Sir,
Gaucher disease is the most common lysosomal storage disease with an estimated incidence of 1/57 000.1 It results from a deficiency in β-glucocerebrosidase and accumulation of glucosylceramide. Typically patients develop hepatosplenomegaly and osseous manifestations. Neuronopathic involvement is less common, but ocular manifestations including oculmotor apraxia and supranuclear gaze abnormalities are usual in Types II and III. Intraocular manifestations including corneal clouding and retinal lesions have also been reported.2, 3 However, little is known about their natural progression.
Case report
We describe the progression of retinal lesions over a 5-year period in a French-Canadian girl born to non-consanguineous parents and diagnosed with Gaucher disease Type III at 21 months of age after presenting with hepatosplenomegaly and recurrent infections. Investigations revealed anaemia, thrombocytopenia and elevated acid phosphatase. The diagnosis was confirmed by low glucocerebrosidase activity. Genetic testing revealed homozygosity for the L444P mutation commonly associated with Type III disease. Treatment with Imiglucerase 60 Units/kg every other week was started.
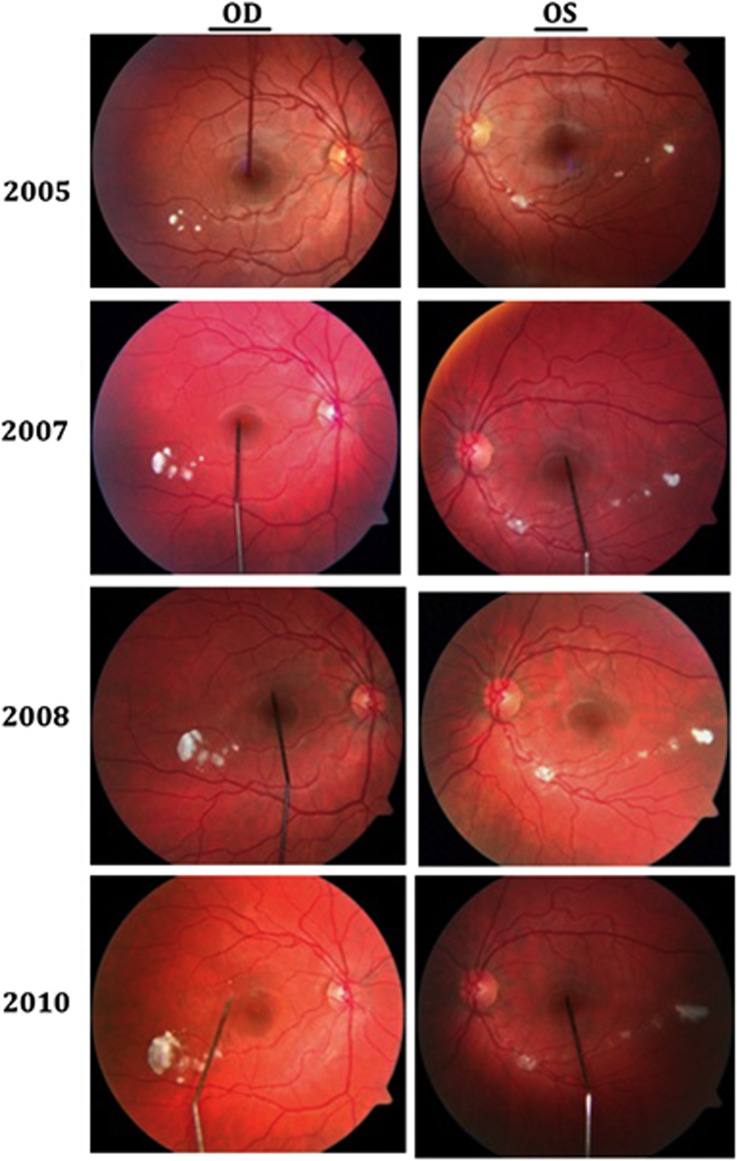
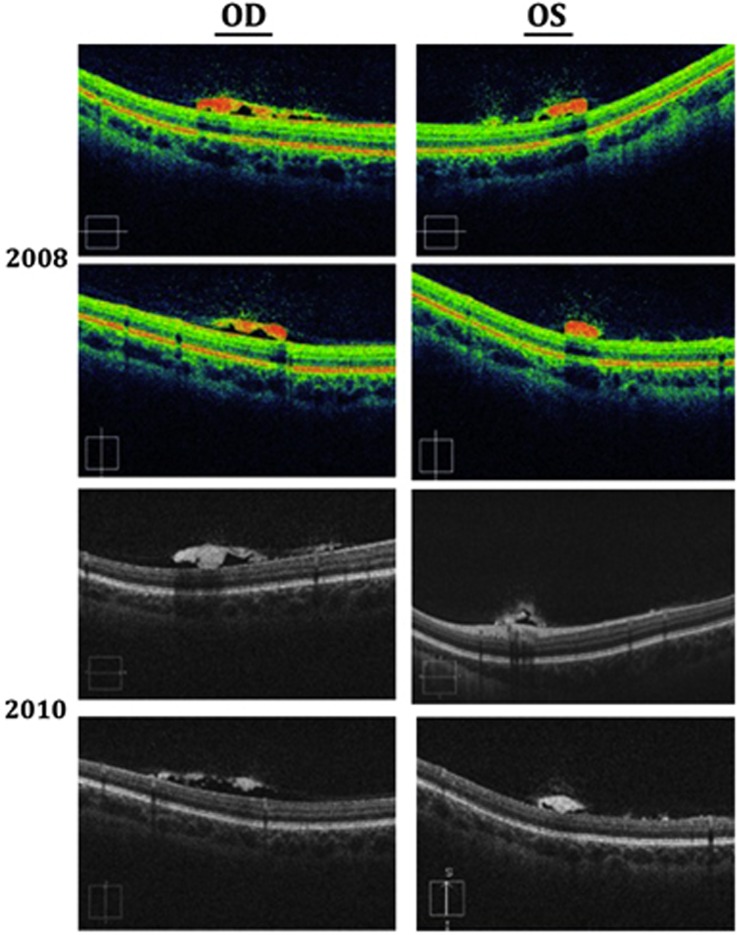
At first her neurological examination was normal but slowing of horizontal saccades was noted at the age of 5 years. Fundoscopy revealed white globular lesions OU at the age of 13 years in 2005, which were confirmed to be pre-retinal on OCT (Figures 1 and 2). Subsequent annual visits showed slow increase in size more pronounced in OD. Visual acuity remained stable at 20/20 OU and there were no changes in electroretinography patterns.
Figure 1.
OU fundus photos between 2005 and 2010.
Figure 2.
OU OCT in 2008 and 2010.
Comment
Retinal lesions have been infrequently reported in Gaucher patients and were thought to represent the eponymous Gaucher cells: pathognomonic macrophages distended with sphingolipid forming a ‘crumpled silk' appearance.3, 4, 5 The pathophysiology of the retinal Gaucher cells is yet to be explained, but the accumulation of higher levels of circulating glucosylceramide in unusual systemic locations has been suggested as causal.5 Progression over time was only reported by Stark6 who described chalk-white spots of varying sizes mainly located peripherally without foveal interference. In our case, the reported lesions did not shrink despite glucocerebrosidase replacement possibly explaining the immune-privilege enjoyed by the eye, which prevents such large proteins from crossing the blood–brain barrier. Although our patient had normal acuity and ERG findings, Seidova et al5 reported pre-retinal lesions and subclinical abnormalities on one ERG recording, which was attributed to the accumulation of storage lipid in glial cells. We believe that our patient's visual acuity was not affected because the reported lesions spared the fovea. Further studies will help to shed light on the precise nature of the retinal lesions seen in Gaucher disease.
The authors declare no conflict of interest.
References
- Meikle PJ, Hopwood JJ, Clague AE, Carey WF. Prevalence of lysosomal storage disorders. JAMA. 1999;281 (3:249–254. doi: 10.1001/jama.281.3.249. [DOI] [PubMed] [Google Scholar]
- Abrahamov A, Elstein D, Gross-Tsur V, Farber B, Glaser Y, Hadas-Halpern I, et al. Gaucher's disease variant characterised by progressive calcification of heart valves and unique genotype. Lancet. 1995;346 (8981:1000–1003. doi: 10.1016/s0140-6736(95)91688-1. [DOI] [PubMed] [Google Scholar]
- Cogan DG, Chu FC, Gittinger J, Tychsen L. Fundal abnormalities of Gaucher's disease. Arch Ophthalmol. 1980;98 (12:2202–2203. doi: 10.1001/archopht.1980.01020041054010. [DOI] [PubMed] [Google Scholar]
- Petrohelos M, Tricoulis D, Kotsiras I, Vouzoukos A. Ocular manifestations of Gaucher's disease. Am J Ophthalmol. 1975;80 (6:1006–1010. doi: 10.1016/0002-9394(75)90329-3. [DOI] [PubMed] [Google Scholar]
- Seidova SF, Kotliar K, Foerger F, Klopfer M, Lanzl I. Functional retinal changes in Gaucher disease. Doc Ophthalmol. 2009;118 (2:151–154. doi: 10.1007/s10633-008-9142-9. [DOI] [PubMed] [Google Scholar]
- Stark H. [Eye changes in Gaucher's disease] Klin Monbl Augenheilkd. 1983;183 (3:216–220. doi: 10.1055/s-2008-1054908. [DOI] [PubMed] [Google Scholar]