Abstract
Background
Few studies of HIV+ individuals in China have examined the associations between HIV-related stress with sleep disturbance and fatigue, which are common complaints among people living with HIV/AIDS (PLWHA). We carried out this study to examine the relationships among perceived stress, sleep disturbance, and fatigue in PLWHA in China.
Methods
A mixed methods study design was used during data collection in Shanghai, China, from December 2009 to March 2010. Qualitative in-depth interviews were conducted with 19 HIV+ females. Additionally, cross-sectional audio computer-assisted self-interviews (ACASI) were conducted to collect quantitative data from a convenience sample of 107 HIV+ patients (84% were male) including the following scales: 1) Perceived Stress Scale for PLWHA, 2) General Sleep Disturbance Scale, and 3) Fatigue Scale.
Results
The major themes that emerged from the in-depth interviews were around life stress with HIV, sleep disturbance, and fatigue. Participants presented varying amounts of stress around worrying about whether to disclose their diagnosis and whether they might transmit the disease to their family. In addition, in the cross-sectional data, 40% of the participants reported clinically significant sleep disturbances (GSDS > 3) with an average of 3 nights of disturbed sleep in the past week (M=2.87, SD=1.21) and moderate fatigue severity (M=5.24, SD=2.27). In mediation analyses, the data suggests that the relationship between perceived stress and fatigue was largely (53%) mediated through sleep disturbance.
Conclusions
Chinese PLWHA described how stress had caused them to become sleepless and fatigued. The quantitative data also demonstrated significant levels of sleep disturbance and fatigue, where were due to perceived stress with HIV disease. A systematic self-management intervention to decrease perceived stress should be designed and implemented in mental health resource-limited settings such as China in order to reduce sleep disturbance and fatigue.
Keywords: China, PLWHA, Perceived stress, Sleep disturbance, Fatigue, Cronbach alpha coefficient
Introduction
People living with HIV/AIDS (PLWHA) around the world have frequently reported stress [1–5]. Perceived stress is defined as a relationship between the environment and the person that is being apprised by the self as tasking or exceeding his or her resources and hence endangering his or her well-being [6,7]. Many newly diagnosed PLWHA suffer from psychological stress like depression, anxiety, hopelessness, and suicidal ideation [8–11]. Perceived stresses also often present as physical symptoms such as headaches, sleep disturbances, fatigue, loss of appetite, and sexual difficulties [12].
There are several factors that contribute to the HIV-related stressors. For example, economic issues were one of the most commonly mentioned in several studies [13,14]. In addition, hopelessness and uncertainty for the future were also related to HIV diagnosis [13,15,16]. However, in many cultures, individuals present somatic complaints including headaches, perturbed sleep, and autonomic symptoms instead of psychological discomforts [17,18].
Specifically, stress has been associated with an increase in the symptoms of depression, high rates of clinical depression, and high rates of post-traumatic stress disorder (PTSD), as well as an increase in the severity of PTSD in PLWHA [19]. Studies have shown that stressful life events are strongly associated with HIV-related psychosocial and physiological effects. Such effects include stress over disclosure of serostatus, stigma associated with HIV, and generalized fatigue [4,20–26]. Perceived stress among PLWHA is related to poor self management skills, inappropriate coping mechanisms, and depression [7]. In addition, stress has been linked to poor ART adherence among PLWHA [19,27]. In a study of a predominantly African American HIV- positive sample, perceived stress was significantly correlated with state and trait anxiety, depression, HIV-related symptoms, sleep quality, daytime sleepiness and fatigue [10].
Chinese PLWHA often faces mental health crises after receiving their HIV diagnosis [28]. It is estimated that more than 70% of the Chinese PLWHA had developed major depression while only less than 10% of them received proper care for worsening mental health conditions [29].
In China, a report on mental stress in HIV-positive plasma/ blood donors found that participants reported high levels of HIV-related stress, depression, and anxiety. Further, the study also showed that greater HIV-related stress, HIV symptoms, and threat appraisal were directly associated with psychological distress [30]. Within the healthcare provider community, these findings have led to an increased awareness of the importance of treating psychological stress in HIV patients.
PLWHA experience lots of stress through experiencing discrimination [31]. In a project conducted to compare the associations between self-reported HIV discrimination and health outcomes among African- American and white women living with HIV, African-American women who reported HIV discrimination had higher mean scores for stress, suicidal ideation, depressive symptoms, number of unprotected sexual episodes; they had lower mean scores for self-esteem, and quality of life, and were more likely not to have sought medical care for HIV/AIDS [32]. Furthermore, experiencing discrimination led to poorer outcomes [33].
Aside from stress, the other most commonly reported symptoms of HIV are sleep disturbances and fatigue [34–37]. Studies show that 30%–100% of HIV-positive individuals experience varying levels of sleep disturbances [5,36,38,39]. Some PLWHA experienced greater sleep disturbance and symptom burden including stress and fatigue and reported more use of sleep medication [38]. Additionally, poor ART adherence was reported by those who suffered difficulty concentrating as a consequence of poor sleep quality [36]. While some study participants admitted that they simply forgot about taking the ART medicine [40,41], a longitudinal study reported close to one third of the participants were asleep during the time that they were supposed to take their medications [36].
Fatigue is a major issue in the HIV-positive population [42–44]. Studies have documented close relationships between psychological stress and fatigue [22,23,45]. Fatigue is defined as a lack of energy, sleepiness, exhaustion, and inability to get enough rest [46]. Factors related to fatigue in PLWHA include lack of exercise, diet imbalance, mental stresses including depression and anxiety, use of alcohol and/or street drugs, side effects from antiretroviral therapy, sleep disturbances, fever, anemia, progression of the disease, and lower CD4 cell counts [22,23,46]. In particular, the connection between sleep disturbance and fatigue is well established [5,36,38,39,42].
In linking these three factors together, studies have examined the association of HIV-related perceived stress with sleep disturbance and fatigue in PLWHA [23,38,42,47]. Reducing perceived stress can decrease perceived depressive symptoms in PLWHA and decrease fatigue levels and sleep disturbance [48]. How perceived stress, sleep disturbances, and fatigue relate to each other is rarely discussed in the PLWHA. Furthermore, few of these studies were focused on the HIV-positive population in resource-limited countries, such as China. In general, Chinese individuals tend to report more physical discomforts rather than psychological symptoms [7,16], so it is possible that assessing psychological well-being by evaluating symptoms such as sleep disturbance and fatigue, rather than mentally stress or “feeling blue” will result in better understanding of their mental health. In this paper, we examined the relationships among perceived stress, sleep disturbance, and fatigue in HIV-positive Chinese patients in Shanghai, China using a sequential mixed research method.
Methods
This project was developed and conducted through an on-going collaboration among U.S. and Chinese investigators at Yale University, University of Washington, and Shanghai Public Health Clinic Center (SPHCC).
This mixed methods study had two components. The qualitative component of this research involved semi-structured interviews with 19 HIV-positive women. The survey component of the research involved audio computer-assisted self-interview (ACASI) questionnaires with 107 HIV-positive patients who were receiving care at SPHCC.
The data were collected from November 2009 to March 2010 at SPHCC, which is one of the premier specialist hospitals for HIV care in China. For both phases of the research, two experienced and Chinese-English bilingual researchers recruited potential participants from both the inpatient and outpatient wards during their hospitalization or routine care visits. SPHCC clinicians informed patients about the study and referred them to research personnel. All study procedures were reviewed and approved by the institutional review boards of SPHCC and the University of Washington. Patients received a small monetary incentive of 100 RMB (∼US$16) for their time.
Measures
Qualitative component
The in-depth interviews were conducted with 19 HIV-positive women in Shanghai, China. The researchers met with HIV-positive women who were interested in the study, explained the procedures, answered issues related to the project, and obtained written consent. In-depth interviews were audio-recorded, conducted in Mandarin, and transcribed in Chinese after the session. Quotations were selected from the transcripts and translated into English for publication. Each interview took between one to two hours and was conducted in a private location. The Chinese-English bilingual researchers in social work and nursing, who conducted all the in-depth interviews.
Interviewers used a checklist during interviews to inquire about the participants’ perceptions of perceived stress, sleep disturbances, and fatigue both before and after their HIV diagnosis. Specific questions included the following: “What are your stressors before and after your diagnosis of HIV?”, “How do those stressors affect your sleep?” and “What is your energy level before and after the disease and before and after taking ART?” The interviewer asked participants whether they took naps during the day and how they felt after waking up from the nap. Generally, the study participants led the discussion, with the interviewers prompting as needed.
Qualitative content analysis [49] with Atlas.ti software (Scientific Software Development version 5.0, 2005) was used to code and analyze the data. After initial coding into broad topical categories, we generated reports for each topic including coded narratives from all the participants to summarize the range of responses. The first and second authors examined the transcripts separately and identified codes to correspond to concepts in the narratives. We then discussed the coding to resolve any disagreements in the meaning and assignment of codes and general patterns observed in the data.
Quantitative component
Participants completed a one-time 60-minute ACASI survey that consisted of standardized measures to assess demographics, HIV-related perceived stress, levels of fatigue, and experiences of sleep disturbance. The measures used have been previously tested in Chinese populations and have shown strong reliability and validity [7,50,51].
Demographics
Participants’ age, sex, marital/partner status, education level, income, residency, sexual preferences, and employment status were collected via self- report.
Perceived stress scale in HIV (PSSHIV)
This 44-item scale was used to evaluate the perceived stress level of PLWHAs in the 8 following factors: social/psychological problems, sexual relationships, functional problems, social acceptance/rejection issues, work-related issues, family/offspring issues, accessibility to treatment, and treatment outcomes. The Cronbach’s alpha values ranged from 0.76 to 0.94 for the overall scale and each of the 8 subscales. Example questions are, “I am afraid that my work will be affected by medical visits” and “HIV/ AIDS decreased my physical strength”. The PSSHIV asks participants to indicate the severity of the stress during last month from 1 (absolutely not stressful) to 5 (extremely stressful). Items are summed to obtain a total mean score that can range from 0 (absolutely not stressful) to 5 (extremely stressful) [7,51] with the cutoff score of 3 for the total scale to distinguish between tolerable stress from highly stressed.
Sleep disturbances
Subjective sleep variables were measured with the 21-item General Sleep Disturbance Scale (GSDS) [52]. The GSDS asks participants to indicate frequency of various sleep-related behaviors during the past week from 0 (not at all) to 7 (everyday). Items refer to the multidimensional aspects of falling asleep and maintaining sleep, as well as aspects of daytime functioning, such as feeling tired or sleepy during the day. Items are summed to obtain a total mean score that can range from 0 (no sleep disturbance) to 7 (frequent sleep disturbance). A cutoff score of 3 for the total scale distinguishes good and poor sleepers. The scale was validated originally with women shift workers [52] and was internally consistent in this sample (Cronbach’s alpha=0.82).
Fatigue
Fatigue was assessed using a seven-item Numerical Rating Scale for Fatigue (NRS-F), which is a self-rated scale from 0 (not fatigued) to 10 (extremely fatigued) with the cutoff mean score of 3.3 [53]. Questions in this section included “we want to know your energy level before you go to sleep, can you say before you go to bed, how your concentration level is? How badly do you want to lie down?” The fatigue scale assessed severity of various fatigue-related behaviors before bedtime from 0 (not at all) to 10 (very badly). Cronbach’s alpha coefficients for the seven-item version of the NRS-F ranged from .87 to .97 for Chinese participants [50,54].
For data analysis, descriptive and bivariate statistics were used to examine the relationship among perceived stress, sleep disturbance, fatigue, and background characteristics. Then, the relationship between fatigue, sleep disturbance, and perceived stress was examined utilizing multiple liner regression, controlling for potential correlates of fatigue. To further explore the relationships among fatigue, sleep disturbance, and stress, mediation analysis is conducted to test whether the relationship between fatigue and stress is mediated through sleep disturbance. Finally bootstrapping, a re-sampling technique, is also applied to draw additional 5,000 datasets to calculate the standard errors of the estimated correlation coefficients for statistical inferences.
Sample size
In this project, we recruited 120 participants for the cross-sectional surveys based on recommendations by Clark-Carter indicating that a medium effect size with 10 independent variables in multiple regression models would require about 120 participants [55]. However, due to a major technical issue (corruption of the hard drive in one research computer) we lost information from 13 of them. However, as this technical issue happened randomly and as we assigned our participants’ data storage randomly to our research computers, theoretically the missing values caused by this event could be conceptualized as “missing completely at random (MCAR) [55].” Thus, it would be safe to use the complete-case analysis.
Results and Discussion
Qualitative reports
The age range of the study participants was 29–59 years old (M=42 years; SD=9.5). One study participant came from a southern province to Shanghai to obtain her ART medication, and all others lived in the Shanghai metropolitan area and its suburbs. Half of the participants migrated from other provinces and resided in Shanghai. More than two-third (68%) of the participants started their ART within a year and 68% of them did not complete any college degree. Eleven of their partners (58%) were not HIV-infected. More than half (53%) of them were not married. One of the study participants contracted HIV from intravenous drug use and three of them contracted HIV from extramarital relationships. The rest of the 15 study participants (79%) were infected by their spouses or boyfriends.
Major themes that emerged from the in-depth interviews were about life stress with HIV, including different perceived stresses, sleep disturbance, and fatigue. Participants presented varying types of perceived stress, such as disclosure stress, marriage stress, stigma, and financial issues related to their HIV.
Perceived stress
Stress about disclosure
Chinese PLWHA often struggle with disclosure of their HIV diagnosis given that HIV is still highly stigmatized. In China, due to the familial-collectivist culture in which stigma would bring shame to families, decisions around familial disclosure become a major stressor for these HIV-positive individuals. A 30-year-old single woman who had obtained her diagnosis after an abortion surgery described how, to protect her parents, she carefully concealed her emotions and her diagnosis so that her parents would not detect any nuance of sadness or despair in her emotions, even though at that moment she really needed their support:
I didn’t tell my parents; they would never be able to take this. At that time I was already sick [due to the abortion]. I felt so stressed and desperate [sighs], as if there was no hope at all [but] I never showed my emotion. I ate and slept just like usual, though I was so sad. I cried only in bed at night so that they wouldn’t see it…No! No! No! I would never want to hurt them.
Stress on marriage
The women’s disclosure decisions were often followed by a range of relational changes, especially when the decision was to inform their husbands. Negative transformations were most salient in women’s marital relationships with an HIV-negative husband. Of the 12 women who disclosed their HIV status to their sero-discordant partners, 6 experienced a termination of the relationship.
One 52-year-old woman who had been married for 20 years separated from her husband after disclosing her HIV status to her husband and in-laws. Although the husband initially wanted to stay in the marriage, his family dissuaded him. Rather than filing for divorce, he simply moved away and stopped contributing to the household financially, leaving the woman and her son to get by on her retirement allowance. During the interview, the study participant cited her in-laws’ words to her husband, “This disease is a horrible one. It can suck up all your money and also destroy a family.”
Stress on stigma/discrimination
Study participants discussed that the HIV by itself is a stressor. A 28-year-old participant said, “I am afraid someone will know that I am HIV-positive. If I were not positive, I would not want to be with those I know are HIV positive”. Another 45-year-old HIV-positive individual mentioned, “I don’t want to be contacted by anyone with HIV or the HIV providers. I don’t want to hear these terms that stress me out. As long as I keep distant from these people, I won’t hear them. Getting too close with them, when these three words are constantly mentioned really makes me stressed.”
One 53-year-old retired woman suffered from self stigma as soon as she got diagnosed. She stated,
“Although none of my family and friends knows this [HIV diagnosis], I still feel everyone treat me differently. Everything changed. I did visit my family, but I found no place for me at home. I really worry how others would see me once they know I got this…I feel, the place I stand on, the chair I sit on, all become ‘contaminated’ and ‘dirty. I really feel this way!”
Stress on financial difficulties
Even with the “Four Frees and One Care” policy in China offering free antiretroviral therapy for rural residents and the urban poor, many HIV-positive individuals still experienced financial difficulties. Many people borrowed money from friends and relatives in order to continue their treatment, which would keep them healthier in order to work for money and pay their loans back. A 27-year-old female participant described how her worsening financial situation caused by HIV treatment induced her stress.
I am very stressed because I have stayed in the hospital for two months now, it costs 80,000 RMB (∼$13,000) already, but my illness is still not getting better. I keep thinking where I could find the money to pay for my treatment? I used to work and it covered part of the insurance. Now, I got this [HIV], there is no way that I can claim this to my company. I am so stressed out now.
Sleep disturbance
Studies have shown that PLWHAs experienced more sleep disturbances compared to the general population.[17,38,56] HIV-positive individuals suffered from difficulty falling asleep, difficulty staying asleep, awakening too early, or unrefreshing sleep in combination with some daytime sleepiness or irritability [57]. Although a variety of factors could contribute to sleep disturbance among PLHWA, a major cause that had influenced the sleep of these women was HIV-related stress. In our sample, 17 out of 19 women expressed they had experienced sleep disturbance as a direct result of HIV-related stress, especially within the first three to six months of their diagnosis. One primary reason is that for many of these women, sleep was usually the time they spent alone. Without other psychological distractions that often occur in the daytime, these women often began to ruminate on stressful events related to their HIV diagnosis. However, it was harder for them to fall asleep when they ruminated over their HIV/AIDS at night. A 45-year-old stay home mom described:
I just can’t fall asleep, no matter how hard I try… Once I recall all the stuff in the past, I just can’t sleep. After I put my kid to bed, I will do some cleaning, and then I will have nothing to do. But when I have nothing to do, I will start to think about how stupid I was, so that now my whole life is ruined. If I didn’t get this disease, I would have a great family…I can’t fall asleep every time after I cry, just can’t sleep at all.
Although some women would regain sleep quality after they adapted to their illness, for others, HIV-related stress and sleep disturbance became chronic. For instance, a woman in her early 40s who lost her husband in 2003 to AIDS explained that, after the death of her husband, as she needed to support two young children alone in Shanghai, she developed constant worries that interfered with her sleeping at night.
I always have bad dreams, and can’t have a good sleep at night… I have been living in fear, after my husband died, till today. I often take sleeping pills. I can’t sleep if I don’t take them…I take four pills every time, but usually people only need two to have a good sleep.
Fatigue
Fatigue is one of the major symptoms related to psychological stress and depression [58]. Although fatigue can be largely explained by psychological factors in current literature, in our sample 10 out of 17 women who have suffered from sleep disturbance also attributed their fatigue to a lack of quality sleep. Without sufficient rest at night, many of them suffered from “low energy” or “dizziness.” A 32-year-old working woman described:
I still feel tired after I got up in the morning, but I needed to get prepared for work… Perhaps coffee was not good for me, but I needed it because I didn’t sleep well and felt dizzy. However, once I took coffee, I can’t sleep at night. I had trouble in getting some sleep at night, but woke up early, which only gave me 4 hours of sleep. I didn’t know how I did my work at that time. I felt so low on energy almost every day. This lasted for about 3 to 4 months [after HIV diagnosis].
For some women, the fatigue engendered from their lack of quality sleep interrupted their daily functions. For example, a 50 year-old business woman decided to retire earlier and reduce her social activities due to her “lack of energy” which was a result of her chronic sleep disturbance.
Before [diagnosis] I had so many friends. But now I reduced my friends to only a few. It was because now I often feel lack of energy. I even can’t stand still as I don’t sleep well. So, that is it, totally different from what I was before…. Because this disease sucks up all of my energy, I have turned down so many offers for business cooperation… Yes, it is quite a pity.
Quantitative reports
In the cross-sectional data, the mean age of the participants was 37.6 years (range=23 to 59, SD=9.7). Sixty-four (60%) of the study participants completed high school education or more. More than one-third of the participants (39%; n = 42) had a monthly income less than 1,999 RMB (∼$322), however, 37% of them (n=39) earned more than 5,000 RMB (∼$645) per month. Furthermore, 82% of them (n=88) felt their income could not meet or just barely met their daily living expenses. Only about a quarter of the participants (n=27) had health insurance to cover their hospital bills, but of those who had health insurance, 93% (n =25) of them stated that their insurance was not adequate to cover the health care expenses. Indeed, almost 60% (n =64) had to suffer from illness due to the inability to pay for healthcare services. More than half of them were currently working (n =50). Also, almost half (n=52) of them had at least one child. Within these 52 parents, only 25 (48%) of the children were living with the study participants. The period for HIV diagnosis ranged from 1 to 16 years (M=4.76, SD=3.05). The mean CD4 count in this sample was 232 cells/mm3.
Also, many study participants did not know their viral load status or had never been tested (n =84; 79%). Detailed demographic data is presented in Table 1. We tested the correlations of each subscale of perceived stress, sleep disturbance, and fatigue as listed in Table 2. Only work-related stress was not correlated to sleep disturbance or fatigue.
Table 1.
Demographic Data.
| N* | N (%) | |
|---|---|---|
| Age (Mean=37.6) | 107 | |
| 23–39 years old | 77 (57) | |
| 40–59 years old | 58 (43) | |
| Education | 107 | |
| Completed high school | 64 (60) | |
| Completed college | 40 (37) | |
| Master’s degree | 3(3) | |
| Income per month | 106 | |
| 0ȓ1,999 RMB | 42 (39) | |
| 2,000–4,999 RMB | 25 (23) | |
| 5,000 RMB and above | 39 (37) | |
| Income adequate to meet daily living expenses | ||
| Totally inadequate | 107 | 40 (37) |
| Barely adequate | 48 (45) | |
| Enough | 19(18) | |
| Have health insurance | 107 | |
| Yes | 27 (25) | |
| With insurance, adequate to cover the health care expenses | 2(7) | |
| Working Status | 107 | |
| Employed | 60 (56) | |
| Have Children | 107 | |
| Yes | 52 (49) | |
| Living with you | 25 (48) | |
| CD4 Count (Mean=232 cells/mm3) | 105 | |
| 0–199 | 51 (49) | |
| 200–299 | 24 (23) | |
| 300–399 | 14(13) | |
| 400–499 | 11 (10) | |
| 500 and above | 5(5) | |
| Viral Load | 107 | |
| Undetectable | 4(4) | |
| Detectable | 19(18) | |
| Never tested | 54 (51) | |
| Don’t know | 30 (28) | |
| Perceived Stress | 104 | |
| 0–2.99 | 52(50) | |
| Sleep Disturbance | 106 | |
| 0–2.99 | 61 (58) | |
| Fatigue | ||
| 0–3.3 | 106 | 21 (20) |
| 3.4–10 | 85 (80) | |
(Total N =107, including missing data)
Table 2.
Correlations among perceived stress, sleep disturbances and fatigue.
| Perceived Stress |
Social psychology program |
Sexual relationship |
Functional problems |
Social accept/ reject |
Work-related issues |
Family offspring issues |
Ace. to Tx | Tx outcome | Fatigue | |
|---|---|---|---|---|---|---|---|---|---|---|
| Perceived Stress Social psychology program | .93* | |||||||||
| Sexual relationship | .86* | .78* | ||||||||
| Functional problems | .84* | .71* | .66* | |||||||
| Social acceptance/rejection | .88* | .83* | .68* | .64* | ||||||
| Work-related issues | .81* | .61* | .61* | .73* | .64* | |||||
| Family offspring issues | .62* | .55* | .56* | .31* | .57* | .43* | ||||
| Accessibility to treatment | .58* | .43* | .39* | .45* | .53* | .53* | .20† | |||
| Treatment outcome | .71* | .51* | .53* | .74* | .51* | .66* | .23† | .53* | ||
| Fatigue | .36* | .38* | .26* | .43* | .25* | .17 | .13* | .23† | .28* | |
| Sleep Disturbance | .40* | .45* | .36* | .37* | .37* | .17 | .22† | .28* | .23† | .59* |
GSDS: General Sleep Disturbance Scale; Ace:Access; Tx: Treatment
P≤0.01
P≤ 0.05
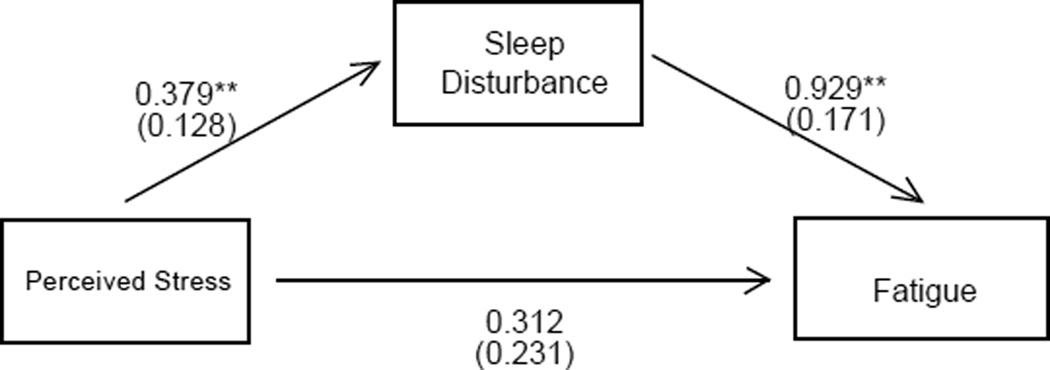
Participants reported a moderate level of stress (M=2.98, SD=1.00). About 40% of the participants reported above clinical threshold of significant sleep disturbances (GSDS>3). Study participants experienced about 3 nights of disturbed sleep in the past week (M=2.87, SD= 1.21) and moderate fatigue severity (M = 5.24, SD=2.27). In addition, perceived stress is positively correlated to sleep disturbance (r=0.40, p<0001) and fatigue severity (r=0.36, p<0.0001) in bivariate analyses. Sleep disturbance was also highly associated with fatigue (r=0.59, p<0001). However, only sleep disturbance remained significantly associated with fatigue (B = 0.929, SE = 0.188, p<001) after other covariates were controlled for, while the relationship between stress and fatigue became non-significant (B=0.312, SE=0.239, p= 0.199). Detailed analysis on Two-way ANOVA of sleep disturbance and fatigue is presented in Table 3. In mediation analyses, although the direct relationship between stress and fatigue was insignificant, both of the indirect relationships through sleep disturbance (B=0.352, bootstrap SE=0.135, p=0.009) and the total relationship between stress and fatigue that summed up both direct and indirect relationships (B = 0.664, bootstrap SE=0.253, p=0.009) were significant at a 0.05 level even after controlling for all the other covariates (Figure 1). This suggests that the relationship between stress and fatigue was largely (53%) mediated through sleep disturbance.
Table 3.
Two-way ANOVA of sleep disturbance and fatigue.
| Sum of Squares | Df | Mean Square | F | Sig. | ||
|---|---|---|---|---|---|---|
| Sleep Disturbance | Between Groups | 22.82 | 1 | 11.82 | 18.18 | .000 |
| Within Groups | 128 | 102 | 1.26 | |||
| Total | 150.82 | 103 | ||||
| Fatigue | Between Groups | 46.73 | 1 | 46.73 | 9.74 | .002 |
| Within Groups | 489.50 | 102 | 4.80 | |||
| Total | 536.24 | 103 |
Figure 1.
Mediation analyses among sleep disturbance, perceived stress, and fatigue.
The standardized beta weights of each variable in the series of regression analyses are shown: **P ≤ 0.01.
Our findings echo with other studies [9,10,23,35,59] indicating that sleep disturbances, which are part of the aspects related to HIV-related physiological and psychosocial associated with stress, are also highly associated with fatigue. The HIV-related stressful life events also contribute to sleep disturbances [10,11].
In our quantitative study, we tested the relationships between perceived stress, sleep disturbance, and fatigue. We found that stress is positively associated with sleep disturbance and fatigue. More specifically, the relationship between stress and fatigue is mediated through sleep disturbance. In the qualitative study, we further confirmed that Chinese HIV-positive patients experienced high levels of stress from a wide array of sources of stress related to their HIV diagnosis. Managing HIV disclosure and stigma in relationships and financial difficulties elevated stress levels among Chinese HIV-positive patients. Additionally, these stressful events could interfere with their sleep, which in turn generates fatigue among this population.
Our results indicated that sleep disturbance mediated the association between perceived stress and fatigue. Previous studies have linked sleep disturbances with stress and fatigue separately in the USA and other countries [10,11,17,23,46] but the present study brings these three factors together to suggest that sleep disturbance may be a critical factor that can mitigate these psychosocial consequences.
The need for intervention in this population is clear. For example, sleep hygiene treatments have been found to be efficacious in several studies [56,60]. Taibi recommends regular bedtimes, regular waking time, exercise, eliminating noise from the bedroom, regulating bedroom temperature, avoiding use of sleeping pills, avoiding caffeine and alcohol, eliminating clocks in the bedroom, avoiding naps during the day, engaging in relaxing activities before bed, limiting liquids, taking warm baths, and using the bedroom only for sleep [56,57]. However, a systematic self-management intervention to decrease perceived stress should be designed for and implemented in mental health resourcelimited settings like China for the optimal goal of decreasing fatigue and enhancing the quality of life.
Limitations
There are several limitations in this study. First, we recruited only HIV-positive Chinese women to describe their experiences in perceived stress, sleep disturbances and fatigues. HIV-positive men were not included in the in-depth interviews. Therefore, we do not know whether HIV-positive men experienced similar episodes of stress, sleep disturbances and fatigue compared to their female counterparts. Second, the relatively small sample size of the cross-sectional survey limited our ability to use more powerful statistical techniques, such as structural equation modeling.
Third, several important factors which might influence sleep quality were not included in the analysis, such as current treatment status, ART use, and potential co-infections like hepatitis B or C. Future follow up studies should include these factors. Fourth, because we did not collect data from age-, ethnic-, and socio-economical-matched HIV negative population, we cannot determine whether the relationships among the three variables observed in this sample of Chinese PLWHA also hold for other Chinese people without HIV/AIDS. Fifth, there are many other factors related to fatigue, for example, lack of exercise, diet, alcohol, drugs, and ART side effects. In this study, we did not focus on other potential moderators; however It would be beneficial in future studies to consider all these possible moderators. Lastly, we did not separate data based on the recruitment sites (the clinic and the floor), therefore, we cannot compare whether the hospitalized participants demonstrated higher stress compared to the outpatient participants.
Conclusions
In this study, Chinese HIV-positive participants described how stress had caused them to experience sleep disturbances and fatigue. The quantitative data also demonstrated significant levels of sleep disturbance influenced fatigue, which were all due to perceived stress related to the HIV disease. This study suggests that healthcare providers should consider interactions between factors at both psychological (e.g., perceived stress) and physiological (e.g., sleep disturbances and fatigue) levels. Furthermore, these study findings suggest that sleep disturbance would be a critical component to fatigue reduction intervention for PLWHA. Multilevel methods that incorporate psychological and physiological level approaches are more likely to yield more effective, longer lasting fatigue reduction. Therefore, intervention design should focus on self-management including stress reduction and relaxation to enhance better sleep hygiene and later, reduce fatigue and achieve a better quality of life.
Acknowledgement
This study resulted (in part) from research supported by the University of Washington Center for AIDS Research (CFAR), an NIH funded program (P30 AI027757), which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NCCAM) through an international pilot grant awarded to Dr. Wei-Ti Chen and by the University of Washington’s (UW) School of Nursing Research & Intramural Funding Program (RIFP). In addition, this publication was supported (in part) from research supported by an NIH funded programs (5R25MH087217; PI: Barbara Guthrie) through the Research Education Institute for Diverse Scholars (REIDS) program awarded to Wei-ti Chen and 1K23NR014107; (PI: Wei-Ti Chen). We would also like to acknowledge Lin Zhang, Yinyin Tu, Ren-Fang Zhang, Li-Jun Zha, Cheng-En Pan, the Association for the Benefit of PLWHA (Beautiful Life-Shanghai) and all of the study participants.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Rao D, Chen WT, Pearson CR, Simoni JM, Fredriksen-Goldsen K, et al. Social support mediates the relationship between HIV stigma and depression/ quality of life among people living with HIV in Beijing, China. Int J STD AIDS. 2012;23:481–484. doi: 10.1258/ijsa.2009.009428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Santis JP, Gonzalez-Guarda RM, Vasquez EP. Psychosocial and cultural correlates of depression among Hispanic men with HIV infection: a pilot study. J Psychiatr Ment Health Nurs. 2012;19:860–869. doi: 10.1111/j.1365-2850.2011.01865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng MC, Feng JY, Chen TC, Lu PL, Ko NY, et al. Stress, needs, and quality of life of family members caring for adults living with HIV/AIDS in Taiwan. AIDS Care. 2009;21:482–489. doi: 10.1080/09540120802290373. [DOI] [PubMed] [Google Scholar]
- 4.Scott-Sheldon LA, Kalichman SC, Carey MP, Fielder RL. Stress management interventions for HIV+ adults: a meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychol. 2008;27:129–139. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vosvick M, Gore-Felton C, Ashton E, Koopman C, Fluery T, et al. Sleep disturbances among HIV-positive adults: the role of pain, stress, and social support. J Psychosom Res. 2004;57:459–463. doi: 10.1016/j.jpsychores.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- 7.Su X, Lau JT, Mak WW, Chen L, Feng T, et al. Development of the perceived stress scale for people living with HIV/AIDS in China. AIDS Patient Care STDS. 2008;22:989–998. doi: 10.1089/apc.2008.0095. [DOI] [PubMed] [Google Scholar]
- 8.Tamblyn JM, Calderon AJ, Combs S, O'Brien MM. Patients from abroad becoming patients in everyday practice: torture survivors in primary care. J Immigr Minor Health. 2011;13:798–801. doi: 10.1007/s10903-010-9429-2. [DOI] [PubMed] [Google Scholar]
- 9.Marion I, Antoni M, Pereira D, Wohlgemuth W, Fletcher MA, et al. Distress, sleep difficulty, and fatigue in women co-infected with HIV and HPV. Behav Sleep Med. 2009;2009;7:180–193. doi: 10.1080/15402000902976721. [DOI] [PubMed] [Google Scholar]
- 10.Hand GA, Phillips KD, Dudgeon WD. Perceived stress in HIV-infected individuals: physiological and psychological correlates. AIDS Care. 2006;18:1011–1017. doi: 10.1080/09540120600568376. [DOI] [PubMed] [Google Scholar]
- 11.Phillips KD, Sowell RL, Rojas M, Tavakoli A, Fulk LJ, et al. Physiological and psychological correlates of fatigue in HIV disease. Biol Res Nurs. 2004;6:59–74. doi: 10.1177/1099800404264846. [DOI] [PubMed] [Google Scholar]
- 12.Chipimo PJ, Tuba M, Fylkesnes K. Conceptual models for mental distress among HIV-infected and uninfected individuals: a contribution to clinical practice and research in primary-health-care centers in Zambia. BMC Health Serv Res. 2011;11:7. doi: 10.1186/1472-6963-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy DA, Roberts KJ, Herbeck DM. HIV-positive mothers with late adolescent/early adult children: "empty nest" concerns. Health Care Women Int. 2012;33:387–402. doi: 10.1080/07399332.2012.655395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang E, Rapkin BD, DeAlmeida C. Are psychological consequences of stigma enduring or transitory? A longitudinal study of HIV stigma and distress among Asians and Pacific Islanders living with HIV illness. AIDS Patient Care STDS. 2006;20:712–723. doi: 10.1089/apc.2006.20.712. [DOI] [PubMed] [Google Scholar]
- 15.Xu J, Sullivan SG, Dou Z, Wu Z. China CIPRA Project 2 TeamEconomic stress and HIV-associated health care utilization in a rural region of China: a qualitative study. AIDS Patient Care STDS. 2007;21:787–798. doi: 10.1089/apc.2007.0005. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J, Zhao G, Li X, Hong Y, Fang X, et al. Positive future orientation as a mediator between traumatic events and mental health among children affected by HIV/AIDS in rural China. AIDS Care. 2009;21:1508–1516. doi: 10.1080/09540120902923048. [DOI] [PubMed] [Google Scholar]
- 17.Chen WT, Lee SY, Shiu CS, Simoni JM, Pan C, et al. Fatigue and sleep disturbance in HIV-positive women: a qualitative and biomedical approach. J Clin Nurs. 2013;22:1262–1269. doi: 10.1111/jocn.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mak WW, Cheung RY, Law RW, Woo J, Li PC, et al. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc Sci Med. 2007;64:1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 19.O'Cleirigh C, Safren S. Optimizing the effects of stress management interventions in HIV. Health Psychol. 2008;27:297–301. doi: 10.1037/a0012607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Voss JG, Dodd M, Portillo C, Holzemer W. Theories of fatigue: application in HIV/AIDS. J Assoc Nurses AIDS Care. 2006;17:37–50. doi: 10.1016/j.jana.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Barroso J, Pence BW, Salahuddin N, Harmon JL, Leserman J. Physiological correlates of HIV-related fatigue. Clin Nurs Res. 2008;17:5–19. doi: 10.1177/1054773807311382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leserman J, Barroso J, Pence BW, Salahuddin N, Harmon JL. Trauma, stressful life events and depression predict HIV-related fatigue. AIDS Care. 2008;20:1258–1265. doi: 10.1080/09540120801919410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salahuddin N, Barroso J, Leserman J, Harmon JL, Pence BW. Daytime sleepiness, nighttime sleep quality, stressful life events, and HIV-related fatigue. J Assoc Nurses AIDS Care. 2009;20:6–13. doi: 10.1016/j.jana.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 25.Ichikawa M, Natpratan C. Quality of life among people living with HIV/ AIDS in northern Thailand: MOS-HIV Health Survey. Qual Life Res. 2004;13:601–610. doi: 10.1023/B:QURE.0000021319.73865.5a. [DOI] [PubMed] [Google Scholar]
- 26.Ware NC, Wyatt MA, Tugenberg T. Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 2006;18:904–910. doi: 10.1080/09540120500330554. [DOI] [PubMed] [Google Scholar]
- 27.Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol. 2007;26:488–495. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen WT, Shiu CS, Simoni JM, Zhao H, Bao MJ, et al. In sickness and in health: a qualitative study of how Chinese women with HIV navigate stigma and negotiate disclosure within their marriages/partnerships. AIDS Care. 2011;23(Suppl 1):120–125. doi: 10.1080/09540121.2011.554521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin H, Hampton Atkinson J, Yu X, Heaton RK, Shi C, et al. Depression and suicidality in HIV/AIDS in China. J Affect Disord. 2006;94:269–275. doi: 10.1016/j.jad.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 30.Meade CS, Wang J, Lin X, Wu H, Poppen PJ. Stress and coping in HIV-positive former plasma/blood donors in China: a test of cognitive appraisal theory. AIDS Behav. 2010;14:328–338. doi: 10.1007/s10461-008-9494-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gagnon AJ, Merry L, Booking J, Rosenberg E, Oxman-Martinez J. South Asian migrant women and HIV/STIs: knowledge, attitudes and practices and the role of sexual power. Health Place. 2010;16:10–15. doi: 10.1016/j.healthplace.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Myer L, Stein DJ, Grimsrud AT, Herman A, Seedat S, et al. DSM-IV-defined common mental disorders: association with HIV testing, HIV-related fears, perceived risk and preventive behaviours among South African adults. S Afr Med J. 2009;99:396–402. [PMC free article] [PubMed] [Google Scholar]
- 33.Wingood GM, Diclemente RJ, Mikhail I, McCree DH, Davies SL, et al. HIV discrimination and the health of women living with HIV. Women Health. 2007;46:99–112. doi: 10.1300/J013v46n02_07. [DOI] [PubMed] [Google Scholar]
- 34.Low Y, Preud'homme X, Goforth HW, Omonuwa T, Krystal AD. The association of fatigue with depression and insomnia in HIV-seropositive patients: a pilot study. Sleep. 2011;34:1723–1726. doi: 10.5665/sleep.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lerdal A, Gay CL, Aouizerat BE, Portillo CJ, Lee KA. Patterns of morning and evening fatigue among adults with HIV/AIDS. J Clin Nurs. 2011;20:2204–2216. doi: 10.1111/j.1365-2702.2011.03751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gay C, Portillo CJ, Kelly R, Coggins T, Davis H, et al. Self-reported medication adherence and symptom experience in adults with HIV. J Assoc Nurses AIDS Care. 2011;22:257–268. doi: 10.1016/j.jana.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corless lB, Bunch EH, Kemppainen JK, Holzemer WL, Nokes KM, et al. Self-care for fatigue in patients With HIV. Oncol Nurs Forum. 2002;29:E60–E69. doi: 10.1188/02.ONF.E60-E69. [DOI] [PubMed] [Google Scholar]
- 38.Lee KA, Gay C, Portillo CJ, Coggins T, Davis H, et al. Types of sleep problems in adults living with HIV/AIDS. J Clin Sleep Med. 2012;8:67–75. doi: 10.5664/jcsm.1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hudson AL, Portillo CJ, Lee KA. Sleep disturbances in women with HIV or AIDS: efficacy of a tailored sleep promotion intervention. Nurs Res. 2008;57:360–366. doi: 10.1097/01.NNR.0000313501.84604.2c. [DOI] [PubMed] [Google Scholar]
- 40.Simoni JM, Amico KR, Pearson CR, Malow R. Strategies for promoting adherence to antiretroviral therapy: a review of the literature. Curr Infect Dis Rep. 2008;10:515–521. doi: 10.1007/s11908-008-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simoni JM. Overview of adherence to antiretroviral therapies. In: Pope C, White R, Malow R, editors. HIV/AIDS: Global Frontiers in Prevention/ Intervention. Taylor & Francis, NY: 2008. [Google Scholar]
- 42.Aouizerat BE, Gay CL, Lerdal A, Portillo CJ, Lee KA. Lack of energy: an important and distinct component of HIV-related fatigue and daytime function. J Pain Symptom Manage. 2013;45:191–201. doi: 10.1016/j.jpainsymman.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aouizerat BE, Miaskowski CA, Gay C, Portillo CJ, Coggins T, et al. Risk factors and symptoms associated with pain in HIV-infected adults. J Assoc NursesAIDSCare. 2010;21:125–133. doi: 10.1016/j.jana.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Groopman JE. Fatigue in cancer and HIV/AIDS. Oncology (Wlliston Park) 1998;12:335–344. [PubMed] [Google Scholar]
- 45.Pence BW, Barroso J, Leserman J, Harmon JL, Salahuddin N. Measuring fatigue in people living with HIV/AIDS: psychometric characteristics of the HIV-related fatigue scale. AIDS Care. 2008;20:829–837. doi: 10.1080/09540120701694063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adinolfi A. Assessment and treatment of HIV-related fatigue. J Assoc Nurses AIDS Care. 2001;12(Suppl):29–34. doi: 10.1177/105532901773742266. [DOI] [PubMed] [Google Scholar]
- 47.Skevington SM. Is quality of life poorer for older adults with HIV/AIDS? International evidence using the WHOQOL-HIV. AIDS Care. 2012;24:1219–1225. doi: 10.1080/09540121.2012.661838. [DOI] [PubMed] [Google Scholar]
- 48.Yeh ML, Hsu ST, Ko WC, Ko NY. [Depressive symptoms in people living with HIV: related factors] Hu Li Za Zhi. 2012;59:40–50. [PubMed] [Google Scholar]
- 49.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 50.Lee SY, Lee KA, Rankin SH, Weiss SJ, Alkon A. Sleep disturbance, fatigue, and stress among Chinese-American parents with ICU hospitalized infants. Issues Ment Health Nurs. 2007;28:593–605. doi: 10.1080/01612840701354505. [DOI] [PubMed] [Google Scholar]
- 51.Su X, Lau JT, Mak WW, Chen L, Choi KC, et al. Perceived discrimination, social support, and perceived stress among people living with HIV/AIDS in China. AIDS Care. 2013;25:239–248. doi: 10.1080/09540121.2012.701713. [DOI] [PubMed] [Google Scholar]
- 52.Lee KA. Self-reported sleep disturbances in employed women. Sleep. 1992;15:493–498. doi: 10.1093/sleep/15.6.493. [DOI] [PubMed] [Google Scholar]
- 53.Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991;36:291–298. doi: 10.1016/0165-1781(91)90027-m. [DOI] [PubMed] [Google Scholar]
- 54.Lee SY, Lee KA. Early postpartum sleep and fatigue for mothers after cesarean delivery compared with vaginal delivery: an exploratory study. J Perinat Neonatal Nurs. 2007;21:109–113. doi: 10.1097/01.JPN.0000270627.73993.b0. [DOI] [PubMed] [Google Scholar]
- 55.Clark-Carter D. Quantitative psychological research: The complete student's companion. Psychology Pres. (3rd) 2009 [Google Scholar]
- 56.Webel AR, Moore SM, Hanson JE, Patel SR, Schmotzer B, et al. Improving sleep hygiene behavior in adults living with HIV/AIDS: a randomized control pilot study of the SystemCHANGE(TM)-HIV intervention. Appl Nurs Res. 2013;26:85–91. doi: 10.1016/j.apnr.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taibi DM. Sleep disturbances in persons living with HIV. J Assoc Nurses AIDS Care. 2013;24:S72–S85. doi: 10.1016/j.jana.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barroso J, Voss JG. Fatigue in HIV and AIDS: an analysis of evidence. J Assoc Nurses AIDS Care. 2013;24:S5–S14. doi: 10.1016/j.jana.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 59.Lee KA, Portillo CJ, Miramontes H. The influence of sleep and activity patterns on fatigue in women with HIV/AIDS. J Assoc Nurses AIDS Care. 2001;12(Suppl):19–27. doi: 10.1177/105532901773742257. [DOI] [PubMed] [Google Scholar]
- 60.Sun WQ, Chen WJ, Jiang YR, Li F, Li SH, et al. [The association of sleep hygiene and sleep quality among school-age children] Zhonghua Yu Fang Yi XueZa Zhi. 2012;46:713–717. [PubMed] [Google Scholar]