Abstract
Objective:
The Protonics brace is a functional resistance brace designed for rehabilitative use in patients with patellofemoral pain syndrome. Our objective was to determine whether the Protonics brace altered quadriceps muscle activity or knee mechanics in healthy subjects.
Design and Setting:
We used a within-subjects design in a laboratory setting.
Subjects:
Nineteen recreationally active college students (10 females, 9 males; age = 22.6 ± 2.8 years; height = 172 ± 9.0 cm, mass = 69.7 ± 12.5 kg) with no history of patellofemoral pain syndrome.
Measurements:
A standard-length Protonics brace was fit to each subject's leg. Surface electromyography of the vastus medialis obliquus, vastus lateralis, and rectus femoris muscles was recorded during a lateral step-down exercise. Lower extremity kinematics and ground reaction force were assessed during stair descent. Subjects performed both tasks under 4 conditions: no brace and brace with low, medium, and high resistance. Electromyography values were normalized to a maximum voluntary isometric contraction. The brace moment was determined by passive testing in an isokinetic dynamometer. Changes in the subject's muscular knee-extension moment were determined by subtracting the extension moment provided by the brace from the total knee-extension moment calculated from motion and force data using an inverse dynamics approach.
Results:
Vastus medialis obliquus activity in the brace at the low- and medium-resistance settings was significantly lower than that measured without the brace. Vastus lateralis activity while wearing the brace at medium resistance was significantly less than in the absence of the brace. Regardless of brace setting, vastus medialis obliquus and vastus lateralis activity in the descending phase of the exercise was less than during the ascending phase. A significant interaction was noted between brace setting and phase of the step-down exercise for rectus femoris activity. Significantly less activity was seen in the descending phase than in the ascending phase. Post hoc testing indicated that, in the descending phase, less activity was demonstrated with the brace at the medium and high settings than at the low setting. Muscle activity at the high setting and activity at low resistance were also significantly less than when the brace was not worn in the ascending phase. Knee flexion and extension moment during stair descent were significantly less at the higher resistance settings.
Conclusions:
Wearing the Protonics brace at moderate or high resistance during the lateral step-down exercise produced less quadriceps activity compared with not wearing the brace. The knee extensor mechanism was unloaded when the brace was worn during stair descent. These findings indicate that the Protonics brace may unload the quadriceps and therefore decrease the load on the patellofemoral joint.
Keywords: patellofemoral pain, knee, unloading
Patellofemoral pain syndrome (PFPS) is the cause of 20% to 40% of visits to sports medicine clinics because of knee disorders1,2 and 10% of all visits to musculoskeletal sports medicine clinics.2 Patellofemoral pain syndrome is especially prevalent in active young adults,3 who constitute the population with whom athletic trainers are most likely to work. The incidence of PFPS in athletes has been reported to be as high as 1 in 4.4 Treating PFPS can be a very frustrating and time-consuming task for both the athlete and athletic trainer, partly because of the multifactorial nature of the condition. Extrinsic factors such as playing surface, overtraining, and footwear can contribute, as can intrinsic factors such as skeletal alignment, muscle weakness, and poor neuromuscular control of the lower extremity.5 Both researchers and practitioners continue to investigate new techniques to more effectively treat PFPS.
A recent addition to PFPS rehabilitation is the Protonics brace (Empi, St Paul, MN), a long-leg brace with a hinged knee that is designed to provide variable resistance to flexion, independent of velocity and gravity6 (Figure 1). According to the manufacturer's Web site, product information, and a continuing education course, the theoretic basis for Protonics rests on the idea that PFPS is caused by biomechanical abnormalities that are related to abnormal pelvic position.7,8 It is proposed that biomechanical abnormalities, such as an anteriorly rotated pelvis and internally rotated femur, and soft tissue abnormalities, such as hypertonicity of the tensor fascia latae and vastus lateralis and iliopsoas muscles, and inhibition of the hamstrings and gluteal muscles may lead to abnormal lateral tracking of the patella and PFPS.7,8 However, caution should be used in interpreting these theories because no evidence to substantiate them is found in the scientific literature.
Figure 1.
Protonics functional resistance system.
The brace is designed to be worn during therapeutic exercises and activities of daily living. Ten settings provide various levels of resistance to knee flexion; with each increased setting, the hamstrings must generate more force to flex the knee. The treatment begins by fitting the brace on the patient's leg and finding the functional resistance setting (FRS). This is the lowest setting at which the patient can ascend and descend one step without pain. An underlying assumption for the FRS is that increased resistance in the hinge causes the quadriceps muscle to be unloaded, thereby reducing muscle activity, patellofemoral joint reaction force, and pain. This assumption has not, however, been tested experimentally. Patients then perform knee-flexion exercises intended to recruit the hamstrings, and the contention is that immediate changes in pelvic position and flexibility of the hip flexors and iliotibial band can be seen because of neural adaptation. The patient wears the brace during daily activity and while traditional PFPS exercises are performed.6,8
Although clinical trials support the effectiveness of the Protonics brace in treating PFPS,9,10 it is not known whether decreases in pain are a result of pelvic repositioning or unloading of the quadriceps while the brace is worn at the FRS. The application of any external force (in this case, the brace) has the potential to change the muscular and mechanical functions of the lower extremity of healthy individuals, as well as those with an injury.11 Therefore, our purposes were to determine (1) whether wearing the brace at various resistance levels during a lateral step-down exercise changes quadriceps muscle activity, and (2) whether wearing the brace at various resistance levels during stair descent changes the biomechanics of the knee. Our hypothesis was that wearing the brace with high resistance would decrease quadriceps electromyographic activity, knee-flexion angle, and knee-extension moment during closed kinetic chain activities.
METHODS
Subjects
Nineteen recreationally active college students (10 females, 9 males; age = 22.6 ± 2.8 years, height = 172 ± 9.0 cm, mass = 69.7 ± 12.5 kg) with no history of anterior knee pain were recruited. Subjects were free from any balance or vestibular disorders and were not suffering from an injury to the lower extremity, hip, or low back at the time of testing. All subjects read and signed an informed consent form approved by the university institutional review board, which also approved the study.
Instrumentation
All subjects were fitted with a regular-sized Protonics knee brace. The Biopac MP100 System (Biopac Systems Inc, Santa Barbara, CA) was used to collect all electromyography (EMG) data, which were recorded from the vastus medialis obliquus (VMO), vastus lateralis (VL), and rectus femoris (RF) using 10-mm contact-area Ag-AgCl disposable electrodes with an interelectrode distance of 1 cm (Biopac Systems Inc). We performed skin preparation and electrode placement according to a standard protocol for surface EMG.12 The following EMG settings were used: band width = 10 to 500 Hz, input impedance = 2 MΩ (differential), common mode rejection ratio = 110 dB, maximum input voltage = ± 10 V, sampling rate = 1000 Hz, gain = 1000. An electrogoniometer (Penny and Giles Biometrics Ltd, Gwent, UK) was used to monitor the knee angle during the lateral step-down.
The Vicon System 370 (Oxford Metrics, Oxford, UK) was used to collect 3-dimensional kinematic data during stair descent. Video images were recorded at 60 Hz. A 7-step staircase with force plates (Kistler Instrument Corp, Amherst, NY) embedded into the second and fourth stairs from the top landing was used. Force-plate data were sampled at 1200 Hz.
Procedures
Lateral Step-Down Exercise
Subject preparation began with our shaving and vigorously cleaning with alcohol the areas of electrode attachment. Two electrodes were applied to the VMO and VL over the area of greatest muscle bulk in the presumed direction of the muscle fibers. The locations were chosen such that the electrodes remained over the muscle during the entire range of motion. The RF electrodes were placed on the anterior thigh halfway between the anterior superior iliac spine and the patella. All electrode positions were confirmed by palpation during contraction of each muscle. An electrogoniometer was placed across the lateral aspect of the knee and used to differentiate between the descending and ascending phases of the step-down exercise.
After electrode placement and a brief warm-up, maximum voluntary isometric contractions (MVICs) were performed and used for normalization. The MVIC was elicited by having the subject stand with his or her back against the wall with the hips and knees flexed to 90° and 60°, respectively. The feet were placed on an angled block to prevent sliding. Subjects were instructed to stand on one leg and push as hard as possible, driving the back against the wall (Figure 2). Three separate 5-second MVIC trials were recorded. Pilot testing indicated this was an effective way to produce an MVIC for the quadriceps in a functional position.13
Figure 2.
Measurements for a closed kinetic chain maximum voluntary isometric contraction were collected and used to normalize all electromyographic data.
To begin the step-down exercise, subjects stood on the test leg at the edge of a 24.5-cm-high block. Subjects were instructed to slowly bend the knee, lowering the opposite leg to lightly touch the floor, and then return to a standing position. Each subject performed 3 lateral step-downs under each of 4 conditions: no brace and wearing the brace with low, medium, and high resistance. These settings were chosen because they cover the range of settings that may be used as the FRS for patients with PFPS. The no-brace condition was always measured first to familiarize the subject with the task. The order of brace-resistance settings was randomly assigned.
Stair Descent
The 10 female subjects also performed stair- descent trials to allow us to determine knee-extension moments. Testing of the females was completed first, and scheduling and equipment constraints prevented similar testing of the 9 male subjects. Kinematic and kinetic variables were determined using the following procedures. Four reflective markers were attached to thermoplastic plates that were attached to the lateral lower extremity with double-sided tape and elastic wrap. Markers were tracked during the stair-descent trials using 6 cameras arranged within 180° of each other to capture unilateral lower extremity motion. Anatomical reference frames were established by identifying control points as described by Cappozzo et al.14 Global and local reference frames were established using a right-handed coordinate system in accordance with International Society of Biomechanics standards.15
Data Acquisition
Data were saved and further analyzed on a personal computer. Because the brace works differently in the descending phase than in the ascending phase, the lateral step-down task was divided into descending and ascending phases based on electrogoniometer data. MATLAB software (Mathworks Inc, Natick, MA) was used to create a custom program for EMG data analysis. The raw EMG signal was corrected for a baseline drift, and the root mean square was calculated over a 0.5- second moving window. The maximum root mean squares of all MVIC trials were averaged and used for normalization. The trial root mean square values were divided by the averaged MVIC value to produce percentage of maximum activity. These data were used for further analyses.
Three-dimensional motions of the pelvis, thigh, shank, and foot segments were computed from target cluster marker locations as a postprocessing step. Kinematic data were filtered at 6 Hz using a fourth-order, zero-lag Butterworth filter.16 The position and orientation of the segments were obtained from marker data using the least squares method.17 Joint angles were derived using a joint coordinate system described by Grood and Suntay.18
We used body-segment kinematics in conjunction with ground reaction forces to compute muscular joint moments using inverse dynamics,16 in which muscular joint moments and net joint reaction forces are computed from measurements of the kinematics of individual body segments. The total internal knee-extension moment was calculated this way. The resistance moment in the brace hinge was determined by testing the brace alone in an isokinetic dynamometer. As the brace was flexed, the dynamometer recorded an extension moment in the brace hinge. Regression equations were used to predict the moment at any flexion angle. The extension moment produced by the subject was calculated by subtracting the resistance moment in the brace hinge from the total internal knee- extension moment throughout the range of motion. The derived value represented the extension moment (or extension torque) that the subject (rather than the brace) produced to control knee flexion.
Statistical Analysis
The dependent variables were a percentage of maximum EMG activity of each of the 3 muscles. We used the Statistical Package for the Social Sciences (version 10.0; SPSS Inc, Chicago, IL) to compute separate, repeated-measures analyses of variance with 2 within-subjects variables: brace condition (no brace or low-, medium-, or high-resistance brace) and phase of the step-down (descending, ascending) for each of the muscles. Additional repeated-measures analyses of variance with one within-subjects variable (brace condition) were calculated for peak knee-flexion angle during stance and internal knee- flexion moment. One subject's kinetic data were not used for technical reasons. The significance level was preset at 0.05 for all analyses, and Tukey post hoc testing was used to identify specific significant relationships.
RESULTS
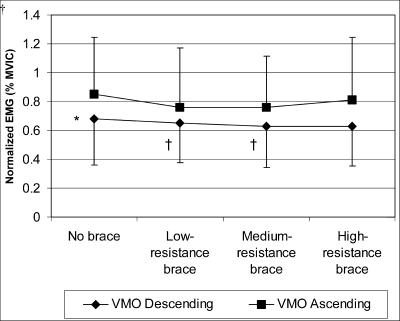
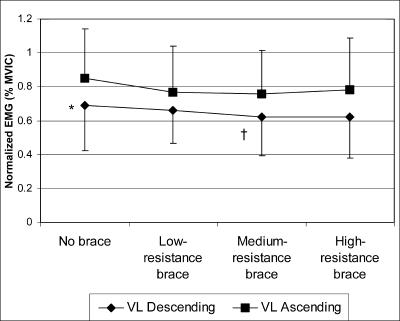
No significant interactions were noted between brace setting and phase for the VMO or VL. There was, however, a significant main effect of brace setting for both the VMO (F3,51 = 7.115, P < .0005; Figure 3) and VL (F3,51 = 5.470, P = .002; Figure 4). The VMO activity at the low- and medium-resistance settings was significantly lower than with the no-brace condition, and VL activity while wearing the brace with medium resistance was significantly less than under the no-brace condition.
Figure 3.
Normalized vastus medialis obliquus activity. *Main effect for phase: independent of brace setting, electromyographic activity (EMG) for the descending phase was significantly less than the ascending phase (P < .05). †Main effect of brace setting: independent of phase, EMG activity for the low-resistance and medium- resistance brace settings was significantly less than under the no- brace condition (P < .05). VMO indicates vastus medial obliquus muscle; MVIC, maximum voluntary isometric contraction.
Figure 4.
Normalized vastus lateralis activity. *Main effect for phase: independent of brace setting, electromyographic (EMG) activity in the descending phase was significantly less than in the ascending phase (P < .05). †Main effect of brace setting: independent of phase, EMG activity at the medium-resistance brace setting was significantly less than under the no-brace condition (P < .05). MVIC indicates maximum voluntary isometric contraction.
Regardless of brace setting, the muscle activity in the descending phase of the exercise was less than that during the ascending phase for both the VMO (F1,17 = 11.775, P = .003) and VL (F1,17 = 37.241, P < .0005; Figures 3 and 4).
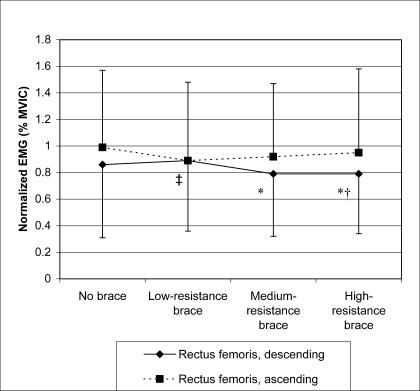
The interaction between brace setting and phase of the step- down for RF activity was significant (F3,51 = 4.518, P = .007). Activity in the descending phase with the brace at the medium and high settings was less than at the low setting (Figure 5). The high setting also resulted in significantly less activity than when the brace was not worn. In the ascending phase, activity at low resistance was significantly less than when the brace was not worn (Tukey post hoc testing, P < .05).
Figure 5.
Normalized rectus femoris activity. *Electromyographic (EMG) activity in the descending phase at the medium- and high- resistance settings was significantly less than at the low-resistance setting (P < .05). †EMG activity at the high-resistance setting in the descending phase was significantly less than with the no- brace condition (P < .05). ‡In the ascending phase, activity at the low-resistance setting was significantly less than when the brace was not worn. MVIC indicates maximum voluntary isometric contraction.
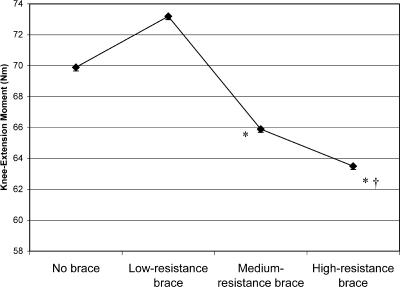
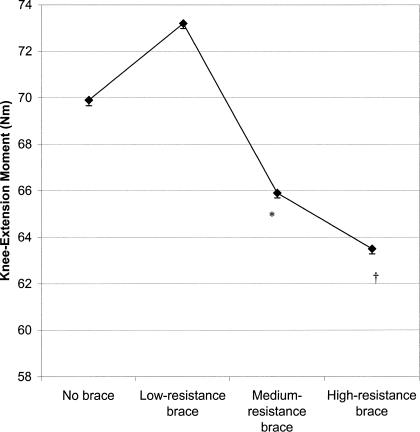
Significant differences in knee flexion during stance (F3,27 = 8.072, P = .001) and knee-extension moment between brace conditions (F3,24 = 6.693, P = .002) were seen. Knee flexion at medium or high resistance was significantly less than when subjects did not wear the brace (Figure 6). Knee flexion at high resistance was also significantly less that at low resistance. The subjects' knee-extension moments were significantly lower at high resistance, compared with all other conditions (Figure 7). The medium-resistance setting also resulted in subjects producing less knee-extension moment than they did in the unbraced or low-resistance conditions.(Tukey post hoc testing, P < .05).
Figure 6.
Knee-flexion angle at each brace condition. *Knee-flexion angle at the medium- and high-resistance brace settings was significantly less than under the no-brace condition (P > .05). †Knee- flexion angle at the high-resistance brace setting was significantly less than at the low-resistance setting (P < .05).
Figure 7.
Knee-extension moment at each brace condition. *Significantly less knee-extension moment with the medium-resistance brace than with either the low-resistance brace or no brace (P < .05). †Significantly less knee-extension moment than with all other conditions (P > .05).
DISCUSSION
Knee flexion during a closed kinetic chain task is controlled primarily by the quadriceps producing a knee-extension moment. The hinge in the Protonics brace is designed to resist flexion with a variable resistance setting. Our results support our initial hypothesis. When worn during a closed kinetic chain task, the brace resists flexion about the knee and therefore assists the quadriceps in controlling knee flexion. Our study has demonstrated that increasing resistance in the brace does decrease knee-flexion angle and knee-extension moment during the stance phase of stair descent. Furthermore, quadriceps activity is significantly decreased when wearing the brace with some level of resistance during a closed kinetic chain knee-flexion exercise, and this may result in a decreased patellofemoral joint reaction force. Thus, the brace does unload the quadriceps in healthy subjects.
Although an overall trend was shown in decreased VMO and VL activity as brace resistance increased, muscle activity with the brace at the high setting did not differ. One possible explanation for this is that the high resistance increased the difficulty of the task, which may have increased the variability in how the subjects performed the task. A second explanation may be that, even though muscle activity in the descending phase at the high setting decreased, muscle activity increased slightly in the ascending phase. This may have suppressed the main effect of brace setting at high resistance. The VMO and VL activity was lower in the ascending phase than in the descending phase.
The RF exhibited activation patterns similar to the VMO and VL. Consistent with the other muscles, RF activity in the descending phase was lower than that during the ascending phase in all conditions except the low setting. Why a difference in phases existed at the low setting for the other muscles but not for the RF is unclear. However, the standard deviations for the RF were almost twice those of the VMO and VL, which may explain the unusual findings. Increased variance may be attributed to the fact that the RF is a biarticular muscle, and its action at the hip and knee would be reflected in the muscle activity.
Authors of other EMG studies of quadriceps activity during the lateral step-down reported similar magnitudes of normalized EMG to those we found.19,20 The current finding of the eccentric, or descending, phase producing less VMO and VL activity than the concentric, or ascending, phase is supported by the previous literature.20–22 Because less torque must be generated during the descending phase and because muscle fibers produce stronger contractions eccentrically, fewer fibers are activated during this phase of the step-down.
In the only published study examining EMG activity in subjects wearing the Protonics brace, Diaz et al23 examined lower extremity muscle activity during gait in normal subjects. At the time of their study, the brace had settings that resisted both flexion and extension. The hypothesis that increasing hamstrings activity would result from resistance to flexion was rejected when the authors found that even at the highest resistance setting, hamstrings activity was not significantly increased during gait. Unlike our findings, quadriceps activity was unchanged when the brace was set to resist flexion.23 The demand on the quadriceps during a step-down is much greater than during level walking and may explain why the quadriceps-unloading effect was not seen during level walking.
The reduced knee flexion we observed is a clinically significant finding because it is a primary determinant of the patellofemoral joint reaction force, which has been related to PFPS.24 This may be beneficial for a patient with PFPS in the acute stages, when little exercise is tolerated because of pain. On the contrary, this finding indicates that the brace may cause changes in movement patterns that may produce detrimental effects in the future. Similar research on the effects of functional knee braces in healthy subjects has proven useful in understanding gait and muscular alterations seen in individuals with anterior cruciate ligament reconstructions.25
Although the internal knee-extension moment is not a direct measure of quadriceps force, the quadriceps are the major contributor to the knee-extension moment. If we assume that the passive knee-extension moments caused by skin and other connective tissues are negligible, we can conclude that the decrease in knee-extension moment is the result of less quadriceps force.
The combination of the EMG, kinematic, and kinetic results provides strong evidence that the Protonics brace unloads the quadriceps. This unloading is likely to decrease patellofemoral joint reaction force, although we did not measure this value directly. A limitation of the study is that the EMG and biomechanical data could not be collected simultaneously because of difficulties encountered in securing the electrodes, marker clusters, and brace at the same time. We felt that examining both the lateral step-down, which is used clinically, and a common activity such as stair descent provided more insight into how the brace affected the extensor mechanism. Although healthy subjects were tested, it is reasonable to assume that the brace would mechanically affect subjects with PFPS the same way, and we will investigate this assumption in a future study. However, we feel that quadriceps unloading may explain why the brace causes immediate pain relief in patients with PFPS.
CONCLUSIONS
We did not address the theories about the relationship between abnormal pelvic rotation and PFPS described by the Protonics manufacturer. Our findings have, however, added to the clinical and scientific knowledge by demonstrating that wearing the Protonics brace with some resistance during a closed kinetic chain task decreases the muscular activity of the VMO, VL, and RF in healthy individuals. These results strongly suggest that the brace unloads the quadriceps muscle, which may reduce patellofemoral joint reaction forces through a functional range of motion, thereby explaining why patients feel immediate relief when the brace is applied. More research is needed to understand how the brace affects patients with PFPS and the long-term effects of Protonics use in these patients.
ACKNOWLEDGMENTS
This research was funded by the Eastern Athletic Trainers' Association Research Committee Award, 2001.
REFERENCES
- 1.DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- 2.Kannus P, Natri A, Paakkala T, Jarvinen M. An outcome study of chronic patellofemoral pain syndrome: seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81:355–363. doi: 10.2106/00004623-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Fulkerson JP, Hungerford DS. Disorders of the Patellofemoral Joint. Baltimore, MD: Williams & Wilkins; 1990. [Google Scholar]
- 4.Devereaux MD, Lachmann SM. Patellofemoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two-year prospective study. Am J Sports Med. 2000;28:480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 6.Protonics Resistance System Owner's Manual. Lincoln, NE: Inverse Corp; 1995. Empi. [Google Scholar]
- 7.Hruska R. Pelvic stability influences lower-extremity kinematics. Biomechanics. 1998;10:23–29. [Google Scholar]
- 8.Hruska R. A New Approach to Treating Patellofemoral Pain. Lincoln, NE: Clinical Education and Resource Center, Empi; 1999. [Google Scholar]
- 9.Timm KE. The clinical and cost-effectiveness of two different programs for rehabilitation following ACL reconstruction. J Orthop Sports Phys Ther. 1997;25:43–48. doi: 10.2519/jospt.1997.25.1.43. [DOI] [PubMed] [Google Scholar]
- 10.Timm KE. Randomized controlled trial of Protonics on patellar pain, position, and function. Med Sci Sports Exerc. 1998;30:665–670. doi: 10.1097/00005768-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Latash ML. Neurophysiological Basis of Movement. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 12.Cram JR, Kasman GS. Introduction to Surface Electromyography. Gaithersburg, MD: Aspen Publishers, Inc; 1998. [Google Scholar]
- 13.Hertel J, Earl JE, Tsang K, Miller SJ. Differences in quadriceps EMG activity during an open and closed kinetic chain knee extension maximal voluntary isometric contractions [abstract] J Athl Train. 2001;36(suppl):S35. [Google Scholar]
- 14.Cappozzo A, Catani R, Della Croce UD, Leardini A. Position and orientation in space of bones during movement: anatomical frame definition and determination. Clin Biomech (Bristol, Avon) 1995;10:171–178. doi: 10.1016/0268-0033(95)91394-t. [DOI] [PubMed] [Google Scholar]
- 15.Wu G, Cavanagh PR. ISB recommendations for standardization in the reporting of kinematic data. J Biomech. 1995;28:1257–1261. doi: 10.1016/0021-9290(95)00017-c. [DOI] [PubMed] [Google Scholar]
- 16.Winter D. Biomechanics and Motor Control of Human Movement. New York, NY: John Wiley & Sons; 1990. [Google Scholar]
- 17.Challis JH. A procedure for determining rigid body transformation parameters. J Biomech. 1995;28:733–737. doi: 10.1016/0021-9290(94)00116-l. [DOI] [PubMed] [Google Scholar]
- 18.Grood E, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: applications to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 19.Cook TM, Zimmerman CL, Lux KM, Neubrand CM, Nicholson TD. EMG comparison of lateral step-up and stepping machine exercise. J Orthop Sports Phys Ther. 1992;16:108–113. doi: 10.2519/jospt.1992.16.3.108. [DOI] [PubMed] [Google Scholar]
- 20.Brask B, Lueke RH, Soderberg GL. Electromyographic analysis of selected muscles during the lateral step-up exercise. Phys Ther. 1984;64:324–329. doi: 10.1093/ptj/64.3.324. [DOI] [PubMed] [Google Scholar]
- 21.Worrell TW, Crisp E, LaRosa C. Electromyographic reliability and analysis of selected lower extremity muscles during lateral step-up conditions. J Athl Train. 1998;33:156–162. [PMC free article] [PubMed] [Google Scholar]
- 22.Selseth A, Dayton M, Cordova M, Ingersoll C, Merrick M. Quadriceps concentric EMG activity is greater than eccentric EMG activity during the lateral step-up exercise. J Sport Rehabil. 2000;9:124–134. [Google Scholar]
- 23.Diaz GY, Averett DH, Soderberg GL. Electromyographic analysis of selected lower extremity musculature in normal subjects during ambulation with and without a Protonics knee brace. J Orthop Sports Phys Ther. 1997;26:292–298. doi: 10.2519/jospt.1997.26.6.292. [DOI] [PubMed] [Google Scholar]
- 24.Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clin Orthop. 1979;144:9–15. [PubMed] [Google Scholar]
- 25.DeVita P, Torry M, Glover KL, Speroni DL. A functional knee brace alters joint torque and power patterns during walking and running. J Biomech. 1996;29:583–588. doi: 10.1016/0021-9290(95)00115-8. [DOI] [PubMed] [Google Scholar]