Abstract
Background and Purpose
To investigate relationships between the degree of early reperfusion achieved on PWI and clinical outcomes in the DEFUSE studies. We hypothesized that there would be a strong correlation between the degree of reperfusion achieved and clinical outcomes in Target mismatch (TMM) patients.
Methods
The degree of reperfusion was calculated based on the difference in PWI volumes (Tmax >6 sec) between the baseline MRI and the early post-treatment follow-up scan. Patients were grouped into quartiles, based on the degree of reperfusion achieved, and the association between the degree of reperfusion and clinical outcomes in TMM and no TMM patients was assessed. Favorable clinical response was determined at day 30 based on the NIHSS and good functional outcome was defined as a modified Rankin Scale score ≤2 at day 90.
Results
This study included 121 patients; 98 of these had TMM. The median degree of reperfusion achieved was not different in TMM patients (60%) vs. No TMM patients (64%) (p=0.604). The degree of reperfusion was strongly correlated with both favorable clinical response (p<0.001) and good functional outcome (p=0.001) in TMM patients; no correlation was present in No TMM. The frequency of achieving favorable clinical response or good functional outcome was significantly higher in TMM patients in the highest reperfusion quartile vs. the lower three quartiles (88% vs. 41% as OR 10.3; 95% CI; 2.8 – 37.5, and 75% vs. 34% as OR 5.9; 95% CI; 2.1 – 16.7, respectively). A receiver operating characteristic (ROC) curve analysis identified 90% as the optimal reperfusion threshold for predicting good functional outcomes.
Conclusion
The degree of reperfusion documented on PWI following reperfusion therapies corresponds closely with clinical outcomes in TMM patients. Reperfusion of 90% or more of the perfusion lesion is an appropriate goal for reperfusion therapies to aspire to.
Keywords: acute stroke, perfusion imaging, reperfusion, endovascular treatment
Introduction
Although angiographic recanalization has been associated with favorable outcomes in numerous acute stroke studies1–3, the association between the degree of reperfusion documented on MRI or CT perfusion imaging and clinical outcomes has only been assessed in a few studies4–6. Furthermore, there are very limited data to support the assertion that reperfusion is associated with favorable clinical outcomes only in the subgroup of patients with imaging based evidence of salvageable tissue7, 8. Perfusion imaging has the potential advantage over arterial recanalization in that it can assessing tissue level flow and provide a quantitative assessment of the volume of tissue that is reperfused.
Most studies that have assessed the relationship between reperfusion and outcomes by using MRI have dichotomized the degree of successful reperfusion into “reperfusion” vs. “no reperfusion” using an arbitrary threshold. This pre-specified threshold for “successful reperfusion” has varied substantially between studies. For example, 30% was used in DEFUSE 16, 50% in DEFUSE 29 and 90% in EPITHET4. It has been hypothesized that only patients with salvageable ischemic tissue are likely to benefit from early reperfusion and that patients without salvageable tissue do not8. The DEFUSE6, 9 and EPITHET4 studies have identified an MRI profile, Target Mismatch, that appears to identify patients who are particularly likely to have favorable clinical and radiographic responses in association with reperfusion.
In this study we investigate the relationship between the degree of early reperfusion achieved on PWI and clinical outcomes. We hypothesized that a strong correlation would exist between the degree of early reperfusion achieved and favorable clinical outcomes in Target mismatch patients (TMM) but that there would be no relationship in patients who do not have Target mismatch (No TMM). In addition, we explore if there is a reperfusion threshold that predicts favorable clinical outcomes in TMM patients with high specificity and good sensitivity.
Methods
This is a post-hoc analysis of the DEFUSE 1 and DEFUSE 2 studies. The design, methodology, and primary results of DEFUSE 16 and DEFUSE 29 have been reported. In DEFUSE 1, a baseline MRI scan was obtained immediately prior to treatment with intravenous tPA; the median time to treatment was 5.5 hours. A follow-up MRI was obtained to assess reperfusion (median 4.0 hours after iv tPA treatment). In DEFUSE 2, a baseline MRI scan was obtained just prior to endovascular therapy (median 6.0 hours between symptom onset and femoral puncture). A follow-up MRI was obtained to assess reperfusion (median 2.8 hours after endovascular treatment).
DWI and PWI volumes were obtained at the time of patient enrollment in DEFUSE 2 using an automated software program: RApid processing of Perfusion and Diffusion (RAPID)10. DEFUSE 1 imaging data were retrospectively analyzed using the same program. The methodology for reprocessing of DEFUSE 1 data with RAPID has been previously reported7. All imaging from DEFUSE 1 was performed on 1.5T MRI scanners; DEFUSE 2 utilized both 1.5T and 3T MRI systems.
The pre-specified Target Mismatch criteria from DEFUSE 2 were applied to both studies for this analysis: 1) a ratio between the volume of critically hypoperfused tissue and ischemic core ≥1.8, with an absolute difference ≥15 ml; 2) ischemic core volume <70 ml and; 3) volume of tissue with a severe delay (Tmax >10 sec) <100 ml. Patients with a baseline PWI (Tmax >6 sec) volume of less than 10 ml were excluded from this analysis because reperfusion could not be assessed in these small lesion patients. The volume of hypoperfusion on PWI (Tmax >6 sec) was assessed before and after the reperfusion treatment and the degree of reperfusion was determined as follows: [(baseline PWI volume – early follow up PWI volume) / baseline PWI volume]×100. Patients were grouped into quartiles according to the degree of reperfusion achieved and the association between the degree of reperfusion and clinical outcomes were assessed separately for patients with and without TMM.
The pre-specified primary and secondary clinical endpoints from the DEFUSE studies were used in this substudy. Favorable clinical response was defined as an improvement in the NIHSS of 8 or more points between baseline and day 30 or an NIHSS score ≤1 at day 30. Good functional outcome was defined as a modified Rankin Scale score ≤2 at day 90.
Using logistic regression analysis, we compared the baseline characteristics between these two cohort studies, and heterogeneity between the DEFUSE 1 and 2 results was assessed by examining the interaction term. Baseline predictors of favorable clinical outcome (age, DWI volume, PWI volume, and NIHSS) previously identified in the DEFUSE studies6, 9 were compared based on the degree of reperfusion obtained (in quartiles) to look for any imbalances in these predictors based on the degree of reperfusion achieved. We also calculated the OR for favorable clinical response and good functional outcome based on each 10% increase in the amount of reperfusion achieved in TMM patients. Adjustments for age and baseline DWI volume were performed in this logistic regression analysis because these variables have previously been shown to be independent predictors of clinical outcomes in the DEFUSE studies.
A receiver operating characteristic (ROC) curve analysis was performed to investigate the optimal reperfusion threshold for predicting favorable clinical outcomes and good functional outcomes in TMM patients. The “optimal threshold” was defined as the threshold produced by Youden Index to achieve highest sensitivity and specificity for predicting good outcome.
Continuous variables were compared with the Mann-Whitney U test (2 groups) or the Kruskal-Wallis test (more than 2 groups). The frequency of favorable clinical response and good functional outcome associated with the degree of reperfusion attained (by quartiles) were assessed using the Cochran-Armitage test for trend. We hypothesize that among TMM patients, the quartile with the highest degree of reperfusion would have greater odds of achieving favorable outcomes compared with the patients the lower three quartiles. All statistical tests were two-tailed and statistical significance was considered at an alpha level of less than 0.05. Statistical analyses were performed with IBM SPSS Statistics (version 20) and SAS/STAT software (version 9.3).
Results
Seventy-four patients were treated with tPA in DEFUSE 1 and endovascular therapy was attempted in 110 patients in DEFUSE 2. 14 patients with technically unsatisfactory baseline PWI scans and 30 patients (25 cases from DEFUSE 1, 5 cases from DEFUSE 2) with baseline PWI (Tmax >6 sec) volumes <10 ml were ineligible for inclusion. An additional 19 patients were excluded because the follow-up MRI was either not performed or technically unsatisfactory. Therefore, total of 121 patients were eligible for this substudy, and of these, 98 had TMM and 23 had No TMM. Clinical characteristics are summarized in table 1. DEFUSE 1 patients were older than DEFUSE 2 patients and hyperlipidemia was more common in DEFUSE 2. There were no statistical differences in baseline NIHSS scores or the timing of the MRI scans in relationship to symptom onset (Table 1).
Table 1.
Characteristics of eligible patients
| Baseline Characteristics | Combined (n=121) | DEFUSE 1 (n=34) | DEFUSE 2 (n=87) |
|---|---|---|---|
| Mean age ± SD * | 67 ± 16 | 75 ± 15 | 65 ± 15 |
| Female | 53% | 59% | 51% |
| Hypertension | 78 (65%) | 20 (59%) | 58 (67%) |
| Diabetes mellitus | 25 (21%) | 10 (29%) | 15 (17%) |
| Hyperlipidemia † | 57 (47%) | 9 (27%) | 48 (55%) |
| Current or past smoker | 53 (44%) | 13 (38%) | 40 (46%) |
| Atrial fibiliration | 41 (34%) | 10 (29%) | 31 (36%) |
| NIHSS baseline (median, IQR) | 14 (10 – 19) | 14 (10 – 17) | 16 (11 – 20) |
| Baseline DWI lesion volume, ml (median, IQR) | 15.2 (5.4 – 32.8) | 11 (2.9 – 25.5) | 16.8 (8.0 – 39.5) |
| Baseline PWI lesion volume, ml (median, IQR) | 81 (48.8 – 114.5) | 77.5 (40.3 – 90.0) | 87.1 (50.5 – 116.7) |
| Treated with iv tPA (%)* | 71 (59%) | 34 (100%) | 37 (43%) |
| Symptom onset to baseline MR, min (median, IQR) | 277 (194 – 321) | 284 (269 – 307) | 270 (162 – 354) |
| Symptom onset to iv tPA (DEFUSE 1 only), min (median, IQR) | 327 (309 – 350) | ||
| Symptom onset to femoral puncture (DEFUSE 2 only), min (median, IQR) | 357 (238 – 460) | ||
| Symptom onset to follow-up MRI, min (median, IQR) | 582 (478 – 701) | 575 (517 – 622) | 600 (418 – 733) |
| Target mismatch (%) | 98 (81%) | 29 (85%) | 69 (79%) |
| Degree of reperfusion obtained (median %, IQR) | 60.0 (15.5 – 95.3) | 60.3 (8.0 – 88.0) | 60.0 (17.0 – 95.5) |
| mRS at 90 days (median, IQR) | 3 (1 – 4) | 4 (2 – 4) | 3 (1 – 4) |
NIHSS =National Institutes of Health Stroke Scale; tPA =tissue plasminogen activator; mRS =modified Rankin Score.
p<0.001,
p=0.005
There was no significant difference in baseline predictors of outcome including age, baseline NIHSS, baseline DWI, or baseline PWI in the quartiles reflecting the degree of reperfusion achieved for either the TMM or No TMM patients (Table 2).
Table 2.
Baseline characteristics of TMM and No TMM patients
| 1st quartile | 2nd quartile | 3rd quartile | 4th quartile | p value* | |
|---|---|---|---|---|---|
| TMM (n=98) | n=25 | n=24 | n=25 | n=24 | |
| Age (years; mean, SD) | 65 (17) | 70 (15) | 71 (17) | 67 (15) | 0.510 |
| NIHSS baseline (median, IQR) | 13 (11 –19) | 17 (10.5 – 20) | 14 (9 – 21) | 12 (10 – 16) | 0.705 |
| Baseline DWI lesion volume, mL (median, IQR) | 7.7 (3.0 – 15.2) | 17.5 (8.8 – 27.5) | 13.5 (10.1 – 26.0) | 8.1 (4.9 – 14.5) | 0.095 |
| Baseline PWI lesion volume, mL (median, IQR) | 74.5 (38.4 – 89.2) | 90.4 (50.6 – 115.2) | 87.1 (60.3 – 107.5) | 73.3 (56.4 – 101.4) | 0.172 |
| No TMM (n=23) | n=6 | n=6 | n=5 | n=6 | |
| Age (years; mean, SD) | 67 (17) | 58 (13) | 65 (19) | 71 (12) | 0.522 |
| NIHSS baseline (median, IQR) | 17 (13 – 18) | 18.5 (18–19) | 17 (13.5 –19) | 19.5 (12 – 25) | 0.515 |
| Baseline DWI lesion volume, mL (median, IQR) | 43 (2 – 92) | 55.1 (19.6 –65.3) | 45.4 (27.7 – 91.3) | 79.0 (47 – 100.9) | 0.548 |
| Baseline PWI lesion volume, mL (median, IQR) | 83.2 (21.8 – 167.5) | 122.5 (76.9 – 134.2) | 73.7 (52.9 – 170.3) | 183.7 (37 – 206.9) | 0.536 |
Kruskal-Wallis test
Quartiles are based on degree of reperfusion achieved; 1st quartile reflects the lowest degree of reperfusion, 4th quartile reflects the highest
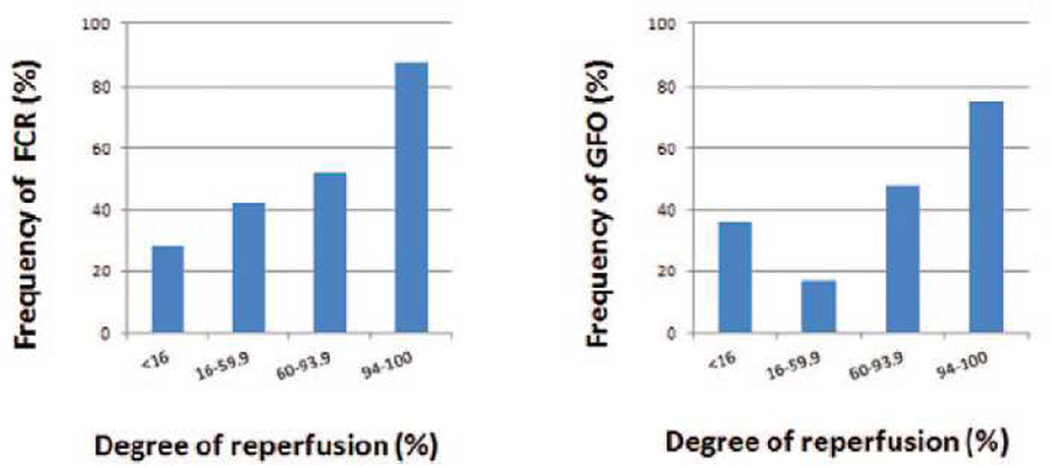
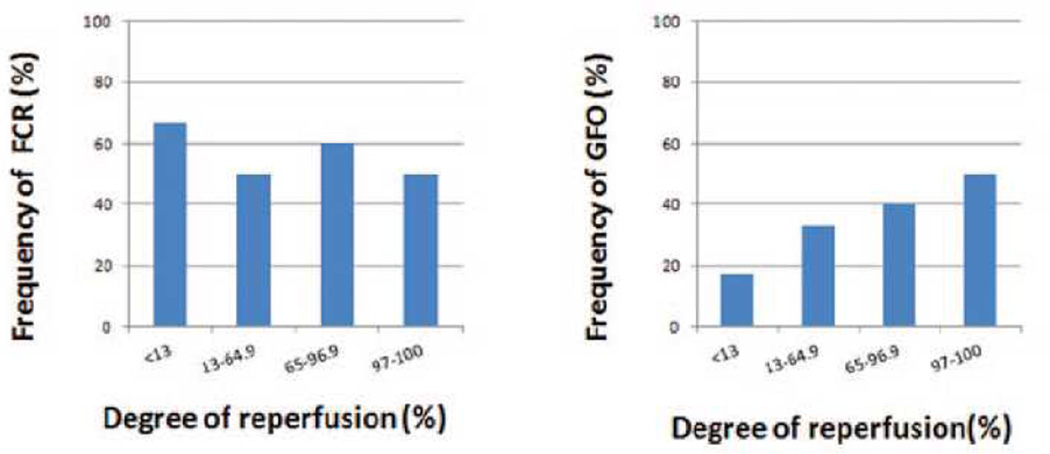
The median degree of reperfusion achieved did not differ between DEFUSE 1 and DEFUSE 2 (Table 1; p=0.936) or between TMM patients (median 59.7%; IQR 16.0 – 92.8) and No TMM patients (median 64.1%; IQR 13.6 – 96.9), p=0.604. The frequency of both favorable clinical response and good functional outcome was highly correlated with the degree of reperfusion (assessed by quartiles) (Cochran-Armitage test for trend: p<0.001, and p=0.001) for TMM patients (Figure 1), but no correlation was present in the No TMM patients. Twenty-eight percent of the TMM patients in the lowest reperfusion quartile (<16% reperfusion) had favorable clinical response compared with 42% in the 2nd quartile (16 – 59.9% reperfusion), 52% in the 3rd quartile (60 – 93.9% reperfusion), and 88% in the highest quartile (94 – 100% reperfusion) (Figure 1). In contrast, no significant relationship between the degree of reperfusion and either favorable clinical response or good functional outcome was present in the No TMM group (Figure 2).
Figure 1.
Association between degree of reperfusion achieved and clinical outcomes in 98 Target Mismatch patients and 23 No Target Mismatch patients. The Target Mismatch group had a statistically significant association (p<0.001 for Favorable clinical response, p=0.001 for Good functional outcome, p values are calculated by Cochran-Armitage test for trend).
Figure 2.
Association between degree of reperfusion achieved and clinical outcomes in 98 Target Mismatch patients and 23 No Target Mismatch patients. In the No Target Mismatch group there was no significant association (p=0.643 for Favorable clinical response, p=0.193 for Good functional outcome, p values are calculated by Cochran-Armitage test for trend).
As hypothesized, the frequency of favorable clinical response was significantly greater for the highest quartile of reperfusion compared with the three lower quartiles (88% vs. 41%, OR 10.3; 95% CI 2.8 – 37.5, p<0.001) in TMM patients. Similarly the percentage of TMM patients with good functional outcomes, was higher in the top quartile of reperfusion compared to the lower three quartiles (75% vs. 34% good functional outcome, OR 5.9; 95% CI 2.1 – 16.7, p<=0.001).
In the logistic regression analysis, the degree of reperfusion was an independent predictor of both good functional outcome and favorable clinical response (p<0.001) for TMM patients. After adjusting for independent predictors of outcome including age and DWI volume, each 10% increase in the degree of reperfusion had an OR of 1.3 (95% CI: 1.13 – 1.49) for favorable clinical response and 1.31 (95% CI: 1.14 – 1.50) for good functional outcome (Table 3).
Table 3.
Logistic Regression analysis
| Variable | p | OR | 95%CI | outcome |
|---|---|---|---|---|
| Age | 0.007 | 0.96 | 0.92–0.99 | favorable clinical response at 30 days |
| baseline DWI lesion | 0.014 | 0.96 | 0.93–0.99 | |
| reperfusion degree | <0.001 | 1.3 | 1.13–1.49 | |
| Age | <0.001 | 0.9 | 0.87–0.95 | good functional outcome at 90 days |
| baseline DWI lesion | 0.007 | 0.95 | 0.93–0.98 | |
| reperfusion degree | <0.001 | 1.31 | 1.14–1.50 |
OR indicates odds ratio adjusted for other variables in the model; DWI - diffusion-weighted magnetic resonance imaging.
Odds ratios for reperfusion degree are calculated for each 10% increase of reperfusion degree
n=98 all target mismatch patients with all 3 variables available were included in the multivariate analysis
The association between the degree of reperfusion achieved and favorable clinical response or good functional outcome for TMM patients in DEFUSE 1 vs. DEFUSE 2 was not different; there was no significant interaction between study group (DEFUSE 1 vs. DEFUSE 2) and reperfusion degree quartiles in the logistic regression analysis (p=0.379 for favorable clinical response, p=0.804 for good functional outcome). This analysis could not be performed in the No TMM cohort because of the small sample size in DEFUSE 1.
The ROC curve identified 87% and 90% as the optimal degree of reperfusion by Youden index for predicting favorable clinical outcomes in TMM patients: reperfusion of 87% of the hypoperfused Tmax >6 lesion had a sensitivity of 55% and specificity of 89% for predicting a favorable clinical response; 90% reperfusion had a 52% sensitivity and 87% specificity for predicting good functional outcome.
Discussion
The results of this study suggest that for patients with the TMM profile on baseline MRI, the degree of early reperfusion attained on PWI is strongly associated with the probability of achieving favorable clinical outcomes. No relationship between the degree of reperfusion and clinical outcomes was apparent in No TMM patients. Furthermore, the TMM patients who had complete or nearly complete reperfusion (the highest quartile of reperfusion, 94 – 100%) had substantially better outcomes than patients who achieved lesser degrees of reperfusion. The ROC analysis identified 90% as the optimal degree of reperfusion to predict good functional outcome with high specificity and good sensitivity. Target mismatch patients who achieved this high degree of reperfusion had exceptional clinical outcomes, including favorable clinical response frequency of nearly 90% and a Rankin 0–2 rate at 90 days of approximately 75%. Therefore, obtaining reperfusion of 90% or more of the perfusion lesion may be an appropriate benchmark for reperfusion therapies to aspire to.
Most previous studies that have assessed the relationship between the degree of reperfusion and clinical outcomes have used angiographic approaches, such as TICI scores2,3,11, to assess recanalization/reperfusion. These studies have typically demonstrated that patients with reperfusion have better clinical outcomes than patients with no reperfusion12,13. In the recent IMS 314 trial, the frequency of good functional outcome (mRS 0–2) in the endovascular group correlated strongly with the degree of reperfusion obtained on the TICI score (P<0.001), however, even among patients with a TICI score of 2b (reperfusion of 50–99% of the vascular distribution of the occluded artery), only 48% had good functional outcome.
Assessing reperfusion with perfusion imaging has some advantages over angiographic assessments at the end of the endovascular procedure. Recanalization of an arterial occlusion does not necessarily result in capillary reperfusion because of the no-reflow phenomenon and tissue reperfusion can occur despite lack of angiographic recanalization via recruitment of collateral flow. Furthermore, assessing reperfusion after completion of the procedure allows for visualization of perfusion changes that occur shortly after completion of the procedure (such as reperfusion related to administration of intra-arterial thrombolytic or improved collaterals).
Our study has some limitations. DEFUSE 1 and 2 used different therapeutic approaches to reperfusion; iv tPA alone in the DEFUSE 1 study, and endovascular therapy (often after initial iv tPA treatment) in the DEFUSE 2 study. Despite this, the studies did not differ in the degree of reperfusion attained and the relationship between the degree of reperfusion and clinical outcomes in TMM patients was consistent between studies. Furthermore, the multivariate analysis demonstrated that the degree of reperfusion achieved was an independent predictor of clinical outcomes in TMM patients. There were relatively few No TMM patients enrolled in the DEFUSE studies. Therefore, studies with larger numbers of No TMM patients are required to clarify the association between reperfusion and clinical outcomes in these patients.
The frequency of favorable clinical response did not correlate well with the frequency of good functional outcome in the No TMM group. This may be due to the small number of patients or the fact that an 8-point improvement in NIHSS score is often inadequate to produce a non-disabled outcome in patients with a high baseline NIHSS score.
We believe the current study is the first to report the association between the degree of PWI-documented reperfusion and clinical outcomes. We demonstrate that TMM patients who achieved complete or nearly complete reperfusion had exceptional clinical outcomes. Furthermore, every 10% of additional reperfusion achieved in TMM patients was associated with a 30% increase in the odds of favorable clinical response and a 31% increase in good functional outcome. The contrasting results of this study for TMM vs. No TMM patients suggest that optimizing patient selection for reperfusion therapies is likely to have an important effect on the clinical outcomes of these interventions.
Acknowledgments
Sources of Funding
The DEFUSE study was supported by the NIH (National Institute on Neurological Disorders and Stroke, RO1 NS39325, G.W.A.; K24 NS044848, G.W.A.).
The DEFUSE 2 study was funded by grants from the National Institute for Neurological Disorders and Stroke (R01 NS03932505 to GWA, K23 NS051372 to MGL).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Dr Albers has served as a consultant for Covidien, Codman, Lundbeck and Genentech and was the Chair of the DSMB for TREVO 2 (Concentric). Drs. Bammer and Albers have equity interest in iSchemaView.
References
- 1.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: A meta-analysis. Stroke. 2007;38:967–973. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the merci retriever in patients with acute ischaemic stroke (SWIFT): A randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–1249. doi: 10.1016/S0140-6736(12)61384-1. [DOI] [PubMed] [Google Scholar]
- 3.Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): A randomised trial. Lancet. 2012;380:1231–1240. doi: 10.1016/S0140-6736(12)61299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis SM, Donnan GA, Parsons MW, Levi C, Butcher KS, Peeters A, et al. Effects of alteplase beyond 3 h after stroke in the echoplanar imaging thrombolytic evaluation trial (EPITHET): A placebo-controlled randomised trial. Lancet Neurol. 2008;7:299–309. doi: 10.1016/S1474-4422(08)70044-9. [DOI] [PubMed] [Google Scholar]
- 5.Parsons M, Spratt N, Bivard A, Campbell B, Chung K, Miteff F, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Engl J Med. 2012;366:1099–1107. doi: 10.1056/NEJMoa1109842. [DOI] [PubMed] [Google Scholar]
- 6.Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: The diffusion and perfusion imaging evaluation for understanding stroke evolution (defuse) study. Ann Neurol. 2006;60:508–517. doi: 10.1002/ana.20976. [DOI] [PubMed] [Google Scholar]
- 7.Lansberg MG, Lee J, Christensen S, Straka M, De Silva DA, Mlynash M, et al. Rapid automated patient selection for reperfusion therapy: A pooled analysis of the echoplanar imaging thrombolytic evaluation trial (EPITHET) and the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Stroke. 2011;42:1608–1614. doi: 10.1161/STROKEAHA.110.609008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher M, Albers GW. Advanced imaging to extend the therapeutic time window of acute ischemic stroke. Ann Neurol. 2013;73:4–9. doi: 10.1002/ana.23744. [DOI] [PubMed] [Google Scholar]
- 9.Lansberg MG, Straka M, Kemp S, Mlynash M, Wechsler LR, Jovin TG, et al. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): A prospective cohort study. Lancet Neurol. 2012;11:860–867. doi: 10.1016/S1474-4422(12)70203-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Straka M, Albers GW, Bammer R. Real-time diffusion-perfusion mismatch analysis in acute stroke. J Magn Reson Imaging. 2010;32:1024–1037. doi: 10.1002/jmri.22338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34:e109–e137. doi: 10.1161/01.STR.0000082721.62796.09. [DOI] [PubMed] [Google Scholar]
- 12.Khatri P, Neff J, Broderick JP, Khoury JC, Carrozzella J, Tomsick T. Revascularization end points in stroke interventional trials: Recanalization versus reperfusion in ims-i. Stroke. 2005;36:2400–2403. doi: 10.1161/01.STR.0000185698.45720.58. [DOI] [PubMed] [Google Scholar]
- 13.The interventional management of stroke (ims) ii study. Stroke. 2007;38:2127–2135. doi: 10.1161/STROKEAHA.107.483131. [DOI] [PubMed] [Google Scholar]
- 14.Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-pa versus t-pa alone for stroke. N Engl J Med. 2013;368:893–903. doi: 10.1056/NEJMoa1214300. [DOI] [PMC free article] [PubMed] [Google Scholar]