Abstract
Objective
Cognitive-Behavioral Therapy for psychosis (CBTp) is an evidence-based treatment for psychosis-related disorders. However, despite the strong evidence-base and inclusion in national treatment guidelines, CBTp remains poorly disseminated in the US. It is proposed that this state is a product of lack of CBTp knowledge among clinical training leaders along with limited availability of training opportunities.
Method
We surveyed training directors in US psychiatry residency and clinical psychology doctoral programs to characterize the penetration of CBTp training and to assess their familiarity with basic CBTp facts.
Results
Directors displayed limited knowledge of CBTp effectiveness, with only 50% of psychiatry and 40% of psychology directors believing that CBTp is efficacious. Only 10% of psychiatry and 30% of psychology directors were aware that the CBTp evidence-base is based on meta-analyses. While 45% of all directors reported that their program offer CBTp training, trainees received limited training - 4 hours of didactics, 21 hours of treatment, and 12 hours of supervision.
Conclusions
CBTp dissemination in the US is characterized by training directors’ minimal awareness of the CBTp evidence-base along with training opportunities that are so limited, as to be unlikely to be adequate to provide CBTp effectively, hence unlikely to improve patients’ psychoses.
Cognitive Behavioral Therapy for psychosis (CBTp) has been recognized as an evidence-based treatment for individuals with schizophrenia and related disorders. CBTp was originally developed to target delusions and hallucinations, and is largely used as an adjunct to antipsychotic medication. Since the early 1990’s, thirty-four randomized clinical trials of CBTp have been published (Wykes et al., 2008), along with a number of meta-analyses indicating that CBTp produces significant reduction in the severity of psychotic symptoms above and beyond the impact of pharmacological treatments, along with significant improvements in negative symptoms, negative mood, and social anxiety ((Wykes et al., 2008; Tarrier & Wykes, 2004). CBTp has been found to be cost-effective (Turkington et al., 2008; Granholm et al., 2005) with the therapeutic gains sustaining up to five years after treatment (Lysaker et al., 2009). Additionally, CBTp with individuals with schizophrenia has been found to increased social functioning and vocational performance (Dixon et al., 2010).
Consistent with these findings, in the United States (US) the use of CBTp is recommended by both the American Psychiatric Association’s (APA) treatment guidelines and the most recent Patient Outcome Research Team report (PORT; Kreyenbuhl et al., 2009). Accordingly, “persons with schizophrenia who have persistent psychotic symptoms while receiving adequate pharmacotherapy should be offered adjunctive cognitive behaviorally oriented psychotherapy to reduce the severity of symptoms. The therapy may be provided in either a group or an individual format and should be approximately 4–9 months in duration” (Kreyenbuhl et al., 2009). In the United Kingdom (UK), the treatment recommendations extend even further - the National Institute for Health and Clinical Excellence (NICE) recommends that CBTp should be offered “to all patients with schizophrenia. This can be started either during the acute phase or later, including inpatient stay.” However, despite the strong evidence-base and the availability of clear guidelines, CBTp remains poorly disseminated in the US where pharmacological interventions remain the nearly exclusive treatment option for psychosis for a preponderance of patients (Olfson et al., 2002; Lehman & Steinwachs, 1998). Yet, as 25–55% of individuals with schizophrenia do not experience full relief from psychotic symptoms in response to pharmacological interventions (Kane, 1999; Pantelis & Barnes, 1996), and 3 out of 4 discontinue their medication within 18 months (Lieberman et al., 2005), many patients in the US may be potentially receiving suboptimal treatment, resulting in increased suffering and dysfunction.
In a review of CBTp, Turkington et al., (2006) contrasted the differences in CBTp dissemination between the US and the UK. The authors pointed out that, while in the UK the dissemination remains far from being complete, CBTp has generally become an accepted part of standard care. In contrast, the authors state that in the US there has been little interest in CBTp. Consistent with this point, out of the 34 CBTp clinical trails listed in the most recent meta-analysis (Wykes et al., 2008), only 5 were completed in the US (vs. 20 in the UK). Turkington and colleagues (2006) attributed the lack of interest in the US to the sometimes acrimonious debates between biological psychiatrists and psychoanalysts starting the in 1950’s, which resulted in antipsychotic medication becoming the primary treatment for psychotic symptoms while psychotherapy being almost completely disavowed. While not discounting this view, there may be more parsimonious explanations for the poor current state of CBTp dissemination in the US – lack of knowledge among current clinical training leaders along with limited availability of training opportunities, which may serve as a “bottleneck” hindering the dissemination of CBTp. However, precise data about CBTp familiarity among clinical leaders and training availability in the US are unknown.
To address these issues, we conducted a survey among clinical training leaders -- training directors in psychiatry residency and clinical psychology doctoral programs in the US. The choice of training directors was based on their role as primary trainers of future clinicians, and thus “gate keepers” of clinical knowledge and training curriculums. Psychiatry residency programs were selected, as psychiatrists are typically the primary clinical providers of patients with schizophrenia in the US. Doctoral-level training programs in clinical psychology were also surveyed, since CBT training for other disorders is commonly offered in these programs. The primary aims were: 1) to characterize the penetration of CBTp training (as well as CBT for other disorders) in US programs; and 2) to assess training directors’ familiarity with basic facts about CBTp.
Method
We conducted a survey to assess our primary aims (see Appendix A). The selection of the questions for the survey was informed by a previous survey on CBT training in psychiatry residency programs in the US (Sudak et al., 2002). Using www.surveymonkey.com, an Internet-based survey software, we invited 389 training directors (178 in psychiatry and 221 clinical psychology) by email to complete the survey. Training directors who successfully completed the survey were entered into a drawing to receive a $250 gift certificate. Data were collected between April and July 2009.
Results
Eighty-six surveys were completed (22% response rate). There were no significant differences between responders and non-responders with regard to number of trainees or number of faculty in their department. Our first aim was to characterize the penetration of CBTp training in US programs among psychiatry and clinical psychology trainees. These data are presented in Table 1. The results indicate that throughout their training, psychiatry residents received on average 21.1 hours of didactic training on schizophrenia, compared to 15.3 hours among clinical psychology students (t=2.14, p=.04; not significant after Bonferroni correction). However, psychiatry residents obtained significantly more first-hand experience treating a substantial number of patients with schizophrenia (10 or more patients), with virtually all residents receiving such exposure (97%) versus only 30% of the psychology trainees (χ2=70.95, p<.001). Specifically, 20% of the clinical psychology trainees treated no more than one patient with schizophrenia during their training and 70% treated no more than four patients with schizophrenia. In contrast, clinical psychology students received substantially more training in CBT for other diagnoses. On average, they attended 74.8 hours of CBT didactic training (vs. 33.2 hours for residents; t=2.11, p=.04), completed 303.6 hours of direct CBT treatment experience (vs. 71.7 hours; t=4.08, p<.001), and received 100.2 hours of CBT supervision (vs. 43.7 hours; t=3.75, p<.001).
Table 1.
Teaching on Schizophrenia and Cognitive-Behavioral Therapy
| Program Type |
N | Mean | SD | t / χ2 (p) |
|
|---|---|---|---|---|---|
| Number of Didactic Teaching Hours Trainees Received on Schizophrenia |
Psychology | 46 | 15.3 | 15.0 | t=2.14 (p=.04) |
| Psychiatry | 40 | 21.1 | 9.8 | ||
| Number of Didactic Teaching Hours Trainees Received on CBT * |
Psychology | 46 | 74.8 | 131.6 | t=2.11 (p=.04) |
| Psychiatry | 40 | 33.2 | 21.8 | ||
| Number of Treatment Hours Trainees Administered CBT * |
Psychology | 46 | 303.6 | 380.0 |
t=4.08 (p<.001) |
| Psychiatry | 40 | 71.7 | 60.0 | ||
| Number of CBT Supervision Hours Received by Trainees* |
Psychology | 46 | 100.2 | 97.1 |
t=3.75 (p<.001) |
| Psychiatry | 39 | 43.7 | 28.7 | ||
| % of Programs in Which Trainees Treated ≥9 Patients with Schizophrenia ** |
Psychology | 14 / 46 (30%) |
χ2=70.95 (p<.001) |
||
| Psychiatry | 39 / 40 (97%) | ||||
Response rate: Psychiatry residency programs = 22% (40/178); Clinical Psychology doctoral programs = 21% (46/221);
CBT for all disorders;
any treatment modality.
Bold type indicates significant differences after Bonferroni correction.
Next, we assessed how many programs offered CBTp training. Among the 86 respondents, 39 training directors (45%) reported that their program offered CBTp training. For these responders, we further evaluated the nature of training offered. As there were no significant differences between the psychiatry and clinical psychology programs, the data were combined. Among programs that offered CBTp, on average trainees received 4.1 hours of CBTp didactic training (SD=3.3), conducted 21.8 hours of face-to-face CBTp treatment (SD=37.8), and received 12.3 hours of supervision (SD=19.2).
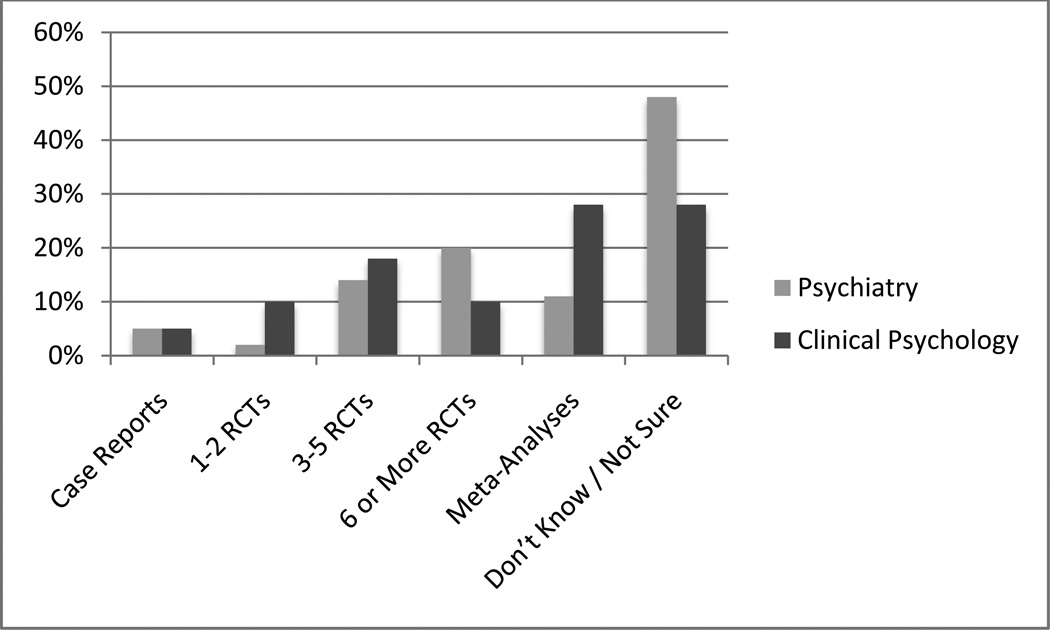
Our second aim was to assess the training directors knowledge of basic evidence-based information about CBTp. Only about half of directors (54% in psychiatry vs. 40% in clinical psychology) stated they believed there is evidence from clinical trials that CBTp is an effective treatment for psychosis. In comparison, virtually all directors believed there is evidence from clinical trials that CBT is an effective treatment for anxiety disorders (95% and 97% for clinical psychology and psychiatry training directors, respectively) and depression (100% and 100%, respectively). Consistent with these data, only 11% of the psychiatry training directors and 28% in clinical psychology ones knew that the evidence base for CBTp is based on meta-analyses of numerous clinical trials, with 48% of the directors in psychiatry programs and 28% of the clinical psychology directors endorsing “Don’t Know / Not Sure” (see Figure 1). Next, responders were asked about their knowledge of the APA practice guidelines for specific schizophrenia symptoms. For hallucinations, only 20% of clinical psychology directors answer positively, compared to 54% in psychiatry (χ2=6.22, p=.02). For delusions, 34% of clinical psychology directors answer positively, compared to 51% of psychiatry directors. Forty-three percent of clinical psychology directors responded “Don’t Know / Not Sure” in response to this question, compared to 21% of psychiatry directors (χ2=4.52, p=04).
Figure 1.
Training Directors’ Knowledge of the Evidence-Base for CBT for Psychosis
RCT – Randomized Clinical Trials.
Discussion
The present study aimed to evaluate the training and dissemination of CBTp in the US by surveying training directors of psychiatry residencies and clinical psychology doctoral programs. Although previous reports characterized CBTp use among US clinicians (Kuller et al., 2010), to the best of our knowledge this is the first systematic characterization of CBTp training and dissemination in academic programs in the US.
Our data indicates that the state of training and dissemination of CBTp in the US is very limited. Although 45% of training directors reported that their program offered CBTp training, inspection of the time invested in such training raises serious concerns about the adequacy and effectiveness of such training. On average, in the course of their clinical training, trainees received approximately 4 hours of CBTp didactic training, conducted 21 hours of face-to-face treatment with schizophrenia patients, and received 12 hours of supervision. There are currently no published training standards for achieving competency in CBTp in the US. However, data from the academic institutions in the UK provides some context about the extent of training required to obtain competency. For example, trainees at a post-graduate certificate program in CBTp at the Institute of Psychiatry in London complete a yearlong training with at least 150 hours of didactic training, 270 hours of face-to-face CBTp with a minimum of 4 patients (>16 sessions over >6 months each), and received 80 hours of supervision (Dr. Suzanne Jolley, Program Leader, personal communication, 2010). None of the surveyed programs reported comparable training. While our findings may potentially result from ascertaining bias (e.g., program directors not interested/knowledgeable about CBT would be more likely to respond), we believe such pattern is unlikely given the director’s knowledge about CBT for depression and anxiety. However, even if this were the case, the 22% response rate would highlight the limited CBTp knowledge/interest among training directors.
The limited training offered to trainees has been demonstrated to be insufficient to produce behavioral change (Farhall et al., 1998). Likewise, the mean number of hours trainees conducted face-to-face CBTp would typically be insufficient to complete a full course of CBTp, resulting in a number of negative consequences. First, patients receiving CBTp treatment from such minimally-trained clinicians are unlikely to experience improvement in their psychotic symptoms. Similarly, trainees who conduct treatment following such limited training are unlikely to see positive results from their interventions, will not experience CBTp competency, and thus will be less likely to use CBTp with future patients. Finally, the poor results from such treatments are likely to perpetuate common views that individuals with schizophrenia do not benefit from psychotherapy and diminish further the potential for CBTp dissemination in the US.
Consistent with these findings, our data indicate that many training directors have sparse knowledge of the evidence-base for CBTp and may not be aware that the training offered in their program is not sufficient to develop CBTp competency. Furthermore, only half of training directors in psychiatry programs, and less than a third in clinical psychology, believed CBTp is an effective treatment for delusions and/or hallucinations. These data stands in sharp contrast to the training directors’ knowledge of the efficacy of CBT to treat depression and anxiety disorders. Similarly, training directors displayed limited knowledge of the evidence base for CBTp, with only 1 out of 10 psychiatry training directors and 3 out of 10 clinical psychology training directors being aware that support for CBTp is based on meta-analyses of numerous randomized clinical trials. Altogether, these data suggest a rather poor state of training and dissemination of CBTp in the US, characterized by training directors’ insufficient knowledge of the CBTp evidence base, along with limited training offered to trainees. Thus, while the dissemination of CBTp share many of the challenges of CBT dissemination in general (Shafran et al., 2009), our findings suggest that the dissemination of CBTp in the US is also facing a distinct challenge – the relatively limited knowledge and familiarity with CBTp among clinical training leaders who serve as “gate keepers” of clinical knowledge and training curriculums.
The reasons for the limited dissemination of CBTp in the US appear systematic and complex. As Turkington and colleagues (2006) clearly noted, the debates between biological psychiatrists and psychoanalysts starting in the 1950’s, which resulted in antipsychotic medication becoming the primary treatment for psychotic symptoms while psychotherapy being almost completely disavowed, appear to have set the foundation for the current state. The increased dominance of the pharmaceutical companies in the US over the years may have potentially exacerbated this trend, leading to more emphasis on biological approaches to the treatment of psychosis, and making psychological approaches, and psychologists, viewed as unessential.
Amelioration of the poor state of CBTp dissemination will require a number of steps. First, initial emphasis should be placed on dissemination of the evidence base and treatment recommendations among “gate keepers” of clinical training, such as training directors, department chairs, leaders in mental health organizations who influence the training of future generations of clinicians, as well as federal and state mental health officials (Berry & Haddock, 2008). This can take the form of publication of manuscripts reviewing the evidence base for CBTp and scheduling of workshops on CBTp during national psychiatry and psychology meetings. A second focus should be on the disseminating of evidence base information on CBTp and treatment recommendations among patients, family members, and caregivers. As many clinicians are not familiar with CBTp, this treatment option is often not discussed with patients and their families, let alone offered. This can take the form of presentations about the evidence-base of CBTp to organizations that cater to patients, family members, and caregivers (i.e., NAMI). Thirdly, at present, mental health providers in the US are not obligated to deliver evidence-based psychological and behavioral treatments, with choice of specific interventions being left to professional judgment. Thus, payments for services are generally not linked to the content of treatment and third-party payers reimburse providers for generic contexts of mental health treatments, such as evaluation, group therapy, inpatient treatment, and case management (Miller et al., 2005). Therefore, standards for training and achieving competency in CBTp should be developed and established. Initial steps to develop such standards are already underway (Morrison & Barratt, 2008).
While increasing the availability and implementation of evidence-based psychological treatments has been identified as a priority area in the NIMH’s strategic plan (Insel, 2009), given the non-centralized structure of the US mental health systems, it remains unclear how best to proceed in disseminating CBTp training. Amelioration of this state is contingent on the availability of effective CBTp training programs, yet the across-the-board incorporation of CBTp into standard psychiatry and psychology training curriculums seem unlikely, given the extensive investment of time and academic resources required to develop CBTp competency. Thus, similarly to the UK, such training may be more amenable to be incorporated into training in psychiatry and psychology programs specializing in treatment of severe mental illness, and/or post-graduate training programs. Consistent with this view, a handful of academic centers in the US have research programs focusing on CBTp. Additionally, in recent years a few independent post-graduate CBTp training programs began to proliferate and offer CBTp training for individuals and institutions.1 Such centers and programs have potential expertise to offer high quality CBTp training and supervision, offering beachheads that will expand the currently minimal dissemination of CBTp in the US. Over time, such centers and programs can increase the availability of clinicians competent in CBTp, and provide foundations for the development of additional CBTp training centers across the US.
Another unaddressed issue is the necessary educational background and qualifications for conducting CBTp. As the primary providers of psychiatric treatment for patients with schizophrenia, psychiatrists would be the obvious candidates to provide CBTp. Evidence suggest that CBTp can be successfully administered by psychiatrists working in public-health services (Turkington D & Kingdon, 2000). However, reports point to a continuous decline in the provision of psychotherapy and an increased emphasis on pharmacotherapy by US office-based psychiatrists (Mojtabai & Olfson, 2008). This trend may potentially be related to the lower financial incentives for psychiatrists to provide psychotherapy, with an average reimbursement for psychotherapy found to be 40 percent less than for equivalent time providing medication management (West et al., 2003). Another option would be to utilize clinical psychologists - in their review of the UK dissemination of CBTp, Tarrier and colleagues (1999) concluded that training should include “a thorough grounding and education in the cognitive and behavioral sciences” (p. 580) and that effectively the most suitable professionals to provide CBTp are clinical psychologists. Indeed, as evident by our findings, clinical psychology trainees receive significantly more training in CBT (for all diagnoses) compared to psychiatry residents, making clinical psychologists solid candidates to become the primary providers of CBTp. Yet, our findings also point to a critical predicament regarding the state of schizophrenia treatment training in the US - while virtually all psychiatry trainees receive ample first-hand exposure to patients with schizophrenia, their training in CBT is rather limited. In contrast, clinical psychology trainees often receive substantial training in CBT (for all diagnoses), but few treat patients with psychotic disorders during their graduate training.
Another option may be the provision of CBTp by psychiatric nurses or social workers. Again, the experience of CBTp dissemination in the UK may prove informative. Starting in the 1990’s, training courses for community psychiatric nurses (CPN) were set up in London and Manchester. The initial evaluation indicated significant clinical benefits (Lancashire et al., 1997), resulting in the National Health Service (NHS) adopting the management and funding for training programs nationally. However, follow-up evaluations of training and dissemination of CBTp, indicated partial success, with the level of skills attained by the CPNs found to be quite modest. Additionally, many of the trained nurses did not return to their workplace or were unable to implement CBTp for a range of organizational reasons (Tarrier et al., 1999). More recent attempts provided mixed results (Turkington et al., 2006; Malik et al., 2009). Regarding the effectiveness and/or efficacy of CBTp being offered by social workers, there are no published reports about assessing this matter. Thus, given the extensive costs and time commitment associated with CBTp training, policy makers and mental health leaders may want to concentrate training resources in order maximize benefit for patients. As many clinical psychologists already obtain broad training in CBT as part of their education, they appear to be best positioned to obtain competency and provide CBTp.
The limitations of the study should be acknowledged. One potential limitation is the response rate to the survey - while the 22% response rate was somewhat disappointing, it is comparable to recently published reports of online surveys of psychiatrists and mental health professionals (19% in Mallinger & Lamberti, 2010; 25% in Bruchmuller et al., 2011; and 8% in Raz et al., 2011). Given that this is the first report on CBTp training and dissemination in the US, our data represent an important, though admittedly imperfect, initial examination of the state of practice in this area. A second potential limitation is the emphasis on self-reports and lack of cross verification of actual training experiences by trainees.
Supplementary Material
Footnotes
Disclosure: The primary author (DK) is a training faculty at The Institute of Cognitive Therapy for Psychosis (ICTP), a post-graduate CBTp training program located in New York City.
References
- Berry K, Haddock G. The implementation of the NICE guidelines for schizophrenia: barriers to the implementation of psychological interventions and recommendations for the future. Psychology and psychotherapy. 2008;81(Pt 4):419–436. doi: 10.1348/147608308X329540. [DOI] [PubMed] [Google Scholar]
- Bruchmuller K, Margraf J, Suppiger A, Schneider S. Popular or unpopular? Therapists' use of structured interviews and their estimation of patient acceptance. Behavior therapy. 2011;42(4):634–643. doi: 10.1016/j.beth.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW Schizophrenia Patient Outcomes Research, T. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhall J, Webster B, Hocking B, Leggatt M, Riess C, Young J. Training to enhance partnerships between mental health professionals and family caregivers: a comparative study. Psychiatric services. 1998;49(11):1488–1490. doi: 10.1176/ps.49.11.1488. [DOI] [PubMed] [Google Scholar]
- Granholm E, McQuaid JR, McClure FS, Auslander LA, Perivoliotis D, Pedrelli P, Jeste DV. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162(3):520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66(2):128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- Kane JM. Pharmacologic treatment of schizophrenia. Biol Psychiatry. 1999;46(10):1396–1408. doi: 10.1016/s0006-3223(99)00059-1. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB Schizophrenia Patient Outcomes Research, T. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2010;36(1):94–103. doi: 10.1093/schbul/sbp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuller AM, Ott BD, Goisman RM, Wainwright LD, Rabin RJ. Cognitive behavioral therapy and schizophrenia: a survey of clinical practices and views on efficacy in the United States and United kingdom. Community mental health journal. 2010;46(1):2–9. doi: 10.1007/s10597-009-9223-6. [DOI] [PubMed] [Google Scholar]
- Lancashire S, Haddock G, Tarrier N, Baguley I, Butterworth CA, Brooker C. Effects of training in psychosocial interventions for community psychiatric nurses in England. Psychiatric services. 1997;48(1):39–41. doi: 10.1176/ps.48.1.39. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Steinwachs DM. Patterns of usual care for schizophrenia: initial results from the Schizophrenia Patient Outcomes Research Team (PORT) Client Survey. Schizophr Bull. 1998;24(1):11–20. doi: 10.1093/oxfordjournals.schbul.a033303. discussion 20–32. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO Clinical Antipsychotic Trials of Intervention Effectiveness, I. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. The New England journal of medicine. 2005;353(12):1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Davis LW, Bryson GJ, Bell MD. Effects of cognitive behavioral therapy on work outcomes in vocational rehabilitation for participants with schizophrenia spectrum disorders. Schizophr Res. 2009;107(2–3):186–191. doi: 10.1016/j.schres.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Malik N, Kingdon D, Pelton J, Mehta R, Turkington D. Effectiveness of brief cognitive-behavioral therapy for schizophrenia delivered by mental health nurses: relapse and recovery at 24 months. J Clin Psychiatry. 2009;70(2):201–207. doi: 10.4088/jcp.07m03990. [DOI] [PubMed] [Google Scholar]
- Mallinger JB, Lamberti JS. Psychiatrists' attitudes toward and awareness about racial disparities in mental health care. Psychiatric services. 2010;61(2):173–179. doi: 10.1176/ps.2010.61.2.173. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben J, Johnson WR. Evidence-based treatment: why, what, where, when, and how? J Subst Abuse Treat. 2005;29(4):267–276. doi: 10.1016/j.jsat.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. National trends in psychotherapy by office-based psychiatrists. Arch Gen Psychiatry. 2008;65(8):962–970. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- Morrison AP, Barratt S. What are the components of CBT for psychosis? A Delphi study. Schizophr Bull. 2010;36(1):136–142. doi: 10.1093/schbul/sbp118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Lewis-Fernandez R, Weissman MM, Feder A, Gameroff MJ, Pilowsky D, Fuentes M. Psychotic symptoms in an urban general medicine practice. Am J Psychiatry. 2002;159(8):1412–1419. doi: 10.1176/appi.ajp.159.8.1412. [DOI] [PubMed] [Google Scholar]
- Pantelis C, Barnes TR. Drug strategies and treatment-resistant schizophrenia. Aust N Z J Psychiatry. 1996;30(1):20–37. doi: 10.3109/00048679609076070. [DOI] [PubMed] [Google Scholar]
- Raz A, Campbell N, Guindi D, Holcroft C, Dery C, Cukier O. Placebos in clinical practice: comparing attitudes, beliefs, and patterns of use between academic psychiatrists and nonpsychiatrists. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2011;56(4):198–208. doi: 10.1177/070674371105600403. [DOI] [PubMed] [Google Scholar]
- Shafran R, Clark DM, Fairburn CG, Arntz A, Barlow DH, Ehlers A, Wilson GT. Mind the gap: Improving the dissemination of CBT. Behav Res Ther. 2009;47(11):902–909. doi: 10.1016/j.brat.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Sudak DM, Beck JS, Gracely EJ. Readiness of psychiatry residency training programs to meet the ACGME requirements in cognitive-behavioral therapy. Acad Psychiatry. 2002;26(2):96–101. doi: 10.1176/appi.ap.26.2.96. [DOI] [PubMed] [Google Scholar]
- Tarrier CB, Haddock Gillian, Nicholas John McGovern. The dissemination of innovative cognitive-behavioural psychosocial treatments for schizophrenia. Journal of Mental Health. 1999;8(6):569–582. [Google Scholar]
- Tarrier N, Wykes T. Is there evidence that cognitive behaviour therapy is an effective treatment for schizophrenia? A cautious or cautionary tale? Behav Res Ther. 2004;42(12):1377–1401. doi: 10.1016/j.brat.2004.06.020. [DOI] [PubMed] [Google Scholar]
- Turkington D, Kingdon D. Cognitive-behavioural techniques for general psychiatrists in the management of patients with psychoses. The British journal of psychiatry : the journal of mental science. 2000;177:101–106. doi: 10.1192/bjp.177.2.101. [DOI] [PubMed] [Google Scholar]
- Turkington D, Kingdon D, Weiden PJ. Cognitive behavior therapy for schizophrenia. Am J Psychiatry. 2006;163(3):365–373. doi: 10.1176/appi.ajp.163.3.365. [DOI] [PubMed] [Google Scholar]
- Turkington D, Sensky T, Scott J, Barnes TR, Nur U, Siddle R, Kingdon D. A randomized controlled trial of cognitive-behavior therapy for persistent symptoms in schizophrenia: a five-year follow-up. Schizophr Res. 2008;98(1–3):1–7. doi: 10.1016/j.schres.2007.09.026. [DOI] [PubMed] [Google Scholar]
- West JC, Wilk JE, Rae DS, Narrow WE, Regier DA. Economic grand rounds: financial disincentives for the provision of psychotherapy. Psychiatric services. 2003;54(12):1582–1583. 1588. doi: 10.1176/appi.ps.54.12.1582. [DOI] [PubMed] [Google Scholar]
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34(3):523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.