Abstract
Stem cells have been successfully used for the treatment of critical limb ischemia (CLI). We conducted a clinical trial to determine the feasibility of using autologous adipose-derived mesenchymal stromal cells (AdMSCs) for the treatment of CLI. Unexpectedly, two diabetic patients developed peripheral microthrombosis. This adverse effect, which contrasts with the reported antithrombotic properties of MSCs, may stem from the diabetic environment that alters the fibrinolytic activity of AdMSCs, thereby increasing the probability of developing thrombosis. Here, we confirm this premise by demonstrating that diabetic AdMSCs cultured in the presence of blood sera expressed and released higher levels of plasminogen activator inhibitor type 1, reduced levels of tissue plasminogen activator, and lower d-dimer formation compared with nondiabetic AdMSCs. Thus, to establish an appropriate cell therapy for diabetic patients, we recommend including new preclinical safety tests, such as the d-dimer and/or the tissue plasminogen activator-to-plasminogen activator inhibitor type 1 ratio tests, to assess fibrinolytic activity of cells before implantation.
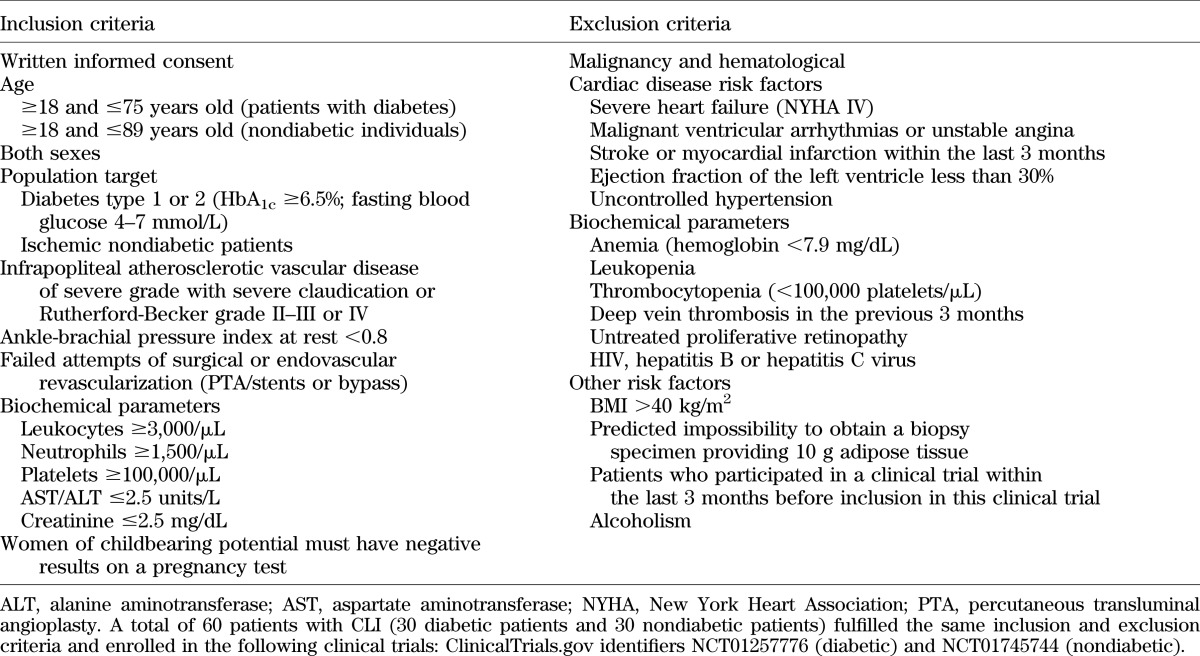
We evaluated the safety and feasibility of using autologous adipose-derived mesenchymal stromal cells (AdMSCs) for diabetic patients (ClinicalTrials.gov identifier: NCT01257776). Two diabetic patients developed distal microthrombosis (DMT) that was controlled with aggressive antithrombotic therapy. DMT was not detected when autologous AdMSCs isolated from nondiabetic patients were used (ClinicalTrials.gov identifier: NCT01745744) under identical conditions, as reported in Table 1, or when autologous bone marrow mononuclear cells (BMMNCs) were transplanted in diabetic patients with critical limb ischemia (CLI) (ClinicalTrials.gov identifier: NCT00872326) (1). Development of AdMSCs-associated DMT has not been previously reported and is in sharp contrast to the described fibrinolytic and antithrombogenic properties of MSCs (2–4). This novel clinical observation raises the possibility that the diabetic milieu of patients may alter the functional properties of AdMSCs, thereby impairing secretion of factors involved in fibrinolysis. To validate this premise, we evaluated whether AdMSCs isolated from diabetic and nondiabetic patients and cultured in the presence of healthy, diabetic, or nondiabetic blood sera displayed differential expression levels of tissue plasminogen activator (tPA) and plasminogen activator inhibitor type 1 (PAI-1), which may result in impaired fibrinolytic activity of AdMSCs derived from diabetic patients.
TABLE 1.
Clinical parameters and inclusion and exclusion criteria of diabetic and nondiabetic patients with CLI
RESEARCH DESIGN AND METHODS
Blood samples.
Human serum was from diabetic (hBS-D) and nondiabetic (hBS-ND) patients with CLI, as well as from healthy volunteers (hBS). All donors provided informed consent that was formerly approved by local and regional medical research ethics committees.
AdMSCs procurement.
AdMSCs were isolated from abdominal adipose tissue biopsy specimens of diabetic (AdMSC-D) and nondiabetic (AdMSC-ND) patients diagnosed with CLI and enrolled in two independent clinical trials (EudraCT: 2008-001387-88 and EudraCT: 2009-013554-32), as previously described (5). AdMSCs were cultured in Mesenchymal Stem Cell Basal Medium (MSCBM, Lonza, Barcelona, Spain) complemented with growth supplements (GS: MSCGM SingleQuots, Lonza), 100 units/mL penicillin-streptomycin, and incubated at 37°C in a 20% O2 and 5% CO2 humidified atmosphere. Control AdMSCs were purchased from ATCC.
Experimental setup.
AdMSCs, AdMSC-D, and AdMSC-ND were plated at a density of 5 × 104 cells/cm2. The following day, the media was replaced with serum/GS-free MSCBM (Lonza) and 24 h after with MSCBM (Lonza) supplemented with GS, hBS, hBS-D, or hBS-ND. Supernatants were collected for ELISA analysis and cells harvested for RNA extraction 24 h after sera addition.
Quantitative RT-PCR.
cDNA was generated from 2 μg RNA using M-MLV Reverse Transcriptase (Promega Biotech, Alcobendas, Spain). Primer sequences for tPA and PAI-1 were designed using Primer3 Software (http://frodo.wi.mit.edu/primer3/) and can be obtained upon request, whereas the housekeeping gene primers for cyclophilin A (PPIA) and 60S acidic ribosomal protein P0 (RPLP) were purchased from Tataabiocenter (Göteborg, Sweden). QT-PCR was performed using a SensiFAST SYBR Lo-ROX Mix (Bioline Reagents Ltd) and a 7500 Real-Time PCR System (Applied Biosystems). Three distinct amplifications were performed for each transcript, and the CT assay was applied to assess relative transcript levels of tPA and PAI-1.
tPA and PAI-1 secretion assay.
Levels of total tPA (free and complexed) and total PAI-1 (active complexed with tPA and latent inactive) secreted in the media of the various experimental groups were quantified using precoated ELISA plates (Bender MedSystems, Vienna, Austria) according to the manufacturer’s instructions.
Fibrin gel culture assay.
Fibrin gels were prepared as previously described (6). Subsequent to polymerization, 1 mL MSCBM without serum or with GS, hBS, hBS-D, or hBS-ND was added to the clotted fibrin gels. Medium was collected 24 h later for d-dimer detection using the Blue D-Dimer Kit (Teco, Neufahrn, Germany). Gels were fixed in formalin and processed for hematoxylin-eosin staining. The free-cell/area was quantified from four arbitrary images per slide per condition using ImageJ freeware.
Statistical analysis.
Unless otherwise stated, data are represented as mean values ± SEM. Data were analyzed with one-way and two-way ANOVA tests. The Tukey test was used for comparisons. Values of P ≤ 0.05 were considered statistically significant.
RESULTS
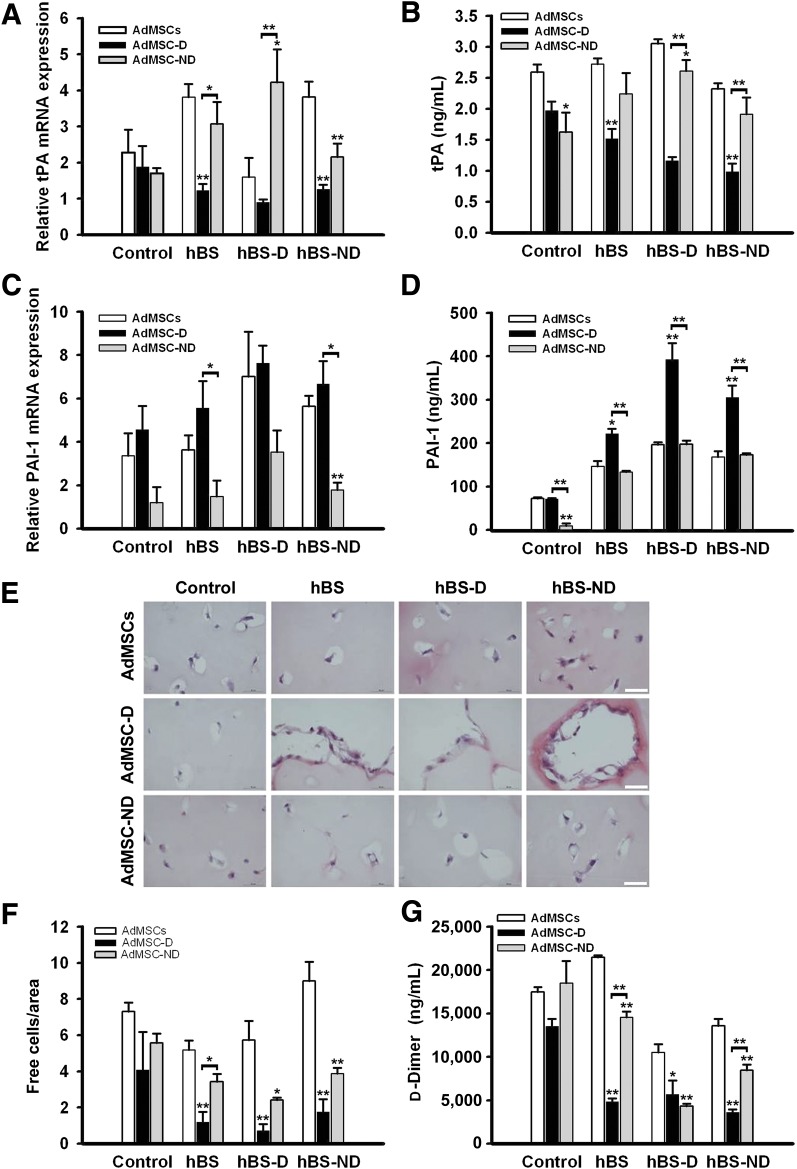
We initially assessed the relative transcript levels of the fibrinolytic promoting factor tPA as well as the amount of secreted protein in isolated AdMSCs, -D, and -ND cultured in the presence of GS (control), hBS, -D, and -ND. In the control condition, all three cell populations exhibited similar tPA mRNA expression levels. However, when cultured in media supplemented with blood sera (hBS, -D, and -ND), tPA transcript levels and secreted protein levels were significantly lower in AdMSC-D compared with AdMSCs and AdMSC-ND, suggesting that the addition of sera, independent of its origin, inhibited tPA expression in AdMSC-D (Fig. 1A and B).
FIG. 1.
AdMSCs derived from diabetic patients display reduced and serum-independent fibrinolytic activity. Expression analysis of tPA and PAI-1 I shown in AdMSCs isolated from AdMSCs, AdMSC-D, and AdMSC-ND and cultured in the presence of GS (control), hBS, hBS-D, and hBS-ND. Detection of tPA mRNA expression (A). tPA protein release shows that the blood sera, independent of its origin, inhibited tPA expression in AdMSC-D (B). PAI-1 mRNA expression (C). D: PAI-1 protein release. Note that AdMSC-D secreted the highest quantity of PAI-1. Relative mRNA expression indicates the ratio between specific gene and housekeeping genes. Values are normalized to the expression in no stimulated AdMSCs, which was arbitrarily set as 1. E: Hematoxylin and eosin staining shows AdMSCs-mediated lysis of the fibrin gel. The cell is surrounded by a clearing zone, except for AdMSC-D, which displays hampered capacity to degrade fibrin gel independently of human blood serum used. Scale bars: 50 µm. F: Free cell/area quantification from hematoxylin-eosin staining of arbitrary images. G: In quantification of d-dimer production of AdMSCs cultured in fibrin clot, AdMSC-D displayed blunted capacity to generate d-dimers independently of serum used. Data are presented as mean values ± SEM (n = 4). Statistical significance: *P ≤ 0.05, **P ≤ 0.01 for AdMSC-D compared with AdMSC-ND.
We next evaluated whether levels of PAI-1 were also altered in AdMSC-D compared with AdMSCs and AdMSC-ND. Overexpression of PAI-1 has been shown to potentially compromise normal fibrin clearance mechanisms and promote pathological fibrin deposition and thrombotic events (7,8). PAI-1 transcript levels were consistently higher in AdMSC-D than in AdMSC-ND in all culture conditions (Fig. 1C). Interestingly, AdMSCs exhibited a similar PAI-1 expression pattern as AdMSC-D. Nonetheless, at the protein levels, AdMSC-D secreted the highest quantity of PAI-1, reaching maximum levels in the presence of hBS-D (400 ng/mL), whereas AdMSCs and AdMSC-ND, independent of serum condition, released ∼150 to 200 ng/mL protein. In presence of GS (control), AdMSCs and AdMSC-D both secreted similar low levels, whereas AdMSC-ND released barely detectable amounts of PAI-1 (Fig. 1D).
We next measured the fibrinolytic activity of the various AdMSCs. Cells were embedded into fibrin clots to mimic an ex vivo fibrinolytic situation and cultured with GS or in the presence of blood sera (hBS, -D, and -ND). Fibrin degradation, as judged by a steady clearing zone surrounding single cells, was significantly hampered in AdMSC-D compared with AdMSCs or AdMSC-ND. This effect appeared to be independent of serum conditions (Fig. 1E and F). In contrast, AdMSCs diplayed the highest number of cell free/area, reaching maximum levels in the presence of hBS-ND. Interestingly, AdMSC-ND cultured in the presence of hBS-D produced significantly less cell free/area than cells cultured in hSB or hSB-ND (Fig. 1E and F). To validate this observation, we measured levels of d-dimer, a by-product of fibrin degradation (Fig. 1G). Consistent with lower cell free/area, AdMSC-D displayed blunted capacity to generate d-dimers, independent of the serum (Fig. 1G). Interestingly, d-dimer production from AdMSC-ND cultured in hBS-D was as low as from AdMSC-D, suggesting that blood derived from diabetic patients may also contain other factors that inhibit fibrinolysis without altering tPA and PAI-1 levels (Fig. 1B and D).
DISCUSSION
Our results clearly demonstrate that diabetic-derived AdMSCs have an altered phenotype indicating the existence of a potential post-transcriptional mechanism that regulates PAI-1 expression levels, typified by its increase resulting in blunted fibrinolytic activity. Exposing AdMSC-D to hBS or hBS-ND did not alter this phenotype, indicating that long-term fibrinolytic modifications have potentially been endowed that cannot be reverted under normal culture conditions. The latter may therefore impart increased susceptibility to develop DMT in patients who receive transplants of diabetic-derived AdMSCs. Interestingly, AdMSC-ND cultured in hBS-D exhibited decreased fibrinolytic activity even though tPA and PAI-1 transcript levels and secreted proteins were not significantly altered by sera conditions. These data suggest that blood-derived factors associated with hyperglycemia most likely also contribute to decrease fibrinolytic activity. To our knowledge, this is the first case report on the adverse effect of using diabetic-derived AdMSCs for cell therapy, which should be taken into account for future clinical management. Thus, because MSCs are widely used in cell therapy, we would recommend including new preclinical safety tests, such as the d-dimer and/or tPA–to–PAI-1 ratio tests, to assess fibrinolytic activity of cells before implantation. Such testing will aid in establishing an appropriate therapy after implantation therapy tailor-made for each individual patients.
ACKNOWLEDGMENTS
The authors are supported by the Fundación Progreso y Salud, Consejería de Salud, Junta de Andalucía (Grant PI-0022/2008) and Consejería de Innovación Ciencia y Empresa, Junta de Andalucía (Grant CTS-6505, INP-2011-1615-900000). Fondo Europeo de Desarrollo Regional (FEDER) cofunded grants from Instituto de Salud Carlos III (Red TerCel-Grant RD06/0010/0025, PI10/00964, and PI10/00871) and the Ministry of Health and Consumer Affairs (Advanced Therapies Program Grant TRA-120). Support from Fundación de la Sociedad Española de Diabetes (FSED) and Fundación Andaluza de Investigación y Desarrollo (FAID) allow access to databanks. CIBER de Diabetes y Enfermedades Metabolicas Asociadas is an initiative of the Instituto de Salud Carlos III.
No potential conflicts of interest relevant to this article were reported.
L.A. and N.E. performed the experiments and researched data. A.H. performed the experiments; researched data; designed the study; and wrote, reviewed, and edited the manuscript. I.P.-C., A.d.l.C., and R.R.-S. provided the samples and contributed to discussion. B.R.G. wrote, reviewed, and edited the manuscript. B.S. designed the study; wrote, reviewed, and edited the manuscript; and financed and coordinated the study. A.H. and B.S. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank members of the Hematology and Haemodynamic Departments (F. Marcos-Sánchez, M. Constantino-Bermejo) of the Hospital Virgen Macarena.
REFERENCES
- 1.Ruiz-Salmeron R, de la Cuesta-Diaz A, Constantino-Bermejo M, et al. Angiographic demonstration of neoangiogenesis after intra-arterial infusion of autologous bone marrow mononuclear cells in diabetic patients with critical limb ischemia. Cell Transplant 2011;20:1629–1639 [DOI] [PubMed] [Google Scholar]
- 2.Hashi CK, Zhu Y, Yang GY, et al. Antithrombogenic property of bone marrow mesenchymal stem cells in nanofibrous vascular grafts. Proc Natl Acad Sci U S A 2007;104:11915–11920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakagami H, Maeda K, Morishita R, et al. Novel autologous cell therapy in ischemic limb disease through growth factor secretion by cultured adipose tissue-derived stromal cells. Arterioscler Thromb Vasc Biol 2005;25:2542–2547 [DOI] [PubMed] [Google Scholar]
- 4.Prockop DJ, Oh JY. Mesenchymal stem/stromal cells (MSCs): role as guardians of inflammation. Mol Ther 2012;20:14–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Planat-Benard V, Silvestre JS, Cousin B, et al. Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation 2004;109:656–663 [DOI] [PubMed] [Google Scholar]
- 6.Neuss S, Schneider RK, Tietze L, Knüchel R, Jahnen-Dechent W. Secretion of fibrinolytic enzymes facilitates human mesenchymal stem cell invasion into fibrin clots. Cells Tissues Organs 2010;191:36–46 [DOI] [PubMed] [Google Scholar]
- 7.Binder BR, Mihaly J, Prager GW. uPAR-uPA-PAI-1 interactions and signaling: a vascular biologist’s view. Thromb Haemost 2007;97:336–342 [PubMed] [Google Scholar]
- 8.Zorio E, Gilabert-Estellés J, España F, Ramón LA, Cosín R, Estellés A. Fibrinolysis: the key to new pathogenetic mechanisms. Curr Med Chem 2008;15:923–929 [DOI] [PubMed] [Google Scholar]