Abstract
Background
The coronary artery calcium (CAC) score predicts coronary heart disease (CHD) events, but methods for interpreting the score in combination with conventional CHD risk factors have not been established.
Methods and Results
We analyzed CAC scores and CHD risk factor measurements from 6757 Black, Chinese, Hispanic and white men and women aged 45–84 years in the Multi-Ethnic Study of Atherosclerosis (MESA). CAC was associated with age, sex, race-ethnicity, and all conventional CHD risk factors. Multivariable models using these factors predicted the presence of CAC (C-statistic = 0.789) and degree of elevation (16% of variation explained), and can be used to update a “pre-test” CHD risk estimate, such as the 10-year Framingham Risk Score, that is based on an individual’s conventional risk factors. In scenarios where a high CAC score is expected, a moderately elevated CAC score of 50 is reassuring (e.g., reducing risk from 10% to 6% in a healthy older white man); but when a low/zero CAC score is expected, even with identical pre-test CHD risk, the same CAC score of 50 may be alarmingly high (e.g., increasing risk from 10% to 20% in a middle-aged black woman with multiple risk factors). Both the magnitude and direction of the shift in risk varied markedly with pre-test CHD risk and with the pattern of risk factors.
Conclusions
Knowing what CAC score to expect for an individual patient, based on their conventional risk factors, may help clinicians decide when to order a CAC test and how to interpret the results.
Keywords: coronary disease, calcium, imaging, epidemiology
INTRODUCTION
Coronary artery calcium (CAC) testing may be useful for guiding interventions to prevent coronary heart disease (CHD)1. CAC scores predict risk for CHD events2, and higher risk individuals are more likely to benefit from prevention interventions such as aspirin and statins3. It is not always clear, however, how clinicians should integrate information from the CAC score with what they already know about a patient’s CHD risk and other characteristics. Prior studies have demonstrated strong associations between CAC and a patient’s age and sex4, 5, race-ethnicity5, and other CHD risk factors such as smoking, blood pressure, diabetes, and cholesterol6, 7. Given these associations, these individual characteristics should influence what CAC score a clinician expects when he or she orders the test in clinical practice. When the actual score is higher than expected, estimates of CHD risk should logically be revised upwards for that patient, and vice versa when the actual score is lower than expected. How the clinician interprets the CAC score and estimates the “post-test” CHD risk, therefore, should depend both on the pre-test risk8 and on a careful analysis of the expected CAC score (i.e., the “prevalence”9 of CAC) in that patient, but methods for integrating risk information from the CAC score with conventional CHD risk factors have not been established. One previous analysis described expected CAC score distributions and relevant methods, but used a convenience sample of clinic patients of unknown race/ethnicity who were referred or self-referred for CAC testing, and only self-reported risk factor data were available7.
The Multi-Ethnic Study of Atherosclerosis (MESA) provides an ideal opportunity to examine CAC score distributions in a multi-ethnic community-based sample of research participants who have also undergone careful measurement of conventional CHD risk factors. Previous analyses of this dataset have yielded widely referenced estimates of the value of the CAC score in terms of predicting future clinical events2, 10. We used results from the baseline MESA examination to estimate associations between the CAC score and conventional CHD risk factors and produce methods for 1) estimating how likely different CAC scores are in a given clinical scenario, and 2) combining the information from the CAC score with the patient’s characteristics and a “pre-test” risk estimate to obtain an integrated “post-test” estimate of CHD risk.
METHODS
Study Sample
MESA is a prospective cohort study of 6814 persons aged 45 to 84 years without known cardiovascular disease at baseline. Participants were recruited from 6 US cities from July 2000 through September 2002 and identified themselves as white (38%), black (28%), Hispanic (22%), or Chinese (12%) at the time of enrollment. The study was approved by the institutional review boards of each site, and all participants gave written informed consent. The study design has been described in detail elsewhere11. Our analysis uses only cross-sectional data from the MESA baseline examination.
The Coronary Artery Calcium (CAC) Score
Carr et al reported the details of the MESA CT scanning and interpretation methods12. Scanning centers assessed coronary calcium by chest computed tomography (CT) with either a cardiac-gated electron-beam CT scanner (Chicago, Illinois; Los Angeles, California; and New York, New York field centers) or a multidetector CT system (Baltimore, Maryland; Forsyth County, North Carolina; and St Paul, Minnesota field centers). Certified technologists scanned all participants twice over phantoms of known physical calcium concentration. A radiologist or cardiologist read all CT scans at a central reading center (Los Angeles Biomedical Research Institute at Harbor– UCLA, Torrance, California). We used the mean Agatston score for the 2 scans in all analyses13. Intraobserver and interobserver agreements were excellent (Kappa=0.93 and 0.90, respectively).
Conventional Coronary Heart Disease (CHD) Risk Factors
The primary predictors in our analysis were race/ethnicity and conventional CHD risk factors including age, sex, blood pressure level and medication use, cholesterol (total and high-density lipoprotein (HDL)), diabetes, and smoking status. These measurements were collected as part of the baseline examination. Blood pressure was measured 3 times using a Dinamap Pro 1000 automated oscillometric sphygmomanometer (Critikon, Tampa, Florida) with the participant in a seated position; the mean of the last 2 blood pressure measurements was used. Total and high-density lipoprotein cholesterol, triglycerides, and plasma glucose were measured from blood samples obtained after a 12-hour fast. Diabetes was defined as a fasting plasma glucose level greater than 126 mg/dl (7.8 mmol/L) or a history of medical treatment for diabetes.
We used the National Cholesterol Education Panel’s Adult Treatment Panel III (ATPIII) guidelines3 version of the Framingham risk score (FRS) to estimate 10-year risk of CHD events using measurements obtained during the MESA research exam. For diabetics, we multiplied the FRS by 1.5 in men and by 1.8 in women, consistent with other published Framingham risk equations14. We used this score, without recalibration for race/ethnicity or otherwise, as the “pre-test CHD risk” as recommended in current guidelines3. An alternate version of our analysis using 5-year risk with recalibration for race-ethnicity using published data15 is provided in the Supplementary Material.
Statistical Analysis
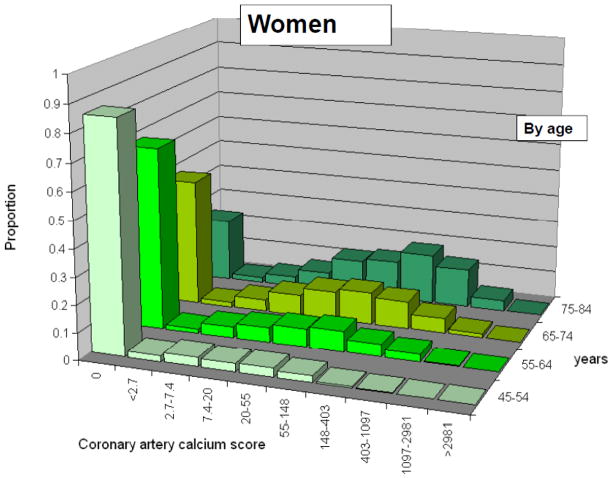
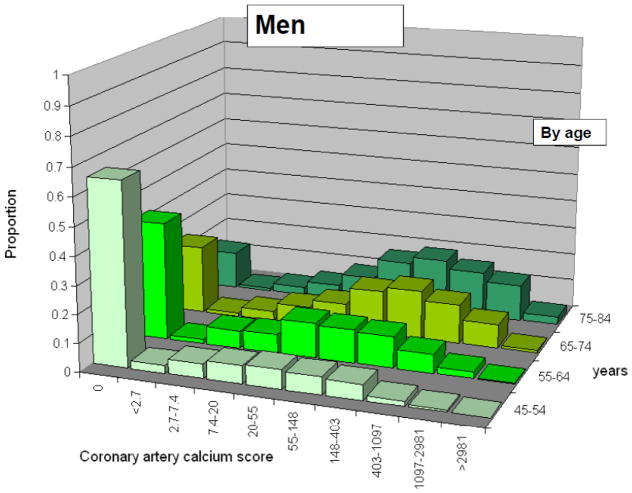
The CAC score distribution is highly skewed and is very frequently zero, and hence is not amenable to a simple normalizing transformation, as noted by others16. After exclusion of zero values, the log-transformed CAC score is approximately normally distributed (Figure). This leads naturally to a two-stage approach to modeling the CAC score distribution, with logistic regression (any CAC vs. none) and then linear regression of the log-transformed CAC score among persons with a non-zero score. This approach allows for parametric multivariable modeling of the CAC score distribution. As in previous analyses7, the two-stage approach outperforms alternate one-stage methods (Supplemental Figure).
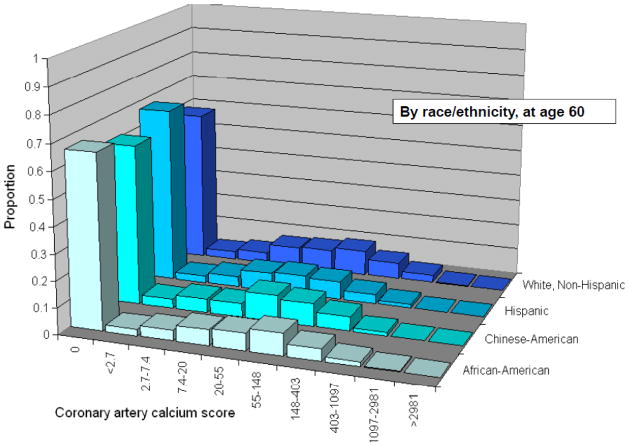
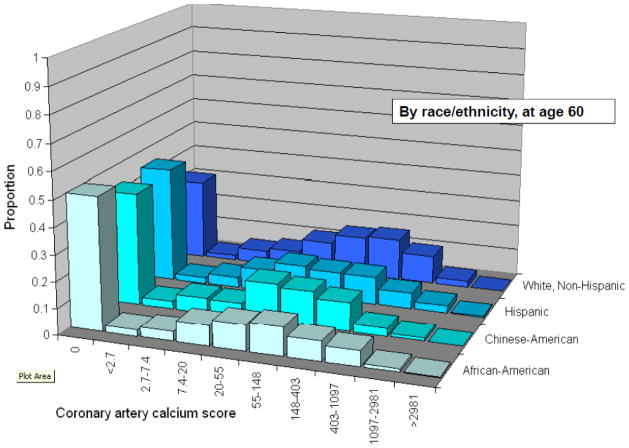
Figure 1.
Distribution of coronary artery calcium scores among men and women, on a logarithmic scale, by age and by race/ethnicity. Categories chosen for histograms are evenly spaced on a logarithmic scale, corresponding to Ln(CAC) scores of <1, 1–2, 2–3, 3–4, 4–5, 5–6, 6–7, 7–8, and >8. The first bar represents subjects with no detectable CAC, which corresponds to an undefined Ln(CAC) value. CAC – Coronary artery calcium
After describing the study sample, we analyzed the expected distribution of the CAC score using the two-step approach described above. We used three pre-specified modeling approaches: 1) using the FRS as the only predictor; 2) using age and sex as the only predictors; and 3) testing a variety of models considering age, sex/race/ethnicity, the conventional CHD risk factors used in the FRS, and diabetes. To refine our model without overfitting, we undertook an unbiased systematic model selection process with 10-fold cross-validation17, considering all possible models that included all the predictors, up to two pairwise interactions (0, 1 or 2), and up to 1 quadratic term (0 or 1) for each continuous variable. The top-performing models in terms of discrimination (cross-validated C-statistic in the logistic regression model, rounded to 3 significant digits) were identified; among these, we chose the simplest for presentation. We then used the same predictors in the second step (linear regression), and present the 10-fold cross-validated R2 value as an optimism-corrected measure of model performance.
Using these models, we calculated the estimated prevalence of a CAC score in the ranges of 0, 1–100, 101–300, and >300. These categories (or similar ones) have been used in publications describing the value of the CAC score in terms of predicting future clinical events2, 7, 18–20, and represent a simple and clinically important scheme for understanding the CAC score. The prevalence of scores in each of these categories is described according to clinical characteristics using the model parameters estimated as above.
As a final step, we used a simple algebraic calculation to combine risk information from conventional CHD risk factors with information from the CAC score. We assumed that the “pre-test risk” (using the FRS3 for this illustration) represents an average of persons with different CAC scores, weighted by the probability of having a CAC score in each category (calculated according to modeling approach 3, described above). The risks in each category (annualized) were assumed to differ according to the adjusted relative risk estimates from Detrano et al2: CAC=0: Reference; CAC=1–100: 3.61; CAC=101–300: 7.73; CAC>300: 9.67. With these assumptions, the “post-test risk” (using information from both the conventional risk factors and the CAC score) can be calculated algebraically. A variety of examples are presented, and an Excel-based calculator that can be used to estimate post-test risk in other clinical scenarios is published in the Online Materials.
RESULTS
The MESA baseline examination included 6814 participants, all of whom had coronary calcium measured; 57 participants (<1%) were excluded because they were missing either total or HDL cholesterol, systolic blood pressure, diabetes, or smoking status, leaving 6757 participants for this analysis. Of these, 27% were African-American (black), 12% were Chinese, 22% were Hispanic, and 39% were non-Hispanic European-American (white); approximately half were women (52%). Clinically relevant differences were apparent across race-ethnicity in systolic blood pressure, diabetes, and smoking (Table 1). Despite identical median FRS’s across race-ethnicity, the prevalence of CAC was significantly different (p<.001), with the highest prevalence of CAC in non-Hispanic white participants. Age, sex and race-ethnicity were all strong predictors of the presence and extent of CAC, and the distributions of log-transformed positive scores were approximately normal (Figure).
Table 1.
Characteristics of MESA participants
| Characteristic | Race/Ethnicity
|
|||
|---|---|---|---|---|
| Black | Chinese-American | Hispanic/Latino | White, Non-Hispanic | |
| N (%), mean ± SD, or median (IQR) | N=1859 | N=800 | N=1494 | N=2604 |
| Age, years | 62 +/− 10 | 62 +/− 10 | 61 +/− 10 | 63 +/− 10 |
| Sex, n (%) women | 1027 (55%) | 413 (52%) | 773 (52%) | 1354 (52%) |
| Systolic blood pressure, mmHg | 132 +/− 22 | 125 +/− 22 | 127 +/−22 | 123 +/− 20 |
| Total cholesterol, mg/dl | 190 +/− 36 | 193 +/− 32 | 198 +/− 37 | 196 +/− 35 |
| HDL cholesterol, mg/dl | 52 +/− 15 | 50 +/− 13 | 48 +/− 13 | 52 +/− 16 |
| Diabetes mellitus, n (%) | 326 (18%) | 105 (13%) | 264 (18%) | 158 (6%) |
| Current smoker, n (%) | 333 (18%) | 45 (6%) | 203 (14%) | 299 (11%) |
| FRS* 10-year CHD risk, median % (IQR) | 6% (2%–14%) | 6% (2%–13%) | 6% (2%–14%) | 6% (2%–13%) |
| Coronary calcium present, n (%) | 813 (44%) | 402 (50%) | 676 (45%) | 1485 (57%) |
- The Framingham Risk Score, from National Cholesterol Education Program’s Adult Treatment Panel (ATPIII) guidelines3, with adjustment for diabetes status (see Methods).
MESA – Multi-Ethnic Study of Atherosclerosis; SD – Standard deviation; HDL – High-density lipoprotein; IQR – Inter-quartile range; FRS – Framingham Risk Score; CHD – Coronary heart disease
The FRS is a strong predictor of CAC (Table 2, Model 1). For each increase of 5% in the 10-year risk for CHD events, the odds of having a positive CAC score nearly doubled (odds ratio (OR) = 1.80, 95% confidence interval (CI): 1.72–1.89) and the CAC score increased by 32% (95%CI: 28%–36%) among persons with CAC. The C-statistic, a measure of how well the model discriminates between persons with and without CAC, was .752 (cross-validated). A second model containing only age and sex performed better (cross-validated C-statistic = .767; Table 2, Model 2).
Table 2.
Predictors of coronary calcium presence and extent
| Model - Predictors | Logistic Regression for Coronary Calcium Presence (score>0) | Linear Regression for Coronary Calcium Extent (ln(coronary calcium score)) among persons with a score>0 | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Odds ratio (95% CI) | p-value | Cross- validated C-statistic | Coefficients (95% CI) | Corresponding percent increase in natural CAC scores* | p-value | Cross- validated R2 | |
| Model 1: FRS Risk Score only*† | |||||||
| - per 5% increase in 10-year CHD risk | 1.80 (1.72–1.89) | <.001 | .752 | 0.28 (0.25–0.31) | 32% (28%–36%) | <.001 | .090 |
| Model 2: Age and sex only* | |||||||
| - Age, per 10 years | 2.60 (2.46–2.76) | <.001 | .767 | 0.96 (0.90–1.02) | 160% (146%–176%) | <.001 | .138 |
| - Male sex | 2.83 (2.53–3.16) | <.001 | 1.04 (.92–1.15) | 183% (153%–216%) | <.001 | ||
| Model 3: All CHD risk factors, race/ethnicity*‡ | |||||||
| - Age, per 10 years | 2.48 (2.33–2.65) | <.001 | .789 | 0.61 (0.54–0.67) | 83% (72%–96%) | <.001 | .160 |
| - White male (vs. white female) | 3.31 (2.73–4.01) | <.001 | 0.88 (0.70–1.06) | 141% (101%–190%) | <.001 | ||
| - Asian female (vs. white female) | 0.87 (0.67–1.13) | .301 | −0.19 (−0.48–0.10) | −18% (−38%–10%) | .190 | ||
| - Asian male (vs. white female) | 1.92 (1.47–2.51) | <.001 | 0.33 (0.067–0.59) | 39% (7%–81%) | .014 | ||
| - Black female (vs. white female) | 0.56 (0.46–0.68) | <.001 | −0.18 (−0.40–0.036) | −17% (−33%–4%) | .102 | ||
| - Black male (vs. white female) | 1.16 (0.95–1.43) | .149 | 0.30 (0.081–0.51) | 35% (8%–67%) | .007 | ||
| - Hispanic female (vs. white female) | 0.55 (0.44–0.68) | <.001 | −0.37 (−0.62– −0.13) | −31% (−46%– −12%) | .003 | ||
| - Hispanic male (vs. white female) | 1.65 (1.33–2.06) | <.001 | 0.53 (0.30–0.75) | 69% (36%–112%) | <.001 | ||
| - Total cholesterol, per 10 mg/dl | 1.057 (1.039–1.075) | <.001 | 0.0088 (−.008–.026) | 1% (−1%–3%) | .312 | ||
| - HDL cholesterol, per 10 mg/dl | 0.892 (0.854–0.931) | <.001 | 0.006 (−0.038–0.050) | 1% (−4%–5%) | .791 | ||
| - Current smoker | 1.57 (1.33–1.86) | <.001 | 0.22 (0.045–0.40) | 25% (5%–49%) | .014 | ||
| - Diabetes mellitus | 1.50 (1.25–1.78) | <.001 | 0.44 (0.28–0.61) | 56% (32%–84%) | <.001 | ||
| - Systolic blood pressure, per 10 mmHg | 1.112 (1.071–1.155) | <.001 | 0.078 (0.039–0.117) | 8% (4%–12%) | <.001 | ||
| - Taking blood pressure medications | 4.9 (2.4–10) | <.001 | 1.15 (0.43–1.87) | 217% (54%–551%) | 0.002 | ||
| - BPmeds * SBP, per 10 mg/dl|| | 0.912 (0.863–0.964) | .001 | −0.065 (−0.119– −0.011) | −6% (−11% – −1%) | 0.018 | ||
- Additional model parameters used for estimating coronary calcium distribution (see Table 3) for Models 1 / 2 / 3 were the intercepts for logistic models on the log-odds scale (−.9649322 / −6.439981 / −7.900618), intercepts for the linear regression model (3.645373 / −.4340681 / −1.411425) and the standard deviation of the residuals for the linear model (1.747866 / 1.701683 / 1.67148).
- The Framingham Risk Score, from National Cholesterol Education Program’s Adult Treatment Panel (ATPIII) guidelines3, with adjustment for diabetes status (see Methods).
- Here, “white” refers to non-Hispanic European-Americans. A Supplemental Table in the Online Materials shows coefficients for a similar model but without race/ethnicity included.
- Interaction between an indicator for taking blood pressure meds (BPmeds) and systolic blood pressure (SBP).
CHD – Coronary heart disease; CI – Confidence interval; HDL – High density lipoprotein; SBP – Systolic blood pressure; BPmeds – Blood pressure medications; FRS – Framingham Risk Score
A model adjusting for age, sex, race-ethnicity and conventional risk factors provided the best discrimination (cross-validated C-statistic .789) and explained the most variation in the CAC score (cross-validated R2 = .160; Table 2, Model 3). In a systematic model selection procedure, the model that used the individual predictor variables from the FRS (including an interaction between systolic blood pressure and use of blood pressure medications), as well as race-ethnicity and diabetes, performed as well or better than models containing additional interactions or nonlinear terms for continuous variables (i.e., no alternatives scored a C-statistic higher than 0.789). Even with adjustment for conventional CHD risk factors, race-ethnicity was a highly significant predictor of CAC; a similar model not including race-ethnicity did not perform as well (cross-validated C-statistic = .778, Supplemental Table in Online Materials). Stratification by race-ethnicity (achieved by inclusion of all pairwise interactions for race-ethnicity with other predictors in the model) did not result in better performance (cross-validated C-statistic = .788); stratification by diabetes status or by sex led to similar results (cross-validated C-statistic = .787 and .788, respectively).
The predicted CAC distribution varied markedly by characteristics of the individual (Table 3). The expected distribution of CAC shifts towards higher scores with increasing FRS (Table 3, panel 1) and even more so with male gender and higher age. For example, the probability of CAC = 0 decreases from 89% in 45 year-old women to 6% in 85 year-old men (Table 3, panel 2). Adding race/ethnicity and using the individual CHD risk factor measurements (instead of the overall FRS) along with age and sex (i.e., Model 3) yields personalized CAC score predictions for any given clinical scenario (examples shown in Table 3, panel 3).
Table 3.
Estimated prevalence of a coronary artery calcium score in each of four standard categories, depending on clinical characteristics
| Model - Clinical characteristics | Estimated prevalence of a CAC score in the given range†, %
|
|||
|---|---|---|---|---|
| 0 | 1–100 | 101–300 | >300 | |
| Model 1: FRS only*† | ||||
| - 2.5% | 66 | 23 | 6 | 5 |
| - 5.0% | 59 | 26 | 8 | 6 |
| - 7.5% | 52 | 30 | 10 | 8 |
| - 10.0% | 45 | 33 | 12 | 11 |
| - 12.5% | 38 | 35 | 14 | 14 |
| - 15.0% | 31 | 36 | 16 | 17 |
| - 17.5% | 25 | 37 | 18 | 20 |
| - 20.0% | 20 | 37 | 19 | 24 |
| Model 2: Age and sex only* | ||||
| - 45-year old woman | 89 | 9 | 1 | 0 |
| - 55-year old woman | 76 | 19 | 3 | 2 |
| - 65-year old woman | 55 | 30 | 8 | 6 |
| - 75-year old woman | 32 | 36 | 16 | 16 |
| - 85-year old woman | 16 | 32 | 21 | 31 |
| - 45-year old man | 75 | 20 | 3 | 2 |
| - 55-year old man | 53 | 31 | 9 | 7 |
| - 65-year old man | 31 | 36 | 17 | 17 |
| - 75-year old man | 14 | 31 | 22 | 33 |
| - 85-year old man | 6 | 22 | 22 | 50 |
| Model 3: All CHD risk factors, race/ethnicity (11 examples)*|| | ||||
| 1 – 45 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 160/60 mg/dl | 76 | 19 | 3 | 2 |
| 2 – 65 year old Asian woman with SBP = 110 mg/dl (no medication), TC/HDL = 160/80 mg/dl | 73 | 21 | 4 | 2 |
| 3 – 45 year old Hispanic woman with SBP = 150 mmHg (no medication), TC/HDL = 210/40 mg/dl who smokes | 84 | 14 | 1 | 0 |
| 4 – 60 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 150/65 mg/dl | 47 | 31 | 12 | 10 |
| 5 - 45 year old black woman with SBP = 145 mmHg on medication, TC/HDL = 240/40 mg/dl who smokes | 79 | 18 | 2 | 1 |
| 6 – 55 year old Hispanic man with SBP = 140 mmHg on medication, TC/HDL = 220/50 mg/dl | 49 | 33 | 10 | 8 |
| 7 – 75 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 170/80 mg/dl | 19 | 30 | 21 | 30 |
| 8 – 45 year old Asian woman with SBP = 155 mmHg on medication, TC/HDL = 250/40 mg/dl who smokes | 68 | 27 | 4 | 2 |
| 9 – 75 year old black man with SBP = 130 mmHg (no medication), TC/HDL = 180/55 | 31 | 34 | 17 | 18 |
| 10 – 55 year old Hispanic woman with SBP = 160 mmHg on medication, TC/HDL = 260/40 mg/dl who smokes | 56 | 34 | 7 | 4 |
| 11 – 80 year old white man with SBP = 130 mmHg on medication, TC/HDL = 210/60 mg/dl | 6 | 22 | 22 | 50 |
- Uses model parameters from Table 2 and the two-step estimation procedure described in the Methods section.
- The Framingham Risk Score, from National Cholesterol Education Program’s Adult Treatment Panel (ATPIII) guidelines3, with adjustment for diabetes status (see Methods).
- All possible combinations of risk factors cannot be described here; only selected scenarios are presented. Results for other clinical scenarios can be calculated using the Excel-based calculator available in the Online Materials. When not otherwise specified, we assumed non-smoker and non-diabetic.
CAC – Coronary artery calcium; CHD – Coronary heart disease; SBP – systolic blood pressure; TC – Total cholesterol; HDLC – High density lipoprotein cholesterol; FRS – Framingham Risk Score
The interpretation of these CAC scores must also be individualized. By integrating the personalized CAC score prediction with the pre-test risk, as from FRS, post-test risk estimates for each CAC score category can be obtained, and these differ sharply across scenarios (Table 4). While a CAC score of zero is generally reassuring (Table 4, all examples), a very high CAC score increases post-test risk only a little when pre-test risk is low (examples 1 and 2). Even more striking is the interpretation of an intermediate score (CAC = 1–100), which is remarkably different across scenarios. For example, in a white man without CHD risk factors, a CAC score of 50 reassuringly reduces the post-test risk estimate (example 7), while in a 55 year old Hispanic woman with many CHD risk factors, the same CAC score would predict an elevation in post-test risk (example 10). Even when pre-test 10-year CHD risk is held constant, such as at 10% (examples 5–7), post-test risk varies markedly depending on the pattern of risk factors. In the elderly white man without risk factors who achieves his pre-test of risk of 10% by virtue of his age alone, even a high CAC score > 100, or even > 300, is quite likely and not overly worrisome (example 7); but in a black woman who achieves her pre-test risk of 10% because of her adverse CHD risk factor profile, a CAC score over 100 would be very rare, and a score between 1–100 would be alarmingly high (example 5). In a middle-aged Hispanic man with a CHD risk of 10%, CAC = 1–100 changes pre-test risk only slightly, while any CAC score over 100 would be concerning (example 6). Note that in all of these “intermediate risk” cases, the likelihood of obtaining a CAC score that might either reassure (post-test risk < 5%) or raise concern (post-test risk > 20%) is relatively high. In patients with high pre-test risk (examples 10 and 11), the likelihood of obtaining a score indicating a post-test risk ≤ 10%, which might decrease the urgency or aggressiveness of preventive therapies, is also moderately high. The Excel-based calculator provided in the Supplemental Materials can be used to obtain these estimates for any given combination of risk factors.
Table 4.
Using the coronary artery calcium score with conventional cardiovascular risk factors to estimate future risk: 11 examples using Model 3
| Clinical scenario|| | Pre-test 10-year CHD risk estimate* | CAC score category | Proportion of CAC scores falling within the given category† | Post-test 10-year risk estimate for each CAC score category‡ |
|---|---|---|---|---|
| 1 – 45 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 160/60 mg/dl | 0: | .76 | 1% | |
| 1% | 1–100: | .19 | 2% | |
| 101–300: | .03 | 5% | ||
| >300: | .02 | 6% | ||
|
| ||||
| 2 – 65 year old Asian woman with SBP = 110 mg/dl (no medication), TC/HDL = 160/80 mg/dl | 0: | .73 | 0% | |
| 1% | 1–100: | .21 | 1% | |
| 101–300: | .04 | 3% | ||
| >300: | .02 | 4% | ||
|
| ||||
| 3 – 45 year old Hispanic woman with SBP = 150 mmHg (no medication), TC/HDL = 210/40 mg/dl who smokes | 0: | .84 | 4% | |
| 5% | 1–100: | .14 | 13% | |
| 101–300: | .01 | 25% | ||
| >300: | .00 | 31% | ||
|
| ||||
| 4 – 60 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 150/65 mg/dl | 0: | .47 | 1% | |
| 5% | 1–100: | .31 | 5% | |
| 101–300: | .12 | 10% | ||
| >300: | .10 | 13% | ||
|
| ||||
| 5 - 45 year old black woman with SBP = 145 mmHg on medication, TC/HDL = 240/45 mg/dl who smokes | 0: | .79 | 6% | |
| 10% | 1–100: | .18 | 20% | |
| 101–300: | .02 | 38% | ||
| >300: | .01 | 45% | ||
|
| ||||
| 6 – 55 year old Hispanic man with SBP = 140 mmHg on medication, TC/HDL = 220/50 mg/dl | 0: | .49 | 3% | |
| 10% | 1–100: | .33 | 12% | |
| 101–300: | .10 | 23% | ||
| >300: | .08 | 28% | ||
|
| ||||
| 7 – 75 year old white man with SBP = 120 mmHg (no medication), TC/HDL = 170/80 mg/dl | 0: | .19 | 2% | |
| 10% | 1–100: | .30 | 6% | |
| 101–300: | .21 | 13% | ||
| >300: | .30 | 16% | ||
|
| ||||
| 8 – 45 year old Asian woman with SBP = 155 mmHg on medication, TC/HDL = 250/40 mg/dl who smokes | 0: | .68 | 7% | |
| 15% | 1–100: | .27 | 25% | |
| 101–300: | .04 | 46% | ||
| >300: | .02 | 54% | ||
|
| ||||
| 9 – 75 year old black man with SBP = 130 mmHg (no medication), TC/HDL = 180/55 | 0: | .31 | 3% | |
| 15% | 1–100: | .34 | 12% | |
| 101–300: | .17 | 24% | ||
| >300: | .18 | 29% | ||
|
| ||||
| 10 – 55 year old Hispanic woman with SBP = 160 mmHg on medication, TC/HDL = 260/40 mg/dl who smokes | 0: | .56 | 8% | |
| 20% | 1–100: | .34 | 27% | |
| 101–300: | .07 | 49% | ||
| >300: | .04 | 57% | ||
|
| ||||
| 11 – 80 year old white man with SBP = 130 mmHg on medication, TC/HDL = 210/60 mg/dl | 0: | .06 | 3% | |
| 20% | 1–100: | .22 | 10% | |
| 101–300: | .22 | 21% | ||
| >300: | .50 | 25% | ||
- The Framingham Risk Score, from the National Cholesterol Education Program’s Adult Treatment Panel (ATPIII) guidelines3. Note: FRS estimates do not depend on race/ethnicity; for an alternate analysis with recalibration for race/ethnicity, see Supplemental Material.
- Uses model parameters from Table 2 (Model 3) and the two-step estimation procedure described in the Methods section. Results are identical to the last panel of Table 3.
- Post-test risk estimates are calculated by assuming that the pre-test 10-year CHD risk estimate represents an average of persons with different CAC scores, weighted by the probability of having a CAC score in each category†. The risk in each category is calculated algebraically using these relative risk estimates from Detrano et al2: CAC=0: Reference; CAC=1–100: 3.61; CAC=101–300: 7.73; CAC>300: 9.67. Resulting risk scores are rounded to the nearest whole percentage. See Methods for details.
- All possible combinations of risk factors cannot be described here; only selected scenarios are presented. Results for other clinical scenarios can be calculated using the Excel-based calculator available in the Online Materials. Where the risk factor level is not specified, we used SBP = 120, no blood pressure medications, TC = 160, HDL = 55, non-smoker, non-diabetic. Note: Pre- and Post-test risk cannot be calculated for diabetics; see Methods.
CHD – Coronary heart disease; CAC score – Coronary artery calcification score; SBP – systolic blood pressure; TC – Total cholesterol; HDLC – High density lipoprotein cholesterol
DISCUSSION
We show here that the distribution and interpretation of the CAC score is critically dependent on individual characteristics of the patient. Interpretation of the measured CAC score differs sharply in different clinical scenarios, even when the overall pre-test CHD risk is similar. It is not enough to know that a patient is “intermediate risk”; one must also have information about which risk factors led to that designation in order to interpret the CAC score. The methods and estimates provided here provide powerful “personalized” predictions that can help clinicians decide when to order a CAC scan and how to interpret the results in order to optimize targeting of CHD prevention interventions.
Our finding that CAC is related to conventional CHD risk factors is consistent with prior studies that consistently demonstrate associations between CAC and conventional risk factors, including age and sex4, 5 as well as blood pressure, lipids, diabetes and smoking6, 7. No prior studies have shown an association between blood pressure medication use and CAC, but this relationship is presumably mediated by past longterm exposure to higher average blood pressure, and prior studies have shown strong relationships between cumulative lifetime exposure to cardiovascular risk factors and CAC21, 22. The relationship with race-ethnicity has also been described5. Unlike prior studies showing the general relationship between the overall FRS and CAC23, we demonstrate here that fitting the CAC score against the individual component CHD risk factor measurements, along with race-ethnicity, provides more accurate CAC score predictions (even when subjected to cross-validation) than using the overall FRS without refitting the components. Our multivariable models provide estimates of the independent associations between risk factors and coronary calcium, as well as a more accurate method for estimating the expected distribution of CAC in any given clinical setting.
The findings are generally consistent with Bayesian reasoning and risk reclassification theory1, 8, 24, 25, which suggest that CAC testing may be most useful for persons who start out as having an “intermediate risk” for CHD. In the examples we provide, the likelihood of obtaining a CAC score that might change management (i.e., pushing it outside of a putative “gray zone” between 5%–20% 10-year risk) is highest in persons with an intermediate pre-test CHD risk (Table 4, examples 5–7, and also 3–4 and 8–9), and is very low in persons who are at very low pre-test risk (examples 1–2). Prior analyses of MESA focusing on reclassification methodology provide empiric evidence for the relatively high reclassification rates we project in our analyses10. Our analyses also project a relatively high rate of downwards reclassification of risk among persons who start off with high CHD risk (examples 10–11), consistent with prior reports of the high negative predictive value of a CAC score of 08, 26, 27.
Unlike prior studies, however, our analysis highlights how important it is to “personalize” the interpretation of the CAC score. While prior studies reported differences in post-test risk for different CAC scores2, they did not compare post-test risk with pre-test risk. Our analyses show that post-test risk changes a different amount in different patients, and sometimes even in the opposite direction, as illustrated most clearly for a CAC score of 1–100 in Table 4 (examples 3, 5 and 8 vs. 7, 9 and 11). The critical factor determining how risk changes from pre- to post-test, as reported theoretically by prior investigators9, is how the actual test result compares with the expected test result in the individual patient (i.e., the conditional “prevalence”9 of that test result). Simply stated, a given test result (e.g., CAC = 50) may be either higher or lower than expected, and the risk estimate should logically shift higher or lower in accordance. By carefully defining the expected test result distribution for a patient, individualized using that patient’s risk factor measurements, we can optimally “personalize” the interpretation of that patient’s CAC score and quantify the expected shift from pre- to post-test in that patient.
No prior studies have presented methods for estimating the expected distribution of the CAC score in any given clinical setting that accounts for both demographic factors (including race-ethnicity) and carefully measured conventional CHD risk factors. The MESA Arterial Age Calculator28 provides CHD risk estimates that use CAC, but they don’t account for the strong correlations between risk factors (other than age) and CAC. In a prior publication7, we presented methods and results similar to what we present here, but that analysis used a convenience sample of patients referred in a clinical context (or self-referred) for a CAC score measurement, and the only information on conventional CHD risk factors was self-reported presence or absence (no continuous measurements). No race-ethnicity information was available. Unlike our prior report, the current results use high-quality measurements of CHD risk factors, take into account degree of elevation (e.g., for blood pressure or cholesterol), and account for the strong effects of race-ethnicity.
Our analysis is subject to a number of important limitations. MESA is a community-based sample including 6 US cities across the country; but it is still possible that participants in the study were not perfectly representative of the US population. For example, research participants are known to be healthier on average than non-participants. While measures of association are relatively robust to this type of selection pressure, the intercepts for our models (which determine overall average prevalence/score) might be subject to selection bias and lower than the average for the population.
Similarly, the FRS pre-test CHD risk estimates used for illustration in Table 4 (and thus the corresponding post-test estimates in that same table) may not always be generalizable given that it was derived from the all-white Framingham study cohort. Methods and estimates required for “recalibration” have been published15. We used these methods to calculate recalibrated 5-year CHD risk scores for race-sex groups for which this is possible, and present an alternate version of Table 4 in the Supplemental Material (Supplemental Table 2; other results are unaffected). Other such substitutions are easily accomplished, and a “user-defined” pre-test risk option is provided in the Excel calculator provided in the Supplemental Material.
Our method of using the CAC score together with conventional CHD risk factors (Table 4) depends on the assumption that the relative risk for CHD associated with different levels of CAC2 is constant across different participant characteristics. For example, the relative risk of 7.73 for a person with a CAC score of 200 vs. a CAC score of 0 is assumed to hold for both young healthy women and for older men with risk factors. While there is evidence that CAC is very predictive across categories of race/ethnicity2, age29, and overall CHD risk30, systematic testing for and quantification of this type of interaction have not been conducted.
These results represent an attempt at producing a clinically-relevant method for using the CAC score in clinical practice. Our results should help clinicians make the decision about when the test is likely to yield actionable results, and how to interpret the CAC score in the light of the patient’s individual risk profile based on their conventional CHD risk factors. The post-test risk estimate can then be used (in place of the pre-test risk estimate) as a more “personalized” guide for how aggressive to be with interventions to prevent the onset of clinical CHD. The net comparative effectiveness and efficiency (cost-effectiveness) of this approach, however, have not been proven. To do so would require randomized controlled trials of an integrated screening and targeted prevention strategy31 or careful modeling of expected benefits, harms and costs32.
Supplementary Material
Clinical Summary.
The coronary artery calcium (CAC) score is a strong predictor of coronary heart disease (CHD) events, but it is not always clear how to interpret the score in the context of a patient’s conventional CHD risk factors like blood pressure, cholesterol, smoking status, etc. This analysis of the Multi-Ethnic Study of Atherosclerosis (MESA) provides a way for clinicians to use conventional CHD risk factor information about a patient to understand how high a CAC score to expect. When the actual score is higher than expected, a clinician’s estimate of that patient’s CHD risk (the “pre-test” risk, for example from Framingham equations), should be adjusted upwards; if it is lower than expected, the clinician’s estimate should be revised downwards. This article describes a method for making this adjustment, and provides examples illustrating the importance of individualized interpretation of the CAC score. These methods may be useful for clinicians deciding when to order a CAC score and how to interpret the results.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Funding Sources: Drs. Pletcher, Pignone and Greenland were supported by a grant from the National Heart, Lung and Blood Institute (R21HL112256). MESA was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-RR-024156 and UL1-RR-025005 from NCRR. Dr. Sibley was supported by the intramural research program of the NIH Clinical Center.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS, Harrington RA, Abrams J, Anderson JL, Bates ER, Grines CL, Hlatky MA, Lichtenberg RC, Lindner JR, Pohost GM, Schofield RS, Shubrooks SJ, Jr, Stein JH, Tracy CM, Vogel RA, Wesley DJ. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 2.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 3.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Janowitz WR, Agatston AS, Kaplan G, Viamonte M., Jr Differences in prevalence and extent of coronary artery calcium detected by ultrafast computed tomography in asymptomatic men and women. Am J Cardiol. 1993;72:247–254. doi: 10.1016/0002-9149(93)90668-3. [DOI] [PubMed] [Google Scholar]
- 5.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 6.Hoff JA, Daviglus ML, Chomka EV, Krainik AJ, Sevrukov A, Kondos GT. Conventional coronary artery disease risk factors and coronary artery calcium detected by electron beam tomography in 30,908 healthy individuals. Ann Epidemiol. 2003;13:163–169. doi: 10.1016/s1047-2797(02)00277-6. [DOI] [PubMed] [Google Scholar]
- 7.Pletcher MJ, Tice JA, Pignone M, McCulloch C, Callister TQ, Browner WS. What does my patient’s coronary artery calcium score mean? Combining information from the coronary artery calcium score with information from conventional risk factors to estimate coronary heart disease risk. BMC Med. 2004;2:31. doi: 10.1186/1741-7015-2-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blaha MJ, Blumenthal RS, Budoff MJ, Nasir K. Understanding the utility of zero coronary calcium as a prognostic test: a Bayesian approach. Circ Cardiovasc Qual Outcomes. 2011;4:253–256. doi: 10.1161/CIRCOUTCOMES.110.958496. [DOI] [PubMed] [Google Scholar]
- 9.Kooter AJ, Kostense PJ, Groenewold J, Thijs A, Sattar N, Smulders YM. Integrating information from novel risk factors with calculated risks: the critical impact of risk factor prevalence. Circulation. 2011;124:741–745. doi: 10.1161/CIRCULATIONAHA.111.035725. [DOI] [PubMed] [Google Scholar]
- 10.Polonsky TS, McClellan RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O’Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 12.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 13.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 14.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershaltz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 15.D’Agostino RB, Grundy S, Sullivan LM, Wilson PW. Validation of the Framingham Coronary Heart Disease Prediction Scores. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 16.Newman AB, Naydeck BL, Sutton-Tyrrell K, Feldman A, Edmundowicz D, Kuller LH. Coronary artery calcification in older adults to age 99: prevalence and risk factors. Circulation. 2001;104:2679–2684. doi: 10.1161/hc4601.099464. [DOI] [PubMed] [Google Scholar]
- 17.Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning. 2. Chapter 7. New York: Springer; 2009. [Google Scholar]
- 18.Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–165. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 19.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 20.Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med. 2004;164:1285–1292. doi: 10.1001/archinte.164.12.1285. [DOI] [PubMed] [Google Scholar]
- 21.Pletcher MJ, Bibbins-Domingo K, Lewis CE, Wei GS, Sidney S, Carr JJ, Vittinghoff E, McCulloch CE, Hulley SB. Prehypertension during young adulthood and coronary calcium later in life. Ann Intern Med. 2008;149:91–99. doi: 10.7326/0003-4819-149-2-200807150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pletcher MJ, Bibbins-Domingo K, Liu K, Sidney S, Lin F, Vittinghoff E, Hulley SB. Non-optimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA (Coronary Artery Risk Development in Young Adults) Study. Ann Internal Med. 2010;153:137–146. doi: 10.1059/0003-4819-153-3-201008030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okwuosa TM, Greenland P, Ning H, Liu K, Bild DE, Burke GL, Eng J, Lloyd-Jones DM. Distribution of coronary artery calcium scores by Framingham 10-year risk strata in the MESA (Multi-Ethnic Study of Atherosclerosis) potential implications for coronary risk assessment. J Am Coll Cardiol. 2011;57:1838–1845. doi: 10.1016/j.jacc.2010.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–935. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 25.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207–112. [DOI] [PubMed] [Google Scholar]
- 26.Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, Callister T, Raggi P, Blumenthal RS, Nasir K. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging. 2009;2:692–700. doi: 10.1016/j.jcmg.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 27.Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffman U, Cury RC, Abbara S, Brady TJ, Budoff MJ, Blumenthal RS, Nasir K. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2:675–688. doi: 10.1016/j.jcmg.2008.12.031. [DOI] [PubMed] [Google Scholar]
- 28.McClelland RL, Nasir K, Budoff M, Blumenthal RS, Kronmal RA. Arterial age as a function of coronary artery calcium (from the Multi-Ethnic Study of Atherosclerosis [MESA]) Am J Cardiol. 2009;103:59–63. doi: 10.1016/j.amjcard.2008.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tota-Maharaj R, Blaha MJ, McEvoy JW, Blumenthal RS, Muse ED, Budoff MJ, Shaw LJ, Berman DS, Rana JS, Rumberger J, Callister T, Rivera J, Agatston A, Nasir K. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J. 2012;33:2955–2962. doi: 10.1093/eurheartj/ehs230. [DOI] [PubMed] [Google Scholar]
- 30.Nasir K, Rubin J, Blaha MJ, Shaw LJ, Blankstein R, Rivera JJ, Khan AN, Berman D, Raggi P, Callister T, Rumberger JA, Min J, Jones SR, Blumenthal RS, Budoff MJ. Interplay of coronary artery calcification and traditional risk factors for the prediction of all-cause mortality in asymptomatic individuals. Circ Cardiovasc Imaging. 2012;5:467–473. doi: 10.1161/CIRCIMAGING.111.964528. [DOI] [PubMed] [Google Scholar]
- 31.Ambrosius WT, Polonsky TS, Greenland P, Goff DC, Jr, Perdue LH, Fortmann SP, Margolis KL, Pajewski NM. Design of the value of imaging in enhancing the wellness of your heart (VIEW) trial and the impact of uncertainty on power. Clin Trials. 2012;9:232–246. doi: 10.1177/1740774512436882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pletcher MJ, Pignone M. Evaluating the clinical utility of a biomarker: a review of methods for estimating health impact. Circulation. 2011;123:1116–1124. doi: 10.1161/CIRCULATIONAHA.110.943860. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.