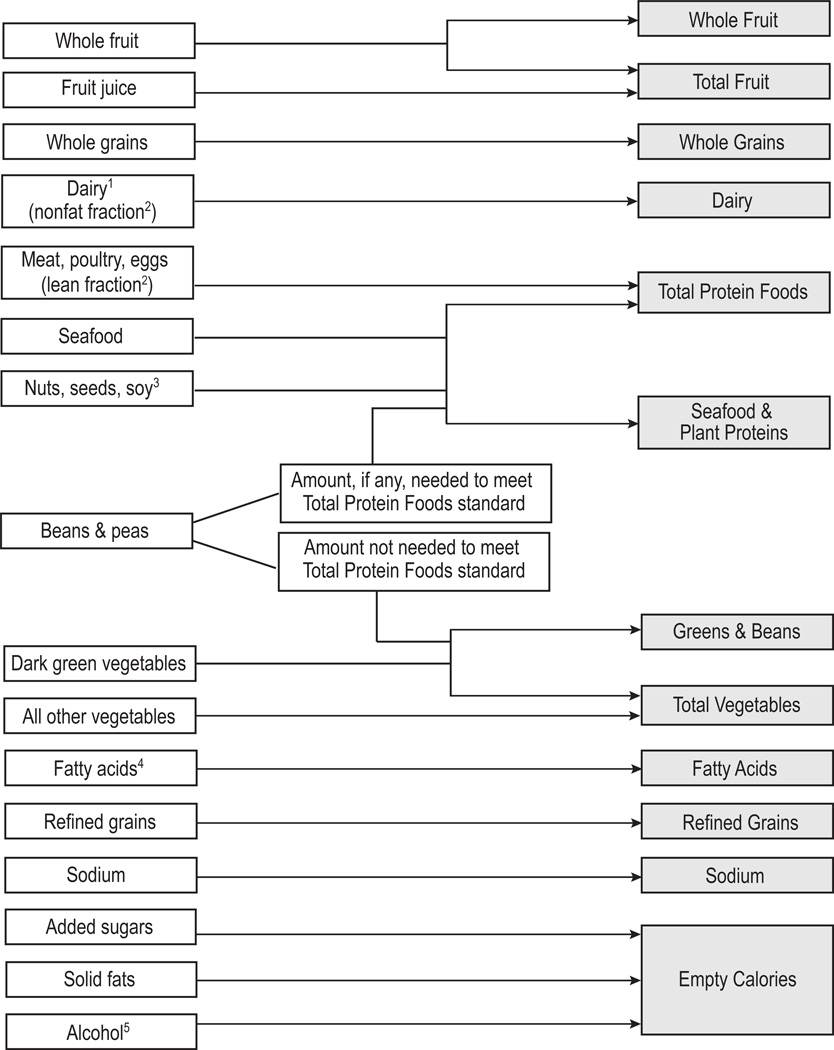
A list of the HEI-2010 and HEI-2005 components along with their point values and scoring standards are found in Table 1. Figure 2 maps the key dietary recommendations found in the 2010 Dietary Guidelines to the components of the HEI-2010. Like its predecessor, the HEI-2010 is made up of 12 components, 9 adequacy components and 3 moderation components (Table 1), and Figure 3 illustrates how the USDA Food Patterns and the nutrients considered in the HEI-2010 relate to the HEI-2010 components. Total Fruit, Whole Fruit, Total Vegetables, Total Grains, and Sodium were carried forward from the HEI-2005. Milk and Meat and Beans were also carried forward but have been renamed Dairy and Total Protein Foods, respectively, for consistency with the 2010 USDA Food Patterns.
Table 1.
Healthy Eating Index-2010 and Healthy Eating Index-2005 components and standards for scoring
| Component | Maximum points |
Standard for maximum score | Standard for minimum score of zero |
|---|---|---|---|
| HEI-20101 | |||
| Adequacy: | |||
| Total Fruit2 | 5 | ≥0.8 cup equiv. per 1,000 kcal | No Fruit |
| Whole Fruit3 | 5 | ≥0.4 cup equiv. per 1,000 kcal | No Whole Fruit |
| Total Vegetables4 | 5 | ≥1.1 cup equiv. per 1,000 kcal | No Vegetables |
| Greens and Beans4 | 5 | ≥ 0.2 cup equiv. per 1,000 kcal | No Dark Green Vegetables or Beans and Peas |
| Whole Grains | 10 | ≥1.5 oz equiv. per 1,000 kcal | No Whole Grains |
| Dairy5 | 10 | ≥1.3 cup equiv. per 1,000 kcal | No Dairy |
| Total Protein Foods6 | 5 | ≥2.5 oz equiv. per 1,000 kcal | No Protein Foods |
| Seafood and Plant Proteins6,7 | 5 | ≥0.8 oz equiv. per 1,000 kcal | No Seafood or Plant Proteins |
| Fatty Acids8 | 10 | (PUFAs + MUFAs)/SFAs ≥2.5 | (PUFAs + MUFAs)/SFAs ≤1.2 |
| Moderation: | |||
| Refined Grains | 10 | ≤1.8 oz equiv. per 1,000 kcal | ≥4.3 oz equiv. per 1,000 kcal |
| Sodium | 10 | ≤1.1 gram per 1,000 kcal | ≥2.0 grams per 1,000 kcal |
| Empty Calories9 | 20 | ≤19% of energy | ≥50% of energy |
| HEI-200510 | |||
| Adequacy: | |||
| Total Fruit2 | 5 | ≥0.8 cup equiv. per 1 | No Fruit |
| Whole Fruit3 | 5 | ≥0.4 cup equiv. per 1 | No Whole Fruit |
| Total Vegetables4 | 5 | ≥1.1 cup equiv. per 1 | No Vegetables |
| Dark Green and Orange Vegetables and Legumes4 | 5 | ≥0.4 cup equiv. per 1 | No Dark Green or Orange Vegetables or Legumes |
| Total Grains | 5 | ≥3.0 oz equiv. per 1 | No Grains |
| Whole Grains | 5 | ≥1.5 oz equiv. per 1 | No Whole Grains |
| Milk5 | 10 | ≥1.3 cup equiv. per 1 | No Milk |
| Meat and Beans6 | 10 | ≥2.5 oz equiv. per 1 | No Meat or Beans |
| Oils11 | 10 | ≥12 grams per 1 | No Oil |
| Moderation: | |||
| Saturated Fat | 10 | ≤7% of energy12 | ≥15% of energy |
| Sodium | 10 | ≤0.7 gram per 1,000 kcal12 | ≥2.0 grams per 1,000 kcal |
| Calories from SoFAAS13 | 20 | ≤20% of energy | ≥50% of energy |
Intakes between the minimum and maximum standards are scored proportionately.
Includes fruit juice.
Includes all forms except juice.
Includes any beans and peas (called legumes in HEI-2005) not counted as Total Protein Foods (called Meat and Beans in HEI-2005).
Includes all milk products, such as fluid milk, yogurt, and cheese, and fortified soy beverages.
Beans and peas are included here (and not with vegetables) when the Total Protein Foods (called Meat and Beans in HEI-2005) standard is otherwise not met.
Includes seafood, nuts, seeds, soy products (other than beverages) as well as beans and peas counted as Total Protein Foods.
Ratio of poly- and monounsaturated fatty acids to saturated fatty acids.
Calories from solid fats, alcohol, and added sugars; threshold for counting alcohol is >13 grams/1000 kcal.
Intakes between the minimum and maximum standards are scored proportionately, except for Saturated Fat and Sodium (see note 12).
Includes non-hydrogenated vegetable oils and oils in fish, nuts, and seeds.
Saturated Fat and Sodium get a score of 8 for the intake levels that reflect the 2005 Dietary Guidelines, <10% of calories from saturated fat and 1.1 grams of sodium/1,000 kcal, respectively. Intakes between the standards for scores of 0 and 8 and between 8 and 10 are scored proportionately.
Calories from solid fats, alcoholic beverages, and added sugars.
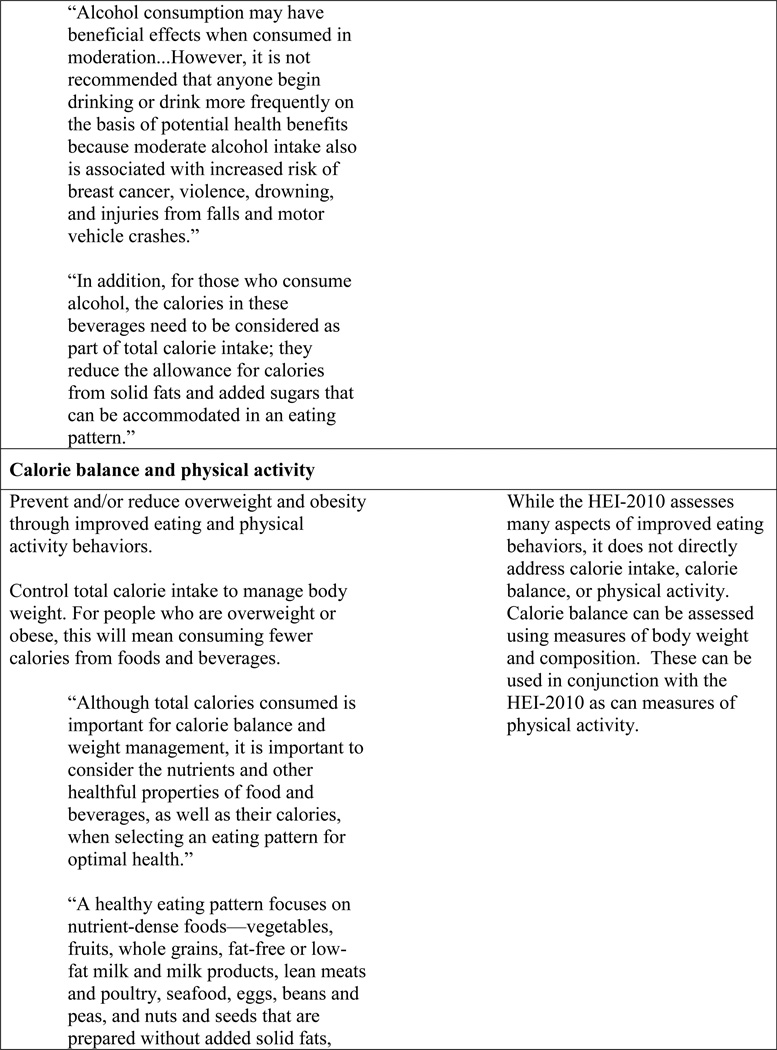
Figure 2.
Healthy Eating Index-2010 (HEI-2010) components mapped to the key dietary recommendations of the Dietary Guidelines for Americans, 20101
Figure 3.
Food groups and subgroups of the USDA Food Patterns, alcohol, and nutrients that contribute to the components of the Healthy Eating Index-2010. 1Includes all milk products, such as fluid milk, yogurt, and cheese, and fortified soy beverages. 2Fat is counted as solid fat. 3Includes nuts, seeds, and soy products (other than beverages). 4Included as a ratio of poly- and monounsaturated fatty acids to saturated fatty acids. 5Only alcohol beyond a moderate amount is considered to be empty calories.
The HEI-2005 component Calories from Solid Fats, Alcoholic Beverages, and Added Sugars has been modified slightly as described below and renamed Empty Calories, a more concise term used to convey this concept to consumers.5 A number of components were changed from the 2005 version: Greens and Beans replaced Dark Green and Orange Vegetables and Legumes; Seafood and Plant Proteins, which represents selected subgroups of protein foods, was introduced; Fatty Acids replaced two components, Saturated Fat and Oils; Refined Grains was added; and Total Grains was eliminated. These new components are described further below. Additional details regarding the differences between the 2005 and 2010 versions, including differences in maximum point values of the components and scoring standards are found in Table 1.
Greens and Beans
Of the five vegetable subgroups found in the 2010 USDA Food Patterns, dark green vegetables and beans and peas (also known as legumes) are the subgroups for which intakes are furthest from recommended levels.6, 7 The HEI-2010 captures these two subgroups as a single component called Greens and Beans. Orange vegetables were included in the vegetable subgroup component of the HEI-2005 (known as Dark Green and Orange Vegetables and Legumes) because they also were among those subgroups of vegetables for which average intakes were furthest from recommended levels. However, when the USDA Food Patterns were updated to reflect the 2010 Dietary Guidelines, the red vegetables were removed from the “other vegetables” subgroup and combined with the orange vegetables to create a new “red-orange” subgroup. Because tomatoes are so frequently consumed, intake of the new red-orange vegetable subgroup is not far from recommended levels; therefore, this subgroup is not included in the HEI-2010.
The standard for the maximum score of the Greens and Beans component is the sum of the least restrictive daily recommendations for those two subgroups of vegetables found in the USDA Food Patterns, expressed on a per 1,000 calorie basis. Any combination of dark green vegetables and beans and peas counts toward meeting the standard. However, when the Total Protein Foods standard is otherwise not met, beans and peas are first counted as protein foods; and only those beans and peas that are not needed to meet the Total Protein Foods standard are then counted toward Greens and Beans (and Total Vegetables) as illustrated in Figure 3. The reason for this is that although the USDA Food Patterns include beans and peas as part of both the vegetable and protein foods groups, they stipulate that they be counted in only one or the other of these groups.1, 8
Seafood and Plant Proteins
The 2010 Dietary Guidelines includes a new recommendation for seafood because of the many benefits it provides, including, but not limited to, its n-3 fatty acid content.1 It is recommended that seafood consumption be increased by replacing some meat and poultry. The Dietary Guidelines also highlight the benefits of vegetarian diets and, for the first time, include lacto-ovo vegetarian and vegan adaptations of the USDA Food Patterns. Both vegetarian diets and consumption of seafood are associated with reduced cardiovascular-related risks;1 therefore, plant proteins and seafood were combined into one component of the HEI-2010. The combination is consistent with the key feature of the HEI that no one food or commodity is required for a perfect score (Figure 1); if a component assessed seafood alone, it would prohibit vegetarian diets from earning a perfect score.
The standard for the maximum score of the Seafood and Plant Proteins component is the sum of the daily recommendations in the USDA Food Patterns for three subgroups of protein foods: seafood, nuts and seeds, and soy products, expressed on a per 1,000 calorie basis (see Figure 3). All seafood, nuts and seeds, and processed soy products (other than soy beverages, which are counted toward the Dairy component) count toward Seafood and Plant Proteins. In addition, any beans and peas that are counted toward the Total Protein Foods standard are counted toward the Seafood and Plant Proteins component.
Fatty Acids
The 2010 Dietary Guidelines state that the type of fat is more important than the total amount of fat and call for replacing saturated fatty acids with monounsaturated and polyunsaturated fatty acids. In the HEI-2010, the ratio of unsaturated fatty acids to saturated fatty acids is used to capture the concept of replacement and the relative balance of the two. This ratio has been used as part of another diet quality score.9
The Fatty Acids component is classified as an adequacy component to reflect the health benefits of poly- and monounsaturated fatty acids. In the USDA Food Patterns, the values of this ratio range from 2.5 to 2.6 among the various calorie levels.6, 10 The least restrictive value of 2.5 was chosen as the standard for the maximum score. The approach for setting the minimum score is described below. Because the Dietary Guidelines also include the DASH Eating Plan as an illustrative dietary pattern, the ratio of unsaturated to saturated fatty acids in the various diets used in the DASH trials was also reviewed. The achieved diets had ratios of 2.4 to 3.1, suggesting that 2.5 is a reasonable standard.11, 12
Refined Grains
Refined Grains is considered a moderation component because the 2010 Dietary Guidelines emphasize that consumption levels are too high. More than 95% of Americans age 2 and older consume more than the amounts recommended in the USDA
Food Patterns.7 The least restrictive of these recommendations, expressed per 1,000 calories, was selected as the standard for the maximum score of 10.
Empty Calories
The 2010 USDA Food Patterns include limits on calories from solid fats and added sugars but do not specifically mention limits on calories from alcohol. The Dietary Guidelines, on the other hand, note that calories from alcohol reduce the calories from solid fats and added sugars that can be accommodated; however, they also acknowledge that moderate drinking has beneficial effects. Therefore, in the HEI-2010, calories from alcohol are considered to be empty calories, but only when alcohol is consumed beyond moderate amounts. The least restrictive of the two levels defined as moderate drinking in the Dietary Guidelines, 2 drinks per day (converted to 28 grams of ethanol), was used to set the threshold for counting alcohol as empty calories. The same value that was used to energy-adjust sodium (2150 calories)3, 13, as described below, was used to energy-adjust the alcohol threshold. Because 28 g ethanol/2150 calories equals 13 g ethanol/1000 calories, up to 13 g of ethanol/1000 calories are not counted towards Empty Calories.
Scoring and Weighting
Assigning HEI-2010 scores to a set of foods requires translating them into amounts of food groups that are consistent with the USDA Food Patterns.6 Mixed foods are disaggregated (i.e., broken down into their ingredients), and any solid fats and added sugars are counted separately.
As noted above, the standards for assigning maximum scores are the least-restrictive recommendations among those that vary by energy level, sex and/or age group. For adequacy components, intakes at the level of the standard or higher receive the maximum number of points. For all adequacy components except Fatty Acids, zero intakes receive a score of zero (Table 1). The 15th percentile of the 2001–2002 population distribution of 1-day intakes was used to set the minimum score of zero for Fatty Acids, the only nutrient-based adequacy component. This was necessary because clear evidence on the level of intake that warrants a score of zero is not available. The methods and dataset used to estimate the 15th percentile are described in detail elsewhere.3, 14 Scores for intakes between the minimum and maximum standards are scored proportionately.
For the three moderation components, intakes at the level of the standard or lower receive the maximum number of points (Table 1). For sodium, the maximum score is assigned to diets that have less than 1,100 mg of sodium per 1,000 calories. This standard is based on the least restrictive of the two levels recommended in the Dietary Guidelines—2,300 mg and 1,500 mg—and was derived using the energy-adjustment factor of 2,300 mg of sodium per 2,150 calories. That standard was employed by the Institute of Medicine to set the Tolerable Upper Intake Levels for children and was based on the estimated median energy intake by adults.13
Compared to the food-based adequacy components, assigning a score of zero for the moderation components is more complicated for two reasons: (1) they are reverse scored, that is, higher intakes receive lower scores, and (2) no scientific evidence clearly specifies how high an intake deserves a score of zero. Consistent with the approach for the HEI-2005, a value at approximately the 85th percentile of the 2001–2002 population distribution of 1-day intakes is used for the minimum score of zero for these components (Table 1). The methods and dataset used to estimate the 85th percentile for each component are described in detail elsewhere.3, 14 As with the food-based adequacy components, scores for intakes between the minimum and maximum standards are scored proportionately.
The HEI-2010 components can be considered as a set of scores, each of which measures compliance with a different aspect of the Dietary Guidelines, and the component scores can be summed to derive a total score. The maximum number of points allocated to each component (Table 1) serves as a weighting factor when the component scores are summed. Most components are weighted equally at 10 points. Fruits, vegetables, and protein foods have two components (total and a subgroup) that are allotted 5 points each. Empty Calories is allotted 20 points because the added sugars, solid fats, and alcoholic beverages that make up this component contribute excess calories and may displace nutrient-dense foods from the diet.1
Estimating HEI-2010 Scores
Whether assessing diets or some aspect of the food environment, the basic steps for deriving HEI-2010 scores are the same: (1) identify the set of foods under consideration; (2) determine the amount of each relevant food group, subgroup, and nutrient in the set of foods; (3) derive the pertinent ratios; and (4) score each component using the appropriate standard.15 However, the ratios and scores can be estimated several ways, depending on the research question and type of data available.
For many applications, an estimate of the mean score for a population, subpopulation, or group is appropriate; and the population ratio method (i.e., the weighted ratio of means, rather than the weighted mean ratio) can be used.16 Major advances have been made in the development of statistical methods for estimating the distribution of scores at the population level for nutrition monitoring purposes and for determining the relationships between a multi-component dietary quality measure and health outcomes.17–22 Guidance on how to use the HEI-2010 in research, including SAS code and macros, is available online.23
Considerations for Interpretation of HEI-2010 Scores
This section describes several considerations relevant to the interpretation of HEI-2010 scores. These include nuances of design that relate to measurement issues, considerations of appropriateness for various groups, characteristics of some components that impact the meaning of scores, and relationships between diet quality and nutrient adequacy.
Density standards are useful not only because they allow common standards to be used, but also because they are independent of an individual’s energy requirement, which is difficult to measure with a reasonable degree of accuracy.3 The use of the least-restrictive standards results in the error being in the same direction (i.e., liberal or highest possible scores), which is advantageous for interpretation. Further, except for Total Protein Foods, very high component scores are rare in the United States, so choosing the least restrictive standard does not limit the range of scores appreciably.
The HEI-2010 is appropriate for all segments of the U.S. population to which the USDA Food Patterns apply, including women who are pregnant or lactating. It does not apply to children younger than 2 years of age or to older children who are consuming breast milk or infant formula.3 The HEI-2010 scoring system reflects the vegetarian and vegan versions of the USDA Foods Pattern as well as the omnivore version. Although the validity of the HEI-2010 has not been specifically determined for ethnic and cultural groups, it can be assumed to be valid for assessing the diets of subpopulations for which the Dietary Guidelines are appropriate because the mixed dishes and sauces that distinguish ethnic and cultural diets would be disaggregated into their ingredients and assigned to food groups which are generally culturally neutral.
The USDA Food Patterns note that beans and peas are considered both protein foods and vegetables and stipulate that they may be counted as only one or the other.1 Like the HEI-2005, the HEI-2010 counts only as many beans and peas toward Total Protein Foods as are needed to meet the standard. The HEI-2010 also counts this amount of beans and peas as Seafood and Plant Proteins. Any amount remaining after the Total Protein Foods standard is met is counted toward Total Vegetables (and Greens and Beans) (see Figure 3). Therefore, diets which include some beans and peas, but meet the Total Protein Foods standard without counting all of them, are likely to receive lower scores for Seafood and Plant Proteins than they would if all the beans and peas had been counted towards this component. Likewise, diets for which at least some beans and peas are used to meet the Total Protein Foods standard are likely to receive lower scores for Total Vegetables and Greens and Beans than they would if all beans and peas had been counted as vegetables.
The HEI-2010 considers alcohol above a threshold level indicative of moderate drinking as empty calories. This approach does not directly address other potential positive and negative biological effects of alcohol, nor does it account for specific questions related to frequency of consumption and amounts consumed on drinking occasions. When using the HEI-2010 to examine relationships between diet quality and health outcomes, additional considerations regarding alcohol may be warranted.22
The HEI-2010 is a measure of diet quality and does not address the appropriateness of energy intake and levels of physical activity, which together determine energy balance. Nonetheless, energy balance is a major focus of the 2010 Dietary Guidelines, and researchers are encouraged to use measures of energy balance and physical activity in conjunction with the HEI-2010.
For children over the age of 8 and adults, diets that have fewer than 1600 calories are less likely than higher calorie diets to be nutritionally adequate even if perfect scores are achieved on the adequacy components of the HEI-2010. The USDA Food Patterns are not designed to ensure nutrient adequacy for individuals over the age of 8 who have energy requirements below 1600 calories because it is difficult to meet their Recommended Dietary Allowances (RDAs) at such low energy levels.6 Furthermore, the USDA Food Patterns do not meet RDAs for vitamins D and E or Adequate Intakes for potassium and choline, so a perfect score on the HEI-2010 may not represent adequate intake of these nutrients to the same degree it does for other nutrients. On the other hand, the nutrient standards for USDA Food Patterns are based on the RDAs and Adequate Intakes, which are too high for assessment purposes.24 This limitation cannot be remedied until Estimated Average Requirements are available for all nutrients of concern.3
The sodium recommendations found in the Dietary Guidelines do not vary with energy intake level; 1 but, consistent with other components, the HEI-2010 sodium scoring standard is energy-adjusted. This standard (1.1 g/1000 calories) is more difficult to meet at lower energy levels than is the absolute limit (2300 mg) on which it is based. An energy-adjusted approach has been used by the Institute of Medicine,13 as mentioned above; and the sodium levels of the diets in the DASH trials were deliberately energy-adjusted,25, 26 lending support to this method.
Conclusions
The HEI-2010 is an updated tool for assessing diet quality as specified by the 2010 Dietary Guidelines for Americans. Like the HEI-2005, the HEI-2010 can be used to assess changes in diet quality over time;27 to examine the relationship between diet cost and diet quality;28, 29 to evaluate the diets of subpopulations,30–38 food environments,15, 39 menus,4, 40 foods provided through USDA nutrition assistance programs,41 and the efficacy of nutrition interventions;42 and to validate other tools.43–45 It can also be used in research to better understand relationships between nutrients, foods, and/or dietary patterns and health-related outcomes.46–67
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Patricia M. Guenther, Center for Nutrition Policy and Promotion U.S. Department of Agriculture 3101 Park Center Dr., Ste. 1034 Alexandria, VA 22302 Telephone: 703-605-0253 Fax:703-305-3300 Patricia.Guenther@cnpp.usda.gov.
Kellie O. Casavale, Office of Disease Prevention and Health Promotion U.S. Department of Health and Human Services 1101 Wootton Pkwy., Ste. LL100 Rockville, MD 20852 Telephone: 240-453-8252 Fax: 240-453-8281 Kellie.Casavale@hhs.gov.
Sharon I. Kirkpatrick, Risk Factor Monitoring and Methods Branch Applied Research Program Division of Cancer Control and Population Sciences National Cancer Institute 6130 Executive Blvd. MSC 7344 Bethesda, MD 20892-7344 Telephone: 301-435-1638 Fax: 301-465-3710 sharon.kirkpatrick@mail.nih.gov.
Jill Reedy, Risk Factor Monitoring and Methods Branch Applied Research Program Division of Cancer Control and Population Sciences National Cancer Institute 6130 Executive Blvd. MSC 7344 Bethesda, MD 20892-7344 Telephone: 301-496-8500 Fax: 301-465-3710 reedyj@mail.nih.gov.
Hazel A.B. Hiza, Center for Nutrition Policy and Promotion U.S. Department of Agriculture 3101 Park Center Dr., Ste. 1034 Alexandria, VA 22302 Telephone: 703-305-2979 Fax: 703-305-3300 hazel.hiza@cnpp.usda.gov.
Kevin J. Kuczynski, Center for Nutrition Policy and Promotion U.S. Department of Agriculture 3101 Park Center Dr., Ste. 1034 Alexandria, VA 22302 Telephone: 703-305-2153 Fax: 703-305-3300 kevin.kuczynski@cnpp.usda.gov.
Lisa L. Kahle, Information Management Services, Inc. 3901 Calverton Blvd, Suite 200 Calverton MD 20705 Telephone: 301-680-9770 Fax: 301-680-8304 kahlel@imsweb.com.
Susan M. Krebs-Smith, Applied Research Program Division of Cancer Control and Population Sciences National Cancer Institute 6130 Executive Blvd. MSC 7344 Bethesda, MD 20892-7344 Telephone: 301-496-8500 Fax: 301-465-3710 sk52r@nih.gov.
References
- 1.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: 2010. http://www.cnpp.usda.gov/dietaryguidelines.htm. [Google Scholar]
- 2.Reedy J, Krebs-Smith SM. A comparison of food-based recommendations and nutrient values of three food guides: USDA's MyPyramid, NHLBI's Dietary Approaches to Stop Hypertension Eating Plan, and Harvard's Healthy Eating Pyramid. J Am Diet Assoc. 2008;108(3):522–528. doi: 10.1016/j.jada.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1854–1864. doi: 10.1016/j.jada.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Agriculture Center for Nutrition Policy and Promotion. [Accessed September 29, 2011];What Are Empty Calories? http://www.choosemyplate.gov/weight-management-calories/calories/empty-calories.html.
- 6.Britten P, Cleveland LE, Koegel KL, Kuczynski KJ, Nickols-Richardson SM. Updated US Department of Agriculture Food Patterns meet goals of the 2010 Dietary Guidelines. J Acad Nutr Diet. 112(10):1648–1655. doi: 10.1016/j.jand.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 7.National Cancer Institute, Applied Research Program, Risk Factor Monitoring and Methods. [Accessed September 29, 2011];Usual dietary intakes: food intakes, US population. 2001–04 http://riskfactor.cancer.gov/diet/usualintakes/pop/#results.html.
- 8.U.S. Department of Agriculture Center for Nutrition Policy and Promotion. [Accessed March 8, 2012];Beans and peas are uniques foods. http://www.choosemyplate.gov/food-groups/vegetables-beans-peas.html.
- 9.Trichopoulou A, Orfanos P, Norat T, et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ. 2005;330(7498):991. doi: 10.1136/bmj.38415.644155.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Agriculture Center for Nutrition Policy and Promotion Web site. [Accessed April 10, 2012];Nutrients in 2010 USDA Food Patterns at all calorie levels. http://www.cnpp.usda.gov/Publications/USDAFoodPatterns/Nutrientsin2010USDAFoodPatternsatAllCalorieLevels.pdf.
- 11.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 12.Lin PH, Aickin M, Champagne C, et al. Food group sources of nutrients in the dietary patterns of the DASH-Sodium trial. J Am Diet Assoc. 2003;103(4):488–496. doi: 10.1053/jada.2003.50065. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 14.National Centers for Health Statistics. [Accessed March 8, 2012];National Health and Nutrition Examination Survey 2001–2002 public data general release file documentation. 2004 http://www.cdc.gov/nchs/data/nhanes/nhanes01_02/general_data_release_doc.pdf.
- 15.Reedy J, Krebs-Smith SM, Bosire C. Evaluating the food environment: application of the Healthy Eating Index-2005. Am J Prev Med. 2010;38(5):465–471. doi: 10.1016/j.amepre.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Freedman LS, Guenther PM, Krebs-Smith SM, Kott PS. A population's mean Healthy Eating Index-2005 scores are best estimated by the score of the population ratio when one 24-hour recall is available. J Nutr. 2008;138(9):1725–1729. doi: 10.1093/jn/138.9.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dodd KW, Guenther PM, Freedman LS, et al. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc. 2006;106(10):1640–1650. doi: 10.1016/j.jada.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Freedman LS, Guenther PM, Dodd KW, Krebs-Smith SM, Midthune D. The population distribution of ratios of usual intakes of dietary components that are consumed every day can be estimated from repeated 24-hour recalls. J Nutr. 2010;140(1):111–116. doi: 10.3945/jn.109.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freedman LS, Guenther PM, Krebs-Smith SM, Dodd KW, Midthune D. A population's distribution of Healthy Eating Index-2005 component scores can be estimated when more than one 24-hour recall is available. J Nutr. 2010;140(8):1529–1534. doi: 10.3945/jn.110.124594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kipnis V, Midthune D, Buckman DW, et al. Modeling data with excess zeros and measurement error: application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics. 2009;65(4):1003–1010. doi: 10.1111/j.1541-0420.2009.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29(27):2857–2868. doi: 10.1002/sim.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang S, Midthune D, Guenther PM, et al. A new multivariate measurement error model with zero-inflated dietary data, and its application to dietary assessment. Ann Appl Stat. 2011;5(2B):1456–1487. doi: 10.1214/10-AOAS446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Cancer Institute, Applied Research Program, Risk Factor Monitoring and Methods. [Accessed September 29, 2011];Healthy Eating Index-2010. http://riskfactor.cancer.gov/tools/hei.
- 24.Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes: Applications in Dietary Assessment. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 25.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 26.Svetkey LP, Sacks FM, Obarzanek E, et al. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-sodium): rationale and design. J Am Diet Assoc. 1999;99(8 Suppl):S96–104. doi: 10.1016/s0002-8223(99)00423-x. [DOI] [PubMed] [Google Scholar]
- 27.Juan WY, Guenther PM, Kott PS. Nutrition Insight 41. Alexandria, VA: United States Department of Agriculture Center for Nutrition Policy and Promotion; 2008. Diet quality of older Americans in 1994–96 and 2001–02 as measured by the Healthy Eating Index-2005. [Google Scholar]
- 28.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am J Clin Nutr. 2011;94(5):1333–1339. doi: 10.3945/ajcn.111.015560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ryden PJ, Hagfors L. Diet cost, diet quality and socio-economic position: how are they related and what contributes to differences in diet costs? Public Health Nutr. 2011;14(1680-92):1–13. doi: 10.1017/S1368980010003642. [DOI] [PubMed] [Google Scholar]
- 30.Guenther PM, Juan WY, Lino M, Hiza HA, Fungwe T, Lucas R. Nutrition Insight 42. Alexandria, VA: United States Department of Agriculture Center for Nutrition Policy and Promotion; 2008. Diet quality of low-income and higher income Americans in 2003–04 as measured by the Healthy Eating Index-2005. [Google Scholar]
- 31.Hiza HAB, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, gender, race/ethnicity, income and education level. Journal of the Academy of Nutrition and Dietetics. doi: 10.1016/j.jand.2012.08.011. In press. [DOI] [PubMed] [Google Scholar]
- 32.Breslow RA, Guenther PM, Juan W, Graubard BI. Alcoholic beverage consumption, nutrient intakes, and diet quality in the US adult population, 1999–2006. J Am Diet Assoc. 2010;110(4):551–562. doi: 10.1016/j.jada.2009.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mancino L, Todd J, Guthrie J, Lin B. How food away from home affects children's diet quality. ERR-104. US Department of Agriculture Economic Research Service; 2010. [Google Scholar]
- 34.Acar Tek N, Yildiran H, Akbulut G, et al. Evaluation of dietary quality of adolescents using Healthy Eating Index. Nutr Res Pract. 2011;5(4):322–328. doi: 10.4162/nrp.2011.5.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blake CE, Wethington E, Farrell TJ, Bisogni CA, Devine CM. Behavioral contexts, food-choice coping strategies, and dietary quality of a multiethnic sample of employed parents. J Am Diet Assoc. 2011;111(3):401–407. doi: 10.1016/j.jada.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duffy P, Zizza C, Jacoby J, Tayie FA. Diet quality is low among female food pantry clients in Eastern Alabama. J Nutr Educ Behav. 2009;41(6):414–419. doi: 10.1016/j.jneb.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 37.Zoellner J, You W, Connell C, et al. Health literacy is associated with Healthy Eating Index scores and sugar-sweetened beverage intake: findings from the rural lower Mississippi delta. J Am Diet Assoc. 2011;111(7):1012–1020. doi: 10.1016/j.jada.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Webber KH, Lee E. The diet quality of adult women participating in a behavioural weight-loss programme. J Hum Nutr Diet. 2011;24(4):360–369. doi: 10.1111/j.1365-277X.2011.01159.x. [DOI] [PubMed] [Google Scholar]
- 39.Krebs-Smith SM, Reedy J, Bosire C. Healthfulness of the U.S. food supply: little improvement despite decades of dietary guidance. Am J Prev Med. 2010;38(5):472–477. doi: 10.1016/j.amepre.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hornick BA, Krester AJ, Nicklas TA. Menu modeling with MyPyramid food patterns: incremental dietary changes lead to dramatic improvements in diet quality of menus. J Am Diet Assoc. 2008 Dec;108(12):2077–2083. doi: 10.1016/j.jada.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 41.US Department of Agriculture, Food and Nutrition Service, Office of Research and Analysis. Nutrient and MyPyramid analysis of USDA foods in five of its food and nutrition programs. 2012 Jan
- 42.Glanz K, Hersey J, Cates S, et al. Effect of a nutrient rich foods consumer education program: results from the Nutrition Advice Study. J Acad Nutr Diet. 2012;112(1):56–63. doi: 10.1016/j.jada.2011.08.031. [DOI] [PubMed] [Google Scholar]
- 43.Bailey RL, Miller PE, Mitchell DC, et al. Dietary screening tool identifies nutritional risk in older adults. Am J Clin Nutr. 2009;90(1):177–183. doi: 10.3945/ajcn.2008.27268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fulgoni VL, Keast DR, Drewnowski A. Development and validation of the Nutrient-rich Foods Index: a tool to measure nutritional quality of foods. J Nutr. 2009;139(8):1549–1554. doi: 10.3945/jn.108.101360. [DOI] [PubMed] [Google Scholar]
- 45.Rovner AJ, Nansel TR, Mehta SN, Higgins LA, Haynie DL, Laffel LM. Development and validation of the type1diabetes nutrition knowledge survey. Diabetes Care. 2012 doi: 10.2337/dc11-2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reedy J, Mitrou PN, Krebs-Smith SM, et al. Index-based dietary patterns and risk of colorectal cancer: the NIH-AARP Diet and Health Study. Am J Epidemiol. 2008;168(1):38–48. doi: 10.1093/aje/kwn097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller PE, Lazarus P, Lesko SM, et al. Diet index-based and empirically derived dietary patterns are associated with colorectal cancer risk. J Nutr. 2010;140(7):1267–1273. doi: 10.3945/jn.110.121780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hamidi M, Tarasuk V, Corey P, Cheung AM. Association between the Healthy Eating Index and bone turnover markers in US postmenopausal women aged >=45 y. Am J Clin Nutr. 2011;94(1):199–208. doi: 10.3945/ajcn.110.009605. [DOI] [PubMed] [Google Scholar]
- 50.Kuczmarski MF, Cremer Sees A, Hotchkiss L, Cotugna N, Evans MK, Zonderman AB. Higher Healthy Eating Index-2005 scores associated with reduced symptoms of depression in an urban population: findings from the Healthy Aging in Neighborhoods of Diversity Across the Life Span (HANDLS) study. J Am Diet Assoc. 2010;110(3):383–389. doi: 10.1016/j.jada.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shah BS, Freeland-Graves JH, Cahill JM, Lu H, Graves GR. Diet quality as measured by the Healthy Eating Index and the association with lipid profile in low-income women in early postpartum. J Am Diet Assoc. 2010;110(2):274–279. doi: 10.1016/j.jada.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 52.Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, Morris MC. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011;93(3):601–607. doi: 10.3945/ajcn.110.007369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Beydoun MA, Kuczmarski MT, Beydoun HA, et al. The sex-specific role of plasma folate in mediating the association of dietary quality with depressive symptoms. J Nutr. 2010;140(2):338–347. doi: 10.3945/jn.109.113878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Beydoun MA, Boueiz A, Shroff MR, Beydoun HA, Wang Y, Zonderman AB. Associations among 25-hydroxyvitamin D, diet quality, and metabolic disturbance differ by adiposity in adults in the United States. J Clin Endocrinol Metab. 2010;95(8):3814–3827. doi: 10.1210/jc.2010-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.de Koning L, Chiuve S, Fung TT, Willett WC, Rimm EB, Hu FB. Diet-quality scores and the risk of type 2 diabetes in men. Diabetes Care. 2011;34(5):1150–1156. doi: 10.2337/dc10-2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nicklas TA, O'Neil CE, Fulgoni VL. Diet quality is inversely related to cardiovascular risk factors in adults. J Nutr. 2012 Oct 17; doi: 10.3945/jn.112.164889. [DOI] [PubMed] [Google Scholar]
- 57.Huffman FG, De La Cera M, Vaccaro JA, et al. Healthy Eating Index and Alternate Healthy Eating Index among Haitian Americans and African Americans with and without Type 2 Diabetes. J Nutr Metab. 2011;2011:398324. doi: 10.1155/2011/398324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Agnoli C, Krogh V, Grioni S, et al. A priori-defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J Nutr. 2011;141(8):1552–1558. doi: 10.3945/jn.111.140061. [DOI] [PubMed] [Google Scholar]
- 59.Xu B, Houston DK, Locher JL, et al. Higher Healthy Eating Index-2005 scores are associated with better physical performance. J Gerontol A Biol Sci Med Sci. 2012;67(1):93–99. doi: 10.1093/gerona/glr159. [DOI] [PubMed] [Google Scholar]
- 60.Xu B, Houston D, Locher JL, Zizza C. The association between Healthy Eating Index-2005 scores and disability among older Americans. Age Ageing. 2012;41(3):365–371. doi: 10.1093/ageing/afr158. [DOI] [PubMed] [Google Scholar]
- 61.Mosher CE, Sloane R, Morey MC, et al. Associations between lifestyle factors and quality of life among older long-term breast, prostate, and colorectal cancer survivors. Cancer. 2009;115(17):4001–4009. doi: 10.1002/cncr.24436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Savoca MR, Arcury TA, Leng X, et al. Association between dietary quality of rural older adults and self-reported food avoidance and food modification due to oral health problems. J Am Geriatr Soc. 2010;58(7):1225–1232. doi: 10.1111/j.1532-5415.2010.02909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Savoca MR, Arcury TA, Leng X, et al. Severe tooth loss in older adults as a key indicator of compromised dietary quality. Public Health Nutr. 2010;13(4):466–474. doi: 10.1017/S1368980009991236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Y, Chen X. Between-group differences in nutrition-and health-related psychosocial factors among US adults and their associations with diet, exercise, and weight status. J Acad Nutr Diet. 2012;112(4):48–498. doi: 10.1016/j.jand.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tsigga M, Filis V, Hatzopoulou K, Kotzamanidis C, Grammatikopoulou MG. Healthy Eating Index during pregnancy according to pre-gravid and gravid weight status. Public Health Nutr. 2011;14(2):290–296. doi: 10.1017/S1368980010001989. [DOI] [PubMed] [Google Scholar]
- 66.Chen X, Cheskin LJ, Shi L, Wang Y. Americans with diet-related chronic diseases report higher diet quality than those without these diseases. J Nutr. 2011;141(8):1543–1551. doi: 10.3945/jn.111.140038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O'Neil CE, Nicklas TA, Rampersaud GC, Fulgoni VL. One hundred percent orange juice consumption is associated with better diet quality, improved nutrient adequacy, and no increased risk for overweight/obesity in children. Nutr Res. 2011;31(9):673–682. doi: 10.1016/j.nutres.2011.09.002. [DOI] [PubMed] [Google Scholar]