Abstract
To assess decision-making for cancer treatment among racial/ethnic minority patients, we systematically reviewed and synthesized evidence from studies of “shared decision-making,” “cancer,” and “minority groups,” using PubMed, PsycInfo, CINAHL, and EMBASE. We identified significant themes that we compared across studies, refined, and organized into a conceptual model.
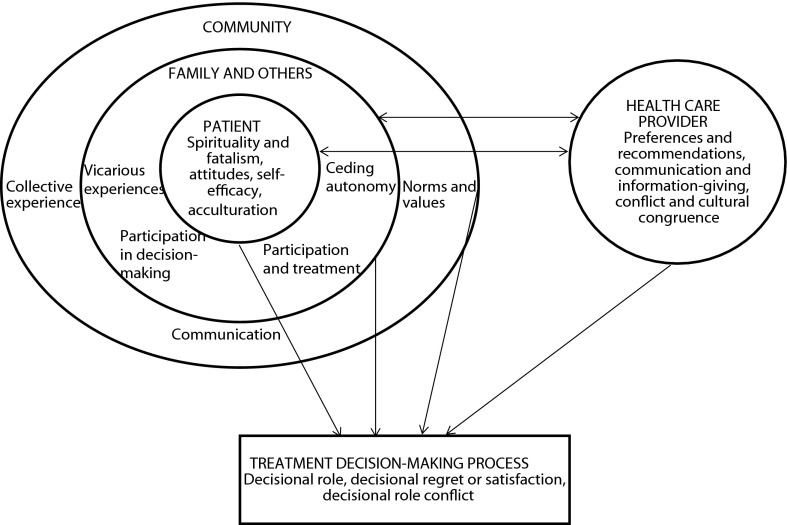
Five major themes emerged: treatment decision-making, patient factors, family and important others, community, and provider factors. Thematic data overlapped categories, indicating that individuals’ preferences for medical decision-making cannot be authentically examined outside the context of family and community.
The shared decision-making model should be expanded beyond the traditional patient–physician dyad to include other important stakeholders in the cancer treatment decision process, such as family or community leaders.
IN SPITE OF DECLINING CANCER incidence and mortality in the United States, minority patients continue to have lower 5-year survival rates than non-Hispanic Whites.1 Although differences in stage at diagnosis may partly account for survival differences, a large proportion of the disparity in survival has been attributed to poorer quality of care, delay in receipt of treatment, or no receipt of treatment among minority patients.2–8 Specific health systems or individual providers no doubt contribute to unnecessary delays in care. However, patients also may have reason to delay or refuse treatment, such as a poor patient–provider relationship or dissatisfaction with the treatment plan.
Effective patient-centered communication and a positive patient–provider relationship have been associated with improved treatment adherence, survival, and health-related quality of life among cancer patients.9,10 Racial and ethnic minority patients are at higher risk than White patients for poor communication and a strained patient–provider relationship, which in turn can lead to delayed or nonstandard care.11–13 Incorporating cultural and individual patient preferences into cancer treatment planning through shared decision-making (SDM) may improve adherence to treatment recommendations and reduce delays in care.14
The SDM model emphasizes the physician’s facilitation of the patient’s involvement in treatment decision-making to improve quality of care and patient centeredness, and thereby improve health outcomes. (In health care, “patient centeredness” includes viewing and treating the patient as a whole and unique person, rather than simply focusing on the disease process.) As opposed to the historical paternalistic or informed decision-making models, the SDM model is defined by a 2-way information exchange between the physician and the patient, followed by discussion of treatment preferences by both parties until they reach consensus on a treatment decision.15 However, cancer patients’ preferred level of involvement in treatment decision-making may vary. A recent review found mixed effects of the impact of SDM interventions on patients’ satisfaction and medication adherence.16 Alignment between patients’ preferred and actual decisional role may be more important to patients’ satisfaction than decisional autonomy.17,18
Taken together, these data suggest that the SDM approach may not be right for every cancer patient. Indeed, the available evidence suggests substantial cultural variation in the cancer treatment decision-making process, including culture-specific differences in communication style, desired amount and type of information, and preferred decisional role.15,19 For patients living in a defined social and cultural context such as an American Indian/Alaska Native (AI/AN) tribe, cultural congruence includes recognition of the decision-making role played by other important stakeholders outside of the patient–physician dyad.20,21
To better assess SDM among racial/ethnic minority cancer patients, we performed a systematic review of the literature on SDM for cancer treatment in ethnic minority groups. We created a conceptual model to expand the SDM model and to identify the multilevel determinants of cancer treatment decision-making among ethnic minority groups, which include factors at the level of the patient, family and significant others, community, and provider. We summarized the literature at each level of the model to determine what is currently known about cultural variation in cancer treatment decision-making, to expose the relevant gaps in knowledge, and to make recommendations for future research.
METHODS
The present systematic literature review followed guidelines put forth by the Institute of Medicine.22 In July 2011, we initiated a search of the published literature using PubMed, PsycInfo, CINAHL, and EMBASE, without applying date limits. As a first step, we searched broadly for “shared decision-making” and “cancer.” Because shared decision-making is a relatively recent concept and therefore is not a standardized keyword search term, we built a search string that captured “shared decision-making” individually for each database using the keyword search terms available (see appendix, available as a supplement to this article at http://www.ajph.org). Next, we limited the search to studies that would capture cancer treatment decision-making and the impact of cultural differences on decision-making among racial/ethnic minority populations. “Minority groups” were defined as populations who were the racial, ethnic, or cultural minority population in the country where the study took place. As with “shared decision-making,” we developed search strategies specific to each database to capture the literature on minority populations.
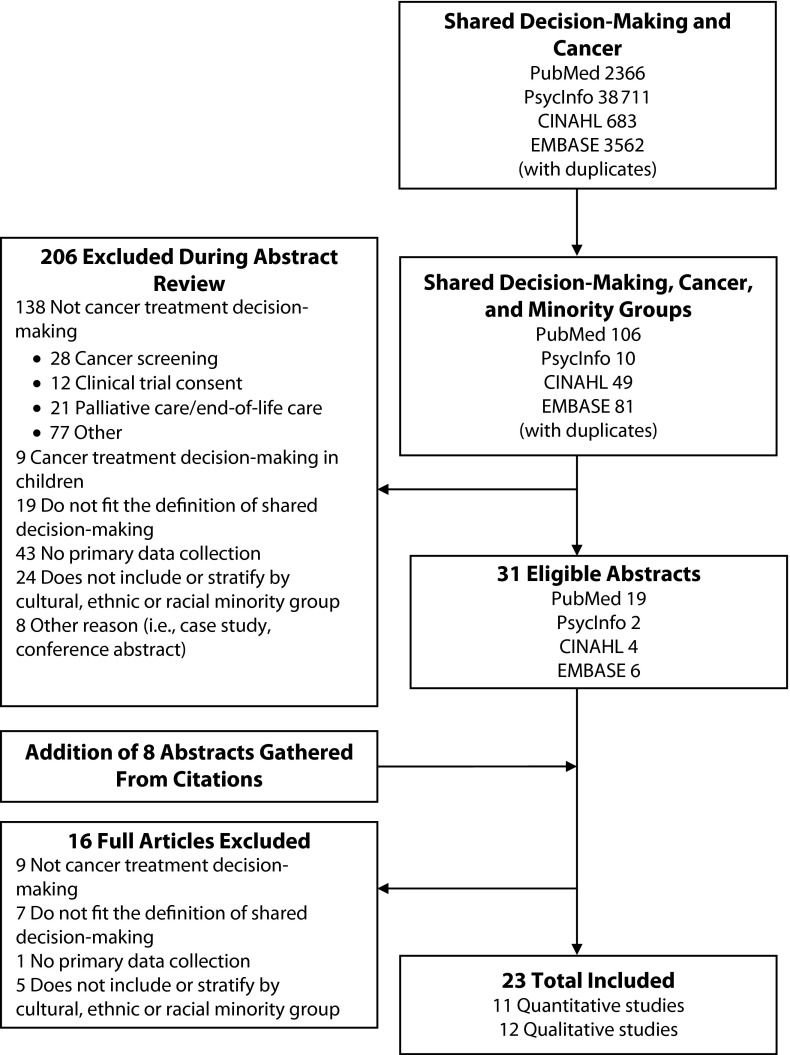
E. L. M. and A. M. M. developed inclusion and exclusion criteria for the systematic review and for the review of the search results, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) schema.23 They excluded studies if they contained no data about cancer treatment decision-making, contained no data for adult patients, contained no primary data, or did not report or stratify by cultural, ethnic, or racial minority group. Both quantitative and qualitative studies were eligible for inclusion. One reviewer assessed 246 abstracts (including duplicates) and excluded 206 on the basis of the exclusion criteria (see the box on this page) as well as 9 duplicates, leaving 31 eligible abstracts. An additional 8 abstracts from the references of the eligible abstracts fulfilled criteria and were included. In the second round of review, 2 reviewers independently reviewed the 39 full text articles to verify eligibility for inclusion by applying the inclusion and exclusion criteria. After discussing discrepancies and reaching consensus, the reviewers excluded 16 of these articles (PRISMA diagram, Figure 1).
FIGURE 1—
Search and selection of published literature on shared decision-making, cancer, and minority groups through July 2011 in 4 electronic databases.
Note. Multiple studies fit more than 1 exclusion criteria.
Inclusion and Exclusion Criteria for a Systematic Literature Review on Shared Decision-Making in Cancer Treatment Among Minority Populations
| Inclusion Criteria |
| • Fit the definition of “shared decision-making.”a |
| • Reported data on cancer treatment decision-making. |
| • Collected primary data. |
| • Included results related to decision-making in a racial/ethnic or cultural minority group.b |
| • Published in a peer-reviewed journal. |
| Exclusion Criteria |
| • Conducted on decision-making for cancer treatment in children. |
| • Data not stratified by race/ethnicity or study did not include a minority groupb in study population. |
| • Conducted on palliative or end-of-life care in cancer treatment. |
Shared decision-making is defined as a 2-way information exchange between the physician and the patient followed by discussion of treatment preferences by both parties until they reach consensus on a treatment decision.15
A racial/ethnic or cultural minority group is defined as a population that was the racial, ethnic, or cultural minority population in the country where the study took place.
We developed a data abstraction tool for the systematic review that captured detailed data from both quantitative and qualitative studies, including study features, sample information, methods, results, conclusions, and assessments of methodological quality. Two reviewers independently abstracted these data points from the final articles, and E. L. M. combined the results. The reviewers resolved disagreements through discussion until consensus was reached.
A number of methods exist to synthesize quantitative and qualitative evidence from a systematic literature review, including narrative summary, content analysis, and qualitative metasummary.24,25 We chose thematic analysis for the present study because of its organizational and structural utility for synthesizing quantitative and qualitative evidence into coherent themes.24 We used an inductive approach—that is, the analysis was directed by the data content. Six steps of thematic analysis proceeded as follows. First, 2 reviewers independently performed an in-depth reading of each article (familiarization with the data). Second, they independently coded data. Third, they searched the data for significant themes relating to the role of shared decision-making in cancer treatment decisions among minority groups. Fourth, the 2 reviewers discussed, compared, and contrasted the themes across studies for further refinement until (fifth) they reached consensus on the final set of data-driven themes, which (sixth) they organized into a conceptual model.
SDM has been studied in the clinical context of very few cancer types, and we found no significant differences by cancer site in the limited available evidence for this study. Therefore, we synthesized findings for all cancer sites combined. We sorted findings and summarized them by theme and study type (quantitative vs qualitative). We report confidence intervals for the findings where available. We also describe racial, ethnic, and gender differences, when available.
RESULTS
A final total of 23 articles26–48—11 quantitative studies26–35,48 and 12 qualitative studies36–47—fulfilled criteria and were included in the study (Table 1). Most of the 11 quantitative studies focused solely on breast cancer (n = 8), followed by multiple cancer sites (n = 2) and prostate cancer (n = 1). Similarly, most of the 12 qualitative studies focused on breast cancer (n = 9), followed by prostate cancer (n = 1), lung cancer (n = 1), and unreported (n = 1). Most studies were conducted in the United States (n = 19). Ten of the quantitative studies compared more than 1 minority group; African Americans were the most commonly represented minority (n = 14), followed by Latinas (n = 6), Asians (n = 1), and an unspecified “other” (n = 3) minority group. Latina populations were frequently divided into low-acculturated and high-acculturated subgroups, defined by language preference (English vs Spanish). By contrast, only 4 of the qualitative studies compared multiple minority groups. Again, African Americans were most frequently represented (n = 5), followed by Asian (n = 4), Latina (n = 3), and Jewish (n = 1) populations. Within the Asian minority group, Chinese were represented in the most studies, followed by Punjabis.
TABLE 1—
Characteristics of Articles Included in a Systematic Literature Review on Shared Decision-Making in Cancer Treatment Among Minority Populations
| Characteristic | Quantitative Studies (n = 11), No. (%) | Qualitative Studies (n = 12), No. (%) |
| Cancer site | ||
| Breast | 8 (73) | 9 (75) |
| Prostate | 1 (9) | 1 (8) |
| Lung | 0 | 1 (8) |
| Multiple | 2 (18) | 0 |
| Not reported | 0 | 1 (8) |
| Study location | ||
| United States | 10 (91) | 9 (75) |
| Outside United States | 1 (9) | 3 (25) |
| Study populationa | ||
| Patients | 11 (100) | 11 (92) |
| Patients’ family and others | 0 | 3 (25) |
| Health care providers | 1 (9) | 3 (25) |
| Minority race/ethnicity of study populationa | ||
| African American | 9 (82) | 5 (42) |
| Latina/Latino | 6 (55) | 3 (25) |
| Asian | 1 (9) | 4 (33) |
| Haredi Ashkenazi Jewish | 0 | 1 (8) |
| Non-Hispanic White | 9 (82) | 3 (25) |
| Other (not specified) | 3 (27) | 1 (8) |
| Level of decision-makinga | ||
| Patient | 11 (100) | 12 (100) |
| Family and others | 5 (45) | 8 (67) |
| Community | 0 | 1 (8) |
Some studies had more than 1 subcategory.
Thematic analysis of the quantitative and qualitative papers revealed 5 major themes: treatment decision-making process, patient factors, factors related to family and important others, community factors, and provider factors. We organized the themes into a conceptual model of the decision-making process for cancer treatment among racial/ethnic minority patients (Figure 2). Several subthemes emerged, particularly among patient factors, which are described in detail in this section. Examples of dominant subthemes include spirituality, attitudes toward treatment, self-efficacy, acculturation, and advocacy (Table 2).
FIGURE 2—
A conceptual model of influences on cancer treatment decision-making among racial/ethnic minority patients.
TABLE 2—
Organization of References Into Conceptual Model Themes in a Systematic Literature Review on Shared Decision-Making in Cancer Treatment Among Minority Populations
| Theme and Subthemes | Quantitative References | Qualitative References |
| Treatment decision-making process | ||
| Decisional role | 26–28,30–34 | 36,38–47 |
| Conflict between actual and preferred decisional role | 28,31 | 39,41,43,45,46 |
| Satisfaction or regret with decision-making or decision | 28,31,48 | 39,41,43–46 |
| Patient factors | ||
| Level of acculturation and language | 26–29,33,48 | 36,37,41,42,44 |
| Spirituality and fatalism | 34 | 36,40,43–45,47 |
| Attitudes about treatment and decision | 27,29,34 | 36,38,43,45 |
| Self-efficacy | 32,33 | 44 |
| Factors of family and important others | ||
| Participation or advocacy of others in decision-making | 26–29,33,35 | |
| Participation or advocacy of others and receipt of treatment | 26–29,33,35 | |
| Consequences of ceding decision-making autonomy | 37–39,41,42,44,45,47 | |
| Vicarious experiences | 35 | 40,43,45 |
| Community factors | ||
| Cultural or community norms and values | 36–38,40,41,45 | |
| Communication with the community | 36,37,42,45 | |
| Decision-making as a collective experience | 37,39,45 | |
| Provider factors | ||
| Provider preferences and recommendations | 27,29,30,35 | 36,39,41,43,47 |
| Provider communication and information giving | 30,32,35 | 36,39,41–46 |
| Conflict and cultural congruence in the patient–provider relationship | 41,42,44 |
Treatment Decision-Making Process
The 3 subthemes of treatment decision-making process were decisional role, decisional regret or satisfaction, and decisional role conflict. Among the quantitative studies, shared and patient-based decision-making were most frequently used for cancer treatment decisions (Table 3). Patients’ decisional roles varied among minority groups and non-Hispanic White patients, but racial differences were not always explicit in the studies. Adoption of an SDM model was reported by 33% to 42% of low-acculturated Latina, high-acculturated Latina, and African American respondents.27,30,31,34 Patient-based decision-making was reported less often among low-acculturated Latina patients (29%–37%) compared with high-acculturated Latina patients (39%–75%).27,28,33,34 High-acculturated Latina patients were more likely to report patient-based decision-making than any other decision-making model, across several studies.27,28,33 Provider-based decision-making was less common, reported by only 10% to 33% of low-acculturated Latina patients, 7% to 27% of high-acculturated Latina patients, and 24% to 27% of African American patients.27,28,33,34
TABLE 3—
Summarization of Findings on Shared Decision-Making From the Quantitative Literature
| Article | Main Outcome Variables | Findings |
| Back and Huak26 | Nondisclosure of diagnosis | A “family-centered decision-making model” was important, with family-initiated nondisclosure of diagnosis to patients in 58 of 66 cases. Nondisclosure occurred more often when patients were older (OR = 7.7; 95% CI = 3.5, 16.8), female (OR = 6.0; 95% CI = 2.7, 13.7), non-English speaking (OR = 7.6; 95% CI = 1.7, 34.5), and in palliative care (OR = 3.2; 95% CI = 1.3, 7.9). |
| Hawley et al.28 | Match between actual and preferred decision-making role; satisfaction with decision or decision-making process | Decision-making: 37% of patients reported shared decision-making. Low-acculturated Latina women were more likely to report surgeon-based decision-making (31% vs 22%–28%; P not reported) and less likely to report patient-based decision-making (30% vs 33%–41%; P < .1). 93% of patients reported a match between preferred and actual involvement. |
| Dissatisfaction and regret: low-acculturated Latina women had the greatest likelihood of dissatisfaction (OR = 5.5; 95% CI = 2.9, 10.5) and regret (OR = 4.1; 95% CI = 2.2, 8.0). Companion presence was associated with lower dissatisfaction (OR = 0.65; 95% CI = 0.44, 0.96). | ||
| Hawley et al.27 | Treatment received | Patient–provider decision-making: surgeon-based decision-making was highest (33.1% vs 24.0%–26.7%) and patient-based decision-making lowest (29.5% vs 33.4%–39.8%) among low-acculturated Latina women. |
| Decision-making role of family and important others: African Americans had the significantly lowest frequency of being accompanied by anyone to a consultation (71.2% vs 77.5%–79.2%; P = .032). Family role in decision-making was significantly highest among low-acculturated Latina women (75.9%), followed by African American (50.3%), high-acculturated Latina (49.4%), and White women (34.1%; P for overall trend < .001). | ||
| Accompaniment to the consultation was associated with greater receipt of mastectomy (relative risk = 1.62; 95% CI = 1.14, 2.21). | ||
| Kaplan et al.29 | Type of treatment received | Patient–provider decision-making: more White women reported that the provider indicated radiation as optional (32.2%) than did high-acculturated Latina (18.7%) and low-acculturated Latina (10.2%) women. |
| Provider recommendation and concerns about survival were the most important influences on surgery decision-making reported by all ethnicities. | ||
| Compared with a recommendation that radiation was optional, provider indication that radiation was necessary was significantly associated with radiation therapy (OR = 8.05; 95% CI = 4.04, 16.03). | ||
| Among patients with breast-conserving surgery who did not undergo radiation therapy, low-acculturated Latina (67%) and high-acculturated Latina (69%) patients more frequently reported lack of provider recommendation as the reason than White women (57%). | ||
| Family influence on decision-making: low-acculturated Latina women rated family influences (P ≤ .01) as a greater influence on decision-making than other groups. | ||
| Katz et al.30 | Type of treatment received; treatment delay; satisfaction with decision or decision-making process | Low-acculturated Latina women had highest odds of low satisfaction with the decision-making process (OR = 3.6; 95% CI = 2.9, 6.9), followed by African American women (OR = 2.2; 95% CI = 1.7, 3.9) and high-acculturated Latina women (OR = 1.3; 95% CI = 1.0, 1.9; P for overall trend < .001). |
| Katz et al.48 | Treatment received | Decision-making: 37.1% of all women reported shared decision-making, 41.0% reported patient-based decision-making, and 21.9% reported provider-based decision-making. Patient-based decision-making was associated with the highest rate of mastectomy receipt. |
| Communication with surgeons: ethnic differences in mastectomy receipt were partially related to information exchange with surgeons. Among women who reported surgeon-based decision-making, more White women reported a discussion only about breast-conserving surgery (50.7%) than did African American (31.4%) and “other” women (26.0%; P = .029). Surgeons were more likely to recommend breast-conserving surgery to White women (51.6%) than to African American (41.7%) and “other” women (41.0%; P < .001). | ||
| Lantz et al.31 | Satisfaction with treatment; satisfaction with decision or decision-making process; regret with decision or decision-making process | Satisfaction with decision-making: most patients were satisfied with the decision-making process (80.6%). Low satisfaction with decision-making was associated with being African American (OR = 1.56; P < .001) and being “other” ethnicity (OR = 2.21; P < .001). Women whose decision-making role was less than or more than their preferred role had increased risk of low satisfaction with the decision-making process (OR = 3.23 [P < .001] and 2.48 [P < .001], respectively). |
| Regret with decision-making: increased regret was associated with being African American (OR = 1.82; P < .001) and being “other” ethnicity (OR = 2.58; P < .001). Women whose decision-making role was less than or more than their preferred role had increased risk of regret (OR = 2.42 [P < .001] and 1.71 [P < .001], respectively). | ||
| Maly et al.33 | Type of treatment received; final treatment decision-maker | Final decision-maker: compared with other ethnicities, low-acculturated Latina women were the least likely to identify themselves as the final decision-maker (36.6%) and most likely to have family or friend make the final decision (49.3%). |
| Family as the decision-maker: low-acculturated Latina (OR = 7.97; 95% CI = 2.43, 26.20) and high-acculturated Latina (OR = 4.48; 95% CI = 1.09, 18.45) women were significantly more likely than White and African American women to have family making the treatment decision. Women who felt efficacious in their ability to communicate with surgeons were less likely to have the family as the final decision-maker (OR = 0.95; 95% CI = 0.91, 0.99). Women whose surgeons had a participatory decision-making style were less likely to have the family as the final decision-maker (OR = 0.98; 95% CI = 0.97, 0.997). Family decision-making was associated with lower odds of breast-conserving surgery (OR = 0.39; 95% CI = 0.18, 0.85). | ||
| Maly et al.32 | Breast cancer knowledge; treatment delay; type of treatment received | Interactive information giving was associated with greater odds of breast cancer knowledge (OR = 1.15; 95% CI = 1.03, 1.27) and breast-conserving surgery (OR = 1.18; 95% CI = 1.05, 1.31) and lower odds of treatment delay (OR = 0.81; 95% CI = 0.72, 0.91). |
| Phipps et al.34 | Patients’ decision-making role | Most patients (42%) reported shared decision-making, followed by patient-based decision-making (31%). Patients reporting shared decision-making had significantly lower religiosity than those reporting provider-based decision-making (P = .02) and minimally higher than those reporting patient-based decision-making (P = .28). |
| Steenland et al.35 | Type of treatment received | Provider communication: African American men were more likely to report communication difficulties with the provider than White men (OR = 3.95; 95% CI = 1.52, 10.30). Men who received no treatment were more likely to report poor communication with the provider than men who received treatment (OR = 5.77; 95% CI = 1.88, 11.46). |
| Provider recommendation: provider recommendation was inversely associated with surgery (OR = 0.25; 95% CI = 0.11, 0.60) and no treatment (OR = 0.16; 95% CI = 0.05, 0.52). | ||
| Spouse, family, and friend recommendation: spouse recommendation was not associated with any treatment. Other family or friend recommendation was positively associated with receiving no treatment (OR = 4.47; 95% CI = 1.45, 13.8) but was not associated with any other treatment choice. |
Note. CI = confidence interval; OR = odds ratio.
Women in all minority groups were significantly less satisfied than White women with their decisions and with the decision-making process. Relative to their White counterparts, low-acculturated Latina patients reported the highest dissatisfaction, with odds ratios ranging from 3.6 (95% confidence interval [CI] = 2.9, 6.9]) to 5.5 (95% CI = 2.9, 10.5), and highest decisional regret (odds ratio [OR] = 4.1; 95% CI = 2.2, 8.0), followed by high-acculturated Latina patients (dissatisfaction OR range = 1.3 [95% CI = 1.0, 1.9] to 3.8 [95% CI = 1.6, 5.1]; regret OR = 2.0 [95% CI = 1.2, 3.7]) and African American patients (dissatisfaction OR range = 2.1 [95% CI = 1.3, 3.4] to 2.2 [95% CI = 1.7, 3.9]; regret OR = 1.8 [95% CI = 1.1, 3.0]).28,30
Two quantitative studies specifically examined conflict or alignment between patients’ preferred decisional role and their actual decisional role.28,31 Most respondents (69%–93%) reported a match between their actual and preferred level of decisional involvement, although low-acculturated Latina women were more likely to report too little involvement. Women whose decision-making role matched their preferences had the highest satisfaction with treatment received, the highest satisfaction with decision-making process, and the lowest decisional regret. By contrast, women whose decision-making role was less or more than they preferred were at increased risk of treatment dissatisfaction (OR range = 1.5–2.6; P < .005), decision-making process dissatisfaction (OR range = 2.5–3.2; P < .001), and high decisional regret (OR range = 1.7–2.4; P < .001).31
Qualitative studies indicated cultural variation in the adoption of different decision-making models and offered some explanatory insights (Table 4). High-acculturated Asian American women preferred a more active decisional role, believing that active engagement was necessary to ensure that the provider presented all treatment options.36 A study of low-acculturated Punjabi women reported low decisional involvement, insufficient information about treatments, and a lack of full engagement in the decision-making process.39 Many (though not all) low-acculturated Chinese and Korean American cancer patients preferred a provider-based decision-making model.36 Another study concurred that Chinese American women reported discomfort with the multiple treatment options presented. They felt it indicated a lack of authority and expertise and they tried to interpret the “real” recommendation.41 Although 1 study found that the majority of Latina and African American cancer patients preferred a significant amount of provider involvement in decision-making, overall, these populations reported feeling disempowered in the decision-making process.42,43,45,46 They expressed the need for more information, empowerment to self-advocate, and physicians’ respect for patients’ autonomy. In a study of Haredi Ashkenazi Jewish women, respondents reported that, although they preferred a rabbi-as-agent model similar to the provider-based decision-making model, they struggled with the consequences and benefits of delegating their decision to an authority figure.38 One study of African American women with breast cancer found that lack of participation in decision-making led many of them to reject chemotherapy.43 Thus, the sense of disempowerment from poorly aligned decision-making preferences and roles could sometimes result in nonadherence to cancer treatment.
TABLE 4—
Summarization of Findings on Shared Decision-Making From the Qualitative Literature
| Article | Research Question | Main Findings for Decision-Making |
| Ashing et al.36 | What are the cultural and socio-ecological factors that influence the breast cancer experience of Chinese, Korean, and “mixed” Asian American women? | Health care professionals’ perspective: Asian American patients (1) exhibited passivity in decision-making and fatalism toward their cancer; (2) tended to rely on word-of-mouth over provider recommendations. |
| Patients’ perspective: less-acculturated patients depended on the provider for treatment decisions because of the provider’s authority. More acculturated women preferred a more active decisional role. Attitudes (concern about burdening the family, sexual health, concern for cost of treatment) influenced treatment decision-making. | ||
| Balneaves et al.37 | What are the experiences and responses of the family members of immigrant Punjabi women diagnosed with breast cancer? | The accepted cultural norm is nondisclosure of a cancer diagnosis to the community and in some cases to the patient. Family advocated for women in the clinical encounter, had to be assertive with providers, and helped with language barriers. |
| Coleman-Brueckheimer et al.38 | To what extent and in what way do Haredi rabbinical authorities participate in breast cancer treatment decision-making? | Involving a rabbi in the decision-making process provided cultural meaning and relieved guilt and blame, but carried the risk of a binding decision. Involving a culture broker in the decision-making was considered advantageous because of high levels of trust in the broker, the broker’s experience interacting with the medical world, and nonbinding decisions, but patients were concerned about confidentiality and gender role conflicts. |
| Howard et al.39 | What are the experiences of Punjabi women with breast cancer, as described by their personal narratives? | Many patients reported following the providers’ treatment advice without question. For some women, family’s decisions took precedence over their own preferences. The women were focused more on the collective, rather than the individual, experiences of breast cancer. However, they felt that they were not given enough information and did not feel fully engaged in the decision-making process. |
| Jones et al.40 | What are the cultural beliefs and attitudes of African American prostate cancer survivors regarding the use of complementary alternative medicine? | Spirituality played a significant role in treatment decision-making for patients who used complementary alternative medicine. Almost all of the men believed that prayer helped to fight again prostate cancer, but none thought that prayer by itself would be sufficient. They believed that God works through health care providers. Trust in providers and in their knowledge was very important for treatment decision-making. Patients reported that changing cultural beliefs have changed treatment decision-making intergenerationally. |
| Killoran and Moyer41 | What are the cultural factors that influence the treatment decision-making by Chinese American patients and the presentation of treatment options by providers? | There was a cultural belief that vanity is dangerous and therefore mastectomy is safer than breast-conserving therapy, which was considered vain. Family, friends, and community reinforced these beliefs among the patients, affecting treatment decision-making and regret. |
| Patient–provider miscommunication: patients felt in conflict with the provider’s decision because the provider did not respect their choice for mastectomy, their fears, and their beliefs. This resulted in a loss of faith in provider, dissatisfaction with treatment, or uncertainty regarding treatment choice, and consideration of nonadherence. | ||
| Provider presentation of treatment: triangulation of multiple data sources showed that providers did not use the mandated handbook on treatment options correctly. Providers conveyed more bias in the discussion of treatment options than they realized. There was a wide variation in providers’ opinions and presentation of options. There was also wide variation in providers’ views about Asian American patients and how to present information to them, including using the family as a guide for nondisclosure. Patients felt uncomfortable with being presented multiple options, thinking that it indicated a lack of authority and expertise. | ||
| Kreling et al.42 | What are older breast cancer patients’ attitudes toward chemotherapy, and what factors influenced their treatment decision-making? | Most patients reported a provider-based decision-making style, which they preferred. Decision-making for chemotherapy was promoted by (1) tailored communication, which included family members; (2) provision of support services for women without support networks; and (3) culturally sensitive provider communication. |
| Latina women faced barriers to chemotherapy use that included employment, insurance, and language issues. They felt little empowerment to seek information. African American women reported that class and education were important determinants of how providers treated them and that they had to be advocates for themselves to be treated well. African American women tended to keep their diagnosis secret, resulting in lack of support from the community. | ||
| Nápoles-Springer et al.43 | How do understanding of ductal carcinoma in situ diagnosis, treatment decision-making processes, and satisfaction with care compare between Latina and White women? | Understanding diagnosis, prognosis, and treatment: White women had a greater understanding of diagnosis, prognosis, and treatment than Latina women. Low-acculturated Latina women wanted more information about surgical treatment. |
| Treatment decision-making process: most White women reported shared decision-making and were more likely to report patient-based decision-making than Latina women. Latina women reported equal occurrence of shared decision-making and provider-based decision-making, and were more likely than White women to report provider-based decision-making. Significant factors affecting decision-making were friends’ and others’ prior experiences, fear of recurrence, and providers’ recommendation. Less-cited factors included attitudes about the procedure, spiritual beliefs, and cost. The factors did not differ by ethnicity. | ||
| Treatment and decisional role satisfaction: patients were satisfied with their lack of decisional involvement and with their treatment decisions when providers’ rationale for the decision was explained clearly and when patients believed themselves to be well informed. Patients were dissatisfied with their lack of involvement if they did not know the other treatment options or providers’ rationale. Patients were dissatisfied with their treatment if they perceived that the providers were unable to commit to a specific treatment recommendation. | ||
| Sheppard et al.45 | What are the key perceptions, enablers, and nurturers that influence African American women’s breast cancer adjuvant therapy decisions? | A common theme was cultural identity and the importance of empowering African American women with information to self-advocate during the decision-making process. Negative perceptions of breast cancer treatment were based primarily on the observation of others receiving treatment. Non–African American providers more often reported their patients as fatalistic. Strong spiritual beliefs were not a primary decision-making resource for these women. |
| Patients were less confident in treatment decisions if they reported poor communication with their providers. Good communication was associated with treatment satisfaction, treatment knowledge, and use of recommended adjuvant treatment. Lack of decision-making participation, passivity in the interaction with providers, and limited questioning led several women to reject chemotherapy. Collectivism, family, the faith community, and others played important roles. | ||
| Sheppard et al.44 | What are the factors that influence Latinas’' factors that influence Latina’ breast cancer treatment decision-making? | Women needed better communication with providers and more information about the disease and treatment in Spanish. The family played a significant decisional role for Latina women. Factors that affected treatment decision-making included for following: positive provider–patient interactions, knowledge of diagnosis and treatment options, self-efficacy in decision-making, low communication skills or language barriers, cancer fatalism, and cultural incongruence with the providers. Patients reported not enough time for decision-making. |
| Williams et al.46 | What are the perceptions of communication and decision-making with providers among African American patients living with cancer and their families? | Provider–patient communication and quality of life: Participants stressed the importance of effective provider–patient communication for quality of life, including recognizing the patient’s individuality and tailoring communication. |
| Decision-making: effective communication, a sense of control (i.e., desire for shared decision-making), and providers’ respect for patients’ autonomy was important for effective decision-making. Respondents noted that not all patients have the capacity to self-advocate because of old age, poverty, or low education. | ||
| Zhang and Siminoff47 | What are the major differences of opinion between patients and family members while making treatment decisions, and why do they exist? | African American families exerted limited pressure on providers. By contrast, White families disagreed with providers on many issues, with or without patients’ concurrence. No African American patients switched doctors. In contrast, 38% of White patients switched doctors and more than 66% were persuaded by caregivers to do so. African American patients and caregivers reported following providers’ recommendations closely and relying heavily on their faith in God. Family discordance in treatment decision-making was common (not stratified by race). |
Patient Factors
Patient factors that influenced the cancer treatment decision-making process were primarily focused on attitudes and deeply held beliefs, as well as tangible aspects of a marginalized social status. The dominant subthemes within patient factors included level of acculturation or language issues, spirituality and fatalism, attitudes about treatment and decision-making, and self-efficacy. We investigated socioeconomic status (SES) as a potential subtheme, but the limited literature did not enable an in-depth investigation of the effect of SES indicators on the decision-making process among racial/ethnic minority patients. One study of African American patients reported similar decisional involvement by SES status, although the small sample size (n = 26) limited the conclusions that could be drawn from the findings.34
Level of acculturation and language issues.
Six quantitative studies included an analytic component to investigate differences in decision-making by minority patients’ level of acculturation and preferred language.26–30,33 Five of the studies investigated decision-making differences between low-acculturated and high-acculturated Latina breast cancer patients.27–30,33 As detailed previously, investigators found statistically significant differences in decision-making, decision-making outcomes, and decision-making factors by acculturation and language. For example, compared with low-acculturated Latina patients, more high-acculturated patients reported patient-based decision-making and fewer reported provider-based decision-making.27,28 Low-acculturated patients tended to be least satisfied with their decision-making role and outcome. One potential explanatory mechanism for these differences by level of acculturation was the need for translation in clinical encounters. In 1 study, only 6% of high-acculturated Latina patients reported needing translation in the clinical encounter, compared with 89% of low-acculturated Latina patients.28 A doctor or staff member translated for 52% of low-acculturated patients, and 36% reported translation by family or friends. The final study examined the role of low acculturation in nondisclosure of diagnosis among minority patients in Singapore,26 and by extension deferment of decision-making to family members. Not speaking English was associated with 7.6 greater odds (95% CI = 1.7, 34.5; P = .009) of nondisclosure of diagnosis among Chinese, Malay, and other minority patients in Singapore.
Spirituality and fatalism.
A single quantitative study34 among African Americans explored intrinsic religiosity, defined as the degree to which participants believe that they have internalized, and live in accordance with, their religious principles. In this study, patients who shared decision-making had lower average religiosity scores than those who reported physician-based decision-making (mean score = 13.5 and 14.7 units, respectively; P = .02).
Several qualitative studies explicated the role of patient spirituality or “faith in God” in cancer treatment decision-making.36,40,43,45,47 Spirituality was cited repeatedly as both a coping mechanism and a factor in the decision-making process. Spirituality was a particularly strong coping mechanism among African Americans.40,45 Specifically, spirituality played a strong role in having faith in the providers, strengthening the relationship with providers, and following the providers’ recommendations for treatment. In these studies, prayer was not viewed as a sufficient treatment option by itself.40,45 For several minority groups, spirituality may have limited patients’ role in decision-making by causing them to put their trust in their providers and in their religious faith; alternatively, highly spiritual patients may have had a psychosocial characteristic that also stimulated a high level of faith in their providers. For example, in a study of low-acculturated Asian Americans, providers reported that patients were more passive in treatment decision-making.36 According to their providers, these patients often viewed their cancer diagnosis and treatment outcome as part of “God’s will” and relied heavily on prayer, which limited their active participation in decision-making.
Attitudes about treatment and decision-making.
Three quantitative studies explored the impact of patients’ attitudes about treatment and decision-making on the decisional process, with mixed findings.27,29,34 One study of African American men and women found that patients held strong supportive attitudes for autonomy in information seeking, but not autonomy in decision-making.34 Patients with higher educational levels had stronger supportive attitudes for autonomy in information seeking and decision-making, but attitudes were similar across income level. Concerns about recurrence, survival, and radiation were self-reported as the most significant attitudinal factors influencing treatment decision-making for Latina, African American, and White women.27,29 One study of breast cancer patients27 found that, compared with low-acculturated Latina and White women, significantly more African American and high-acculturated Latina women reported concerns about recurrence (61.4%–64.1% vs 55.6%–55.8% of patients; P for overall trend = .044) and body image (22.3%–25.3% vs 17.2%–19.8%; P for overall trend = .01) as important factors in decision-making. Significantly fewer White women reported radiation concerns as a major decisional influence than low-acculturated Latina, high-acculturated Latina, and African American women (17.2% vs 26.8%–30.9%; P for overall trend < .001). Another study29 found that, although concerns about survival and radiation did not significantly differ between groups, low-acculturated Latina women rated concerns about appearance (i.e., body image; P ≤ .001), surgical consequences (P ≤ .001), and cost (P ≤ .001) as greater decisional influences than did high-acculturated Latina and White women.
Four qualitative studies explored the theme of patients’ attitudes in treatment and treatment decision-making in greater detail. Many of the factors or concerns around decision-making were in direct conflict, thereby heightening patients’ anxiety.36,38,43,44 For example, a study with low-acculturated Korean and Chinese American patients and high-acculturated Asian American patients found that adopting a “positive attitude” played a central role in treatment and treatment decision-making for Korean patients and for highly acculturated patients.36 The highly acculturated group defined a positive attitude as taking an active decisional role, whereas the Korean group viewed it as deferring to the provider in decision-making. Concurrent with the desire to adopt or display a positive attitude were concerns about pain and suffering (Korean and high-acculturated Asian American patients), public displays of suffering (Koreans), and survival (Chinese and high-acculturated Asian Americans). In studies of Latina women with breast cancer, fear of chemotherapy and side effects was a significant factor in treatment decision-making,44 concurrent with deep fears of recurrence (presumably reduced by use of chemotherapy).43
Self-efficacy.
Two quantitative studies with similar study populations examined patients’ self-efficacy in communication with surgeons as a factor in cancer treatment decision-making.32,33 In 1 study, White, Latina, and African American women who felt efficacious in their ability to communicate with their surgeons had lower odds of deferring the final treatment decision to family members (OR = 0.95; 95% CI = 0.91, 0.99; P = .009) than women who did not feel efficacious.32 The other study found no association between self-efficacy and cancer knowledge or treatment outcomes across White, Latina, and African American women.33 Neither reported the distribution of self-efficacy scores across racial/ethnic groups. A qualitative study of Latina breast cancer patients44 indicated that self-efficacy in making decisions and communicating with providers was a key theme discussed in the focus groups.
Factors Regarding Family and Important Others
Family and important others played a role in the cancer treatment decision-making process. The dominant subthemes within this level of factors included participation and advocacy in decision-making, impact of participation and advocacy on receipt of treatment, consequences of ceding decision-making autonomy to important others, and the experiences of important others.
Participation and advocacy of important others in decision-making.
Six quantitative studies examined the role of family and important others in the clinical encounter in general and decision-making specifically.26–29,33,35 Types of family and important others differed by study, including all companions, spouse or partner, family, and friends. A general trend existed for family and others playing an important role for low-acculturated Latina women and a smaller role for African American and White women. Two studies found that most women (70%–79% overall) had a companion present at their consultation with the provider.27,28 African American women had a lower frequency of accompaniment (71.2%) than either low-acculturated and high-acculturated Latina women or White women (77.5%–79.2%; P for overall trend = .032).27
The importance of companion types in decision-making and the decision role they played differed significantly by race/ethnicity. High-acculturated Latina women (59.3%) were more likely to indicate that their spouse or partner played an important role in decision-making than low-acculturated Latina women (54.3%), White women (51.6%), and African American women (44.5%; P for overall trend = .015).27 Despite the apparent importance of spouse or partner in decision-making, another study found that no high-acculturated Latina women and very few low-acculturated Latina women (4.2%) or African American women (3.0%) identified the spouse or partner as the final treatment decision-maker (P for group differences = .19).33 Family and friends appeared to play a more significant role than spouses or partners in decision-making, especially among low-acculturated Latina patients.27,29,33 Low-acculturated Latina women were much more likely to report family (75.9%) and friends (45.4%) as important in decision-making than African American women (50.3% and 25.6%, respectively), high-acculturated Latina women (49.4% and 18.2%), and White women (34.1% and 13.7%; P for overall trend < .001).27 Moreover, significantly more low-acculturated Latina women identified family or friend as the final decision-maker (49.3%) than African American women (3.0%), high-acculturated Latina women (17.9%), and White women (2.2%; P for group differences < .001).33 A study of Asian patients in Singapore found that a “family-centered” decision-making model was most important to this population.26
Only 1 study adjusted for potential confounders to study the role of important stakeholders outside the patient–provider dyad in minority patient cancer treatment decision-making.33 Adjusting for demographic and clinical factors, patients’ self-efficacy, social support, and providers’ participatory style, the authors found that both low-acculturated Latina women (OR = 7.97; 95% CI = 2.43, 26.20) and high-acculturated Latina women (OR = 4.48; 95% CI = 1.09, 18.45) were significantly more likely than White and African American women to have family making the cancer treatment decision. Women who felt efficacious in their ability to communicate with surgeons (OR = 0.95; 95% CI = 0.91, 0.99) and whose surgeons had a participatory decision-making style (OR = 0.98; 95% CI = 0.97, 0.997) were less likely to have the family as the final decision-maker.
Participation and advocacy of others and receipt of treatment.
Six quantitative studies examined the impact of a companion’s presence and decision-making participation on treatment-related outcomes, with mixed results.26–29,33,35 One study found that a companion’s presence at the decision-making clinical encounter was associated with lower decision dissatisfaction among cancer patients (OR = 0.65; 95% CI = 0.44, 0.96), but not regret (OR = 0.72; 95% CI = 0.43, 1.1).28 A companion’s presence was positively associated with receipt of mastectomy (relative risk [RR] = 1.62; 95% CI = 1.14, 2.21), whereas a strong spousal decision-making role was negatively associated with mastectomy (RR = 0.53; 95% CI = 0.36, 0.78).27 The spousal role was not associated with any treatment of prostate cancer.35 Interactions between others’ decision-making role and race/ethnicity were not reported in the studies.
Consequences of ceding decision-making autonomy.
Eight qualitative studies explored nuances and consequences of the role of family and other important stakeholders outside the patient–provider dyad in decision-making. For racial and ethnic minority cancer patients, family members were important advocates in the clinical encounter and provided social and decisional support, facilitated communication with providers, and helped overcome language barriers.37–39,41,42,44,45 Family members commonly had a substantial impact on treatment decision-making and outcomes,37,39,41,42,44,45 and in some cases impeded receipt of treatment42,45 or requested nondisclosure of diagnosis to the patient.37 In several studies, the treatment preferences of family and others dominated patients’ preferences, specifically with Chinese, Punjabi, and Haredi Ashkenazi patients.38,39,41 For the most part, deferring to others’ decisions for their cancer treatment appeared to give patients more satisfaction with treatment and the decision-making process, whereas opposing others’ recommendations or preferences could lead to decisional regret.38,39,41 However, a number of patients also expressed anxiety or regret associated with leaving the decision up to others, particularly when the treatment preferences of the patients and others were conflicted.38,41
Vicarious experiences.
In addition to directly affecting treatment decision-making through decisional participation and recommendations, family, friends, and other important stakeholders indirectly influenced patients’ cancer treatment decision-making through their personal experiences with cancer. In 1 small quantitative study of prostate cancer treatment among African American men, patients were more likely to choose brachytherapy because they had friends who had received this treatment (OR = 2.04; P ≤ .1).35
Three qualitative studies investigated the theme of others’ cancer experiences and treatment decision-making with African American prostate cancer patients,40 Latina and White breast cancer patients,43 and African American breast cancer patients.45 Prior experiences of friends and family43 as well as cancer survivor mentors45 substantially influenced decision-making about treatments and sometimes engendered a fatalistic attitude toward treatment. Similarly, vicarious experiences were cited as reasons for the use of complementary and alternative medical cancer treatments,40 sometimes without the knowledge of the biomedical provider.
Community Factors
In addition to main partners, family, friends, and other important stakeholders, the patients’ community played both positive and negative roles in the cancer treatment decision-making process. Studies used the term “community” to describe a variety of types of groups of individuals, including the faith community, neighborhoods, cancer survivors, and an unspecified “community.” The dominant subthemes included cultural and community norms and values, communication with the community, and decision-making as a collective process.
Cultural and community norms and values.
One way through which the community influenced the decision-making process was the formation and communication of collective norms and values, which was explored in 5 qualitative studies.37,38,40,41,45 Cultural norms and values actively shaped which treatment to receive for Chinese American and Haredi breast cancer patients in 2 studies.38,41 Many Chinese American breast cancer patients reported cultural pressure to receive modified radical mastectomy instead of breast-conserving surgery, even if the former procedure was not medically required, because breast-conserving surgery was seen as “vain” and oncologically less safe.41 The desire to adhere to religious law figured prominently in Haredi breast cancer patients’ decisions about what treatment to receive and when to receive it.38 Moreover, rabbis and cultural brokers served as sources of information for cultural norms and values for treatment decision-making and, for some patients, made the treatment decision. Among these women, concerns about guilt, blame, and confidentiality and fears about a binding and disagreeable treatment decision were important in identifying which, if any, religious authority figure they would defer their treatment decision-making to.38 A study of African American men found that increased formal education compared with previous generations and changing cultural norms about medical treatment resulted in a new preference for allopathic medicine over root and folk medicine to treat cancer.40
In addition to influencing which treatments to receive, cultural norms shaped disclosure and others’ involvement. The cultural norm of collectivism—defined as a social, communal way of living characterized by mutual obligations and expectations within groups—played a positive role through the support and involvement of family and the faith community.45 However, it could also play an adverse role if family involvement was negative, leading to treatment delay and limited disclosure of the condition to the family.
Communication with the community.
Four qualitative studies explored communication with the community during the cancer treatment decision-making process in minority populations.36,37,42,45 Fear of stigmatization influenced many patients not to disclose their cancer diagnosis to the community, which resulted in lack of community support.37,45 Many breast cancer patients reported little or no communication about their diagnosis and treatment with their neighbors36; however, communication with the community of cancer survivors was viewed as important.45
Decision-making as a collective experience.
For Punjabi and African American breast cancer patients, the cancer diagnosis and treatment decision-making was viewed as a collective experience shared with their family, but most Punjabi and some African American patients kept the diagnosis secret from the community to avoid stigmatization.37,45 Because of their desire to adhere to Jewish law, Haredi breast cancer patients viewed treatment decision-making and the treatment experience as a collective experience shared within their religious community.38
Provider Factors
Providers’ preferences and recommendations.
Five large surveys confirm that providers’ recommendations were the most important positive influence on treatment decision-making overall.29–31,35,48 Conversely, the perceived absence of providers’ advocacy of a particular treatment was associated with reduced uptake of that treatment. In some studies, the strength of the provider’s advocacy varied by the patient’s ethnicity. For example, among breast cancer patients who had breast-conserving therapy but did not undergo radiation therapy, 67% of low-acculturated Latina patients, 69% of high-acculturated Latina patients, and 57% of White patients reported lack of provider recommendation as the reason.29 Compared with a recommendation that radiation was optional, providers’ indication that radiation was necessary was significantly associated with receipt of radiation therapy (OR = 8.05; 95% CI = 4.04, 16.03). Providers’ indication that it was unnecessary (or no indication) was significantly associated with nonreceipt of radiation (OR = 0.09; 95% CI = 0.04, 0.19). In another large survey, racial differences in the operation type appeared to be related to perceived communication content.30 Compared with Whites, African American breast cancer patients reported that surgeons placed less emphasis on breast-conserving therapy. These patients in turn were more likely to opt for mastectomy over breast-conserving therapy. Notably, abdicating the decision-making role to providers was also associated with the highest rates of decisional regret and dissatisfaction.31
Five qualitative studies underscored the perceived importance of displaying respect for the providers’ status as an authority figure across racial and ethnic groups.36,39,41,43,47 In a study of patients with advanced lung cancer, African American patients were more likely than Whites to follow providers’ recommendations even when in conflict with the family.47 The authors interpreted higher compliance among minority patients as a sign of reduced agency and fewer advocates within the hospital and health care system. Similarly, in studies of Asian women with breast cancer, patients often consented to the provider-recommended treatment even when it was in conflict with personal or community values.36,41
Provider communication and information giving.
Provider communication permeated nearly all aspects of the decision-making process. Three quantitative studies reported on dimensions of communication that went beyond simple information giving. Compared with White women with breast cancer, African American women in a population-based survey reported less optimal engagement from their surgeons about their desires and expectations for surgery, leading to more decisional uncertainty.30 These findings were confirmed and extended by another study of White, Latina, and African American women32 that found that interactive information giving on the part of the surgeon was associated with higher odds of knowledge (OR = 1.15; 95% CI = 1.03, 1.27), lower odds of delay in treatment (OR = 0.81; 95% CI = 0.72, 0.91), and higher odds of breast-conserving therapy (OR = 1.18; 95% CI = 1.05, 1.31). Racial/ethnic differences in knowledge and use of breast-conserving therapy disappeared after adjustment for provider communication style. Finally, a survey of African American and White men with prostate cancer35 found that African American men were 4 times more likely to report poor communication with their providers (OR = 3.95; 95% CI = 1.52, 10.30), and this in turn was highly associated with nonreceipt of treatment (OR = 5.77; 95% CI = 1.88, 11.46).
Eight qualitative studies explored the effect of provider communication on the cancer treatment decision-making process.36,39,41–46 Across studies, the theme of needing more provider time, individualized attention, and culturally sensitive communication was commonly iterated. Study participants indicated that provider-based decision-making was acceptable provided the providers’ rationale was clearly explained to them.43–45 Patients wanted informative communication that included both elicitation of their values and guidance for treatment.
Supportive communication from the provider was as important for treatment adherence as informative communication. In a study comparing Latina and White women with ductal carcinoma in situ, Latinas consistently reported more distress than White women, which was alleviated when providers were sensitive to their emotional needs.43 Participants were dissatisfied when providers did not provide supportive communication and highly appreciative when it was provided.36
Conflict and cultural congruence in the patient–provider relationship.
Three qualitative studies41,42,44 discussed conflict related to the presence or absence of cultural congruence (defined as cultural diversity, awareness, sensitivity, and competence) at the level of the health care provider.49 In some instances, the cultural focus was SES, as in a study of African American breast cancer patients who reported that class and education were important determinants in how providers treated them.42 They felt that they had to advocate in the clinical encounter to be treated well by the clinician. In other instances, language barriers contributed to culturally incongruent interactions. For example, Latina women reported that the lack of supportive communication, language barriers, and otherwise incongruent interactions made them fearful of asking questions and leaving the decision to the provider.44 Patients who perceived that providers did not respect their choices, fears, or beliefs lost faith in their providers and considered nonadherence to treatment recommendations.41
DISCUSSION
We reviewed a broad array of studies examining treatment decision-making among racial/ethnic minorities with cancer and found several commonalities across studies. Common themes fit into multiple categories, including treatment decision-making process, individual patient factors, factors related to family and important others, community factors, and provider factors. Thematic data overlapped categories substantially, indicating that individuals’ perceptions and preferences for medical decision-making cannot be authentically examined outside the context of family and community—and that this may be especially so among ethnic minority patients. In addition, the SDM process is operationalized during communication between the patient and the provider. Thus, the important linkages between themes were social support, communication, and cultural congruence.
Social Support
Social support was generally provided by spouse and family but could also include friends, community members, and members or leaders of a religious community. Although several studies noted that social support had the potential of reducing individual autonomy and contributing to nonreceipt of treatment, strong social support more commonly resulted in decision-making for more aggressive treatment. These findings are supported across other diseases50 and have been expanded by studies indicating that providers are more likely to recommend more aggressive treatment when they perceive strong social support.51,52 In fact, the presence of strong social support was associated robustly with improved cancer survival,53 suggesting that social support may be an appropriate area for intervention in a patient-centered approach to cancer care.
Communication
Among cancer patients, effective provider communication was associated with improved psychological outcomes (e.g., reduced anxiety, improved psychological adjustment to diagnosis), quality of life, and physiological functioning,14 as well as significantly increased adherence to treatment recommendations.54 Despite these benefits, we found that cancer patients continued to have high rates of unmet communication needs from their providers, and these unmet needs were amplified among racial/ethnic minority patients. Our findings are supported by the few studies conducted on provider communication with indigenous patients worldwide, which identify significant challenges and a high prevalence of miscommunication.19,21,55–57 Challenges to communication include different communication styles, different medical belief models, language barriers, lack of provider skills in cross-cultural communication, lack of patients’ control, lack of providers’ knowledge of indigenous culture and history, distrust of providers and the health care system, lack of a personal relationship between the provider and patient, and an alienating health care environment.21,55–58 Cultural values and norms among racial/ethnic minority populations may have a significant impact on patient–provider communication, which warrants further investigation.59
Cultural Congruence
We found that cultural congruence was primarily explored in terms of language among quantitative studies. Across studies, low-acculturated minority women reported less participation in and satisfaction with cancer treatment decision-making, which sometimes led to nonadherence to care. The qualitative studies were more likely to explore nuances of cultural competence and to offer examples of how providers might bridge cultural divides. Given that a culturally congruent approach to care has been associated with improved communication, less use of costly services (such as clinic vs emergency department), and better health outcomes,49 the case for understanding and strengthening cultural congruence among providers is strong. This is especially so among socially vulnerable minority patients, for whom family and community relationships are an important source of identity and support.
This systematic review was initially motivated by an inquiry into cancer treatment decision-making processes among AI/AN patients, but our search was limited by a dearth of relevant data. Although AI/AN groups have the lowest cancer rates among racial/ethnic minority populations in the United States, they also have the highest mortality and lowest 5-year survival rates after diagnosis.1,60,61 As with other racial/ethnic minority groups, differences in quality of treatment, delay in receipt of treatment, and lack of treatment likely play a significant role in cancer survival disparities,2,3,7,8,62 and enhancing the patient–provider relationship and satisfaction with the treatment plan may play an important role in addressing these disparities. In our experience, traditional models of SDM may be inappropriate to AI/AN communities.49,63 The community and family play significant roles in health care decision-making for AI/AN patients.20,21,55 Moreover, miscommunication between health care providers and indigenous populations is pervasive and often unrecognized, with negative consequences for the clinical encounter and treatment adherence.19 Incorporating cultural and individual preferences into the treatment decision-making process may substantially improve cross-cultural communication between providers and AI/AN patients. The SDM model should therefore be extended beyond the traditional patient–physician dyad, especially among AI/AN cancer patients.
Our review has limitations that must be noted. First, as with any systematic review, our search may have been subject to publication bias. To mitigate this, we used comprehensive search terms, searched several large databases linked to different disciplines in which the topic is studied, and carefully reviewed the reference lists of included publications. However, it is possible that important data may not have been published or that papers may have been missed. Second, we included studies with a broad variety of racial and ethnic minority patients, which certainly cannot represent the experiences or perspectives of a single group. However, with a broad search we can understand common experiences and themes in cancer treatment decision-making among all minority patients. Furthermore, the findings of our review are limited by the available literature. Most of the studies included in our review were on breast cancer, based in the United States, and conducted among African Americans, which may limit the generalizability of the findings to other cancer sites, countries, and racial and ethnic minority groups. Because our review was motivated by treatment decision-making in AI/AN populations, the model needs to be applied and further refined in this group to enhance utility.
In spite of these limitations, we believe that the synthesized data present a compelling need to expand the SDM model beyond the traditional patient–provider dyad to other significant stakeholders, including the family, social supporters, and the minority community. Decision aids for treatment and screening decisions have been found to improve the decision-making process,64 and further work is needed to develop such aids to include important stakeholders outside the patient–provider dyad. An extended, shared decision-making approach may be particularly appropriate among AI/ANs, who are at higher risk for nonadherence to cancer care and for cancer mortality than any other ethnic group in the United States. Although individual AI/ANs may choose not to reside on reservation lands or not to participate in tribal activities, AI/ANs who are more strongly affiliated with traditional native culture have been significantly less likely to be adherent to cancer-screening regimens.20,65,66 The sensitive inclusion of family members or tribal leaders in the cancer treatment decision process could facilitate communication and cultural congruence, and may ultimately have an impact on adherence to recommended cancer care.
Acknowledgments
E. L. Mead was supported by a National Institutes of Health National Research Service Award (T32 CA009314).
These data were presented in a substantially abbreviated poster format at the Academy Health Annual Research Meeting; June 24–26, 2012; Orlando, FL.
Human Participant Protection
No protocol approval was required because no human participants were involved.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 2.Caplan LS, May DS, Richardson LC. Time to diagnosis and treatment of breast cancer: results from the National Breast and Cervical Cancer Early Detection Program, 1991–1995. Am J Public Health. 2000;90(1):130–134. doi: 10.2105/ajph.90.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fesinmeyer MD, Goulart B, Blough DK, Buchwald D, Ramsey SD. Lung cancer histology, stage, treatment, and survival in American Indians and Alaska Natives and whites. Cancer. 2010;116(20):4810–4816. doi: 10.1002/cncr.25410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris AM, Billingsley KG, Hayanga AJ, Matthews B, Baldwin LM, Birkmeyer JD. Residual treatment disparities after oncology referral for rectal cancer. J Natl Cancer Inst. 2008;100(10):738–744. doi: 10.1093/jnci/djn396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris AM, Rhoads KF, Stain SC, Birkmeyer JD. Understanding racial disparities in cancer treatment and outcomes. J Am Coll Surg. 2010;211(1):105–113. doi: 10.1016/j.jamcollsurg.2010.02.051. [DOI] [PubMed] [Google Scholar]
- 6.Revels SL, Morris AM, Reddy RM, Akateh C, Wong SL. Racial disparities in esophageal cancer outcomes. Ann Surg Oncol. 2013;20(4):1136–1141. doi: 10.1245/s10434-012-2807-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94(5):334–357. doi: 10.1093/jnci/94.5.334. [DOI] [PubMed] [Google Scholar]
- 8.Wilson RT, Adams-Cameron M, Burhansstipanov L et al. Disparities in breast cancer treatment among American Indian, Hispanic and non-Hispanic white women enrolled in Medicare. J Health Care Poor Underserved. 2007;18(3):648–664. doi: 10.1353/hpu.2007.0071. [DOI] [PubMed] [Google Scholar]
- 9.Street RL, Jr, Voigt B. Patient participation in deciding breast cancer treatment and subsequent quality of life. Med Decis Making. 1997;17(3):298–306. doi: 10.1177/0272989X9701700306. [DOI] [PubMed] [Google Scholar]
- 10.Tattersall MH, Butow PN, Clayton JM. Insights from cancer patient communication research. Hematol Oncol Clin North Am. 2002;16(3):731–743. doi: 10.1016/s0889-8588(02)00022-9. [DOI] [PubMed] [Google Scholar]
- 11.Ashton CM, Haidet P, Paterniti DA et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18(2):146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saha S, Arbelaez JJ, Cooper LA. Patient–physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93(10):1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62(3):355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 14.Arora NK. Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med. 2003;57(5):791–806. doi: 10.1016/s0277-9536(02)00449-5. [DOI] [PubMed] [Google Scholar]
- 15.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 16.Joosten E, de Weert G, Sensky T, van der Staak C, de Jong C. Effect of shared decision-making on therapeutic alliance in addiction health care. Patient Prefer Adherence. 2008;2:277–285. doi: 10.2147/ppa.s4149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med. 2001;52(12):1865–1878. doi: 10.1016/s0277-9536(00)00303-8. [DOI] [PubMed] [Google Scholar]
- 18.Polacek GN, Ramos MC, Ferrer RL. Breast cancer disparities and decision-making among US women. Patient Educ Couns. 2007;65(2):158–165. doi: 10.1016/j.pec.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 19.Cass A, Lowell A, Christie M et al. Sharing the true stories: improving communication between Aboriginal patients and healthcare workers. Med J Aust. 2002;176(10):466–470. doi: 10.5694/j.1326-5377.2002.tb04517.x. [DOI] [PubMed] [Google Scholar]
- 20.Canales MK. Connecting to nativeness: the influence of women’s American Indian identity on their health-care decisions. Can J Nurs Res. 2004;36(4):18–44. [PubMed] [Google Scholar]
- 21.Kaufert JM, Putsch RW, Lavallee M. End-of-life decision making among Aboriginal Canadians: interpretation, mediation, and discord in the communication of “bad news.”. J Palliat Care. 1999;15(1):31–38. [PubMed] [Google Scholar]
- 22.Institute of Medicine. Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 23.Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy. 2005;10(1):45–53. doi: 10.1177/135581960501000110. [DOI] [PubMed] [Google Scholar]
- 25.Sandelowski M, Barroso J, Voils CI. Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Res Nurs Health. 2007;30(1):99–111. doi: 10.1002/nur.20176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Back MF, Huak CY. Family centered decision making and non-disclosure of diagnosis in a South East Asian oncology practice. Psychooncology. 2005;14(12):1052–1059. doi: 10.1002/pon.918. [DOI] [PubMed] [Google Scholar]
- 27.Hawley ST, Griggs JJ, Hamilton AS et al. Decision involvement and receipt of mastectomy ethnic minorly and ethnically diverse breast cancer patients. J Natl Cancer Inst. 2009;101(19):1337–1347. doi: 10.1093/jnci/djp271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hawley ST, Janz NK, Hamilton A et al. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Educ Couns. 2008;73(2):363–370. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaplan CP, Nápoles AM, Hwang ES et al. Selection of treatment among Latina and non-Latina white women with ductal carcinoma in situ. J Womens Health (Larchmt) 2011;20(2):215–223. doi: 10.1089/jwh.2010.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katz SJ, Lantz PM, Janz NK et al. Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol. 2005;23(24):5526–5533. doi: 10.1200/JCO.2005.06.217. [DOI] [PubMed] [Google Scholar]
- 31.Lantz PM, Janz NK, Fagerlin A et al. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res. 2005;40(3):745–767. doi: 10.1111/j.1475-6773.2005.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maly RC, Leake B, Silliman RA. Breast cancer treatment in older women: impact of the patient–physician interaction. J Am Geriatr Soc. 2004;52(7):1138–1145. doi: 10.1111/j.1532-5415.2004.52312.x. [DOI] [PubMed] [Google Scholar]
- 33.Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group difference in treatment decision-making and treatment received among older breast carcinoma patients. Cancer. 2006;106(4):957–965. doi: 10.1002/cncr.21680. [DOI] [PubMed] [Google Scholar]
- 34.Phipps E, Madison N, Polansky M, Tester W. The importance of patient participation in second-line chemotherapy decisions: perspectives of African-American patients. J Natl Med Assoc. 2008;100(12):1434–1440. doi: 10.1016/s0027-9684(15)31543-1. [DOI] [PubMed] [Google Scholar]
- 35.Steenland K, Goodman M, Liff J et al. The effect of race and rural residence on prostate cancer treatment choice among men in Georgia. Urology. 2011;77(3):581–587. doi: 10.1016/j.urology.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 36.Tam Ashing K, Padilla G, Tejero J, Kagawa-Singer M. Understanding the breast cancer experience of Asian American women. Psychooncology. 2003;12(1):38–58. doi: 10.1002/pon.632. [DOI] [PubMed] [Google Scholar]
- 37.Balneaves LG, Bottorff JL, Grewal SK, Naidu P, Johnson JL, Howard AF. Family support of immigrant Punjabi women with breast cancer. Fam Community Health. 2007;30(1):16–28. doi: 10.1097/00003727-200701000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Coleman-Brueckheimer K, Spitzer J, Koffman J. Involvement of rabbinic and communal authorities in decision-making by Haredi Jews in the UK with breast cancer: an interpretative phenomenological analysis. Soc Sci Med. 2009;68(2):323–333. doi: 10.1016/j.socscimed.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 39.Howard AF, Bottorff JL, Balneaves LG, Grewal SK. Punjabi immigrant women’s breast cancer stories. J Immigr Minor Health. 2007;9(4):269–279. doi: 10.1007/s10903-007-9044-z. [DOI] [PubMed] [Google Scholar]
- 40.Jones RA, Taylor AG, Bourguignon C et al. Complementary and alternative medicine modality use and beliefs among African American prostate cancer survivors. Oncol Nurs Forum. 2007;34(2):359–364. doi: 10.1188/07.ONF.359-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Killoran M, Moyer A. Surgical treatment preferences in Chinese-American women with early-stage breast cancer. Psychooncology. 2006;15(11):969–984. doi: 10.1002/pon.1032. [DOI] [PubMed] [Google Scholar]
- 42.Kreling B, Figueiredo MI, Sheppard VL, Mandelblatt JS. A qualitative study of factors affecting chemotherapy use in older women with breast cancer: barriers, promoters, and implications for intervention. Psychooncology. 2006;15(12):1065–1076. doi: 10.1002/pon.1042. [DOI] [PubMed] [Google Scholar]
- 43.Nápoles-Springer AM, Livaudais JC, Bloom J, Hwang S, Kaplan CP. Information exchange and decision making in the treatment of Latina and white women with ductal carcinoma in situ. J Psychosoc Oncol. 2007;25(4):19–36. doi: 10.1300/J077v25n04_02. [DOI] [PubMed] [Google Scholar]
- 44.Sheppard VB, Figueiredo M, Cañar J et al. Latina a Latina: developing a breast cancer decision support intervention. Psychooncology. 2008;17(4):383–391. doi: 10.1002/pon.1239. [DOI] [PubMed] [Google Scholar]
- 45.Sheppard VB, Williams KP, Harrison TM et al. Development of decision-support intervention for black women with breast cancer. Psychooncology. 2010;19(1):62–70. doi: 10.1002/pon.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams SW, Hanson LC, Boyd C et al. Communication, decision making, and cancer: what African Americans want physicians to know. J Palliat Med. 2008;11(9):1221–1226. doi: 10.1089/jpm.2008.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang AY, Siminoff LA. The role of the family in treatment decision making by patients with cancer. Oncol Nurs Forum. 2003;30(6):1022–1028. doi: 10.1188/03.ONF.1022-1028. [DOI] [PubMed] [Google Scholar]
- 48.Katz SJ, Lantz PM, Paredes Y et al. Breast cancer treatment experiences of Latinas in Los Angeles County. Am J Public Health. 2005;95(12):2225–2230. doi: 10.2105/AJPH.2004.057950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schim SM, Doorenbos A, Benkert R, Miller J. Culturally congruent care: putting the puzzle together. J Transcult Nurs. 2007;18(2):103–110. doi: 10.1177/1043659606298613. [DOI] [PubMed] [Google Scholar]
- 50.Waljee AK, Higgins PD, Waljee JF et al. Perceived and actual quality of life with ulcerative colitis: a comparison of medically and surgically treated patients. Am J Gastroenterol. 2011;106(4):794–799. doi: 10.1038/ajg.2011.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bogart LM, Kelly JA, Catz SL, Sosman JM. Impact of medical and nonmedical factors on physician decision making for HIV/AIDS antiretroviral treatment. J Acquir Immune Defic Syndr. 2000;23(5):396–404. doi: 10.1097/00126334-200004150-00006. [DOI] [PubMed] [Google Scholar]
- 52.Pini TM, Hawley ST, Li Y, Katz SJ, Griggs JJ. The influence of non-clinical patient factors on medical oncologists’ decisions to recommend breast cancer adjuvant chemotherapy. Breast Cancer Res Treat. 2012;134(2):867–874. doi: 10.1007/s10549-012-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kroenke CH, Quesenberry C, Kwan ML, Sweeney C, Castillo A, Caan BJ. Social networks, social support, and burden in relationships, and mortality after breast cancer diagnosis in the Life After Breast Cancer Epidemiology (LACE) study. Breast Cancer Res Treat. 2013;137(1):261–271. doi: 10.1007/s10549-012-2253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haskard-Zolnierek KB. Communication about patient pain in primary care: development of the Physician–Patient Communication about Pain scale (PCAP) Patient Educ Couns. 2012;86(1):33–40. doi: 10.1016/j.pec.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 55.Kelly L, Brown JB. Listening to native patients. Changes in physicians’ understanding and behaviour. Can Fam Physician. 2002;48:1645–1652. [PMC free article] [PubMed] [Google Scholar]
- 56.Shahid S, Finn LD, Thompson SC. Barriers to participation of Aboriginal people in cancer care: communication in the hospital setting. Med J Aust. 2009;190(10):574–579. doi: 10.5694/j.1326-5377.2009.tb02569.x. [DOI] [PubMed] [Google Scholar]
- 57.Towle A, Godolphin W, Alexander T. Doctor–patient communications in the Aboriginal community: towards the development of educational programs. Patient Educ Couns. 2006;62(3):340–346. doi: 10.1016/j.pec.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 58.Barton SS, Anderson N, Thommasen HV. The diabetes experiences of Aboriginal people living in a rural Canadian community. Aust J Rural Health. 2005;13(4):242–246. doi: 10.1111/j.1440-1584.2005.00709.x. [DOI] [PubMed] [Google Scholar]
- 59.Parker PA, Aaron J, Baile WF. Breast cancer: unique communication challenges and strategies to address them. Breast J. 2009;15(1):69–75. doi: 10.1111/j.1524-4741.2008.00673.x. [DOI] [PubMed] [Google Scholar]
- 60.Espey DK, Wu XC, Swan J et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110(10):2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 61.Smith CB, Bonomi M, Packer S, Wisnivesky JP. Disparities in lung cancer stage, treatment and survival among American Indians and Alaskan Natives. Lung Cancer. 2011;72(2):160–164. doi: 10.1016/j.lungcan.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 62.Petereit DG, Rogers D, Govern F et al. Increasing access to clinical cancer trials and emerging technologies for minority populations: the Native American Project. J Clin Oncol. 2004;22(22):4452–4455. doi: 10.1200/JCO.2004.01.119. [DOI] [PubMed] [Google Scholar]
- 63.Schim SM, Doorenbos AZ. A three-dimensional model of cultural congruence: framework for intervention. J Soc Work End Life Palliat Care. 2010;6(3–4):256–270. doi: 10.1080/15524256.2010.529023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stacey D, Kryworuchko J, Bennett C, Murray MA, Mullan S, Legare F. Decision coaching to prepare patients for making health decisions: a systematic review of decision coaching in trials of patient decision AIDS. Med Decis Making. 2012;32(3):E22–E33. doi: 10.1177/0272989X12443311. [DOI] [PubMed] [Google Scholar]
- 65.Haozous EA, Knobf MT. “All my tears were gone”: suffering and cancer pain in southwest American Indians. J Pain Symptom Manage. 2013;45(6):1050–1060. doi: 10.1016/j.jpainsymman.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]