Abstract
In this 2 part series, analysis of the risk stratification tools that are available and definition of the scope of the problem and potential solutions through a review of the literature is presented. A systematic review was used to identify articles for risk stratification and interventions. Three risk stratification systems are discussed, STRATIFY, Morse Fall Scale, and the Hendrich Fall Risk Model (HFRM). Of these scoring systems, the HFRM is the easiest to use and score. Predominantly, multifactorial interventions are used to prevent patient falls. Education and rehabilitation are common themes in studies with statistically significant results. The second article presents a guide to implementing a quality improvement project around hospital falls. A 10-step approach to Plan-Do-Study-Act (PDSA) cycles is described. Specific examples of problems and analysis are easily applicable to any institution. Furthermore, the sustainability of interventions and targeting new areas for improvement are discussed. Although specific to falls in the hospitalized patient, the goal is to present a stepwise approach that is broadly applicable to other areas requiring quality improvement.
Keywords: accidental falls, inpatient, quality improvement
Introduction
A stepwise approach to decreasing inpatient falls is proposed. Because such projects by necessity require support from the hospital administration, a methodology of determining institutional return on investment (ROI) is presented as well. By following a rigorous process during the planning and implementation phases of a project, one is well positioned to assess the impact of the interventions. Finally, one may decide to expand the scope of the project beyond a pilot while at the same time assuring maintenance of the new, improved baseline. With this skillset, the neurohospitalist has the ability to improve patient care as well as hospital finances and further validate the role of the inpatient specialist.
Implementation of Quality Improvement Principles to Hospital Falls
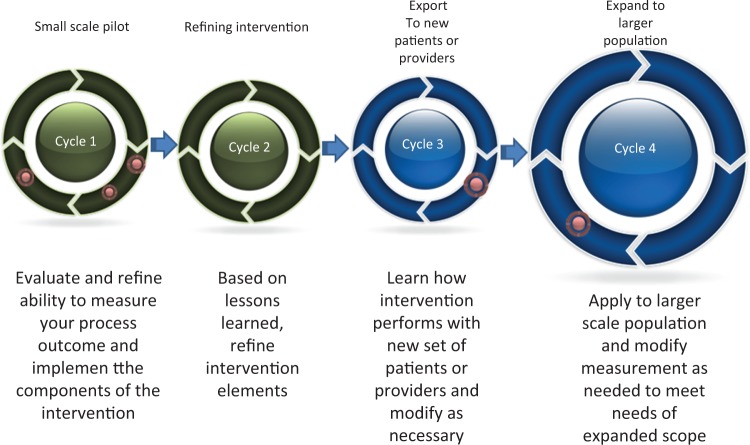
Randomized trials demonstrate that hospital falls are a modifiable hazard of hospitalization. The following is a step-by-step framework (Figure 1) for the translation of this research into action. With the patient experience paramount, the goal is reduction in fall-related patient harm while maximizing safe mobility. Additional benefits can include building interdisciplinary team collaboration within the institution, advancing the culture of safety, and cost savings by reducing expenditure on treatment of preventable injuries.
Figure 1.
Applying PDSA cycles.
Step 1: Assemble the QI Team
Falls are multifactorial and no individual provider is likely to be able to create significant and lasting impact on fall-related harms acting in isolation. Effective fall reduction will require system change and interprofessional collaboration. As such, the quality improvement (QI) team will also require a diverse multidisciplinary composition.1 The team will benefit from a project leader with credibility, interpersonal skills, and sufficient time devoted to the project to be effective in the role.2 An active champion in the team from both nursing and physician disciplines is highly desirable. Given that major risk factors for falls include weakness, gait instability, and problematic medications, the QI team may also benefit from representation from therapy and pharmacy. The core implementation team will need to be small enough to be manageable and meet regularly. Teams of at least 5 and not more than 15 are recommended.3 Additional content experts, departmental, or unit-based champions can be involved in an as-needed basis and updated regularly on the project’s progress. Early in the project a timeline for meetings and means of intrateam communication will need to be established.
Engagement by the hospital’s quality and patient safety department is advisable as the project will require the ability to access hospital adverse event reporting systems (ERSs) and receive regular reports on falls. Advanced statistics support is not required for implementation of most fall reduction programs but a data analyst with ability to generate run charts or control charts is necessary. Finally, change management may meet resistance. A sponsor from the executive team of the hospital can provide the team resources and authority necessary to overcome obstacles.4 Diversity of backgrounds within the team contributes to innovation. A high degree of connectivity of team members to the clinicians the project is attempting to influence facilitates dissemination of interventions.3
Step 2: Establish Reporting of Metrics
Establish the core metric which will be tracked. The overarching goal of the project is to reduce fall-related injuries. As falls with injury are relatively rare, the project will also need to examine all hospital falls regardless of whether they resulted in adverse outcomes. Raw number of falls or number of falling patients may be misleading if census is subject to variation. A number of metrics for falls can be used to track the impact of the QI program such as proportion of patients who fell, proportion of patients having fall-related injury, falls per 1000 patient bed days (fall rate), or falls with injury per 1000 patient bed days (fall injury rate).5 Fall rate and fall injury rate are excellent metrics used in most rigorous studies for monitoring change in falls over time, and between control and intervention units.5–10 They are insensitive to variability in census or length of stay, allow comparison between dissimilar units, and reflect accurately the contribution of repeat fallers to overall fall rates.
For the project to be effective, data reporting on falls will be needed on an ongoing basis, usually monthly. Short intervals between fall events and reflection of this in the data available are advantageous to allow evaluation of rapid improvement cycles. Hospitals have voluntary adverse incident reporting systems that will generally form the basis for the fall rate reports although evidence suggests such adverse events are underreported to these databases.11 More detailed “post-fall huddle” forms or in-depth root cause analyses/sentinel event investigations of individual falls can supplement the standardized reporting structure by providing details and narrative description of falls (see In-Depth Fall Analysis).
It may be advantageous to separate out subsets of falls (assisted vs unassisted) or fallers (first time vs repeat fallers, by unit or service, etc). Subgroup reporting capability may assist in understanding the impact of the intervention but can be overwhelming if too many reports are being reviewed simultaneously. The team may select to do subgroup analysis as an intermittent snapshot to answer a specific question about where to focus energy or resources or to adapt intervention to a new population within the hospital.
Inclusion and exclusion criteria represent a second important decision. Standardized and widely understood criteria will be needed to determine whether an event qualifies as a fall or a fall-related injury. The World Health Organization definition of a fall includes any unintentional descent to the ground, floor, or other lower level.12 Some of the published literature limits analysis to patients who reach the floor or only falls with “potential for injury.”7–9 Lack of consistency in which events the hospital staff would report to hospital fall reporting systems has been identified in the literature as creating barriers to effective QI.13 Inconsistency in reporting also introduces a bias to the data collection if the educational component of the fall reduction program induces falls to be reported which were not represented in the baseline data. The definition for what qualifies as a fall or injury should be consistent with the institutions reporting criteria and should not be changed once the project begins.
Estimate ROI
The project is designed to decrease injury rates and thereby could reduce institutional cost as a result of hospital fall-related trauma care, extra length of stay as a result of injuries, staff injuries associated with patient falls, and malpractice litigation. The ROI calculates the impact of the project on the financial performance of the hospital. Estimates of project ROI can be used to justify expenditures associated with implementation. According to 1 study, patients who fall with serious injury cost $13 806 more in total operating cost to the hospital compared to matched patients who do not fall.14 This does not account for indirect cost such as malpractice liability or staff injury related to patient falls. A meta-analysis of multidisciplinary fall prevention interventions in the acute care setting estimated reduction in fall rates by 10% (although data on reduction of serious injuries is lacking).15 Hospital baseline fall rates range from 2 to 10 per 1000 patient bed days.15 Serious injury results from 2% to 9% of falls.14 Using the fall rate and serious fall-related injury rate from within your institution and the estimated cost of resources used for the fall-reduction program this data can be used to calculate the estimated ROI for this project.
Example:
Assumptions: cost of fall with serious injury $13 806, approximately 5% of the falls lead to serious injury. The QI fall reduction projects can reduce this by 10%.
A 300-bed hospital has a fall rate of 5.91/1000 patient bed days over the last 12 months. The 300 beds and 80% occupancy over 365 days equals 87 600 patient bed days each year in the hospital.
Estimated rate of serious injuries: 5.91 × 5% = 0.3 per 1000 patient bed days.
A 10% reduction reduces fall rate to 5.3 and serious injury rate to 0.27 per 1000 patient bed days.
Cost savings = 0.03 less serious injuries per 1000 patient bed days × 87 600 patient bed days in a year × $13 806 per serious injury = $36 282
If project costs are $4500 for upgrade of EMR to include fall assessment field with automated triggers, staff education time, gait belts, and ambulation aids for all high-risk patients.
ROI = ($36 282 − $4500)/$4500 = 7.06 in the first year.
Step 3: Tracking Change
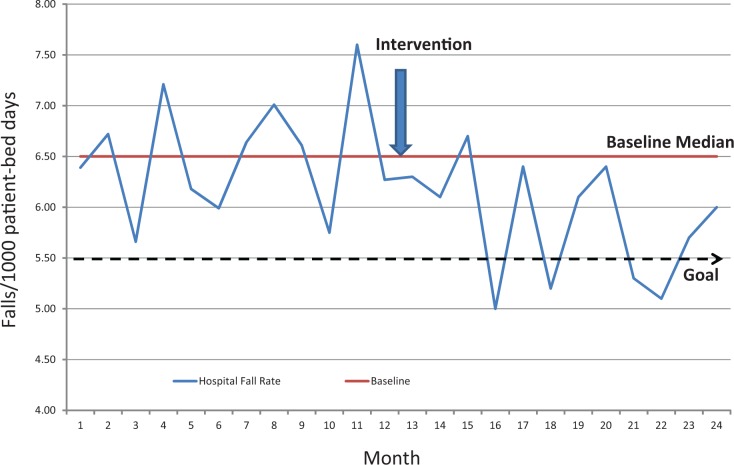
An effective means of graphically representing change in fall rates over time is the run chart. In its simplest form, this is a graph with the x-axis representing time and the y-axis representing fall rate (Figure 2). Each data point represents the fall rate over the selected time interval (month) for the population. Calculate the median rate from the time period before starting new interventions and put this in the chart as the baseline.
Figure 2.
Hospital fall rates.
The run chart allows rapid visual assessment as to whether the process is stable and the impact of new interventions. Statistical process control methods are beyond the scope of this article but the simple run chart is a powerful tool for monitoring response to change in an outcome such as falls over time.16
Balancing Measures
The third law of Newtonian physics posits that for every action there is an equal and opposite reaction. The corollary in QI is for each initiative designed to improve a given metric there is a tendency for unintended consequence on an unmeasured variable. Balancing measures attempt to control for this by explicitly monitoring the factors most likely to be adversely impacted by the project. For fall reduction projects, consider measuring effect on nursing staff time, staffing ratios on budget, or changes in patient mobility as a result of the initiative. Consider getting input from patients before and after the intervention. The ultimate recipients of the fall reduction initiative are the patients and it is worth considering their input and feedback throughout the project.
Step 4: Analyze Institution-Specific Circumstances and Risk Factors for Falls
It is wise to avoid the misstep of jumping to a solution before the institution-specific problem has been examined fully. Often from the institutional fall incident reporting database more detailed composite information can be obtained about the circumstances and risk factors surrounding falls. The following information is relevant in individualizing which elements of interventions demonstrated effective in the literature are of greatest yield when applied to a specific unit or institution.
Demographics of the patients who falls in the study area (medical diagnoses, age, gender, and service).
Circumstances surrounding the fall (ambulation, toileting, from bed, from chair, and time of day or night).
Risk factors (prior falls, medications, baseline leg weakness, gait abnormality, cognitive impairment, and incontinence).
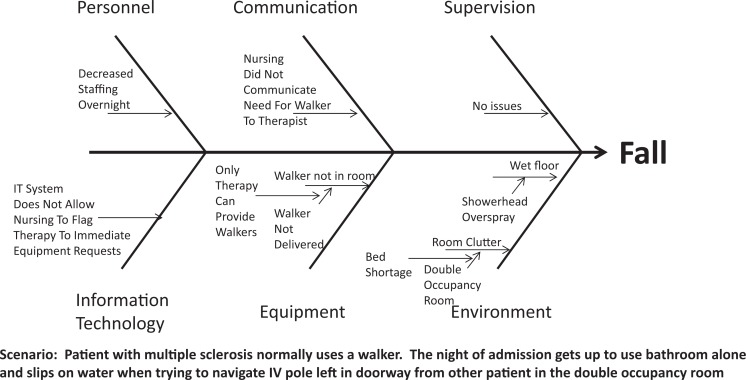
In-Depth Fall Analysis
Consider creation of a cause and effect (fishbone, Figure 3) diagram to examine factors contributing to falls. For a specific fall, examine all the contributors from different categories (examples include personnel, communication, supervision, information technology, environment, and equipment). For each identified contributor ask “why” to get at underlying factors. As an example, for a patient who fell in the bathroom, do not stop at “staff did not remain with patients during toileting”. Ask “why”? Is it because staff are not expected to do this, do not know about expectations, tasks that pull them away which the institution has prioritized over fall reduction, inefficiencies resulting in insufficient staff time, or inadequate staff ratios for the complexity of the patients? For each underlying answer ask “why” to get at foundational contributors to falls in the institution.
Figure 3.
Cause and effect diagram (fishbone).
Step 5: Select Pilot Site for Intervention
Institutional culture is critical to the success of the pilot stage of a fall reduction project.17 This includes visible leadership commitment to patient safety and QI as it applies to falls. The fall reduction initiative must be perceived as having institutional priority and urgency.4 Importantly, frontline staff culture on the site of the initial pilot is also a key determinant of the project outcomes. At the pilot stage, this involves change in usual processes of care or work flow and a willingness to experiment with processes which, while supported by the literature, are new within that specific unit. Frontline support is essential. A unit which has a recognized problem with falls, a recent adverse outcome as a result of a fall-related injury, existing interprofessional teamwork structure, and/or prior positive experience with QI may make an ideal pilot site. A compelling patient case of preventable fall-related injury can be used to drive urgency for change. 18 The QI team should seek input and active participation of frontline staff in the design and implementation stages of the project.
Step 6. Determine Points of Leverage for Interventions
With input from frontline clinicians, points of intervention should be selected from those employed in successful programs described in the literature. Decide whether the elements will be applied to all patients, applied based on individual risk factors, or selected based on level of fall risk assessment. Look for mismatch between current practice and elements of evidence-based multifactorial interventions (see Table 1 from Inpatient Falls: Defining the Problem and Identifying Possible Solutions. Part I).
Step 7: Evaluate Adherence to Each Element of the Intervention
It is critically important in evaluating the impact of a multicomponent intervention to be able to assess adherence to the individual elements. Failure to demonstrate improvement can be attributed to ineffective intervention elements, incorrect application of intervention elements, or inadequate uptake of the element into practice. Plan to disseminate intervention through the pilot site, document staff education and competence, and assess adherence and correct utilization of intervention elements. This form of evaluation can be thought of as assessing “process measures.” Prior research identifies nonadherence as a reason for ineffective fall prevention programs7 and nonadherence to protocol in as much as 4 in 10 shifts.19 Problems with uptake or adherence to specific intervention elements can prompt small PDSA cycles of the process uptake itself.
Step 8: Study Impact of Changes
Examine the impact of new interventions on the overall rate of fall and fall-related injury rates. In general, if 5 consecutive data points are in a consistent trend or if 6 consecutive points are all shifted below the prior median then this represents a process alteration resulting in a significant change.16
Failure to demonstrate improvement in fall rates should prompt review of the data gathered to assess whether the interventions were targeted correctly, staff was properly trained in their use, and adherence to protocol was complete. Deficiencies in one of these measures can prompt a second cycle designed to address this failing. If these elements were performed adequately then this suggests need for additional or alternative intervention elements.
Step 9: Review Lesions Learned from First Cycle and Expand Scope or Scale of Project
If process change was effectively implemented and has resulted in an improvement in the fall rates, then it can be expanded to additional units and modified to be employed in units or patient populations different from the pilot site. Celebrate short-term wins but do not declare victory until the process has been expanded and sustained.4 In general, be cautious about scaling up more than 5-fold or in scaling up in both size and scope (fundamentally different population) at the same time. Recognize that an intervention which is effective on a neurologic rehabilitation unit may not translate to the workflow of a very different site such as a neurology intensive care unit. Consider an explicit cycle to expand to 5 additional sites within the hospital or to modify for efficacy in a different patient population. Once the rollout process has been solidified and the interventions have been refined to meet the needs of different patient populations then it is ready for incorporation hospital-wide.
Step 10: Maintain the New Baseline
One of the pitfalls of QI to avoid is to assume that an intervention, once proven effective, will remain effective without ongoing monitoring. Studies demonstrate the risk that an effective project will fail to be maintained.20 Staff turnover, competing priorities, and human forgetfulness will conspire to chip away at prior gains. Continue to track fall rates and monitor for regression. Quality should be considered a process and not an event.
Conclusion
A rigorous QI project has the potential to effect clinical change for a population of patients. These endeavors have financial implications for all components of the health care system. By taking a stepwise approach, one can assure this change and justify the effort in doing so. Inpatient falls are an area ripe for such intervention. Inpatient fall reduction may serve as an excellent demonstration project, harnessing the potential of the neurohospitalist model of care.
Footnotes
Authors’ Note: All authors have contributed substantively to the conception design and analysis, the drafting of the manuscript or critical revision for important intellectual content, and final approval of the version to be published.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Santana C, Curry L, Nembhard I, Berg D, Bradley E. Behaviors of successful interdisciplinary hospital quality improvement teams. J Hosp Med. 2011;6(9):501–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mills P, Weeks W. Characteristics of successful quality improvement teams: lessons from five collaborative projects in the VHA. Jt Comm J Qual Saf. 2004;30(3):152–162 [DOI] [PubMed] [Google Scholar]
- 3. Meltzer D, Chung J, Khalili P, et al. Exploring the use of social network methods in designing healthcare quality improvement teams. Soc Sci Med. 2010;71(6):1119–1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kotter J. Leading change: why transformation efforts fail. Harvard Buisness Rev. Jan 2007;1–10 [Google Scholar]
- 5. Brandis S. A collaborative occupational therapy and nursing approach to falls prevention in hospital inpatients. J Qual Clin Pract. 1999;19(4):215–220 [DOI] [PubMed] [Google Scholar]
- 6. Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA. 2010;304(17):1912–1918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schwendimann R, Bühler H, De Geest S, Milisen K. Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program. BMC Health Serv Res. June 2006;6:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krauss MJ, Tutlam N, Costantinou E, Johnson S, Jackson D, Fraser VJ. Intervention to prevent falls on the medical service in a teaching hospital. Infect Control Hosp Epidemiol. 2008;29(6):539–545 [DOI] [PubMed] [Google Scholar]
- 9. Mitchell A, Jones N. Striving to prevent falls in an acute care setting–action to enhance quality. J Clin Nurs. 1996;5(4):213–220 [DOI] [PubMed] [Google Scholar]
- 10. Williams TA, King G, Hill AM, et al. Evaluation of a falls prevention programme in an acute tertiary care hospital. J Clin Nurs. 2007;16(2):316–324 [DOI] [PubMed] [Google Scholar]
- 11. Classen D, Resar R, Griffin F, et al. "Global trigger tool" shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff. 2011;30(4):581–589 [DOI] [PubMed] [Google Scholar]
- 12. Kalache A, Fu D, Yoshida S. WHO Global Report on Falls Prevention in Older Age. France: World Health Organization;2007 [Google Scholar]
- 13. Haines T, Beradette M, Hons BP, Varghese P, Fleming J, Gray L. Inconsistency in classification and reporting of in-hospital falls. J Am Geriatr Soc. 2009;57(3):517–523 [DOI] [PubMed] [Google Scholar]
- 14. Wong C, Recktenwald A, Jones M, Waterman B, Bollini M, Cunagan C. The cost of serious fall-related injuries at three midwestern hospitals. Jt Comm J Qual Patient Saf. 2011;37(2):81–87 [DOI] [PubMed] [Google Scholar]
- 15. DiBardino D, Cohen E, Didwania A. Meta-analysis: multidisciplinary fall prevention strategies in the acute care inpatinet population. J Hosp Med. 2012;7(6):497–503 [DOI] [PubMed] [Google Scholar]
- 16. Perla R, Provost L, Murray S. The run chart: A simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf. 2011;20(1):46–51 [DOI] [PubMed] [Google Scholar]
- 17. Noble D, Lemer C, Stanton E. What has change management in industry got to do with improving patient safety? Postgrad Med J. 2011;87(1027):345–348 [DOI] [PubMed] [Google Scholar]
- 18. Varkey P, Antonio K. Change management for effective quality improvement: a primer. Am J Med Qual. 2010;25(4):268–273 [DOI] [PubMed] [Google Scholar]
- 19. Bakarich A, McMillan V, Prosser R. The effect of a nursing intervention on the incidence of older patient falls. Aust J Adv Nurs. 1997;15(1):26–31 [PubMed] [Google Scholar]
- 20. Dempsey J. Falls prevention revisited: a call for a new approach. J Clin Nurs. 2004;13(4):479–485 [DOI] [PubMed] [Google Scholar]