Abstract
Objective To determine whether, and to what extent, fall prevention exercise interventions for older community dwelling people are effective in preventing different types of fall related injuries.
Data sources Electronic databases (PubMed, the Cochrane Library, Embase, and CINAHL) and reference lists of included studies and relevant reviews from inception to July 2013.
Study selection Randomised controlled trials of fall prevention exercise interventions, targeting older (>60 years) community dwelling people and providing quantitative data on injurious falls, serious falls, or fall related fractures.
Data synthesis Based on a systematic review of the case definitions used in the selected studies, we grouped the definitions of injurious falls into more homogeneous categories to allow comparisons of results across studies and the pooling of data. For each study we extracted or calculated the rate ratio of injurious falls. Depending on the available data, a given study could contribute data relevant to one or more categories of injurious falls. A pooled rate ratio was estimated for each category of injurious falls based on random effects models.
Results 17 trials involving 4305 participants were eligible for meta-analysis. Four categories of falls were identified: all injurious falls, falls resulting in medical care, severe injurious falls, and falls resulting in fractures. Exercise had a significant effect in all categories, with pooled estimates of the rate ratios of 0.63 (95% confidence interval 0.51 to 0.77, 10 trials) for all injurious falls, 0.70 (0.54 to 0.92, 8 trials) for falls resulting in medical care, 0.57 (0.36 to 0.90, 7 trials) for severe injurious falls, and 0.39 (0.22 to 0.66, 6 trials) for falls resulting in fractures, but significant heterogeneity was observed between studies of all injurious falls (I2=50%, P=0.04).
Conclusions Exercise programmes designed to prevent falls in older adults also seem to prevent injuries caused by falls, including the most severe ones. Such programmes also reduce the rate of falls leading to medical care.
Introduction
Fall related injuries are common,1 2 3 result in considerable healthcare utilisation, and are a major cause of long term pain and functional impairment among older adults.4 They also increase considerably the risk of discharge to a nursing home5 and have a high economic cost.6
It has been established that well designed exercise programmes can prevent falls in older adults living at home.7 8 However, evidence that these programmes can also prevent injuries caused by falls is poor. This void is partly because most previous trials were underpowered to examine the effect of exercise on injurious falls, in particular the most severe falls. In a supplementary analysis, the recently updated Cochrane review of interventions for preventing falls in older adults living at home examined the effect of exercise on fractures specifically.7 This analysis, which was based on six trials, showed that fall prevention exercise programmes are associated with a significantly lower risk of fractures.
To our knowledge, no review or meta-analysis has examined the effect of fall prevention exercise programmes on other injurious falls outcomes that are common and that can also have important medical, psychological, and economic consequences. Besides causing fractures or other serious injuries, falls leading to medical care ought to be considered since their cost to society is high and their burden on the healthcare system heavy.6 9 Even falls causing relatively minor injuries are important to consider, as they too may have serious consequences, such as diminished self confidence, social isolation, and restriction on activity, which in turn will accelerate functional decline and increase the risk of placement in a nursing home.4
Using a meta-analytical approach, we reviewed the current evidence about the effect of exercise interventions designed for community dwelling older adults on different outcomes of injurious falls, based on severity or medical care. There is no consensus about the outcomes of fall related injuries that should be evaluated in controlled trials, and published trials reporting injurious falls use quite different definitions.10
Methods
An essential first step of our work was to group definitions of injurious falls found in the studies selected for this review into more homogeneous categories to allow pooling of data. This systematic review was conducted in accordance with the PRISMA guidelines.11
Search strategy and study selection
We searched the Cochrane Library, PubMed, Embase, and CINAHL to identify relevant studies published in peer reviewed journals from inception to July 2013. In the Cochrane Library the search terms were: (fall) and (exercise or tai chi or training or physical activity) excluding (Alzheimer or Parkinson’s or dementia or nursing home or protocol or athletes) in the title or abstract of trials, with the word “prevention” in the text and the word variations option enabled. We also selected references in relevant reviews for screening.7 8 10 Two investigators (FEK, PDM) independently screened the titles, abstracts, and full text of identified papers to determine their eligibility for inclusion (see supplementary file). Discrepancies were resolved by discussion.
Inclusion criteria were randomised controlled trials of fall prevention exercise interventions, published in English or French, targeting community dwelling adults aged over 60 years, and providing quantitative data on injurious falls, serious falls, fall related injuries, or fall induced fractures. We included studies where exercise was compared with no intervention (usual activity or usual care) or a placebo control intervention (for example, general health education classes, social visits, or a low intensity exercise programme not designed to modify the risk of falling). We excluded studies in which exercise was part of a multifactorial programme such that participants received other interventions (for example, home management, visual treatment) in addition to exercise, and when participants were selected for a specific neurodegenerative disease or any other characteristic that greatly affected the risk of falling but was not correctable by exercise (such as severe visual impairment).
Data extraction and quality assessment
We used a form designed for this review to extract data on study and intervention characteristics, quality assessment, and outcomes (see supplementary file). The taxonomy for fall prevention interventions developed by the Prevention of Falls Network Europe (ProFaNE)12 was used to describe the characteristics of the interventions provided (for example, participants’ selection criteria, type of exercises, and intervention procedures). This tool uses internationally agreed criteria to evaluate systematically the content and format of fall prevention interventions. We also extracted the definitions and methods used to collect falls and to classify fall related injuries, as well as the number, rate, or risk ratio of injurious falls and any available data on the nature of the injuries. We contacted authors of included articles to obtain more detailed data on the outcomes of injurious falls (for example, if authors reported the number of participants with an injurious fall but not the total number of injurious falls, or data on falls resulting in fractures but not data on other injurious falls).
After reviewing the case definitions used in the selected studies, we sought to group definitions of injurious falls into more homogeneous categories to allow results to be compared across studies and the data to be pooled. The ProFaNE group recently proposed a standardised classification of injurious falls to be used in future randomised controlled trials.10 As a foundation for developing a retrospective classification of the definitions of injurious falls found in the studies selected for this review, we used the ProFaNE classification along with the standardised classification of Campbell and Robertson,13 which is the classification most often used in published trials of these interventions.14 We also recorded any reports of adverse effects associated with interventions.
We followed the recommendations of the Cochrane Collaboration15 to assess risk of bias in the following domains: random sequence generation (selection bias), allocation concealment (selection bias), blinding of the assessment of falls and injurious falls (detection bias), and incomplete outcome data (attrition bias). We also assessed bias in the recall of falls owing to unreliable methods of ascertainment,16 using the criteria developed for the Cochrane review of fall prevention trials.7 The methods used to confirm serious injurious falls were also examined: we judged self reports from participants to be at a high risk of bias, whereas we considered the use of medical records or radiography reports (for fractures) to be at low risk. Two authors (FEK, PDM) independently assessed the risks of bias and extracted data. Disagreement was resolved by consensus or adjudication by a third party.
Statistical analysis
The rate ratio of injurious falls was the outcome of interest. If the rate ratio was not presented in the article, we calculated it from the ratio of the total number of injurious falls divided by the total length of time falls were monitored (person years) in the two comparison groups. In cases where data were available only for people who had completed the study, or where the trial authors had stated there were no losses to follow-up, we assumed that these participants had been followed up for the maximum possible period. We estimated the standard error of the rate ratio by using the formula given in the Cochrane handbook.17
We used the generic inverse variance method in Review Manager (RevMan 5.1) to group the trial results and we compiled forest plots for each category of injurious falls. To allow for variability among the participants, type of exercise intervention, and outcome definitions we used a random effect model. We report the pooled rate ratios for each injurious fall outcome, along with 95% confidence intervals. We assessed heterogeneity with the Q test and the I² statistic.18
We conducted a prespecified subgroup analysis based on fall risk at enrolment (a priori); that is, trials with participants selected for inclusion based on fall history or other specific risk factors for falling (at higher risk) compared with non-selected participants. We also explored the possible impact of risk of bias on statistically significant pooled estimates of exercise effect by removing studies of poorer quality—that is, those for which the risk of bias was unclear for at least three of the quality components considered, or the risk was at least unclear for one category and high for another. To explore the possibility of publication bias we constructed funnel plots of effect estimates against their standard errors for analyses that contained at least 10 data points.
Results
The search strategy produced 1011 potentially eligible papers. Based on titles and abstracts we sought the full text articles of 199 selected references. Ultimately this systematic review included 17 trials (fig 1).
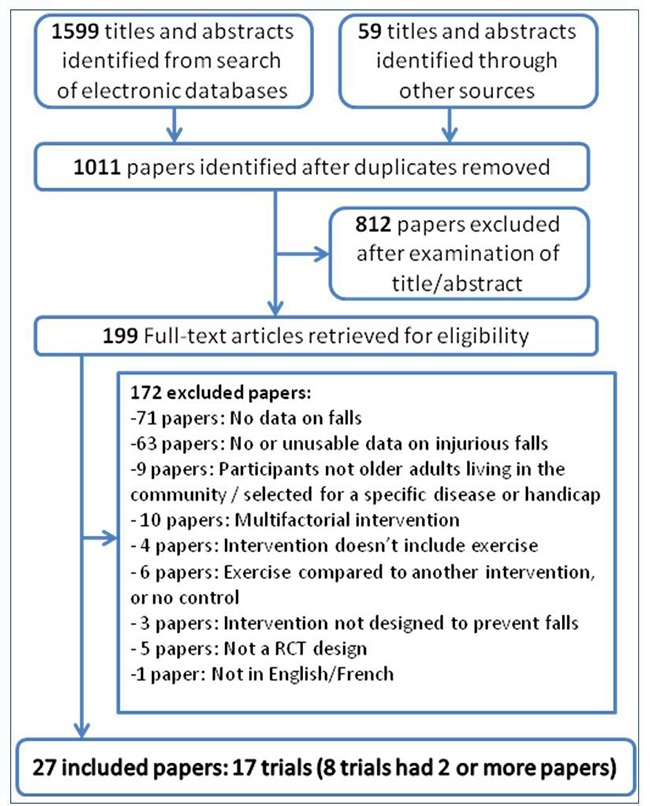
Fig 1 Flow chart of study identification process
Characteristics of included studies and interventions
The 17 studies in the meta-analysis included a total of 2195 participants randomised in the exercise groups and 2110 randomised in the control groups, with sample sizes in individual studies ranging from 53 to 486 participants. The mean age of the overall population was 76.7 years, and around 77% were women. Seven studies selected participants based on a higher risk of falls—that is, history of falling, age over 80 years, or physical limitations (as measured by simple functional tests).13 19 20 21 22 23 24 Fourteen trials delivered the exercise intervention in a group setting, and six of those supplemented the group sessions with home exercise. In the other three trials, the intervention consisted of individualised exercises delivered at home.13 22 25 Tai Chi was the exclusive exercise intervention in two of the studies26 27; the rest of the interventions included a gait, balance, and functional training component. Most also included strength/resistance training exercises. One study compared two similar multiple component exercise interventions, one with added endurance training, with the control group.20 In the analysis, the two exercise groups were combined to create a single pairwise comparison (intervention versus control). Table 1 summarises the characteristics of the included studies.
Table 1.
Study characteristics
| Trial | No randomised (% women) | Mean age (years) | Participant selection criteria | Type of exercise* | Moderate to high challenge to balance† | Mode of delivery | Exercise sessions frequency | Programme duration | Follow-up period (for recording fall data) (months) | Comparison group | Rate ratio‡ for all falls (fall rate in controls (person/year)) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Barnett 200319 | 163 (67) | 74.9 | ≥65, ≥1 risk factors for falling | Gait, balance, and functional training; strengthening exercises; flexibility | Yes | Home exercise+group exercise | 1 hour/week plus home exercise | 1 year | 12 | No intervention | 0.60 (0.36 to 1.00) (0.95) |
| Campbell 199713 | 233 (100) | 84.1 | ≥80 | Gait, balance, and functional training; strengthening exercises; flexibility; general physical activity | Yes | Home exercise | 30 minutes×3/week | 1 year | 12 | Social visit by research nurse | 0.68 (0.51 to 0.89) (1.34) |
| Cornillon 200231 | 303 (83) | 71 | ≥65, activities of daily living independent | Gait, balance, and functional training | Yes | Group exercise | 1 session/week | 8 weeks | 12 | No intervention | 0.82 (0.58 to 1.17) (0.47) |
| Fitzharris 201028 | 1090 (59.8) | 76.1 | ≥70 | Gait, balance, and functional training; strengthening exercises; flexibility | No | Home exercise+group exercise | 1 hour/week+daily home exercise | 15 weeks | 18 | Factorial design: all groups that did not have exercise | 0.79 (0.66 to 0.94) (1.14) |
| Freiberger 201220 | 207 (44) | 76.1 | ≥70, fell in past 6 months or fear of falling | Gait, balance, and functional training; strengthening exercises; endurance | Yes | Group exercise | 1 hour×2/week | 16 weeks | 24 | No intervention | 0.82 (0.62 to 1.08) (0.67) |
| Haines 200921 | 53 (60) | 80.7 | ≥65, gait instability or use of mobility aid; discharged from hospital | Gait, balance, and functional training; strengthening exercises; 3D (modified Tai Chi exercises) | Yes | Home exercise | 3 to 7/week | 18 weeks | 6 | No intervention | 0.72 (0.33 to 1.57) (1.09) |
| Kemmler 201029 | 246 (100) | 69.1 | ≥65 | Gait, balance, and functional training; strengthening exercises; flexibility | No | Home exercise+group exercise | 60 minutes×2/week+home exercise (20 minutes×2/week) | 18 month | 18 | Low to moderate intensity (low frequency) “Wellness programme” | 0.60 (0.47 to 0.76) (0.28) |
| Korpelainen 200633 | 160 (100) | 73 | Low bone mineral density (hip T score <2) | Gait, balance, and functional training; strengthening exercises; 3D (dancing) | Yes | Home exercise+group exercise | 1 hour/week+home exercise (20 minutes daily) | 18 month | 30 | Twice yearly seminars on health related topics | 0.79 (0.59 to 1.06) (0.53) |
| Li 200526 | 256 (70) | 77.5 | ≥70, walks independently | 3D (Tai Chi) | Yes | Group exercise | 1 hour×3/week | 26 weeks | 6 | Low level stretching | 0.45 (0.29 to 0.69) (0.53) |
| Luukinen 200722 | 486 (78) | 88 | ≥85, ≥1 risk factor for falling, or ≥2 falls in past year | Gait, balance, and functional training; flexibility; general physical activity; other | No | Home exercise+group exercise | Individually prescribed, frequency depends on individuals | 16 months | 16 | Asked to visit general practitioner without written intervention form | 0.93 (0.80 to 1.09) (1.15) |
| McRae 199432 | 80 (100) | 71.1 | ≥60 | Gait, balance, and functional training | No | Group exercise | 1hour×3/week | 1 year | 12 | Group discussions (health promotion, safety education) | 1.28 (0.90. 1.83) (—) |
| McMurdo 199734 | 118 (100) | 64.5 | ≥60, postmenopausal | Gait, balance, and functional training; strengthening exercises | No | Group exercise | 45minutes×3/week | 30 weeks | 24 | 1000 mg calcium carbonate daily (also in intervention group) | 0.53 (0.28 to 1.00) (—) |
| Means 200530 | 338 (57) | 73.5 | ≥65, able to walk at least 30 feet without assistance | Gait, balance, and functional training; strengthening exercises; flexibility | No | Group exercise | 90 minutes×3/week | 6 weeks | 6 | Group seminars on non-health related topics | 0.41 (0.27 to 0.62) (1.18) |
| Robertson 200125 | 240 (68) | 80.9 | ≥75 | Gait, balance, and functional training; strengthening exercises; flexibility; general physical activity | Yes | Home exercise | Individually prescribed; at least 3 times a week (about 30 min/session+walking 2×/week | 1 year | 12 | Usual care | 0.54 (0.3 to 0.90) (1.01) |
| Skelton 200523 | 100 (100) | 72.8 | ≥65, ≥3 falls in past year | Gait, balance, and functional training; strengthening exercises; flexibility; endurance | Yes | Home exercise+group exercise | 1 hour/week+home exercise (30 minutes×2/week) | 36 weeks | 9 | Home based seated exercises not designed to improve fitness or balance | 0.69 (0.50 to 0.96) (3.12) |
| Smulders 201024 | 96 (94) | 71 | ≥65, osteoporosis, ≥1 falls in past year; able to walk 15 minutes without device | Gait, balance, and functional training; general physical activity; endurance; other | Yes | Group exercise | 11 exercise sessions | 5.5 weeks | 12 | Usual care | 0.61 (0.40 to 0.94) (1.18) |
| Wolf 199627 | 136 (81) | 76.2 | ≥70, ambulatory | 3D (Tai Chi) | Yes | Group exercise | 45 minutes/week | 15 weeks | 8 | Group discussions on topics of interest to older people | 0.67 (0.41 to 1.09) (1.82) |
*ProFaNe classification of exercise intervention.12
†Moderately challenging=two of the following criteria, or highly challenging=all three criteria: movement of the centre of mass, narrowing of the base of support, and minimising limb support.54
‡Ratio of risk of being a faller in two comparison groups.
Classification of injurious falls
The definition and classification of injurious falls varied substantially and most trials did not provide a reference for their definition. Injurious falls usually included diverse consequences, ranging from relatively minor injuries such as bruises or abrasions to fractures or other serious injuries requiring hospital admission.19 25 26 28 Most often the definition referred to either the presence of symptoms or the use of medical care.13 19 25 26 28 In other cases, injurious falls meant simply any self reported physical consequence of a fall, without any details.20 21 24 29 30 Some definitions specifically required the use of medical care,21 23 25 28 31 32 by using non-specific terms such as “fall for which medical care was sought,” “falls requiring medical care/medical attention,” or “medical consultations/visits.” When serious injuries were distinguished or specifically reported, their definition was more homogeneous across studies. Such injuries usually included fractures, severe soft tissue injuries requiring suturing, or other injuries leading to hospital admission.22 24 25 27 31 Some studies reported only fractures.33 34
Based on our review of case definitions used in the 17 studies, we distinguished four categories of injurious falls: those resulting in any reported consequences, including specific symptoms (ranging from bruises and cuts to more serious injuries such as fractures) or medical care; those resulting in medical care; those resulting in serious injuries such as fractures, head trauma, soft tissue injury requiring suturing, or any other injury requiring admission to hospital; and those resulting in fractures.
These categories represent increasingly specific subgroups of all injurious falls, which can also be considered to correspond to increasing levels of severity (except for those resulting in fracture, which is simply a specific type of serious injury).
Depending on the available data, a given study could contribute data relevant to one or more categories of injurious falls. Table 2 gives the definitions of injurious falls reported in each selected article (as a direct quotation), the category or categories of injurious falls in which it was classified for this review, and the rate ratio used in the corresponding analysis. For two studies, the rate ratio could not be calculated because the authors provided only the number of participants who had an injurious fall (rather than the number of such falls). In these cases, we used the ratio of the risk of at least one injurious fall in both groups instead. Of note, the outcomes of injurious fall in those studies were severe injuries26 and fractures,34 two outcomes that are relatively rare, so that the risk ratio was likely to be close to the rate ratio.
Table 2.
Injurious falls: extracted definitions and subsequent categorisation with estimates of intervention related fall reduction
| Trial | Extracted definitions | Rate Ratio of injurious falls | |||
|---|---|---|---|---|---|
| A: all injurious falls | B: falls resulting in medical care | C: falls resulting in serious injuries | D: falls resulting in fractures | ||
| Barnett 200319 | “Falls that resulted in bruises, strains, cuts and abrasions, back pain and fractures” (A) | 0.73 (046 to 1.17) | — | — | — |
| Campbell 199713 | Falls were classified as resulting in “serious” injury if the fall resulted in a fracture, admission to hospital or stitches were required, “moderate” injury if bruising, sprains, cuts, abrasions or reduction in physical function for at least three days resulted, or if the participant sought medical help, (A=moderate+severe), (C=severe). “Falls for which medical care sought” (B) | 0.45 (0.30 to 0.67) | 0.97 (0.58 to 1.64) | 0.82 (0.37 to 1.79) | — |
| Cornillon 200231 | “Cumulative number of medical consultations” (B). “Falls requiring hospitalization” (C) | — | 1.16 ( 0.57 to 2.37) | 0.15 (0.02 to 1.16) | — |
| Fitzharris 201028 | “Cut, scrape, gash, bruise or fracture; a head injury resulted or where the fall resulted in hospitalization” (A), “Falls requiring medical care” (B) | 0.85 (0.70 to 1.04) | 0.74 (0.50 to 1.10) | — | — |
| Freiberger 201220 | “Number of injurious falls” (A) | 0.70 (0.46 to 1.08) | — | — | — |
| Haines 200921 | “Falls with self-reported physical injury” (A), “Falls resulting in medical review (general practitioner or hospital medical officer if fall took place in a hospital)” (B), “Falls resulting in fracture” (D) | 0.82 (0.32 to 2.12) | 0.34 (0.07 to 1.62) | — | 0.88 (0.08 to 9.70) |
| Kemmler 201029 | “Subjects who experienced injurious falls” (A), “Fractures due to falls” (D) | 0.65† (0.45 to 0.92) | — | — | 0.49 (0.18 to 1.30) |
| Korpelainen 200633 | “Fall-related fractures” (D) | — | — | — | 0.36 (0.14 to 0.93) |
| Li 200526 | “If falls resulted in fractures, head injuries, sprains, bruises, scrapes, or other serious joint injuries or if the participant sought medical care” (A), “Medical care visits resulting from a fall” (B), “Severe falls requiring medical Attention” (C) | 0.40 (0.17 to 0.95) | 0.31 (0.11 to 0.85) | 0.28* (0.09 to 0.88) | — |
| MacRae 199432 | “Fall related injury requiring medical attention” (B) | — | 0.18 (0.02 to 1.77) | — | — |
| Lukkinen 200722 | “The injuries included fractures, dislocations and soft tissue injuries needing suturing and even more severe injuries” (C) | — | — | 0.94 (0.60 to 1.49) | — |
| McMurdo 199734 | Number of people with fractures (D) | — | — | — | 0.22* (0.01 to 4.59) |
| Means 200530 | “Any detectable residual adverse physical change persisting beyond 1 hr after the fall” (A) | 0.35 (0.22 to 0.56) | — | — | — |
| Robertson 200125 | “If bruising, sprains, cuts, abrasions, or reduction in physical function for at least three days resulted or if the participant sought medical help (moderate injuries), “Fall resulted in a fracture, admissions to hospital with an injury, or stitches were required” (severe injuries) (A=moderate+severe), (C=severe), “Falls for which medical care sought” (B) | 0.80 (0.53 to 1.21) | 0.64 (0.35 to 1.17) | 0.22 (0.04 to 0.95) | 0.28(0.06 to 1.32) |
| Skelton 200523 | “Falls requiring medical attention” (B) | — | 0.60 (0.33 to 1.08) | — | — |
| Smulders 201024 | “Self-reported injuries” (A), Fractures, concussion and wounds that needed suturing (C), Fractures reported as a consequence of a fall (D) | 0.55 (0.32 to 0.96) | — | 0.19 (0.02 to 1.57) | 0.31 (0.03 to 2.93) |
| Wolf 199627 | “Fall that resulted either in fractures; head injuries requiring hospitalization; joint dislocations; sprains defined as injury to a ligament when joint carried through range of motion greater than normal; other non-specified serious joint injuries; and lacerations required sutures” (C) | — | — | 0.69 (0.42 to 1.12) | — |
| Pooled rate ratio | 0.63 (0.52 to 0.77) | 0.70 (0.53 to 0.92) | 0.57 (0.37 to 0.90) | 0.39 (0.23 to 0.66) | |
*Risk ratio of at least one injurious fall (rate ratio unavailable).
†Unpublished data on total number of injurious falls provided by authors.
Methodological quality
Table 3 shows the results of the analysis of risk of bias. Although few studies were judged at high risk in any one domain, the quality of some studies could not be judged with any certainty in several domains. Prospective daily calendars returned monthly are the preferred method for recording falls,16 and most of the trials used this method. However, only six of the 11 trials that reported data on serious injuries used medical records to confirm the injury.
Table 3.
Assessment of risk of bias in included studies
| Trial | Random sequence generation | Allocation concealment | Methods of ascertaining falls | Blinding of falls and injurious fall assessment | Incomplete outcome data | Methods of ascertaining serious injuries |
|---|---|---|---|---|---|---|
| Barnett 200319 | Unclear | Low | Unclear | Unclear | Low | NA |
| Campbell 199713 | Low | Low | Low | Unclear | Low | Low |
| Cornillon 200231 | Low | Unclear | Low | Unclear | Low | Unclear |
| Fitzharris 201028 | Low | Low | Low | Low | Unclear | NA |
| Freiberger 201220 | Low | Low | Low | Low | Unclear | NA |
| Haines 200921 | Low | Low | Low | Low | Low | High |
| Kemmler 20109 | Low | Low | Low | Low | Low | High |
| Korpelainen 200633 | Low | Low | High | Low | Low | Low |
| Li 200526 | Low | Unclear | Low | Low | Low | Low |
| Luukinen 200722 | Low | Unclear | High | Low | Low | Low |
| MacRae199432 | Unclear | High | Low | Unclear | High | NA |
| McMurdo 199734 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Means 200530 | Low | Unclear | Low | Low | High | NA |
| Robertson 200125 | Low | Low | Low | Low | Low | Low |
| Skelton 200523 | Unclear | Unclear | Low | Low | Low | NA |
| Smulders 201024 | Unclear | Unclear | Low | Low | Low | High |
| Wolf 199627 | Low | Unclear | Low | Unclear | Unclear | Low |
Effect of exercise on injurious falls
Figure 2 shows the forest plots of the exercise effect estimate by category of injurious fall. Most of the exercise interventions tended to reduce injurious falls in all categories. Ten trials provided figures for all injurious falls; the pooled estimated rate ratio was 0.63 (0.51 to 0.77, I²=50%, P=0.04). The pooled estimate for falls resulting in medical care was 0.70 (0.54 to 0.92, I²=20%, P=0.27, eight trials) and for falls resulting in serious injuries was 0.57 (0.36 to 0.90, I²=46%, P=0.09, seven trials). Exercise seemed to significantly decrease the rate of falls resulting in fractures as well, with a pooled effect of 0.39 (0.23 to 0.66, I²=0%, P=0.96, six trials).
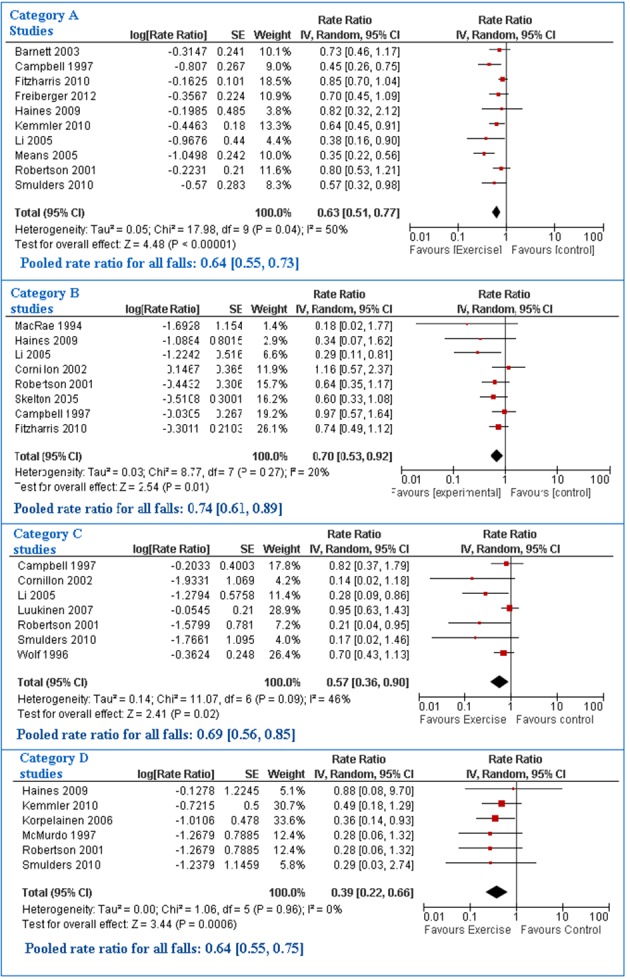
Fig 2 Forest plots of studies for four injurious fall categories: A, all injurious falls; B, falls resulting in medical care; C, falls resulting in serious injuries; and D, falls resulting in fractures
Sensitivity and subgroup analyses
To explore the possible impact of risk of bias on the exercise effect, we removed from the analyses studies for which the risk of bias was unclear for at least three of the quality components considered,19 27 31 34 or for which the risk was at least unclear for one component and high for another.22 24 30 32. This barely changed the pooled estimate of the effect of exercise in any of the four injurious fall categories, but it greatly reduced the heterogeneity between studies included in the analysis of all injurious falls (rate ratio 0.69, 95% confidence interval 0.58 to 0.82, I2=26%, P=0.22, eight trials).
In the subgroup analysis of the effect of exercise in reducing injurious falls based on risk of falls at enrolment, no significant difference was found in pooled estimates between trials with participants selected for their higher risk of falling13 19 20 21 24 and trials with unselected participants,25 26 28 29 30 in any of the four categories.
Publication bias
The funnel plot constructed from the 10 trials included in the analysis of all injurious falls shows a barely asymmetrical scatter (fig 3).
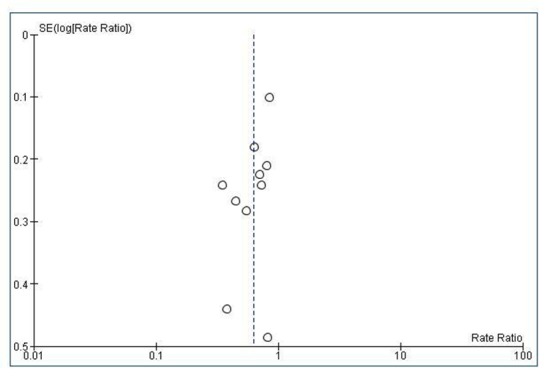
Fig 3 Funnel plot of studies included in analysis of all injurious falls
Adverse reactions
A total of eight participants in two studies reported brief temporary musculoskeletal discomfort related to exercise.21 33 No other adverse events, in particular no fall related injuries occurring during the exercise sessions, were reported in any of the included studies. Only six trials specifically reported the absence of adverse reactions.
Discussion
This systematic review provides evidence that fall prevention exercise programmes for older people not only reduce the rates of falls but also prevent injuries resulting from falls in older community dwelling people. The protective effect seems most pronounced for the most severe fall related injuries: the estimated reduction is 37% for all injurious falls, 43% for severe injurious falls, and 61% for falls resulting in fractures.
Many of the risk factors for falls and fall induced injuries are similar.35 These factors are correctable by well designed exercise programmes, even in the very old and frail.26 36 37 All exercise programmes that have proved to be effective for fall prevention (and all trials included in this review) emphasise balance training, and there is now ample evidence that this type of programme improves balance ability.13 38 However, most programmes are multicomponent—that is, also include other types of exercise such as gait and functional training, strengthening exercises, flexibility, and endurance. There is evidence that these types of interventions can improve reaction time, gait, muscle strength, coordination, and overall physical functioning as well as cognitive functions, especially executive function.19 28 39 It is therefore thought that exercise prevents injurious falls not only by improving balance and decreasing the risk of falling, but also by improving cognitive functioning,41 and the speed and effectiveness of protective reflexes (such as quickly extending an arm or grabbing nearby objects) or the energy absorbing capacity of soft tissues (such as muscles), thereby diminishing the force of impact on the body.40 41 Hence, for any given initial energy of a fall, improved protective responses should decrease the severity of the resulting trauma, which may explain why the estimated protective effect of exercise is stronger for severe injurious falls than for all injurious falls, the latter including severe but also minor and moderate injuries.
Although exercise reduces the severity of injury, the pooled effect of exercise on reducing all injurious falls (37%) was larger than the effect of exercise on falls resulting in medical care (30%) (which are presumably more severe). However, medical care seeking behaviour is influenced by the type and availability of care and sociodemographic characteristics as well as by other personal factors such as personality, pain tolerance, and anxiety.42 43 Accordingly, the mere fact that medical care was sought does not necessarily imply that an injury was more severe, although this is probably less true when different categories of injurious falls are examined within the same population. Of the 10 studies included in the analysis of all injurious falls, five also contributed to the analysis of falls resulting in medical care,13 21 25 26 28 and three also contributed to the analysis of severe injurious falls.13 25 26 Within these studies, the point estimate of the effect of exercise decreased from all injurious falls to falls resulting in medical care for all studies but one, and from falls resulting in medical care to severe injurious falls for all studies. These results support the argument that exercise reduces the severity of the injuries caused by falls.
Other risk factors are specific to the risk of trauma during a fall, and correction of these factors by exercise may also help explain the larger protective effect of exercise on serious injuries such as fractures. In particular, low bone mass is a major determinant of the risk of fracture once a fall begins. In three of the five trials included in the analysis of fall related fractures,29 33 34 the intervention was specifically designed to improve bone mass and hence included high intensity impact exercise in addition to balance, gait, and functional exercises. It resulted in a significant positive effect on bone mass at bone sites that varied with the study. However, these interventions were tested in women who were on average less than 75 years of age and did not have specific risk factors for falling. Hence, they may not be appropriate for older people aged more than 75 years, who are at the highest risk of falls and fractures, especially hip fractures.
The large estimated pooled effect of more moderate intensity exercise training on serious injuries found in this meta-analysis suggests that reducing the risk of falling and improving protective responses during a fall are important and feasible means of preventing fractures and other serious injuries in elderly people, as others have emphasised.44 45 46 47 48 This finding is especially important because large epidemiological studies have shown that most fractures in the population occur in people at moderate “bone risk” for their age.49 50 Hence, while prescription of antiosteoporotic drug treatments is currently recommended for older people with low bone mass, who are at the highest risk of fracture, additional effective strategies that can be proposed to larger segments of the elderly population will be necessary to significantly reduce the burden of fractures in this population.51 Fall prevention exercise training seems to be one such strategy.
Comparisons with other reviews
One group of researchers conducted an individual level data meta-analysis of the results of four trials conducted by their fall prevention research group to estimate the overall effect of the Otago individualised strength and balance exercise programme on falls and injuries.14 The study demonstrated a 35% reduction in the risk of an injurious fall (moderate or serious), a result similar to that presented here, but it failed to show a significant reduction in serious fall related injuries. A more recent review including three additional trials of the Otago exercise programme,52 failed to support the previous finding that the programme significantly reduced the risk of injurious falls, possibly because of a lack of access to individual level data or because of differences in the implementation and supervision of the programme (as suggested by the significantly lower compliance rates reported in the three additional trials than in the first four).
The recent Cochrane review of fall prevention interventions conducted a specific analysis to examine the effect of exercise interventions on the risk of fall related fractures and obtained similar results (pooled relative risk 0.34, 95% confidence interval 0.18 to 0.63).7 Of the six trials included in the Cochrane analysis, five are also included in our analysis. We excluded the one study because participants were recruited in the hospital while in the acute phase of an injury (hip fracture) so that the results of this trial may not be comparable to those not recruiting on the basis of an injury.53 Inversely, we included one study29 that compared an exercise intervention including balance, gait, and strengthening and flexibility exercises to a “wellness” exercise programme designed not to affect the risk of falling, whereas this study was not considered in the Cochrane analysis of fracture risk.
Strengths and limitations of this review
Heterogeneity was notable among studies included in the analysis of all injurious falls (I²=50%, P=0.04). Although no significant heterogeneity was detected in the analysis of severe injurious falls, the inconsistency was also moderately large (I²=46%, P=0.09). Pooled data from studies with significant heterogeneity require cautious interpretation because this indicates the possibility of meaningful differences between these studies. Although this review focused on interventions based solely on exercise and targeting specifically community dwelling elderly people, the selected interventions are still quite diverse, in particular in terms of intervention components (type of exercises, intensity, frequency, mode of delivery, and total duration) and inclusion criteria for participants. Similar or even larger measures of heterogeneity have also been reported in other meta-analyses of fall prevention exercise interventions.7 54
To explore possible reasons for heterogeneity, we carried out pre-planned subgroup analyses based on fall risk at enrolment and found no difference in pooled estimates between trials with participants selected for their higher risk of falling versus lower risk (unselected), for any of the four categories of injurious falls. Among intervention components, the type of exercise seems to be a key factor that influences effectiveness against falls: interventions including a balance training component seem to be more effective.7 54 55 One study found that the intensity of the balance training component was also important: interventions that include moderate to high challenging exercises (that is, standing exercises in which people sought to stand with their feet closer together or on one leg, to minimise use of their hands to assist, and to practice controlled movements of the centre of mass) are more effective in reducing falls than interventions that include less challenging balance exercises.8 All interventions included in this review include a balance training component, hence we performed an additional subgroup analysis by comparing trials where the exercise programme provided a moderate or high challenge to balance (based on Sherrington’s definition),13 19 20 21 23 24 25 26 27 31 33 versus a low challenge.22 28 29 30 32 34 No significant difference in exercise effect was found between the two subgroups with regard to the reduction in all injurious falls or falls resulting in medical care. For severe injurious falls and falls resulting in fractures, there were not enough studies to perform subgroup analyses by intensity of balance training. The relatively small number of studies included in this review did not allow us to perform additional subgroup analyses exploring the effect of other components within interventions or other factors related to the way interventions were implemented that might have affected results.
Although we tried to reduce heterogeneity in the definitions of injurious falls as much as possible by grouping them in more homogeneous categories, remaining inconsistency in definitions may also help explain the heterogeneity observed between studies. In the category of all injurious falls, in particular, several studies used imprecise definitions of injurious falls20 21 24 29 30 but were nevertheless included in the analysis since this category is the largest and refers to any types of physical consequences of a fall. We performed a sensitivity analysis excluding from the analysis of this category studies that used imprecise definitions: the resulting pooled rate ratio was similar to that obtained in the main overall analysis (0.69, 0.53 to 0.90, I2=49%, P=0.10) and indicated that our results are robust to differences in outcome definitions between studies. Results of the sensitivity analysis excluding trials judged to be at higher risk of bias in all four categories of injurious falls barely changed the pooled effect estimates and indicates that our results are also robust to key risks of bias.
The funnel plot of the 10 trials contributing to the analysis of all injurious falls showed a barely asymmetrical scatter. Asymmetrical funnel plots may indicate publication bias or may be due to exaggeration of treatment effects in small studies of low quality.15 However, the funnel plot in this analysis showed no clear evidence of “small study effects.” Note that almost all the trials included in this review were designed to prove that exercise has an effect on the fall rate and not on the rate of injurious falls. Among the 17 studies considered in this review, eight did not demonstrate that exercise had a significant effect on falls. Moreover, the pooled effect of exercise on the rate ratio of falls was 0.68 (95% confidence interval 0.61 to 0.77), which is similar to the effect of exercise reported in the Cochrane review.7 These points suggest that the trials included in this review, because they presented data on fall related injuries, do not represent a special selection of fall prevention exercise trials biased towards “positive” trials for all falls. None the less, we cannot exclude the possibility that trials are more likely to report injurious falls when there tend to be a positive effect on injurious falls. It is also possible that some trials did not report data on injurious falls simply because these data were not collected.
Only minor adverse reactions were reported in two of the 17 included studies. However, close to half of the selected studies did not even mention intervention adverse effects. It has also been suggested that exercise fall- prevention programmes may have adverse psychological effects that may affect the quality of life (for example, through self imposed activity restriction).56 57 Some studies have reported the effect of the intervention on fear of falling, physical activity levels, or other dimensions of quality of life.19 21 24 26 27 Their results show either no effect or a tendency towards a beneficial effect of the intervention on these outcomes, in particular a reduction in fear of falling. More complete data on adverse physical reactions as well as on psychological and quality of life outcomes would improve our ability to judge the overall benefit of exercise fall prevention interventions. Another limitation of the included studies is that they often lack information on “intermediate” outcomes such as gait, balance, and other physical or cognitive functions, which would help us to understand how exercise “works” and design optimum programmes. Future trials should also provide more detailed descriptions of implementation procedures, whether planned or unplanned, so that readers can judge the applicability of the programme in different settings or on a larger scale.
Conclusion and recommendations
The results presented in this paper show a positive effect of exercise on injurious falls, including the most severe falls and those that result in medical care—that is, those with the greatest consequences for people’s health and use of resources. These results should provide useful additional evidence for healthcare providers to encourage participation in exercise fall prevention programmes, and further justification for decision makers to provide funding for those programmes.
Systematic reporting of falls and injuries should be implemented in future randomised controlled trials, where the different levels of severity of the injury should be standardised and defined in advance, to improve the comparison between studies and subsequently the accuracy of pooled estimates for each category of falls. Future trials should also aim to deal with some of the limitations of published studies, in particular by providing data on other important outcomes (physical and cognitive functional capacities, psychological outcomes, and quality of life) and a thorough description of the implementation process.
What is already known on this topic
Falls and the resulting injuries are among the most serious and common medical problems experienced by older adults
Well designed exercise programmes can prevent falls in older adults living at home
But there is no clear evidence that these programmes can also prevent severe or more moderate injuries caused by falls.
What this study adds
Exercise programmes designed to prevent falls in older community dwelling people seem to reduce injuries caused by falls, including the most severe injuries
Such programmes also seem to reduce falls resulting in medical care
We thank Jo Ann Cahn for her help with preparing the manuscript and Philippe Ravaud (Inserm U738, France; French Cochrane Centre, Paris, France) for his helpful comments and advice on some methodological aspects of our review.
Contributors: FEK and PAD conceived the study, performed the review, and drafted the manuscript. BC and MAC contributed to data quality assessment and outcomes classification and reviewed the manuscript for important intellectual content. FEK performed the data analysis. PAD is the guarantor.
Funding: This research received no specific funding.
Competing interests: The authors declare no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Ethical approval: Not required.
Data sharing: No additional data available.
Transparency: The lead author affirms that the manuscript is an honest, accurate, and transparent account of the review being reported; that no important aspects of the review have been omitted; and that any discrepancies from the review as planned have been explained.
Cite this as: BMJ 2013;347:f6234
Web Extra. Extra material supplied by the author
Data extraction form
Decision after assessing full text articles for eligibility
References
- 1.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35(suppl 2):ii37-41. [DOI] [PubMed] [Google Scholar]
- 2.Stevens JA, Mack KA, Paulozzi LJ, Ballesteros MF. Self-reported falls and fall-related injuries among persons aged ≥65 years—United States, 2006. J Safety Res 2008;39:345-9. [DOI] [PubMed] [Google Scholar]
- 3.Morrison A, Fan T, Sen SS, et al. Epidemiology of falls and osteoporotic fractures: a systematic review. Clin Outcomes Res 2013;5:9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EMM, Panneman MJM, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma 2011;71:748-53. [DOI] [PubMed] [Google Scholar]
- 5.Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol 2013;178:418-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int 2010;21:1295-306. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull 2011;22:78-83. [DOI] [PubMed] [Google Scholar]
- 9.Shumway-Cook A, Ciol M, Hoffman J, Dudgeon B, Yorkston K, Chan L. The bottom line. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther 2009;89:324-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwenk M, Lauenroth A, Stock C, Rodriguez Moreno R, Oster P, McHugh G, et al. Definitions and methods of measuring and reporting on injurious falls in randomised controlled fall prevention trials: a systematic review. BMC Med Res Methodol 2012;12:501-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamb SE, Becker C, Gillespie LD, Smith JL, Finnegan S, Potter R, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011;12:125-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315:1065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta-analysis of individual-level data. J Am Geriatr Soc 2002;50:905-11. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hannan MT, Gagnon MM, Aneja J, Jones RN, Cupples LA, Lipsitz LA, et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am J Epidemiol 2010;171:1031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JP, Green S, Collaboration C. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008.
- 18.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. [DOI] [PubMed] [Google Scholar]
- 19.Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing 2003;32:407-14. [DOI] [PubMed] [Google Scholar]
- 20.Freiberger E, Häberle L, Spirduso WW, Rixt Zijlstra GA. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: a randomized controlled trial. J Am Geriatr Soc 2012;60:437-46. [DOI] [PubMed] [Google Scholar]
- 21.Haines TP, Russell T, Brauer SG, Erwin S, Lane P, Urry S, et al. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from hospital: a pilot randomized controlled trial. Clin Rehabil 2009;23:973-85. [DOI] [PubMed] [Google Scholar]
- 22.Luukinen H, Lehtola S, Jokelainen J, Väänänen-Sainio R, Lotvonen S, Koistinen P. Prevention of disability by exercise among the elderly: a population-based, randomized, controlled trial. Scand J Prim Health Care 2006;24:199-205. [DOI] [PubMed] [Google Scholar]
- 23.Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise—FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005;34:636-9. [DOI] [PubMed] [Google Scholar]
- 24.Smulders E, Weerdesteyn V, Groen BE, Duysens J, Eijsbouts A, Laan R, et al. Efficacy of a short multidisciplinary falls prevention program for elderly persons with osteoporosis and a fall history: a randomized controlled trial. Arch Phys Med Rehabil 2010;91:1705-11. [DOI] [PubMed] [Google Scholar]
- 25.Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: randomised controlled trial. BMJ 2001;322:697-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 2005;60:187-94. [DOI] [PubMed] [Google Scholar]
- 27.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc 1996;44:489-97. [DOI] [PubMed] [Google Scholar]
- 28.Fitzharris MP, Day L, Lord SR, Gordon I, Fildes B. The Whitehorse NoFalls trial: effects on fall rates and injurious fall rates. Age Ageing 2010;39:728-33. [DOI] [PubMed] [Google Scholar]
- 29.Kemmler W, von Stengel S, Engelke K, Haberle L, Kalender WA. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: The Randomized Controlled Senior Fitness and Prevention (SEFIP) Study. Arch Intern Med 2010;170:179-85. [DOI] [PubMed] [Google Scholar]
- 30.Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil Assoc Acad Physiatr 2005;84:238-50. [DOI] [PubMed] [Google Scholar]
- 31.Cornillon E, Blanchon MA, Ramboatsisetraina P, Braize C, Beauchet O, Dubost V, et al. Impact d’un programme de prévention multidisciplinaire de la chute chez le sujet âgé autonome vivant à domicile, avec analyse avant-après des performances physiques. Ann Readapt Med Phys 2002;45:493-504. [DOI] [PubMed] [Google Scholar]
- 32.MacRae PG, Feltner ME, Reinsch SA. 1-year exercise program for older women: effects on falls, injuries, and physical performance. J Aging Phys Act 1994;2:127-42. [Google Scholar]
- 33.Korpelainen R, Keinänen-Kiukaanniemi S, Heikkinen J, Väänänen K, Korpelainen J. Effect of impact exercise on bone mineral density in elderly women with low BMD: a population-based randomized controlled 30-month intervention. Osteoporos Int 2005;17:109-18. [DOI] [PubMed] [Google Scholar]
- 34.McMurdo MET, Mole PA, Paterson CR. Controlled trial of weight bearing exercise in older women in relation to bone density and falls. BMJ 1997;314:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tinetti ME. Preventing falls in elderly persons. N Engl J Med. 2003;348:42-9. [DOI] [PubMed] [Google Scholar]
- 36.Iwamoto J, Suzuki H, Tanaka K, Kumakubo T, Hirabayashi H, Miyazaki Y, et al. Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporos Int 2009;20:1233-40. [DOI] [PubMed] [Google Scholar]
- 37.Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc 1995;43:1198-206. [DOI] [PubMed] [Google Scholar]
- 38.Howe TE, Rochester L, Jackson A, Banks PMH, Blair VA. Exercise for improving balance in older people. Cochrane Database Syst Rev 2007;(4):CD004963. [DOI] [PubMed] [Google Scholar]
- 39.Liu-Ambrose T, Nagamatsu LS, Graf P, Beattie BL, Ashe MC, Handy TC. Resistance training and executive functions: a 12-month randomized controlled trial. Arch Intern Med 2010;170:170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. J Am Geriatr Soc 1993;41:1226-34. [DOI] [PubMed] [Google Scholar]
- 41.Quant S, Maki BE, Verrier MC, McIlroy WE. Passive and active lower-limb movements delay upper-limb balance reactions. Neuroreport 2001;12:2821-5. [DOI] [PubMed] [Google Scholar]
- 42.Cummings P, Koepsell TD, Mueller BA. Methodological challenges in injury epidemiology and injury prevention research. Annu Rev Public Health 1995;16:381-400. [DOI] [PubMed] [Google Scholar]
- 43.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998-2011. Psycho-Soc Med 2012;9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int 2009;20:2111-25. [DOI] [PubMed] [Google Scholar]
- 45.Kannus P, Parkkari J, Niemi S, Palvanen M. Fall-induced deaths among elderly people. Am J Public Health 2005;95:422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jarvinen TLN, Sievanen H, Khan KM, Heinonen A, Kannus P. Shifting the focus in fracture prevention from osteoporosis to falls. BMJ 2008;336:124-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin FC. Next steps for falls and fracture reduction. Age Ageing 2009;38:640-3. [DOI] [PubMed] [Google Scholar]
- 48.Skelton DA, Beyer N. Exercise and injury prevention in older people. Scand J Med Sci Sports 2003;13:77-85. [DOI] [PubMed] [Google Scholar]
- 49.Stone KL, Seeley DG, Lui L-Y, Cauley JA, Ensrud K, Browner WS, et al. BMD at multiple sites and risk of fracture of multiple types: long-term results from the study of osteoporotic fractures. J Bone Miner Res 2003;18:1947-54. [DOI] [PubMed] [Google Scholar]
- 50.Dargent-Molina P, Favier F, Grandjean H, Baun C, Schott AM, Hausherr E, et al. Fall-related factors and risk of hip fracture the EPIDOS prospective study. Lancet 1996;348:145-9. [DOI] [PubMed] [Google Scholar]
- 51.Cheung AM, Detsky AS. Osteoporosis and fractures: missing the bridge? JAMA 2008;299:1468-70. [DOI] [PubMed] [Google Scholar]
- 52.Thomas S, Mackintosh S, Halbert J. Does the ‘Otago exercise programme’ reduce mortality and falls in older adults?: a systematic review and meta-analysis. Age Ageing 2010;39:681-7. [DOI] [PubMed] [Google Scholar]
- 53.Bischoff-Ferrari HA, Dawson-Hughes B, Platz A, Orav EJ, Stähelin HB, Willett WC, et al. Effect of high-dosage cholecalciferol and extended physiotherapy on complications after hip fracture: a randomized controlled trial. Arch Intern Med 2010;170:813-20. [DOI] [PubMed] [Google Scholar]
- 54.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008;56:2234-43. [DOI] [PubMed] [Google Scholar]
- 55.Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Miller JP, Mulrow CD, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA 1995;273:1341-7. [PubMed] [Google Scholar]
- 56.Laybourne AH, Biggs S, Martin FC. Falls exercise interventions and reduced falls rate: always in the patient’s interest? Age Ageing 2008;37:10-3. [DOI] [PubMed] [Google Scholar]
- 57.Sjösten N, Vaapio S, Kivelä S-L. The effects of fall prevention trials on depressive symptoms and fear of falling among the aged: a systematic review. Aging Ment Health 2008;12:30-46. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data extraction form
Decision after assessing full text articles for eligibility


