Abstract
OBJECTIVE
Transcription factor 7-like 2 (TCF7L2) polymorphisms are strongly associated with type 2 diabetes, but controversially with plasma lipids and cardiovascular disease. Interactions of the Mediterranean diet (MedDiet) on these associations are unknown. We investigated whether the TCF7L2-rs7903146 (C>T) polymorphism associations with type 2 diabetes, glucose, lipids, and cardiovascular disease incidence were modulated by MedDiet.
RESEARCH DESIGN AND METHODS
A randomized trial (two MedDiet intervention groups and a control group) with 7,018 participants in the PREvención con DIetaMEDiterránea study was undertaken and major cardiovascular events assessed. Data were analyzed at baseline and after a median follow-up of 4.8 years. Multivariable-adjusted Cox regression was used to estimate hazard ratios (HRs) for cardiovascular events.
RESULTS
The TCF7L2-rs7903146 polymorphism was associated with type 2 diabetes (odds ratio 1.87 [95% CI 1.62–2.17] for TT compared with CC). MedDiet interacted significantly with rs7903146 on fasting glucose at baseline (P interaction = 0.004). When adherence to the MedDiet was low, TT had higher fasting glucose concentrations (132.3 ± 3.5 mg/dL) than CC+CT (127.3 ± 3.2 mg/dL) individuals (P = 0.001). Nevertheless, when adherence was high, this increase was not observed (P = 0.605). This modulation was also detected for total cholesterol, LDL cholesterol, and triglycerides (P interaction < 0.05 for all). Likewise, in the randomized trial, TT subjects had a higher stroke incidence in the control group (adjusted HR 2.91 [95% CI 1.36–6.19]; P = 0.006 compared with CC), whereas dietary intervention with MedDiet reduced stroke incidence in TT homozygotes (adjusted HR 0.96 [95% CI 0.49–1.87]; P = 0.892 for TT compared with CC).
CONCLUSIONS
Our novel results suggest that MedDiet may not only reduce increased fasting glucose and lipids in TT individuals, but also stroke incidence.
Although transcription factor 7-like 2 (TCF7L2) gene is the strongest and most widely replicated locus associated with type 2 diabetes (1–5), there are very few studies that have examined the association between genetic variation in this gene and cardiovascular disease (6–9). Neither do we know how diet modulates the associations between this gene and type 2 diabetes, plasma glucose concentrations, plasma lipids, other cardiovascular risk factors, or cardiovascular events (10). A deeper understanding of these associations and dietary interactions is crucial for improving existing, or designing new, interventions in primary prevention of cardiovascular diseases in high-risk subjects. The product of TCF7L2 is a high-mobility box-containing transcription factor that plays a role in activating many genes (11,12). The mechanism through which the TCF7L2 is associated with type 2 diabetes has yet to be determined (13), although various hypotheses have been proposed (14–17). The rs7903146 polymorphism (C>T) is one of the most important genetic variants influencing type 2 diabetes risk (18). At present, the prevalence of the 7903146T allele, associated with higher type 2 diabetes risk, is lower than that of the C allele in Caucasians. However, Helgason et al. (19) reported that the rs7903146T allele is probably the ancestral allele, suggesting that changes in its prevalence are due to positive selection, driven, among other things, by dietary factors. Thus, a study (20) highlighted the north–south gradient for the 7903146T allele found in Europe, the frequency of this allele being higher in Mediterranean populations (∼0.4) than in Northern Europeans (∼0.2). Although there is evidence that the Mediterranean food pattern may reduce type 2 diabetes risk (21) and cardiovascular disease incidence (22), no studies have investigated the influence of Mediterranean diet (MedDiet) on TCF7L2 gene effects. Some investigations (23–25) have analyzed the interaction between dietary factors and TCF7L2 gene variation on incidence of type 2 diabetes, but the results are inconclusive. In addition to type 2 diabetes risk and fasting glucose concentrations, the TCF7L2-rs7903146 polymorphism has also been associated with other diabetes-related traits such as plasma lipid concentrations (26–28), metabolic syndrome (29,30), and even with increased atherosclerosis and cardiovascular disease risk (7–9). Although a few studies have found interactions among dietary polyunsaturated fatty acids, saturated fat, or proteins in determining plasma lipids or metabolic syndrome components (29–32), there are no data on the influence of an overall healthy food pattern, such as the MedDiet pattern, in modulating the associations between the TCF7L2-rs7903146 polymorphism and these traits.
Moreover, no study has examined the influence of a dietary intervention with MedDiet on the effects of the TCF7L2 polymorphisms on incidence of cardiovascular events. Thus, our aims were 1) to investigate the influence of prerandomization adherence to the MedDiet pattern in modulating the associations between the TCF7L2-rs7903146 polymorphism and fasting glucose, type 2 diabetes, plasma lipids, and incidence of major cardiovascular diseases (stroke and myocardial infarction); and 2) to assess the modulation of the effect of this polymorphism on the incidence of these cardiovascular events through long-term postrandomization intervention (median ∼5 years) with MedDiet in a large nutrition intervention trial (22).
RESEARCH DESIGN AND METHODS
Subjects
We included the 7,018 participants (2,993 men and 4,025 women) entering the PREvención con DIetaMEDiterránea (PREDIMED) trial from whom DNA was isolated, the TCF7L2-rs7903146 polymorphism determined, and who had valid data for the main clinical and lifestyle variables analyzed. The PREDIMED study is a multicenter clinical trial (ISRCTN35739639) aimed at assessing the effects of the MedDiet on the primary prevention of cardiovascular disease (22,33). The completion date of this study was December 2010. The 7,018 participants analyzed did not differ in the main characteristics from those of the total cohort (7,447). Details of this study have been fully described elsewhere (22,34). Briefly, from October 2003, potential high-cardiovascular-risk subjects were selected by physicians in primary care centers. Eligible subjects were community-dwelling people (aged 55–80 years for men, 60–80 years for women) who fulfilled at least one of two criteria: type 2 diabetes (35) and three or more cardiovascular risk factors (hypertension, dyslipidemia, BMI ≥25 kg/m2, current smoking, or a family history of premature cardiovascular disease). Exclusion criteria included a personal history of cardiovascular disease, any severe chronic illness, and drug or alcohol addiction (33). Participants were randomly assigned to three interventions: MedDiet with extra virgin olive oil (EVOO), MedDiet with mixed nuts, and control group (low-fat diet). Participants assigned to both MedDiet groups received intensive training to follow the MedDiet and allotments of either EVOO (50 mL/day) or mixed nuts (30 g/day) at no cost (22,34). Participants assigned to the control diet received recommendations to reduce the intake of all types of fat. A detailed description of the nutritional interventions has been provided elsewhere (22). Subjects were followed up for a median of 4.8 years (interquartile range 2.8–5.8 years). The Institutional Review Board of each participating center approved the study protocol, and all participants provided written informed consent.
Demographic, clinical, anthropometric, and dietary measurements
The baseline examination included assessment of standard cardiovascular risk factors, medication use, sociodemographic factor, and lifestyle variables, as previously detailed (33,34). Food consumption was determined by a validated semiquantitative 137-item food frequency questionnaire (36). The glycemic index (GI) for food and beverage items was estimated by using average values from the 2002 international tables of GI and glycemic load (GL) and expanded in 2008 (37) with glucose as the reference food. Dietary GL was calculated considering the quality and the amount of carbohydrate (GL = [GI × amount of available carbohydrate]/100) (38). A validated 14-item questionnaire indicating the degree of adherence to the traditional MedDiet was also administered (39). Each question was scored 0 or 1 (Supplementary Table 1). The final score ranged from 0–14. The greater the score, the greater the adherence to the MedDiet. Dichotomous variables of prerandomization adherence to the MedDiet and nutrient intake were created using sample means as cutoff points. Physical activity was estimated by the Minnesota Leisure Time Physical Activity Questionnaire as previously reported (34). Weight and height were measured with calibrated scales and a wall-mounted stadiometer, respectively. BMI was calculated as weight in kilograms divided by the square of height in meters.
Outcome ascertainment
The primary end point was the occurrence of the major cardiovascular events and comprised stroke, myocardial infarction, or cardiovascular death (22). We used four sources of information to identify end points: 1) repeated contacts with participants, 2) family physicians, 3) yearly review of medical records, and 4) consultation of the National Death Index. All medical records related to end points were examined by the end point adjudication committee, whose members were blind to treatment allocation. Only end points confirmed by the adjudication committee that occurred between 1 October 2003 and 1 December 2010 were included in the analyses. The criteria for adjudicating primary outcomes are detailed elsewhere (22).
Biochemical determinations, DNA extraction, and genotyping
At baseline, blood samples were obtained from each participant after an overnight fast, frozen at −80°C, and shipped to central laboratories for analyses. Fasting glucose, total cholesterol, triglycerides, HDL cholesterol (HDL-C), and LDL cholesterol (LDL-C) were measured using standard enzymatic automated methods as previously described (33). In patients whose triglyceride levels were <400 mg/dL, LDL-C concentrations were estimated using the Friedewald formula. Biochemical data could not be obtained for all of the 7,018 participants at baseline (ranging from n = 6,568 for total cholesterol and 6,201 for fasting glucose).
Genomic DNA was extracted from buffy coat with the MagNaPure LC DNA solation Kit (Roche Diagnostics, Mannheim, Germany). The TCF7L2-rs7903146 was genotyped on a 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA) using a fluorescent allelic discrimination TaqMan assay. The calling rate was >95%; 5% of samples were randomly selected and genotyped a second time, and there were no discrepancies.
Statistical analyses
The χ2 tests were used to test differences in percentages. Triglycerides were log-transformed for statistical analyses. The t and ANOVA tests were applied to compare crude means. Multivariate adjustments for continuous variables were carried out by covariance analysis. Models were adjusted for age, sex, BMI, type 2 diabetes, total energy intake, alcohol consumption, smoking, physical activity, and medications (antidiabetic, lipid-lowering, and antihypertensive drugs). Dichotomous variables for dietary intake and physical activity were created using as cutoff the sample means. Logistic regression methods were also used for prevalence of type 2 diabetes. To test the interaction between the TCF7L2-rs7903146 polymorphism, adherence to MedDiet, or the other dietary variables on cardiovascular risk factors at baseline, separate multivariate regression models including the corresponding main effects and interaction terms in addition to control for potential confounders were fitted assuming codominant or recessive genetic effects. Stratified analyses were also carried out. To examine the association between MedDiet and cardiovascular events, we used Cox regression models with the length of follow-up as the primary time variable. The exposure time was calculated as the time between recruitment and the date of death for deceased participants or the last study visit or the last recorded clinical event of participants who did not die. We evaluated the association between both prerandomization adherence to the MedDiet (low and high) and the postrandomization intervention with MedDiet (analyses were based on the intention-to-treat principle) and cardiovascular events. Hazard ratios (HRs) with 95% CI for the TCF7L2-rs7903146 genotypes were calculated and stratified by MedDiet (prerandomization adherence to the MedDiet or intervention with MedDiet, pooling together the groups supplemented with EVOO and nuts vs. the control group). In the multivariable model 1, covariates were sex, age, and recruitment center and intervention group. A multivariable model 2 was also fitted including additional adjustment for type 2 diabetes, BMI, smoking, drinking, total energy intake, and prerandomization adherence to the MedDiet. Kaplan-Meier survival curves were plotted to estimate the probability of remaining free of myocardial infarction during follow-up. Statistical analyses were performed with the SPSS package, version 17.0 (SPSS, Chicago, IL). All tests were two-tailed, and P values <0.05 were considered statistically significant.
RESULTS
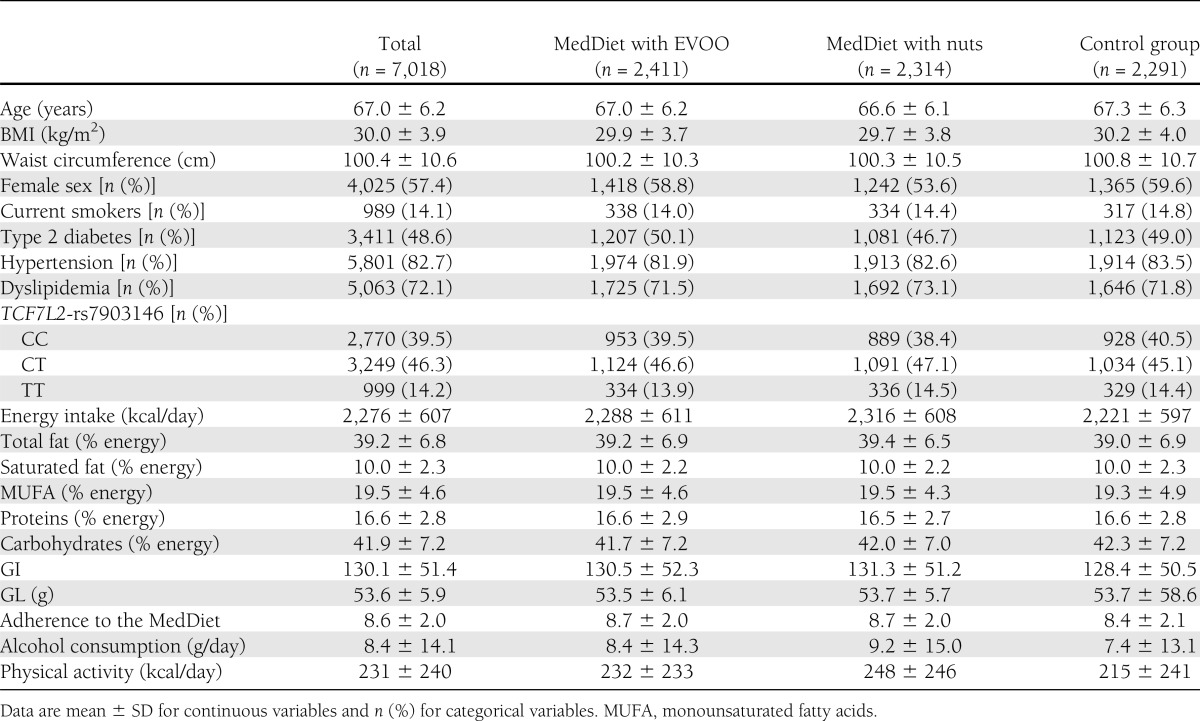
Table 1 shows demographic, biochemical, clinical lifestyle, and genetic characteristics of the 7,018 participants in the PREDIMED study at baseline according to the randomized allocation to the three dietary intervention groups: MedDiet supplemented with EVOO, MedDiet supplemented with nuts, and control group. In the whole population, prevalence of type 2 diabetes, dyslipidemia, obesity, and hypertension was high. We did not find significant differences in medication use among the intervention groups at baseline: 48.0% of subjects were on lipid-lowering drugs, 72.5% on antihypertensive drugs, 32.1% on oral hypoglycemic agents, and 6.9% on insulin. In the whole population, mean prerandomization adherence to MedDiet was 9 ± 2 points. For the TCF7L2-rs7903146, overall prevalence of TT individuals was 14.2%. Genotype frequencies did not deviate from Hardy-Weinberg equilibrium expectations (P = 0.380).
Table 1.
Demographic, clinical, lifestyle, and genetic characteristics of the study participants at baseline according to the intervention groups
Association between the TCF7L2-rs7903146 polymorphism and type 2 diabetes, fasting glucose, and plasma lipid concentrations at baseline
As expected, this polymorphism presented a highly significant association with type 2 diabetes (Supplementary Table 2), TT individuals having greater risk compared with CC homozygotes (odds ratio 1.87 [95% CI 1.62–2.17]). We also observed a highly significant association (P < 0.001) between the polymorphism and fasting glucose. This association remained statistically significant even after adjustment for type 2 diabetes, although losing much of its statistical significance (P = 0.021). We did not observe any significant associations between the TCF7L2-rs7903146 polymorphism and plasma lipids (total cholesterol, triglycerides, LDL-C, and HDL-C at baseline in the population as a whole) (Supplementary Table 2).
Gene–diet interactions of the TCF7L2-rs7903146 polymorphism and prerandomization adherence to the MedDiet on type 2 diabetes and fasting glucose
We did not find a statistically significant interaction between adherence to the MedDiet (low and high strata based on the population mean) and the TCF7L2-rs7903146 polymorphism in determining prevalence of type 2 diabetes (P interaction: 0.251). Likewise, no statistically significant interactions were detected when two categories of other dietary variables (carbohydrates, fiber, GI, GL, total fat, saturated fat, and proteins) were analyzed (results not shown). This may be due in part to the fact that we are dealing with prevalent cases of type 2 diabetes. Therefore, we analyzed how current fasting glucose concentrations are modulated by the MedDiet and the TCF7L2 polymorphism to better understand the relationship between present dietary intake and a TCF7L2 polymorphism-related trait.
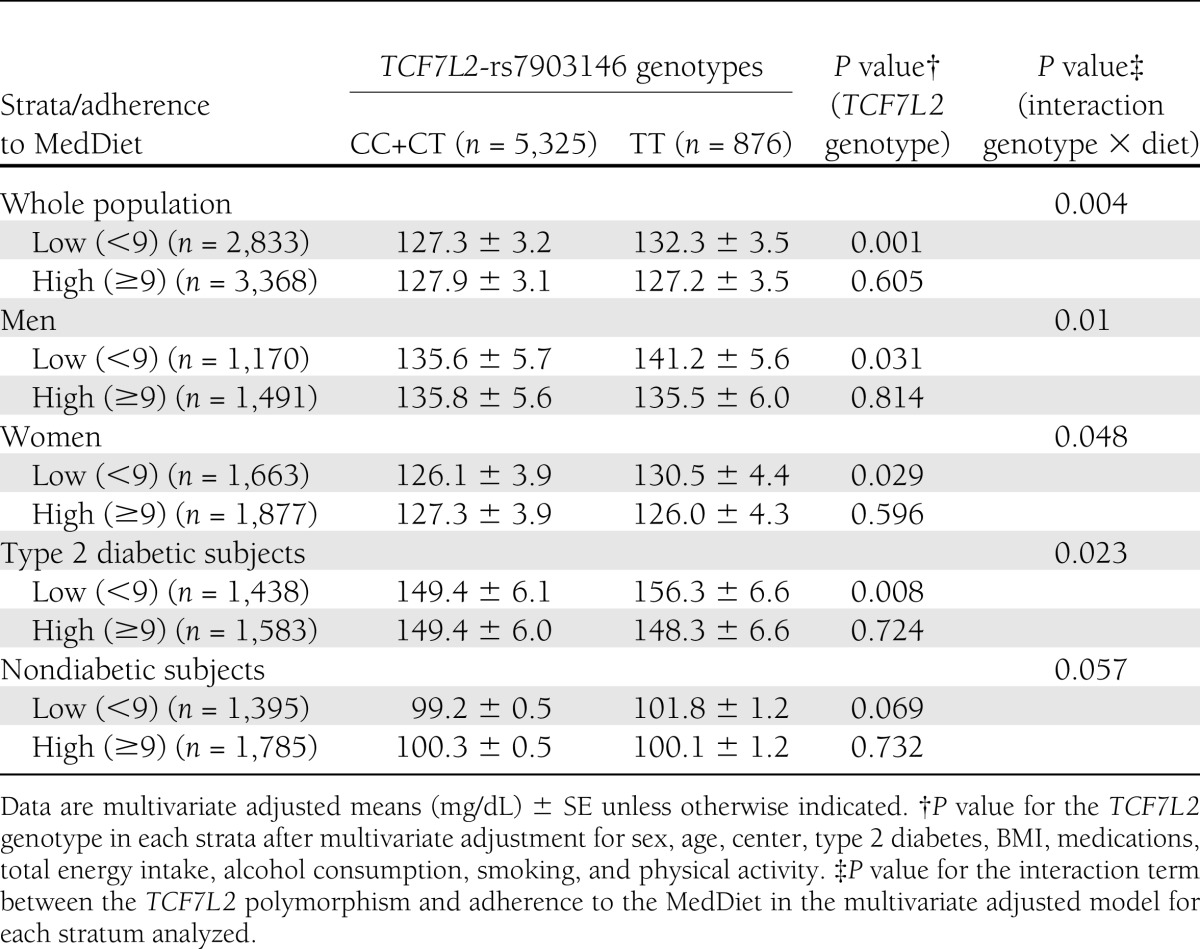
We detected a statistically significant interaction (P = 0.014) between the TCF7L2 polymorphism (three categories) and prerandomization adherence to the MedDiet as dichotomous in determining fasting glucose concentrations (Supplementary Fig. 1A). When adherence to MedDiet was low (below the sample mean, 9 points), we observed the predictable effects of the TCF7L2-rs7903146 polymorphism on fasting glucose concentrations (higher concentrations in TT individuals), reaching statistically significant results (P = 0.001) even after adjustment for type 2 diabetes, BMI, and other confounding variables. However, when adherence to MedDiet was high (≥9 points), no higher fasting glucose concentrations were observed in TT individuals (P = 0.282). As the effects of this interaction were mainly observed for TT individuals, we analyzed them in comparison with CC+CT in a recessive model, and a more statistically significant interaction term was obtained (P = 0.004). This interaction effect (as recessive) was also statistically significant on considering the score of adherence to MedDiet as a continuous variable from 0 to 14 (P interaction: 0.033) (Supplementary Fig. 1B). In a sensitivity analysis, we also studied the homogeneity of this interaction in different strata (Table 2). By sex, the interaction effect was statistically significant in both men and women. When we stratified the analysis according to diabetes status, the interaction effect was higher and clearly significant for type 2 diabetes subjects (P interaction: 0.023). In nondiabetic subjects, although a similar trend was observed, the interaction term was borderline significant (P = 0.057). However, the test of heterogeneity for the interaction among the polymorphism, MedDiet, and type 2 diabetes was not statistically significant (P = 0.348).
Table 2.
Interaction between the TCF7L2 polymorphism (recessive model) and prerandomization adherence to the MedDiet in determining fasting plasma glucose concentrations
We also analyzed the gene–diet interaction of other dietary variables (GL, GI, total fat, saturated fat, fiber, carbohydrates, and proteins) on fasting glucose at baseline and for neither of them did we find statistically significant interactions (not shown).
Interaction between prerandomization adherence to the MedDiet and the TCF7L2-rs7903146 polymorphism on plasma lipid concentrations
Using the same recessive interaction model, we found statistically significant gene–diet interactions (Supplementary Table 3) in determining total cholesterol, LDL-C, and triglycerides (P interaction: 0.005, 0.003, and 0.046, respectively). When adherence to MedDiet was low, TT individuals presented higher concentrations of total cholesterol, LDL-C, and triglycerides than CC+CT subjects. However, when adherence was high, these effects were not observed in TT individuals, and plasma concentrations of these parameters did not differ between genotypes. No significant interaction was detected for HDL-C.
Association between the TCF7L2-rs7903146 polymorphism and incidence of cardiovascular events after 4.8 years of follow-up: modulation by prerandomization adherence to the MedDiet
After a median follow-up of 4.8 years (interquartile range 2.8–5.8 years), 262 major cardiovascular events occurred among the 7,018 participants analyzed (30,359 person-years of observation). Of these, 130 were strokes, 98 were myocardial infarctions, and the others were cardiovascular deaths. In the whole population, we did not observe statistically significant associations between the TCF7L2-rs7903146 polymorphism and any cardiovascular event (P = 0.450 for total cardiovascular events, P = 0.170 for stroke, and P = 0.849 for myocardial infarction). HRs (95% CI) for TT subjects compared with CC homozygotes were 1.22 (0.85–1.75) for total cardiovascular events and 1.55 (0.95–2.53) for stroke incidence in a model adjusted for sex, age, center, type 2 diabetes, and dietary intervention group. Further adjustment for other covariates did not change the significance of results. In the stratified analysis by type 2 diabetes, we observed higher HRs in subjects with type 2 diabetes, but the results did not reach statistical significance.
On analyzing total cardiovascular events by levels of prerandomization adherence to the MedDiet, the risk associated with the TT genotype compared with CC individuals tended to be higher in the lower stratum (<9 points) of adherence, but did not reach statistical significance (Supplementary Table 4). Moreover, on considering stroke incidence, we obtained statistically significant results (Supplementary Table 4). When prerandomization adherence to MedDiet was low, TT subjects presented higher risk of stroke than CC homozygotes (HR 2.44 [95% CI 1.26–4.72] in the adjusted model including diabetes). No higher risk was found when adherence to MedDiet was high (HR 0.99 [95% CI 0.44–2.22] in the adjusted model including diabetes). No modification of the effect was detected for myocardial infarction (not shown).
Effect of the intervention with MedDiet on the association between the TCF7L2-rs7903146 polymorphism and incidence of cardiovascular events after 4.8-year postrandomization follow-up
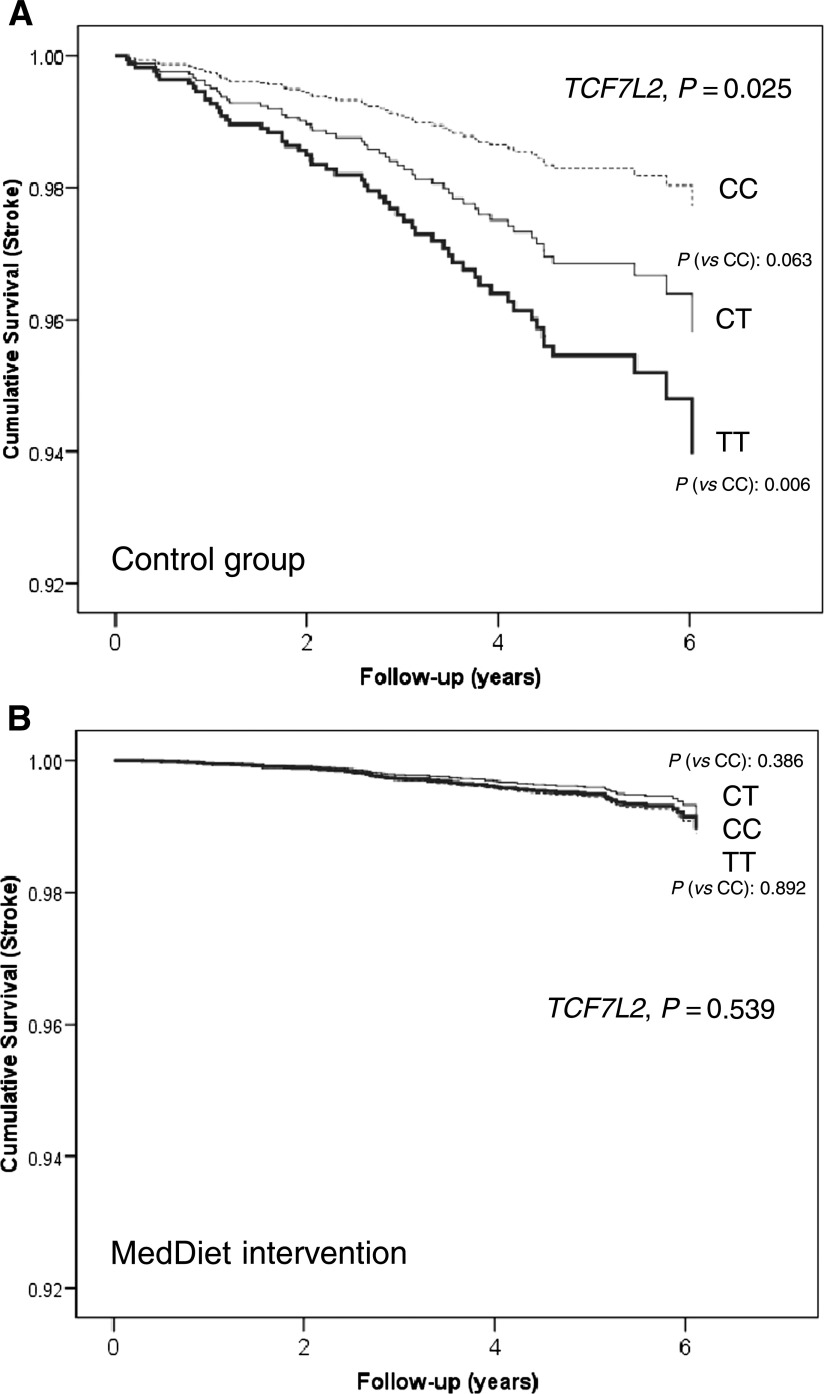
The most important results of the current study, as they came from a randomized trial and have a higher level of evidence, were obtained when considering the intervention with MedDiet (Table 3). Changes in dietary intake by intervention groups in the PREDIMED study have been widely detailed in our previous work (22). After a mean of 4.8 years of follow-up, we observed a significantly higher incidence of stroke in TT subjects in the control group (HR 3.06 [95% CI 1.43–6.59] in the adjusted model including diabetes) compared with CC homozygotes, but no significantly higher risks were observed in the MedDiet intervention groups either when grouped together (HR 1.02 [95% CI 0.52–1.99] for TT compared with CC) or considered separately (HR 1.13 [95% CI 0.49–2.64] in the MedDiet + EVOO and HR 0.89 [95% CI 0.26–2.99] in the MedDiet + nuts). Although we did not observe statistically significant differences between CT and CC individuals in determining stroke risk in the control group (P = 0.063), it should be noted that the CT group is intermediate in terms of the magnitude of risk. This trend toward a gene-dosage effect contributes to increasing the causality of our stroke-related findings. Figure 1 shows cumulative stroke free-survival per TCF7L2-rs7903146 genotypes in the control group (Fig. 1A) and the MedDiet intervention groups (Fig. 1B).
Table 3.
Incidence rates and HRs for total cardiovascular events and stroke stratified by the TCF7L2-rs7903146 polymorphism and the dietary intervention group after a median of 4.8 years of follow-up (multivariate adjusted models)
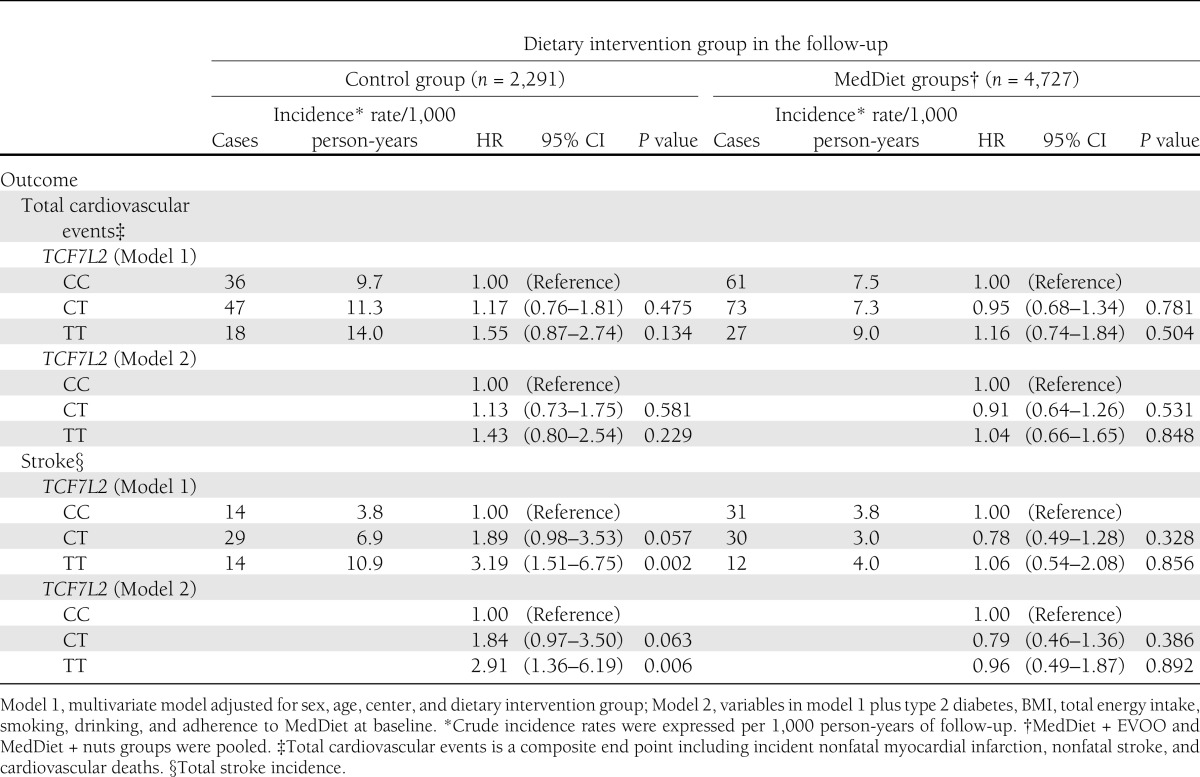
Figure 1.
Cumulative stroke free-survival by TCF7L2-rs7903146 genotypes in the control group (A) (n = 2,291) and in the MedDiet intervention groups (B) (n = 4,827). Cox regression models with outcome of stroke and the TCF7L2-rs7903146 polymorphism (CC, CT, and TT) adjusted by sex, age, center, type 2 diabetes, BMI, intervention group, alcohol, smoking, total energy intake, and adherence to the MedDiet at baseline. The P values for the TCF7L2 polymorphism and for the corresponding genotypes (CT vs. CC or TT vs. CC) were obtained in the multivariable adjusted models.
CONCLUSIONS
In this study undertaken on a large sample of high-cardiovascular-risk subjects, we found, consistent with previous studies (1–5,10), that the TCF7L2-rs7903146 polymorphism is a strong genetic determinant of type 2 diabetes risk and fasting glucose concentrations, TT individuals being those who presented a higher prevalence of type 2 diabetes and higher fasting glucose. In this study, however, we have described for the first time that prerandomization adherence to the MedDiet is capable of modulating the effects of the TCF7L2-rs7903146 polymorphism on fasting glucose concentrations, so that a higher adherence to the MedDiet attenuates the genetic increase of fasting glucose concentrations in TT individuals. We have consistently observed this effect in the whole population and in both men and women. Moreover, and more important, we have described for the first time that dietary intervention with a randomly assigned MedDiet may modulate the association of the TCF7L2-rs7903146 polymorphism with stroke incidence. Although several previous studies have analyzed the association between TCF7L2 polymorphisms and cardiovascular risk, the results are controversial (6–9,40). In the first report of the Atherosclerosis Risk in Communities (ARIC) study (6), TCF7L2 polymorphisms were not significantly associated with incident coronary heart disease, ischemic stroke, or cardiovascular disease in the whole cohort, although greater risk was found in white patients with diabetes (HR 1.21; P = 0.04). Some years later, a second reanalysis of the ARIC study (8) reported a higher risk of coronary heart disease among lean TT individuals (HR 1.42 [95% CI 1.03–1.97]). Muendlein et al. (40), using a population of Austrian patients undergoing coronary angiography, did report a higher risk of coronary atherosclerosis associated with the 7903146T allele for the whole population (odds ratio 1.29 [95% CI 1.09–1.53]), but, in the stratified analysis by diabetes status, they found that this association was strong in type 2 diabetes patients but not in nondiabetic subjects. Conversely, Sousa et al. (7) found in Brazilian patients that the 7903146T allele was associated with a higher prevalence and severity of coronary atherosclerosis in nondiabetic patients. These contradictory results may be due to either the different demographic and clinical characteristics of the patients included in each study or to the contribution of interactions with different environmental factors.
In our study, although we did not find any significant association of the TCF7L2-rs7903146 polymorphism with cardiovascular events on the population as a whole, we did find a very important modulation by the MedDiet on stroke incidence. TT individuals with a lower prerandomization adherence to MedDiet presented a statistically significant higher stroke risk than CC individuals. More important is that, despite this starting point, the intervention with MedDiet over a median of 4.8 years follow-up had a greater influence on stroke. Hence, TT individuals assigned to the control group presented a higher stroke incidence than CC individuals. However, stroke incidence was not greater in TT individuals in the MedDiet intervention groups, so reversing the genetic susceptibility conferred by the TCF7L2-rs7903146 polymorphism. These results are especially important given that the allocation to the MedDiet intervention was randomly assigned. No previous study has analyzed the dietary modulation of the TCF7L2-rs7903146 polymorphism on cardiovascular events, so more studies are required to confirm our findings. We do not know the mechanisms by which this modulation takes place, but the results obtained in our study do show a significant gene–diet interaction between the rs7903146 polymorphism and prerandomization adherence to the MedDiet in determining fasting glucose and plasma lipids, so that higher adherence results in a lower concentration of these cardiovascular risk factors in TT individuals compared with that which they would have with a lower adherence to the MedDiet. The association of the TCF7L2- rs7903146 polymorphism with plasma lipids is controversial, and we found great variability in results depending on the different populations analyzed (26–30), suggesting a possible modulation of this association by diet. Although no previous study has analyzed the influence of the MedDiet on this association, some gene–diet interactions have indeed been described between TCF7L2 polymorphisms and several macronutrients in determining plasma lipids; e.g., with dietary polyunsaturated fatty acids in determining fasting VLDL concentrations and postprandial triglyceride-rich lipoproteins in the Genetics of Lipid-Lowering Drugs and Diet Network (GOLDN) study (31) and with saturated fat on the metabolic-syndrome related variables in the LIPGENE study (29). Our findings, however, go further as we have found an interaction with the whole dietary pattern instead of individual components.
Considering the gene–diet interaction with MedDiet that we have found on glycemia and lipids, lower plasma concentrations of these atherogenic factors would lead over time to lower stroke incidence in TT subjects on a MedDiet than in those who are not. The modulation of stroke incidence by MedDiet is observed equally in the MedDiet + EVOO and in the MedDiet + nuts intervention groups, so that our results suggest once again that it is the overall MedDiet pattern rather than specific foods that contribute to not increasing stroke risk in TT individuals. Although we also have found that TT individuals randomly assigned to the control group had a higher incidence of total cardiovascular events, our results did not reach the statistical significance. Taking into account that we have reported (22) a higher effect of the intervention with MedDiet on reducing stroke incidence than myocardial infarction, the results obtained in our work for the TCF7L2-rs7903146 polymorphism are in line with this observation. The major strength of our study is the large sample size in a long-term nutritional intervention randomized trial with MedDiet, which presents the highest level of evidence in nutritional studies. However, the interactive findings on stroke risk after intervention with MedDiet rest on relatively few stroke cases. Despite this limitation, the fact that the results obtained, when considering adherence to the MedDiet at baseline go in the same direction, strengthens this gene–diet interaction.
In conclusion, we have described for the first time that the association between the TT genotype and fasting glucose is modulated by adherence to the MedDiet. This interaction occurs not only for fasting glucose but also for lipids. A greater prerandomization adherence to MedDiet leads to a reduction in fasting glucose, total cholesterol, LDL-C, and triglycerides in TT individuals who have high genetic susceptibility to increased levels compared with other genotypes. Importantly, we observed that intervention with a randomly assigned MedDiet reduced the risk of stroke in TT individuals. These results, based on a dietary intervention study, support the benefits of a MedDiet, especially for genetically susceptible individuals, and emphasize the importance of studying entire dietary patterns rather than individual components.
Supplementary Material
Acknowledgments
This study was funded by the Spanish Ministry of Health (Instituto de Salud Carlos III) and the Ministry of Economy and Innovation (projects PI051839, PI070240, PI1001407, G03/140, CIBER 06/03, RD06/0045, PI07-0954, CNIC-06, PI11/02505, SAF2009-12304, and AGL2010-22319-C03-03), Fondo Europeo de Desarrollo Regional, contracts 53-K06-5-10 and 58-1950-9-001 from the U.S. Department of Agriculture Research Service, and the Generalitat Valenciana (AP111/10, AP-042/11, BEST11-263, BEST/2011/261, GVACOMP2011-151, ACOMP/2011/145, ACOMP/2012/190, and ACOMP/2013/159). J.S.-S. is a nonpaid member of the Scientific Advisory Board of the International Nut Council. E.R. is a nonpaid member of the California Walnut Commission Scientific Advisory Committee.
No potential conflicts of interest relevant to this article were reported.
None of the funding sources played a role in the design, collection, analysis, or interpretation of the data or in the decision to submit the manuscript for publication.
D.C. conceived the study concept and design, obtained funding, acquired data, analyzed and interpreted data, wrote the manuscript, and reviewed and edited the manuscript. P.C. performed the experiments, acquired data, and reviewed and edited the manuscript. J.V.S. conceived the study concept, acquired data, analyzed and interpreted data, and reviewed and edited the manuscript. R.E. conceived the study concept and design, obtained funding, acquired data, analyzed and interpreted data, and reviewed the manuscript. J.R.-S. and M.A.M. acquired data and reviewed the manuscript. M.A.M.-G. conceived the study concept and design, obtained funding, and reviewed and edited the manuscript. J.S.-S., M.I.C., F.A., J.L., L.S.-M., M.F., and E.G.-G. conceived the study concept and design, obtained funding, and reviewed the manuscript. O.C. analyzed and interpreted data and reviewed and edited the manuscript. V.R.-G. obtained funding and reviewed the manuscript. J.W. obtained data and reviewed the manuscript. X.P. conceived the study concept and design and reviewed the manuscript. C.O.-A. performed the experiments, acquired data, and reviewed the manuscript. J.A.M. reviewed the manuscript. J.I.G. interpreted data and reviewed and edited the manuscript. E.R. and J.M.O. conceived the study concept and design, obtained funding, interpreted data, and reviewed and edited the manuscript. D.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the participants for the enthusiastic collaboration, the PREDIMED personnel for excellent assistance, and the personnel of all affiliated primary care centers.
Footnotes
Clinical trial reg. no. ISRCTN35739639, www.isrctn.org.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-0955/-/DC1.
References
- 1.Grant SF, Thorleifsson G, Reynisdottir I, et al. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 2006;38:320–323 [DOI] [PubMed] [Google Scholar]
- 2.Florez JC, Jablonski KA, Bayley N, et al. Diabetes Prevention Program Research Group TCF7L2 polymorphisms and progression to diabetes in the Diabetes Prevention Program. N Engl J Med 2006;355:241–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tong Y, Lin Y, Zhang Y, et al. Association between TCF7L2 gene polymorphisms and susceptibility to type 2 diabetes mellitus: a large Human Genome Epidemiology (HuGE) review and meta-analysis. BMC Med Genet 2009;10:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Voight BF, Scott LJ, Steinthorsdottir V, et al. MAGIC investigators. GIANT Consortium Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nat Genet 2010;42:579–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng S, Zhu Y, Lü B, Xu F, Li X, Lai M. TCF7L2 gene polymorphisms and type 2 diabetes risk: a comprehensive and updated meta-analysis involving 121,174 subjects. Mutagenesis 2013;28:25–37 [DOI] [PubMed] [Google Scholar]
- 6.Bielinski SJ, Pankow JS, Folsom AR, North KE, Boerwinkle E. TCF7L2 single nucleotide polymorphisms, cardiovascular disease and all-cause mortality: the Atherosclerosis Risk in Communities (ARIC) study. Diabetologia 2008;51:968–970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sousa AG, Marquezine GF, Lemos PA, et al. TCF7L2 polymorphism rs7903146 is associated with coronary artery disease severity and mortality. PLoS ONE 2009;4:e7697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kucharska-Newton AM, Monda KL, Bielinski SJ, et al. Role of BMI in the association of the TCF7L2 rs7903146 variant with coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) study. J Obes 2010;2010:651903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winter Y, Back T, Scherag A, et al. Evaluation of the obesity genes FTO and MC4R and the type 2 diabetes mellitus gene TCF7L2 for contribution to stroke risk: the Mannheim-Heidelberg Stroke study. Obes Facts 2011;4:290–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornelis MC, Hu FB. Gene-environment interactions in the development of type 2 diabetes: recent progress and continuing challenges. Annu Rev Nutr 2012;32:245–259 [DOI] [PubMed] [Google Scholar]
- 11.Jin T, Liu L. The Wnt signaling pathway effector TCF7L2 and type 2 diabetes mellitus. Mol Endocrinol 2008;22:2383–2392 [DOI] [PubMed] [Google Scholar]
- 12.Ip W, Shao W, Chiang YT, Jin T. The Wnt signaling pathway effector TCF7L2 is upregulated by insulin and represses hepatic gluconeogenesis. Am J Physiol Endocrinol Metab 2012;303:E1166–E1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grant SF. Understanding the elusive mechanism of action of TCF7L2 in metabolism. Diabetes 2012;61:2657–2658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyssenko V, Lupi R, Marchetti P, et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 2007;117:2155–2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Norton L, Fourcaudot M, Abdul-Ghani MA, et al. Chromatin occupancy of transcription factor 7-like 2 (TCF7L2) and its role in hepatic glucose metabolism. Diabetologia 2011;54:3132–3142 [DOI] [PubMed] [Google Scholar]
- 16.Savic D, Ye H, Aneas I, Park SY, Bell GI, Nobrega MA. Alterations in TCF7L2 expression define its role as a key regulator of glucose metabolism. Genome Res 2011;21:1417–1425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shao W, Wang D, Chiang YT, et al. The Wnt signaling pathway effector TCF7L2 controls gut and brain proglucagon gene expression and glucose homeostasis. Diabetes 2013;62:789–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmer ND, Hester JM, An SS, et al. Resequencing and analysis of variation in the TCF7L2 gene in African Americans suggests that SNP rs7903146 is the causal diabetes susceptibility variant. Diabetes 2011;60:662–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Helgason A, Pálsson S, Thorleifsson G, et al. Refining the impact of TCF7L2 gene variants on type 2 diabetes and adaptive evolution. Nat Genet 2007;39:218–225 [DOI] [PubMed] [Google Scholar]
- 20.Guinan KJ. Worldwide distribution of type II diabetes-associated TCF7L2 SNPs: evidence for stratification in Europe. Biochem Genet 2012;50:159–179 [DOI] [PubMed] [Google Scholar]
- 21.Salas-Salvadó J, Bulló M, Babio N, et al. PREDIMED Study Investigators Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011;34:14–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Estruch R, Ros E, Salas-Salvadó J, et al. PREDIMED Study Investigators Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–129023432189 [Google Scholar]
- 23.Cornelis MC, Qi L, Kraft P, Hu FB. TCF7L2, dietary carbohydrate, and risk of type 2 diabetes in US women. Am J Clin Nutr 2009;89:1256–1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher E, Boeing H, Fritsche A, Doering F, Joost HG, Schulze MB. Whole-grain consumption and transcription factor-7-like 2 (TCF7L2) rs7903146: gene-diet interaction in modulating type 2 diabetes risk. Br J Nutr 2009;101:478–481 [DOI] [PubMed] [Google Scholar]
- 25.Hindy G, Sonestedt E, Ericson U, et al. Role of TCF7L2 risk variant and dietary fibre intake on incident type 2 diabetes. Diabetologia 2012;55:2646–2654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Melzer D, Murray A, Hurst AJ, et al. Effects of the diabetes linked TCF7L2 polymorphism in a representative older population. BMC Med 2006;4:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanghera DK, Nath SK, Ortega L, et al. TCF7L2 polymorphisms are associated with type 2 diabetes in Khatri Sikhs from North India: genetic variation affects lipid levels. Ann Hum Genet 2008;72:499–509 [DOI] [PubMed] [Google Scholar]
- 28.Perez-Martinez P, Perez-Caballero AI, Garcia-Rios A, et al. Effects of rs7903146 variation in the Tcf7l2 gene in the lipid metabolism of three different populations. PLoS ONE 2012;7:e43390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillips CM, Goumidi L, Bertrais S, et al. Dietary saturated fat, gender and genetic variation at the TCF7L2 locus predict the development of metabolic syndrome. J Nutr Biochem 2012;23:239–244 [DOI] [PubMed] [Google Scholar]
- 30.Delgado-Lista J, Perez-Martinez P, García-Rios A, et al. Pleiotropic effects of TCF7L2 gene variants and its modulation in the metabolic syndrome: from the LIPGENE study. Atherosclerosis 2011;214:110–116 [DOI] [PubMed] [Google Scholar]
- 31.Warodomwichit D, Arnett DK, Kabagambe EK, et al. Polyunsaturated fatty acids modulate the effect of TCF7L2 gene variants on postprandial lipemia. J Nutr 2009;139:439–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fisher E, Meidtner K, Angquist L, et al. Influence of dietary protein intake and glycemic index on the association between TCF7L2 HapA and weight gain. Am J Clin Nutr 2012;95:1468–1476 [DOI] [PubMed] [Google Scholar]
- 33.Estruch R, Martínez-González MA, Corella D, et al. PREDIMED Study Investigators Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006;145:1–11 [DOI] [PubMed] [Google Scholar]
- 34.Martínez-González MA, Corella D, Salas-Salvadó J, et al. PREDIMED Study Investigators Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol 2012;41:377–385 [DOI] [PubMed] [Google Scholar]
- 35.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2008;31(Suppl. 1):S55–S60 [DOI] [PubMed] [Google Scholar]
- 36.Fernández-Ballart JD, Piñol JL, Zazpe I, et al. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr 2010;103:1808–1816 [DOI] [PubMed] [Google Scholar]
- 37.Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care 2008;31:2281–2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu S, Willett WC, Stampfer MJ, et al. A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr 2000;71:1455–1461 [DOI] [PubMed] [Google Scholar]
- 39.Schröder H, Fitó M, Estruch R, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011;141:1140–1145 [DOI] [PubMed] [Google Scholar]
- 40.Muendlein A, Saely CH, Geller-Rhomberg S, et al. Single nucleotide polymorphisms of TCF7L2 are linked to diabetic coronary atherosclerosis. PLoS ONE 2011;6:e17978. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.