Abstract
Objective
To assess the impact of the American Urological Association guidelines advocating partial nephrectomy for T1 tumors guidelines on the likelihood of undergoing partial nephrectomy.
Materials and Methods
We analyzed the Nationwide Inpatient Sample, a dataset encompassing 20% of all United States inpatient hospitalizations, from 2007 through 2010. Our dependent variable was receipt of radical vs. partial nephrectomy (55.50, 55.51, 55.52, and 55.54 vs. 55.4) for a renal mass (ICD-9 code 189.0). The independent variable of interest was time of surgery (before or after the establishment of AUA guidelines); covariates included a diagnosis of chronic kidney disease (CKD), overall comorbidity, age, race, gender, geographic region, income, and hospital characteristics. Bivariate and multivariable adjusted logistic regression was used to determine the association between receipt of partial nephrectomy and time of guideline establishment.
Results
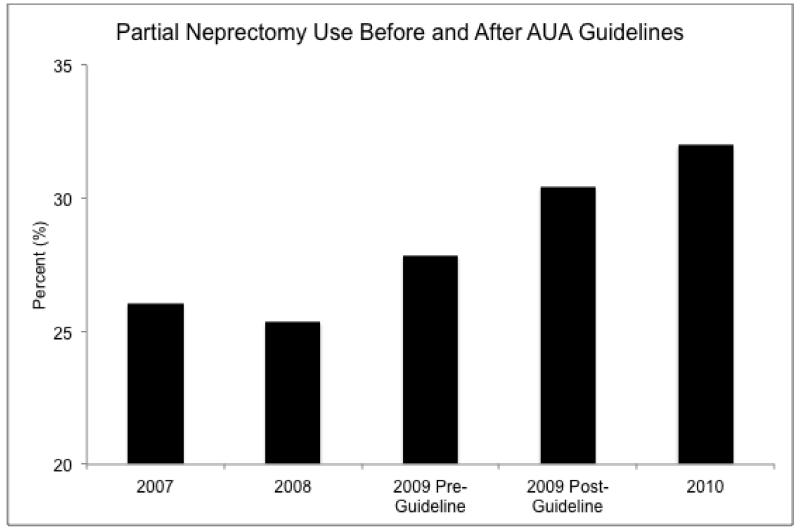
We identified 26,165 patients with renal tumors who underwent surgery. Prior to the guidelines, 4031 (27%) patients underwent partial nephrectomy compared to 3559 (32%) after. On multivariable analysis, undergoing surgery after the establishment of guidelines (OR 1.20 [95% Cl 1.08-1.32], p<0.01) was an independent predictor of partial nephrectomy. Other factors associated with partial nephrectomy were urban location, surgery at a teaching hospital, large hospital bed size, Northeast location, and Black race. Female gender and CKD were not associated with partial nephrectomy.
Conclusions
Although adoption of partial nephrectomy increased after establishment of new guidelines on renal masses, partial nephrectomy remains an underutilized procedure. Future research must focus on barriers to adoption of partial nephrectomy and how to overcome them.
Keywords: American Urological Association guideline, renal mass, partial nephrectomy
Since the seminal report of Miller and cols stressing the underuse of PN in US [1], the subject has become of outmost interest in the urological community. The practice of PN has been associated to multiple factors among others type of hospital, gender and race, income, insurance status, regional distribution and surgeon’s preferences and volume [2, 3].
Bjurlin and cols assess in the present issue, the influence of the AUA guidelines for the Management of Renal Masses on the national trend in utilization of PN. As others [4,5] they utilize the National Inpatient Sample database although theirs includes a more recent time frame, from 2007 to 2010. The selection of this narrow interval around the publication of the AUA guideline (April 2009) aims to minimize the effect of the rise of PN rates. Their results, as all the previous ones, support a steady and consistent increasing use of PN. Specifically, PN rate increased from 27% before AUA guideline publication to 32% afterwards, suggesting that this guideline might have had a positive effect in the use of PN.
Their data shows indeed an association between the increasing use of PN and the AUA guideline and a statistically significant increase in the likelihood of PN after AUA guideline publication. However association does not necessarily mean causality. In fact their study can neither rule-out the influence of other factors in the increasing use of PN nor exclude the logical implementation of a surgical technique. Furthermore, although statistically significant, the magnitude of the difference before and after AUA guideline publication is small and a net increment of 5% through 4 years might be considered marginally clinically relevant and similar to the increments described previously to the publication of the AUA guideline [3-5].
These reflections do not discredit the value of the AUA guidelines for the Management of Renal Masses and the effort of Bjurlin and cols. On the contrary, this excellent document is more than adequate to improve process and structure of care and the present report opens a line of future investigation. It is likely that a longer period of time will be necessary to measure its effects on patients health outcomes otherwise scarcely studied [6]. Multiple barriers modulate the adherence to guidelines and there is a high level of variation in effects across recommendations [7].
Guidelines on the other hand are not documents ahead of their time. More frequent than not, both technical implementation and development of comprehensive guidelines are parallel phenomena. Consequently a strong association is not strange but causality not necessarily inferred. At the same time other factors as awareness of the deleterious effect of RN, implementation of surgical armamentarium, introduction of effective haemostatic agents, expansion of Robotic surgery and installment of dedicated Uro-oncology fellowships among others might have influenced the increase in the use of PN and represent important confounders not taken into account in their analysis.
Figure 1.
Table 1.
Bivariate analysis of radical and partial nephrectomy use among patients undergoing kidney surgery for kidney cancer
| Radical Nephrectomy (%) |
Partial Nephrectomy (%) |
p value | |
|---|---|---|---|
| CKD | |||
| No | 5806 (31) | 2544 (34) | |
| Yes | 12769 (69) | 5046 (66) | <0.01 |
| Guidelines | |||
| Pre | 11050 (59) | 4031 (53) | <0.01 |
| Post | 7527 (41) | 3559 (47) | |
| Year | <0.01 | ||
| 2007 | 4303 (23) | 1574 (21) | |
| 2008 | 5169 (28) | 1826 (24) | |
| 2009 | 4669 (25) | 2027 (27) | |
| 2010 | 4434 (24) | 2163 (28) | |
| Age | |||
| 18-44 | 2025 (11) | 1158 (15) | <0.01 |
| 45-64 | 6177 (33) | 2852 (38) | |
| 65-74 | 7297 (39) | 2917 (38) | |
| 75+ | 3061 (17) | 651 (9) | |
| Race | |||
| White | 11699 (78) | 4797 (77) | <0.01 |
| Black | 1282 (9) | 630 (10) | |
| Other | 2013 (13) | 806 (13) | |
| Gender | |||
| Female | 7166 (39) | 2919 (39) | 0.92 |
| Male | 11352 (61) | 4638 (61) | |
| Comorbidities | |||
| 0 | 4225 (23) | 1910 (25) | <0.01 |
| 1-2 | 11101 (60) | 4554 (60) | |
| 3+ | 3249 (17) | 1126 (15) | |
| Household Income | |||
| $63K+ | 4675 (26) | 2257 (31) | |
| $1-38,999 | 4274 (24) | 1575 (21) | <0.01 |
| $39K-47,999 | 4620 (25) | 1721 (23) | |
| $48K-62,999 | 4617 (25) | 1839 (25) | |
| Insurance | |||
| Public | 9061 (49) | 3033 (40) | <0.01 |
| Private | 8497 (46) | 4160 (55) | |
| Other | 978 (5) | 381 (5) | |
| Hospital location | |||
| Rural | 1292 (7) | 329 (4) | <0.01 |
| Urban | 17101 (93) | 7175 (96) | |
| Teaching status | |||
| Teaching | 11121 (60) | 5659 (75) | <0.01 |
| Non-teaching | 7272 (40) | 1845 (25) | |
| Bed Size | |||
| Small | 1827 (10) | 644 (9) | <0.01 |
| Medium | 3902 (21) | 1279 (17) | |
| Large | 12664 (69) | 5581 (74) | |
| Region | |||
| South | 6049 (33) | 2166 (29) | |
| Northeast | 3590 (19) | 2056 (27) | <0.01 |
| Midwest | 4687 (25) | 1909 (25) | |
| West | 4249 (23) | 1459 (19) |
Table 2.
Multivariable logistic regression to determine the association between time period of surgery and likelihood of partial nephrectomy among patients undergoing surgery for kidney cancer
| Odds Ratio (95% Cl) |
p value | |
|---|---|---|
| CKD | ||
| No | 1.00 | Ref |
| Yes | 0.95 (0.88-1.02) | 0.16 |
| Guidelines | ||
| Pre | 1.00 | Ref |
| Post | 1.20 (1.08-1.32) | <0.01 |
| Year | 1.04 (0.99-1.09) | 0.93 |
| Age | ||
| 18-44 | 1.00 | Ref |
| 45-64 | 0.83 (0.76-0.91) | <0.01 |
| 65-74 | 0.73 (0.67-0.80) | <0.01 |
| 75+ | 0.40 (0.35-0.44) | <0.01 |
| Race | ||
| White | 1.00 | Ref |
| Black | 1.13 (1.02-1.25) | 0.026 |
| Other | 0.93 (0.85-1.03) | 0.15 |
| Gender | ||
| Female | 1.00 | Ref |
| Male | 1.03 (0.98 -1.10) | 0.25 |
| Comorbidities | ||
| 0 | 1.00 | Ref |
| 1-2 | 0.99 (0.91-1.07) | 0.79 |
| 3+ | 0.88 (0.79-0.97) | 0.014 |
| Household | ||
| Income | ||
| $63K+ | 1.00 | Ref |
| $1-38,999 | 0.82 (0.75-0.89) | <0.01 |
| $39K-47,999 | 0.83 (0.77-0.91) | <0.01 |
| $48K-62,999 | 0.87 (0.80 -0.94) | <0.01 |
| Hospital location | ||
| Rural | 1.00 | Ref |
| Urban | 1.32 (1.16 1.51) | <0.01 |
| Teaching status | ||
| Teaching | 1.00 | Ref |
| Non-teaching | 1.80 (1.69-1.92) | <0.01 |
| Bed Size | ||
| Small | 1.00 | Ref |
| Medium | 1.33 (1.21-1.47) | <0.01 |
| Large | 1.02 (0.91-1.14) | 0.77 |
| Region | ||
| South | 1.00 | Ref |
| Northeast | 1.40 (1.30-1.51) | <0.01 |
| Midwest | 1.08 (1.00-1.17) | 0.045 |
| West | 0.98 (0.91-1.07) | 0.67 |
Table 3.
The interaction between time period of surgery and chronic kidney disease and its association withlikelihood of partial nephrectomy among patients undergoing surgery for kidney cancer.
| Variable | Odds Ratio (95% Cl) | p value |
|---|---|---|
| Surgery Date ± CKD* | ||
| Pre-guidelines+No CKD | 1.00 | Ref |
| Post guidelines+No CKD | 1.19 (1.05-1.35) | <0.01 |
| Pre-guidelines+CKD | 1.05 (0.96-1.15) | 0.30 |
| Post guidelines+CKD | 1.20 (1.08-1.34) | <0.01 |
Adjusted for year of surgery, age, race, gender, household income, insurance, hospital location, hospital teaching status, bed size, and region.
Acknowledgements
This study used 2007 – 2010 Healthcare Cost and Utilization Project Nationwide Inpatient Sample as well as the 2009-2010 Area Resource File. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of United States Department of Health and Human Services Agency for Healthcare Research and Quality as well as the Health Resources and Services Administration in the creation of these databases.
Funding:
The Louis Feil Charitable Lead Trust
United States Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service. Dr. Makarov is a VA HSR&D Career Development awardee at the Manhattan VA.
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
The authors would like to acknowledge Huilin Li, Phd, Department of Biostatistics, New York University for her programming assistance.
Appendix
Appendix 1.
ICD-9-CM diagnostic codes for etiologies of CKD.
| Risk for renal impairment | ICD-9-CM Diagnostic Code |
|---|---|
| Diabetes | 250 |
| Hypertensive disease | 401.x |
| 402.x | |
| 403.00 | |
| 403.10 | |
| 403.90 | |
| 404.00 | |
| 404.01 | |
| 404.10 | |
| 404.11 | |
| 404.90 | |
| 404.91 | |
| 405.x | |
| Chronic Kidney Disease | 585.1 |
| 585.2 | |
| 585.3 | |
| 585.4 | |
| 585.9 | |
| Nephrotic syndrome | 581.x |
| Chronic glomerulonephritis | 582.x |
| Nephritis and nephropathy, not specified as acute or chronic |
583.x |
| Cystic kidney disease | 753.1 |
| Atherosclerosis | 440.1 |
| Amyloidosis | 277.3x |
| Sickle-cell disease | 282.6x |
| Systemic lupus erythematosus | 710.0 |
| Arteritis/vasculitis unspecified | 447.6 |
| Lupus erythematosus | 695.4 |
| Tobacco use disorder | 305.1 |
| Vesicoureteral reflux | 593.7x |
| Hyperplasia of prostate, unspecified, with urinary obstruction and other lower urinary tract symptoms |
600.91 |
| Hypertrophy (benign) of prostate with urinary obstruction and other lower urinary tract symptoms |
600.01 |
| Urinary tract infection, site not specified | 599.0 |
| Disorders resulting from impaired renal function |
588.x |
| Small kidney of unknown cause | 589.x |
| Infections of kidney | 590.x |
| Acute glomerulonephritis | 580.x |
| Renal agenesis and dysgenesis (Solitary kidney) |
753.0 |
| Renal sclerosis, unspecified | 587 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: None
This manuscript was presented at the 2012 Society of Urologic Oncology Annual Meeting, Bethesda, Maryland, November, 2012.
REFERENCES
- 1.Miller DC, Hollingsworth JM, Hafez KS, Daignault S, Hollenbeck BK. Partial nephrectomy for small renal masses: an emerging quality of care concern? J Urol. 2006;175:853–7. doi: 10.1016/S0022-5347(05)00422-2. [DOI] [PubMed] [Google Scholar]
- 2.Weight CJ, Crispen PL, Breau RH, Kim SP, Lohse CM, Boorjian SA, Thompson RH, Leibovich BC. Practice-Setting and Surgeon Characteristics Heavily Influence the Decision to Perform Partial Nephrectomy among American Urologic Association Surgeons. BJU Int. 2013;111:731–838. doi: 10.1111/j.1464-410X.2012.11112.x. [DOI] [PubMed] [Google Scholar]
- 3.Cooperberg MR, Mallin K, Kane CJ, Carroll PR. Trends for stage I renal cell carcinoma. J Urol. 2011;186:304–9. doi: 10.1016/j.juro.2011.03.130. [DOI] [PubMed] [Google Scholar]
- 4.Patel SG, Penson DF, Pabla B, et al. National trends in the use of partial nephrectomy: a rising tide that has not lifted all boats. J Urol. 2010;187:816–21. doi: 10.1016/j.juro.2011.10.173. [DOI] [PubMed] [Google Scholar]
- 5.Kim SP, Shah ND, Weight CJ, et al. Contemporary trends in nephrectomy for renal cell carcinoma in the United States: results from a population based cohort. J Urol. 2011;186:1779–85. doi: 10.1016/j.juro.2011.07.041. [DOI] [PubMed] [Google Scholar]
- 6.Lugtenberg M, Burgers JS, Westert GP. Effects of evidence-based clinical practice guidelines on quality of care: a systematic review. Qual Saf Health care. 2009;18(5):385–92. doi: 10.1136/qshc.2008.028043. [DOI] [PubMed] [Google Scholar]
- 7.Cabana MD, Rand SC, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? JAMA. 1999;282(15):1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]