Abstract
This study examined non-maternal involvement in feeding during the first two years of life and its association with breastfeeding duration, early introduction of complementary foods, and dietary intakes of selected foods and beverages. Data were from the Infant Care, Feeding and Risk of Obesity Study, a cohort of 217 low-income, African-American mother-infant dyads, followed from 3-18 months postpartum. Non-maternal caregivers (NMCs) were defined as persons involved in feeding an infant/toddler 50% or more of the total daily feedings. Use of any NMC and the type of NMC was tabulated for each study visit (3, 6, 9, 12, and 18 months). At each time point, more than half of all households reported a NMC. Fathers, grandmothers, and licensed childcare providers were the most common types of NMCs. In longitudinal models adjusted for confounding variables, NMC use was associated with a decreased likelihood of continued breastfeeding, and an increased likelihood of infants and toddlers consuming juice or whole fruit. Given the high prevalence of non-maternal involvement in feeding, interventions targeting multiple family members are warranted as they are likely to be more effective than those targeting the mother alone.
Keywords: infant, toddler, feeding, caring, obesity
Introduction
It is well documented that the prevalence of obesity among children and adolescents ages two to 19 years has more than tripled since 1980 (Ogden and Carroll 2010). Among infants and toddlers, the increase has been smaller, yet still substantial—in 2010 compared to 1976-1980, 35% more children less than two years had a high weight-for-length z-score (WLZ) (WLZ ≥95th percentile) (Ogden et al. 2002, 1728-1732; Ogden et al. 2012, 483-490). In light of these trends, obesity prevention has begun earlier in life, with a growing number of interventions targeting risk factors during the first two years (Ciampa et al. 2010, 1098-1104).
There are several dietary factors occurring during infancy which may have protective effects against later obesity. Several meta-analyses have reported similar findings that breastfeeding confers a small, protective effect against obesity or overweight in childhood or adolescence (OR=0.78, 95% CI: 0.72-0.84)(Arenz et al. 2004, 1247-56; Horta et al. 2007). Duration of any breastfeeding may be particularly important in light of the findings by Harder, Bergmann, Kallischnigg, and Plagemann (2005) that each month of breastfeeding was associated with a four percent decrease in the risk of overweight (95% CI: 0.94, 0.98)(Harder et al. 2005, 397-403).
Several factors during the period of complementary feeding may also play a role in obesity prevention. Complementary feeding is the transitional process between exclusive milk feeding in which nutritive foods and beverages other than breast milk or infant formula are gradually introduced. Both the American Academy of Pediatrics and the World Health Organization recommend that complementary feeding begin at six months, after a period of exclusive breastfeeding(American Academy of Pediatrics Committee on Nutrition 2009, 113-29; World Health Organization 2003). However, many infants are fed complementary foods before this time(Grummer-Strawn, Scanlon, and Fein 2008, S36-42; Wasser et al. 2011, 229-237), some as early as seven to 10 days postpartum(Bronner et al. 1999, 457-61). In a recent systematic review, Moorcroft, Marshall and McCormick (2011) reported no clear association between the age of introduction of complementary foods and obesity (Moorcroft, Marshall, and McCormick 2011, 3-26). However, studies were highly heterogeneous in terms of the exposure (early introduction to complementary foods) and the outcome (infant and child obesity) preventing the conduct of a meta-analysis and the ability to make robust conclusions.
A less studied but emerging area of interest is the quality of the diet during the span of complementary feeding. Several rounds of data from the Feeding Infants and Toddlers Study (FITS), a nationally representative sample of young children from birth to four years, have raised concern about the quality of the diet during this time of transition (Fox et al. 2004a, s22-30; Skinner et al. 2004, s65-70; Skinner, Ziegler, and Ponza 2004, s45-50; Siega-Riz et al. 2010, S38-51). The latest estimates from FITS continue to show that approximately 25% of infants and toddlers fail to consume any amount of whole fruit and 30% consume no whole vegetables on a given day. In contrast, nearly 20% of infants, ages six to 8.9 months, consume a dessert or sweet in a day, with the proportion increasing to 80.6% of toddlers consuming such foods at 21-23.9 months (Siega-Riz et al. 2010, S38-51). While the data is limited among infants and toddlers (Dattilo et al. 2012, 123023), these patterns are troubling since low intakes of whole fruits and vegetables and high intakes of energy-dense foods, such as desserts and sweets and sweetened beverages, have been associated with obesity among older children and adults (Flynn et al. 2006, 7-66; Swinburn et al. 2004, 123-146).
An important social change paralleling the rise in childhood obesity is the increase in mothers participating in the labor force (Anderson and Butcher 2006, 19-45). Between 1970 and 2000, the rate of mothers in the labor force, either employed or looking for work, increased from 38% to 68%(Ehrle, Adams, and Tout 2001). The increase was even more dramatic among mothers with children under the age of three, with 24% of such mothers in the labor force in 1970 and 57% in 2000 (Bianchi and Casper 2000; Ehrle, Adams, and Tout 2001)(merged). These changes in maternal employment have had implications for childcare arrangements of young children while the mother is working. The use of non-parental care begins early in life, with approximately half of all 9-month-olds in a regular non-parental care arrangement: 26% in relative care, 15% in non-relative care, 9% in center-based care, and 1% in multiple arrangements (Mulligan et al. 2005).
Despite these social changes, relatively little is known about the types of non-maternal caregivers involved in feeding infants and toddlers and the impact they may have on early dietary habits. To fill this gap, the current study sought to answer several research questions. To what extent do non-maternal caregivers share responsibility for feeding during the first two years of life? What types of non-maternal caregivers are used most frequently? Is NMC involvement associated with breastfeeding, timing of introduction of complementary foods, and dietary intakes among infants and toddlers?
Methods
Study design and participants
Data are from the Infant Care, Feeding and Risk of Obesity Study (Infant Care), an observational cohort of 217 low-income mother-infant dyads from 3 to 18 months after delivery (Slining et al. 2009, 51; Slining et al. 2010, 20-25.e1; Thompson et al. 2009, 210-221; Wasser et al. 2011, 229-237). First-time African-American mothers aged 18 to 35 years were recruited through the North Carolina Supplemental Nutrition Program for Women Infants and Children (WIC) and assessed during in-home visits at infant ages 3, 6, 9, 12, and 18 months. Exclusion criteria for the Infant Care Study included delivery at <35 weeks gestation or presence of any of the following conditions: Down syndrome, epilepsy, cleft lip/palate, cerebral palsy, failure to thrive, mental retardation, severe food allergies, and any condition that might affect appetite, feeding, or growth. Data were collected from 2003 to 2007. The institutional review board of the University of North Carolina at Chapel Hill approved this study.
Measures
Non-maternal caregivers
Non-maternal caregivers (NMCs) were defined in Infant Care as those persons involved in feeding an infant or toddler 50% or more of his/her total feedings in a day. At each study visit, NMCs were identified through a series of three questions. First, the mother was asked how many times the index child was usually fed in a day. Fifty percent of this number was then calculated and mothers were asked if there was anyone, other than herself, responsible for feeding the index child that number of times (or more) in a day. If the mother affirmed use of a NMC, she was asked how the person was related to the index child. A total of six variables were created, one representing any use of a NMC and five representing the type of NMC. Categories for type of NMC included father, grandmother, other relative (e.g. aunt, cousin), non-relative (e.g. babysitter, nanny), and licensed child care provider, which included child care centers and family day care homes.
Infant and toddler dietary intake
During each home visit, mothers completed a questionnaire assessing current breastfeeding status (still breastfeeding “yes/no”) and a 24-hour dietary recall (DR). To improve estimates of usual food intakes, the Infant Care Study collected two additional 24-hour DRs, which were taken by telephone on random, nonconsecutive days within two weeks of the home visit (Thompson and Subar 2008, 3-40; 1). Mothers were aware of the timing of home visits and telephone recalls and were instructed in advance to obtain information about any foods and beverages consumed by the infant while not in her care. The 24-hour DR was administered and analyzed using the 2005 version of the Nutrition Data System for Research (NDSR) (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). Study personnel were trained by an NDSR–certified staff member of the University of North Carolina at Chapel Hill Nutrition Epidemiology Core.
We used data from NDSR to create several variables of interest, including early introduction to complementary foods before four months of age and intake of a series of foods and beverages associated, either positively or negatively, with obesity among older children and adults (Flynn et al. 2006, 7-66; Swinburn et al. 2004, 123-146), namely low energy-dense foods (whole fruits and whole vegetables) and foods and beverages high in energy-density (100% juice, fried potatoes, desserts and sweets, sweetened beverages, and salty snacks). This latter set of variables was patterned after the major and minor food groups utilized in FITS (Fox et al. 2004b, s22-30; Siega-Riz et al. 2010, S38-51). For each of these major and minor food groups, two variables were created: the proportion of infants and toddlers consuming any amount, and total daily servings consumed. Serving sizes rather than gram amounts were chosen as serving sizes are based on commonly used household metrics, such as cups, ounces, and tablespoons, and may be easier for researchers and public health workers to translate to parents and caregivers. When reporting servings of the major and minor food groups of interest, we adjusted the NDSR adult-based serving sizes to those appropriate for infants and toddlers, as has been done in previous studies (Hoerr et al. 2006, 1766-1773; Cox et al. 1997, 1382-6; quiz 1387-8). This is a necessary step as the serving sizes in NDSR are adult-sized—drawn from the Dietary Guidelines for Americans (DGAs) or, for foods that are not recommended in the DGAs, the food-label serving sizes from the Food and Drug Administration. Age-adjusted serving sizes were based on the ratio of infant to adult energy requirements. For example, to calculate the age-adjustment factor for a 6-month-old boy, the dietary reference intake (DRI) for energy for a 6-month-old boy at the median weight-for-age was divided by the DRI for energy for a 30-year-old male with a healthy body-mass-index (BMI) (18.5-24.9) and low-active to active lifestyle (Institute of Medicine 2005). Calculations were done separately for boys and girls at each age (6, 9, 12, and 18 months). However, ratios did not differ by gender, resulting in the following single set of adjustment factors: 3.92 at 6 months, 3.45 at 9 months, 3.08 at 12 months, and 2.63 at 18 months. Examples of age-adjusted serving sizes for selected food items are provided in Table 1.
Table 1.
Examples of age-adjusted serving sizes for selected food items.
| Food item | NDSR Adult Serving Size | Age-adjusted Serving Size
|
|
|---|---|---|---|
| Age (mo)
| |||
| 6 and 9a | 12 and 18b | ||
| Fruit juice | 4 fl oz | 1 fl oz | 1½ fl oz |
| Fruit, fresh, frozen, or canned | ½ cup chopped (8 Tbsp) | 2 Tbsp | 3 Tbsp |
| Vegetables, raw, cooked, or canned | ½ cup chopped | 2 Tbsp | 3 Tbsp |
| Fried potatoes | ½ cup (10-14 fries) | 2 Tbsp (3-4 fries) | 3 Tbsp (4-5 fries) |
| Cookies, chocolate chip, commercially prepared | 30 g (2½ cookies) | 8 g (2/3 cookie) | 11 g (1 cookie) |
| Sweetened beverages | 8 fl oz | 2 fl oz | 3 fl oz |
| Ice cream | ½ cup | 1/8 cup (2 Tbsp) | 3 Tbsp |
| Cheese puffs | 28 g (32 pieces) | 0.3 ounces (8-9 pieces) | 10 g (11-12 pieces) |
Servings at both and six and nine months are approximately one-quarter that of an adult
Servings at both and 12 and 18 months are approximately one-third that of an adult
Confounding variables
Potential confounding variables were drawn from the literature and include factors associated with infant and toddler feeding practices (Hendricks et al. 2006a, S135-48) as well as non-maternal caregiving in general (Bianchi and Casper 2000; Ehrle, Adams, and Tout 2001). These maternal and household characteristics encompass: any maternal employment, any maternal college education, maternal age, marital status, and maternal depression. Maternal depression was measured using the Center for Epidemiological Studies Depression Scale, with a score of 16 or greater indicating the presence of maternal depressive symptoms (Radloff 1977, 385).
Statistical analyses
Descriptive statistics were used to examine study variables at each time point (3, 6, 9, 12, and 18 months) with the exception of daily servings of foods and beverages during the period of complementary feeding. We do examine ‘any intake’ of foods and beverages between three to 18 months, but examination of daily servings would require calculation of serving sizes for three-month-olds, which is inappropriate for infants younger than six months. This step revealed positively skewed distributions for the daily serving size variables, with heavy clustering at zero (i.e., many non-consumers of particular foods or beverages). For these variables, we present the data in terms of the proportion of infants or toddlers consuming any amount of a food group or food item as well as the median among consumers only. We also examined cross-tabulations at each time point between any NMC usage or type of NMC usage and dichotomous variables expected to change over time (still breastfeeding and any intake of selected foods and beverages). This step revealed small cell sizes for some cross-tabulations, which had implications for the number of visits included in longitudinal models. For each model, we specify the number of visits included and the sample size.
To examine longitudinal associations between maternal and household characteristics and NMC variables, we used random-effects logistic regression models in which NMC usage was the dependent variable and independent variables were selected maternal and household characteristics plus a series of dummy variables representing study visit. Next, we ran cross-sectional logistic regression models using data from the 3-month visit, one unadjusted and one adjusted for potential confounders, to test for associations between NMC usage and early introduction to complementary foods (<4 months). At the 3-month visit (n=217), 42 infants were between 2.7 and 2.9 months old, 162 were between 3.0 and 3.9 months old, and 1 was ≥4.0 months old. To determine longitudinal associations between NMC usage and the dichotomous dietary variables (any breastfeeding and any intake of selected foods and beverages), we ran a series of unadjusted and adjusted random-effects logistic regression models. Except for the ‘any breastfeeding’ variable, which included data between 3-9 months, the random-effects logistic regression models included dietary intake for a selected food group for all time points between 6-18 months as the dependent variable and NMC usage for all time points between 6-18 months as the main independent variable. These models test for concurrent associations between change in NMC usage with change in dietary intake. For daily servings of the selected foods and beverages, a similar set of random-effects tobit models were run, with lower limit censoring set at zero. Data presented are post-estimation marginal effects among consumers only [E(y∣y>0)]. Coefficients should be interpreted as the effect of NMC use versus no NMC use on the intake, among consumers only, of daily servings of selected foods and beverages.
Finally, differences in baseline characteristics between completers and non-completers were assessed at each study visit to test the effects of attrition. T-tests were used for continuous variables and chi-square or Fisher’s exact tests for categorical variables. Stata (release 12, 2012, StataCorp, College Station, TX) was used for all statistical procedures. Significance was set at P<0.05 for all tests.
Results
Sample characteristics
Among this sample of young, first-time, African-American mothers, there was generally a high prevalence of single-headed households and maternal obesity (Table 2). In an examination of attrition over time, tests of baseline differences between completers and non-completers revealed few significant differences. There were slightly more mothers at 12 months with at least some college education or who were married. At 18 months, slightly more mothers were married and household size was lower.
Table 2.
Characteristics of mothers and infants participating in the Infant Care, Feeding, and Risk of Obesity study.
| Study Visit
|
|||||
|---|---|---|---|---|---|
| 3-month | 6-month | 9-month | 12-month | 18-month | |
|
| |||||
| mean±SD/n(%) | |||||
| Total (n) | 217 | 161 | 165 | 151 | 129 |
| Infant characteristics | |||||
| Age (months) | 3.2±0.3 | 6.4±0.5 | 9.4±0.5 | 12.6±0.7 | 19.1±2 |
| Gestational age (weeks) | 39.5±1.5 | 39.6±1.4 | 39.5±1.4 | 39.6±1.4 | 39.5±1.4 |
| Birthweight (kg) | 3.2±0.5 | 3.3±0.5 | 3.2±0.5 | 3.2±0.5 | 3.2±0.5 |
| Female | 116 (53.5) | 85 (53.5) | 85 (51.8) | 80 (54.8) | 68 (52.7) |
| Weight-for-height Z score | 0.6±1 | 0.5±1.1 | 0.5±1.1 | 0.4±1.1 | 0.3±1.1 |
| Infant overweighta | 63 (29) | 41 (25.8) | 40 (24.4) | 32 (21.9) | 25 (19.4) |
| Maternal and household characteristics | |||||
| Age (years) | 22.7±3.8 | 22.9±3.8 | 23.3±4 | 23.7±3.9 | 24.3± |
| Maternal education | |||||
| Less than highschool | 58 (27.1) | 43 (26.7) | 45 (27.6) | 41 (27.3) | 35 (27.1) |
| Highschool graduate | 65 (30.4) | 45 (28) | 46 (28.2) | 37 (24.7)** | 34 (26.4) |
| Any college | 91 (42.5) | 73 (45.3) | 72 (44.2) | 72 (48)** | 60 (46.5) |
| Married | 21 (9.8) | 17 (10.6) | 19 (12.3) | 16 (11.8)* | 16 (15.8)** |
| Any maternal employment | 115 (53.7) | 97 (61.8) | 101 (63.5) | 83 (58.5) | 61 (60.4) |
| Maternal obesity (BMI≥30) | 96 (44.2) | 71 (44.1) | 73 (44.8) | 63 (42) | 55 (42.6) |
| Maternal depressionb | 62 (29.1) | 40 (27.6) | 37 (23.6) | 24 (17.1) | 35 (34) |
| Household size | 3.9±1.7 | 4.1±1.7 | 3.6±1.5 | 3.5±1.5 | 3.3±1.3** |
| Infant diet | |||||
| Ever breastfed | 151 (69.6) | 119 (73.9) | 119 (72.2) | 108 (72) | 94 (72.9) |
| Still breastfeeding | 49 (22.6) | 24 (14.4) | 19 (11.5) | 8 (5.2) | 3 (2.2) |
| Any intake of food groups/items | |||||
| Whole fruit | 55 (25.1) | 116 (72.1) | 111 (67.3) | 98 (64.9) | 88 (68.2) |
| Vegetables, excluding fried potatoes | 50 (22.8) | 113 (70.2) | 144 (87.3) | 136 (90.1) | 124 (96.1) |
| Juice | 53 (24.2) | 99 (61.5) | 130 (78.9) | 136 (90.1) | 117 (90.1) |
| Fried potatoes | 0 | 9 (5.6) | 33 (20) | 58 (38.4) | 71 (55) |
| Desserts and sweets, excluding beverages | 0 | 45 (28) | 105 (63.6) | 120 (79.5) | 121 (93.8) |
| Sweetened beverages | 3 (1.4) | 7 (4.4) | 33 (20) | 69 (45.7) | 89 (69) |
| Salty snacks | 1 (0.5) | 4 (2.5) | 12 (7.3) | 36 (23.8) | 59 (45.7) |
| Daily servings of food groups/items | |||||
| Whole fruit | -- | 1.8±0.3 | 1.9±0.2 | 2.1±0.4 | 1.7±0.2 |
| Vegetables, excluding fried potatoes | -- | 1.8±0.3 | 1.7±0.1 | 2±0.2 | 2.3±0.2 |
| Juice | -- | 2.3±0.3 | 2.9±0.4 | 4.9±0.4 | 5.3±0.5 |
| Fried potatoes | -- | 0.3±0.1 | 0.6±0.2 | 1.1±0.2 | 0.9±0.1 |
| Desserts and sweets, excluding beverages | -- | 1.4±0.4 | 1.4±0.2 | 1.6±0.3 | 2.2±0.2 |
| Sweetened beverages | -- | 0.2±0.2 | 0.7±0.2 | 1.2±0.2 | 1.5±0.2 |
| Salty snacks | -- | 0.2±0.1 | 0.1±0 | 0.6±0.1 | 0.9±0 |
>90th percentile 2000 CDC NCHS growth charts
Score ≥16 on the Center for Epidemiological Studies Depression Scale
Significantly different from baseline at P<0.05.
Significantly different from baseline at P<0.001.
Infant and toddler dietary intakes
Across study visits, approximately 30% of infants and toddlers consumed no whole fruit in a day, and at the majority of visits, a higher proportion of infants and toddlers consumed juice than whole fruit (Table 2). By 18-months, nearly all toddlers consumed at least some amount of whole vegetables. Few infants consumed fried potatoes, sweetened beverages, or salty snacks at six months; however, by 18-months, approximately half or more of all toddlers were consuming these foods or beverages. Nearly all 18-month-olds consumed at least some solid dessert or sweet in a given day.
When examining amounts, daily servings of whole fruits and vegetables excluding fried potatoes remained fairly stable over time. At any given age, infants and toddlers consumed approximately 1.8 servings of whole fruit in a day and 1.5-2.0 servings of vegetables. Conversely, average daily servings of most high energy-dense foods and beverages more than doubled between six and 18 months. Translated into common household measures, total daily servings among 18-month-olds were as follows: 5 tablespoons (Tbsp) of whole fruit, 7 Tbsp of vegetables excluding fried potatoes, 8 fluid ounces of juice, 4 French fries or tater tots, 1¼ chocolate chip cookies, 5 fluid ounces of sweetened beverages, and nearly 10 grams of salty snacks, such as 11-12 cheese puffs.
Use of non-maternal caregivers (NMCs)
More than half of all households reported the use of a NMC at each time point (Figure 1). The most frequent types of NMCs were fathers, grandmothers, and licensed childcare providers. The use of licensed childcare providers was significantly greater among older infants and toddlers, with the odds of a licensed childcare provider as the NMC being approximately three and four times greater among 12- and 18-month-olds than 3-month-olds, respectively (Table 3). Conversely, fathers may be more likely to share responsibility for feeding early in infancy as the odds for fathers, while non-significant, were lower at each time point compared to the 3-month-visit.
Figure 1.
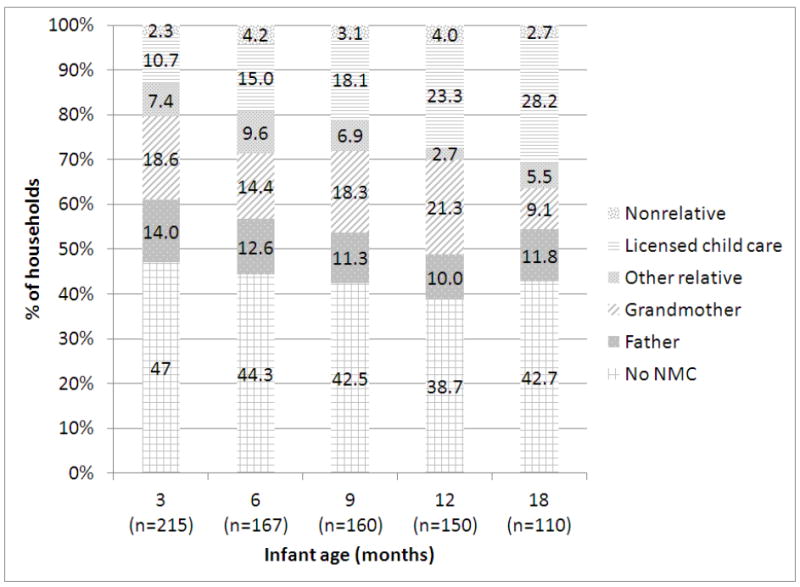
Use of non-maternal caregivers (NMCs), by infant age.
Table 3.
Longitudinal associations between maternal and household characteristics and use of non-maternal caregivers (NMCs), by any NMC and type of NMC (n=206).
| Any NMCa | Father as NMCa | Grandmother as NMCa | Licensed Provider as NMCa | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Odds Ratio (95% Confidence Interval) | ||||||||
| Any maternal employment | 6.19*** | 3.94, 9.75 | 1.81 | 0.95, 3.45 | 8.22*** | 3.65, 18.48 | 2.86** | 1.43, 5.72 |
| Married | 1.01 | 0.45, 2.25 | 7.38** | 2.37, 23.00 | 0.09* | 0.01, 0.94 | 1.18 | 0.30, 4.70 |
| Maternal depression | 1.10 | 0.70, 1.74 | 0.89 | 0.44, 1.81 | 0.68 | 0.32, 1.43 | 0.95 | 0.46, 1.97 |
| Any maternal college | 0.76 | 0.44, 1.36 | 0.81 | 0.34, 1.94 | 0.50 | 0.18, 1.39 | 1.99 | 0.72, 5.49 |
| Maternal age | 0.96 | 0.89, 1.03 | 0.89 | 0.78, 1.00 | 0.83* | 0.70, 0.97 | 1.03 | 0.90, 1.17 |
| Infant age | ||||||||
| 3 months (ref) | -- | -- | -- | -- | -- | -- | -- | -- |
| 6 months | 1.06 | 0.62, 1.81 | 0.81 | 0.37, 1.76 | 0.56 | 0.25, 1.28 | 1.80 | 0.76, 4.26 |
| 9 months | 1.14 | 0.65, 2.00 | 0.51 | 0.22, 1.20 | 1.32 | 0.59, 2.95 | 2.06 | 0.85, 4.97 |
| 12 months | 1.19 | 0.62, 2.29 | 0.40 | 0.14, 1.13 | 2.46 | 0.93, 6.53 | 2.79* | 1.01, 7.74 |
| 18 months | 1.04 | 0.52, 2.10 | 0.55 | 0.19, 1.59 | 0.64 | 0.20, 2.04 | 4.05* | 1.40, 11.68 |
Model includes data from visits 3-18.
P <0.05,
P <0.01,
P <0.001
Any maternal employment was the strongest predictor of NMC use, except for in the model specifically testing predictors of father involvement in feeding (Table 3). For fathers, being married was the strongest and only significant predictor of their involvement in feeding. In contrast, grandmother involvement in feeding was significantly less likely in married households and maternal age was inversely associated with their use.
NMCs and probability of dietary intake
There was no association between NMC use and early introduction of complementary foods (Table 4). However, there were several significant findings in longitudinal logistic regression models (Tables 4 and 5). Use of any NMC was associated with a 95% decrease in the odds of breastfeeding. This model only included data from 3-9 months due to low proportions of mothers still breastfeeding after this time. Use of any NMC was also associated with an increase in the odds of infants and toddlers consuming whole fruit or juice. By type of NMC, the only significant finding was that the use of grandmothers increased the odds of an infant or toddler consuming juice by 97%. In the adjusted models, several maternal characteristics were significantly associated with any intake of foods and beverages (data not shown). For example, in the adjusted model with any NMC as the dependent variable, a one-year increase in maternal age (years) was associated with an increased likelihood of consuming fruit [Odds Ratio (OR) = 1.09, 95% Confidence Interval (CI): 1.02, 1.16] and maternal depression with an increased likelihood of consuming fried potatoes (OR=2.14, 95% CI: 1.15, 3.99).
Table 4.
Results of logistic regression models examining associations between use of non-maternal caregivers (NMCs) and infant and young child feeding practices.
| Early Complementary Feedinga,b (n=209) |
Any Breastfeedinga,c (n=210) |
Any Whole Fruita,d (n=210) |
Any Vegetablesa,d (n=210) |
Any Juicea,d (n=210) |
|
|---|---|---|---|---|---|
|
| |||||
| Odds Ratio (95% Confidence Interval) | |||||
| Any NMC | 1.71 (0.83, 3.53) | 0.05 (0.00, 0.50) | 1.51 (1.03, 2.23) | 1.25 (0.79, 1.99) | 1.64 (1.01, 2.67) |
| Type of NMC | |||||
| Father | 1.32 (0.52, 3.35) | -- | 1.12 (0.64, 1.97) | 0.93 (0.48, 1.8) | 0.83 (0.42, 1.64) |
| Grandmother | 1.16 (0.51, 2.65) | -- | 0.92 (0.57, 1.5) | 0.89 (0.5, 1.59) | 1.97 (1.02, 3.81) |
| Licensed Provider | 1.69 (0.65, 4.42) | -- | 1.55 (0.93, 2.59) | 0.96 (0.52, 1.79) | 1.2 (0.61, 2.34) |
All models were adjusted for maternal employment, marital status, maternal depression, any maternal college, and maternal age
Cross-sectional model using only data from the 3-month visit.
Includes data from visits occurring between 3-9 months.
Includes data from visits occurring between 6-18 months.
Table 5.
Results of logistic regression models examining associations between use of non-maternal caregivers (NMCs) and infant and young child feeding practices.
| Any Fried Potatoesa,b (n=173) |
Any Desserts and Sweetsa,b (n=173) |
Any Sweetened Beveragesa,b (n=173) |
Any Salty Snacksa,b (n=173) |
|
|---|---|---|---|---|
|
| ||||
| Odds Ratio (95% Confidence Interval) | ||||
| Any NMC | 0.82 (0.46, 1.43) | 1.20 (0.77, 1.86) | 1.17 (0.65, 2.12) | 1.45 (0.67, 3.12) |
| Type of NMC | ||||
| Father | 1.13 (0.48, 2.69) | 0.85 (0.44, 1.67) | 1.71 (0.71, 4.11) | 2.06 (0.66, 6.39) |
| Grandmother | 0.97 (0.48, 1.96) | 0.74 (0.42, 1.28) | 0.97 (0.46, 2.05) | 1.03 (0.40, 2.69) |
| Licensed Provider | 0.75 (0.38, 1.48) | 1.30 (0.75, 2.26) | 1.28 (0.63, 2.62) | 0.71 (0.28, 1.79) |
All models were adjusted for maternal employment, marital status, maternal depression, any maternal college, and maternal age
Includes data from visits occurring between 6-18 months.
NMCs and amount of dietary intake
Results of longitudinal random-effects tobit models showed no significant associations between use of NMCs, neither by any NMC nor by type of NMC, on infant and toddler dietary intake (Tables 6 and 7). As with the ‘any intake’ models, several maternal characteristics were associated with daily servings of foods and beverages. In the adjusted model with any use of a NMC as the main independent variable, a one-unit increase in maternal age was associated with 0.05 more servings of whole fruit (95% CI: 0.01, 0.08); any maternal college with fewer servings of fried potatoes (β = -0.19, 95% CI: -0.02, -0.35), sweetened beverages (β = -0.22, 95% CI: -0.01, -0.43), and salty snacks (β = -0.2, 95% CI: -0.05, -0.35); and maternal depression with more servings of salty snacks (β = 0.2, 95% CI: 0.05, 0.35)
Table 6.
Results of longitudinal tobit models examining associations between use of non-maternal caregivers (NMCs) and daily servings of selected foods and beverages (n=173).
| Whole Fruita,b | Whole Vegetables (excluding fried potatoes)a,b | Fruit Juicea,b | |
|---|---|---|---|
|
| |||
| β (95% Confidence Interval)c | |||
| Any NMC | 0.04 (-0.18, 0.26) | -0.01 (-0.25, 0.24) | 0.27 (-0.2, 0.74) |
| Type of NMC | |||
| Father | -0.06 (-0.39, 0.26) | -0.23 (-0.57, 0.11) | -0.43 (-1.11, 0.24) |
| Grandmother | -0.13 (-0.41, 0.14) | 0.1 (-0.23, 0.42) | 0.49 (-0.18, 1.15) |
| Licensed Provider | 0.25 (-0.04, 0.53) | 0.05 (-0.25, 0.35) | 0.56 (-0.07, 1.2) |
All models were adjusted for maternal employment, marital status, maternal depression, any maternal college, and maternal age.
Models include data from visits occurring between 6-18 months.
Point estimates and confidence intervals are marginal effects among consumers[E(y|y>0)].
Table 7.
Results of longitudinal tobit models examining associations between use of non-maternal caregivers (NMCs) and infant and toddler dietary intakes (n=173).
| Fried Potatoesa,b | Desserts and Sweetsa,b | Sweetened Beveragesa,b | Salty Snacksa,b | |
|---|---|---|---|---|
|
| ||||
| β (95% Confidence Interval)c | ||||
| Any NMC | 0.02 (-0.12, 0.16) | 0.1 (-0.12, 0.33) | 0.06 (-0.13, 0.25) | 0.08 (-0.04, 0.21) |
| Type of NMC | ||||
| Father | -0.02 (-0.24, 0.20) | -0.06 (-0.40, 0.28) | 0.27 (-0.04, 0.58) | 0.07 (-0.13, 0.27) |
| Grandmother | 0.08 (-0.11, 0.27) | -0.07 (-0.36, 0.22) | -0.03 (-0.27, 0.21) | 0.02 (-0.14, 0.19) |
| Licensed Provider | 0.07 (-0.12, 0.25) | 0.16 (-0.12, 0.44) | 0.09 (-0.15, 0.32) | 0.04 (-0.12, -0.19) |
All models were adjusted for maternal employment, marital status, maternal depression, any maternal college, and maternal age.
Models include data from visits occurring between 6-18 months.
Point estimates and confidence intervals are marginal effects among consumers [E(y|y>0)].
Discussion
Knowing who shares responsibility for feeding during the first two years of life is important in light of the increasing number of obesity-prevention interventions aimed at infants and toddlers (Ciampa et al. 2010, 1098-1104). An examination of these interventions reveals that most target one primary caregiver, most often the mother. Data from the current study supports the need to consider inclusion of multiple caregivers, as we document, in a cohort of low-income African-American mother-infant dyads, a high prevalence of non-maternal involvement in feeding between three to 18 months of age.
At each time point, more than half of the mothers in the Infant Care sample were employed and the types of NMCs utilized in this study were similar to the primary care arrangements used by employed mothers in a national sample. According to data from the U.S. Census Bureau, employed mothers utilized the following types of care for their infants and toddlers while working: fathers (27% and 24.2%, respectively), grandmothers (34% and 30.5%, respectively) and licensed child care providers (27.5% and 37.2%, respectively) (Laughlin 2010). This finding adds another layer of complexity to the study of infant and toddler dietary intakes—the first two years of life is a period of fairly rapid exposure to a variety of foods and beverages, all of which is likely to be influenced by multiple caregivers, including their level of nutrition knowledge and their beliefs and behaviors about infant and toddler feeding (Scaglioni et al. 2011, 2006S-2011S).
Despite the high prevalence of non-maternal involvement in infant and toddler feeding, we document only a few associations between their use and early dietary intake. Even in models adjusted for confounding variables, use of NMCs was shown to decrease the odds of any continued breastfeeding. One logical explanation is that the use of a NMC is a proxy for a mother that must be away from her infant for reasons above and beyond that of employment, as this was controlled for in our models. It is also possible that our results reflect a cumulative effect of the negative role that each different type of caregiver might have on breastfeeding. Two of the strongest predictors of breastfeeding duration are a woman’s intention to breastfeed and her breastfeeding self-efficacy, each of which is influenced, positively or negatively, by people in her social network (Bentley et al. 1999b, 27-34; Bentley, Dee, and Jensen 2003, 305S-309S; DiGirolamo et al. 2005, 208-226; Meedya, Fahy, and Kable 2010, 135-145). There is also growing evidence on the importance of formal childcare arrangements, such as center-based licensed care, which has been associated with a decreased likelihood of breastfeeding as well as an increased likelihood of feeding complementary foods before four months (Kim and Peterson 2008, 627-33; Pearce et al. 2012, 39-42). The use of childcare could also be a proxy for a mother that is often away from her infant; however, recent studies have documented the need for breastfeeding-friendly policies and practices in childcare settings (Benjamin et al. 2009, e104-11; Cameron et al. 2012, 163-166). For example, Benjamin et al. (2009) analyzed childcare regulations related to infant feeding practices in all U.S. states and census regions and found that only 11 states (22%) had regulations specific to breastfeeding promotion or support and only 2 states (4%) had regulations specific to delaying complementary foods until six months (Benjamin et al. 2009, e104-11).
In longitudinal models examining associations between NMC use and any intake of obesity-related foods and beverages, our findings were mixed. The use of any NMC increased the odds of an infant or toddler consuming any whole fruit, but also increased the odds of them consuming any juice. Among the types of NMCs, a significant finding was that grandmother involvement in feeding increased the odds of juice consumption by 97%. Although controversial (Nicklas, O’Neil, and Kleinman 2008, 557-565), a few studies have documented positive associations between juice consumption and childhood overweight (Dennison, Rockwell, and Baker 1997, 15-22; Dennison et al. 1999, 346-352). Because excessive juice consumption can also be associated with undernutrition and short stature, as well as diarrhea, flatulence, abdominal distention, and tooth decay, the American Academy of Pediatrics (AAP) recommends juice not be given to infants less than 6 months of age and that it be limited to 4-6 fluid ounces per day among older infants and toddlers (Committee on Nutrition 2001, 1210-3). The average amount of fruit juice consumed by 18-month-olds in our sample (8 fluid ounces per day) was approximately twice this recommended level. Why grandmothers were associated with increased odds of infants and toddlers consuming juice is unclear. Several studies have found that grandmothers influence the timing of the introduction of complementary foods (Bentley et al. 1999a, 1085-100; Corbett 2000, 73-81; Bentley, Dee, and Jensen 2003, 305S-309S), but there is little research on their role in infant feeding thereafter. It is possible that grandmothers are unaware of the AAP recommendations as juice consumption was less of a concern during their time of childrearing, perhaps in part because so fewer forms were available (Dennison 1996, 4S-11S). However, given that use of a grandmother as the NMC was not associated with greater amounts of juice consumption—results discussed in more detail below—we cannot conclude that their impact on juice consumption is necessarily negative. Juice served in age-appropriate amounts can be a healthful beverage.
Why use of any NMC was associated with increased odds of whole fruit consumption among infants and toddlers is also unclear, particularly since there were no significant findings by type of NMC. A possibility is that the combined influence of grandmothers and licensed childcare providers is driving this finding, but that our sample size limited the ability to detect their separate effects. Among adults, fruit and vegetable consumption increases with age and is greatest among those 65 years of age and older—more adults ≥65 years consume two or more servings of fruit a day (41.3%) as compared to those 18-24 years (30.8%) (Centers for Disease Control 2010). It has also been shown that older adults (≥55 years) are more likely than younger adults (20-39 years) to rate nutrition as very important when shopping for food (OR=1.97, 95% CI: 1.70-2.28) (Bowman 2005, 281). The use of a licensed childcare provider might increase the likelihood of fruit consumption as all childcare facilities in North Carolina are mandated to follow the meal pattern guidelines of the Child and Adult Care Food Program (CACFP) (North Carolina Division of Child Development 2010, 43), a federally funded and state-administered nutrition assistance program. These meal patterns require fruit to be served at breakfast and lunch, beginning during late infancy.
In models examining amount of dietary intake, we found no significant associations with NMC involvement. It is important to note that the NDSR data collection method did not differentiate the types and amounts of foods and beverages fed by different types of caregivers. Therefore findings represent broad associations between non-maternal involvement in feeding and dietary intakes rather than direct comparisons of the types of foods and beverages fed by mothers versus NMCs. We believe this limitation has stronger implications for models examining amount of consumption versus any consumption, as there is likely to be more error in maternal second-hand reports of the former versus the latter. It is also possible that this set of analyses was limited by the sample size and less power to detect small differences in amounts of actual consumption versus probabilities of any consumption.
Thus, our data suggests that NMC involvement in feeding has limited impact on the intake of obesity-related foods and beverages during the period of complementary feeding, particularly for intake of high energy-dense foods such as fried potatoes, desserts and sweets, and salty snacks. However, the inclusion of NMCs in nutrition education is still imperative as we have documented they are highly involved in the feeding of infants and toddlers. Indeed, our analyses only suggest that NMCs may be no worse than mothers in exposing very young children to potentially obesogenic foods and beverages, but that overall intake patterns in this sample is concerning. Similar to findings from FITS (Siega-Riz et al. 2010, S38-51), exposure to obesity-related foods and beverages in the Infant Care sample began as early as six months and continued through 18 months. Given the substantial involvement of NMCs, interventions aimed at establishing healthy eating habits early in life are likely to be more effective when multiple caregivers are engaged rather than only the mother or other primary caregiver (American Dietetic Association 2006, 925; Birch and Ventura 2009, S74-81).
Additional important findings of this research are the associations between maternal and household characteristics and intakes of obesity-related foods and beverages. Higher maternal age and any maternal college were protective against intakes of obesity-related foods and beverages—the same factors associated with higher consumption of fruits and vegetables and lower consumption of sweetened beverages, desserts and candy, and salty snacks among the FITS sample (Hendricks et al. 2006b, S135-48). Our finding that maternal depressive symptoms are associated with higher intakes of potentially obesogenic foods before two years of age adds to the growing body of evidence showing maternal depression to be a risk factor for suboptimal infant and toddler feeding practices (Dennis and McQueen 2007, 590-594; Hurley et al. 2008, 799-805; McLearn et al. 2006, 279-284; Paulson, Dauber, and Leiferman 2006, 659-668). The negative impact of postpartum depression on breastfeeding outcomes has been well studied (Field 2010, 1-6) and our data shows that maternal depression negatively impacts the quality of the complementary diet as well. In light of depression’s adverse impacts on general parenting and quality of early interactions, some have called for universal screening of maternal and paternal depression by pediatricians (Field 2010, 1-6).
The current study had several important strengths, including a longitudinal design and analysis of a wide variety of dietary variables, but it also had several limitations in addition to those already mentioned. The sample consisted of infants and toddlers of low-income, first-time African-American mothers, and the results should only be generalized to this subset of the population. Additionally, the measure of NMC involvement was dichotomous, defined as those responsible for feeding an infant or toddler 50% or more of the time. Future research might benefit from a more continuous measure of non-maternal involvement. Finally, loss to follow-up is always a concern with longitudinal studies. However, examination of participant attrition in our sample revealed few significant differences in infant, maternal, or household characteristics between the baseline (three-month) sample and the sample at each subsequent study visit.
Conclusions
The current study documents a high prevalence of non-maternal involvement in feeding among infants and toddlers of low-income, first-time African-American mothers. The types of NMCs sharing responsibility for feeding were most frequently fathers, grandmothers, and licensed child care providers. We also document that NMC involvement is associated with lower likelihood of continued breastfeeding and higher likelihood of children consuming juice or whole fruit. Given the high prevalence of non-maternal involvement in feeding, interventions targeting multiple family members are warranted as they are likely to be more effective than those targeting the mother alone.
Highlights.
Non-maternal caregivers (NMCs) are highly involved in feeding infants and toddlers.
Common NMCs were fathers, grandmothers, and licensed childcare providers.
NMC involvement is associated with infant and young child feeding practices.
Acknowledgments
Funding: This research was supported by Grant R01 HD42219-02, Grant DK56350, and Grant T32 HD057824-03 from the National Institutes of Health/NICHD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Pediatrics Committee on Nutrition. Complementary Feeding. In: Kleinman RE, editor. Pediatric Nutrition Handbook. Elk Grove, IL: American Academy of Pediatrics; 2009. pp. 113–29. [Google Scholar]
- American Dietetic Association. Position of the American Dietetic Association: individual-, family-, school-, and community-based interventions for pediatric overweight. 2006;106(6):925. doi: 10.1016/j.jada.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Anderson PM, Butcher KE. Childhood obesity: trends and potential causes. The Future of children / Center for the Future of Children, the David and Lucile Packard Foundation. 2006;16(1):19–45. doi: 10.1353/foc.2006.0001. [DOI] [PubMed] [Google Scholar]
- Arenz S, Ruckerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity--a systematic review. Int J Obes Relat Metab Disord. 2004;28(10):1247–56. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- Benjamin SE, Taveras EM, Cradock AL, Walker EM, Slining MM, Gillman MW. State and regional variation in regulations related to feeding infants in child care. Pediatrics. 2009;124(1):e104–11. doi: 10.1542/peds.2008-3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley M, Gavin L, Black MM, Teti L. Infant feeding practices of low-income, African-American, adolescent mothers: an ecological, multigenerational perspective. Soc Sci Med. 1999;49(8):1085–100. doi: 10.1016/s0277-9536(99)00198-7. [DOI] [PubMed] [Google Scholar]
- Bentley ME, et al. Sources of influence on intention to breastfeed among African-American women at entry to WIC. J Hum Lact. 1999;15(1):27–34. doi: 10.1177/089033449901500109. [DOI] [PubMed] [Google Scholar]
- Bentley ME, Dee DL, Jensen JL. Breastfeeding among low income, African-American women: power, beliefs and decision making. The Journal of nutrition. 2003;133(1):305S–309S. doi: 10.1093/jn/133.1.305S. [DOI] [PubMed] [Google Scholar]
- Bianchi SM, Casper LM. American Families. 2000;55(4) [Google Scholar]
- Birch LL, Ventura AK. Preventing childhood obesity: what works? International journal of obesity. 2009;33(Suppl 1):S74–81. doi: 10.1038/ijo.2009.22. [DOI] [PubMed] [Google Scholar]
- Bowman SA. Food shoppers’ nutrition attitudes and relationship to dietary and lifestyle practices. Nutrition Research. 2005;25(3):281. [Google Scholar]
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane database of systematic reviews (Online) 2007;(1) doi: 10.1002/14651858.CD001141.pub3. CD001141. [DOI] [PubMed] [Google Scholar]
- Bronner YL, et al. Early introduction of solid foods among urban African-American participants in WIC. J Am Diet Assoc. 1999;99(4):457–61. doi: 10.1016/S0002-8223(99)00112-1. [DOI] [PubMed] [Google Scholar]
- Cameron B, Javanparast S, Labbok M, Scheckter R, McIntyre E. Breastfeeding support in child care: an international comparison of findings from Australia and the United States. Breastfeeding Medicine. 2012;7(3):163–166. doi: 10.1089/bfm.2011.0032. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. State-specific trends in fruit and vegetable consumption among adults-United States, 2000-2009. MMWR. 2010;59(35) [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Breastfeeding trends and updated national health objectives for exclusive breastfeeding--United States, birth years 2000-2004. MMWR. 2007;56(30):760–3. [PubMed] [Google Scholar]
- Ciampa PJ, et al. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Archives of Pediatrics & Adolescent Medicine. 2010;164(12):1098–1104. doi: 10.1001/archpediatrics.2010.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Nutrition. American Academy of Pediatrics: The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107(5):1210–3. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- Corbett KS. Explaining infant feeding style of low-income black women. J Pediatr Nurs. 2000;15(2):73–81. doi: 10.1053/jn.2000.5445. [DOI] [PubMed] [Google Scholar]
- Cox DR, Skinner JD, Carruth BR, Moran J, 3rd, Houck KS. A Food Variety Index for Toddlers (VIT): development and application. Journal of the American Dietetic Association. 1997;97(12):1382–6. doi: 10.1016/s0002-8223(97)00334-9. quiz 1387-8. [DOI] [PubMed] [Google Scholar]
- Dattilo AM, Birch L, Krebs NF, Lake A, Taveras EM, Saavedra JM. Need for early interventions in the prevention of pediatric overweight: a review and upcoming directions. Journal of obesity. 2012;2012:123023. doi: 10.1155/2012/123023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatrica (Oslo, Norway : 1992) 2007;96(4):590–594. doi: 10.1111/j.1651-2227.2007.00184.x. [DOI] [PubMed] [Google Scholar]
- Dennison BA. Fruit juice consumption by infants and children: a review. Journal of the American College of Nutrition. 1996;15(5 Suppl):4S–11S. doi: 10.1080/07315724.1996.10720475. [DOI] [PubMed] [Google Scholar]
- Dennison BA, Rockwell HL, Baker SL. Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity. Pediatrics. 1997;99(1):15–22. [PubMed] [Google Scholar]
- Dennison BA, Rockwell HL, Nichols MJ, Jenkins P. Children’s growth parameters vary by type of fruit juice consumed. Journal of the American College of Nutrition. 1999;18(4):346–352. doi: 10.1080/07315724.1999.10718874. [DOI] [PubMed] [Google Scholar]
- DiGirolamo A, Thompson N, Martorell R, Fein S, Grummer-Strawn L. Intention or experience? Predictors of continued breastfeeding. Health Education & Behavior. 2005;32(2):208–226. doi: 10.1177/1090198104271971. [DOI] [PubMed] [Google Scholar]
- Ehrle J, Adams G, Tout K. Who’s caring for our youngest children?: Child care patterns of infants and toddlers. 2001;(42) [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant behavior & development. 2010;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn MA, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ’best practice’ recommendations. Obesity reviews. 2006;7(Suppl 1):7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- Fox MK, Pac S, Devaney B, Jankowski L. Feeding infants and toddlers study: What foods are infants and toddlers eating? J Am Diet Assoc. 2004;104(1 Suppl 1):s22–30. doi: 10.1016/j.jada.2003.10.026. [DOI] [PubMed] [Google Scholar]
- Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008;122(Suppl 2):S36–42. doi: 10.1542/peds.2008-1315d. [DOI] [PubMed] [Google Scholar]
- Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. American Journal of Epidemiology. 2005;162(5):397–403. doi: 10.1093/aje/kwi222. [DOI] [PubMed] [Google Scholar]
- Hendricks K, Briefel R, Novak T, Ziegler P. Maternal and child characteristics associated with infant and toddler feeding practices. J Am Diet Assoc. 2006;106(1 Suppl 1):S135–48. doi: 10.1016/j.jada.2005.09.035. [DOI] [PubMed] [Google Scholar]
- Hoerr SL, Horodynski MA, Lee SY, Henry M. Predictors of nutritional adequacy in mother-toddler dyads from rural families with limited incomes. Journal of the American Dietetic Association. 2006;106(11):1766–1773. doi: 10.1016/j.jada.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Horta BL, Bahl R, Martines JC, Victora CG. Evidence on the long-term effects of breastfeeding: systematic reviews adn meta-analyses 2007 [Google Scholar]
- Hurley KM, Black MM, Papas MA, Caulfield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. The Journal of nutrition. 2008;138(4):799–805. doi: 10.1093/jn/138.4.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Anonymous Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) Washington, DC: The National Academies Press; 2005. Energy. [Google Scholar]
- Kim J, Peterson KE. Association of infant child care with infant feeding practices and weight gain among US infants. Arch Pediatr Adolesc Med. 2008;162(7):627–33. doi: 10.1001/archpedi.162.7.627. [DOI] [PubMed] [Google Scholar]
- Laughlin L. Who’s minding the kids? Child care arrangements: Spring 2005/Summer 2006. Current Population Reports. 2010 Aug [Google Scholar]
- Li R, Darling N, Maurice E, Barker L, Grummer-Strawn LM. Breastfeeding rates in the United States by characteristics of the child, mother, or family: the 2002 National Immunization Survey. Pediatrics. 2005;115(1):e31–7. doi: 10.1542/peds.2004-0481. [DOI] [PubMed] [Google Scholar]
- McLearn KT, Minkovitz CS, Strobino DM, Marks E, Hou W. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Archives of Pediatrics & Adolescent Medicine. 2006;160(3):279–284. doi: 10.1001/archpedi.160.3.279. [DOI] [PubMed] [Google Scholar]
- Meedya S, Fahy K, Kable A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women and birth : journal of the Australian College of Midwives. 2010;23(4):135–145. doi: 10.1016/j.wombi.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Moorcroft KE, Marshall JL, McCormick FM. Association between timing of introducing solid foods and obesity in infancy and childhood: a systematic review. Maternal & child nutrition. 2011;7(1):3–26. doi: 10.1111/j.1740-8709.2010.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulligan GM, Brimhall DA, West J, Chapman C. Child care and early education arrangements of infants, toddlers, and preschoolers: 2001. 2005 Nov [Google Scholar]
- Nicklas TA, O’Neil CE, Kleinman R. Association between 100% juice consumption and nutrient intake and weight of children aged 2 to 11 years. Archives of Pediatrics & Adolescent Medicine. 2008;162(6):557–565. doi: 10.1001/archpedi.162.6.557. [DOI] [PubMed] [Google Scholar]
- North Carolina Division of Child Development. Nutrition Standards. Chapter 9: Child Care Rules. 2010:43. [Google Scholar]
- Ogden CL, Carroll MD. Prevalence of obesity among children and adolescents: United States, trends 1963-1965 through 2007-2008. NCHS Health E-Stats. 2010 Jun [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA : the journal of the American Medical Association. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- Pearce A, et al. Childcare use and inequalities in breastfeeding: findings from the UK Millennium Cohort Study. Archives of Disease in Childhood. 2012;97(1):39–42. doi: 10.1136/adc.2009.177337. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385. [Google Scholar]
- Scaglioni S, Arrizza C, Vecchi F, Tedeschi S. Determinants of children’s eating behavior. The American Journal of Clinical Nutrition. 2011;94(6 Suppl):2006S–2011S. doi: 10.3945/ajcn.110.001685. [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Deming DM, Reidy KC, Fox MK, Condon E, Briefel RR. Food consumption patterns of infants and toddlers: where are we now? Journal of the American Dietetic Association. 2010;110(12 Suppl):S38–51. doi: 10.1016/j.jada.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Skinner JD, Ziegler P, Pac S, Devaney B. Meal and snack patterns of infants and toddlers. Journal of the American Dietetic Association. 2004;104(1 Suppl 1):s65–70. doi: 10.1016/j.jada.2003.10.021. [DOI] [PubMed] [Google Scholar]
- Skinner JD, Ziegler P, Ponza M. Transitions in infants’ and toddlers’ beverage patterns. J Am Diet Assoc. 2004;104(1 Suppl 1):s45–50. doi: 10.1016/j.jada.2003.10.027. [DOI] [PubMed] [Google Scholar]
- Slining M, Adair LS, Goldman BD, Borja JB, Bentley M. Infant overweight is associated with delayed motor development. The Journal of pediatrics. 2010;157(1):20–25.e1. doi: 10.1016/j.jpeds.2009.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slining MM, Adair L, Goldman BD, Borja J, Bentley M. Infant temperament contributes to early infant growth: A prospective cohort of African American infants. The international journal of behavioral nutrition and physical activity. 2009;6:51. doi: 10.1186/1479-5868-6-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn BA, Caterson I, Seidell JC, James WP. Diet, nutrition and the prevention of excess weight gain and obesity. Public health nutrition. 2004;7(1A):123–146. doi: 10.1079/phn2003585. [DOI] [PubMed] [Google Scholar]
- Thompson AL, Mendez MA, Borja JB, Adair LS, Zimmer CR, Bentley ME. Development and validation of the Infant Feeding Style Questionnaire. Appetite. 2009;53(2):210–221. doi: 10.1016/j.appet.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson FE, Subar AF. Dietary Assessment Methodology. In: Coulston AM, Boushey CJ, editors. Nutrition in the Prevention and Treatment of Disease. San Diego, CA: Elsevier Academic Press; 2008. pp. 3–40.pp. 1 [Google Scholar]
- Wasser H, et al. Infants perceived as “fussy” are more likely to receive complementary foods before 4 months. Pediatrics. 2011;127(2):229–237. doi: 10.1542/peds.2010-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global Strategy for Infant and Young Child Feeding 2003 [Google Scholar]


