Abstract
In most shoulder conditions a loss of glenohumeral motion results in shoulder performance impairments. However, in the overhead athlete loss of glenohumeral internal rotation, termed glenohumeral internal rotation deficiency (GIRD), is a normal phenomenon that should be expected. Without a loss of glenohumeral internal rotation the overhead athlete will not have the requisite glenohumeral external rotation needed to throw a baseball at nearly 100 miles per hour, or serve a tennis ball at velocities of 120 miles per hour or more. Not all GIRD is pathologic.
The authors of this manuscript have defined two types of GIRD; one that is normal and one that is pathologic. Anatomical GIRD (aGIRD) is one that is normal in overhead athletes and is characterized by a loss of internal rotation of less than 18°‐20° with symmetrical total rotational motion (TROM) bilaterally. Pathologic GIRD (pGIRD) is when there is a loss of glenohumeral internal rotation greater than 18°‐20° with a corresponding loss of TROM greater than 5° when compared bilaterally. A more problematic motion restriction may be that of a loss of TROM in the glenohumeral joint. Recent evidence supports that a loss of TROM is predictive of future injury to the shoulder in professional athletes. Additionally, external rotation deficiency (ERD), the difference between external rotation (ER) of the throwing shoulder and the non‐throwing shoulder of less than 5°, may be another predictor of future shoulder injury and disability.
Level of Evidence:
5
Keywords: External rotation deficiency, glenohumeral internal rotation deficit, total rotation motion
INTRODUCTION
The series of articles titled “The Disabled Throwing Shoulder: Spectrum of Pathology”1–3 presented an overview of the known mechanics of the overhead throwing motion and described the relationship of mechanics to throwing injuries. One of the important concepts related to shoulder injury in the overhead athlete that was discussed in detail was the loss of shoulder motion, specifically named glenohumeral internal rotation deficit (GIRD). In the 10 years that followed, numerous articles have been published related to GIRD and its proposed deleterious effects on the throwing shoulder. Burkhart et al1–3 proposed that GIRD was at the core of many throwing injuries. The authors of this commentary believe that excessive GIRD can in some instances be problematic in the throwing shoulder, but it may be far less common than it commonly presented in the medical literature. The authors believe that GIRD, in isolation, is less of a potential problem than GIRD with concomitant TROM loss (compared to the non‐throwing shoulder). This clinical commentary will attempt to dispel some of the myths and concerns with losses of motion about the glenohumeral joint and describe methods to assess and treat this condition. Additionally recent findings related to the new concepts of TROM and external rotation deficiency (ERD) will be discussed.
The overhead throwing motion is used in many common competitive and recreational sporting activities. The fastest joint velocities experienced by the human body occur during this motion and extreme stresses are exerted upon the body with each throw/movement. During a baseball pitch, an athlete generates a tremendous demand on the glenohumeral joint as the shoulder internal rotation (IR) velocity peaks higher than 7,000 degrees per second, while rotational torque of around 70 Nm is exerted.4–6 To be successful at pitching, both high velocity and accuracy have to occur repetitively, without injury to the soft tissues that help stabilize and dynamically control the glenohumeral joint. It has been proposed that the high forces and torques placed upon the shoulder joint complex during throwing may contribute to the high injury rate in baseball.7–9 Additionally, the ability to throw at high velocities requires adaptations to occur within the athlete’s shoulder complex that are not typically seen in the non‐dominant side of throwers, or in the shoulders of non‐throwing individuals. One of these adaptations is the shift of motion that occurs in athletes who utilize the overhead throwing motion. For example, the throwing shoulder is typically able to externally rotate approximately 180°, the amount of glenohumeral range of motion (ROM) attained at the end of the cocking phase of throwing, in order to generate the high rotational forces needed to pitch a baseball.4 This unique characteristic of the overhead throwing motion has been consistently described in the literature as a gain in shoulder glenohumeral external rotation (ER) and a loss of shoulder glenohumeral IR.10–20 However, the ability to achieve the full 180° is achieved by the utilization of segments within the kinematic chain including the glenohumeral joint, scapulothoracic articulation, and extension of the segments of the spine. In pitchers, this shift in total arc of motion occurs despite the fact that the TROM (e.g., sum of ER + sum of IR) is equal bilaterally.11,13,18,19,21
MEASUREMENT TECHNIQUE
In order for the rehabilitation specialist to evaluate if a ROM gain or loss exists, a concerted effort must be made to use a reproducible measurement technique for examination of shoulder rotation motion. A detailed examination of shoulder and glenohumeral joint ROM as well as examination of the entire kinematic chain is key to a thorough evaluation of an overhead athlete. Measurement of several cardinal movements of the shoulder are important, however isolated glenohumeral joint IR, ER and TROM have significant clinical importance and will be discussed in greater length and detail.
Selective loss of IR shoulder motion on the dominant extremity has been consistently reported in patient populations as well as in overhead athletes such as elite tennis players13,22, professional and youth baseball pitchers,13,23,24,25 and softball players.25 Testing ROM of the shoulder can utilize a standard goniometric procedure or the use of a bubble inclinometer. When using the goniometer technique the fulcrum is placed over the olecranon process.
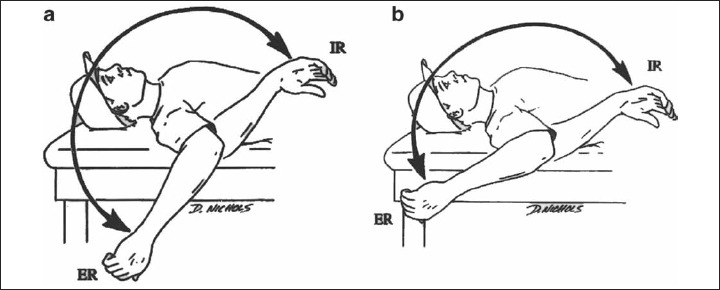
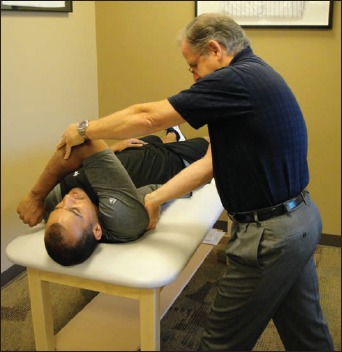
For assessment of shoulder IR, the patient should be placed supine with the shoulder at 90° of abduction in the plane of the scapula (10–15° anterior to the coronal plane) with the elbow flexed to 90°. To begin the forearm is placed vertically. The examiner then passively internally rotates the glenohumeral joint while maintaining stabilization of the scapula via gentle palpation of the coracoid process, to feel for motion, and minimize scapulothoracic contribution or compensatory movement which occurs at the end of IR motion. When the scapula begins to move into protraction and or anterior tilt, the measurement should be taken (Figure 1). A towel roll or consistent positioning by the clinicians supporting hand(s) is recommended to ensure that the humerus remains in the desired position throughout the measurement.
Figure 1.

Measurement of glenohumeral internal rotation with scapula stabilized.
Wilk et al26 has studied three methods of glenohumeral joint IR measurement (no stabilization, stabilization with hand on front of shoulder, and C‐shape stabilization with fingers posteriorly and thumb on coracoid process). The “C” shape type grasp with the four lesser fingers on the scapula posteriorly and the thumb on the coracoid anteriorly shown in figure 1 was the method of stabilization that produced the optimal amount of scapular stabilization and also proved reliable in both intra‐rater and inter‐rater applications. Again, the use of a consistent, reliable method for ROM measurements of IR and ER motion are a critical part of the complete evaluation of both the overhead athlete and the general orthopedic patient with a shoulder condition.
For assessment of shoulder ER, the shoulder is typically placed in the scapular plane (10–15° anterior to the coronal plane) and abducted to 90 degrees during measurement. A towel roll or consistent positioning by the clinicians supporting hand(s) is recommended to ensure that the humerus remains in the desired position throughout the measurement. To start the forearm is placed vertical (perpendicular to the support surface). The examiner then passively externally rotates the humerus while maintaining stabilization of the scapula. End range of glenohumeral ER is determined when resistance to any further motion is felt and attempts to overcome the resistance causes a posterior tilt or retraction of the scapula.27 (Figure 2).
Figure 2.

Measurement of glenohumeral external rotation.
In addition to the careful attention to stabilization and positioning during rotational measurements, additional consideration is given to achievement/assignment of end position. Many studies have utilized active or passive range of motion (PROM) without overpressure to minimize the measurement error inherent when measuring PROM with overpressure at end ROM.13,25,26,28,29 The use of the force of gravity to consistently achieve a stable end point position is recommended to enhance reliability and provide a consistent measurement of humeral rotation.
The Link between GIRD & TROM & Shoulder Injuries
Wilk et al originally proposed the TROM concept, where the amount of ER and IR at 90° of abduction are added together and a TROM arc is determined (Figure 3).30 This concept of TROM is useful in order to understand the rotational adaptations that occur and give early evidence of potentially deleterious alterations in rotation motion.31 The authors reported the TROM in the throwing shoulders of professional baseball pitchers to be within 5° of the non‐throwing shoulder.24 Furthermore, it was suggested that a TROM arc outside the 5° range may be a contributing factor to shoulder injuries.
Figure 3.
a. Total range of motion (TROM) dominant shoulder, b. TROM, non‐dominant shoulder.
Pitchers whose TROM comparison was outside the 5° acceptable difference range exhibited a 2.5 times greater risk of sustaining a shoulder injury.23 Twenty‐nine of the 37 recorded injuries (78%) were sustained in throwers whose TROM was greater than 176°. Stretching to increase IR PROM, in an attempt to treat the GIRD, may result in an increase of TROM (greater than 176°) or outside the 5° acceptable window compared to the contralateral shoulder. This may lead to an increased risk of injury due to the increased demands on the dynamic and static stabilizers surrounding the glenohumeral joint. Most studies have shown that TROM should be symmetric in throwers, however the TROM of overhead athletes should not exceed 186° as an absolute number.31 Further research is needed to explore the relationships between TROM asymmetry and alterations and shoulder injuries. The authors believe TROM is a valuable assessment tool and an important component in PROM assessment of throwers shoulders. This should be incorporated in the thrower’s shoulder examination to determine if a ROM discrepancy is present in the athlete.
Recently, Wilk et al31 have introduced a concept referred to as external rotation deficiency (ERD). External rotation deficiency is defined as the difference between ER of the throwing shoulder and the non‐throwing shoulder of less than 5°. Therefore, when comparing a players’ ER PROM from side‐to‐side, an ER difference of greater than 5°is expected, and would indicate that a player’s ER gain on his throwing side is significant enough to contribute to the demands of throwing, specifically during the late‐cocking phase of the pitching motion. A pitcher with ER side‐to‐side difference of <5° may impart increased stresses on the static glenohumeral stabilizers, thereby contributing to an increased risk of injury over the career of the athlete. In an unpublished study examining this phenomenon, players with ERD demonstrated 2.3 times increased risk of sustaining a shoulder injury that required a stint on the disabled list, as compared to players without insufficient ER motion.32 Therefore, the authors believe TROM differences, especially where there is an insufficient ER PROM on the dominant side as compared to the non‐dominant side, may put the pitcher at a higher risk for injury.
Normative Data
Population specific normative data is an important consideration for the interpretation of ROM of the overhead athlete. As mentioned throughout this commentary, IR and ER PROM measures performed at 90° of glenohumeral joint abduction while in the scapular plane are an essential part of the evaluation of the overhead athlete. Combined, these measures create the TROM.23 Several key studies with large sport‐specific subject populations are presented here to provide a resource to enhance and facilitate the interpretation of ROM measures of the overhead athlete (Table 1).
Table 1.
Normative Range of Motion Measures for Overhead Athletes.
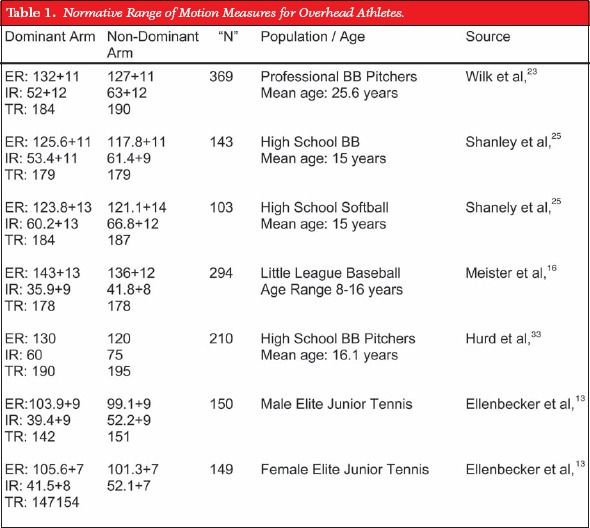 |
In general, studies involving baseball pitchers show nearly symmetric total rotation ROM profiles, characterized by increased dominant arm ER and decreased dominant arm IR.23,32,33 This has been reported at the professional level13,23,32 as well as in high school and developmental age players.16,25,33 TROM in these studies with very large samples sizes are typically within 5° when compared between the dominant and non‐dominant side. This is consistent with the recent recommendation of Wilk et al, as well as the authors of this commentary that TROM in the baseball pitcher should be within the 5° bilateral difference consistently reported in the literature.23,24,32
Ellenbecker et al, have reported decreases of 5–10° on average in the dominant arm TROM parameter in uninjured elite level tennis players (Table 1).13,28 These differences in TROM are slightly larger than those reported in professional and developmental age throwing athletes. Similarly, Reese et al34 reported decreases in dominant arm TROM in elite level volleyball players who were uninjured. These normative data profiles can assist clinicians in interpreting the actual ROM measures taken in the overhead athlete in these populations.
CURRENT RECOMMENDATIONS FOR INTERPRETING GIRD AND TROM DEFICITS
A threshold to determine what can be considered a clinically significant loss of IR is vitally important to the implementation of programs designed to prevent and treat glenohumeral motion loss. Although a popular focus of the thrower’s shoulder, GIRD is just one aspect of the evaluation of the overhead athlete. In order to most accurately determine clinically significant findings when designing treatment programs, TROM, ERD, and IR end feel must all be taken into consideration.
As previously discussed, a loss of IR itself can be considered a normal variation observed in asymptomatic overhead athletes. It should be stressed that GIRD is not specifically related to any single type of injury. Because GIRD or loss of IR ROM is a common finding in overhead athletes the authors would like to propose or name a second type of GIRD which is non‐pathologic. We would propose referring to this normal loss of IR alone, with adequate ER gain and TROM within 5° of the uninvolved side as an anatomical glenohumeral internal rotation deficit (a‐GIRD). Despite the documented presence of a‐GIRD among throwers, the term GIRD often has a negative connotation, implying that any side‐to‐side loss of IR may be pathological or may contribute to future injury. This has resulted in a trend towards assuming many of the hypothesized theories of loss of IR are present in each person and a standardized prescription of stretches and exercises based on assumption without the performance of a thorough clinical physical examination. A shoulder that has GIRD and a concomitant loss of TROM or an increase in ERD would be considered by the authors to be a pathologic glenohumeral internal rotation deficit or (p‐GIRD).
In determining clinically significant p‐GIRD, one must also carefully evaluate ER, and thus TROM. Wilk et al reported that in 362 healthy throwers, TROM was within 5° of the uninvolved side for all subjects.23 Ellenbecker et al13 reported on asymptomatic professional baseball pitchers and asymptomatic elite tennis players and reported that TROM was within 5° of their uninvolved side for the baseball pitchers and within 10° of the uninvolved side for the elite tennis players. Furthermore, Wilk et al reported that a difference of greater than 5° of TROM correlated with shoulder injuries.24
Several operational definitions have been used to describe the pathologic condition that is defined as GIRD. GIRD is generally defined as the loss in degrees of glenohumeral IR of the dominant shoulder compared with the non‐dominant shoulder. Calculation of GIRD has been previously reported per Burkhart et al1–3 and others.17 Burkhart reports that an acceptable level of GIRD is defined as: 1) less than 20° loss of shoulder IR comparing shoulders bilaterally, or 2) greater than a 10% loss of the total rotation seen in the non‐throwing shoulder (Non dominant shoulder IR + ER ROM) x 10%). Using this determination for example, assuming the non‐dominant shoulder has a total arc of motion of 160° degrees, the 10% rule would equate to only 16° of loss being required for the determination of GIRD, rather than the standard 20° loss typically needed. More recently Kibler et al have defined GIRD as side‐to‐side asymmetry greater than 18°.31
Burkhart et al3 have reported that as long as an athlete’s GIRD is less than or equal to their ER gain (ERG), the throwing shoulder will have no abnormal rotational kinematics and function properly. Problems can occur when the amount of the GIRD exceeds the ERG (GIRD: ERG ratio > 1.0). Furthermore, they report that the risk of structural injury is directly proportional to the increase in the GIRD: ERG ratio. For example see clinical scenario #1:
Clinical Scenario #1
| Dominant Shoulder | Non Dominant Shoulder | Difference | |
|---|---|---|---|
| Internal Rotation | 50° | 80° | 30° |
| External Rotation | 140° | 110° | 30° |
In the example above, there is an ERG = 30°, while GIRD = 30°. The ratio would be 30/30 = 0.0. In this case, because there is a loss of IR of 30°, and an ERG of 30°, the ratio is not > 1.0, and the overhead athlete would not be in danger of injury from the apparent IR ROM deficiency. Additionally, looking at the TROM concept it is seen the dominant shoulder has 190° of TROM, while the non‐dominant also has 190°, with no TROM difference. In this example, the athlete’s TROM is equal bilaterally. If a treatment program were implemented to gain an additional 10° of IR, this would also increase the athlete’s TROM by 10°. This increase in TROM may in fact create an environment of compromised static stability and challenge the dynamic stabilizers to a level that they are unable to successfully perform in stabilizing the glenohumeral joint. In the authors’ experience, this situation of increasing TROM on the dominant side is more disadvantageous to the overhead athlete than a loss of IR. Wilk et al reported that increasing TROM exhibited a higher correlation to shoulder injuries than GIRD.32 Therefore this overhead athlete’s lost IR motion may be qualified as a‐GIRD and not considered pathologic.
Clinical Scenario #2
| Dominant Shoulder | Non Dominant Shoulder | Difference | |
|---|---|---|---|
| Internal Rotation | 20° | 60° | 40° |
| External Rotation | 130° | 110° | 20° |
In clinical scenario #2 a totally different situation exists with similar losses of IR motion seen. In this second scenario ERG = 20°, while the GIRD = 40°. The ratio would be 40/20 = 1.5. In this case, there is a GIRD of 40°, and the ratio is > 1.0. This athlete would be in danger of injury. In assessment of the TROM concept the dominant shoulder has 150° of TROM, while the non‐dominant has 170°, with a difference in TROM of 20° when compared bilaterally. With a 40° loss of GH IR and a 20° loss of TROM this overhead athlete has been determined to have p‐GIRD and may be at risk for shoulder injuries.
Historically, previous authors1–3 have attempted to define GIRD as any side to side difference in IR and more recently a loss of 18° of IR in comparison to the non‐dominant arm.31,35 This approach of assigning an arbitrary number to define GIRD has several limitations and may be actually disadvantageous in the long term. When reviewing the previous studies that have quantified the ROM characteristics of overhead athletes, a common finding between each of the studies is the large standard deviation of measurements, ranging from 7° to 27° for IR and TROM measurements.11,13,15,17–19,24,36,37 This large standard deviation implies a wide variation of actual measurement values between subjects, making an arbitrary definition of GIRD not likely to be applicable to a wide range of athletes.
Based on this review of the literature, it is the authors’ preference to base treatment more on TROM rather than IR measurements alone. If the TROM is equal bilaterally, treatments designed to increase IR motion are not recommended, regardless of how large side‐to‐side differences are observed. In the instances where there is a significant deficit of IR and TROM, methods should be utilized to increase shoulder rotation ROM. Gaining shoulder rotational ROM can be achieved through the use of stretching techniques or through the use of manual therapy joint mobilization methods which will be detailed later in this manuscript.
Overview of Motion Loss in the Overhead Athlete
In an overhead athlete with limited motion, a comprehensive examination must be performed to determine the direction of motion limitation. A computed tomography (CT) scan or bony evaluation is done to determine if a humeral retroversion exists because fixed osseous transverse plane deformities are not changed through therapeutic intervention. Physiological active range of motion (AROM) and PROM as well as the accessory, joint play and component movements are all assessed to determine where the motion limitations are occurring. After identifying the direction of the limitation, next the examination of the patient to determine the cause of the motion limitation is performed. The differential diagnosis of tissue causing the motion limitation can be: osseous vs. non‐contractile vs. contractile.
The scientific and clinical rationale behind managing the hypomobile shoulder is predicated on treating soft tissue in order to create a plastic deformation response. Regardless of whether the limitation is non‐contractile (primarily involving scar tissue, fascia, ligaments, or capsule), or contractile tissue (involving the muscle tendon unit), contractures lead to an alteration in soft tissue and glenohumeral joint arthrokinematics and ultimately decreases in ROM. Although the clinician quantitatively measures the goniometric limitations in the physiological ROM, it is also important to recognize the morphological changes that can occur at the cellular level. Intermolecular and intramolecular cross‐links form in the periarticular connective tissue, causing shortening, resultant contractures, and development of adhesions. Functional impairments and movement dysfunctions created by the hypomobile tissue are assessed through a comprehensive examination of the overhead athlete, including legs, hip and core control, spine mobility, and a complete upper quarter examination. Sport specific qualitative and quantitative movements assessments can determine how the hypomobility is affecting the entire kinematic chain.38
The primary rationale supporting the use of stretching exercises for remodeling and increasing ROM is the biological principle that periarticular connective tissues (PCT’s) will remodel over time in response to the type and amount of physical stress they receive. Remodeling is a biological phenomenon that occurs over long periods of time rather than a mechanically induced changes occurring within minutes. Soft tissue remodeling along the lines of imparted stress is called “Davis’s Law of Soft Tissue Remodeling”. The desired result of treatment is to create a permanent change in the collagen tissue along the lines of stress, also known as plastic deformation. This occurs when micro trauma at the cellular level breaks cross‐links of the periarticular connective tissue (which form between the collagen bundles and create motion limitations) thereby creating elongation of collagen bundles.
In overhead athletes who present with either a significant limitation of either internal rotation (pGIRD) or have ERD, AND a concomitant significant loss of TROM several approaches can be used to normalize these motion restrictions. The use of the total end range time (TERT) formula is probably saved for those with severe motion restrictions and may be used for recalcitrant motion restrictions in athletes seen following shoulder surgeries or for those athletes who may suffer from a secondary adhesive capsulitis or general painful and stiff shoulder and not for those with general loss of motion. For overhead athletes with motion restrictions a more common form of treatment may be the use of joint mobilizations or stretching techniques. Joint mobilization techniques should only be used after a thorough evaluation has determined whether limitations are due to pain or capsular limitations. Lastly, the most common form of gaining motion in the overhead athlete is through stretching techniques, which will be described last in this manuscript.
Clinical Use of the TERT Approach
An overview of the specific rehabilitation approach and techniques to treat the non‐contractile hypomobile tissue using the TERT formula (Low load, long duration stretching) are as follows:
Exercises for the entire kinematic chain
Active metabolic warm‐up for 10 minutes
First TERT stretch for 10–20 minutes while heat is applied
Manual therapy interventions (contract‐relax, hold relax techniques, muscle energy technique (MET)
Resisted exercises (rhythmic stabilization (RS), isotonics) for the purpose of maintaining/gaining dynamic stability of newly gained PROM
Other – dynamic exercises for glenohumeral and scapulothoracic stability
Second TERT stretch for 10–20 minutes while cryotherapy is applied
Third TERT in home exercise program (HEP)
Working the entire kinematic chain includes the legs, core (trunk) stabilization, scapulothoracic, glenohumeral, rotator cuff, and total arm strengthening (TAS). Basic foundational exercises of each link in the kinematic chain should be performed to ensure that no individual muscle weaknesses will cause muscles proximal and distal to compensate or create abnormal synergy patterns of movement. If appropriate, neuromuscular dynamic stability exercises can also be performed to activate the proper synergy patterns for the sport.
Soft tissue elongation (plastic deformation) can be affected by: temperature (heat), force, time, and temperature (cooling). TERT Formula: (Clinical application). The first TERT can be performed by the passive warm‐up and stretching at the start of the treatment program.
Therefore, the first step is an active metabolic warm‐up on an upper body ergometer/rowing machine/etc. The warm‐up provides an internal warm up to heat the tissue and increase malleability.
Immediately following the active internal metabolic warm‐up, a passive warm‐up is followed which is the first “TERT” formula. The passive warm‐up uses an external heat modality, such as diathermy, hot packs, or ultrasound to target the hypomobile tissue while in a stretched position for approximately 20 minutes. However in a busy clinic this treatment is oftentimes administered for 10 minutes due to patient tolerance. Twenty minutes, three times per day for a total duration of 60 minutes per day of TERT is recommended.39,40
The active and passive warm‐ups optimize the extensibility of collagen. After preparing the tissue with the heating modalities, hands‐on interventions are performed. Hands‐on interventions enhance the remodeling and realignment of the collagen fibers, to increase the PROM of the hypomobile tissue.
Clinical Application of Manual Therapy
Does manual therapy work? What does the research demonstrate? The scientific and clinical rationale behind manual therapy is based on clinical effects. Clinical effects have been described as decreasing pain, neuromodulation, placebo effect, hand contact on the patient, believability of the effectiveness of the technique, facilitating synovial lubrication to a joint, and creating a deformation of the non‐contractile tissue (s). The Orthopedic Section of the American Physical Therapy Association has recently released evidence of manual therapy for adhesive capsulitis in the Clinical Practice Guidelines for Shoulder Pain and Mobility Deficits: Adhesive Capsulitis.41 Although loss of shoulder motion in the overhead athlete and loss of motion due to adhesive capsulitis are two totally different pathological processes, compelling evidence for use of joint mobilization and stretching may be useful for both populations. Although focusing mostly on the mechanical effects and deformation of the tissue, Jacobs and Sciascia42 have classified stretch intensity into the following categories: Low intensity: < 9 Nm of torque, Moderate intensity: 9 Nm – 38 Nm, High intensity: 39 Nm – 107 Nm. But the question still remains regarding: how much force is actually required to create the plastic deformation of the shoulder joint capsule? Level V evidence by Muraki et.al43 using a biaxial servohydraulic test machine with 21 posterior capsules harvested from fresh‐frozen shoulders, assigned 3 different loading groups simulating joint mobilizations. While oscillatory joint mobilization to a force of 5‐N resulted in temporary elongation of the posterior capsule, mobilization to loads of 20 and 40‐N resulted in sustained elongation for up to 1 hour. Findings also suggest that mobilizations up to loads that represent the beginning of the linear region of the load displacement curve could be performed without serious damage to the posterior capsule.
Consequently, manual therapy was investigated in a controlled laboratory testing using normal shoulders.44 Since many physical therapists regularly perform PROM assessments or joint mobilizations on patients with hypomobility of the shoulder; there is a need to objectively document the actual forces being applied. PROM assessments were performed on 30 physically active subjects (60 shoulders) testing 4 motions (1. anterior glide, 2. posterior glide, 3. ER physiological PROM, and 4. IR physiological PROM). A hand held dynamometer (HHD) recorded pressures applied in each motion. Testing positions were randomized and data collection was blinded. A total of 720 PROM assessments and mobilization movements were performed. For ER and IR PROM assessments, the forces were multiplied by the distance between the olecranon and ulnar styloid processes to calculate the resulting torques. Correlational analyses between each PROM assessment with height, mass and body mass index were conducted. Separate gender by limb analyses of variance were conducted for each PROM assessment. Mean anterior glide force was 13.1 kg (1.7 kg SD) (28.8 lbs), Mean posterior glide force was 16.9 kg (3.0 SD) (37.2 lbs), Mean ER torque was 6.55 kg. (1.55 SD)(CI‐5.8–7.35) (14.41 lbs), Mean IR torque was 6.0 kg. (2.15 SD)(CI‐5.5–6.65) (13.2 lbs).43 Based on Muraki, et.al.43 and the results of this study, it appears that the accessory movement mobilizations performed here are primarily affecting the transition zones of the load deformation curve which can lead to the plastic deformation changes in the tissue.
The next question was whether the manual therapy forces are applied consistently? Intratester reliability for quantification of forces with accessory and physiological movements were performed using computerized instrumented shoulder models. Fifty physical therapy students performed two trials of movements on a shoulder model testing motions of: anterior glide (AG), posterior glide (PG), IR and ER on two separate occasions. ICC’s greater than 0.75 represent good reliability and less than 0.75 reflect moderate to poor reliability.45 The results showed students demonstrated good ICC’s in all of the various manual movements performed on a computerized instrumented shoulder model, with the exception of AG IV. (See Table 2).46,47
Table 2.
Forces Applied During Glenohumeral Manual Therapy.
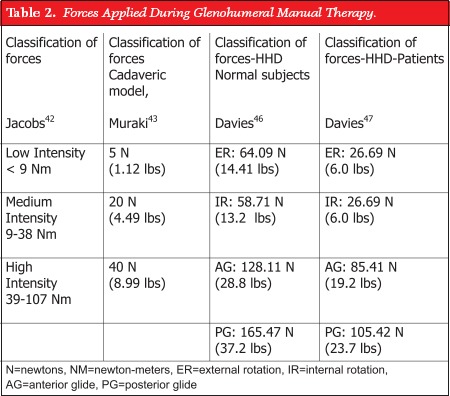 |
The key to the success of this treatment approach is to gain neuromuscular dynamic control over the newly gained ROM. Having PROM in a joint without dynamic control is useless, it is not functional ROM, and actually predisposes the patient to potential injury.
At the completion of the stretching and exercises that have increased the PROM, the involved area is then placed in the second TERT position, which is stretching with cryotherapy.
The third part of the TERT formula is to use the prolonged stretch in a home exercise program (HEP) for the time differential that has not been performed in the clinic since the proposed time for the stretch is 60 minutes.
If the patient’s limitation is due to changes within the muscle‐tendon unit (MTU), then static stretching is usually performed to create the changes in the length of the MTU. The stretching can be static holds, proprioceptive neuromuscular facilitation (PNF) contract‐relax, PNF hold‐relax, etc. Reinold et al46 demonstrated in professional baseball players how quickly the changes occur within the MTU; within minutes of completing an activity and the limitations remain for at least 24 hours without any interventions. Decreases of approximately 9° in IR were measured immediately following an episode of throwing. This is likely due to eccentric muscle actions that create microtrauma to the series and parallel elastic components within the MTU leading to the decreased viscosity, which needs to be addressed. Bandy has performed several studies to establish the optimum time for stretching the MTU.49–52 The results demonstrated 30 second static stretches were a sufficient time to create a change in the flexibility of the MTU. Feland however, demonstrated in patients older than 65 years of age the need to sustain the stretch for a longer period of time to create flexibility increases.53 In order to create the changes required the static stretches had to be held for a duration of 60 seconds.
OVERVIEW OF CLINICAL STRETCHING TECHNIQUES
Several stretching techniques have been described and are purported to provide stretching or mobilization of the posteroinferior soft tissue structures. One such method that has gained interest recently has been called the “sleeper stretch”.1,54,55 To perform the sleeper stretch the patient is placed in the side lying position with the weight of the body stabilizing the scapula against the table. The shoulder and elbow are flexed to 90°. A passive IR moment is applied at the wrist of the involved upper extremity via the opposite extremity. This stretch/mobilization can be done at both 90° (Figure 4) and at 45° (Figure 5) of glenohumeral joint elevation. When the sleeper stretch is performed at 90° with IR, it has the potential to iatrogenically impinge the shoulder. The roll‐over sleeper stretch is similar to the standard sleeper stretch except that the shoulder is only flexed to 45° and the patient rolls forward (placing the glenohumeral joint in a more horizontal adducted position) to approximately 30–40° from vertical side lying (Figure 6). The authors feel that in many athletes the roll over sleeper stretch may be too aggressive of a technique and can create pain, and should be used with caution. The modified sleeper stretch (30° of scaption) has been demonstrated with cadaveric models to produce the best stretch on the posterior capsule.56 This is the position recommended by the authors of this commentary since it better isolates the posterior shoulder and decreases risk of impingement due to 45° position rather than standard sleeper at 90°. A recent second modification of the sleeper stretch that the authors would like to introduce is performed with the patient sideling and the glenohumeral joint at 90° of abduction. Instead of staying directly in side lying (vertical body position) the patient performs a quarter turn toward their back‐placing their glenohumeral joint in the scapular plane (Figure 7a and b). This has been observed clinically to reduce glenohumeral joint impingement complaints.
Figure 4.

Sleeper stretch, performed at 90 degrees of abduction.
Figure 5.

Sleeper stretch, performed at 45 degrees of abduction.
Figure 6.

“Rollover” sleeper stretch, top view, b. front view of same.
Figure 7.
a. Alternate sleeper stretch position, quarter turn backward to decrease impingement symptoms. b. front view of same.
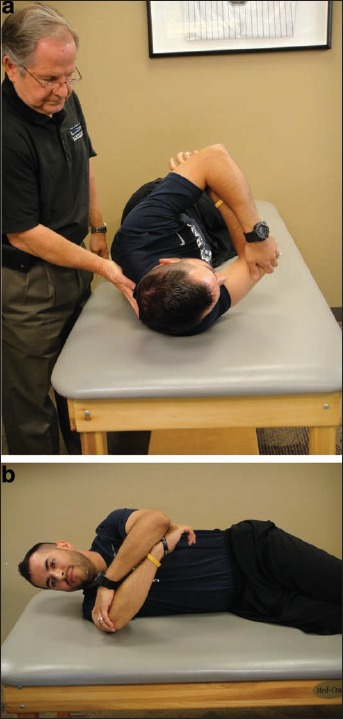
Another popular stretch is the cross‐body stretch. In this stretch the shoulder is elevated to approximately 90° of flexion and then pulled across the body into horizontal adduction with the opposite arm.57–59 This stretching method has been criticized in the past due to its inability to selectively stretch the posterior capsule.1,60 Clinicians believe that scapulothoracic tissues may also be stretched with this technique, although no biomechanical studies or tissue strain studies have been performed to prove or disprove this theory. If stretching the posterior soft tissues (rather than posterior capsule) is indicated, then this stretch may be one to consider. The horizontal adduction stretch with scapular stabilization described by Wilk et al is a stretching technique that appears to selectively stretch the posterior structures of the glenohumeral joint.30 The patient lies supine while the clinician stabilizes the patient’s scapula with one hand and imparts a horizontal adduction moment to the humerus with the other hand. Because the clinician is stabilizing the scapula, less tissue stretch should be imparted to the posterior scapular muscles, and more to the posterior cuff muscles. (Figure 8).
Figure 8.
Supine cross body stretch, with scapular stabilization.
Each of these stretching techniques should be held for approximately 30 seconds, in younger athletes, which has been determined to be the optimal time frame for stretching musculoskeletal structures.49–52 Prior to attempting to throw, a dynamic form of stretching may be more appropriate as research has indicated that static stretching results in decreased muscle strength and performance acutely.
Proposed Mechanisms of Intervention for Motion Loss
There are several randomized controlled trials of stretching procedures for posterior shoulder tightness. Manske et al61 assessed changes in glenohumeral IR ROM in a healthy population with pre‐determined posterior shoulder tightness as measured by bubble goniometer. Outcomes for this study were increases in IR measurements following an intervention of either the cross‐body stretch or the cross‐body stretch plus the addition of posterior capsule joint mobilization techniques. Although not at a statistically significant level, following four weeks of intervention the cohort that received additional joint mobilization techniques had greater increases in their IR ROM. Furthermore, that same group retained a greater amount of IR motion following a four‐week washout period.
McClure et al60 assessed changes in glenohumeral IR ROM in normal individuals with pre‐determined posterior shoulder tightness. Outcomes for this study were increases in glenohumeral internal rotation with the intervention of either the cross‐body stretch (19.9°) or the sleeper stretch (9.8°). Although not at a statistically significant level greater improvements were seen from the cohort that performed the cross‐body stretch. This may have been a surprising finding to many since many purport that the cross‐body stretching maneuver may allow scapular substitution due to the lack of ability to stabilize the scapular sufficiently. One assumes that the sleeper stretch allows for scapular stabilization since the patient is lying on the lateral border of the scapula while performing the stretch. McClure also reported that the cross‐body stretch demonstrated greater stretching compliance at 89% compared to 81% for the sleeper stretch.
Lintner et al15 assessed 85 male professional pitchers for GIRD and divided them into two groups: those that had greater than three or more years of posterior shoulder stretching experience and those that had less than three years of posterior shoulder stretching experience. The pitchers that had greater than three years of posterior shoulder stretching experience exhibited greater IR ROM (74.3° vs. 54.3°). The actual amount of GIRD was greater in the less than 3‐year stretching experience group. The authors also found that there appears to be a progressive increase in IR and TROM that correlates to the number of years in a stretching program. It is worth pointing out that this increase appears to plateau after three years. This study provides evidence that a consistent stretching program may be beneficial for those with posterior soft tissue restrictions.
Kibler and Chandler62 evaluated changes in ROM of competitive male and female junior tennis players following a specific stretching program. These fifty‐one athletes: 29 males (mean age 13.6) and 22 females (mean age 13.2) were measured at baseline, one, and two years following stretching program. These athletes were compared to age and sex‐matched control subjects. Specific stretching that may be more beneficial for tennis players for the posterior shoulder in this study included the behind the back tennis racquet stretch. The changes observed over time indicate most of the difference in motion occurred during the first year, with smaller amounts of motion change seen during the second year.
Stretching and mobilization techniques have both been shown to achieve increased ROM in overhead athletes with motion restrictions. Regarding stretching and mobilization techniques, several important points are worth mentioning. First, controversy still exists on what exactly what the best technique is for gaining mobility. In lower extremity literature there appears to be a large amount of evidence that the acute effects of static stretching immediately prior to muscle performance results in a decrease in physical performance. This appears to be opposite in reviewing the clinical literature regarding overhead athletes and the upper extremity. Knudson et al found no short‐term effect of the addition of a static stretching program to warm‐up on tennis serve speed and service percentage in adults.63 Additionally, Haag et al found that the addition of static stretching did not have a significant impact on baseball pitching performance in collegiate Division III baseball pitchers velocity or accuracy.64 It should be stressed that in these studies static stretching was the type that was performed. These studies did not use low‐load long‐duration (LLLD) stretching prior to throwing. The authors of this commentary recommend LLLD stretching to gain lost motion, but this form of stretching should not be encouraged as a warm‐up immediately before throwing or before tennis serving. Prior to overhead sports stretching is encouraged through manual techniques and through plyometrics. Additionally, joint mobilizations in the overhead athletes’ shoulder should also be used very cautiously. Careful examination of glenohumeral ROM and joint end feels should be used prior to using mobilization techniques that require increasing capsular laxity.
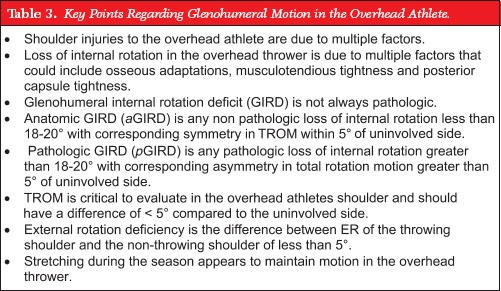
CONCLUSIONS
In summary, if the overhead athlete has alterations of glenohumeral motion, a comprehensive examination must be performed to determine the direction of motion that is limited and the specific tissues that cause the limitation. Key points related to glenohumeral joint motion in overhead athletes can be seen in Table 3. In overhead athletes a limitation of glenohumeral motion is required to perform motions such as throwing and serving. This loss of motion is normal and not pathologic. In extreme cases glenohumeral motion may be restricted to the point of actually causing pathology. Then, the appropriate intervention to address identified limitations can be chosen from those presented in this commentary, which are provided based upon a review of the evidence, when available.
Table 3.
Key Points Regarding Glenohumeral Motion in the Overhead Athlete.
 |
REFERENCES
- 1. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part I: Pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420 [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder. Spectrum of pathology. Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19:531–539 [DOI] [PubMed] [Google Scholar]
- 3. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661 [DOI] [PubMed] [Google Scholar]
- 4. Dillman CJ, Fleisig GS, Andrews JR. Biomechanics of pitching with emphasis upon shoulder kinematics. J Orthop Sports Phys Ther. 1993;18:402–408 [DOI] [PubMed] [Google Scholar]
- 5. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanism. Am J Sports Med. 1995;23(2):233–239 [DOI] [PubMed] [Google Scholar]
- 6. Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech 1999;32:1371–1375 [DOI] [PubMed] [Google Scholar]
- 7. Andrews JR, Fleisig GS. Preventing throwing injuries. J Orthop Sports Phys Ther. 1998;27:187–188 [DOI] [PubMed] [Google Scholar]
- 8. Conte S, Requa RK, Garrick JG. Disability days in major league baseball. Am J Sports Med. 2001;29(4):431–436 [DOI] [PubMed] [Google Scholar]
- 9. Fleisig GS, Barrentine SM, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421–437 [DOI] [PubMed] [Google Scholar]
- 10. McFarland EG, Wasik M, Epidemiology of collegiate baseball injuries. Clin J Sports Med. 1998;8(1):10–13 [DOI] [PubMed] [Google Scholar]
- 11. Crockett HG, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26 [DOI] [PubMed] [Google Scholar]
- 12. Downar JM, Saues EL. Clinical measures of shoulder mobility in the professional baseball player. J Athl Train. 2005;40(1):23–29 [PMC free article] [PubMed] [Google Scholar]
- 13. Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34(12):2052–2056 [DOI] [PubMed] [Google Scholar]
- 14. Johnson L. Patterns of shoulder flexibility among college baseball players. J Athl Train. 1992;27(1):44–49 [PMC free article] [PubMed] [Google Scholar]
- 15. Lintner D, Mayol M, Uzodinma O, Jones R, Labossiere D. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sports Med. 2007;35(4):617–621 [DOI] [PubMed] [Google Scholar]
- 16. Meister K, Day T, Horodyski MB, Daminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33(5):693–698 [DOI] [PubMed] [Google Scholar]
- 17. Myers JP, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391 [DOI] [PubMed] [Google Scholar]
- 18. Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30(3):347–353 [DOI] [PubMed] [Google Scholar]
- 19. Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30(3):354–360 [DOI] [PubMed] [Google Scholar]
- 20. Ruotolo C, Price E, Panchal A, Loss of total arc of motion in collegiate baseball players. J Shoulder Elbow Surg. 2006;15(1):67–71 [DOI] [PubMed] [Google Scholar]
- 21. Brown LP, Niehues SL, Harrah A, Yavorsky P, Hirshman HP. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1998;16:577–585 [DOI] [PubMed] [Google Scholar]
- 22. Roetert EP, Ellenbecker TS, Brown SW. Shoulder internal and external rotation range of motion in nationally ranked junior tennis players: A longitudinal analysis. J Strength Cond Res. 2000;14(2):140–143 [Google Scholar]
- 23. Wilk KE, Macrina LC, Arrigo C. Passive range of motion characteristics in the overhead baseball pitcher and their implications for rehabilitation. Clin Orthop Rel Res. 2012;470(6):1586–1594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD 2nd, Harker P, Paparesta N, Andrews JR. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39:329–335 [DOI] [PubMed] [Google Scholar]
- 25. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med 2011;39:1997–2006 [DOI] [PubMed] [Google Scholar]
- 26. Wilk KE, Reinold MM, Macrina LC, Porterfield R, Devine KM, Suarez K, Andrews JR. Glenohumeral internal rotation measurements differ depending on stabilization techniques. Sports Health. 2009;12:131–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Norkin CC, White DJ. Measurement of Joint Motion. A Guide to Goniometry 3rd ed. F.A. Davis Company, Philadelphia, 2003 [Google Scholar]
- 28. Ellenbecker TS, Roetert EP, Piorkowski PA, Schulz DA. Glenohumeral joint internal and external rotation range of motion in elite junior tennis players. J Orthop Sports Phys Ther. 1996;24(6):336–341 [DOI] [PubMed] [Google Scholar]
- 29. Ellenbecker TS. Clinical Examination of the Shoulder. St Louis, MO: Elsevier Saunders; 2004 [Google Scholar]
- 30. Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead athlete. Am J Sports Med. 2002;30(1):136–151 [DOI] [PubMed] [Google Scholar]
- 31. Kibler WB, Kuhn JE, Wilk KE, et al. The disabled throwing shoulder: Spectrum of pathology – 10‐year update. Arthroscopy 2013;29(1):141–161 [DOI] [PubMed] [Google Scholar]
- 32. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of shoulder range of motion and shoulder injuries in professional baseball pitchers: A 8 year prospective study. Presented at 2013 AOSSM Annual Conference, July 2013 [Google Scholar]
- 33. Hurd WJ, Kaplan KM, ElAttrache NS, Jobe FW, Morrey BF, Kaufman KR: A profile of glenohumeral internal and external rotation motion in the uninjured high school baseball pitcher: Part I: Motion. J Athletic Train 2011;46(3):282–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reeser JC, Joy EA, Porucznic CA, Berg RL, Colliver EB, Willick SE. Risk factors for volleyball‐related shoulder pain and dysfunction. Phys Med Rehabil. 2012;2:27–36 [DOI] [PubMed] [Google Scholar]
- 35. Kibler WB, Sciascia A, Moore S. An acute throwing episode decreases shoulder internal rotation. Clin Orthop Rel Res. 2012;470(6):1545–1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38(1):21–26 [DOI] [PubMed] [Google Scholar]
- 37. Borsa PA, Wilk KE, Jacobson JA, Scibek JS, Dover GC, Reinold MM, Andrews JR. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am J Sports Med. 2005;33(9):1392–1399 [DOI] [PubMed] [Google Scholar]
- 38. Kibler WB. Rehabilitation of rotator cuff tendinopathy. Clin Sports Med. 2003;22:837–847 [DOI] [PubMed] [Google Scholar]
- 39. McClure PW, Flowers KR. Treatment of limited shoulder motion: a case study based on biomechanical considerations. Phys Ther. 1992;72(12):926–936 [DOI] [PubMed] [Google Scholar]
- 40. McClure PW, Blackburn LG, Dusold C. the use of splints in the treatment of joint stiffness: biological rationale and an algorithm for making clinical decisions. Phys Ther. 1994;74(12):1101–1107 [DOI] [PubMed] [Google Scholar]
- 41. Kelley M, Shaffer MA, Kuhn JE, et al. Shoulder pain and mobility deficits: Adhesive capsulitis. Clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2013;43(5):A1–A28 [DOI] [PubMed] [Google Scholar]
- 42. Jacobs CA, Sciascia AD. Factors that influence the efficacy of stretching programs for patients with hypomobility. Sports Health 2011;3(6):520–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Muraki T, et al. The effect of cyclic loading simulating oscillatory joint mobilization on the posterior capsule of the glenohumeral joint: a cadaveric study. JOSPT; 2011;41:311–318 [DOI] [PubMed] [Google Scholar]
- 44. Davies GJ, Riemann BL, Tankovich M, Jacobs C, King JE. Objective quantification of the forces used with accessory/joint play and physiological manual therapy techniques for the shoulder. Manuscript in review – Man Ther, 2013 [Google Scholar]
- 45. Portney, Watkins Foundations of Clinical Research: Applications to Practice, 3rd ed, 2009 [Google Scholar]
- 46. King E, Davies GJ, Cunningham TC. Intratester reliability for quantification of forces with accessory and physiological movements using computerized instrumented shoulder models. Poster presented at APTA‐CSM, San Diego, CA, 2013 [Google Scholar]
- 47. Davies GJ, King JE, Cunningham TC. Stratified student physical therapists Intra‐tester reliability for quantification of forces with accessory and physiological movements using computerized instrumented shoulder models. Poster presented at APTA‐CSM, San Diego, CA, 2013 [Google Scholar]
- 48. Reinold MM, Wilk KE, Macrina LC, Sheheane C, Dun S, Fleisig GS, Crenshaw K, Andrews JR. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36(3):523–527 [DOI] [PubMed] [Google Scholar]
- 49. Bandy WD, Irion JM. The effect of time on static stretching on the flexibility of the hamstring muscles. Phys Ther 1994;74:845–850 [DOI] [PubMed] [Google Scholar]
- 50. Bandy WD, Irion JM, Briggler M. The effect of time and frequency of static stretch on flexibility of the hamstring muscles. Phys Ther 1997;77:1090–1096 [DOI] [PubMed] [Google Scholar]
- 51. Warren CG, Lehmann JF. et al. Heat and stretch procedures: an evaluation using rat tail tendon. Arch Phys Med Rehabil 1976;57:122–126 [PubMed] [Google Scholar]
- 52. Bandy WD, Irion JM, Briggler M. The effect of static stretch and dynamic range of motion on the flexibility of the hamstring muscles. J Orthop Sports Phys Ther 1998;27:295–300 [DOI] [PubMed] [Google Scholar]
- 53. Feland JB, Myrer JW, Schulthies SS, Fellingham GW, Measom GW. The effect of duration of stretching of the hamstring muscle group for increasing range of motion in people aged 65 years or older. Phys Ther 2001;81(5):1110–117 [PubMed] [Google Scholar]
- 54. Bach HG, Goldberg BA. Posterior capsular contracture of the shoulder. J Am Acad Orthop Surg 2006;14:265–277 [DOI] [PubMed] [Google Scholar]
- 55. Weldon EG, Richardson AB. Upper extremity overuse injuries in swimming. A discussion of swimmer’s shoulder. Clin J Sports Med 2001;20:423–438 [DOI] [PubMed] [Google Scholar]
- 56. Izumi T, Aoki M, Muraki T, Hidaka E, Miyamoto S. Stretching positions for the posterior capsule of the glenohumeral joint: strain measurement using cadaver specimens. Am J Sports Med 2008;38(5):257–261 [DOI] [PubMed] [Google Scholar]
- 57. Bandy WD, Sanders B. Therapeutic Exercise: Techniques for Intervention. Baltimore, MD: Lippincott Williams & Wilkins, 2001 [Google Scholar]
- 58. McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3‐dimensional kinematics in people with shoulder impingement syndrome before and after a 6‐week exercise program. Phys Ther 2004;84:832–848 [PubMed] [Google Scholar]
- 59. Tyler TF, Nicholas SJ, Lee SJ, Mullaney M, McHugh MP. Correction of posterior shoulder tightness is associated with symptoms resolution in patients with internal impingement. Am J Sports Med. 2010;38(1):114–119 [DOI] [PubMed] [Google Scholar]
- 60. McClure P. et al. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther 2007;37(3):108–114 [DOI] [PubMed] [Google Scholar]
- 61. Manske RC, Meschke M, Porter A, Smith B, Reiman M. A randomized controlled single‐blinded comparison of stretching versus stretching and joint mobilization for posterior shoulder tightness measured by internal rotation motion loss. Sports Health 2010;2(2):94–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kibler WB, Chandler TJ. Range of motion in junior tennis players participating in an injury risk modification program. J Sci Med Sport 2003;6(1):51–62 [DOI] [PubMed] [Google Scholar]
- 63. Knudson DV, Noffal GJ, Bahamonde, Bauer JA, Blackwell JR: Stretching has no effect on tennis serve performance. J Strength Cond Res. 2004;18(3):654–656 [DOI] [PubMed] [Google Scholar]
- 64. Haag SJ, Wright GA, Gillette CM, Greany JF. Effects of acute static stretching of the throwing shoulder on pitching performance of national collegiate athletic association division III baseball players. J Strength Cond Res. 2010;24(2):452–427 [DOI] [PubMed] [Google Scholar]


