Abstract
Little is known about the deleterious effects of injurious falls relative to those of other disabling conditions or whether these effects are driven largely by hip fractures. From a cohort of 754 community-living elders of New Haven, Connecticut, we matched 122 hospitalizations for an injurious fall (59 hip-fracture and 63 other fall-related injuries) to 241 non–fall-related hospitalizations. Participants (mean age: 85.7 years) were evaluated monthly for disability in 13 activities and admission to a nursing home from 1998 to 2010. For both hip-fracture and other fall-related injuries, the disability scores were significantly greater during each of the first 6 months after hospitalization than for the non–fall-related admissions, with adjusted risk ratios at 6 months of 1.5 (95% confidence interval (CI): 1.3, 1.7) for hip fracture and 1.4 (95% CI: 1.2, 1.6) for other fall-related injuries. The likelihood of having a long-term nursing home admission was considerably greater after hospitalization for a hip fracture and other fall-related injury than for a non–fall-related reason, with adjusted odds ratios of 3.3 (95% CI: 1.3, 8.3) and 3.2 (95% CI: 1.3, 7.8), respectively. Relative to other conditions leading to hospitalization, hip-fracture and other fall-related injuries are associated with worse disability outcomes and a higher likelihood of long-term nursing home admissions.
Keywords: accidental falls, activities of daily living, aged, cohort studies, nursing homes
Each year, about a third of community-living persons aged 65 years or older will fall, and about half of these individuals will experience multiple falls (1–3). For every 10 falls, 1 will result in a serious injury such as a fracture, joint dislocation, traumatic brain injury, or soft tissue damage (3–7). In 2009, emergency departments in the United States treated 2.2 million older persons for nonfatal injurious falls, leading to more than 582,000 hospital admissions (8).
According to the Centers for Disease Control and Prevention, falls among older persons cost the US health-care system $28.2 billion per year, and most of this cost is incurred by injurious falls leading to hospitalization (8). Falls, particularly those resulting in injury, are independently associated with a decline in the ability to carry out important functional activities, such as bathing, dressing, shopping, and housekeeping, and with an increased risk of a long-term nursing home admission (9, 10). Little is known, however, about the deleterious effects of injurious falls relative to those of other disabling conditions or whether these effects are driven largely by hip fractures, which have long been considered the most devastating consequence of a fall (3, 11). If policy makers had access to this information, they would be better equipped to allocate precious resources for the prevention and treatment of the common disabling conditions of aging.
Increasing evidence indicates that falls are preventable. In randomized, controlled intervention trials, the rate of falling has been reduced by up to 40% (12). The preventive strategies tested in these trials, including adjustments in medications, exercise regimens, and behavioral recommendations, are feasible and relatively cost effective. Moreover, a recent study demonstrated that the dissemination of evidence about fall prevention, coupled with interventions to change clinical practice, reduces the rate of injurious falls by nearly 10%, potentially leading to large health-care savings (13).
In the current study, which used a matched cohort design, we evaluated the associations between an injurious fall and changes in functional status, including basic, instrumental, and mobility activities, and admissions to a nursing home, including those that were long-term. We tested the hypotheses that older persons who experienced an injurious fall leading to hospitalization would have worse disability outcomes over a 6-month period and a higher likelihood of long-term nursing home admissions than their counterparts who were hospitalized for a non–fall-related reason, and that these associations would be observed not only for hip fracture but also for other fall-related injuries. If injurious falls are associated with greater morbidity than other disabling conditions, they may warrant increased attention by policy makers and clinicians as a target for prevention and treatment.
MATERIALS AND METHODS
Study population
Participants were drawn from the Precipitating Events Project (PEP), an ongoing longitudinal study, described in detail elsewhere (14, 15), of 754 community-living persons, aged 70 years or older, who were initially nondisabled in 4 basic activities of daily living—bathing, dressing, walking across a room, and transferring from a chair. Potential participants were members of a large health plan and were excluded for significant cognitive impairment with no available proxy (16), life expectancy <12 months, plans to move out of the area, or inability to speak English. On the basis of our initial sample size calculations, persons who were physically frail were oversampled. Only 4.6% of persons contacted refused screening, and 75.2% of those eligible agreed to participate and were enrolled from March 1998 to October 1999. Persons who refused to participate did not differ significantly from those who were enrolled in terms of age or sex. The study protocol was approved by the Yale Human Investigation Committee, and all participants provided informed consent.
Data collection in the Precipitating Events Project
Comprehensive home-based assessments were completed at baseline and subsequently at 18-month intervals for 108 months, while telephone interviews were completed monthly through June 30, 2010. For participants who had significant cognitive impairment or were otherwise unavailable, we interviewed a proxy informant, using a rigorous protocol, with demonstrated reliability and validity (16). Deaths were ascertained by review of the local obituaries and/or from an informant during a subsequent telephone interview, with a completion rate of 100%. A total of 476 (63.1%) participants died after a median follow-up of 78 months, while 36 (4.8%) dropped out of the study after a median follow-up of 26.5 months. Data were otherwise available for 99.2% of the 71,792 monthly interviews. During the comprehensive assessments, data were collected on demographic characteristics, 9 self-reported, physician-diagnosed chronic conditions, body mass index (17), cognitive status (18), depressive symptoms (19), and physical frailty, which was defined on the basis of slow gait speed (20).
Assessment of disability
Complete details regarding the assessment of disability are provided elsewhere (15, 16, 21). During the monthly interviews, we asked participants, “At the present time, do you need help from another person to (complete the task)?” for each of the 4 basic activities (bathing, dressing, walking across a room, and transferring from a chair), 5 instrumental activities (shopping, housework, meal preparation, taking medications, and managing finances), and 3 mobility activities (walk a quarter mile (0.40 km), climb a flight of stairs, and lift and carry 10 pounds (4.5 kg)). For these 12 activities, disability was operationalized as the need for personal assistance. Participants were also asked about a fourth mobility activity, “Have you driven a car during the past month?” Participants who responded “No” were deemed to have stopped driving. To maintain consistency with the other activities, these participants were classified as being “disabled” in driving that month (21). To address the small amount of missing data on disability, we used multiple imputation with 100 random draws per missing observation (22).
Assessment of hospitalizations and nursing home admissions
Information on hospitalizations and nursing home admissions was obtained during the monthly interviews. Participants were asked whether they had stayed at least overnight in a hospital since the last interview, that is, during the past month. The accuracy of these reports, based on an independent review of hospital records, was high, as denoted by a sensitivity of 93.3% (95% confidence interval (CI): 90.5, 96.1) and a specificity of 99.3% (95% CI: 99.0, 99.6). Participants who were hospitalized were also asked to provide the primary reason for their admission. These reasons were subsequently grouped into distinct diagnostic categories by using a revised version of a previously published protocol (23). Agreement relative to an independent review of hospital records was 82% (24).
Participants were also asked whether they had been admitted to a nursing home during the past month. The accuracy of these reports, based on an independent review of medical records, was high, as denoted by a sensitivity of 96.3% (95% CI: 89.2, 100) and a specificity of 100% (95% CI: 88.1, 100).
Study design
To address our research questions, we used a matched cohort design, which has been recommended for studies of injury (25, 26). This design reduces bias with little loss of precision (27), allows for multiply matched controls per case (28), and permits the use of generalized estimating equations, which accounts for the correlation of observations within each cluster of matched observations (29).
Assembly of analytical sample
We identified 2 groups of participants who had been living in the community immediately prior to an acute hospital admission. The “exposed” group included participants who were hospitalized for an injurious fall, while the “unexposed” group included participants who were hospitalized for a non–fall-related reason. These groups are subsequently referred to as cases and controls, respectively. Injurious falls included fractures, head trauma, soft tissue injuries, lacerations, and other fall-related complications such as rhabdomyolysis. For both groups, participants were excluded if they were disabled in all 13 of the basic, instrumental, and mobility activities (i.e., completely disabled) in the month prior to the hospitalization. This was necessary so that participants had the opportunity to become more disabled following the acute hospital admission. Participants were allowed to contribute more than 1 qualifying hospitalization to each of the 2 groups, but not more than 1 within an 18-month interval, that is, since the last comprehensive assessment. Of the 151 hospitalizations for an injurious fall, 24 occurred among participants who were living in a nursing home, and 5 occurred among participants who were completely disabled. The remaining 122 hospitalizations for an injurious fall occurred in 107 participants, who had 1 fall-related admission (n = 92) and 2 fall-related admissions (n = 15), respectively.
To assemble the control group, we attempted to select 2 qualifying, non–fall-related hospitalizations for each of the 122 fall-related hospitalizations (28). Through the use of a SAS macro (30), controls were sequentially matched with cases on the following 3 features: 1) sex; 2) participant's age (within 4 years) at the time of hospitalization; and 3) number of disabilities (within 1 disability) out of the 12 possible in the month prior to the hospitalization. To avoid potential confounding with unmeasured, fall-related covariates, participants who had a hospitalization for an injurious fall (i.e., cases) were not eligible to serve as controls. Because only 1 suitable control could be identified for 3 of the fall-related hospitalizations, the number of qualifying, non–fall-related hospitalizations was 241. These occurred in 192 participants who had 1 (n = 149), 2 (n = 37), and 3 (n = 6) non–fall-related hospitalizations, respectively.
For all cases and controls, hospital admissions, including the primary diagnosis, were confirmed, and length of hospital stay was determined by review of medical records and linkage to Medicare claims data (31).
Statistical analysis
The reasons for the fall-related and non–fall-related hospitalizations were tabulated. For hip fracture and other fall-related injuries, respectively, relevant demographic and clinical characteristics were compared between participants in the case and control groups. P values were calculated from either binary or Poisson generalized linear models that adjusted for the correlation between the matched cases and controls by using an unstructured matrix.
The primary outcome included the number of disabilities in all 13 basic, instrumental, and mobility activities. To determine whether our findings were consistent across these 3 domains, we also evaluated the number of disabilities in the 4 basic, 5 instrumental, and 4 mobility activities, respectively, as secondary outcomes. Because each outcome represents a count, we fit Poisson models to compare the disability scores as least-squares means at each time point over the 6 months of follow-up. A 6-month time period is often used when evaluating disability following hospitalization (32). In addition, we have previously demonstrated that recovery of independent function is relatively uncommon beyond 6 months among newly disabled older persons (13). The models included an interaction term between follow-up month and fall status (hip fracture, other fall-related injury, and non–fall-related). Two sets of risk ratios were subsequently calculated to determine the proportional difference in disability scores for the 2 falls groups relative to the control group. The Poisson models invoked generalized estimating equations and were adjusted for the matching factors (age, sex, and number of disabilities in the relevant activities in the month prior to hospitalization); for the fixed effects of race, education, living situation, number of chronic conditions, body mass index, cognitive impairment, depressive symptoms, physical frailty, number of months since the prior comprehensive assessment, length of hospital stay (as an indicator of severity of illness), and month of follow-up after the index hospitalization; and for the correlation among each matched-falls case and its controls with a first-order autoregressive structure. These analyses were repeated with a sample that included only the first fall-related hospitalization of each case participant (n = 107) and his/her matched controls (n = 211). All models were checked for fit by examining residuals.
Next, we evaluated the associations of the hip fracture and other fall-related hospitalizations, respectively, relative to those of the non–fall-related hospitalizations, on admissions to a nursing home using logistic regression analysis. We evaluated any admission from the hospital to a nursing home and, subsequently, the subset of these admissions that were long term, defined as being a resident of a nursing home for 4 consecutive monthly interviews (33). This choice is consistent with the criteria used previously (10). The logistic regression models were adjusted for the correlation among each matched-falls case and its controls by using compound symmetry and for the fixed effects of age, sex, race, education, living situation, number of chronic conditions, body mass index, cognitive impairment, depressive symptoms, physical frailty, number of months since the prior comprehensive assessment, length of hospital stay, and number of disabilities in all activities in the month prior to hospitalization. These models were evaluated with the Hosmer-Lemeshow lack-of-fit test statistic.
All analyses were performed by using SAS, version 9.2, software (SAS Institute, Inc., Cary, North Carolina), and P < 0.05 (2-tailed) was used to indicate statistical significance.
RESULTS
Table 1 provides the reasons for hospitalization. Nearly half of the injurious falls were hip fractures, about a third included other types of fractures, and the remainder included nonfracture injuries (e.g., head trauma, soft tissue injury, rhabdomyolysis). The most common diagnostic categories for the non–fall-related hospitalizations included cardiac-related conditions (e.g., coronary heart disease and congestive heart failure), infections (e.g., pneumonia and sepsis), arthritis, cancer, and stroke.
Table 1.
Reasons for Hospitalization, New Haven, Connecticut, 1998 − 2010
| No. | % | |
|---|---|---|
| Fall related (n = 122) | ||
| Hip fracture | 59 | 48.4 |
| Other fractures | 40 | 32.8 |
| Other injuries | 23 | 18.9 |
| Non–fall related (n = 241)a | ||
| Cardiac | 54 | 22.4 |
| Infection | 38 | 15.8 |
| Arthritis | 18 | 7.5 |
| Cancer | 17 | 7.1 |
| Stroke | 13 | 5.4 |
| Gastrointestinal bleed | 11 | 4.6 |
| Dehydration or electrolyte disturbance | 11 | 4.6 |
| Pulmonary, other than pneumonia | 10 | 4.2 |
| Renal failure | 7 | 2.9 |
| Altered mental status | 7 | 2.9 |
| Syncope | 7 | 2.9 |
| Hematological | 5 | 2.1 |
| Other medical | 24 | 10.0 |
| Other surgical | 16 | 6.6 |
| Psychiatric | 3 | 1.2 |
a Grouped into distinct diagnostic categories, as described in Materials and Methods; the first 12 categories are presented in order of frequency of occurrence, from highest to lowest.
Table 2 provides the characteristics of the matched cohort according to the type of injurious fall. For both hip fracture and other fall-related injuries, cases and controls were generally well matched, with few statistically significant differences. The mean age ranged from 85.3 to 86.2 years, and nearly 70% were women. For both sets of cases and controls, body mass index was significantly greater in the non–fall group than the fall group. Severity of illness, as denoted by length of hospital stay, was comparable for the hip fracture cases and controls but was lower in the other fall-related injury cases than controls. In the month prior to hospitalization, the mean number of disabilities differed little between the 2 fall and non–fall groups.
Table 2.
Characteristics of Matched Cohort According to Type of Injurious Fall, New Haven, Connecticut, 1998 − 2010a
| Characteristic | Hip Fracture |
Other Fall-related Injuries |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (n = 59) |
Controls (n = 116) |
P Value | Cases (n = 63) |
Controls (n = 125) |
P Value | |||||||||
| No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | |||
| At time of hospitalization | ||||||||||||||
| Age, years | 86.2 (5.5) | 85.8 (5.0) | 0.69 | 85.6 (6.0) | 85.3 (5.6) | 0.08 | ||||||||
| Female sex | 41 | 69.5 | 80 | 69.0 | 0.20 | 44 | 69.8 | 87 | 69.6 | 0.33 | ||||
| Non-Hispanic white | 58 | 98.3 | 104 | 89.7 | 0.11 | 57 | 90.5 | 115 | 92.0 | 0.73 | ||||
| Did not complete high school | 16 | 27.1 | 41 | 35.3 | 0.22 | 18 | 28.6 | 47 | 37.6 | 0.24 | ||||
| Months since prior comprehensive assessment | 8.8 (4.5) | 8.5 (5.4) | 0.61 | 8.5 (5.6) | 9.3 (5.2) | 0.33 | ||||||||
| Length of stay, days | 6.8 (4.2) | 6.4 (6.9) | 0.63 | 5.6 (2.9) | 7.1 (7.9) | 0.04 | ||||||||
| At time of prior comprehensive assessment | ||||||||||||||
| Lives alone | 25 | 42.4 | 61 | 52.6 | 0.14 | 37 | 58.7 | 64 | 51.2 | 0.30 | ||||
| No. of chronic conditions | 1.9 (1.5) | 2.4 (1.2) | 0.06 | 2.3 (1.3) | 2.2 (1.2) | 0.63 | ||||||||
| Body mass indexb | 23.7 (5.0) | 26.2 (5.2) | <0.001 | 25.0 (5.0) | 26.8 (5.6) | 0.03 | ||||||||
| Cognitive impairmentc | 14 | 23.7 | 28 | 24.1 | 0.80 | 7 | 11.1 | 27 | 21.6 | 0.06 | ||||
| Depressive symptomsd | 11 | 18.6 | 22 | 19.0 | 0.90 | 19 | 30.2 | 24 | 19.2 | 0.09 | ||||
| Physically fraile | 41 | 69.5 | 66 | 56.9 | 0.08 | 42 | 66.7 | 87 | 69.6 | 0.61 | ||||
| Month prior to hospitalization | ||||||||||||||
| No. of disabilitiesf | ||||||||||||||
| All activities (0–12) | 4.2 (3.4) | 4.3 (3.5) | 0.16 | 5.0 (3.8) | 4.9 (3.7) | 0.04 | ||||||||
| Basic activities (0–4) | 0.4 (0.8) | 0.4 (0.8) | 0.78 | 0.7 (1.1) | 0.5 (0.9) | 0.47 | ||||||||
| Instrumental activities (0–5) | 2.0 (1.8) | 2.1 (1.8) | 0.12 | 2.3 (1.7) | 2.3 (1.9) | 0.62 | ||||||||
| Mobility activities (0–4) | 1.7 (1.3) | 1.8 (1.4) | 0.77 | 2.1 (1.5) | 2.0 (1.5) | 0.71 | ||||||||
Abbreviation: SD, standard deviation.
a As described in Materials and Methods, up to 2 controls were sequentially matched with cases on the basis of sex, participant age (within 4 years) at the time of hospitalization, and the number of disabilities (within 1 disability) in all activities in the month prior to hospitalization. P values were calculated from either binary or Poisson generalized linear models that adjusted for the correlation between the matched cases and controls by using an unstructured matrix.
b Body mass index:weight (kg)/height (m)2.
c Defined as score <24 on the Folstein Mini-Mental State Examination.
d Defined as score ≥20 on the Center for Epidemiological Studies-Depression Scale.
e Defined on the basis of slow gait speed, as described in Materials and Methods.
f The values below within parentheses represent the potential range for the number of disabilities for the corresponding set of activities. Participants were excluded if they were disabled in all 13 activities.
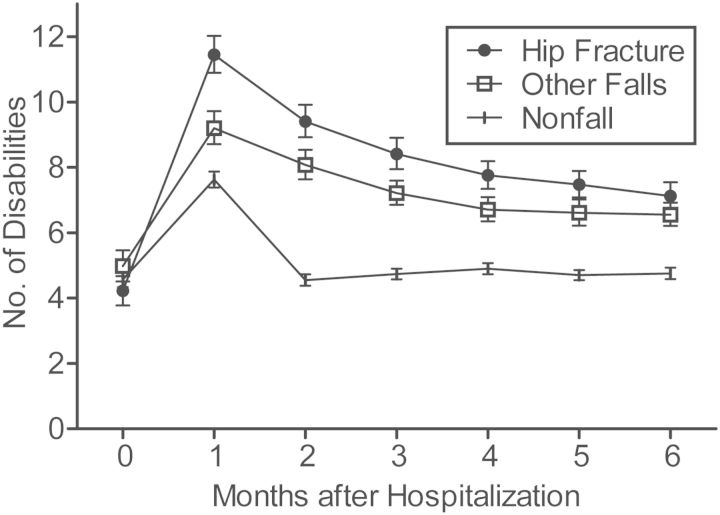
Figure 1 shows the course of disability in all activities after hospitalization for hip fracture, other fall-related injuries, and non–fall-related reasons. For both hip fracture and other fall-related injuries, the disability scores were significantly greater at each time point after hospitalization than the scores for non–fall-related reasons, with adjusted risk ratios, shown in Table 3, ranging from 1.5 (95% CI: 1.4, 1.7) at 1 month to 2.1 (95% CI: 1.8, 2.4) at 2 months for hip fracture and from 1.2 (95% CI: 1.1, 1.3) at 1 month to 1.8 (95% CI: 1.5, 2.0) at 2 months for other fall-related injuries. Although participants who were hospitalized for a hip fracture or other fall-related injury demonstrated some recovery, they were more disabled at 6 months than they had been before the fall. In contrast, participants who were hospitalized for a non–fall-related reason returned to their premorbid level of function within the first 2 months. Decline in function after hospitalization was most pronounced for participants with hip fracture; yet, at 6 months their disability scores of 7.1 (95% CI: 6.7, 7.5) were only modestly greater than the scores of 6.6 (95% CI: 6.2, 6.9) for participants with other fall-related injuries. Although the range of possible scores differed, the results were comparable for basic, instrumental, and mobility activities, respectively, as shown in Figure 2 and Table 3. As shown in Web Figures 1 and 2 available at http://aje.oxfordjournals.org/, the results did not change appreciably when the analyses were limited to the first hospitalization for an injurious fall.
Figure 1.
Course of disability in all 13 activities over the 6-month follow-up period among participants who were hospitalized for a hip fracture, other fall-related injury, and non–fall-related reason, respectively, New Haven, Connecticut, 1998−2010. Values represent the least-squares mean number of disabilities, accompanied by standard errors. 0 on the x-axis denotes preadmission to the hospital.
Table 3.
Proportional Differences in Disability Scores, Expressed as Adjusted Risk Ratios, for the 2 Fall Groups Relative to the Non–Fall Group, New Haven, Connecticut, 1998−2010a
| Month After Hospitalization |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
2 |
3 |
4 |
5 |
6 |
|||||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Hip fracture | ||||||||||||
| All activities | 1.5 | 1.4, 1.7 | 2.1 | 1.8, 2.4 | 1.8 | 1.6, 2.0 | 1.6 | 1.4, 1.8 | 1.6 | 1.4, 1.8 | 1.5 | 1.3, 1.7 |
| Basic activities | 2.1 | 1.7, 2.5 | 3.4 | 2.6, 4.4 | 2.5 | 1.9, 3.3 | 2.0 | 1.6, 2.6 | 2.1 | 1.6, 2.8 | 1.9 | 1.4, 2.5 |
| Instrumental activities | 1.4 | 1.2, 1.5 | 1.9 | 1.7, 2.2 | 1.7 | 1.5, 1.9 | 1.5 | 1.3, 1.7 | 1.5 | 1.3, 1.7 | 1.4 | 1.2, 1.7 |
| Mobility activities | 1.4 | 1.2, 1.5 | 1.8 | 1.6, 2.1 | 1.6 | 1.5, 1.9 | 1.5 | 1.3, 1.7 | 1.5 | 1.3, 1.7 | 1.5 | 1.3, 1.6 |
| Other falls | ||||||||||||
| All activities | 1.2 | 1.1, 1.3 | 1.8 | 1.5, 2.0 | 1.5 | 1.3, 1.7 | 1.4 | 1.2, 1.5 | 1.4 | 1.2, 1.6 | 1.4 | 1.2, 1.6 |
| Basic activities | 1.4 | 1.1, 1.7 | 2.5 | 1.9, 3.1 | 1.7 | 1.3, 2.2 | 1.6 | 1.2, 2.1 | 1.9 | 1.4, 2.6 | 1.6 | 1.2, 2.2 |
| Instrumental activities | 1.2 | 1.1, 1.3 | 1.7 | 1.4, 2.0 | 1.5 | 1.3, 1.7 | 1.3 | 1.2, 1.5 | 1.3 | 1.2, 1.5 | 1.3 | 1.2, 1.5 |
| Mobility activities | 1.1 | 1.0, 1.2 | 1.6 | 1.4, 1.9 | 1.5 | 1.3, 1.7 | 1.3 | 1.2, 1.5 | 1.3 | 1.2, 1.5 | 1.3 | 1.2, 1.5 |
Abbreviations: CI, confidence interval; RR, risk ratio.
a The Poisson models invoked generalized estimating equations and were adjusted for 1) the matching factors (age, sex, and number of disabilities in the relevant activities in the month prior to hospitalization); 2) the fixed effects of race, education, living situation, number of chronic conditions, body mass index, cognitive impairment, depressive symptoms, physical frailty, number of months since the prior comprehensive assessment, length of hospital stay, and month of follow-up after the index hospitalization; and 3) the correlation among each matched-falls case and its controls with a first-order autoregressive structure.
Figure 2.
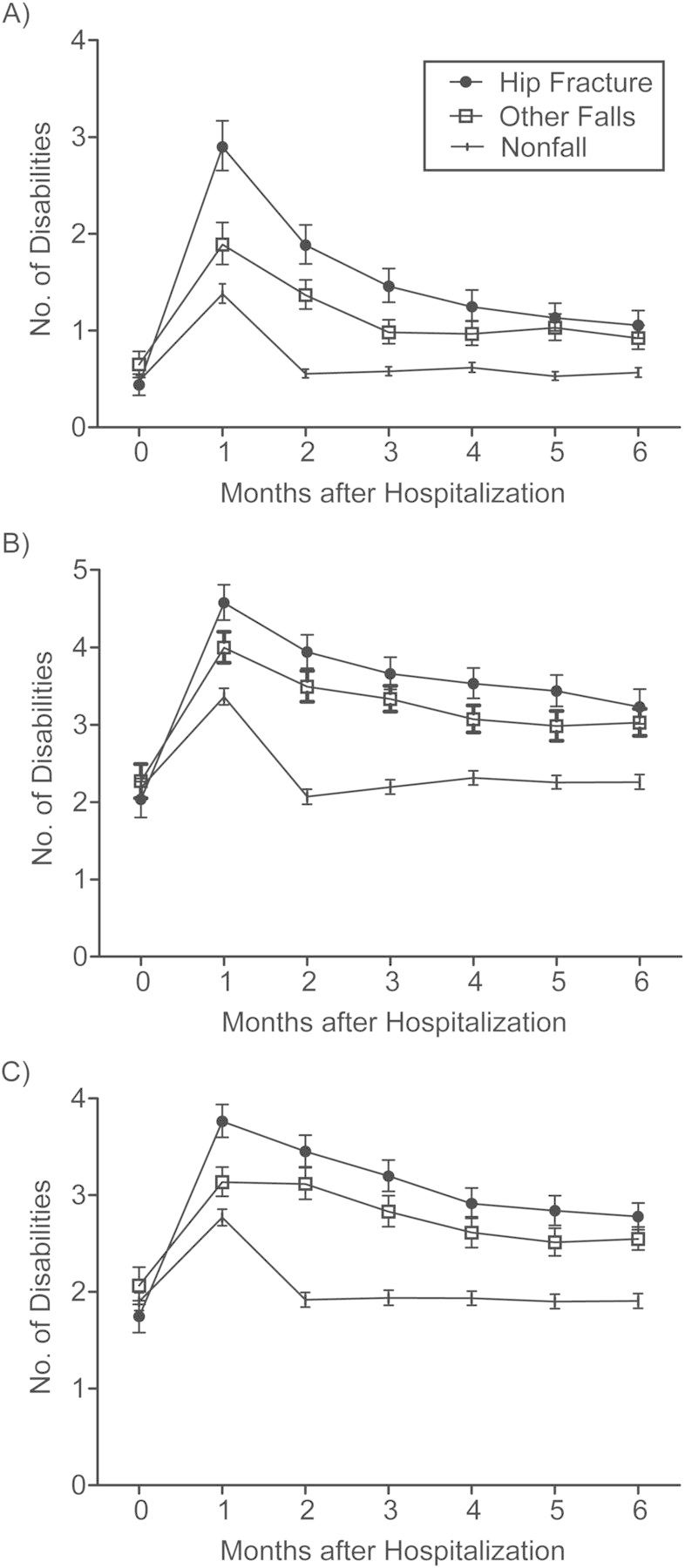
Course of disability in the 4 basic (A), 5 instrumental (B), and 4 mobility (C) activities over the 6-month follow-up period among participants who were hospitalized for a hip fracture, other fall-related injury, and non–fall-related reason, respectively, New Haven, Connecticut, 1998−2010. Values represent the least-squares mean number of disabilities, accompanied by standard errors. 0 on the x-axis denotes preadmission to the hospital.
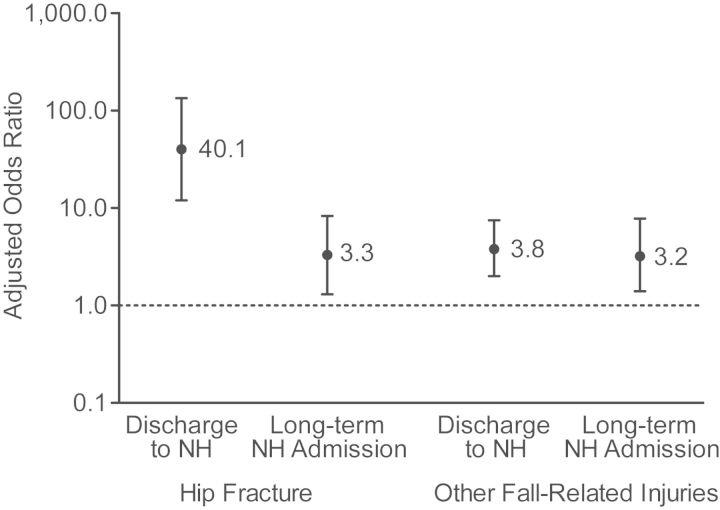
Of the 241 hospitalizations for a non–fall-related reason, 87 (36.1%) resulted in discharge to a nursing home, and 21 (8.7%) led to a long-term nursing home admission. The corresponding values were 56 (94.9%) and 11 (18.6%) for hip fracture and 41 (65.1%) and 13 (20.6%) for other fall-related injury. In multivariable analyses, as shown in Figure 3, the likelihood of being discharged to a nursing home and of having a long-term nursing home admission was considerably greater after hospitalization for a hip fracture and other fall-related injury, respectively, than for a non–fall-related reason.
Figure 3.
Multivariable associations for exposure to hip fracture and other fall-related injuries, respectively, relative to exposure to non–fall-related hospitalizations, on discharge to a nursing home and long-term nursing home admission, New Haven, Connecticut, 1998 − 2010. Point estimates are provided for the adjusted odds ratios, which are accompanied by 95% confidence intervals. NH, nursing home.
DISCUSSION
In this prospective study of community-living older persons, we found that participants who were hospitalized for an injurious fall had worse disability outcomes over a 6-month period and a higher likelihood of long-term nursing home admissions than participants who were hospitalized for a non–fall-related reason. The adverse consequences of injurious falls, relative to those of the other disabling conditions, were observed not only for hip fracture, but also for other fall-related injuries. These findings suggest that the prevention and treatment of injurious falls should be a high priority when decisions are made to allocate resources aimed at reducing the burden of disability in older persons.
Although the high morbidity associated with injurious falls has been well established (10), no prior study, to our knowledge, has evaluated the association of injurious falls relative to that of other disabling conditions on important clinical outcomes. In the current study, participants who were hospitalized for an injurious fall were age-, sex-, and disability-matched to participants who were hospitalized for a non–fall-related reason. These non–fall-related hospitalizations included a diverse array of medical and surgical conditions that were highly morbid, as evidenced by the large increases in disability scores observed during the first month following hospitalization and a 0.11 probability of death within 6 months that exceeded the 0.09 probability of death of the fall-related hospitalizations. Nonetheless, participants who were hospitalized for an injurious fall, including hip fracture and other fall-related injuries, respectively, had higher disability scores at 1 month and a slower and less complete recovery of prehospital function over the following 5 months than participants who were hospitalized for a non–fall-related reason. These findings were observed consistently across 3 different domains of functioning (basic, instrumental, and mobility activities). The adverse consequences of injurious falls were accompanied by greater nursing home utilization, including long-term stays, relative to hospitalizations for a non–fall-related reason.
These findings are important because injurious falls are costly and preventable (8, 12, 13). Based on evidence that has accumulated over the past 2 decades, the US Preventive Services Task Force now recommends exercise or physical therapy and vitamin D supplementation to prevent falls in community-dwelling adults aged 65 years or older who are at increased risk for falls (34). Because they are associated with greater morbidity than other disabling conditions, injurious falls warrant increased attention by policy makers and clinicians as a target for prevention and treatment. Although less pronounced in the short term, the deleterious effects of other fall-related injuries, in terms of severity of disability and likelihood of a long-term nursing home admission, were comparable to those of hip fracture at 6 months, indicating that the long-term sequelae of injurious falls are not limited to hip fracture. To our knowledge, prior studies have not directly compared the adverse consequences of hip fracture with those of other fall-related injuries.
Our study included monthly assessments of the exposures (fall-related and non–fall-related hospitalizations) and outcomes (disability and nursing home admissions), with few missing data and few losses to follow-up for reasons other than death. The frequency of these assessments allowed us to establish temporal precedence and, hence, strengthen potential causal associations between the exposures and outcomes. Although residual confounding is always a possibility in an observational study, participants in the fall and nonfall groups were well matched on the most important prognostic characteristics, including prehospital function, and the multivariable analyses adjusted for a large array of demographic and clinical features, including number of comorbidities, body mass index, cognitive impairment, depressive symptoms, and physical frailty, which were reassessed at 18-month intervals. Additional strengths of the study include an analytical plan that allowed us to distinguish the effects of other fall-related injuries from those of hip fracture and the use of medical records and Medicare claims data to confirm all hospitalizations, including the primary diagnosis, and to determine length of hospital stay.
Nonetheless, our results should be interpreted in the context of several potential limitations. First, to make full use of our longitudinal data, participants were allowed to contribute more than one observation to the analysis. Rigorous methods were used to account for the correlation among the matched cases and controls, and the results were comparable when only the first hospitalization for an injurious fall was evaluated. Second, information was not available on severity of hospital illness; hence, it is possible that participants who were admitted for a fall-related injury were sicker than those who were admitted for a non–fall-related reason. Our multivariable analyses accounted for length of hospital stay, which is often used as an indicator of severity of illness (35). Third, information on the other clinical features was collected during the prior comprehensive assessment rather than during the index hospitalization. For both the cases and controls, the average time between the prior comprehensive assessment and index hospitalization was 8.7 months. Finally, because our study participants were members of a single health plan in a small urban area and were oversampled for slow gait speed, our results may not be generalizable to older persons in other settings. However, the demographic characteristics of our cohort reflect those of older persons in New Haven County, Connecticut, which are similar to the characteristics of the US population as a whole, with the exception of race or ethnic group. The generalizability of our results is enhanced by our high participation rate, which was >75%.
In summary, relative to other disabling conditions, injurious falls are associated with worse disability outcomes and a higher likelihood of long-term nursing home admissions. The adverse consequences of injurious falls, moreover, are not limited to hip fracture. These findings, coupled with prior knowledge, suggest that enhanced efforts to prevent and treat injurious falls could help to alleviate the burden of disability in older persons.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Internal Medicine, Yale School of Medicine, New Haven, Connecticut (Thomas M. Gill, Terrence E. Murphy, Evelyne A. Gahbauer, Heather G. Allore).
The work for this report was supported by a grant from the National Institute on Aging (R37AG17560). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). T.M.G. is the recipient of a Midcareer Investigator Award in Patient-Oriented Research (K24AG021507) from the National Institute on Aging.
We thank Denise Shepard, Andrea Benjamin, Barbara Foster, and Amy Shelton for assistance with data collection; Wanda Carr and Geraldine Hawthorne for assistance with data entry and management; Linda Leo-Summers for assistance with the figures; Peter Charpentier for design and development of the study database and participant-tracking system; and Joanne McGloin for leadership and advice as the Project Director.
Conflict of interest: none declared.
REFERENCES
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261(18):2663–2668. [PubMed] [Google Scholar]
- 3.Self-reported falls and fall-related injuries among persons aged > or =65 years—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(9):225–229. [PubMed] [Google Scholar]
- 4.O'Loughlin JL, Robitaille Y, Boivin JF, et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–354. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46(5):M164–M170. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 6.Sattin RW, Lambert Huber DA, DeVito CA, et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol. 1990;131(6):1028–1037. doi: 10.1093/oxfordjournals.aje.a115594. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME, Doucette J, Claus E, et al. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(11):1214–1221. doi: 10.1111/j.1532-5415.1995.tb07396.x. [DOI] [PubMed] [Google Scholar]
- 8.Cost of falls among older adults. Atlanta, GA: Centers for Disease Control and Prevention; 2012. http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html. (Accessed December 10, 2012) [Google Scholar]
- 9.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53A(2):M112–M119. doi: 10.1093/gerona/53a.2.m112. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 11.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 12.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 doi: 10.1002/14651858.CD007146.pub3. 9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359(3):252–261. doi: 10.1056/NEJMoa0801748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill TM, Desai MM, Gahbauer EA, et al. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 15.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291(13):1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 16.Gill TM, Hardy SE, Williams CS. Underestimation of disability among community-living older persons. J Am Geriatr Soc. 2002;50(9):1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 17.Hardy SE, Gill TM. Factors associated with recovery of independence among newly disabled older persons. Arch Intern Med. 2005;165(1):106–112. doi: 10.1001/archinte.165.1.106. [DOI] [PubMed] [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 19.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 20.Gill TM, Gahbauer EA, Allore HG, et al. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166(4):418–423. doi: 10.1001/archinte.166.4.418. [DOI] [PubMed] [Google Scholar]
- 21.Gill TM, Gahbauer EA, Murphy TE, et al. Risk factors and precipitants of long-term disability in community mobilty: a cohort study of older persons. Ann Intern Med. 2012;156(2):131–140. doi: 10.1059/0003-4819-156-2-201201170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56(3):436–443. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferrucci L, Guralnik JM, Pahor M, et al. Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled. JAMA. 1997;277(9):728–734. [PubMed] [Google Scholar]
- 24.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 25.Cummings P, McKnight B, Greenland S. Matched cohort methods for injury research. Epidemiol Rev. 2003;25:43–50. doi: 10.1093/epirev/mxg002. [DOI] [PubMed] [Google Scholar]
- 26.Olson CM, Cummings P, Rivara FP. Association of first- and second-generation air bags with front occupant death in car crashes: a matched cohort study. Am J Epidemiol. 2006;164(2):161–169. doi: 10.1093/aje/kwj167. [DOI] [PubMed] [Google Scholar]
- 27.Ming K, Rosenbaum PR. A note on optimal matching with variable controls using the assignment algorithm. J Comput Graph Stat. 2001;10(3):455–463. [Google Scholar]
- 28.Ming K, Rosenbaum PR. Substantial gains in bias reduction from matching with a variable number of controls. Biometrics. 2000;56(1):118–124. doi: 10.1111/j.0006-341x.2000.00118.x. [DOI] [PubMed] [Google Scholar]
- 29.Greenland S. Modelling risk ratios from matched cohort data: an estimating equation approach. Appl Statist. 1994;43(1):223–232. [Google Scholar]
- 30.Bergstralh EJ, Kosanke JL, Jacobsen SJ. Software for optimal matching in observational studies. Epidemiology. 1996;7(3):331–332. [PubMed] [Google Scholar]
- 31.Wolinsky FD, Miller TR, An H, et al. Hospital episodes and physician visits: the concordance between self-reports and Medicare claims. Med Care. 2007;45(4):300–307. doi: 10.1097/01.mlr.0000254576.26353.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barry LC, Murphy TE, Gill TM. Depression and functional recovery after a disabling hospitalization in older persons. J Am Geriatr Soc. 2011;59(7):1320–1325. doi: 10.1111/j.1532-5415.2011.03453.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gill TM, Allore HG, Han L. Bathing disability and the risk of long-term admission to a nursing home. J Gerontol A Biol Sci Med Sci. 2006;61(8):821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- 34.Moyer VA U.S. Preventive Services Task Force. Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(3):197–204. doi: 10.7326/0003-4819-157-3-201208070-00462. [DOI] [PubMed] [Google Scholar]
- 35.Sager MA, Rudberg MA, Jalaluddin M, et al. Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc. 1996;44(3):251–257. doi: 10.1111/j.1532-5415.1996.tb00910.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.