Abstract
Health care organizations are continually challenged with improving the safety of and the quality of care delivered to patients. Research studies often bring to the forefront interventions that health care organizations may choose to institute in an effort to provide evidence-based, quality care. Rapid response teams are one such intervention. Rapid response teams were introduced by the Institute for Healthcare Improvement as part of their “100,000 Lives” Campaign. Rapid response teams are one initiative health care organizations can implement in an effort to improve the quality of care delivered to patients. This article uses Donabedian’s model of structure, process, and outcomes to discuss the United States health care systems, rapid response teams, and the outcomes of rapid response teams. National and organizational policy implications associated with rapid response teams are discussed and recommendations made for future research.
Keywords: rapid response teams, quality of care, Donabedian, health care policy, patient outcomes
The Institute for Healthcare Improvement introduced rapid response teams (RRTs) as an intervention that health care organizations (HCOs) can implement in an effort to decrease patient mortality and improve patient safety. The need for improving the United States health care system is evident in the literature (Chassin, Galvin, & the National Roundtable on Health Care Quality, 1998). For example, in-hospital costs associated with CPR alone is estimated to cost the health care industry US $1 billion annually (Garretson, Rauzi, Meister, & Schuster, 2006). Therefore, initiatives aimed at decreasing the number of in-hospital cardiac arrests that require CPR may play an important role in decreasing the cost of health care. These initiatives may also decrease in-hospital mortality rates and improve patient safety.
The Institute for Healthcare Improvement introduced RRTs as part of its 100,000 Lives Campaign in an effort to reduce mortality and morbidity (Saver, 2006). The Institute for Healthcare Improvement (IHI; 2007) argued that RRTs might enable organizations the opportunity to decrease the number of in-hospital deaths and cardiac arrests, which, in turn, improve patient care and decrease health care costs. Implementation of RRTs changes how care is provided to patients who become critically ill in medical and surgical units and are in need of immediate intervention. These changes in the process of care are ultimately aimed at improving the outcomes of care (i.e., decreased cardiac arrests and mortality rates). Evidence of a statistically significant relationship between RRTs and improved patient outcomes, such as mortality rates and reduced length of stay, may enhance quality of care delivered to patients and decrease health care costs associated with CPR.
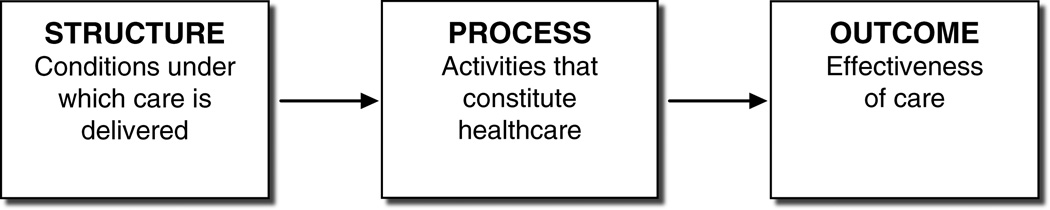
Donabedian’s model of structure, process, and outcomes (Figure 1) is well-known to HCOs and useful for studying the conditions under which care is delivered (structure), monitoring the activities that constitute health care (process), and assessing the effectiveness (outcomes) of health care (Jonas, Goldsteen, & Goldsteen, 2007). This framework may serve as a guide for evaluating how a change in the process of care, such as the implementation of RRTs, may require a change in the structures within which care is delivered (i.e., United States health care systems or individual HCOs). A change in the process of care may also be expected to influence the subsequent outcomes of care within these structures.
Figure 1.
Donabedian’s conceptual framework to evaluate the quality of medical care.
Note. From “Evaluating the Quality of Health Care,” by A. Donabedian, 1966. The Milbank Memorial Fund Quarterly, 16.
The purpose of this article is to discuss the introduction of RRTs by HCOs as a quality improvement initiative and the policy implications associated with these teams using Donabedian’s model as a framework.
LITERATURE REVIEW
Structure of Care: U.S. Health Care Systems
The U.S. health care systems may be generally characterized as highly decentralized and fragmented (Jonas et al., 2007). The health care systems consist of government, private for-profit, and private not-for-profit organizations. These organizations face enormous challenges to provide quality patient care in the face of rapidly escalating health care costs, increased numbers of uninsured people, sicker hospital inpatients, and difficult managed-care directives demanding shorter lengths of stay. The United States spends 16% of its GDP on health care. That’s double the medical spending of other industrialized countries. Yet, despite the large amounts of money spent, the relative quality of care delivered is questionable (Schoen, Davis, How, & Schoenbaum, 2006).
The Institute of Medicine report To Err is Human: Building a Safer Health System (Kohn, Corrigan, & Donaldson, 1999) highlights the costliness of problems such as increased hospital stay and decreased patient satisfaction, and it recommended strategies to improve patient safety. A subsequent report, Crossing the Quality Chasm (Briere, 2001), focused on the quality of care in the U.S. health care system. Six aims were suggested to improvement: Health care should be safe, effective, patient-centered, timely, efficient, and equitable. These, and subsequent reports by the Institute of Medicine, formed the launch pad for HCOs to reevaluate the quality of care delivered to patients.
National organizations such as the National Quality Forum, Leapfrog, the Joint Commission (until June 2007 known as the Joint Commission of Accreditation of Healthcare Organizations), and the Institute for Healthcare Improvement have instituted processes to provide HCOs with tools to improve the delivery of care and subsequent patient outcomes. The National Quality Forum is a non-profit organization that focuses on the development of national strategies to measure health care quality and report outcomes of care. Leapfrog is a coalition of public and private organizations and major corporations that rewards HCOs for advances in patient safety and quality of care. It also assists the public in making informed decisions on choosing hospitals to provide the care they need. The Joint Commission is a national hospital accrediting body that contributes to the health care quality arena through the development and enforcement of national patient safety goals as part of their accreditation program. The Institute for Healthcare Improvement was founded in 1991 as a non-profit organization with a focus on innovation at the bedside (Grimes, Thornell, Clark, & Viney, 2007). The Institute for Healthcare Improvement introduced RRTs as part of its 100,000 Lives Campaign that consisted of six strategic measures to reduce mortality and morbidity (Saver, 2006) and in turn improve patient safety and the quality of care delivered to patients. This initiative followed on the heels of the Institute of Medicine report, Crossing the Quality Chasm (Briere, 2001), which highlighted the status of patients’ safety and the quality of care delivered in the United States. It argued that the health care delivery system does not effectively translate knowledge into practice leading to care that is inconsistent and lacks in quality. It is hoped that evidence of a statistically significant relationship between RRTs and improved patient outcomes, such as mortality rates and reduced length of stay, may lead to an increase in the adoption of RRTs by HCOs. That, in turn, may enhance the quality of care delivered to patients in the United States.
Within the framework of Donabedian’s model, the deployment of RRTs provides HCOs with an opportunity to change the processes of care in an organization with the goal to improve outcomes of care.
Process of Care: RRTs
Although originally from Australia, RRTs have also been implemented in United Kingdom and United States (Garretson et al., 2006). RRTs involve providers, usually some combination of critical care staff physicians, nurses, and/or respiratory therapists, that come to the bedside of a potentially deteriorating patient with the goal of intervening and preventing progression to cardiac and/or respiratory arrest (Winters & Dorman, 2006). It is known that patients who progress to cardiac arrest usually display symptoms of deterioration up to 6 hours before a cardiopulmonary arrest (Garretson et al., 2006). The assumption underlying RRTs is that if medical intervention occurs during the time of physiological instability, progression to cardiac and/or respiratory arrest can often be prevented with a subsequent reduction in mortality rates (Winters, Pham, & Pronovost, 2006).
RRTs are also known as medical emergency teams (Bellomo et al., 2004; Braithwaite et al., 2004) and as critical care outreach teams (DeVita, Braithwaite, Mahidhara, Foraida, & Simmons, 2004). Medical emergency teams, critical care outreach teams, and RRTs are conceptualized as a group of experts responding to a medical emergency prior to cardiopulmonary arrest. This distinguishes the RRTs from code teams who respond when cardiopulmonary arrest has already occurred. For this paper the term RRT will be used.
Several RRT staffing models exist: (a) RRTs are staffed by an intensive care unit (ICU) physician, an ICU registered nurse, and a respiratory therapist, (b) an ICU registered nurse and a respiratory therapist, or (c) an ICU registered nurse alone. Although the staffing model most often seen in the literature is that of an ICU physician and ICU registered nurse, further research is necessary to determine which staffing model yields the best patient outcomes. The scope of RRT practice within hospitals is usually limited to medical-surgical units because the underlying concept of the team is to bring intensive care resources (staff and equipment) to the patient’s bedside.
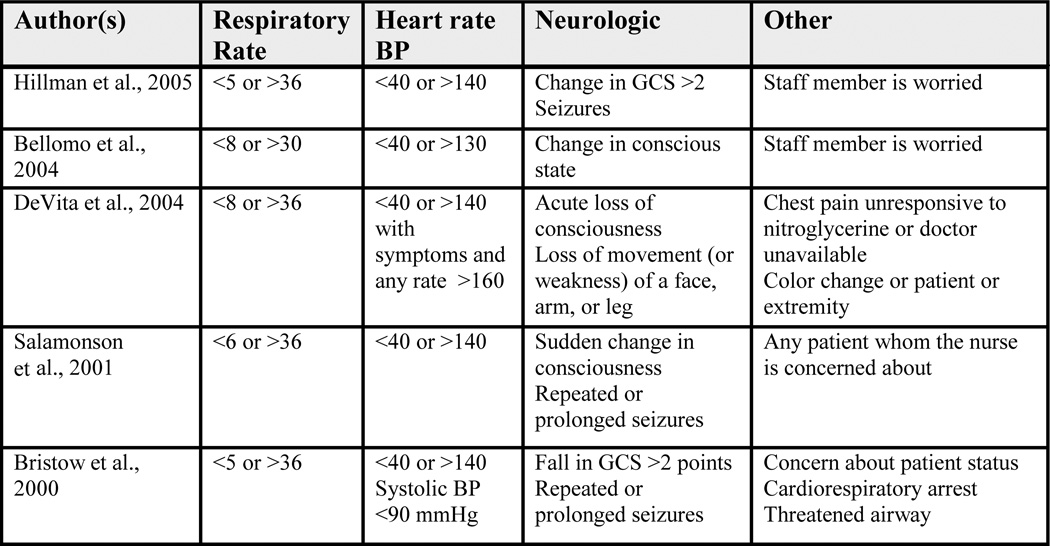
When a patient meets objective or subjective calling criteria, RRTs are activated by nurses. Many HCOs have instituted specific objective RRT calling criteria (see Figure 2). Research indicates that hospital staff is more inclined to call the RRT in the presence of clearly established calling criteria (DeVita et al., 2006). However, it must be noted that in most cases, RRT calling criteria include subjective measures such as “any patient you are seriously worried about” (Hillman et al., 2005, p. 2092) or “any patient whom you are concerned about” (Salamonson, Kariyawasam, Van Heere, & O’Connor, 2001, p. 141). Including subjective measures as part of calling criteria allows staff the opportunity to call the team even when objective signs and symptoms of deterioration are absent. A recent study on RRT calling criteria indicated that respiratory rate, heart rate, systolic blood pressure, and level of consciousness were the best predictors of patients at risk for cardiac arrest, unplanned ICU admission, or unexpected death (Cretikos et al., 2007). Although these criteria had high specificity, the sensitivity and positive predictive value remained relatively low. This finding underscores the need for further research on RRTs and the calling criteria used to activate these teams and the standardization of calling criteria across organizations.
Figure 2.
Rapid response team calling criteria.
Note. Heart rate is per minute; GCS = Glasgow Coma Scale.
Outcomes of Care: The Effectiveness of RRTs
The Institute for Healthcare Improvement’s 100,000 Lives Campaign measures the effectiveness of RRTs as “lives saved.” This is calculated as the difference between the number of expected deaths (the number that would have occurred had no improvements been made) and the number of actual hospital deaths during the campaign period (IHI, 2007). To date, the Institute for Healthcare Improvement has estimated that 122,300 lives were saved in an 18-month period (May 2004–June 2006; IHI, 2007).
Research studies examining the relationship between RRTs and patient outcomes have used several outcome measures. Those most frequently measured include cardiac arrest, in-hospital death, and unplanned ICU admission (Bristow et al., 2000; Hillman et al., 2005; Kenward, Castle, Hodgetts, & Shaikh, 2004; Salamonson et al., 2001). Other outcomes studied include the relationship between RRTs and medical errors (diagnostic, treatment, or preventive errors) (Braithwaite et al., 2004) and also RRTs and adverse events (acute myocardial infarction, pulmonary embolism, respiratory failure, stroke, and severe sepsis) (Bellomo et al., 2004).
Research results on RRTs and subsequent outcomes are conflicting. The Institute for Healthcare Improvement cited several studies that showed a significant relationship between RRTs and (a) reduced non-ICU arrests, (b) reduced postoperative emergency ICU transfers and deaths, (c) a reduction in arrests prior to ICU transfer, and (d) a decrease in the incidence of cardiopulmonary arrests (IHI, 2007). A quasi-experimental study by Bellomo and colleagues (2004) that looked at RRTs and associated outcomes of the surgical patient population of a large (>400 beds) teaching hospital in Australia was able to demonstrate a reduction in postoperative adverse events, deaths, and emergency ICU admission. Buist and colleagues (2002) were also able to demonstrate an associated reduction in the incidence of unexpected cardiac deaths and mortality rates.
However, several other studies have been unable to demonstrate significant relationship between RRTs and unexpected deaths, cardiopulmonary arrests, and death without a prior Do Not Resuscitate (DNR) order (Bristow et al., 2000; DeVita et al., 2004; Hillman et al., 2005; Jolley, Holaday, Lonbardozzi, & Harmon, 2007; Jones et al., 2007; Kenward et al., 2004; Salamonson et al., 2001). The only Institute for Healthcare Improvement reported outcome supported by these studies is the relationship between RRTs and unanticipated ICU admissions.
Several possibilities exist as to why research on RRTs and patient outcomes show conflicting results. Although most of the studies were consistent in their conceptualization of RRTs, they were inconsistent in staffing models and calling criteria. Furthermore, study designs selected were most often quasi-experimental designs that lacked randomization. This limits the generalizability of the findings. The context in which these studies occurred is also very different, further limiting generalizability: Some studies occurred in teaching hospitals (Australia) whereas others were in public hospitals (United Kingdom). Other issues related to internal and external validity can be raised, but those issues fall outside the scope of this paper. However, the inconsistency of findings indicates the need for standardization of concepts and terms along with further research to bring clarity to the function and effectiveness of RRTs.
One study by Jones and colleagues (2007) found that patient mortality rates and cardiac arrests decreased after hospital staff training on RRTs but prior to implementation of the team. This indicates that staff training and development itself influenced patient outcomes. Therefore, one can argue that RRT implementation raised nurses’ awareness of the clinical signs and symptoms of patient physiological deterioration leading to an increase in RRT calls (novelty effects). It also underscores the value of hospital staff training and development and its subsequent role in patient outcomes.
The implementation of RRTs and their influence on organizational outcomes such as patient satisfaction, cost of care, employee satisfaction, and employee turnover have not yet been studied. Anecdotal evidence suggests that the presence of RRTs improves communication between care providers and increases employee satisfaction (Simmons, 2004; Duncan, 2005). However, further research is necessary to evaluate the relationship between organizational outcomes and implementation of RRTs.
POLICY IMPLICATIONS AND FUTURE RESEARCH
The Adoption of RRTs
Many HCOs have deployed RRTs despite the limitations and conflicting findings of research studies on their effectiveness. The Institute for Healthcare Improvement estimate that 3,100 hospitals have joined the 100,000 Lives Campaign. Of these hospitals, roughly 60% have deployed RRTs.
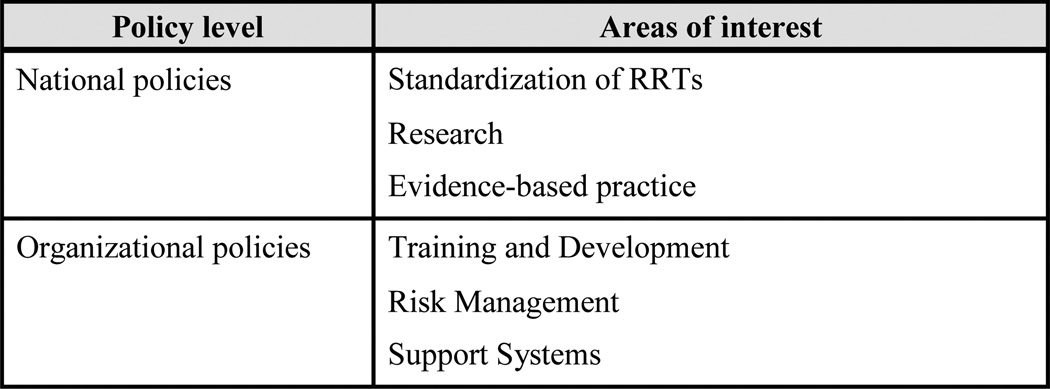
The Joint Commission, responsible for the accreditation of HCOs, has added the development of a “method that enables health care staff members to directly request additional assistance from a specially trained individual(s) when the patient’s condition appears to be worsening” (Joint Commission, 2008) to their National Patient Safety Goals. Although they do not explicitly call for RRTs, it is clear that the concept behind the National Patient Safety Goals is the universal establishment of RRTs within the health care setting. HCOs have until January 2009 to implement this national patient safety goal. Given that hospitals have to comply with the National Patient Safety Goals for accreditation purposes, widespread adoption and integration of RRTs is a virtual certainty. But, the adoption of RRTs and the limited evidence associated with RRTs has significant implications for policymakers on an organizational and national level (see Figure 3).
Figure 3.
National and organizational policy implications.
Note. RRT = rapid response team.
National Policies: Standardization, Research Studies, and Evidence-Based Practice
Standardization
One of the largest issues in research and practice surrounding RRTs is their lack of standardization (DeVita et al., 2006). RRTs are consistently conceptualized as a team of experts who come to the bedside of a potentially deteriorating patient. However, how RRTs are implemented, the staffing model used, the calling criteria, the training and development of hospital staff prior to implementation, and what exactly the team will do during the intervention differ between organizations. These differences restrict the ability of practitioners to determine the best methods to implementing RRTs as well as drawing conclusions on their reported outcomes.
However, with the endorsement of the Institute for Healthcare Improvement and the Joint Commission, RRTs will be widely adopted within the next year. Given this “push” for adoption but lack of standardization, one strategy will be for national organizations like the Joint Commission, the Institute for Healthcare Improvement, and the Agency for Healthcare Research and Quality to establish policies that will increase funding for future research on RRTs. Studies that examine the staffing models, calling criteria, outcomes to be measured, and staff education and training to produce the best patient outcomes (e.g., decrease cardiac arrests and in-hospital mortality) may lead to better results in the U.S. health care system as a whole. Combined with a successful standardization of RRT practices, this may be able to significantly improve upon the currently limited positive outcomes observed in individual hospitals.
Research Studies
While a limited number of studies on RRTs were conducted in the United States, the majority of studies have been done in Australia and in the United Kingdom. More U.S. research studies are necessary due to the possibility that hospitals in Australia and the United Kingdom may differ significantly from American hospitals in the context within which care is provided as well as processes used to provide it. More U.S.–based research will enhance our understanding of RRTs and how they function in the U.S. health care system and the best practices and protocols for their implementation.
The majority of research studies on RRTs and patient outcomes use a quasi-experimental pre–post research design. Though studies on RRTs can be strengthened by using experimental research designs, it may be considered unethical to conduct since it will require withholding care from patients (the control group) that are in need of immediate intervention.
Should more research funding go towards RRTs given the limited evidence on their effectiveness? Given the Joint Commission’s National Patient Safety Goals requiring HCOs to adopt an initiative such as RRTs if they wish to acquire Joint Commission accreditation, the answer is a resounding “yes.” Research is necessary to establish “best practices” to enhance the function and outcomes of RRTs and to facilitate evidence-based practice. Without evidence-based practice, HCOs that adopt RRTs may approach the implementation of RRTs from a trial-anderror perspective. This would almost certainly lead to a waste of valuable resources such as time and money.
Proof of positive patient outcomes associated with RRTs may also have implications on future hospital reimbursement processes. For example, evidence suggests that the presence of RRTs in the HCO leads to a reduction in unanticipated ICU admissions. What if chart reviews of an ICU patient indicate that physiological signs of patient deterioration were present a few hours prior to cardiac and/or respiratory arrest? What if an RRT was not activated during the time of physiological instability prior to that patient’s admission to the ICU? Could the Center for Medicare and Medicaid Services and other health insurance companies refuse to reimburse hospitals for the unplanned ICU admission?
Evidence-Based Guidelines
The American Heart Association has developed guidelines for advanced cardiac life support that practitioners use in the event of a cardiac and/or respiratory arrest. Code teams that respond to the patient’s bedside after a cardiac and/or respiratory arrest use these guidelines to intervene and “rescue” the patient. Advanced cardiac life support guidelines have been widely adopted in HCOs and are considered evidence-based practice.
The adoption and implementation of RRTs in HCOs may necessitate the development of guidelines similar to advanced cardiac life support to drive the practice of RRTs. One strategy may be for the American Heart Association to research and establish evidence-based RRT guidelines. The American Heart Association is well-respected in the field of basic and advanced life support measures. Therefore, RRT guidelines developed and supported by the American Heart Association could help to increase their adoption and possibly lead to standardization in RRT practices across HCOs.
Organizational Policies and Training and Development, Risk Management, and Support Systems
Training and Development
Organizational policies related to staff training and development are necessary for the successful implementation of RRTs. Anecdotal evidence suggests that hospital staff training and development, prior to the implementation of RRTs, plays an important role in their successful implementation (Garretson et al., 2006; Scholle & Mininni, 2006). The nature and quality of staff training and development programs can significantly enhance the function of RRTs within HCOs.
Nursing staff development departments can play a critical role in the education and training of nursing staff prior to the deployment of RRTs. Through ongoing education, they can assist the organization in maximizing the utilization of RRTs (Thomas, VanOyen, Rasmussen, Dodd, & Whildin, 2007). Orientation programs for incoming nurses (experienced and new graduates) to a HCO must train them on when to call the team and what their role is once the team arrives. If the American Heart Association establishes RRT guidelines similar to the currently well-established advanced cardiac life support guidelines and certification program, nursing staff development departments may need to provide nurses with the necessary training to achieve certification in those guidelines.
With the implementation of RRTs, continuing medical education departments need strategies to train medical staff on the utilization of RRTs and provide training for those physicians who would be on the teams. Medical schools and nursing schools would both need to adapt existing policies related to medical and nursing student education respectively to include training on the scope and utilization of RRTs.
Organizational policies that emphasize the importance of hospital staff training and continuing education on RRTs will help facilitate learning within the organization because these policies encourage mobilization of resources such as personnel, time, and equipment. Such policies will also create an organizational mandate for training that can serve as an incentive to motivate staff to attend RRT training sessions.
Another potential strategy is the adoption of human resource practices that will enhance team learning and education within a HCO. The success of RRTs is dependent on the HCO providing team members with training on the dynamics and processes of appropriate teamwork. Human resource policies and practices should focus on team-building activities to enhance the listening, communication, and conflict management skills of team members (Bolman & Deal, 2003). These skills will enhance teamwork and, ultimately, the team’s performance.
Risk Management
Risk management policies are also important for RRT implementation. Policies should establish reporting mechanisms and/or guidelines for hospital staff and RRTs when they are faced with quality improvement problems. These policies should clearly identify the role of the RRT in the identification of quality improvements within the RRT or with respect to the medical–surgical staff they relate with during a RRT call. Risk management policies should create a psychologically safe environment that encourages staff to identify potential quality improvement needs, either within the RRT or the medical–surgical unit, without fear of retribution. Error reporting should be encouraged through the adoption of organizational policies that shift the focus from blaming individuals and on to understanding the underlying organizational processes that lead to the errors.
Organizational policies should further establish guidelines for the reporting of RRT calls, events that occurred during the call, and outcomes associated with the call. Standardized RRT call report sheets, similar to “code” sheets, will facilitate the reporting of calls and the activities that encompass them (i.e., medication administration, vital signs observed, and physicians consulted). Consistency in data reporting within a HCO will enhance and expedite data collection processes for future research studies. Data consistency may also encourage HCO staff to conduct their own studies on RRTs and will help to guide the performance improvement efforts associated with RRTs within the organization.
Risk management policies should clearly establish the role of the RRT within organizations to mitigate the risks associated with the use of RRTs. Organizational policies should clearly indicate: the knowledge and skills required of RRT members; who is responsible for selecting team members; the scope of practice of the team; what the responsibility of the team is at the conclusion of the RRT call (e.g., report and feedback mechanisms, debriefing sessions); how the competency of team members will be evaluated and maintained; and how the performance of the team will be monitored and evaluated.
HCOs may choose to draw from ICU physicians and nurses to staff RRTs; however, redistribution of staff can have further risk management implications. For example, when ICU nurses are pulled away from their patients to respond to RRT calls, who will be responsible for the care of their patients? What is the associated risk of a unit functioning with a reduced number of staff during the RRT call? And how will the organization deal with such a reduction in staff in areas such as California that have mandated staffing levels?
Support Systems
Policies addressing support systems for RRTs and hospital staff must be present. RRTs can only be successful if they are provided with the necessary resources to function effectively (Bolman & Deal, 2003; Thomas et al., 2007). RRTs need ICU physicians, nurses, and/or respiratory therapists to staff them. Equipment, such as cardiac monitors and defibrillators, need to be readily available for use. And quick access to medications for emergent use must be present. Challenges abound. Will the RRT staff be a dedicated team or will they be “pulled” from the ICU at the time of a call? What support systems will be put in place to support a critical care unit that must function without a staff member during a RRT call?
Another support system shown to enhance the effectiveness of RRTs is the presence of the standardized communication technique SBAR (situation, background, assessment, recommendation) (Thomas et al., 2007). Communication failures are a significant cause of adverse events in health care (Dayton & Henriksen, 2007), and the implementation of SBAR or other standardized communication tools among the hospital staff may reduce these adverse events. The use of standardized communication processes, like SBAR, can improve communication between RRT members as well as between the RRT and the nursing staff who activated the call. These improvements may decrease the risk of errors during a RRT call. This, in turn, would likely improve the effectiveness of the RRT and the patient outcomes associated with the call.
RRTs: An Opportunity for Researchers and Clinicians
Despite conflicting evidence on RRT effectiveness, RRTs are here to stay. The lack of definitive evidence supporting this initiative, now adopted by organizations to improve patient outcomes in the clinical setting, provides an excellent opportunity for researchers and clinicians to work together. Clinicians who have worked with RRTs directly (e.g., staffing the team, calling the team) and indirectly (e.g., performance improvement and risk management departments) are excellent sources of information on RRTs. They are in an ideal position to provide anecdotal evidence of what has worked and what has not in the real life settings. The observations of clinical staff regarding RRTs may provide researchers with ideas for further research on these teams.
Researchers, on the other hand, should develop studies to evaluate the many different aspects of RRTs (e.g., calling criteria, staffing models, protocols for practice). They can work with clinicians to implement the findings of such studies and encourage evidence-based practice in the clinical setting.
CONCLUSION
RRTs were launched as an initiative by the Institute for Healthcare Improvement to decrease in-hospital deaths and cardiac arrests; however, there is not clear evidence of positive patient outcomes associated with RRT implementation. Yet, RRTs are being widely adopted in the United States, United Kingdom, and Australia. It is therefore prudent that policies at the national and organizational level are developed to assist hospital staff to deploy these teams in the best possible way to reach the best patient outcomes. Policies that address (a) standardization of RRTs, (b) funding for research, (c) development of evidence-based practice guidelines, (d) staff training and development, (e) risk management, and (f) support systems for RRTs are all necessary. The development of such policies will serve multiple important functions. They will safeguard the interest of patients by improving the quality of care and enhancing patient’s safety in HCOs. They will protect and serve hospital staff through the development of clear guidelines within which hospital staff and RRT members can function. And they will benefit the population at large if improved quality of care leads to a reduction in mortality and morbidity rates. They may even pave the way for a modest lessening of the overall cost of care.
Acknowledgments
I would like to thank Dr. Diane Kjervik, JD, RN, FAAN, Professor and Chair, Health Care Environments Division, School of Nursing, University of North Carolina at Chapel Hill and Dr. Julie Jacobson Vann, PhD, MS, RN, Clinical Assistant Professor, Health Care Systems, School of Nursing, University of North Carolina at Chapel Hill for their valuable input, support, and encouragement to me in submitting this manuscript for publication. I would also like to thank my advisor Dr. Cheryl Jones, PhD, RN, FAAN, for her support and encouragement. Lastly, thank you to the anonymous reviewers for their helpful insight and feedback. Partial funding was provided by the National Institute of Nursing Research, Grant number 5T32NR008856.
Biography
Biographical Data. Deonni Stolldorf is a third-year predoctoral fellow in health care quality and patient outcome in the School of Nursing at the University of North Carolina at Chapel Hill.
Footnotes
Copyright of Journal of Nursing Law is the Springer Publishing Company, Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
REFERENCES
- Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Critical Care Medicine. 2004;32(4):916–921. doi: 10.1097/01.ccm.0000119428.02968.9e. [DOI] [PubMed] [Google Scholar]
- Bolman LG, Deal TE. Reframing organizations: artistry, choice, and leadership. San Francisco: John Wiley & Sons; 2003. [Google Scholar]
- Braithwaite RS, DeVita MA, Mahidhara R, Simmons RL, Stuart S, Foraida M. Use of medical emergency team responses to detect medical errors. Quality and Safety in Health Care. 2004;13:255–259. doi: 10.1136/qshc.2003.009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere R. Institute of Medicine: Crossing the quality chasm. Washington DC: National Academy Press; 2001. [Google Scholar]
- Bristow PJ, Hillman KM, Chey T, Daffurn K, Jacques TC, Norman SL, et al. Rates of in-hospital arrests, deaths and intensive care admissions: The effect of a medical emergency team. The Medical Journal of Australia. 2000;173:236–240. doi: 10.5694/j.1326-5377.2000.tb125627.x. [DOI] [PubMed] [Google Scholar]
- Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospitals: preliminary study. British Medical Journal. 2002;324(7334):387–390. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin MR, Galvin RW the National Roundtable on Health Care Quality. The urgent need to improve health care quality. Journal of the American Medical Association. 1998;280:100–105. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- Cretikos M, Chen J, Hillman K, Bellomo R, Finfer S, Flabouris A. The objective medical emergency team activation criteria: A case-control study. Resuscitation. 2007;73:62–72. doi: 10.1016/j.resuscitation.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Dayton E, Henriksen K. Communication failure: Basic components, contributing factors, and the call for structure. Journal on Quality and Patient Safety. 2007;33(1):34–47. doi: 10.1016/s1553-7250(07)33005-5. [DOI] [PubMed] [Google Scholar]
- DeVita MA, Braithwaite RS, Mahidhara R, Foraida M, Simmons RL. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Quality and Safety in Health Care. 2004;13:251–254. doi: 10.1136/qshc.2003.006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Critical Care Medicine. 2006;34(9):2463–2478. doi: 10.1097/01.CCM.0000235743.38172.6E. [DOI] [PubMed] [Google Scholar]
- Donabedian A. Evaluating the quality of medical care. The Milbank Memorial Fund Quarterly. 1966;16(52):166–206. [PubMed] [Google Scholar]
- Garretson S, Rauzi MB, Meister J, Schuster J. Rapid response teams: A proactive strategy for improving patient care. Nursing Standard. 2006;21(9):35–40. doi: 10.7748/ns2006.11.21.9.35.c6408. [DOI] [PubMed] [Google Scholar]
- Grimes C, Thornell B, Clark AP, Viney M. Developing rapid response teams. Clinical Nurse Specialist. 2007;21(3):85–92. doi: 10.1097/00002800-200703000-00007. [DOI] [PubMed] [Google Scholar]
- Hillman K, Chen J, Cretikos M, Bellomo DB, Doig G, Flabouris A. Introduction of the medical emergency team system: A cluster-randomized controlled trial. The Lancet. 2005;365(9477):2091–2097. doi: 10.1016/S0140-6736(05)66733-5. [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. [Retrieved on October, 15, 2007];100K Lives Initiative: Some is not a number, soon is not a time. 2007 from http://www.ihi.org/IHI/Programs/Campaign/100kCampaignOverviewArchive.htm. [Google Scholar]
- The Joint Commission. [Retrieved on October, 29, 2008];National patient safety goals. 2008 from http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals. [Google Scholar]
- Jolley J, Holaday B, Lonbardozzi KAK, Harmon C. Rapid response teams: Do they make a difference? Dimensions of critical care nursing. 2007;26(6):253–260. doi: 10.1097/01.DCC.0000297401.67854.78. [DOI] [PubMed] [Google Scholar]
- Jonas S, Goldsteen RL, Goldsteen K. An introduction to the U.S. health care system. 6th ed. New York: Springer Publishing Company; 2007. [Google Scholar]
- Jones D, Opdam H, Egi M, Goldsmith D, Bates S, Gutteridge G, et al. Long-term effect of a medical emergency team on mortality in a teaching hospital. Resuscitation. 2007;74(2):235–241. doi: 10.1016/j.resuscitation.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation. 2004;61(3):257–263. doi: 10.1016/j.resuscitation.2004.01.021. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS. Institute of Medicine: To err is human. Washington, DC: National Academy Press; 1999. [Google Scholar]
- Salamonson Y, Kariyawasam A, van Heere B, O’Connor C. The evolutionary process of medical emergency team implementation: Reduction in unanticipated ICU transfers. Resuscitation. 2001;49(2):135–141. doi: 10.1016/s0300-9572(00)00353-1. [DOI] [PubMed] [Google Scholar]
- Saver C. Beyond expectations. Nursing Management. 2006;37(10):37–42. [PubMed] [Google Scholar]
- Schoen C, Davis K, How SKH, Schoenbaum SC. U.S. health system performance: A national scorecard. Health Affairs. 2006;25:w457–w475. doi: 10.1377/hlthaff.25.w457. [DOI] [PubMed] [Google Scholar]
- Scholle CC, Mininni NC. Best-practice interventions: How a rapid response team saves lives. Nursing. 2006;36(1):37–40. doi: 10.1097/00152193-200601000-00037. [DOI] [PubMed] [Google Scholar]
- Thomas K, VanOyen M, Rasmussen D, Dodd D, Whildin S. Rapid response teams: challenges, solutions, benefits. Critical Care Nurse. 2007;27(1):20–27. [PubMed] [Google Scholar]
- Winters B, Dorman T. Patient-safety and quality initiatives in the intensive care unit [Electronic version] Current Opinions in Anesthesiology. 2006;19:140–144. doi: 10.1097/01.aco.0000192769.94279.69. [DOI] [PubMed] [Google Scholar]
- Winters BD, Pham J, Pronovost PJ. Rapid response teams: Walk, don’t run. Journal of the American Medical Association. 2006;296(13):1645–1647. doi: 10.1001/jama.296.13.1645. [DOI] [PubMed] [Google Scholar]