Abstract
Background and study aims
There are no definite guidelines regarding colonoscopic evaluation for the indication of constipation, a common gastrointestinal complaint. The aim of our study was to determine the risk of finding significant lesions in patients undergoing colonoscopy for the indication of constipation alone compared with constipation with another indication or average-risk screening.
Patients and methods
A retrospective review of the Clinical Outcomes Research Initiative database was carried out for colonoscopies undertaken between 1 January 2000 and 30 June 2003. A total of 41,775 index colonoscopies performed for the indications of average-risk screening, constipation only or constipation with another indication were identified. Logistic regression analyses were performed for constipation alone versus constipation with another indication, and for constipation alone versus average-risk screening.
Results
Constipation alone did not show any increased risk of significant findings on colonoscopy. Constipation and the presence of another indication, however, had a statistically significant increased risk of a significant finding on colonoscopy. The indication of constipation alone had a lower risk of significant findings on colonoscopy compared with average-risk screening. Variations in the definition of constipation used was a limitation of the study.
Conclusions
Colonoscopy for constipation alone has a lower yield for significant findings compared with average-risk screening and constipation with another indication; hence, colonoscopy should not be done for constipation alone.
Introduction
Constipation is one of the most common gastrointestinal complaints, resulting in approximately 2.5 million physician visits per year in the United States [1]. The prevalence of constipation has been reported to vary between 2% and 27% in North America, which has been attributed primarily to a wide variation in the constipation criteria used rather than socioeconomic or other factors [2–4]. The American Gastroenterological Association (AGA) recommends colonoscopy for patients with constipation when they are older than 50 years and have had no prior screening [5]. The American Society for Gastrointestinal Endoscopy (ASGE), however, does not endorse colonoscopy for the indication of constipation [6]. Literature review does not reveal a consensus regarding the role of colonoscopy for constipation [7–11]. The aim of our study was to determine the prevalence of colonoscopically defined malignant and premalignant lesions based on a large database of a broad-base population, with the hypothesis that constipation alone is not associated with an increased finding rate compared with average-risk screening.
Patients and methods
The Clinical Outcomes Research Initiative
The Clinical Outcomes Research Initiative (CORI) database is a national endoscopic database developed to perform outcomes research in gastrointestinal endoscopy. It includes 70 practice sites in 24 states with approximately 400 participating endoscopists. In order to protect patient confidentiality, all patient and physician identifiers are removed from the data file before transmission from the local site. Site compliance is assessed annually to ensure inclusion of at least 95% of endoscopic reports for participating endoscopists. The practice sites include private practices, universities, and Veterans’s Administration hospitals.
Patients
The CORI database was reviewed for colonoscopies that were performed based on procedure indication between 1 January 2000 and 30 June 2003. During the study period, 305,027 colonoscopies were carried out, of which 287,112 were index colonoscopies. Index colonoscopy was defined as the first colonoscopy per patient recorded in the CORI database since 1 January 1998. A total of 41,775 index colonoscopies fulfilled the indication requirement of constipation alone, constipation with another symptom or average-risk screening colonoscopy. We excluded patients < 20 years old from the analysis.
Criteria used
The following procedure indications were used to select colonoscopies from the CORI database: 1) constipation only, 2) constipation plus another indication, which included anemia, hematochezia, positive fecal occult blood test (FOBT), weight loss, change in bowel habits or abdominal pain/bloating, and 3) average-risk screening. A significant finding on colonoscopy was defined as a suspected malignant tumor or polyp > 9 mm. It is important to emphasize that the results of histopathology are not incorporated routinely into the CORI database and, therefore, these findings represent suspicion of disease at the end of the endoscopy procedure. However, earlier studies have shown the significance of size association with malignant potential [12]. The definition of constipation was dependent on the endoscopist who entered the data.
Statistical analysis
SAS software v.8 (SAS Institute, Cary, North Carolina, USA) was used to perform statistical analysis. Logistic regression analyses were carried out to: a) examine constipation only versus average-risk screening, and b) examine constipation alone versus constipation with another indication, which included hematochezia, positive FOBT, anemia or weight loss. The odds ratio (OR) of each outcome was separately calculated with the 95% confidence interval (CI). Odds ratios were also calculated for demographic factors. All indicators were categorized as dichotomous variables, and the significance of all variables in the models was assessed using a likelihood-ratio test statistic obtained from a logistic regression model. The multivariate logistic regression model was utilized to generate the estimated probability of the outcome occurring given specified levels of the variables in the model.
Results
Demographic and clinical information
The demographic and clinical characteristics of the study population are shown in Table 1. A total of 41,775 index colonoscopies fulfilled the study criteria. Average-risk screening was the most common indication for colonoscopy (78.5 %) followed by constipation with another indication (13.7 %) and constipation alone (7.8 %). Mean age at the time of colonoscopy for the indication of constipation alone and average-risk screening was 61.6 years and 63.0 years, respectively. The white non-Hispanic population was the largest race/ethnicity across all indication groups (87 %). There was almost equal representation of males (49 %) and females (51 %). In all, 72% of the patients underwent colonoscopy in a community setting, whereas 20% attended academic settings, and 8% Veteran’s Administration hospitals. The number of significant lesions (> 9mm polyp or suspected malignant tumor) found on colonoscopy in each indication is also shown in Table 1.
Table 1.
Demographic data and Clinical information
| Demographics |
Indication
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Constipation + |
Screening N = 32808 |
||||||||
| Alone N = 3264 |
Anemia N = 375 |
Bleed N = 2323 |
FOBT N = 694 |
Weight loss N = 376 |
Bowel habit change N = 904 |
Abdominal Pain N = 2330 |
|||
|
| |||||||||
| Age | Mean (SD) |
61.6 (14.1) |
65.2 (15.3) |
56.8 (14.4) |
61.7 (15.8) |
67.1 (15.3) |
61.9 (13.9) |
58.0 (15.6) |
63.0 (9.2) |
| <50 | 609(19) | 75 (20) | 715 (31) | 166 (24) | 58(15) | 170 (19) | 736 (32) | 773 (2) | |
| 50-59 | 900 (28) | 65 (17) | 692 (30) | 148 (21) | 57(15) | 237 (26) | 543(23) | 13124(40) | |
| 60-69 | 736(23) | 70 (19) | 441(19) | 140 (21) | 60 (16) | 212(23) | 445 (19) | 10712 (33) | |
| ≥ 70 | 1019 (31) | 165 (44) | 475 (21) | 240 (35) | 201 (53) | 285 (32) | 606 (26) | 8199(25) | |
| Gender |
|
||||||||
| Female | 2131 (65) | 228 (61) | 1524(66) | 428 (62) | 199(53) | 595 (66) | 1739 (75) | 15154(46) | |
| Male | 1133(35) | 147 (39) | 799 (34) | 266 (38) | 177(47) | 309 (34) | 591 (25) | 17654(54) | |
|
|
|||||||||
| Ethnicity | |||||||||
| White¶ | 2608 (80) | 243 (65) | 1793 (77) | 464 (67) | 287 (76) | 791(88) | 1795(77) | 28418 (87) | |
| Black¶ | 345 (11) | 75 (20) | 202 (9) | 102(15) | 48 (13) | 61 (7) | 213 (9) | 2232 (7) | |
| Hispanic | 264 (8) | 50(13) | 282(12) | 104 (15) | 33 (9) | 38 (4) | 284(12) | 1708 (5) | |
| Othera¶ | 47 (1) | 7 (2) | 46 (2) | 24 (4) | 8 (2) | 14 (2) | 38 (2) | 450(1) | |
| Clinical Setting |
|||||||||
|
|
|||||||||
| Community | 2352 (72) | 254 (68) | 1830(79) | 543 (78) | 255 (68) | 819 (91) | 1910 (82) | 24827 (76) | |
| Academic | 638 (20) | 50 (13) | 337 (15) | 70 (10) | 58(15) | 68 (8) | 335(14) | 6228(19) | |
| VAb | 274 (8) | 71 (19) | 156 (7) | 81 (12) | 63 (17) | 17 (2) | 85 (4) | 1753 (5) | |
Other; Asian and pacific islander
VA, Veteran’s administration
Non-hispanic
Significant findings on colonoscopy for constipation only and average-risk screening Findings from the constipation only group and the average-risk screening group were compared using logistic regression analysis (shown as a Forrest plot in Fig. 1). The analysis was adjusted for age, sex, ethnicity, and clinical setting. The constipation only group had a 20% lower risk of a significant finding compared with average-risk screening (OR for constipation 0.79, 95%CI 0.65–0.96). Hispanic (OR 1.66) and other non-Hispanic (OR 2.16) groups had a statistically significant increased risk of a significant finding compared with the reference white non-Hispanic population in this comparison. Males were more likely to have a significant finding compared with females (OR 1.59). Overall, increasing age did not show an increased risk of a positive finding; only the age group 50–59 years showed a significant elevated risk, with an odds ratio of 1.28.
Figure 1.
Odds ratio (OR) for significant finding on colonoscopy for constipation only versus average-risk screening. Forrest plot depicting logistic regression analysis. CI, confidence interval; 1VA, Veteran’s Administration. *Other, Asian/Pacific Islander.
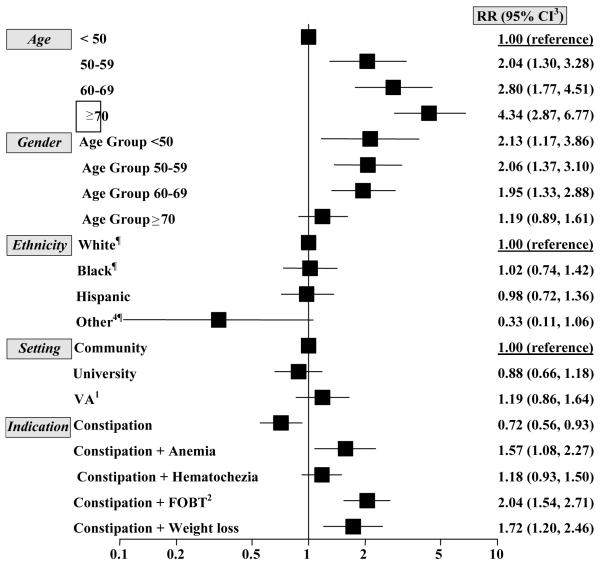
Significant findings on colonoscopy for constipation with and without another indication Fig. 2 shows odds ratios for significant findings on colonoscopy based on covariates that include age, sex, ethnicity, and clinical setting. Constipation groups included constipation only, and constipation with another indication (hematochezia, anemia, positive FOBT or weight loss). Groups that included constipation with another indication were not mutually exclusive. For odds ratio assessment of constipation with another indication, all indication groups (except for constipation only) that did not fit that particular category served as the reference group.
Figure 2.
Adjusted relative risk (ARR) of significant Endoscopic finding based on demographic factors among different constipation groups (constipation alone or constipation along with anemia, hematochezia, positive FOBT or weight loss). Gender group is further divided based on age groups. Indication of endoscopy included constipation alone or constipation along with another indication. Except for constipation only, the remaining groups are not mutually exclusive. The logistic regression model was adjusted for age, gender, race/ethnicity and setting (Community, University or VA). 1VA, Veteran’s administration; 2FOBT, Positive fecal occult blood test; 3CI, Confidence interval; ¶Non-Hispanic; 4Other, Asian/Pacific Islander.
An increased risk of significant findings with increasing age was observed. Patients in the age group ≥ 70 years were four times more likely to have a significant finding than patients < 50 years. No significantly increased risk associated with ethnic background was found when using the white non-Hispanic population as the reference group (Black non-Hispanic OR 1.02, Hispanic OR 0.98; and Asian/Pacific Islander non-Hispanic population OR 0.33). Male or female sex was evaluated with regard to age group and showed a decreasing risk difference between males and females with increasing age. Constipation alone did not show any increased risk (OR 0.72), whereas constipation with another indication was associated with statistically increased risk of significant findings on colonoscopy, with the exception of constipation with hematochezia, which showed a nonsignificant trend towards increased findings.
Discussion
There is no conclusive consensus in the literature regarding the association between constipation and colon cancer [8–11, 13, 14]. In the Nurses Health Study, Dukas et al. concluded that there was no increased risk of colorectal cancer in individuals with constipation [8]. Similar results were shown by Pepin and Ladabaum in a study of 563 constipated patients [9]. By contrast, in the Miyagi cohort study, results suggested an association between constipation and laxative use and the risk of colon cancer [11]. Similarly, a meta-analysis by Sonnenberg and Muller showed a risk for colorectal cancer with constipation (pooled OR 1.48; 95%CI 1.32–1.66) [7].
By utilizing a large standardized endoscopy database, our study aimed to determine whether or not there is an increased rate of finding premalignant and malignant lesions on colonoscopy performed solely for the indication of constipation. The strengths of this study include the large number of patients derived from different settings (both academic and non-academic centers). In comparison to previous studies, our investigation compared the finding rate in the presence of constipation with an average-risk screening group. Thus, we were able to directly and more accurately compare any effect of constipation that may influence the finding rate over and above average-risk screening.
We compared constipation alone with average-risk screening controls. Patients with constipation alone had a lower finding rate than individuals undergoing colonoscopy for average-risk screening (OR 0.79). Our results also show that the symptom of constipation alone does not confer increased risk of significant findings on colonoscopy (OR 0.72), in fact a decreased risk was found. A statistically significant higher rate of findings was observed in patients with constipation with another indication such as anemia, weight loss, bleeding or positive FOBT (Fig. 2). Every risk factor needs sufficient time to play a role in the development of malignancy. In our study, although constipation alone does not seem to be related to an increase in endoscopic findings, it is still conceivable that the duration of constipation or other associated factors such as laxative use may be a contributing factor to the development of malignancy [7, 11].
There are several limitations to our study. First, there is no definition for constipation within the CORI database, as data input is physician-dependent. However, previous studies have all used variable definitions of constipation [8, 11]. Moreover, although our 41,775 colonoscopies represented index cases within CORI since 1998, we cannot be certain that a patient had not undergone prior lower endoscopy and for what indication. Histopathology is not routinely available within CORI, which means that the definition of a significant finding (polyp > 9mm and suspected malignant tumor) is based on subjective appearance and size rather than objective confirmation. However, polyp size is reliably predictive of malignant potential [12, 15]. Finally, there may be under-reporting of constipation as a symptom, which will limit the numbers in our comparison.
In conclusion, our results show that there is no association between constipation alone and an increased risk of significant endoscopic findings when compared with average-risk screening, and hence, constipation on its own should not be used as an indication for colonoscopy. There was increased risk of findings in cases with constipation with other indications. These patients should be considered for evaluation with colonoscopy. Patients older than 50 years with constipation should undergo average-risk colonoscopy screening.
Footnotes
Competing interests: Dr Eisen is the Executive Co-Director of the Clinical Outcomes Research Initiative (CORI), a non-profit organization that receives funding from federal and industry sources. The CORI database is used in this study. This potential conflict of interest has been reviewed and managed by the OHSU Conflict of Interest in Research Committee.
References
- 1.Sonnenberg A, Koch TR. Epidemiology of constipation in the United States. Dis Colon Rectum. 1989;32:1–8. doi: 10.1007/BF02554713. [DOI] [PubMed] [Google Scholar]
- 2.American College of Gastroenterology Chronic Constipation Task Force An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100(Suppl 1):S1–4. doi: 10.1111/j.1572-0241.2005.50613_1.x. [DOI] [PubMed] [Google Scholar]
- 3.Stewart WF, Liberman JN, Sandler RS, et al. Epidemiology of constipation (EPOC) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol. 1999;94:3530–3540. doi: 10.1111/j.1572-0241.1999.01642.x. [DOI] [PubMed] [Google Scholar]
- 4.Pare P, Ferrazzi S, Thompson WG, et al. An epidemiological survey of constipation in canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol. 2001;96:3130–3137. doi: 10.1111/j.1572-0241.2001.05259.x. [DOI] [PubMed] [Google Scholar]
- 5.Locke GR, 3rd, Pemberton JH, Phillips SF. American Gastroenterological Association Medical Position Statement: guidelines on constipation. Gastroenterology. 2000;119:1761–1766. doi: 10.1053/gast.2000.20390. [DOI] [PubMed] [Google Scholar]
- 6.Qureshi W, Adler DG, Davila RE, et al. ASGE guideline: guideline on the use of endoscopy in the management of constipation. Gastrointest Endosc. 2005;62:199–201. doi: 10.1016/j.gie.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Sonnenberg A, Muller AD. Constipation and cathartics as risk factors of colorectal cancer: a meta-analysis. Pharmacology. 1993;47(Suppl 1):224–233. doi: 10.1159/000139862. [DOI] [PubMed] [Google Scholar]
- 8.Dukas L, Willett WC, Colditz GA, et al. Prospective study of bowel movement, laxative use, and risk of colorectal cancer among women. Am J Epidemiol. 2000;151:958–964. doi: 10.1093/oxfordjournals.aje.a010139. [DOI] [PubMed] [Google Scholar]
- 9.Pepin C, Ladabaum U. The yield of lower endoscopy in patients with constipation: survey of a university hospital, a public county hospital, and a Veterans Administration medical center. Gastrointest Endosc. 2002;56:325–332. doi: 10.1016/s0016-5107(02)70033-3. [DOI] [PubMed] [Google Scholar]
- 10.Roberts MC, Millikan RC, Galanko JA, et al. Constipation, laxative use, and colon cancer in a North Carolina population. Am J Gastroenterol. 2003;98:857–864. doi: 10.1111/j.1572-0241.2003.07386.x. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe T, Nakaya N, Kurashima K, et al. Constipation, laxative use and risk of colorectal cancer: The Miyagi Cohort Study. Eur J Cancer. 2004;40:2109–2115. doi: 10.1016/j.ejca.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. New Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 13.Kune GA, Kune S, Field B, Watson LF. The role of chronic constipation, diarrhea, and laxative use in the etiology of large-bowel cancer. Data from the Melbourne Colorectal Cancer Study. Dis Colon Rectum. 1988;31:507–512. doi: 10.1007/BF02553722. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs EJ, White E. Constipation, laxative use, and colon cancer among middle-aged adults. Epidemiology. 1998;9:385–391. [PubMed] [Google Scholar]
- 15.Harewood GC, Lieberman DA. Prevalence of advanced neoplasia at screening colonoscopy in men in private practice versus academic and Veterans Affairs medical centers. Am J Gastroenterol. 2003;98:2312–2316. doi: 10.1111/j.1572-0241.2003.07677.x. [DOI] [PubMed] [Google Scholar]