Abstract
Background and Purpose
Studies suggest that family caregiver well-being (ie,, depressive symptoms and life satisfaction) may affect stroke survivor depressive symptoms. We used mediation analysis to assess whether caregiver well-being might be a factor explaining stroke survivor depressive symptoms, after controlling for demographic factors and stroke survivor impairments and problems.
Methods
Caregiver/stroke participant dyads (N=146) completed measures of stroke survivor impairments and problems and depressive symptoms and caregiver depressive symptoms and life satisfaction. Mediation analysis was used to examine whether caregiver well-being mediated the relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms.
Results
As expected, more stroke survivor problems and impairments were associated with higher levels of stroke survivor depressive symptoms (P < .0001). After controlling for demographic factors, we found that this relationship was partially mediated by caregiver life satisfaction (29.29%) and caregiver depressive symptoms (32.95%). Although these measures combined to account for 40.50% of the relationship between survivor problems and impairments and depressive symptoms, the direct effect remained significant.
Conclusions
Findings indicate that stroke survivor impairments and problems may affect family caregivers and stroke survivors and a high level of caregiver distress may result in poorer outcomes for stroke survivors. Results highlight the likely importance of intervening with both stroke survivors and family caregivers to optimize recovery after stroke.
Keywords: caregiver depressive symptoms, caregiver well-being, stroke depressive symptoms
Stroke is a leading cause of serious, long-term disability in the United States,1 and survivors experience multiple physical, psychological, and emotional changes that often lead to depressive symptoms.2 Most stroke survivors return to the community and rely on family caregivers to assist in managing stroke-related deficits.3 However, family members may have trouble adapting to the caregiver role, and stressors such as stroke survivor functional deficits often lead to depressive symptoms4 and less life satisfaction in caregivers.5
Stroke survivor impairments and problems affect many aspects of daily living for caregivers, but data also suggest that caregivers who have a positive well-being, including few depressive feelings6 and higher life satisfaction,7 may be better emotionally equipped to handle the stresses of caregiving5 and potentially reduce stroke survivor depressive symptoms.8
Although stroke survivor impairments and problems, caregiver depressive symptoms and life satisfaction, and survivor depressive symptoms appear to be related, the direction of these relationships remains unclear.8,9 Empirical findings suggest that caregiver well-being, including depressive symptoms and life satisfaction, and care recipient functioning may have a reciprocal influence on each other. In this study, we used mediation analysis, a statistical approach that examines the process underlying observed relationships between variables. Mediation analysis cannot prove causation, but it allows for an examination of whether factors such as caregivers’ well-being alter the relationship between stroke survivors’ impairments and depressive symptoms.10 We were unable to identify any studies of mediation related to poststroke depression. Therefore, we believe this study is one of the first to apply mediation analysis to this question in a population-based sample of stroke survivors and their caregivers. This topic is important; if the well-being of family caregivers affects the outcomes of stroke survivors, then caregivers should be considered as as a key element of stroke rehabilitation and intervention.
The purpose of this study was to examine whether caregiver well-being (ie, depressive symptoms and life satisfaction) was a mediator of the relationship between impairments and problems and depressive symptoms in stroke survivors. We hypothesized that higher numbers of problems would be associated with more depressive symptoms and that caregiver well-being would be a mediator of this relationship. Specifically, we hypothesized that more stroke survivor problems would be associated with poor caregiver well-being, which would be associated with more stroke survivor depressive symptoms.
Methods
Participants and setting
Data for these analyses were drawn from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study, an ongoing, national, epidemiologic investigation of stroke incidence and mortality that enrolled 30,239 participants, 45 years of age or older, from 2003 to 2007.11,12 After stroke survivors were identified by the REGARDS project, they were recruited, along with primary family caregivers, to participate in the ancillary Caring for Adults Recovering from the Effects of Stroke (CARES) project. Participants in the CARES sample were drawn from 30 states across the country, resulting in a wide variety of demographic characteristics and a more generalizable investigation of stroke survivors and their caregivers. The CARES project is an epidemiologically based study that comprises Caucasians and African Americans.7,13,14
Participants were recruited between 2005 and 2010 and consisted of 146 community-dwelling residents who were stroke survivors from the REGARDS project who also participated in the CARES project and who met the following criteria: (1) were 45 years of age or older; (2) had medical records for a stroke event; (3) were community-dwelling residents an average of 9 months after the stroke event; and (4) designated a family member or close friend who was serving as an informal caregiver or had served previously in this capacity after the stroke event. Potential participants were excluded if reported strokes could not be confirmed by medical records or were adjudicated as transient ischemic attacks or other nonstroke medical problems or if they were residents of nursing homes or other residential care facilities.
Stroke caregivers met the following criteria: (1) were 19 years of age or older; (2) were able to speak English and hear well enough to engage in telephone interviews with a trained researcher; (3) confirmed they were a family member or close friend who \ was currently serving or had previously served as an informal caregiver following the stroke event; and (4) were reachable by telephone. Caregivers (n = 141) provided an average of 5.87 hours per day (SD 7.05) in the caregiver role .
Of 241 screened dyads, 47 were not eligible to participate in the study (eg, stroke survivor did not have a caregiver or lived in a nursing home or other long-term care residence), which left 194 who were eligible to participate. Of these, we successfully enrolled 146 (76%) of the contacted dyads. Data from the baseline CARES stroke survivors and caregivers’ telephone interviews were used for these analyses.
A cross-sectional design was used. All procedures for this study were approved by the institutional review board of the University of Alabama at Birmingham. After obtaining informed consent, trained research interviewers collected stroke survivor and caregiver demographic information and data on caregiver-reported stroke survivor impairments and problems, caregiver and stroke survivor depressive symptoms, and caregiver life satisfaction.
Procedures
An initial baseline CARES interview was conducted by telephone approximately 9 months after the stroke event. Medical records were examined independently by at least 2 trained physician adjudicators, including at least 1 stroke neurologist, to confirm stroke events and determine stroke type (ischemic vs hemorrhagic). Other extracted variables included the affected cerebral hemisphere (left, right, bilateral), length of the acute hospital stay, and discharge status (eg, to home, to a rehabilitation facility, or to a nursing home). Interviews with caregivers and stroke survivors were conducted in their home by trained research personnel via telephone. Each participant received $20 for participating in this project.
Demographic data
Demographic information was collected from caregivers and care recipients to allow an examination of associations between these characteristics and the criterion variable. Demographic variables of stroke survivors included age, race, gender, educational level (collected from an earlier interview in the REGARDS study), and co-residence with the caregiver. Demographic variables of caregivers included age, gender, and educational level.
Stroke survivor impairments and problems
Caregivers reported the occurrence of stroke survivor impairments and problems during the previous week (ie, physical symptoms, cognitive/memory problems, emotional problems, and problems in completing activities of daily living/instrumental activities of daily living) using a 28-item instrument. The instrument has been shown to have good concurrent validity (correlating over .62 with the Barthel Index and Rankin scores). The coefficient alpha for this scale is 0.92.7
Caregiver depressive symptoms
Caregiver depressive symptoms were assessed with the Center for Epidemiologic Studies Depression Scale (CES-D),15 a 20-item Likert-type scale. The CES-D has been used in numerous studies,6,14 supporting adequate psychometric properties (α = 0.89, in our sample). Higher scores indicate more depressive symptomatology.
Caregiver life satisfaction
Caregiver life satisfaction was assessed with the Life Satisfaction Index (LSI-Z), a 13-item scale that measures positive feelings of accomplishment and general morale.16 Scores range from 0 to 26, with higher scores representing greater life satisfaction. It has adequate psychometric properties.17 The coefficient alpha in our sample was 0.73. The LSI-Z has been used successfully with caregivers from diverse racial/ethnic backgrounds and age groups.18,19
Stroke survivor depressive symptoms
Stroke survivor depressive symptoms were also assessed with the CES-D,15 with a coefficient alpha of 0.90 in our sample.
Statistical analyses
We used bivariate linear regression models to examine relationships between demographic variables and stroke survivor depressive symptoms. Demographic variables significantly associated with stroke survivor depressive symptoms were included as covariates within subsequent regression models. We examined mediating factors using the joint significance test of alpha (α) and beta (β). Krause et al10 compared 12 methods of testing mediation, including the commonly used one proposed by Baron and Kenny,20,21 and results revealed the joint significance test of α and β to be the best mediational method after its ability to control for a type I error and its computational ease and versatility had been considered. In this approach, there must be an initial relationship between the independent variable and the outcome. If this relationship is present, regression analyses are conducted to determine whether (a) the independent variable is a predictor of the mediator and (b) the mediator is a predictor of the criterion variable, after controlling for the independent variable. If both are true, joint significance is obtained and mediation is present. “Full” mediation refers to the direct effect of the independent variable on the outcome becoming nonsignificant, and “partial” mediation (the direct effect remaining significant) suggests that the mediator cannot completely explain the direct effect and other factors may need to be considered.
The significance level for all tests was set at P < .05. Standardized betas were used to determine how much the direct effect between stroke survivor impairments and problems and stroke survivor depressive symptoms was reduced by examining caregiver depressive symptoms and caregiver life satisfaction as mediators in separate models, as well as, by examining their effects in a model that included both potential mediators.
Results
The sample consisted of 146 stroke survivor/caregiver dyads. Stroke survivors ranged in age from 52 to 94 years, with 133 (91.1%) ischemic strokes, 12 (8.2%) hemorrhagic strokes, and 1 (0.7%) undefined stroke event. Of the survivors, 10 (7%) reported a previous stroke event. Stroke survivors with a previous history of stroke reported less education, and their caregivers reported they had more problems than individuals without a previous stroke event (P < .01). There were no additional differences in variables of interest. Stroke survivors had an average score of 9.57 (SD 9.99; range, 0–48) on the CES-D, and 21.92% had scores of 16 or greater associated with being at risk for clinical depression.
Caregivers ranged in age from 19 to 95 years. They reported an average of 7.55 (SD 6.44) impairments/problems for their care recipients and had a mean score of 20.16 (SD 4.58) on the LSI-Z. The mean score on the CES-D for caregivers was 6.89 (SD 8.52; range, 0–48), and 10.96% had scores of 16 or greater. Bivariate regression models revealed that older stroke survivor age, Caucasian race, male gender, higher education level, co-residence with the caregiver, and older caregiver age were each associated with fewer stroke survivor depressive symptoms. Bivariate associations between demographics and stroke survivor depressive symptoms are presented in Table 1. Therefore, these 6 demographic variables were included as covariates in subsequent models.
Table 1.
Bivariate associations between demographics and stroke survivor depressive symptoms
| Mean (SD) | n (%) | b | Standard error |
B | t statistic | P value | |
|---|---|---|---|---|---|---|---|
| Stroke survivor demographics | |||||||
| Age, years | 74.66 (7.82) | −0.248 | 0.104 | −0.194 | −2.37 | .0190 | |
| African American | 62 (42.47) | 3.974 | 1.645 | 0.197 | 2.42 | .0170 | |
| Female | 74 (50.68) | 3.286 | 1.636 | 0.165 | 2.01 | .0464 | |
| Education level a | 1.73 (1.08) | −2.200 | 0.750 | −0.238 | −2.93 | .0039 | |
| Co-residence with caregiver | 98 (67.12) | −4.181 | 1.731 | −0.197 | −2.42 | .0170 | |
| Caregiver demographics | |||||||
| Age | 63.72 (13.44) | −0.140 | 0.061 | −0.189 | −2.31 | .0223 | |
| Female gender | 114 (78.08) | 0.848 | 2.004 | 0.035 | 0.42 | .6727 | |
| Education levelb | 14.17 (2.70) | −0.468 | 0.305 | −0.127 | −1.53 | .1275 |
Note: b = unstandardized estimate; B = standardized estimate.
Stroke survivor education level: 0 = less than high school, 1 = high school graduate, 2 = some college, 3 = college graduate.
Caregiver education level: years of education from 0 to 20.
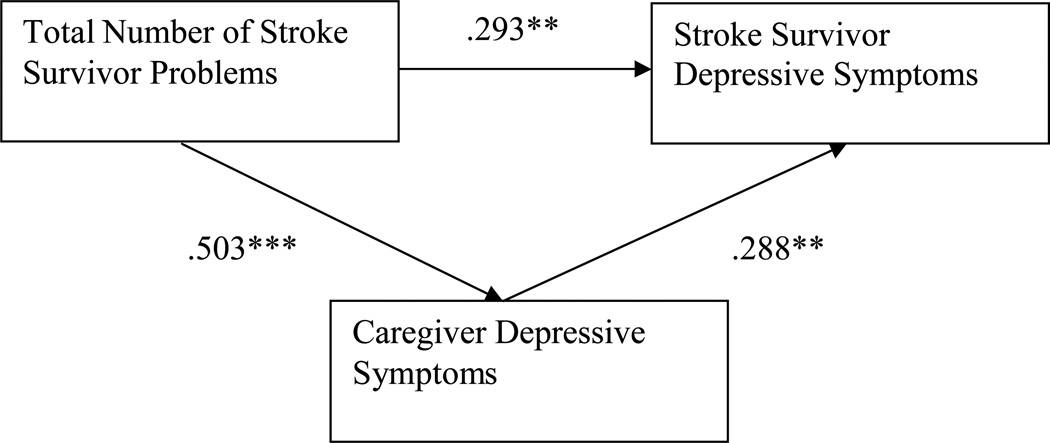
A multivariable, covariate-adjusted regression model with stroke survivor depressive symptoms as the dependent variable and stroke survivor age, race, gender, education level, co-residence with the caregiver, caregiver age, and stroke survivor impairments as predictors was examined. Older stroke survivor age and co-residence with the caregiver were associated with fewer stroke survivor depressive symptoms (P < .05). On the other hand, a greater number of stroke survivor impairments and problems were associated with stroke survivors reporting more depressive symptoms (standardized estimate B = 0.437; P < .0001). When caregiver depressive symptoms were examined as a potential mediator of this relationship, total stroke survivor impairments and problems remained associated with stroke survivor depressive symptoms. Additionally, a higher number of caregiver depressive symptoms were associated with stroke survivors reporting more depressive symptoms, after controlling for stroke survivor impairments and problems. The direct effect of total stroke survivor impairments and problems on stroke survivor depressive symptoms was not completely explained, suggesting that partial mediation was present. The examination of caregiver depressive symptoms as a potential mediator of the relationship between stroke survivor problems and stroke survivor depressive symptoms is presented in Figure 1. Inclusion of caregiver depressive symptoms in the model reduced the strength of the direct relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms by 32.95% [(0.437 − 0.293) / 0.437].
Figure 1.
Caregiver depressive symptoms as a mediator of the relationship between stroke survivor problems and stroke survivor depressive symptoms
Note: Standardized estimates are shown; * p < .05, ** p < .001, *** p < .0001.
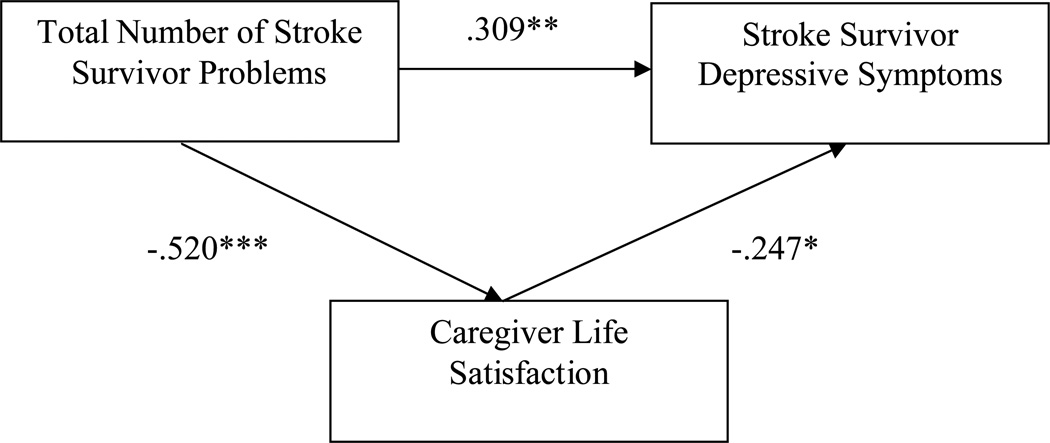
Caregiver life satisfaction was also examined as a potential mediator of the relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms. Total stroke survivor impairments and problems were associated with caregiver life satisfaction, and better caregiver life satisfaction was associated with fewer stroke survivor depressive symptoms, after controlling for total stroke survivor impairments and problems. The direct effect of total stroke survivor impairments and problems on stroke survivor depressive symptoms remained significant, suggesting that partial mediation was present. The examination of caregiver life satisfaction as a potential mediator of the relationship between stroke survivor problems and stroke survivor depressive symptoms is presented in Figure 2. Inclusion of caregiver life satisfaction in the model reduced the strength of the direct relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms by 29.29% [(0.437 − 0.309) / 0.437].
Figure 2.
Caregiver life satisfaction as a mediator of the relationship between stroke survivor problems and stroke survivor depressive symptoms
Note: Standardized estimates are shown; * p < .05, ** p < .001, *** p < .0001.
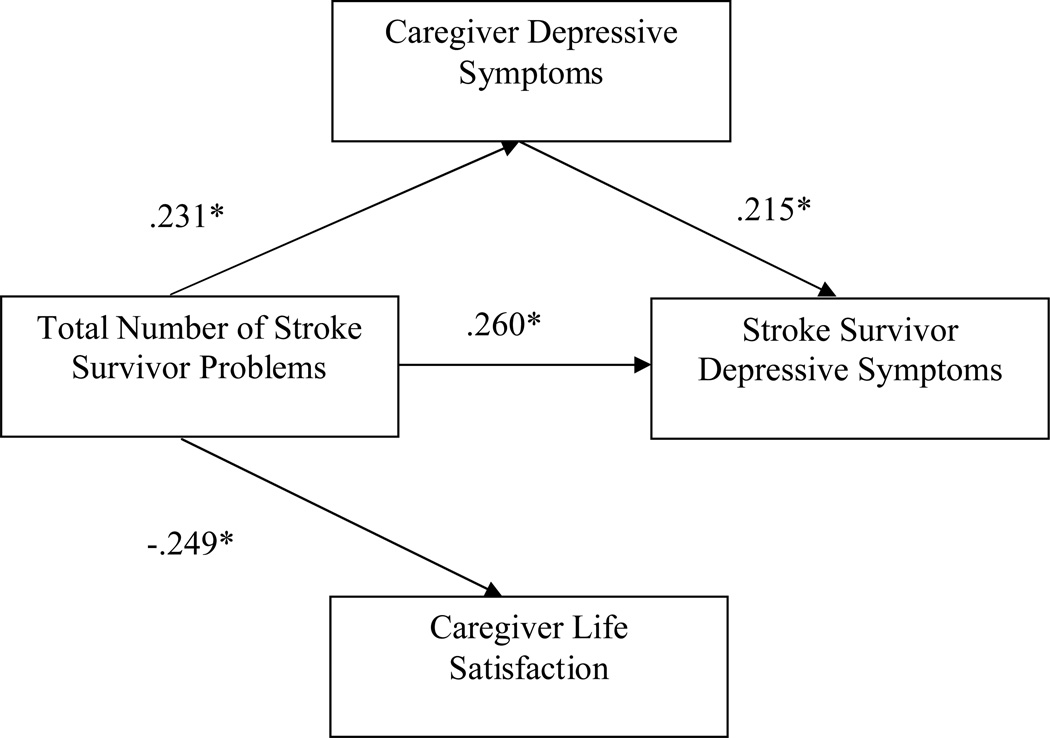
Finally, caregiver depressive symptoms and life satisfaction were examined together as potential mediators of the relationship between stroke survivor impairments and problems and depressive symptoms. In the covariate adjusted model, total stroke survivor impairments and problems were associated with caregiver life satisfaction, caregiver depressive symptoms, and stroke survivor depressive symptoms. Additionally, caregiver depressive symptoms were associated with stroke survivor depressive symptoms. However, caregiver life satisfaction was not associated with stroke survivor depressive symptoms, after controlling for other variables in the model. This was due to the moderate correlation between caregiver depressive symptoms and caregiver life satisfaction (r = −0.62, P < .0001). Therefore, caregiver life satisfaction served as a partial mediator of the relationship between stroke survivor problems and stroke survivor depressive symptoms, but much of this effect overlaps with caregiver depressive symptoms. The direct effect of total stroke survivor impairments and problems on stroke survivor depressive symptoms remained significant, suggesting that partial mediation was present. The examination of caregiver depressive symptoms and life satisfaction as potential mediators of the relationship between stroke survivor problems and stroke survivor depressive symptoms is depicted in Figure 3. Both caregiver depressive symptoms and life satisfaction together reduced the direct effect by 40.50% [(0.437 − 0.260) / 0.437].
Figure 3.
Caregiver depressive symptoms and life satisfaction as mediators of the relationship between stroke survivor problems and depressive symptoms
Note: Standardized estimates are shown; * p < .05, ** p < .001, *** p < .0001
Discussion
Our results strongly supported our hypothesis that caregiver well-being was a mediator of the relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms. As in previous studies, stroke survivor impairments and problems were strong correlates of stroke survivor depression and family caregiver well-being. In fact, other studies have demonstrated that stroke survivor cognitive/memory and emotional problems and functional deficits often lead to both caregiver2,4 and stroke survivor22,23 depressive symptoms and to lower caregiver life satisfaction.5, 24
The unique contribution of our findings is the mediational results. Even after controlling for demographic variables, caregiver well-being accounted for substantial amounts of variance in the relationship between stroke survivor impairments and problems and stroke survivor depressive symptoms. This ranged from 29.29% (using caregiver life satisfaction) to 40.50% (using both caregiver life satisfaction and caregiver depressive symptoms) of the relationship between survivor problems and impairments and depressive symptoms.
These findings suggest that family caregiver reactions to stroke survivor problems and impairments can influence stroke survivors’ well-being. Mediation analysis cannot provide definitive proof of a causal relationship, but it does allow for examination of whether a proposed causal ordering is consistent with these data. In this case, it appears likely that stroke survivor impairments and problems have effects on both caregivers and stroke survivors, and caregiver well-being may affect the emotional responses of stroke survivors.
There are plausible mechanisms to explain this relationship. Caregivers who react to stroke with depression and low life satisfaction may be less effective in promoting stroke survivor recovery. Emotional contagion may also occur. Distressed, pessimistic, negative family caregivers may provide an emotional context that is itself very discouraging to stroke survivors.25 Although our research focused on stroke survivor depressive symptoms as an outcome, other empirical findings suggest that caregiver depressive symptoms increase the risk for other poor outcomes, such as limited functional recovery26 and institutionalization.27 The extant literature also indicates that several stroke survivor and caregiver demographic characteristics potentially affect stroke survivor depressive symptoms.26
This research has the advantages of applying mediation analysis to an important area of stroke research, and we have the additional strength of drawing on a large sample of stroke survivors and caregivers for these analyses. There are limitations to our project. These results are cross-sectional. Although mediation analysis identifies whether a particular causal model is plausible given the association between variables, longitudinal analysis would be superior in assessing a proposed causal ordering. Future studies should apply mediation analysis to longitudinal data to determine whether these associations are found prospectively. Depression is common among stroke survivors who experience reductions in physical functioning. Future studies should examine stroke survivors in the acute phase and the distress associated with their loss in functioning. Such studies could assess the use of antidepressants and other forms of treatment following a stroke event in an attempt to determine whether they are beneficial.
The sample in this study differs from samples in many previous studies of stroke survivors and caregivers. One strength of our project is that as a population-based study of stroke, it likely includes many more mild stroke cases than are found in studies that recruit participants from clinical settings7,13 Depressive scores are lower and life satisfaction scores are higher than in participants of other studies.4,5 Further, survivor depressive scores are lower than those scores from other studies, suggesting a higher level of well-being.2,23 This finding may be due to our inclusion of milder strokes and the timing of our assessments at 9 months post stroke on average, reflecting a point at which the majority of initial symptoms may have abated. It will be important to replicate our findings with those from other samples experiencing greater stroke functional deficits, higher depressive scores, and lower life satisfaction. Even though the stroke survivor impairments and problems instrument has research to support its concurrent validity and reliability, it will also be important to replicate this work with other measures of stroke survivor impairment.
Further, caregiver well-being was operationalized as depressive symptoms and life satisfaction. We recognize that there are many other indices of caregiver well-being, and other studies might explore whether other indicators of well-being yield similar results. Additionally, caregivers rated stroke survivor impairments in this investigation. Although rating of functional deficits by trained raters would have been desirable, empirical data have shown moderate to high levels of stroke survivor-proxy agreement.28 Although proxies tend to rate stroke survivor impairment as more severe, observable behaviors such as stroke survivor impairments are more consistent.29 In a comparison of telephone interviews and face-to-face interviews, the 2 methods appear to be highly correlated.30
Conclusion
Both caregiver depressive symptoms and life satisfaction may affect stroke survivor depressive symptoms. Other studies suggest that intervention components of skill development, education, and problem solving may improve the well-being of caregivers.31,32 Family-oriented interventions that strengthen communication and joint problem-solving and decrease relationship stress around the illness appear to be valuable in improving physical health outcomes and lessening mental health problems.32 Further, interventions of longer duration appear to be more valuable than those of shorter duration. Findings of this study emphasize the potential importance of developing caregiver interventions to improve caregiver mental health, with the result of lessening stroke survivor depressive symptoms as well.
Acknowledgments
Financial support/disclosure: The research reported in this article was supported by an investigator-initiated grant (R01 NS045789, David L. Roth, PI) and by a cooperative agreement (U01 NS041588) from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis, or interpretation of the data.
Footnotes
Additional contributions: The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
REFERENCES
- 1.Centers for Disease Control and Prevention. [Accessed August 8, 2010];Stroke facts. 2010 http://www.cdc.gov/stroke/facts.htm.
- 2.Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis. 2009;27(suppl 1):204–214. doi: 10.1159/000200461. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. [Accessed August 6, 2010];Health, United States, 2008: with special feature on the health of young adults. 2008 http://www.cdc.gov/nchs/data/hus/hus08.pdf#highlights.
- 4.Visser-Meily A, Post M, van de Port I, et al. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke: course and relations with coping strategies. Stroke. 2009;40:1399–1404. doi: 10.1161/STROKEAHA.108.516682. [DOI] [PubMed] [Google Scholar]
- 5.Visser-Meily A, Post M, Schepers V, et al. Spouses' quality of life 1 year after stroke: prediction at the start of clinical rehabilitation. Cerebrovasc Dis. 2005;20:443–448. doi: 10.1159/000088983. [DOI] [PubMed] [Google Scholar]
- 6.Suh M, Kim K, Kim I, et al. Caregiver's burden, depression and support as predictors of post-stroke depression: a cross-sectional survey. Int J Nurs Stud. 2005;42:611–618. doi: 10.1016/j.ijnurstu.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Haley WE, Allen JY, Grant JS, et al. Problems and benefits reported by stroke family caregivers: results from a prospective epidemiological study. Stroke. 2009;40:2129–2133. doi: 10.1161/STROKEAHA.108.545269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perrin PB, Heesacker M, Stidham BS, et al. Structural equation modeling of the relationship between caregiver psychosocial variables and functioning of individuals with stroke. Rehabil Psychol. 2008;53:54–62. [Google Scholar]
- 9.Barskova T, Wilz G. Interdependence of stroke survivors' recovery and their relatives' attitudes and health: a contribution to investigating the causal effects. Disabil Rehabil. 2007;29:1481–1491. doi: 10.1080/09638280601029399. [DOI] [PubMed] [Google Scholar]
- 10.Krause MR, Serlin RC, Ward SE, et al. Testing mediation in nursing research: beyond Baron and Kenny. Nurs Res. 2010;59:288–294. doi: 10.1097/NNR.0b013e3181dd26b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howard VJ, Cushman M, Pulley L, et al. REasons for Geographic and Racial Differences in Stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 12.Howard VJ, Kleindorfer DO, Judd SE, et al. Disparities in stroke incidence contributing to disparities in stroke mortality [published online ahead of print January 24, 2011] [Accessed March 30, 2011];Ann Neurol. doi: 10.1002/ana.22385. http://onlinelibrary.wiley.com/doi/10.1002/ana.22385/pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roth DL, Haley WE, Clay OJ, et al. Race and gender differences in 1-year outcomes for community-dwelling stroke survivors with family caregivers. Stroke. 2011;42:626–631. doi: 10.1161/STROKEAHA.110.595322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haley WE, Roth DL, Kissela B, et al. Quality of life after stroke: a prospective longitudinal study [published online ahead of print December 7, 2010] [Accessed March 30, 2011];Qual Life Res. doi: 10.1007/s11136-010-9810-6. http://www.springerlink.com/content/p53601j0206h1062/fulltext.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 16.Wood V, Wylie ML, Sheafor B. An analysis of a short self-report measure of life satisfaction: correlation with rater judgments. J Gerontol. 1969;24:465–469. doi: 10.1093/geronj/24.4.465. [DOI] [PubMed] [Google Scholar]
- 17.Weitzenkamp DA, Gerhart KA, Charlifue SW, et al. Spouses of spinal cord injury survivors: the added impact of caregiving. Arch Phys Med Rehabil. 1997;78:822–827. doi: 10.1016/s0003-9993(97)90194-5. [DOI] [PubMed] [Google Scholar]
- 18.Clay OJ, Roth DL, Wadley VG, Haley WE. Changes in social support and their impact on psychosocial adjustment of African American and white dementia caregivers over a five-year period. Int J Geriatr Psychiatry. 2008;23:857–862. doi: 10.1002/gps.1996. [DOI] [PubMed] [Google Scholar]
- 19.Burton AM, Haley WE, Small BJ, Finley P, Dillinger-Vasille M, Schonwetter R. Predictors of well-being in bereaved former hospice caregivers: the role of caregiving stressors, appraisals, and social resources. Palliat Support Care. 2008;6:149–158. doi: 10.1017/S1478951508000230. [DOI] [PubMed] [Google Scholar]
- 20.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 21.Kenny DA. [Accessed March 30, 2011];Mediation. 2009 http://davidakenny.net/cm/mediate.htm.
- 22.Carod-Artal FJ, Trizotto DS, Coral LF, Moreira CM. Determinants of quality of life in Brazilian stroke survivors. J Neurol Sci. 2009;284(1–2):63–68. doi: 10.1016/j.jns.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Teoh V, Sims J, Milgrom J. Psychosocial predictors of quality of life in a sample of community-dwelling stroke survivors: a longitudinal study. Top Stroke Rehabil. 2009;16(2):157–166. doi: 10.1310/tsr1602-157. [DOI] [PubMed] [Google Scholar]
- 24.Pinquart M, Sörensen S. Associations of caregiver stressors and uplifts with subjective well-being and depressive mood: a meta-analytic comparison. Aging Ment Health. 2004;8:438–449. doi: 10.1080/13607860410001725036. [DOI] [PubMed] [Google Scholar]
- 25.Eisenkraft N, Elfenbein HA. The way you make me feel: evidence for individual differences in affective presence. Psychol Sci. 2010;21:505–510. doi: 10.1177/0956797610364117. [DOI] [PubMed] [Google Scholar]
- 26.Klinedinst NJ, Gebhardt MC, Aycock DM, et al. Caregiver characteristics predict stroke survivor quality of life at 4 months and 1 year. Res Nurs Health. 2009;32:592–605. doi: 10.1002/nur.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayes J, Chapman P, Young LJ, et al. The prevalence of injury for stroke caregivers and associated risk factors. Top Stroke Rehabil. 2009;16:300–307. doi: 10.1310/tsr1604-300. [DOI] [PubMed] [Google Scholar]
- 28.Sneeuw KC, Sprangers MA, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J Clin Epidemiol. 2002;55:1130–1143. doi: 10.1016/s0895-4356(02)00479-1. [DOI] [PubMed] [Google Scholar]
- 29.Duncan PW, Lai SM, Tyler D, Perera S, Reker DM, Studenski S. Evaluation of proxy responses to the Stroke Impact Scale. Stroke. 2002;33:2593–2599. doi: 10.1161/01.str.0000034395.06874.3e. [DOI] [PubMed] [Google Scholar]
- 30.Carrete P, Augustovski F, Gimpel N, et al. Validation of a telephone-administered Geriatric Depression Scale in a Hispanic elderly population. J Gen Intern Med. 2001;16:446–450. doi: 10.1046/j.1525-1497.2001.016007446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bakas T, Farran CJ, Austin JK, et al. Stroke caregiver outcomes from the Telephone Assessment and Skill-Building Kit (TASK) Top Stroke Rehabil. 2009;16(2):105–121. doi: 10.1310/tsr1602-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartmann M, Bäzner E, Wild B, et al. Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: a meta-analysis. Psychother Psychosom. 2010;79(3):136–148. doi: 10.1159/000286958. [DOI] [PubMed] [Google Scholar]