Abstract
Hydrochlorothiazide (HCTZ) is one of the most widely prescribed antihypertensive medications. Although it is well known that HCTZ is associated with hyperglycemia and hypertriglyceridemia, the mechanisms underlying these adverse effects are not well understood. We performed a genome-wide association study and meta-analysis of the change in fasting plasma glucose and triglycerides in response to HCTZ from two different clinical trials: the Pharmacogenomic Evaluation of Antihypertensive Responses and the Genetic Epidemiology of Responses to Antihypertensive studies. Two single-nucleotide polymorphisms (rs12279250 and rs4319515 (r2=0.73)), located at 11p15.1 in the NELL1 gene, achieved genome-wide significance for association with change in fasting plasma triglycerides in African Americans, whereby each variant allele was associated with a 28 mg dl−1 increase in the change in triglycerides. NELL1 encodes a cytoplasmic protein that contains epidermal growth factor-like repeats and has been shown to represses adipogenic differentiation. These findings may represent a novel mechanism underlying HCTZ-induced adverse metabolic effects.
Keywords: pharmacogenomics, NELL1, hydrochlorothiazide, hyperglycemia, hypertriglyceridemia
Introduction
Hypertension is major risk factor for stroke, cardiovascular and kidney diseases.1 Hydrochlorothiazide (HCTZ) is a widely prescribed thiazide diuretic for initial and combination drug treatment of hypertension2 with over 110 million prescriptions annually in the United States, but its ability to produce a variety of adverse metabolic effects (AMEs), such as hyperglycemia3, 4, 5 and dyslipidemia,3, 6, 7, 8 is well known. Despite being recognized for decades, the mechanisms of these thiazide-induced AMEs are not well understood. The ability of thiazides to increase glucose has primarily been attributed to their ability to cause hypokalemia,8, 9 thereby impairing insulin secretion. However, the associations between glucose increase and potassium lowering are mostly based on study-level associations of average changes, and we previously did not observe a relationship between patient-level changes in glucose and potassium, raising questions about this mechanism.10 More recently, additional mechanisms have been suggested including their ability to increase visceral and hepatic fat accumulation, which could promote insulin resistance.11 The mechanisms underlying thiazide-induced increases in triglycerides are even less well understood. It has been suggested that thiazides' ability to cause volume depletion produces hemoconcentration of lipoproteins. Volume contraction stimulates the renin–angiotensin–aldosterone system thereby stimulating catecholamine release and subsequent adipose tissue lipolysis. However, various studies have found that the degree of hemoconcentration is inconsistent.12, 13 Another possible mechanism is an incremental reduction of lipoprotein lipase activity due to interference in the production, release or action of insulin by HCTZ.13 One way to help identify underlying mechanisms of these adverse effects and to distinguish among these competing hypotheses is to identify genetic variations that are predictive of inter-individual variation in AME after HCTZ treatment. Using a genome-wide association study (GWAS) it is possible to identify genes or genomic regions associated with a phenotype without a priori knowledge of a biologic effect of the gene on the trait of interest. In this study, we report the results of the first GWAS of HCTZ-induced AMEs in European- and African-American hypertensive patients from two different pharmacogenetic studies.
Materials and methods
Study population
Phenotype and genotype data were collected from the Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR—clinicaltrials.gov identifier NCT00246519) study and the Genetic Epidemiology of Responses to Antihypertensive (GERA—clinicaltrials.gov identifier NCT00005520) study. In both studies, participants had mild-to-moderate primary hypertension without a history of heart disease or diabetes mellitus. Primary hypertension was defined as blood pressure (BP) levels >140/90 mm Hg or current use of prescription antihypertensive medications in the absence of a known cause for elevated BP. If at any time during the study protocols described below the average diastolic BP (DBP) rose to >110 mm Hg or the systolic BP to >180 mm Hg, participants were withdrawn from further study participation and prescribed effective antihypertensive drug therapy. Details about the study designs and exclusion and inclusion criteria have been described previously.14, 15 Briefly, in the PEAR study, individuals of any race-ethnicity and gender combination from age 17 to 65 years old with mild-to-moderate primary hypertension were recruited. Participants were enrolled in Gainesville, Fl, USA; Atlanta, GA, USA; and Rochester, MN, USA. All participants were newly diagnosed hypertensives, untreated hypertensives or treated hypertensives taking less than three antihypertensive drugs. The protocol of the study was as follows: a wash out period of approximately 4 weeks was done in order to remove the effects of previous BP medication (if any) from the participants. If at the end of the wash out period the average seated home DBP was>85 mm Hg, office DBP was>90 mm Hg and the home and office systolic BP was <180 mm Hg the individuals were enrolled into the randomized phase. All biological samples (blood and urine) were collected in the fasting state. As soon as the baseline evaluations were completed, the individuals were randomized to HCTZ (thiazide diuretic 12.5 mg orally once daily) or atenolol (β-blocker 50 mg orally once daily) for 3 weeks, with dose doubling (25 mg) for those with BP>120/70 mm Hg for an additional 6 weeks. More than 90% of PEAR participants received the higher 25 mg dose of HCTZ. For this AME GWAS analysis, we used only the patients randomized to the HCTZ from the PEAR study, referred to hereafter as PEAR HCTZ monotherapy.
In the GERA study, African Americans and European Americans with primary hypertension were recruited at Emory University in Atlanta, GA, USA and at the Mayo Clinic in Rochester, MN, USA, respectively. The protocol for the GERA study was as follows: a wash out period of at least 4 weeks was done in order to remove the effects of previous BP medication. If at the end of the wash out period the average office DBP was >90 mm Hg, qualifying individuals were treated with HCTZ (25 mg orally once daily) for 4 weeks. BP was measured in the seated position using a mercury sphygmomanometer and blood samples were obtained for baseline biochemical measurements. At the end of the 4-week diuretic treatment period, BP was measured and blood samples were again obtained for biochemical measurements. All blood collections were done in the morning after 8 h of fasting.
All patients enrolled in PEAR and GERA provided written informed consent, and the institutional review boards of participating study centers approved the study protocols.
Phenotype and genotype data
All biomedical measurements were made in a central laboratory at the Mayo Clinic. In the PEAR study, these methods were implemented on a Hitachi 911 Chemistry Analyzer (Roche Diagnostics, Indianapolis, IN, USA). In the GERA study, plasma glucose concentrations were determined by automated spectrophotometric methods implemented on an IL Monarch Chemistry system 760 (Instrumentation Laboratories, Lexington, MA, USA). Triglyceride concentrations were determined spectrophotometrically using Roche reagents on a Cobas Mira analyzer (Roche Diagnostics, Somerville, NJ, USA). In both studies, plasma glucose and triglyceride concentrations were measured at the end of the wash out period (baseline) and at the end of the HCTZ period (final). Glucose and triglyceride responses to HCTZ were defined as the difference between the levels at the final and the baseline visits. Individuals with response values under or over 3 standard errors from the mean response were removed from the analysis. Plasma insulin, which was used as a covariate during statistical analyses, was measured using the Access Ultrasensitive Insulin immunoassay system (Beckman Instruments, Chaska, MN, USA).
In the PEAR study, individuals were genotyped on the Illumina HumanOmni1-Quad (Illumina, San Diego, CA, USA). GERA participants from the opposite extremes of the DBP response distribution were genotyped using the GeneChip Human Mapping 500k Array (Affymetrics, Santa Clara, CA, USA) using standard procedures. As part of routine quality control steps, single-nucleotide polymorphisms (SNPs) with minor allele frequency <1%, call rates <95%, Hardy–Weinberg equilibrium P-values ⩾10−5 and individuals with >10% missing genotypes were removed from the analysis. The software MACH16 (www.sph.umich.edu/csg/abecasis/MACH/download) was used to impute the approximate 2.5 million HapMap SNPs using the phase II CEU as the reference panel for European Americans and a cosmopolitan sample of CEU and YRI for African Americans. Quality control for the imputed results was done using standard procedures (RSQ_HAT <0.3 and minor allele frequency ⩽0.05). MACH generated a file with the highest posterior probabilities for each imputed SNP, which was used in the analysis. After quality control and imputation, there were >2 million SNPs used for the genotype–phenotype association studies in each race-study group.
Statistical analysis
Analyses were done by self-reported race within each study and later the results were combined across studies within races using meta-analysis using a fixed effect model17 weighted by the inverse of the variance of the race and study-specific β-estimates. Linear regression assuming an additive model was performed using ProbABEL18 to evaluate the association between each SNP and metabolic responses to HCTZ. The variables sex, age, waist circumference, baseline glucose or triglycerides, and baseline insulin were used as covariates. The inclusion of the baseline value as covariate has both detractors19, 20 and supporters,21, 22 and our goal was to identify loci that influence change in glucose and triglycerides independent of any baseline effects.
To avoid the possibility of spurious association as the result of population substructure,23, 24 the two first principal component scores were used as covariates in the analysis. These principal component scores were obtained using the EIGENSTRAT24 software (genepath.med.harvard.edu/∼reich/EIGENSTRAT.htm). After meta-analysis, the definition of statistical significance was P<5 × 10−8 and the same direction of effects (that is, the sign of β) in each study. A statistically suggestive P-value was defined as P<1 × 10−5 and the same direction of effects and was used in order to avoid discounting true positive associations.
Results
Baseline characteristics of the European-American and African-American study participants are shown in Tables 1a and 1b, which shows the relative similarity in participant characteristics between the two studies. In both PEAR and GERA, there were a higher percentage of European-American male participants, while for African Americans there were a higher percentage of females. Average age and body mass index were nearly identical in PEAR and GERA. Baseline triglycerides were higher in European Americans from GERA compared with the other groups. Response to HCTZ treatment are shown in Table 2, and document that HCTZ significantly increased glucose and triglyceride in both race groups in both studies.
Table 1. PEAR and GERA sample characteristics measured at baseline.
| (a) Variables | PEAR: European Americans | GERA: European Americans |
|---|---|---|
| Total | 229 | 196 |
| Gender (% men) | 59.8 | 57.1 |
| Age (years) | 49.9±9.4 | 48.5±7.3 |
| Waist circumference (cm) | 94.8±13.6 | 103.7±14.7 |
| Insulin (μIU ml−1) | 9.4±8.7 | 8.5±4.9 |
| Plasma glucose (mg dl−1) | 92.9±12.2 | 92.4±12.5 |
| Plasma triglyceride (mg dl−1) | 149.6±100.9 | 184.3±97.55 |
| Systolic blood pressure (mm Hg) | 151.8±13.5 | 142.6±12.6 |
| Diastolic blood pressure (mm Hg) | 97.9±5.8 | 95±5.7 |
| (b) Variables | PEAR: African Americans | GERA: African Americans |
|---|---|---|
| Total | 148 | 194 |
| Gender (% men) | 37.84 | 48.5 |
| Age (years) | 47.4±8.9 | 47.4±6.3 |
| Waist circumference (cm) | 97.3±13.5 | 96.8±14.4 |
| Insulin (μIU ml−1) | 9.9±9.6 | 12.9±10.1 |
| Plasma glucose (mg dl−1) | 90.8±12.7 | 97.4±14.4 |
| Plasma triglyceride (mg dl−1) | 105.84±93.98 | 122.42±57.52 |
| Systolic blood pressure (mm Hg) | 151.8±13.14 | 150.8±14.9 |
| Diastolic blood pressure (mm Hg) | 97.9±5.8 | 97.2±5.5 |
Abbreviations: GERA, Genetic Epidemiology of Responses to Antihypertensive; PEAR, Pharmacogenomic Evaluation of Antihypertensive Responses.
Table 2. HCTZ treatment response in PEAR and GERA sample.
| (a) Variables | PEAR: European Americans | GERA: European Americans |
|---|---|---|
| Plasma glucose response (mg dl−1) | 1.44±8.9 (P=0.01) | 3.03±7.6 (P<0.0001) |
| Plasma triglyceride response (mg dl−1) | 8.21±58.7 (P=0.2) | 14.57±59.9 (P<0.0001) |
| (b) Variables | PEAR: African Americans | GERA: African Americans |
|---|---|---|
| Plasma glucose response (mg dl−1) | 2.55±10.8 (P<0.005) | 4.3±9.5 (P<0.0001) |
| Plasma triglyceride response (mg dl−1) | 7.95±40.6 (P=0.02) | 9.56±40.3 (P<0.0001) |
Abbreviations: GERA, Genetic Epidemiology of Responses to Antihypertensive; PEAR, Pharmacogenomic Evaluation of Antihypertensive Responses.
GWAS of adverse effect of HCTZ on glucose
The meta-analysis of glucose change during HCTZ treatment revealed no SNPs that achieved the a priori definition of genome-wide significance in either European Americans or African Americans. The Manhattan plots and QQ plots for these analyses are shown in the online Supplementary Figures S1 and S3 (Supplementary Information) However, in European Americans 48 SNPs from 8 genomic regions achieved our definition of suggestive significance with P<1 × 10−5 having effects in the same direction in both studies. Similarly, in African Americans 61 SNPs in 12 genomic regions met these criteria. Each of these SNPs is summarized in Supplementary Tables S1.1, S1.2 and S3.1, S3.2 (Supplementary Information).
GWAS of adverse effect of HCTZ on triglycerides
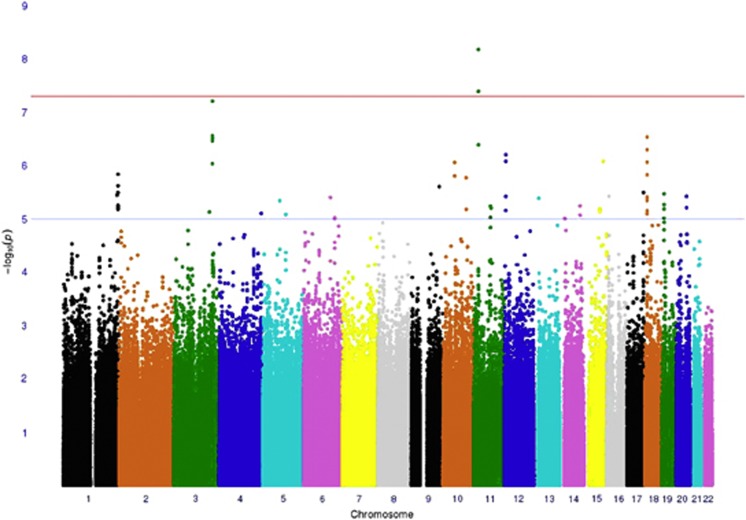
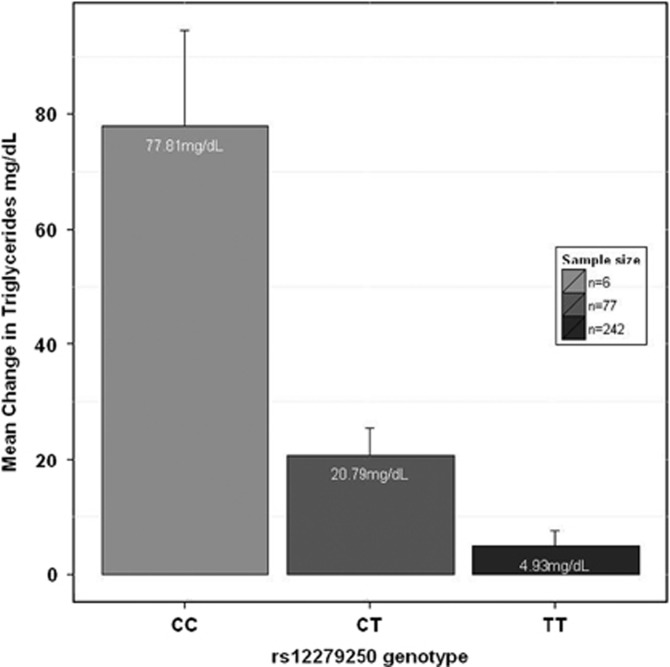
Among African Americans, two SNPs (rs12279250 and rs4319515 (r2=0.73)) on chromosome 11, reached genome-wide significance (β=28 mg dl−1, P=6.6 × 10−9 and β=27 mg dl−1, P=4.05 × 10−8, respectively). The Manhattan plot is shown in Figure 1, and Figure 2 displays the triglyceride response by genotype in both PEAR and GERA. These SNPs are in the NELL1 gene, whose encoded protein is involved in adipose cell differentiation.25 No SNPs achieved genome-wide significance for triglyceride response among European Americans.
Figure 1.
Genome-wide association study (GWAS) meta-analysis Manhattan plot showing the association of triglyceride response to hydrochlorothiazide (HCTZ) treatment in African Americans in the Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR) and the Genetic Epidemiology of Responses to Antihypertensive (GERA) studies. Two single nucleotide polymorphisms (SNPs) on chromosome 11 showed genome-wide significance (P=5 × 10−8). Eighteen loci showed P-values less than the suggestive threshold (P=1 × 10−5).
Figure 2.
Means change in triglycerides adjusted for sex, age, waist circumference, base line insulin, base line triglycerides, and the two principal components depending on rs12279250 genotype (CC, CT, TT) for Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR) and the Genetic Epidemiology of Responses to Antihypertensive (GERA) studies. Error bars represent s.e.m.
As was the case with the HCTZ-induced change in glucose, the triglyceride response also had many SNPs that met our suggestive significance threshold. In European Americans, 25 SNPs in 10 genomic regions met the threshold of P<1 × 10−5 with a same direction effect, with 77 SNPs in 27 genomic regions meeting this threshold in African Americans. Many of these SNPs were genes previously associated with metabolic syndrome, diabetes, insulin and other metabolic traits. These SNPs are described in detail in Supplementary Tables S2.1, S2.2 and S4.1, S4.2 (Supplementary Information).
Discussion
We conducted a GWAS and meta-analysis of adverse metabolic responses to HCTZ from two studies of hypertensive patients. We focused on change in glucose and triglycerides, which are known adverse effects of thiazide diuretics and may partially offset the antihypertensive benefit of HCTZ.3 Among African Americans, two SNPs in NELL1 achieved genome-wide significance for their association with triglyceride response. NELL-1 protein has osteoinductive properties26 and has been found to repress adipogenic differentiation in both unipotent preadipocytes and in multipotent adipose-derived stromal cells.25 The regulation of adipose stores through differentiation is tightly controlled, with adverse metabolic consequences of disordered fat storage occurring in the setting of either too much (obesity) or too little fat (lipodystrophy).27 Therefore, we conjecture that HCTZ could be modulating adipocyte differentiation through NELL1 leading to accumulation of plasma triglycerides in susceptible patients. Further studies to elucidate how HCTZ might influence NELL1 function are necessary. As our GWAS association was obtained through a meta-analysis, confirmation of these results will be required in an independent sample of hypertensive patients treated with HCTZ. However, this effect was observed in two independent samples included in the meta-analysis, and the magnitude of the effect is clinically relevant.
In addition to the SNPs achieving genome-wide significance for triglycerides, there were numerous other SNPs in both African Americans and Europeans Americans that met our suggestive threshold of 1 × 10−5 with same direction effects. These included SNPs in multiple genes that have previously been associated with a variety of relevant metabolic traits. For example, in European Americans SNP rs17560407 in chromosome 5 had the lowest P-value (P=5.41 × 10−7) for triglyceride response. This SNP is close to the myocyte enhancer factor 2C gene, which regulates GLUT4 expression in both skeletal muscle and adipose tissue28 and has been associated with type 2 diabetes.29 Another gene related to GLUT4 translocation in adipocytes30 in which we had a suggestive signal for triglyceride response is the pleckstrin homology-like domain, family B, member 1(PHLDB1) located on chromosome 11 (rs11216831, P=4.11 × 10−6). On chromosome 7, rs4722750 (P=8.51 × 10−6) is close to the JAZF zinc-finger 1 gene,31, 32 which was previously identified in a GWAS of type 2 diabetes. Similarly, among African Americans we also identified a number of SNPs in genes previously associated with metabolic traits. For example, genes that have been related to the metabolic syndrome include angiopoietin-like 6 (ref. 33) on chromosome 19 (rs2116940, P=3.39 × 10−6), growth differentiation factor 3 (ref. 34) on chromosome 12 (rs12307997, P=6.24 × 10−7) and ubiquitin-like 5 (ref. 35) on chromosome 19 (rs2116940, P=3.39 × 10−6). On chromosome 1 and close to rs11810574 (P=3.60 × 10−6) is the gene cholinergic receptor muscarinic 3, which has been associated with insulin secretion.36
For glucose response, no SNP achieved genome-wide significance in either race group, but as with triglycerides, there were many reaching our suggestive threshold that have previously been associated with diabetes or other metabolic traits. Specifically, the region near rs7762018 was associated with type 1 diabetes in an affected sib-pair analysis,37 and confirmed later in a larger family study38 and later in GWA studies.39 Previous meta-analysis40 and candidate gene study41 have shown a significantly increased risk of type 2 diabetes with the polymorphism Thr394Thr(G/A) in the peroxisome proliferator-activated receptor gamma, coactivator 1 alpha gene in Indians and Asians, which is close to rs1511453 (P=4.71 × 10−6) on chromosome 4. The SNP rs6859974 is close to the mannosyl (alpha-1,3)-glycoprotein beta-1,2-N-acetylglucosaminyltransferase gene (MGAT1) which is related to fatty acid metabolism.42 MGAT1 was also previously associated with obesity in linkage and GWAS.43 SNPs with suggestive associations in African Americans for glucose response included SNPs from two genes previously reported in other GWAS of T2D,44 major facilitator superfamily domain containing 9 close to rs13402330 (P=5.58 × 10−6) on chromosome 2 and branched chain amino-acid transaminase 1, close to rs7965364 (P=6 × 10−6) on chromosome 12. In another region on chromosome 12, the SNP rs7964748 (P=2.45 × 10−6) is next to the insulin-like growth factor 1 gene, which is associated to fasting insulin and insulin resistance (homeostatic model assessment-insulin resistance).45 SNP rs225675, located on chromosome 6, and is near G protein-coupled receptor 126 gene, which was associated with body mass index in a previous GWAS.46
It has been hypothesized that the mechanism by which HCTZ leads to hyperglycemia involves increased potassium excretion and hypokalemia leading to defects in insulin secretion.47 However, this hypothesis has been controversial given that many genetic causes of chronic hypokalemia (for example, Gitelman's syndrome) are not associated with hyperglycemia or increased risk of diabetes.48 Therefore, it is interesting to note that none of the genes identified to be suggestively associated with change in glucose were obviously related to potassium transport or excretion.8 As such, our results are more consistent with a mechanism involving insulin resistance, perhaps secondary to visceral fat redistribution and hepatic fat accumulation as suggested by Eriksson et al.11
Herein, we report the first GWAS to our knowledge of HCTZ-induced AMEs. The strengths of this study include the population-based design, the high quality of genotyping and phenotyping, the wash out period of all antihypertensives before initiation of HCTZ, as well as detailed follow-up of study participants. At the same time, we are aware of the limitation posed by small sample sizes, especially to detect true effects size. We are also aware of possible biases resulting from inclusion of the baseline value as a covariate.19 Although under-powered, it is interesting to note that many of our suggestive regions have been identified through previous GWAS results as being related to type 2 diabetes, obesity, fatty acid metabolism, lipid metabolism, glucose metabolism or body mass index or to other a priori identified biologic candidate genes (please see http://hyper.ahajournals.org). However, the associations we have identified are novel in that they have not previously been related to drug-induced adverse metabolic side effects. These findings may help provide insight into the mechanisms of antihypertensive-induced AMEs. It will be important to replicate these findings identified through meta-analysis in independent populations of individuals treated with thiazide diuretics.
Acknowledgments
We acknowledge and thank the valuable contributions of the study participants, study physicians, support staff and the technical assistance: Zhiying Wang, Megan Grove, Jodie Van De Rostyne, Jeremy Palbicki, Robert Tarrell and Prabin Thapa. The GERA study was supported by NIH grants HL74735, HL53335, and the Mayo Foundation. The PEAR study was supported by a grant from the National Institutes of Health (Bethesda, MD, USA), grant U01 GM074492, funded as part of the Pharmacogenetics Research Network. This work was also supported by the following grants from the NIH National Center for Research Resources: grant M01 RR00082 and UL1 RR029890 to the University of Florida, grants UL1 RR025008 and M01 RR00039 to Emory University, and UL1 RR024150 to Mayo Clinic.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website (http://www.nature.com/tpj)
Supplementary Material
References
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens (Greenwich ) 2010;12:927–934. doi: 10.1111/j.1751-7176.2010.00373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston MC. The effects of antihypertensive drugs on glucose intolerance in hypertensive nondiabetics and diabetics. Am Heart J. 1988;115:640–656. doi: 10.1016/0002-8703(88)90816-2. [DOI] [PubMed] [Google Scholar]
- Pepine CJ, Cooper-Dehoff RM. Cardiovascular therapies and risk for development of diabetes. J Am Coll Cardiol. 2004;44:509–512. doi: 10.1016/j.jacc.2004.03.071. [DOI] [PubMed] [Google Scholar]
- Verdecchia P, Reboldi G, Angeli F, Borgioni C, Gattobigio R, Filippucci L, et al. Adverse prognostic significance of new diabetes in treated hypertensive subjects. Hypertension. 2004;43:963–969. doi: 10.1161/01.HYP.0000125726.92964.ab. [DOI] [PubMed] [Google Scholar]
- Lakshman MR, Reda DJ, Materson BJ, Cushman WC, Freis ED. Diuretics and beta-blockers do not have adverse effects at 1 year on plasma lipid and lipoprotein profiles in men with hypertension. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Arch Intern Med. 1999;159:551–558. doi: 10.1001/archinte.159.6.551. [DOI] [PubMed] [Google Scholar]
- Mantel-Teeuwisse AK, Kloosterman JM, Maitland-van der Zee AH, Klungel OH, Porsius AJ, de BA. Drug-induced lipid changes: a review of the unintended effects of some commonly used drugs on serum lipid levels. Drug Saf. 2001;24:443–456. doi: 10.2165/00002018-200124060-00003. [DOI] [PubMed] [Google Scholar]
- Sica DA. Diuretic-related side effects: development and treatment. J Clin Hypertens (Greenwich ) 2004;6:532–540. doi: 10.1111/j.1524-6175.2004.03789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan NM.Clinical Hypertension7th editionWillians & Wilkins; 1998 [Google Scholar]
- Smith SM, Anderson SD, Wen S, Gong Y, Turner ST, Cooper-Dehoff RM, et al. Lack of correlation between thiazide-induced hyperglycemia and hypokalemia: subgroup analysis of results from the pharmacogenomic evaluation of antihypertensive responses (PEAR) study. Pharmacotherapy. 2009;29:1157–1165. doi: 10.1592/phco.29.10.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson JW, Jansson PA, Carlberg B, Hagg A, Kurland L, Svensson MK, et al. Hydrochlorothiazide, but not Candesartan, aggravates insulin resistance and causes visceral and hepatic fat accumulation: the mechanisms for the diabetes preventing effect of Candesartan (MEDICA) Study. Hypertension. 2008;52:1030–1037. doi: 10.1161/HYPERTENSIONAHA.108.119404. [DOI] [PubMed] [Google Scholar]
- Perez-Stable E, Caralis PV. Thiazide-induced disturbances in carbohydrate, lipid, and potassium metabolism. Am Heart J. 1983;106:245–251. doi: 10.1016/0002-8703(83)90124-2. [DOI] [PubMed] [Google Scholar]
- Grimm RH, Leon AS, Hunninghake DB, Lenz K, Hannan P, Blackburn H. Effects of thiazide diuretics on plasma lipids and lipoproteins in mildly hypertensive patients: a double-blind controlled trial. Ann Intern Med. 1981;94:7–11. doi: 10.7326/0003-4819-94-1-7. [DOI] [PubMed] [Google Scholar]
- Johnson JA, Boerwinkle E, Zineh I, Chapman AB, Bailey K, Cooper-Dehoff RM, et al. Pharmacogenomics of antihypertensive drugs: rationale and design of the Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR) study. Am Heart J. 2009;157:442–449. doi: 10.1016/j.ahj.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AB, Schwartz GL, Boerwinkle E, Turner ST. Predictors of antihypertensive response to a standard dose of hydrochlorothiazide for essential hypertension. Kidney Int. 2002;61:1047–1055. doi: 10.1046/j.1523-1755.2002.00200.x. [DOI] [PubMed] [Google Scholar]
- Li Y, Willer C, Sanna S, Abecasis G. Genotype imputation. Annu Rev Genomics Hum Genet. 2009;10:387–406. doi: 10.1146/annurev.genom.9.081307.164242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normand SL. Meta-analysis: formulating, evaluating, combining, and reporting. Stat Med. 1999;18:321–359. doi: 10.1002/(sici)1097-0258(19990215)18:3<321::aid-sim28>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Aulchenko YS, Struchalin MV, van Duijn CM. ProbABEL package for genome-wide association analysis of imputed data. BMC Bioinformatics. 2010;11:134. doi: 10.1186/1471-2105-11-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour MM, Weuve J, Berkman LF, Kawachi I, Robins JM. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am J Epidemiol. 2005;162:267–278. doi: 10.1093/aje/kwi187. [DOI] [PubMed] [Google Scholar]
- McArdle PF, Whitcomb BW. Improper adjustment for baseline in genetic association studies of change in phenotype. Hum Hered. 2009;67:176–182. doi: 10.1159/000181156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee for Proprietary Medicinal Products (CPMP) Committee for Proprietary Medicinal Products (CPMP): points to consider on adjustment for baseline covariates. Stat Med. 2004;23:701–709. doi: 10.1002/sim.1647. [DOI] [PubMed] [Google Scholar]
- Senn S. Change from baseline and analysis of covariance revisited. Stat Med. 2006;25:4334–4344. doi: 10.1002/sim.2682. [DOI] [PubMed] [Google Scholar]
- Campbell CD, Ogburn EL, Lunetta KL, Lyon HN, Freedman ML, Groop LC, et al. Demonstrating stratification in a European American population. Nat Genet. 2005;37:868–872. doi: 10.1038/ng1607. [DOI] [PubMed] [Google Scholar]
- Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet. 2006;38:904–909. doi: 10.1038/ng1847. [DOI] [PubMed] [Google Scholar]
- James AW, Pan A, Chiang M, Zara JN, Zhang X, Ting K, et al. A new function of Nell-1 protein in repressing adipogenic differentiation. Biochem Biophys Res Commun. 2011;411:126–131. doi: 10.1016/j.bbrc.2011.06.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Kuroda S, Carpenter D, Nishimura I, Soo C, Moats R, et al. Craniosynostosis in transgenic mice overexpressing Nell-1. J Clin Invest. 2002;110:861–870. doi: 10.1172/JCI15375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis GF, Carpentier A, Adeli K, Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr Rev. 2002;23:201–229. doi: 10.1210/edrv.23.2.0461. [DOI] [PubMed] [Google Scholar]
- Thai MV, Guruswamy S, Cao KT, Pessin JE, Olson AL. Myocyte enhancer factor 2 (MEF2)-binding site is required for GLUT4 gene expression in transgenic mice. Regulation of MEF2 DNA binding activity in insulin-deficient diabetes. J Biol Chem. 1998;273:14285–14292. doi: 10.1074/jbc.273.23.14285. [DOI] [PubMed] [Google Scholar]
- Lu W, Yan X, Huang Q, Hu Y, Zhong M, Huang Z, et al. [Study of the 482G/A variation in PGC-1alpha gene domain MEF2C as possible mechanism of type 2 diabetes] Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2008;25:616–623. [PubMed] [Google Scholar]
- Zhou QL, Jiang ZY, Mabardy AS, Del Campo CM, Lambright DG, Holik J, et al. A novel pleckstrin homology domain-containing protein enhances insulin-stimulated Akt phosphorylation and GLUT4 translocation in adipocytes. J Biol Chem. 2010;285:27581–27589. doi: 10.1074/jbc.M110.146886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees SD, Hydrie MZ, Shera AS, Kumar S, O'Hare JP, Barnett AH, et al. Replication of 13 genome-wide association (GWA)-validated risk variants for type 2 diabetes in Pakistani populations. Diabetologia. 2011;54:1368–1374. doi: 10.1007/s00125-011-2063-2. [DOI] [PubMed] [Google Scholar]
- Vangipurapu J, Stancakova A, Pihlajamaki J, Kuulasmaa TM, Kuulasmaa T, Paananen J, et al. Association of indices of liver and adipocyte insulin resistance with 19 confirmed susceptibility loci for type 2 diabetes in 6,733 non-diabetic Finnish men. Diabetologia. 2011;54:563–571. doi: 10.1007/s00125-010-1977-4. [DOI] [PubMed] [Google Scholar]
- Legry V, Goumidi L, Huyvaert M, Cottel D, Ferrieres J, Arveiler D, et al. Association between angiopoietin-like 6 (ANGPTL6) gene polymorphisms and metabolic syndrome-related phenotypes in the French MONICA Study. Diabetes Metab. 2009;35:287–292. doi: 10.1016/j.diabet.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Tobin JF, Celeste AJ. Bone morphogenetic proteins and growth differentiation factors as drug targets in cardiovascular and metabolic disease. Drug Discov Today. 2006;11:405–411. doi: 10.1016/j.drudis.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Jowett JB, Elliott KS, Curran JE, Hunt N, Walder KR, Collier GR, et al. Genetic variation in BEACON influences quantitative variation in metabolic syndrome-related phenotypes. Diabetes. 2004;53:2467–2472. doi: 10.2337/diabetes.53.9.2467. [DOI] [PubMed] [Google Scholar]
- Guo Y, Traurig M, Ma L, Kobes S, Harper I, Infante AM, et al. CHRM3 gene variation is associated with decreased acute insulin secretion and increased risk for early-onset type 2 diabetes in Pima Indians. Diabetes. 2006;55:3625–3629. doi: 10.2337/db06-0379. [DOI] [PubMed] [Google Scholar]
- Luo DF, Bui MM, Muir A, Maclaren NK, Thomson G, She JX. Affected-sib-pair mapping of a novel susceptibility gene to insulin-dependent diabetes mellitus (IDDM8) on chromosome 6q25-q27. Am J Hum Genet. 1995;57:911–919. [PMC free article] [PubMed] [Google Scholar]
- Luo DF, Buzzetti R, Rotter JI, Maclaren NK, Raffel LJ, Nistico L, et al. Confirmation of three susceptibility genes to insulin-dependent diabetes mellitus: IDDM4, IDDM5 and IDDM8. Hum Mol Genet. 1996;5:693–698. doi: 10.1093/hmg/5.5.693. [DOI] [PubMed] [Google Scholar]
- Bradfield JP, Qu HQ, Wang K, Zhang H, Sleiman PM, Kim CE, et al. A genome-wide meta-analysis of six type 1 diabetes cohorts identifies multiple associated Loci. PLoS Genet. 2011;7:e1002293. doi: 10.1371/journal.pgen.1002293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Mo X, Chen S, Lu X, Gu D. Association of peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PPARGC1A) gene polymorphisms and type 2 diabetes mellitus: a meta-analysis. Diabetes Metab Res Rev. 2011;27:177–184. doi: 10.1002/dmrr.1158. [DOI] [PubMed] [Google Scholar]
- Song J, Liu YY, Long Y, Tian HM, Liu R, Li XJ, et al. [PPARGC1A gene Thr394Thr G/A polymorphism and its association with type 2 diabetes mellitus and insulin resistance in a Chinese population] Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2010;27:550–553. doi: 10.3760/cma.j.issn.1003-9406.2010.05.016. [DOI] [PubMed] [Google Scholar]
- Jacobsson JA, Rask-Andersen M, Riserus U, Moschonis G, Koumpitski A, Chrousos GP, et al. Genetic variants near the MGAT1 gene are associated with body weight, BMI and fatty acid metabolism among adults and children. Int J Obes (Lond) 2011;36:119–129. doi: 10.1038/ijo.2011.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson A, Marroni F, Hayward C, Franklin CS, Kirichenko AV, Jonasson I, et al. Linkage and genome-wide association analysis of obesity-related phenotypes: association of weight with the MGAT1 gene. Obesity (Silver Spring) 2010;18:803–808. doi: 10.1038/oby.2009.359. [DOI] [PubMed] [Google Scholar]
- Rampersaud E, Damcott CM, Fu M, Shen H, McArdle P, Shi X, et al. Identification of novel candidate genes for type 2 diabetes from a genome-wide association scan in the Old Order Amish: evidence for replication from diabetes-related quantitative traits and from independent populations. Diabetes. 2007;56:3053–3062. doi: 10.2337/db07-0457. [DOI] [PubMed] [Google Scholar]
- Dupuis J, Langenberg C, Prokopenko I, Saxena R, Soranzo N, Jackson AU, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010;42:105–116. doi: 10.1038/ng.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JZ, Medland SE, Wright MJ, Henders AK, Heath AC, Madden PA, et al. Genome-wide association study of height and body mass index in Australian twin families. Twin Res Hum Genet. 2010;13:179–193. doi: 10.1375/twin.13.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte JD, Cooper-Dehoff RM. Mechanisms for blood pressure lowering and metabolic effects of thiazide and thiazide-like diuretics. Expert Rev Cardiovasc Ther. 2010;8:793–802. doi: 10.1586/erc.10.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison DH, Loffing J. Thiazide effects and adverse effects: insights from molecular genetics. Hypertension. 2009;54:196–202. doi: 10.1161/HYPERTENSIONAHA.109.129171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.