Abstract
Background and Purpose
The American Heart Association developed Life’s Simple 7 (LS7) as a metric defining cardiovascular health. We investigated the association between LS7 and incident stroke in black and white Americans.
Methods
REGARDS is a national population-based cohort of 30,239 blacks and whites, aged ≥45 years, sampled from the US population in 2003 – 2007. Data were collected by telephone, self-administered questionnaires and an in-home exam. Incident strokes were identified through bi-annual participant contact followed by adjudication of medical records. Levels of the LS7 components (blood pressure, cholesterol, glucose, body mass index, smoking, physical activity, and diet) were each coded as poor (0 point), intermediate (1 point) or ideal (2 points) health. An overall LS7 score was categorized as inadequate (0–4), average (5–9) or optimum (10–14) cardiovascular health.
Results
Among 22,914 subjects with LS7 data and no previous cardiovascular disease, there were 432 incident strokes over 4.9 years of follow-up. After adjusting for demographics, socioeconomic status, and region of residence, each better health category of the LS7 score was associated with a 25% lower risk of stroke (HR=0.75, 95% CI = 0.63, 0.90). The association was similar for blacks and whites (interaction p-value = 0.55). A one point higher LS7 score was associated with an 8% lower risk of stroke (HR=0.92, 95% CI=0.88, 0.95).
Conclusion
In both blacks and whites better cardiovascular health, based on the LS7 score, is associated with lower risk of stroke, and a small difference in scores was an important stroke determinant.
Keywords: Stroke, Racial differences, Risk factors, Life’s Simple 7
Stroke is the fourth leading cause of death in the United States, and the leading cause of adult disability with direct and indirect costs exceeding $50 billion annually.1 Previous studies demonstrated that most cardiovascular disease (CVD) events including stroke are preventable by optimizing a few key indicators of cardiovascular health.2, 3 In 2010, the American Heart Association/American Stroke Association (AHA/ASA) proposed a population metric to define and track the nation’s cardiovascular health through time. 4 This metric was released as a score called Life’s Simple 7 (LS7). The LS7 metric emphasizes primordial prevention and includes seven modifiable components, including three health factors (glucose, cholesterol and blood pressure) and four health behaviors (body mass index, physical activity, diet and cigarette smoking), categorizing each of these seven factors into ideal, intermediate, and poor levels. Incorporation of modifiable risk factors in the LS7 metric was intentional to promote translation into prevention programs, particularly lifestyle change, a potent weapon in the battle against CVD.5
Recent evidence suggested that presence of more ideal cardiovascular health factors from the LS7 metric is associated with lower CVD and all-cause mortality. 6–8 There are limited data available pertaining to stroke.9 More broadly, there are scarce data on the utility of a composite measure of biological and behavioral risk factors in predicting stroke. Using data from the Reasons for Geographic And Racial Differences in Stroke (REGARDS) study, we determined the association between LS7 and incident stroke, and examined differences by race.
METHODS
Study Participants and Data Collection
The REGARDS study is a population-based cohort study of stroke incidence and cognitive function among US adults ≥45 years of age, oversampling blacks and residents of the southeastern “stroke belt region”.10 Potential participants were identified from commercially available lists of US residents and recruited through a mailing followed by telephone calls. Overall, 30,239 participants were enrolled between 2003 and 2007. Socio-demographic and clinical data were collected with standardized methods at baseline through a telephone interview, an in-home examination and self-administered questionnaires. We included participants with data on blood pressure, cholesterol, glucose, body mass index (BMI), smoking, diet and physical activity (LS7 components). We excluded participants with a self-reported history of stroke, peripheral vascular disease, or coronary heart disease. The Food Frequency Questionnaire (FFQ) documented dietary intake patterns for the one year preceding the in-home visit. 11 The REGARDS study protocol was approved by the Institutional Review Boards at the collaborating centers and all participants provided informed consent.
Life’s Simple 7
Components of the LS7 metric include cigarette smoking, BMI, blood pressure, cholesterol, blood glucose, physical activity and diet. Physical activity and diet classification were modified from the original LS7 definitions (Appendix: online supplement). Diet information was missing for 6,086 (27%), and was imputed. Each LS7 component was given a point score of 0, 1 or 2 to represent poor, intermediate, or ideal health, respectively.12 An overall LS7 score ranging from 0–14 was calculated as the sum of the LS7 component scores. This score was classified as inadequate (0–4), average (5–9) or optimum (10–14) cardiovascular health.
Study Outcome
Participants or their proxies were contacted every 6 months by telephone. Details on stroke adjudication have been published. 13 Stroke events were defined according to the World Health Organization (WHO) definition.14 Events not meeting the WHO definition but characterized by symptoms lasting <24 hours, with neuroimaging consistent with acute ischemia or hemorrhage were also classified as stroke events. Time to a stroke event was recorded as the number of days between the baseline examination and the date of stroke event. Participants who did not develop a stroke were censored on their date of death or last follow-up contact, whichever occurred first.
Statistical Analyses
Baseline characteristics were calculated and compared according to race and LS7 categories using chi-square statistics. The distribution of LS7 components and number of ideal health factors were compared by race and sex. For each LS7 component, stroke incidence rates and adjusted hazard ratios for stroke were calculated separately for blacks and whites. Cox proportional hazards models were used, adjusting for age, race, sex, region of residence (stroke belt or other), income and education. Hazard ratios of stroke across overall LS7 categories (optimum and average vs. inadequate) were calculated. LS7 score was also examined as a continuous variable, considering the hazard ratio per a one point higher overall LS7 score. Hazard ratios for stroke were also calculated for increasing number of ideal health factors with the reference group defined as having no ideal factors. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
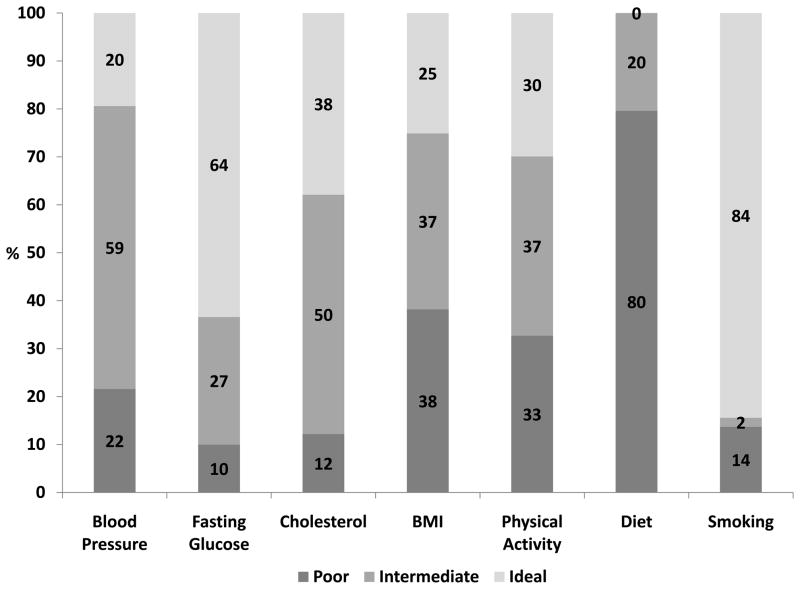
There were 22,914 participants with data on LS7 and no previous CVD. Mean age was 65 years, 42% were black, and 58% female. Socio-demographic factors for LS7 categories by race are presented in Table 1. Male sex, low income, less education and current alcohol use were associated with poorer cardiovascular health in both blacks and whites. The distribution of LS7 categories differed significantly between blacks and whites. Whites had a higher proportion of people in the optimum cardiovascular health category (19%) as compared to blacks (7%) irrespective of age, sex, income, education and geographic region. The distribution of ideal status varied widely across LS7 factors (Figure 1), ranging from 84% of participants having ideal status for smoking, to 0% of participants having an ideal diet.
Table 1.
Baseline characteristics of 22, 914 REGARDS study participants by race and LS7 health categories
| Cardiovascular Health Categories | ||||||||
|---|---|---|---|---|---|---|---|---|
| Blacks (n=9,553) | Whites (n=13,361) | |||||||
| Characteristic | Optimum n=692 |
Average n=7302 |
Inadequate n=1559 |
P-value | Optimum n=2589 |
Average n=9756 |
Inadequate n=1016 |
P-value |
|
Age ≤65 years % >65 years % |
7.4 | 75.7 | 16.9 | 0.13 | 20.5 | 71.2 | 8.3 | <0.001 |
| 7.0 | 77.4 | 15.5 | 18.1 | 75.1 | 6.8 | |||
|
Sex Male % Female% |
8.6 | 78.4 | 12.9 | <0.001 | 18.5 | 74.9 | 6.6 | <0.001 |
| 6.5 | 75.3 | 18.2 | 20.1 | 71.4 | 8.4 | |||
|
Income >$20,000k % ≤ $20,000k % |
8.1 | 77.2 | 14.7 | <0.001 | 20.2 | 72.9 | 6.8 | <0.001 |
| 4.6 | 74.1 | 21.3 | 12.4 | 73.5 | 14.1 | |||
|
Education >12 years % ≤12 years % |
7.9 | 77.1 | 14.9 | <0.001 | 20.1 | 72.7 | 7.2 | <0.001 |
| 4.1 | 73.2 | 22.7 | 8.3 | 78.8 | 13.1 | |||
|
Geographic Region Belt % Non-belt % |
7.3 | 76.1 | 16.6 | 0.18 | 19.6 | 72.7 | 7.7 | 0.24 |
| 7.0 | 78.1 | 14.9 | 18.5 | 74.2 | 7.3 | |||
|
Alcohol consumption Current % Former % |
7.8 | 75.9 | 16.2 | 0.008 | 21.3 | 72.0 | 6.7 | <0.001 |
| 6.9 | 75.5 | 17.6 | 14.9 | 74.8 | 10.2 | |||
LS7= Life’s Simple 7
Figure 1.
Distribution of LS7 components among REGARDS participants
The mean (SD) overall LS7 score was 7.2 (± 2.2) points. Adjusting for age and sex, the mean (± SD) overall LS7 score was lower for blacks (6.5 ± 2.0) than whites (7.6 ± 2.1). Blacks had fewer ideal factors compared with whites. Only 3% of blacks and 8% of whites had five or more ideal factors (Figure: online supplement).
Over 4.9 years of follow-up, there were 432 incident strokes (232 in whites and 200 in blacks). For many LS7 components, stroke incidence was lowest in those with ideal status and highest in those with poor levels (Table 2). For example, for blood pressure incidence rates per 10,000 person years for poor, intermediate and ideal status were 3.2, 1.8 and 1.1, respectively, for blacks and 2.4, 1.9 and 0.8, respectively, for whites. The adjusted hazard ratios for some LS7 components (total cholesterol, blood pressure, blood glucose and smoking), showed a graded relationship with stroke, particularly among whites (Table 2).
Table 2.
Incidence rates and adjusted HR of stroke for LS7 components among REGARDS participants by race
| Overall | Blacks | Whites | |||||
|---|---|---|---|---|---|---|---|
| IR† | HR* (95% CI) | IR | HR (95% CI) | IR | HR (95% CI) | ||
| Total cholesterol (n=22,106) | Ideal | 1.9 | 0.8 (0.6, 1.1) | 2.3 | 0.7 (0.4, 1.0) | 1.6 | 0.7 (0.5, 1.2) |
| Intermediate | 1.8 | 0.8 (0.6, 1.0) | 1.8 | 0.8 (0.5, 1.3) | 1.8 | 0.8 (0.6, 1.3) | |
| Poor | 2.1 | Ref | 2.5 | Ref | 1.8 | Ref | |
| Blood pressure (n=22,864) | Ideal | 0.9 | 0.4 (0.3,0.6) | 1.1 | 0.4(0.2, 0.7) | 0.8 | 0.5 (0.3, 0.8) |
| Intermediate | 1.8 | 0.7(0.6, 0.9) | 1.8 | 0.6(0.4, 0.8) | 1.9 | 0.9 (0.6, 1.3) | |
| Poor | 2.8 | Ref | 3.2 | Ref | 2.4 | Ref | |
| Blood Glucose (n=22,551) | Ideal | 1.6 | 0.6 (0.5, 0.9) | 1.7 | 0.7 (0.4, 1.1) | 1.5 | 0.6 (0.4, 1.0) |
| Intermediate | 2.3 | 0.9 (0.6, 1.2) | 2.5 | 1.0 (0.6, 1.6) | 2.2 | 0.8 (0.5, 1.4) | |
| Poor | 2.5 | Ref | 2.4 | Ref | 2.6 | Ref | |
| Physical activity (n=22,585) | Ideal | 1.8 | 0.9 (0.7, 1.1) | 1.8 | 0.8 (0.6,1.2) | 1.8 | 0.9 (0.6, 1.3) |
| Intermediate | 1.8 | 0.9 (0.6, 1.1) | 2.0 | 0.9 (0.7, 1.3) | 1.6 | 0.9 (0.6, 1.2) | |
| Poor | 2.0 | Ref | 2.2 | Ref | 1.9 | Ref | |
| Healthy diet score (n=16,829) | Ideal** | - | - | ||||
| Intermediate | 1.8 | 1.0 (0.7, 1.3) | 2.2 | 1.1 (0.7,1.8) | 1.5 | 0.9 (0.6, 1.3) | |
| Poor | 1.9 | Ref | 2.0 | Ref | 1.7 | Ref | |
| Smoking (n=22,914) | Ideal | 2.2 | 0.6 (0.5, 0.8) | 2.9 | 0.3 (0.1, 1.2) | 1.6 | 0.5 (0.4, 0.7) |
| Intermediate | 2.3 | 0.5 (0.2, 1.1) | 1.9 | 0.7 (0.5, 1.0) | 2.5 | 0.7 (0.3, 1.8) | |
| Poor | 2.4 | Ref | 2.3 | Ref | 2.4 | Ref | |
| Body mass index (n=22,771) | Ideal | 2.1 | 1.0 (0.8, 1.3) | 2.2 | 1.1 (0.7,1.6) | 1.9 | 1.0 (0.7, 1.4) |
| Intermediate | 1.9 | 1.1 (0.9, 1.4) | 2.1 | 1.1(0.8,1.6) | 1.7 | 1.1 (0.8, 1.6) | |
| Poor | 2.0 | Ref | 2.3 | Ref | 1.9 | Ref | |
adjusted for age, gender, income, education, alcohol use, geographic region
category had no data
Incident rate per 10,000 person-years
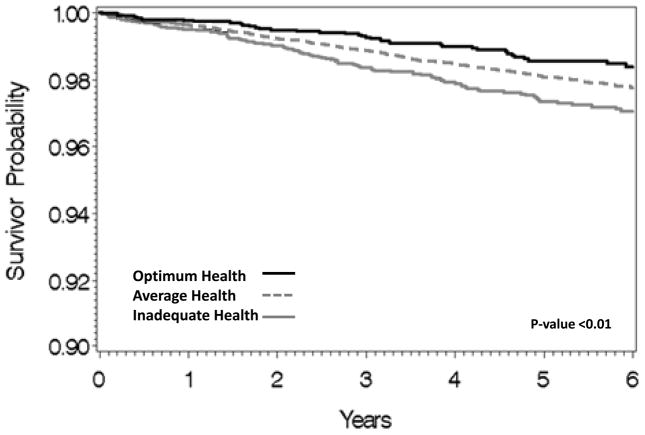
The overall LS7 score categories of cardiovascular health were inversely associated with incident stroke in a graded fashion (Figure 2). Stroke incidence rates were 2.4 per 10,000 person-years among those with inadequate health and 1.3 per 10,000 person-years with optimum health. After multivariable adjustment, with LS7 score category modeled as an ordinal variable, each better health category was associated with a 25% lower risk of incident stroke (HR=0.75, 95% CI = 0.63, 0.90). Compared with the inadequate health category, those with average (HR=0.72, 95% CI= 0.55, 0.96) or optimum (HR=0.52, 95% CI= 0.35, 0.76) health had lower stroke risk. Although the association of LS7 category and stroke was not statistically significant among blacks (Table 3), the crude and adjusted hazard ratios were similar for blacks and whites (p-value for interaction = 0.55).
Figure 2.
Survival free from stroke by cardiovascular health categories
Table 3.
Incidence rate and adjusted hazard ratio (95% CI) of incident stroke for categories of overall LS7 Score by race
| Overall (n=22,914) | Blacks (n=9,553) | Whites (n=13,361) | ||||
|---|---|---|---|---|---|---|
| IR† | HR* (95% CI) | IR | HR (95% CI) | IR | HR (95% CI) | |
| Cardiovascular Health Categories | ||||||
| Optimum | 1.3 | 0.52 (0.35, 0.76) | 1.6 | 0.63 (0.33, 1.22) | 1.2 | 0.49 (0.29, 0.89) |
| Average | 1.9 | 0.73 (0.55, 0.96) | 1.9 | 0.76 (0.53, 1.10) | 1.7 | 0.71 (0.46, 1.10) |
| Inadequate | 2.4 | 1.0 | 2.4 | 1.0 | 2.2 | 1.0 |
| P for trend | <0.001 | 0.22 | 0.04 | |||
| CV Health Score per unit increase | 0.92 (0.88, 0.95) | 0.93 (0.87, 0.98) | 0.91 (0.86, 0.96) | |||
adjusted for age, sex, income, alcohol use, education, geographic region
LS7=Life’s Simple 7
Incident rate per 10,000 person-years
For the total LS7 score on a continuous scale from 0 (all 7 poor) to 14 (all 7 ideal), a one point higher LS7 score was associated with an 8% lower risk of stroke (HR=0.92, 95% CI=0.88, 0.95) and this was similar in blacks and whites (Table 3). The association of LS7, or its individual components, with stroke risk did not differ after exclusion of those with hemorrhagic stroke (n=81). (HR for ischemic stroke = 0.90, 95% CI = 0.86, 0.95). Finally, increasing number of ideal factors was inversely associated with risk of stroke in both blacks and whites. Even those with only 1 ideal factor compared with those with 0 ideal factors had a lower stroke risk (HR 0.70, 95% CI= 0.42, 1.19).Those with 6 versus 0 ideal factors had a multivariable adjusted hazard ratio of 0.34 (95% CI =0.08, 1.52) (Table 4). In sensitivity analysis, results were similar when participants with imputed diet scores were excluded, or were all assumed to have a poor diet or an intermediate diet.15
Table 4.
Adjusted hazard ratios for incident stroke associated with number of ideal LS7 components
| No. of Ideal Health Metrics | Overall | Blacks | Whites | |||
|---|---|---|---|---|---|---|
| Stroke (n) | HR* (95% CI) | Stroke (n) | HR (95% CI) | Stroke (n) | HR (95% CI) | |
| 0 (n=576) | 16 | Ref | 8 | Ref | 8 | Ref |
| 1 (n=4465) | 99 | 0.70 (0.42, 1.19) | 56 | 0.86 (0.41, 1.81) | 43 | 0.51 (0.24, 1.20) |
| 2 (n=7249) | 155 | 0.67 (0.40, 1.13) | 74 | 0.81 (0.39, 1.69) | 81 | 0.49 (0.24, 1.02) |
| 3 (n=6105) | 104 | 0.53 (0.31, 0.90) | 43 | 0.66 (0.31, 1.41) | 61 | 0.38 (0.18, 0.80) |
| 4 (n=3187) | 40 | 0.40 (0.23, 0.73) | 15 | 0.58 (0.25, 1.38) | 25 | 0.27 (0.12, 0.60) |
| 5 (n=1117) | 16 | 0.50 (0.25, 1.0) | 3 | 0.51 (0.14, 1.96) | 13 | 0.38 (0.16, 0.92) |
| 6 (n=216) | 2 | 0.34 (0.08, 1.52) | 1 | 0.50 (0.56, 1.07) | 1 | 0.15 (0.02, 1.19) |
adjusted for age, sex, socioeconomic, alcohol use, education, geographic region
DISCUSSION
The stroke epidemic can be curtailed with a multidisciplinary strategy that identifies and manages stroke risk factors.16 The AHA developed the LS7 metric as part of its strategic impact goal to improve the cardiovascular health of all Americans by 20%, by 2020. Our study shows that the LS7 metric is a useful tool to describe the risk of incident stroke and has the potential to help refine population interventions to reduce stroke incidence rates in the US population. Using a simple point system to represent the LS7 metric, an incremental increase in the overall LS7 score (inadequate to average to optimum) was associated with a 25% lower risk of incident stroke. However, there were important differences in population levels of LS7, as blacks had lower levels of cardiovascular health factors than whites. These findings suggest that comprehensive population-based interventions targeting risk factors included in the LS7 will be critical to support the attainment of the AHA’s 2020 impact goal for cardiovascular health, reduce the incidence and prevalence of stroke, and eliminate disparities.
The prevalence of ideal cardiovascular health is extremely low in the United States as measured in national studies and other cohorts including REGARDS.6, 17 The distribution of ideal factors in REGARDS was similar to the NHANES and Atherosclerosis Risk in Communities Study (ARIC) studies. 7, 18 Our study from a more contemporary cohort demonstrates that blacks have lower levels of ideal factors compared with whites and also presents analysis of stroke. The association of LS7 and stroke was not statistically different in blacks than whites. This finding needs confirmation from other studies or further follow-up in REGARDS. National statistics and REGARDS findings demonstrated higher stroke incidence and stroke mortality rates for blacks compared with whites, possibly due to the higher prevalence of hypertension, obesity, and diabetes among blacks, although the higher risk factor levels only explain about 50% of the excess risk.13, 19, 20 Understanding the basis for these differences will be important to design and effectively implement stroke prevention programs among blacks.
The Northern Manhattan Study (NOMAS) study previously reported that increasing numbers of ideal health factors for LS7 was associated with reduced stroke risk. 9 Our findings expand on these by considering the full range of poor to intermediate to ideal LS7 score. Moreover, we showed that a one-point increase in overall LS7 score, which corresponds to improvement of one component of the LS7 score by one level (e.g. from poor to intermediate or from intermediate to ideal) was associated with an 8% lower risk of stroke. Thus, unlike NOMAS, our findings support the hypothesis that small shifts in the population distribution of risk factors can have a dramatic impact on reducing the disease burden in populations.21 Although there were differences in associations of each component of LS7 with stroke risk, the overall metric is conceptualized as a broad public health metric for CVD prevention and we demonstrate the utility of this metric specifically for stroke risk.
Improvements in a single health behavior could result in a reduction of CVD, and also improvements of other cardiovascular health factors (e.g. obesity, cholesterol). Indeed, these components are interrelated and do not operate in silos. Previous studies also support the potential of using population-based strategies targeting multiple risk factors simultaneously to achieve reductions in stroke and CVD rates in communities. 2, 22
Our study has several strengths including the large national sample, with over-sampling of blacks to allow examination of racial differences. Data collection used standardized questionnaires and measured, not self-reported risk factor levels. There was rigorous ascertainment of stroke outcomes including adjudication of stroke events by neurologists. There are also some limitations to our study. Health factors and behaviors were measured only once and thus we cannot assess whether changes in LS7 score affect stroke incidence, and we expect some misclassification. The cooperation rate for participation in REGARDS was 49%. Although, this is similar to other large national cohorts, this may limit generalizability of the findings. We also used a modified definition for physical activity and diet for computation of the LS7 score.
In conclusion, in this large population-based sample of US adults age 45 and older, a healthier cardiovascular disease risk factor profile, as defined by the LS7 score, was associated with a substantially reduced risk of stroke. Based on our findings, differences in LS7 score corresponding to an improvement by one level of one component of the LS7 metric may result in substantial reductions in stroke risk. This provides confidence that meeting the AHA goals for LS7 may lead to reduction in stroke incidence. Future studies are needed to determine the actual risk reduction benefit that can be achieved through an intervention approach to improve health behaviors and risk factors in the LS7 metric
Supplementary Material
Acknowledgments
Sources of Funding
REGARDS is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH), Department of Health and Human Service. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the NINDS or the NIH or the Centers for Disease Control and Prevention. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org Dr. Vaccarino is funded through K24 HL077506
Footnotes
Disclosures: None
References
- 1.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 2.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282:2012–8. doi: 10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 3.Vasan RS, Sullivan LM, Wilson PW, Sempos CT, Sundstrom J, Kannel WB, et al. Relative importance of borderline and elevated levels of coronary heart disease risk factors. Ann Intern Med. 2005;142:393–402. doi: 10.7326/0003-4819-142-6-200503150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–84. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 6.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–6. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–95. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–83. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125:2975–84. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 11.Block G, Thompson FE, Hartman AM, Larkin FA, Guire KE. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Am Diet Assoc. 1992;92:686–93. [PubMed] [Google Scholar]
- 12.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular Health Behavior and Health Factor Changes (1988–2008) and Projections to 2020: Results from the National Health and Nutrition Examination Surveys (NHANES) Circulation. 2012 doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–27. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke. 1989;20:1407–31. doi: 10.1161/01.str.20.10.1407. [DOI] [PubMed] [Google Scholar]
- 15.DBR . Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 2004. [Google Scholar]
- 16.Gorelick PB, Sacco RL, Smith DB, Alberts M, Mustone-Alexander L, Rader D, et al. Prevention of a first stroke: a review of guidelines and a multidisciplinary consensus statement from the National Stroke Association. JAMA. 1999;281:1112–20. doi: 10.1001/jama.281.12.1112. [DOI] [PubMed] [Google Scholar]
- 17.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011;123:850–7. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, et al. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–75. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Casper MLBE, Williams GI., Jr . Atlas of stroke mortality: racial, ethnic, and geographic disparities in the United States. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 21.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32. doi: 10.1093/ije/30.3.427. discussion 33–4. [DOI] [PubMed] [Google Scholar]
- 22.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation. 2008;118:947–54. doi: 10.1161/CIRCULATIONAHA.108.781062. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.