Abstract
Background:
Our aim was to investigate if patients with suspected myocardial infarction (MI) and a new or presumed new left bundle branch block (nLBBB) were treated according to the ESC reperfusion guidelines and to compare them with patients having a previously known LBBB (oLBBB). Furthermore, we investigated the prevalence of ST-segment concordance in this population.
Methods:
Retrospective data was collected from the Swedeheart registry for patients admitted to the cardiac care unit at Örebro University Hospital with LBBB and suspected MI during 2009 and 2010. The patients were divided in two age groups; <80 or ≥80 years and analysed for LBBB chronicity (nLBBB or oLBBB), MI, and reperfusion treatment. We also compared our data with the national Swedeheart database for 2009.
Results:
A total of 99 patients fulfilled the inclusion criteria. A diagnosis of MI was significantly more common in the group ≥80 years compared to the group <80 years (53.8 vs. 25%, p=0.007). The rate of MI was similar in the groups with nLBBB and oLBBB (33 and 37% respectively, p=0.912). Of the 36 patients with a final diagnosis of MI, only eight (22%) had nLBBB. Reperfusion treatment, defined as an acute coronary angiography with or without intervention, was significantly more often performed in patients with nLBBB compared to patients with oLBBB (42 vs. 8%, p<0.001). The rate of MI and reperfusion treatment did not differ between our institution and the Swedish national data. ST-concordance was present in only two cases, one of which did not suffer an MI.
Conclusions:
The proportion of patients receiving reperfusion treatment was low, but higher in nLBBB, reflecting a partial adherence to the guidelines. We found no correlation between LBBB chronicity and MI. Furthermore, only a minority of the MIs occurred in patients with nLBBB. ST-concordance was found in only one of 36 MI cases, indicating lack of sensitivity for this test.
Keywords: Acute myocardial infarction, acute reperfusion treatment, branch block chronicity, bundle branch block, left bundle branch block, myocardial infarction
Introduction
Several studies have shown that the mortality in patients with myocardial infarction (MI) and left bundle branch block (LBBB) on admission electrocardiogram (ECG) is 2–3 times higher than in MI patients without LBBB.1–6 This can be explained, at least partially, by the fact that patients with LBBB are older and more often suffer from multivessel coronary artery disease, heart failure as well as other comorbidities.7–9 Additionally, patients with LBBB and suspected MI less often receive reperfusion treatment, probably due to their higher risk profile as well as diagnostic difficulties.8,10,11 In 1996, based on data from a large fibrinolysis trial, Sgarbossa et al.12 published criteria for detecting MI in patients with LBBB. A finding of ST-segment deviation concordant with the QRS complex was shown to have a very high specificity for MI. According to later reports, the sensitivity seems to be low, thus limiting the clinical usefulness of these criteria.13–17
A meta-analysis of trials comparing fibrinolytic therapy with placebo in patients with suspected MI showed a survival benefit in patients with either ST-segment elevation or bundle branch block (BBB) on admission ECG.18 These results were soon reflected in the international guidelines.19,20 In subsequent revised guidelines, published 2003 and 2004,21,22 the recommendation for reperfusion treatment in BBB was limited to patients with new or presumed new LBBB.
The purpose of this retrospective study was to evaluate the adherence to the European Society of Cardiology (ESC) reperfusion guidelines and to investigate the age and sex distribution, the rate of reperfusion treatment and MI diagnosis in patients with new or old LBBB (nLBBB or oLBBB) admitted to the cardiac care unit at the department of cardiology, Örebro University Hospital during 2009 and 2010. Furthermore we wanted to investigate the proportion of patients with ST-segment concordance.
Methods
Patient data was collected retrospectively from the local Swedeheart registry. Swedeheart (the Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) is a nationwide on-line registry covering acute and chronic ischaemic heart disease, as well as catheter-based or surgical coronary and valvular interventions. All Swedish hospitals with acute coronary care participate, as well as all hospitals with coronary interventions or cardiac surgery. For acute coronary care, 120 demographic, clinical and outcome variables are registered. (More information is available at http://www.ucr.uu.se/swedeheart/index.php/annual-report.) The registry data is monitored systematically and has shown a 96% agreement with chart data. All patients included in the registry are informed of their participation and the anonymity of the data.
We included all patients with a suspected myocardial infarction and LBBB on admission ECG. Patients transferred from other hospitals were excluded in order to avoid selection bias of patients identified as candidates for reperfusion therapy. Registry data was checked against hospital records for each patient. In accordance with the national Swedeheart annual report, we divided the patients in two age groups: <80 years and ≥80 years. For both groups we analysed the proportion of patients diagnosed with MI according to International Classification of Diseases codes I21–I23 and the proportion of patients given acute reperfusion treatment. The presence of LBBB on admission ECG, as well as chronicity and signs of ST-concordance was evaluated by one of the authors (VL) and ambiguous cases were classified by consensus among the authors. Finally, we compared the data from our hospital with the whole national database for 2009, with the exception of LBBB chronicity and ST-concordance, which are not registered in Swedeheart.
In accordance with the Swedeheart registry, we used the universal definition of myocardial infarction23 with a typical rise and/or fall in troponins in combination with relevant clinical symptoms or ECG changes. During the study period we used a troponin-I assay (Abbott Architect; Abbott Laboratories, Abbott Park, Illinois, USA) with a diagnostic threshold of 0.1 µg/l. In Swedeheart, acute reperfusion treatment is defined as fibrinolytic treatment or an acute coronary angiography, with or without intervention, in patients presenting within 12 hours from the initial symptoms of MI. In Sweden today, fibrinolytic treatment is given only at a few remote hospitals and not at all at our institution. The rationale for including coronary angiography without intervention in the definition of reperfusion treatment is that it reflects adherence to guidelines in the setting of ST-segment elevation or nLBBB, given the knowledge that not all patients with these ECG-changes actually have occlusive coronary artery disease. Since fibrinolytic treatment of MI is not practiced at our institution, we replaced the term ‘reperfusion treatment’ with ‘acute angiography’ (AA), including both patients with and without intervention.
In the Swedeheart registry, LBBB is defined as a QRS-duration >0.12 s, a wide monophasic R in leads I, V5, and V6 and absence of Q in V5 and V6. LBBB not known to be old was classified as nLBBB, whereas patients with a previous ECG in the database showing LBBB were classified as having oLBBB. ST-concordance was defined as ST-elevation ≥1 mm in leads with a positive QRS or ST-segment depression ≥1 mm in leads V1–V3.
For statistical analysis, the treatment variables were defined in dichotomous terms before analysis using Fishers Exact test and when possible χ2-test. To compare groups, t-test was performed, and when normality test failed, Mann–Whitney rank sum test. p-values <0.05 were considered significant. The software used was Sigma Stat version 3.5.
Results
The study included 99 patients with a mean age of 74.2 years. Table 1 shows demographic data in relation to the chronicity of LBBB. Patients with oLBBB significantly more often had previous MI, congestive heart failure and previous percutaneous coronary intervention. The sex distribution was almost equal. Female patients were slightly older, but this difference was not statistically significant. The proportion of patients with nLBBB was equal between the sexes, and there were no significant differences regarding AA or diagnosis of MI (Table 2).
Table 1.
Demographic data in relation to chronicity of LBBB.
| nLBBB (n=24) | oLBBB (n=75) | p | |
|---|---|---|---|
| Age (years) | 69.8 | 75.6 | 0.10 |
| Diabetes mellitus | 5 (21) | 23 (31) | 0.502 |
| Hypertension | 9 (37.5) | 26 (35) | 0.781 |
| History of smoking | 12 (50) | 33 (44) | 0.994 |
| Previous MI | 1 (4) | 47 (63) | <0.001 |
| Heart failure | 1 (4) | 24 (32) | 0.014 |
| Hyperlipidaemia | 8 (33) | 44 (59) | 0.054 |
| Previous stroke | 1 (4) | 12 (16) | 0.179 |
| Previous PCI | 1 (4) | 35 (47) | <0.001 |
| Previous CABG | 2 (8) | 16 (21) | 0.226 |
| Acute angiography | 10 (42) | 6 (8) | <0.001 |
| Diagnosis of MI | 8 (33) | 28 (37) | 0.912 |
Values are mean or n (%).
CABG, coronary artery bypass graft; MI, myocardial infarction; nLBBB, new left bundle branch block; oLBBB, old left bundle branch block; PCI, percutaneous coronary intervention.
Table 2.
Gender comparison.
| Male (n=54) | Female (n=45) | p | |
|---|---|---|---|
| Age (years) | 72.5±12.1 | 76.3±9.4 | 0.097 |
| nLBBB | 13 (24) | 11 (24) | 0.847 |
| Acute angiography | 10 (19) | 6 (13) | 0.672 |
| Diagnosis of MI | 23 (43) | 13 (29) | 0.339 |
Values are mean±SD or n (%).
MI, myocardial infarction; nLBBB, new left bundle branch block.
As shown in Table 3, the group <80 years comprised 60 patients and the group ≥80 years comprised 39 patients. The diagnosis of MI was significantly more common in the patient group ≥80 years than in the group <80 years (54 vs. 25 % respectively, p=0.007). In order to further explore the relationship between age and MI, we also dichotomized the study population at 70 and 60 years. In both cases, MI was more common in the older age group, although the difference was not significant at the cut-point of 60 years (proportion with MI: ≥70 years 45%; <70 years 18%, p=0.015; ≥60 years 39%, <60 years 18%, p=0.319).
Table 3.
Data from the local Swedeheart registry for LBBB (n=99), Örebro 2009–2010.
| <80 years (n=60) |
≥80 years (n=39) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| nLBBB 17 (28) |
oLBBB 43 (72) |
nLBBB 7 (18) |
oLBBB 32 (82) |
||||||||||||
| MI 7 (41) | No MI 10 (59) | MI 8 (19) | No MI 35 (81) | MI 1 (14) | No MI 6 (86) | MI 20 (62) | No MI 12 (38) | ||||||||
| AA | No AA | AA | No AA | AA | No AA | AA | No AA | AA | No AA | AA | No AA | AA | No AA | AA | No AA |
| 5(71) | 2(29) | 5(50) | 5(50) | 1(12) | 7(88) | 2(6) | 33(94) | 0 | 1 | 0 | 6 | 3(15) | 17(85) | 0 | 12 |
Values are n (%). MI was observed more often in patients ≥80 years compared to <80 years (p=0.007). In the older age group, MI was almost exclusively limited to oLBBB (p=0.035) whereas an opposite trend was observed in the younger group (p=0.099).
AA, acute angiography; MI, myocardial infarction; nLBBB, new left bundle branch block; oLBBB, old left bundle branch block.
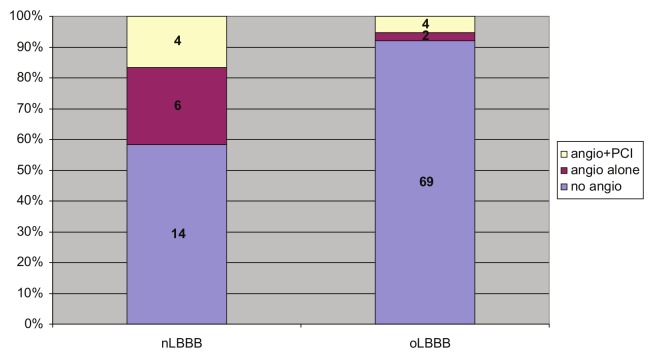
The diagnosis of MI was observed in eight of 24 patients with nLBBB and 28 of 75 patients oLBBB (33 vs. 37% respectively, p=0.912) (Figure 1). In the younger group, there was a trend towards MI being seen more frequently in nLBBB than in oLBBB (41 vs. 19%, p=0.099) (Figure 1). In patients ≥80 years, MI was diagnosed significantly more often in oLBBB than in nLBBB (62 vs. 17%, p=0.035) (Figure 1).
Figure 1.
Diagnosis of MI according to chronicity of LBBB and age. MI was observed in eight of 24 patients with nLBBB and 28 of 75 patients with oLBBB (33.3 vs. 37.3%, p=0.912). In patients <80 years, there was a trend towards MI being seen more frequently in nLBBB than in oLBBB (41 vs. 18%, p=0.099), whereas in patients ≥80 years, MI was seen significantly more often in oLBBB (p=0.035). MI was significantly more common in patients ≥80 years than in patients <80 (p=0.007). MI, myocardial infarction; nLBBB, new left bundle branch block; oLBBB, old left bundle branch block.
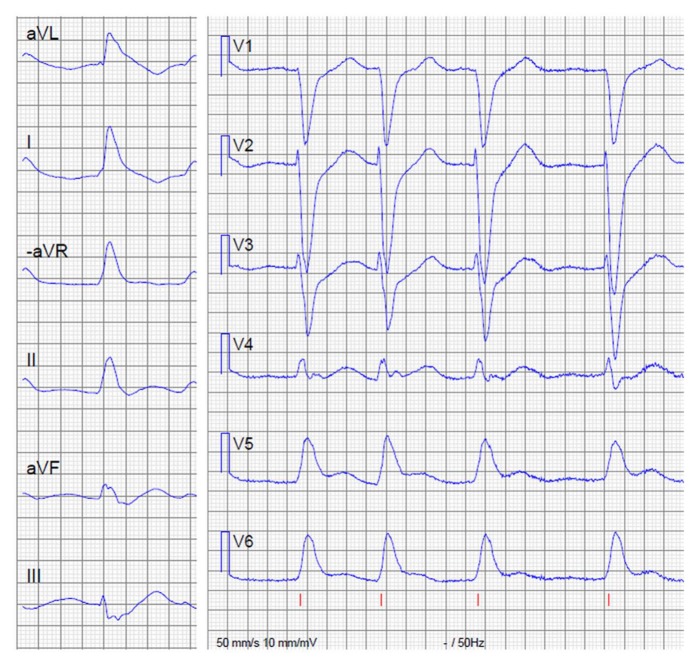
AA was performed significantly more often in patients with nLBBB than in patients with oLBBB (42 vs. 8% respectively, p<0.001) (Figure 2), and the difference was especially pronounced in the group <80 years (59 vs. 7% respectively, p<0.001) (Table 3). No difference in this regard was detected in patients ≥80 years, where the frequency of AA in general was low (three of 39 patients). Of the 16 patients undergoing AA, a coronary intervention was performed in eight cases (50%), all of which received a final diagnosis of MI. Among the eight patients undergoing angiography but no intervention, five patients had a normal coronary angiogram, whereas three patients had multivessel disease but no identifiable culprit lesion or coronary occlusion. In this group, only one patient was diagnosed with MI.
Figure 2.
Proportion of patients undergoing acute angiography with or without intervention, in relation to chronicity of LBBB. Absolute patient numbers are given in the diagram. AA was significantly more often performed in patients with nLBBB compared to patients with oLBBB (42 vs. 8%, p<0.001). Of 10 patients with nLBBB undergoing AA, only 4 had an MI treated with coronary intervention. nLBBB, new left bundle branch block; oLBBB, old left bundle branch block; PCI, percutaneous coronary intervention.
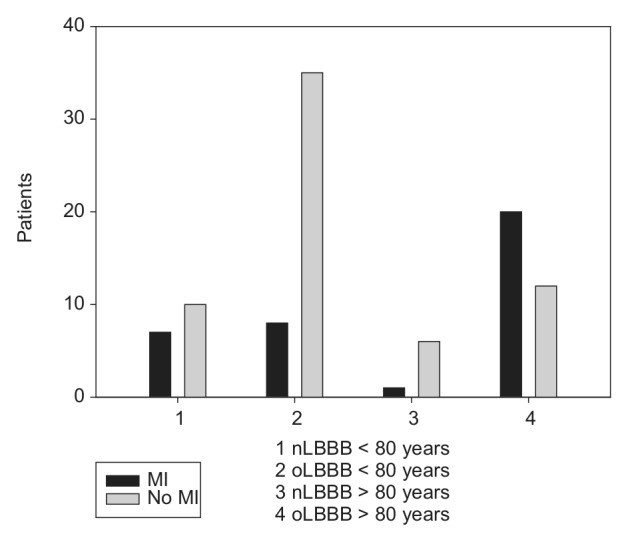
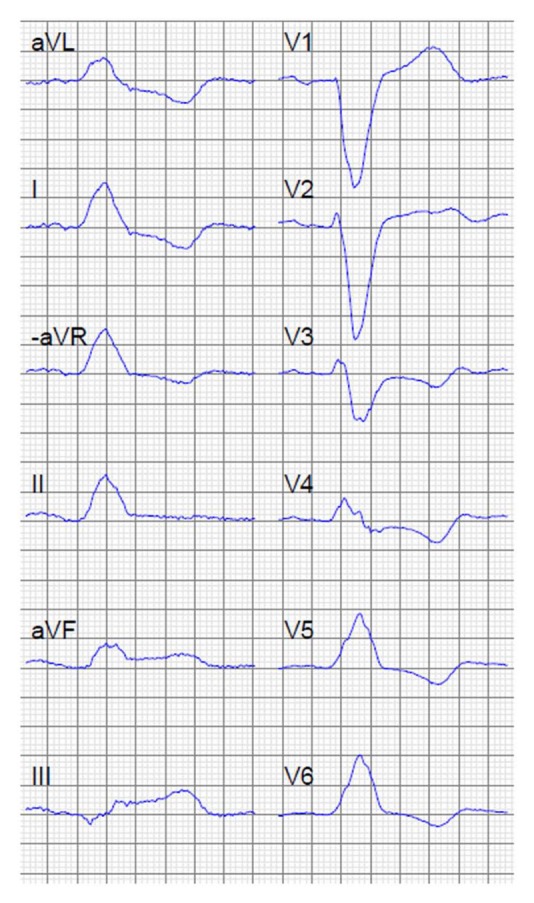
Two (2%) of the patients had ST-concordance on the admission ECG. One of them (Figure 3) underwent urgent coronary angiography and percutaneous coronary intervention for an occluded circumflex coronary artery. The other ECG (Figure 4) was somewhat atypical but the authors concurred that it fulfilled the criteria for ST-concordance. The patient had clinical and radiological signs of pneumonia and died after 9 hours. Coronary angiography was not performed, and troponin, sampled 7 hours after first symptoms, was negative. We conclude that this patient probably did not suffer from an acute MI.
Figure 3.
ECG showing ST-concordance in inferior leads. The patient had an occluded circumflex coronary artery.
Figure 4.
ECG showing ST-concordance in lateral precordial leads. The patient died 9 hours after admission and had negative troponin-I 7 hours after debut of symptoms. X-ray showed pneumonia.
During 2009, 3001 patients with LBBB were included in the national Swedeheart registry (Table 4). There were no significant differences regarding age distribution, rate of MI, or reperfusion treatment between the national database and our study population.
Table 4.
Data from the Swedeheart national database for LBBB (n=3001), 2009.
| <80 years (n=1692) |
≥80 years (n=1309) |
||||||
|---|---|---|---|---|---|---|---|
| MI 599 (35) | No MI 1093 (65) | MI 699 (53) | No MI 610 (47) | ||||
| RT | No RT | RT | No RT | RT | No RT | RT | No RT |
| 139 (23) | 460 (77) | 90 (8) | 1003(92) | 61 (9) | 638 (91) | 15 (2) | 595 (98) |
Values are n (%). Compared to our local database, there were no significant differences regarding proportion of patients ≥80 years, diagnosis of MI, or reperfusion treatment.
MI, myocardial infarction; nLBBB, new left bundle branch block; oLBBB, old left bundle branch block; RT, acute reperfusion treatment (fibrinolysis or coronary angiography±intervention).
Discussion
The overall proportion of patients with MI in the study population was 36%. This corresponds well with previously published data from cardiac care unit settings7–9 and with the Swedeheart database for 2009, where the proportion was 43% (Table 4). In prospective studies from emergency departments, i.e. in less selected populations, the rate of MI in patients with LBBB is even lower (6–29%).13,24 Furthermore, in the emergency department study by Chang et al.,24 the rate of MI did not differ between patients with LBBB and patients with other ECG findings. This raises the question whether LBBB is a sign of acute MI or rather a sign of underlying structural heart disease, including coronary heart disease and previous MI.25 Furthermore, the frequency of LBBB increases with age.26 We observed a higher frequency of MI in older patients. This is in accordance with previously published studies,1 as well as with the national Swedeheart database for 2009 (Table 4).
Of the 36 patients with a final diagnosis of MI, only eight (22%) had nLBBB (Figure 1). This frequency is lower than in studies from the 1970s27,28 but comparable to a recent report from Chang et al.24 This may reflect temporal changes in the MI population with increasing age and comorbidities. This issue is discussed at length in a recent review by Neeland et al.25
As mentioned earlier, the study aimed at evaluating to what degree we adhere to ESC guidelines regarding acute reperfusion therapy. In clinical practice, reperfusion therapy must be administered before the diagnosis of MI is confirmed biochemically. We therefore find it relevant to include the whole population in the analysis, regardless of final diagnosis. In the whole population, only 16% (16/99) underwent AA. In the group with nLBBB, the corresponding figure is 42% (10/24). If we focus on patients with nLBBB and a final diagnosis of MI, the rate of AA was 63% (5/8). The figures reflect at least a partial adherence to the guidelines and are comparable to previously published registry data7,29 as well as the Swedeheart database from 2009 (Table 4).
Seven (44%) of the 16 AA patients did not suffer an acute MI, the majority having a normal coronary angiogram. Five of the seven patients without MI had nLBBB. Only eight of the 16 acute coronary angiographies led to an intervention. This illustrates the issue of false-positive cath-lab activation, a problem that has been discussed in several recent publications.30,31
Although comparable to data from other centres, our rate of AA reflects a rather poor adherence to the present reperfusion guidelines. It is also much lower than in ST-segment elevation MI, where in our institution AA is performed in well over 95% of cases (unpublished data). There are probably many reasons for this. The patients’ older age and frequent comorbidities, often with contraindications to invasive or aggressive antithrombotic treatment, is probably the primary reason. We also hypothesize that diagnostic difficulties and the frequent false-positive cath-lab activations may create a form of clinical nihilism. This can only be overcome with more knowledge regarding acute diagnostic and therapeutic measures in LBBB. The optimal rate of reperfusion therapy in this population is difficult to ascertain. It is noteworthy that only 50% of the angiographies in our study showed a coronary occlusion warranting intervention. If fibrinolysis had been our reperfusion strategy, these patients would have been exposed to the bleeding risk but probably none of the benefits of reperfusion.
In this study, we did not evaluate the proportion of patients with severe comorbidities or contraindications to reperfusion therapy, but it is reasonable to assume that it is higher in patients with LBBB than in patients with ST-segment elevation. Neeland et al.25 have proposed an algorithm based on circulatory status, Sgarbossa criteria, bedside echocardiography, and serial biomarker testing. Prospective trials are badly needed to evaluate this and other diagnostic methods in this patient group.
We found no difference in the prevalence of MI between the group with nLBBB and the group with oLBBB. There were diverging trends in the two age groups, but the small sample size prevents further conclusions, and the finding warrants further studies in larger populations. The lack of correlation between chronicity of LBBB and MI has been shown in other studies, with larger populations than ours.13,24 As mentioned before, the guidelines originally advocated reperfusion therapy to all patients with BBB and a clinical suspicion of MI, based on the Fibrinolytic Therapy Trialists’ meta-analysis of trials on fibrinolytic therapy.18 For reasons that are unclear, and without stating scientific references, both the European21 and the American guidelines22 later limited their recommendations to patients with new, or presumed new, LBBB. A reason for this may have been the ambition to avoid giving fibrinolytic drugs to patients without occluded coronary vessels, but we can find no support in the literature for the notion that patients with nLBBB more often have acutely occluded coronary vessels than patients with oLBBB, or, for that matter, patients with right BBB (RBBB). This latter group was subject to a recent study by Widimsky et al.32 who showed that coronary occlusion was in fact more common in RBBB than in LBBB, the mortality was higher, and in almost half of the RBBB-cases concomitant ST-segment elevation was absent. In this context, we find it noteworthy that a majority (78%) of the MI patients in our study had an old LBBB. Strict adherence to guidelines that advocate reperfusion therapy only in nLBBB will leave this group untreated. The patients with oLBBB in our study more often had previous MI and heart failure, as well as previous revascularization. This probably reflects more severe coronary disease. There may be differences between oLBBB and nLBBB regarding the type and size of MI, as well as the potential benefit of reperfusion therapy. Further studies are needed to clarify this.
There is a great need for new tools to identify patients with LBBB and suspected MI who actually suffer from a coronary occlusion and will benefit from acute reperfusion therapy. Much hope was placed in the previously mentioned Sgarbossa criteria.12 We found only two patients (2%) with ST-concordance on the admission ECG, and only one of them had an MI. Our findings are well in accordance with other studies13–17 showing a lack of sensitivity for these criteria.
Our study is limited by its small size; it is retrospective and based on registry data. Starting from April 2012, the Swedeheart registry includes data on the chronicity of LBBB. This will enable us to expand the current analysis to a large number of patients and we plan to report these data in the future.
In conclusion, we found no correlation between LBBB chronicity and MI and only a minority of the MIs occurred in patients with nLBBB. The rate of acute reperfusion treatment was low, reflecting diagnostic difficulties and patient comorbidities. ST-concordance does not seem to be the tool that will solve the diagnostic problems. If our data are confirmed in larger studies, the present reperfusion guidelines regarding LBBB may have to be re-evaluated.
Acknowledgments
The authors would like to thank Scott Montgomery for his help with the manuscript.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Shlipak MG, Go AS, Frederick PD, et al. Treatment and outcomes of left bundle-branch block patients with myocardial infarction who present without chest pain. National Registry of Myocardial Infarction 2 Investigators. J Am Coll Cardiol 2000; 36: 706–712 [DOI] [PubMed] [Google Scholar]
- 2. Wong CK, French JK, Aylward PE, et al. Patients with prolonged ischemic chest pain and presumed-new left bundle branch block have heterogeneous outcomes depending on the presence of ST-segment changes. J Am Coll Cardiol 2005; 46: 29–38 [DOI] [PubMed] [Google Scholar]
- 3. Dissmann R, Kamke W, Reibis R, et al. Prognostic impact of left bundle-branch block in the early stable phase after acute myocardial infarction. Int J Cardiol 2008; 130: 438–443 [DOI] [PubMed] [Google Scholar]
- 4. Wong CK, Stewart RA, Gao W, et al. Prognostic differences between different types of bundle branch block during the early phase of acute myocardial infarction: insights from the Hirulog and Early Reperfusion or Occlusion (HERO)-2 trial. Eur Heart J 2006; 27: 21–28 [DOI] [PubMed] [Google Scholar]
- 5. Brilakis ES, Wright RS, Kopecky SL, et al. Bundle branch block as a predictor of long-term survival after acute myocardial infarction. Am J Cardiol 2001; 88: 205–209 [DOI] [PubMed] [Google Scholar]
- 6. Di Chiara A, Marinigh R. [Bundle-branch block in the course of myocardial infarction. Recent advances]. Recenti Prog Med 2006; 97: 401–404 [PubMed] [Google Scholar]
- 7. Stenestrand U, Tabrizi F, Lindback J, et al. Comorbidity and myocardial dysfunction are the main explanations for the higher 1-year mortality in acute myocardial infarction with left bundle-branch block. Circulation 2004; 110: 1896–1902 [DOI] [PubMed] [Google Scholar]
- 8. Moreno R, Garcia E, Lopez de, Sa E, et al. Implications of left bundle branch block in acute myocardial infarction treated with primary angioplasty. Am J Cardiol 2002; 90: 401–403 [DOI] [PubMed] [Google Scholar]
- 9. Guerrero M, Harjai K, Stone GW, et al. Comparison of the prognostic effect of left versus right versus no bundle branch block on presenting electrocardiogram in acute myocardial infarction patients treated with primary angioplasty in the primary angioplasty in myocardial infarction trials. Am J Cardiol 2005; 96: 482–488 [DOI] [PubMed] [Google Scholar]
- 10. Yeo KK, Li S, Amsterdam EA, et al. Comparison of clinical characteristics, treatments and outcomes of patients with ST-elevation acute myocardial infarction with versus without new or presumed new left bundle branch block (from NCDR(R)). Am J Cardiol 2012; 109: 497–501 [DOI] [PubMed] [Google Scholar]
- 11. Lopes RD, Siha H, Fu Y, et al. Diagnosing acute myocardial infarction in patients with left bundle branch block. Am J Cardiol 2011; 108: 782–788 [DOI] [PubMed] [Google Scholar]
- 12. Sgarbossa EB, Pinski SL, Barbagelata A, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. N Engl J Med 1996; 334: 481–487 [DOI] [PubMed] [Google Scholar]
- 13. Kontos MC, Aziz HA, Chau VQ, et al. Outcomes in patients with chronicity of left bundle-branch block with possible acute myocardial infarction. Am Heart J 2011; 161: 698–704 [DOI] [PubMed] [Google Scholar]
- 14. Kontos MC, McQueen RH, Jesse RL, et al. Can myocardial infarction be rapidly identified in emergency department patients who have left bundle-branch block? Ann Emerg Med 2001; 37: 431–438 [DOI] [PubMed] [Google Scholar]
- 15. Gunnarsson G, Eriksson P, Dellborg M. ECG criteria in diagnosis of acute myocardial infarction in the presence of left bundle branch block. Int J Cardiol 2001; 78: 167–174 [DOI] [PubMed] [Google Scholar]
- 16. Li SF, Walden PL, Marcilla O, et al. Electrocardiographic diagnosis of myocardial infarction in patients with left bundle branch block. Ann Emerg Med 2000; 36: 561–565 [DOI] [PubMed] [Google Scholar]
- 17. Jain S, Ting HT, Bell M, et al. Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol 2011; 107: 1111–1116 [DOI] [PubMed] [Google Scholar]
- 18.Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group Lancet 1994; 343: 311–322 [PubMed] [Google Scholar]
- 19.Acute myocardial infarction: pre-hospital and in-hospital management. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 1996; 17: 43–63 [DOI] [PubMed] [Google Scholar]
- 20. Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA Guidelines for the Management of Patients With Acute Myocardial Infarction: Executive Summary and Recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 1999; 100: 1016–1030 [DOI] [PubMed] [Google Scholar]
- 21. Van de Werf F, Ardissino D, Betriu A, et al. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 2003; 24: 28–66 [DOI] [PubMed] [Google Scholar]
- 22. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol 2004; 44: E1–E211 [DOI] [PubMed] [Google Scholar]
- 23. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation 2007; 116: 2634–2653 [DOI] [PubMed] [Google Scholar]
- 24. Chang AM, Shofer FS, Tabas JA, et al. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. Am J Emerg Med 2009; 27: 916–921 [DOI] [PubMed] [Google Scholar]
- 25. Neeland IJ, Kontos MC, de Lemos JA. Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J Am Coll Cardiol 2012; 60: 96–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eriksson P, Hansson PO, Eriksson H, et al. Bundle-branch block in a general male population: the study of men born 1913. Circulation 1998; 98: 2494–2500 [DOI] [PubMed] [Google Scholar]
- 27. Hindman MC, Wagner GS, JaRo M, et al. The clinical significance of bundle branch block complicating acute myocardial infarction. 1. Clinical characteristics, hospital mortality, and one-year follow-up. Circulation 1978; 58: 679–688 [DOI] [PubMed] [Google Scholar]
- 28. Gann D, Balachandran PK, Sherif NE, et al. Prognostic significance of chronic versus acute bundle branch block in acute myocardial infarction. Chest 1975; 67: 298–303 [DOI] [PubMed] [Google Scholar]
- 29. Go AS, Barron HV, Rundle AC, et al. Bundle-branch block and in-hospital mortality in acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. Ann Intern Med 1998; 129: 690–697 [DOI] [PubMed] [Google Scholar]
- 30. Larson DM, Menssen KM, Sharkey SW, et al. ‘False-positive’ cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA 2007; 298: 2754–2760 [DOI] [PubMed] [Google Scholar]
- 31. Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J 2010; 160: 995–1003, 1003 e1001–1008. [DOI] [PubMed] [Google Scholar]
- 32. Widimsky P, Rohac F, Stasek J, et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? Eur Heart J 2012; 33: 86–95 [DOI] [PMC free article] [PubMed] [Google Scholar]