Abstract
Chronic pain is a major clinical problem, yet the mechanisms underlying the transition from acute to chronic pain remain poorly understood. In mice, reduced expression of GPCR kinase 2 (GRK2) in nociceptors promotes cAMP signaling to the guanine nucleotide exchange factor EPAC1 and prolongs the PGE2-induced increase in pain sensitivity (hyperalgesia). Here we hypothesized that reduction of GRK2 or increased EPAC1 in dorsal root ganglion (DRG) neurons would promote the transition to chronic pain. We used 2 mouse models of hyperalgesic priming in which the transition from acute to chronic PGE2-induced hyperalgesia occurs. Hyperalgesic priming with carrageenan induced a sustained decrease in nociceptor GRK2, whereas priming with the PKCε agonist ΨεRACK increased DRG EPAC1. When either GRK2 was increased in vivo by viral-based gene transfer or EPAC1 was decreased in vivo, as was the case for mice heterozygous for Epac1 or mice treated with Epac1 antisense oligodeoxynucleotides, chronic PGE2-induced hyperalgesia development was prevented in the 2 priming models. Using the CFA model of chronic inflammatory pain, we found that increasing GRK2 or decreasing EPAC1 inhibited chronic hyperalgesia. Our data suggest that therapies targeted at balancing nociceptor GRK2 and EPAC1 levels have promise for the prevention and treatment of chronic pain.
Introduction
According to a recent report by the NIH, chronic pain affects more than 100 million people in the United States (1). The same report concludes that increased understanding of the mechanisms contributing to the development of chronic pain is key to finding novel interventions by which to prevent it.
Inflammatory mediators induce pain by direct activation of nociceptive terminals, but also increase the sensitivity to painful stimuli, a phenomenon known as hyperalgesia (2–4). This inflammatory hyperalgesia is generated by peripheral sensitization of nociceptive neurons as well as by central sensitization at the level of the spinal cord (5–7). In most cases, inflammatory pain and hyperalgesia resolve after resolution of inflammation or after tissues heal. However, in a significant subset of patients, pain does not resolve, and chronic pain develops. For example, approximately 10%–15% of patients with herpes zoster–induced rash develop postherpetic pain, defined as pain lasting at least 3 months after healing of the rash (8). Chronic postsurgical pain is observed even more frequently, for example, in patients undergoing thoracotomy (50%), breast surgery (30%), or cholecystectomy (10%–20%) (9).
The mechanisms underlying the development of persistent pain are poorly understood, and this is a major limitation for identification of new and adequate treatments. At the level of signaling pathways in peripheral nociceptors, recent studies have shown that mammalian target of rapamycin– (mTOR-) and ERK-dependent pathways play a critical role in chronic pain (10–14). Models of hyperalgesic priming have been developed as a tool to study the transition to chronic pain (10, 15, 16). In these models, short-lasting hyperalgesia is induced by intraplantar injection of, for example, a low dose of carrageenan, the PKCε activator ΨεRACK (HDAPIGYD; pseudoreceptor octapeptide for activated PKCε), or the inflammatory cytokine IL-6 into the hind paw (10, 15, 16). After this transient period of hyperalgesia, changes occur in primary sensory neurons that lead to marked prolongation of the hyperalgesic response to a subsequent exposure to the inflammatory mediator PGE2 (10, 15–17). Both mTOR- and ERK-dependent pathways play a critical role in nociceptive plasticity in hyperalgesic priming (10). In addition, in rats primed with carrageenan or ΨεRACK, prolonged PGE2-induced hyperalgesia depends on activation of ERK and PKCε. In naive rats, the classic cAMP/PKA pathway is critical for the transient hyperalgesia in response to PGE2 (17). cAMP-to-PKCε signaling is thought to be mediated via exchange protein directly activated by cAMP (EPAC; refs. 18, 19), and EPAC activation by intraplantar injection of the specific agonist 8-pCPT-2′-O-Me-cAMP (8-pCPT) induces hyperalgesia via a PKCε-dependent route (20).
We identified nociceptor GPCR kinase 2 (GRK2) as a novel regulator of the duration of inflammatory hyperalgesia (21–27). GRK2 restrains signaling by promoting desensitization of GPCRs (28) and/or by interacting with multiple components of intracellular signaling pathways (22, 29, 30).
Using sensory neuron–specific Grk2-heterozygous mice (SNS-Grk2+/– mice), which have a cell-specific approximately 50% decrease in nociceptor GRK2, we previously showed that mechanical hyperalgesia induced by PGE2 and other cAMP-inducing agents was significantly prolonged in mice with low nociceptor GRK2 (22, 25). Inhibition of PKA did not affect PGE2 hyperalgesia in SNS-Grk2+/– mice, whereas inhibition of PKCε or ERK prevented the prolongation of PGE2 hyperalgesia (22, 25). These findings indicate that the prolongation of PGE2 hyperalgesia in GRK2-deficient mice involves activation of PKCε- and ERK-dependent signaling pathways (17, 22, 25). We also showed that GRK2 interacts with EPAC1 and inhibits EPAC signaling to its downstream target, RAP1 (22). Moreover, chronic inflammatory pain is associated with a decrease in GRK2 in nociceptors (25). In addition, Ferrari and coworkers showed that a transient decrease in GRK2 resulting from treating rats intrathecally with Grk2 antisense oligodeoxynucleotides (asODNs) prolonged hyperalgesia, in this case via a PKCε-independent and PKA- and SRC tyrosine kinase–dependent mechanism (31).
Here we tested the hypothesis that protein levels of GRK2 and EPAC1 in nociceptors represent key factors regulating persistent hyperalgesia. Using 2 mouse models of hyperalgesic priming, prior nociceptive sensitization with carrageenan and with ΨεRACK, we showed that the induced transition to chronic PGE2 hyperalgesia was mediated by decreased GRK2 and increased EPAC1, respectively. We also showed that the prolongation of PGE2 hyperalgesia in primed mice was inhibited by either upregulation of GRK2 or downregulation of EPAC1 after development of the primed state. These effects occurred regardless of whether GRK2 was decreased or EPAC1 was increased. Changing the balance between GRK2 and EPAC1 may have more general relevance for hyperalgesia, as we also showed using the CFA model of chronic inflammatory pain, in which increasing GRK2 or downregulating EPAC1 inhibited persistent mechanical hyperalgesia.
Results
Hyperalgesic priming.
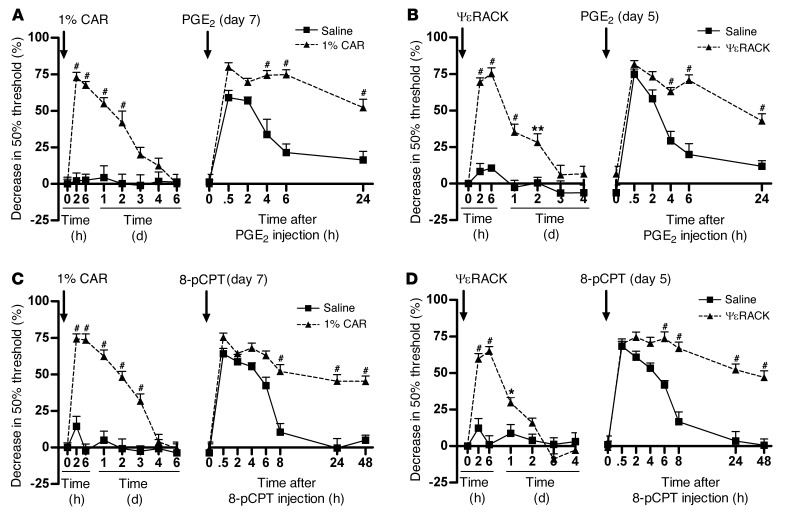
Hyperalgesic priming was induced in mice with an intraplantar injection of carrageenan or ΨεRACK. At 7 days after carrageenan and 5 days after ΨεRACK injection, primed mice received an intraplantar injection of PGE2 or the EPAC activator 8-pCPT.
In carrageenan-primed mice, PGE2-induced mechanical hyperalgesia lasted more than 24 hours, whereas in saline-treated mice, PGE2 hyperalgesia resolved within 6 hours (Figure 1A). In ΨεRACK-primed mice, PGE2 hyperalgesia was also prolonged to more than 24 hours (Figure 1B). Moreover, hyperalgesia induced by 8-pCPT exceeded 48 hours in carrageenan- and ΨεRACK-primed mice, compared with less than 8 hours in control mice (Figure 1, C and D).
Figure 1. Hyperalgesic priming in mice.
(A and C) 7 days after intraplantar carrageenan (CAR; 1%, 5 μl) or saline pretreatment or (B and D) 5 days after intraplantar ΨεRACK (1 μg/paw) or saline pretreatment, mice received an intraplantar injection of (A and B) PGE2 (100 ng/paw) or (C and D) 8-pCPT (12.5 ng/paw). Changes in 50% paw withdrawal threshold were monitored over time. Data represent mean ± SEM. n = 8 per group. *P < 0.05, **P < 0.01, #P < 0.001.
Carrageenan priming also prolonged hyperalgesia induced by the cAMP-inducing mediator epinephrine from 4 days in control mice to almost 2 weeks in primed mice (Supplemental Figure 1A; supplemental material available online with this article; doi: 10.1172/JCI66241DS1). Interestingly, carrageenan priming did not affect hyperalgesia induced by IL-1β (Supplemental Figure 1B), a proinflammatory mediator that does not induce cAMP signaling, but promotes hyperalgesia via a p38-mediated pathway.
GRK2 levels in primary sensory neurons of primed mice.
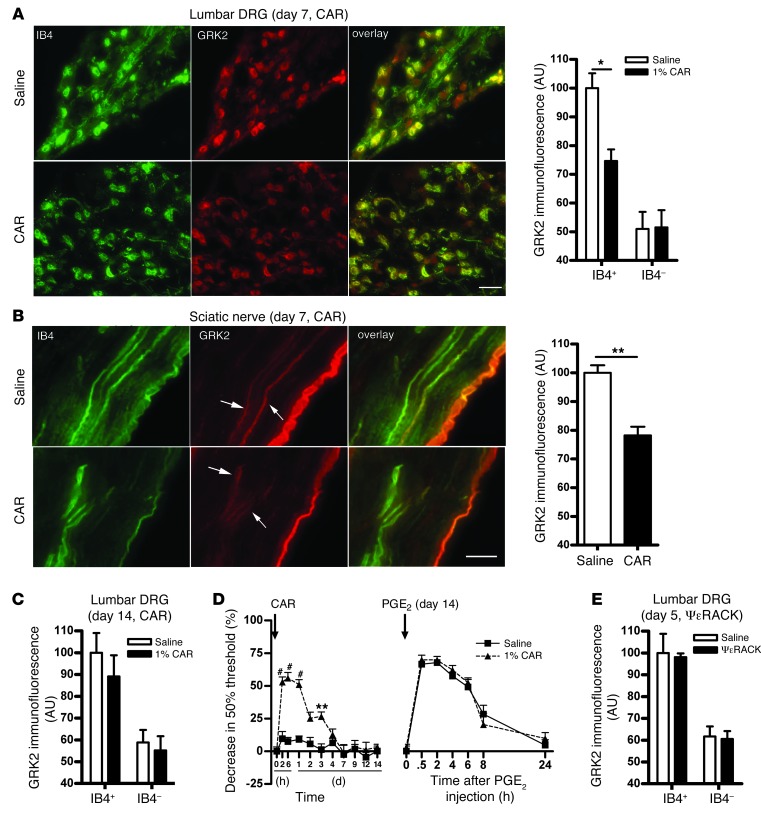
We next determined whether hyperalgesic priming by carrageenan decreases neuronal GRK2 protein levels in dorsal root ganglion (DRG) and sciatic nerve. Because the isolectin B4–positive (IB4+) subpopulation of DRG neurons is known to be involved in hyperalgesic priming (32, 33), we used IB4 as a marker to identify this specific subgroup of sensory neurons.
At 3 and 7 days after intraplantar carrageenan injection into the hind paws, the level of GRK2 in small-diameter IB4+ neurons was reduced by approximately 25% in lumbar DRG (Figure 2A and Supplemental Figure 2). There was no change in GRK2 protein levels in small-diameter IB4– neurons in lumbar DRG after carrageenan priming (Figure 2A and Supplemental Figure 2). In addition, GRK2 levels did not change in thoracic DRG neurons at any time point (Supplemental Figure 3). Western blot analysis of DRG homogenates did not detect changes in GRK2 protein at day 7 after carrageenan priming (Supplemental Figure 4). This is likely due to reduced GRK2 only in IB4+ sensory neurons in response to intraplantar carrageenan.
Figure 2. Carrageenan- and ΨεRACK-induced changes in sensory neuron GRK2 protein expression.
(A and B) Mice received an intraplantar injection of 1% carrageenan or saline, and 7 days later, GRK2 protein levels in IB4+ and IB4– neurons from lumbar DRG, thoracic DRG, and sciatic nerve fibers were quantified by immunofluorescence analysis. Shown are representative images of IB4 (green) and GRK2 (red) double staining of (A) lumbar DRG and (B) sciatic nerves, and mean GRK2 immunofluorescence intensity in (A) lumbar or thoracic DRG and (B) sciatic nerve fibers. Scale bars: 50 μm. (C) Mean GRK2 immunofluorescence intensity in lumbar DRG at 14 days after intraplantar carrageenan or saline. (D) 14 days after carrageenan or saline pretreatment, mice received an intraplantar injection of PGE2 (100 ng/paw). Changes in 50% paw withdrawal threshold were monitored over time. (E) Mean GRK2 immunofluorescence intensity in lumbar DRG at 5 days after intraplantar ΨεRACK or saline. Data represent mean ± SEM (n = 4 per group), based on approximately 300 neurons from lumbar DRG per mouse. *P < 0.05, **P < 0.01, #P < 0.001.
The carrageenan-induced GRK2 decrease in the soma of IB4+ sensory neurons was also reflected in a decrease in axonal GRK2; at 7 days after carrageenan injection, the level of GRK2 in IB4+ fibers was reduced by approximately 20% in the carrageenan- versus the saline-pretreated group (Figure 2B).
At day 14 after intraplantar carrageenan injection, GRK2 levels in small-diameter IB4+ sensory neurons had returned to baseline levels (Figure 2C). The primed state had also resolved at 14 days after carrageenan injection; the course of PGE2 hyperalgesia did not differ between the saline- and carrageenan-pretreated groups at this time point (Figure 2D). These findings show that resolution of the primed state is associated with normalization of GRK2 protein levels.
Notably, when we evaluated GRK2 levels in lumbar DRG at 5 days after ΨεRACK priming, we did not observe any change in GRK2 level. The levels of GRK2 were similar in small-diameter IB4+ lumbar sensory neurons from ΨεRACK-primed and saline-treated mice (Figure 2E). Furthermore, no changes in GRK2 levels were observed in IB4– lumbar DRG neurons or in thoracic DRG neurons after ΨεRACK priming (Supplemental Figure 3).
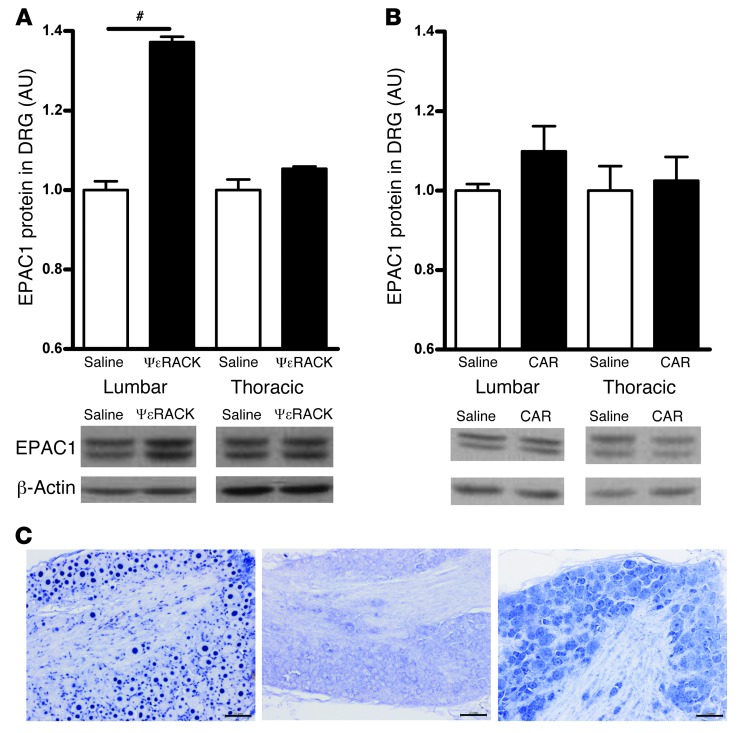
EPAC1 level in DRG after carrageenan and ΨεRACK priming.
After both carrageenan and ΨεRACK priming, hyperalgesia induced by 8-pCPT was significantly prolonged. These findings indicate that in both cases, the primed state is associated with a prolonged hyperalgesic response to EPAC activation. We hypothesized that either a decrease in GRK2 or an increase in EPAC1 would be sufficient to facilitate EPAC1-mediated signaling leading to prolonged PGE2 hyperalgesia. To test this hypothesis, we measured the level of EPAC1 in DRG in these 2 priming conditions. The antibodies available for EPAC1 did not allow reliable staining for this protein in sensory neurons. Therefore, we analyzed EPAC1 levels by Western blotting. EPAC1 levels in lumbar DRG of ΨεRACK-primed mice were increased by approximately 35% compared with levels in saline-treated mice, whereas carrageenan priming did not induce a detectable change in EPAC1 (Figure 3, A and B). To determine which cells in the DRG express EPAC1, we used an in situ hybridization approach. Virtually all neurons in the DRG stained positively for Epac1 mRNA (Figure 3C).
Figure 3. EPAC1 level in DRG after carrageenan- and ΨεRACK-induced priming.
(A and B) EPAC1 protein level in DRG, determined by Western blot analysis of DRG tissue homogenates, at (A) 5 days after ΨεRACK priming and (B) 7 days after carrageenan priming. Data represent mean ± SEM (n = 4 per group). #P < 0.001. (C) Cellular distribution of Epac1 mRNA expression was analyzed by in situ hybridization analysis of lumbar DRG from untreated mice. Representative example from 1 mouse of 3 with similar results. Left: Nuclear staining of positive control (U6 small nuclear RNA probe). Middle: Negative control probe. Right: Epac1 probe. Scale bars: 20 μm.
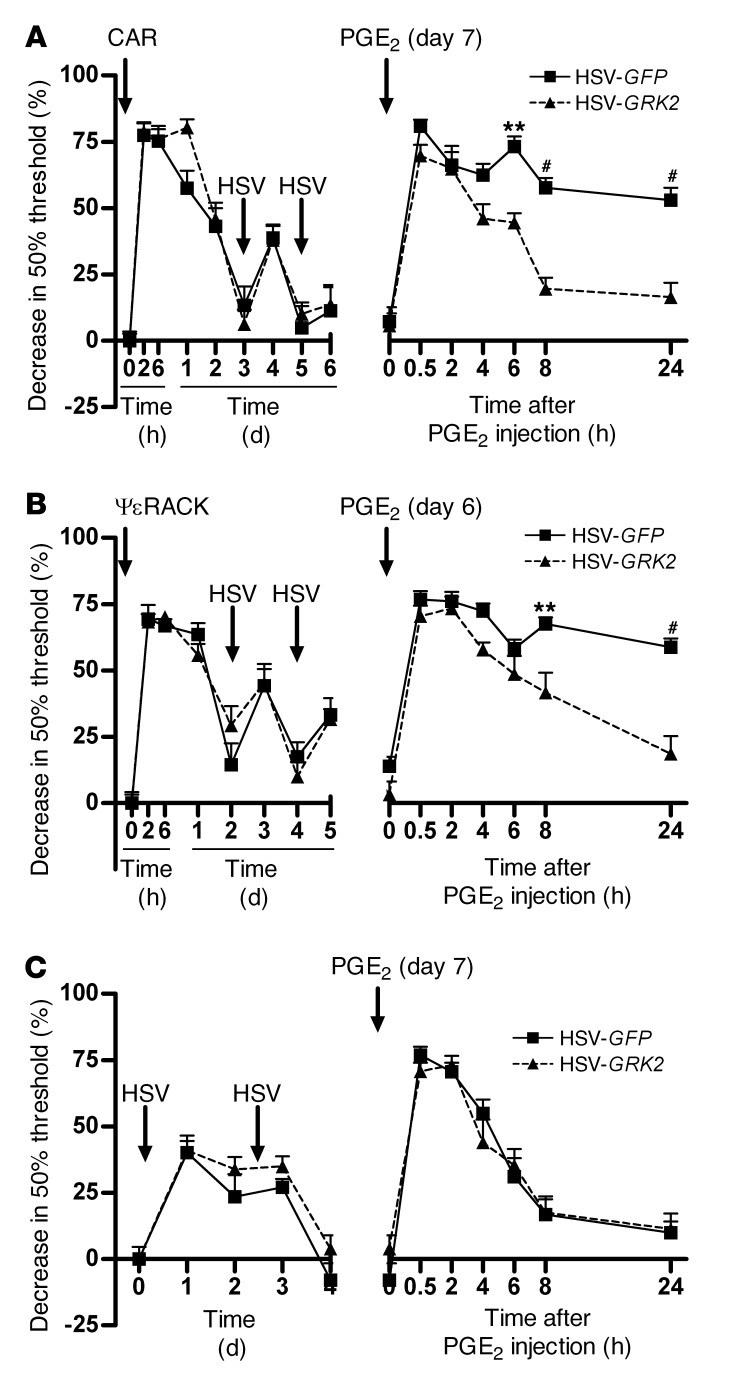
Effect of GRK2 gene transfer on treatment of hyperalgesic priming.
To determine whether the observed changes in GRK2 and EPAC1 levels in the DRG represent potential targets for the prevention of chronic pain, we first examined the effect of increasing GRK2 in DRG neurons in vivo after hyperalgesic priming with carrageenan and ΨεRACK. We used a herpes simplex virus (HSV; ref. 34) vector encoding bovine GRK2 and GFP as a reporter protein (referred to herein as HSV-GRK2) or a control HSV vector containing GFP only (HSV-GFP). In carrageenan-primed mice, treatment with 2.5 μl of 1.4 × 107 pfu/ml HSV-GRK2 at days 3 and 5 significantly shortened PGE2 hyperalgesia compared with mice treated with HSV-GFP (Figure 4A). In ΨεRACK-primed mice, HSV-GRK2 also shortened PGE2 hyperalgesia compared with mice treated with the same dose of HSV-GFP (Figure 4B). This effect of GRK2 overexpression occurred even though ΨεRACK priming did not induce a detectable decrease in GRK2 protein in DRG neurons (Figure 2E).
Figure 4. Effect of HSV-mediated GRK2 overexpression on carrageenan- and ΨεRACK-induced hyperalgesic priming.
(A) Carrageenan-primed, (B) ΨεRACK-primed, or (C) naive control mice were inoculated intraplantarly with 2 injections of HSV-GRK2 or HSV-GFP (1.4 × 107 pfu/ml, 2.5 μl/paw) followed by PGE2 (100 ng/paw). Changes in 50% paw withdrawal threshold were monitored over time. Data represent mean ± SEM (n = 8 per group). **P < 0.01, #P < 0.001.
PGE2 hyperalgesia lasted about 8 hours in both HSV-GRK2– and HSV-GFP–treated mice that had not been exposed to carrageenan or ΨεRACK (Figure 4C), which indicates that in naive mice, GRK2 overexpression in sensory neurons does not affect the pain response.
Inoculation with HSV induced a transient and small increase in mechanical sensitivity that resolved within 1–2 days and was independent of the presence of GRK2 (Figure 4, A–C). Therefore, it is unlikely that this acute response to the virus contributed to the observed inhibition of the primed phenotype.
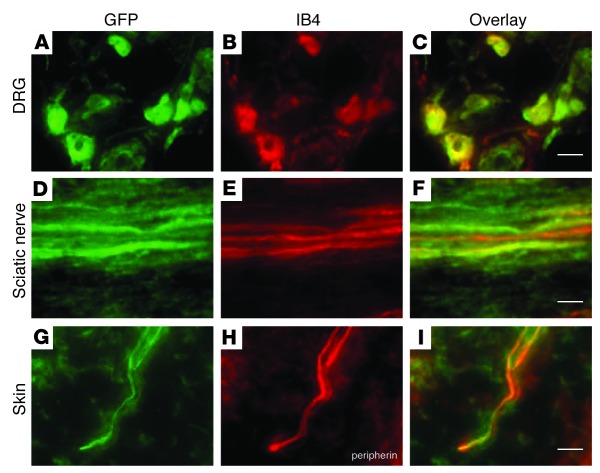
To confirm successful GRK2 gene transfer, we analyzed expression of the GFP reporter in lumbar DRG, sciatic nerve, and skin of the injected paw 3 days after the last HSV injection. GFP expression was clearly visible in both IB4+ and IB4– small-diameter DRG neurons and in both IB4+ and IB4– fibers in the sciatic nerve (Figure 5, A–F). GFP was also detected in peripherin+ nerves in the skin (Figure 5, G–I).
Figure 5. HSV-mediated overexpression of GRK2 and GFP.
Expression of GFP (A, D, and G), an indicator of successful transgene expression, was observed in IB4+ lumbar DRG neurons (B), IB4+ sciatic nerve fibers (E), and peripherin+ nerve endings (H) in the skin at 2 days after the last inoculation with HSV-GRK2 in primed mice. (C, F, and I) Merged images showing overlay. Scale bars: 20 μm.
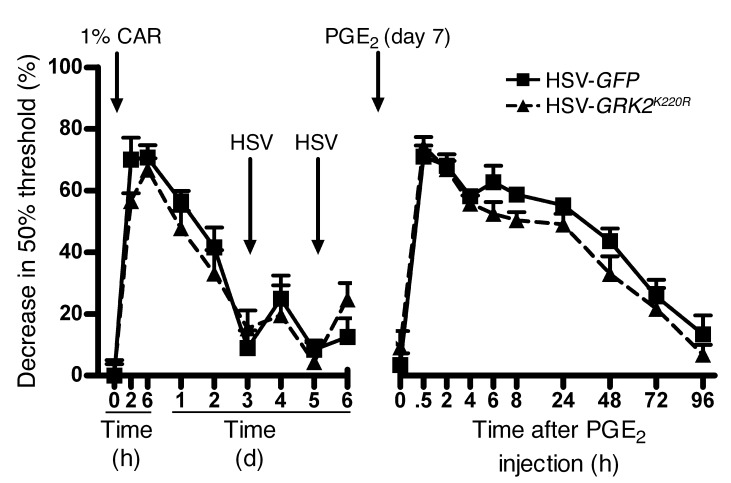
Next, we determined whether GRK2 kinase activity is required to prevent transition to chronic pain after priming, using an HSV construct expressing GRK2K220R, the kinase-dead mutant of GRK2 (35). GRK2K220R did not reverse the primed state (Figure 6). The course of PGE2 hyperalgesia in primed mice treated with HSV-GRK2K220R was similar to that of primed mice receiving control HSV-GFP inoculation.
Figure 6. Effect of overexpression of the GRK2 kinase-dead mutant, GRK2K220R, on carrageenan-induced hyperalgesic priming.
Carrageenan-primed mice were inoculated intraplantarly with 2 injections of HSV-GRK2K220R or HSV-GFP followed by PGE2 (100 ng/paw). Changes in 50% paw withdrawal threshold were monitored over time. Data represent mean ± SEM (n = 8 per group).
Collectively, our data indicate that, independently of whether priming decreased GRK2 or increased EPAC1 expression, HSV-mediated GRK2 overexpression was sufficient to reverse the primed state, thereby preventing the development of persistent hyperalgesia.
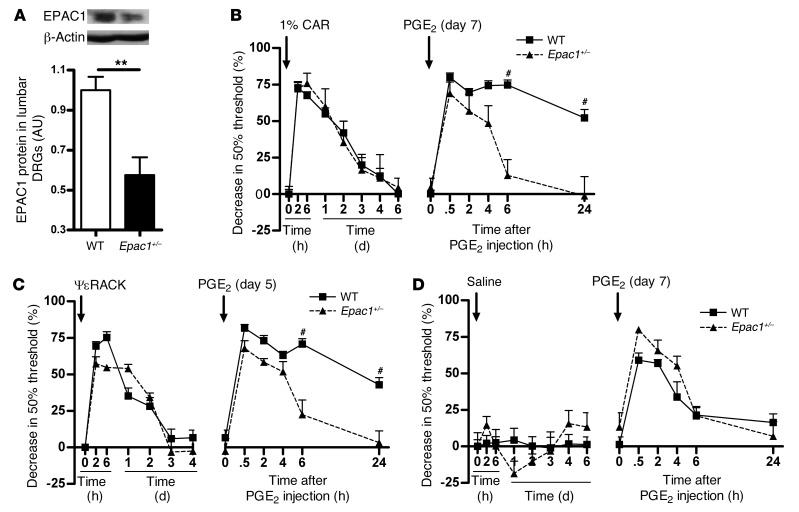
Hyperalgesic priming in Epac1+/– mice.
To further test our hypothesis that the GRK2/EPAC1 system regulates the transition to chronic hyperalgesia in primed mice, we used mice with heterozygous knockout of Epac1 (Epac1+/– mice; ref. 36). These mice had an approximately 50% reduction in EPAC1 protein in the DRG (Figure 7A). In response to carrageenan and ΨεRACK priming, Epac1+/– mice did not show the prolongation of PGE2 hyperalgesia observed in WT mice (Figure 7, B and C). The course of PGE2 hyperalgesia did not differ between Epac1+/– and WT mice that were not primed (Figure 7D).
Figure 7. Hyperalgesic priming in Epac1+/– mice.
(A) EPAC1 protein level, determined by Western blot analysis of DRG tissue homogenates from WT and Epac1+/– mice (n = 4 per group). (B) 7 days after carrageenan pretreatment (n = 4 per group), (C) 5 days after intraplantar ΨεRACK pretreatment (1 μg/paw in 5 μl saline; n = 6 per group), or (D) 7 days after saline pretreatment (n = 4 per group), mice received an intraplantar injection of PGE2 (100 ng/paw in 2.5 μl saline). Changes in 50% paw withdrawal threshold were monitored over time. Data represent mean ± SEM. **P < 0.01, #P < 0.001.
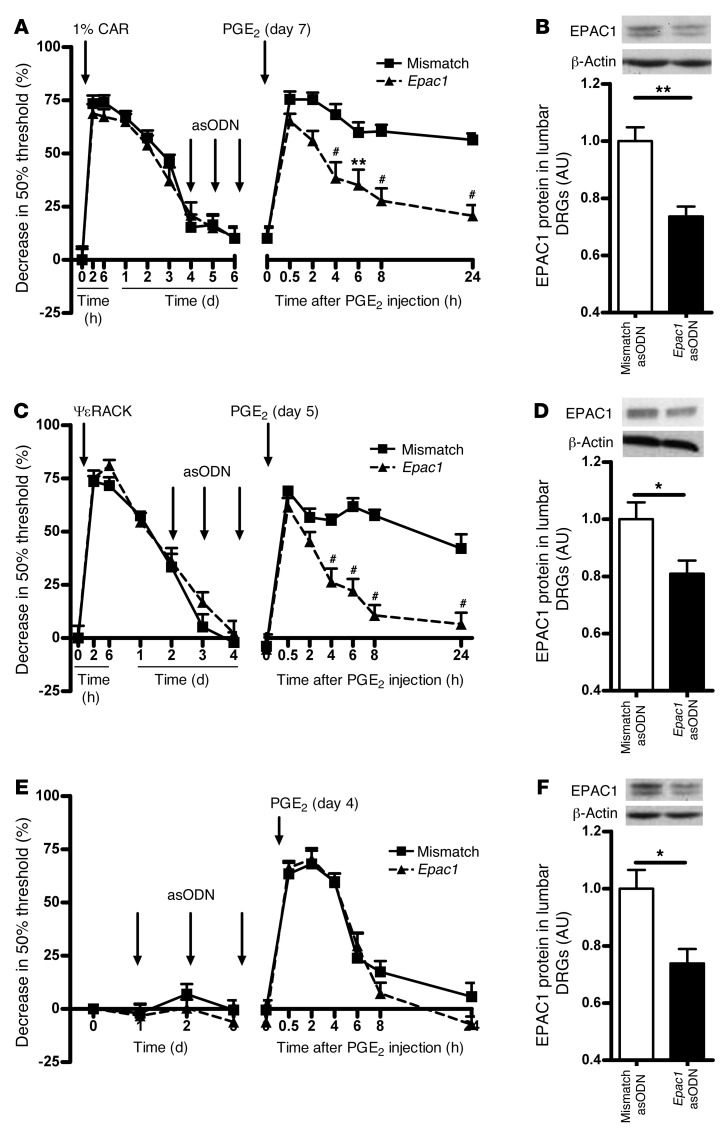
Effect of intrathecal Epac1 asODNs on hyperalgesic priming.
The results we obtained in Epac1+/– mice suggested that hyperalgesic priming can be prevented by lowering EPAC1 levels. We next tested whether the primed state can also be treated by temporarily downregulating EPAC1 protein levels in sensory neurons using intrathecal injection of Epac1 asODNs. Epac1 asODN treatment significantly reduced the duration of PGE2 hyperalgesia in mice primed with carrageenan or ΨεRACK (Figure 8, A and C). In lumbar DRG, protein levels of EPAC1 in carrageenan- and ΨεRACK-primed mice decreased significantly after intrathecal Epac1 asODN injection (Figure 8, B and D).
Figure 8. Effect of intrathecal Epac1 asODNs on carrageenan- and ΨεRACK-induced hyperalgesic priming.
3 days before intraplantar PGE2 injection (100 ng/paw, in 2.5 μl saline), mice primed with (A and B) carrageenan or (C and D) ΨεRACK or (E and F) naive mice received 3 daily intrathecal injections of Epac1 or mismatch control asODNs. (A, C, and E) Changes in 50% paw withdrawal threshold were monitored over time (n = 8 per group). (B, D, and F) EPAC1 levels were determined by Western blot 2 days after the last asODN treatment (n = 4 per group). Data represent mean ± SEM. *P < 0.05, **P < 0.01, #P < 0.001.
The Epac1 asODN–mediated decrease in EPAC1 protein levels did not change the baseline mechanical pain threshold or the duration and severity of acute PGE2 hyperalgesia in naive mice (Figure 8, E and F). Intrathecal administration of Epac1 asODNs did not affect the protein levels of EPAC2 (Supplemental Figure 5).
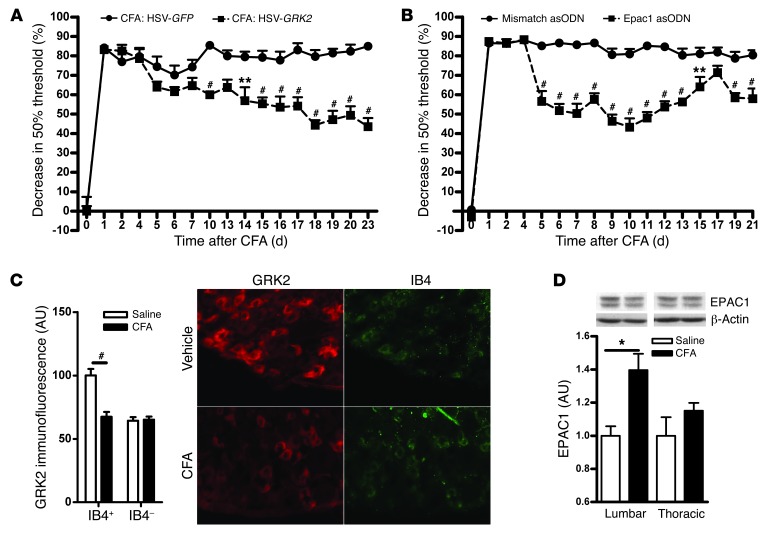
Effect of HSV-GRK2 or intrathecal Epac1 asODN in a model of chronic inflammatory pain.
To determine the broader relevance of the GRK2/EPAC1 system for chronic pain, we used the CFA model of chronic inflammatory pain. HSV-GRK2 treatment significantly attenuated the chronic mechanical hyperalgesia that developed in response to CFA (Figure 9A). Intrathecal administration of Epac1 asODNs also reduced the chronic CFA-induced mechanical hyperalgesia (Figure 9B). In CFA-treated mice, GRK2 levels in IB4+ DRG neurons were decreased at day 5 after CFA injection (Figure 9C). We did not detect changes in GRK2 protein by Western blot analysis (Supplemental Figure 6). Consistent with earlier studies (37), DRG EPAC1 levels were increased in CFA-treated mice (Figure 9D).
Figure 9. Effect of intraplantar HSV-GRK2 or intrathecal Epac1 asODNs on mechanical hyperalgesia in CFA-induced chronic inflammatory pain.
(A and B) Mice were treated (A) intraplantarly with HSV-GRK2 or HSV-GFP on days 4, 6, 13, and 16 after intraplantar CFA (n = 6 per group) or (B) intrathecally with Epac1 or mismatch asODNs on days 4, 5, 6, 8, and 10 after intraplantar CFA (n = 8 per group). Changes in 50% paw withdrawal threshold were monitored over time. (C) Lumbar DRG were collected on day 5 after intraplantar CFA or saline, and GRK2 protein levels in DRG neurons were analyzed as described in Figure 1. Scale bar: 50 μm. (D) EPAC1 protein levels in lumbar DRG were quantified by Western blotting at day 5 after intraplantar saline or CFA (n = 4 per group). Data represent mean ± SEM. *P < 0.05, **P < 0.01, #P < 0.001.
Discussion
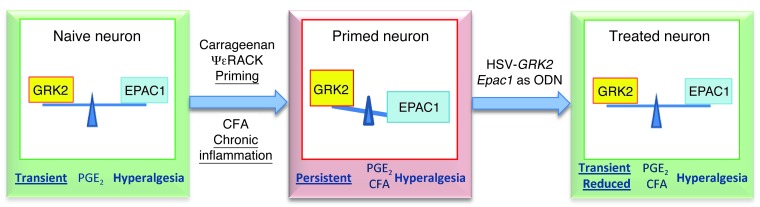
Although it is widely accepted that acute and chronic pain are different entities that depend on specific neurobiological pathways, knowledge about the underlying mechanisms remains limited. Here, we uncovered 2 key regulators of the development and maintenance of persistent pain in response to repeat or chronic inflammation: the kinase GRK2, and the cAMP sensor EPAC1. Specifically, using carrageenan and ΨεRACK priming as mouse models of the transition to persistent hyperalgesia, we showed that the prolongation of the hyperalgesic response in primed mice is associated with a sustained decrease in GRK2 level or increase in EPAC1 level in DRG (Figure 10). The functional importance of this observation is attested by our findings that increasing nociceptor GRK2 or decreasing EPAC1 prevented persistent hyperalgesia in primed mice. Notably, increasing GRK2 expression prevented the prolongation of PGE2 hyperalgesia in primed mice, regardless of whether GRK2 was decreased (after carrageenan priming) or EPAC1 was increased (after ΨεRACK priming). Similarly, downregulating EPAC1 inhibited the primed phenotype when GRK2 was decreased without a change in EPAC1 (in the carrageenan model), as well as when GRK2 was unchanged and EPAC1 was increased (in the ΨεRACK model). On the basis of these novel findings, we propose that an imbalance between the protein levels of GRK2 and EPAC1 is sufficient to cause the prolongation of hyperalgesia in primed mice. We also propose that reestablishing the GRK2/EPAC1 balance can be considered as a novel avenue for the prevention of persistent pain.
Figure 10. Schematic representation of our working model.
Decreased GRK2 in peripheral sensory neurons and/or increased EPAC1 promotes the development of persistent hyperalgesia. Treatment with intraplantar HSV-GRK2 or intrathecal Epac1 asODNs normalizes the GRK2/EPAC1 balance, leading to inhibition of persistent hyperalgesia.
Importantly, the role of GRK2 and EPAC1 is not restricted to persistent hyperalgesia in priming models. In the well-established model of CFA-induced chronic inflammatory pain, DRG GRK2 was increased and EPAC1 decreased. Moreover, increasing GRK2 or decreasing EPAC1 during ongoing inflammatory pain inhibited chronic CFA-induced hyperalgesia. This is important because it indicates that targeting GRK2/EPAC1 may both prevent chronic pain and combat existing chronic pain, such as that experienced by patients with painful inflammatory diseases like arthritis.
We confirmed earlier findings that DRG EPAC1 levels are increased in the CFA model of chronic inflammatory pain (37). In addition, we showed that the CFA model was associated with reduced GRK2 in IB4+ nociceptors. Interestingly, the mechanical hyperalgesia that develops in the CFA model was inhibited by increasing nociceptor GRK2 or by decreasing EPAC1 levels. DRG EPAC1 levels are also increased in the L5 spinal nerve transection model of chronic neuropathic pain in mice (38). In addition, nerve damage–induced mechanical hyperalgesia was significantly reduced in Epac1+/– and Epac1–/– mice (38). In vitro, EPAC1 signaling enhances Piezo2-mediated mechanotransduction in sensory neurons (38). Our findings demonstrated that EPAC1 is also a key to promoting mechanical hyperalgesia in primed mice as well as in a classic model of chronic inflammatory pain. Moreover, our findings indicate that decreased nociceptor GRK2 promotes persistent hyperalgesia in a priming model and contributes to chronic inflammatory pain. It remains to be determined whether HSV-GRK2–mediated overexpression of GRK2 also attenuates chronic neuropathic pain.
In naive animals, cAMP-inducing agents such as PGE2 and epinephrine induce hyperalgesia via the classic cAMP target PKA (17, 22, 25). However, in primed rats or in mice with genetically low levels of nociceptor GRK2, inhibition of PKA does not inhibit hyperalgesia induced by these agents. In primed rats or nociceptor GRK2–deficient mice, inhibition of PKCε or ERK prevents prolongation of 8-Br-cAMP, PGE2, or epinephrine hyperalgesia. These findings indicate that priming and Grk2 deficiency both promote ERK- and PKCε-mediated hyperalgesic signaling in response to cAMP-inducing agents (17, 22, 25). Levine and colleagues were the first to show that activation of the alternative cAMP sensor EPAC induces hyperalgesia via a PKCε-mediated pathway (20). Hyperalgesia induced by 8-pCPT is also prolonged in conditions of SNS-Grk2 deficiency (22). Moreover, in vitro, low GRK2 promotes 8-pCPT signaling to the EPAC target RAP1 and to ERK (22). On the basis of these earlier in vitro findings and our present in vivo findings, we hypothesize that the shift in the balance between GRK2 and EPAC1 levels in the DRG in primed mice and in mice with chronic inflammatory pain may promote EPAC1 signaling and persistent mechanical hyperalgesia. Consistently, hyperalgesia induced by 8-pCPT was prolonged after priming with carrageenan as well as ΨεRACK. Treatment of primed mice with HSV-GRK2K220R did not reverse the primed state, which indicates that GRK2 kinase activity is required for inhibiting pain signaling. Future studies should investigate whether GRK2 directly phosphorylates EPAC1 to inhibit EPAC1 activation and control the pain response.
Earlier studies have shown that activation of the mTOR pathway and protein translation in the periphery are required for development of IL-6– and carrageenan-induced priming of the subsequent response to PGE2 (10, 11, 17, 39). Axonal protein synthesis under the control of mTOR and ERK activation contribute to chronic pain in multiple other models as well (12–14). ERK activation also contributes to the prolonged PGE2 hyperalgesia in Grk2-deficient mice, and ERK activation by 8-pCPT is increased in Grk2-deficient cells (22). Notably, stimulation of prostate cancer cells with 8-pCPT activates the mTOR pathway (40, 41). Thus, it is conceivable that increased EPAC signaling promotes persistent pain via downstream activation of ERK and mTOR signaling pathways, leading to peripheral protein translation.
GRK2 protein is reduced in peripheral blood lymphocytes from humans with rheumatoid arthritis or multiple sclerosis (42, 43) and in splenocytes from rats with adjuvant arthritis or EAE (44, 45). In all these examples, the reduction in GRK2 was not associated with a change in Grk2 mRNA, which indicates that regulation takes place at the posttranslational level. The inflammation in rats with adjuvant arthritis spontaneously resolves approximately 30 days after induction. However, GRK2 levels in splenocytes were still reduced by 50% 2 weeks after resolution of inflammation (44). Similarly, we showed here that GRK2 levels in DRG neurons remained decreased even after resolution of the inflammation-induced hyperalgesia. Very little is known about regulation of the cellular level of EPAC1, and it remains to be determined via which mechanism the amount of GRK2 protein is kept at a lower level in IB4+ nociceptors or the DRG EPAC1 content is maintained at a higher level during the primed state.
Both in the carrageenan model of hyperalgesic priming and in the CFA model of chronic inflammatory pain, the reduction in GRK2 expression was restricted to small-diameter IB4+ sensory neurons. It is well known that specific sets of sensory neurons are involved in different pain modalities and, more importantly, different types of chronic pain (46–49). The IB4+ subset of DRG neurons specifically responds to inflammatory stimuli injected intraplantarly (46–49). Depletion of IB4+ neurons completely ablates the primed phenotype, which indicates that priming induces changes with functional consequences specifically for IB4+ neurons (32, 33). Moreover, selective changes occur in specific sets of neurons during inflammatory pain, including specific changes limited to IB4+ neurons (33, 50, 51). It remains to be determined, however, which mechanisms govern the decrease in GRK2 specifically in IB4+ small-diameter DRG neurons.
GRK2 was decreased in IB4+ DRG neurons in the carrageenan model of hyperalgesic priming as well as in the CFA model of chronic inflammatory pain that depends on Nav1.8+ nociceptors (52). After administration of HSV-GRK2, the GFP reporter protein was detected predominantly in IB4+ small-diameter neurons and in IB4+ nerve fibers in the sciatic nerve. This distribution of transgene expression after HSV-mediated gene transfer is consistent with earlier reports (53) and highlights HSV-mediated gene transfer as a specific tool by which to target small-diameter sensory neurons important in inflammatory pain processing. Nociceptor-specific targeting of GRK2 might prevent adverse effects in large-diameter neurons, likely leaving touch sensations unaffected (53). Indeed, mechanical sensitivity in naive mice, as determined using von Frey hairs, was unaffected by HSV-GRK2. Similarly, Grk2-deficient mice exhibit normal heat sensitivity under baseline conditions (21). Whether acute nociception of noxious stimuli such as mechanical pressure or heat is affected by changing EPAC1 levels remains to be determined.
HSV-GRK2 treatment shortened PGE2 hyperalgesia in primed mice and attenuated CFA-induced chronic hyperalgesia. These findings are consistent with our hypothesis that reduced GRK2 in IB4+ nociceptors is a key factor that contributes to priming and to chronic inflammatory pain. Unfortunately, the available EPAC1 antibodies did not allow reliable quantification of EPAC1 expression in DRG neurons by immunohistochemistry, and therefore we do not know in which DRG neurons EPAC1 levels were increased after priming. However, in situ hybridization analysis demonstrated that Epac1 mRNA was expressed in all cells in the DRG, including small-diameter neurons. We also showed that reducing DRG EPAC1 expression reversed the primed phenotype; this was the case even when DRG EPAC1 levels were not affected as GRK2 levels increased in small-diameter IB4+ neurons. Notably, expression of GRK2 using the HSV-GRK2 amplicon also inhibited the primed phenotype when GRK2 levels were not affected as EPAC1 levels were increased, for example, after ΨεRACK priming. Taken together, these findings support the hypothesis that a GRK2/EPAC1-dependent pathway in small-diameter nociceptors contributes to the primed phenotype. However, we cannot presently exclude that other, or additional, effects of changing GRK2 and EPAC1 levels in these and other cells ultimately are responsible for the observed inhibition of the primed phenotype when increasing GRK2 or decreasing EPAC1.
GRK2 and EPAC1 are widely expressed in both human and rodent tissues, including brain, heart, and thyroid gland, and are likely to regulate a wide array of physiological processes (18, 19, 54–58). Therefore, changes in the protein levels of GRK2 and EPAC1 in other tissues may have important consequences for cAMP signaling and (patho)physiology. This potentially widespread importance of GRK2/EPAC1 makes it unlikely that systemic treatments aimed at increasing GRK2 or decreasing EPAC1 will be of therapeutic benefit. The approach we used here, in which we locally administered HSV amplicons to overexpress GRK2 specifically in the area in which the increased pain response occurs, may be much more relevant. Another benefit of targeting the GRK2/EPAC system in sensory neurons is that by directly targeting intracellular signaling pathways involved in the transition to chronic pain, only the “pathological” transition to chronic pain is targeted, while evolutionary beneficial acute pain is not affected. Indeed, our data showed that increasing GRK2 in naive mice did not affect acute mechanical PGE2 hyperalgesia. In addition, acute carrageenan and ΨεRACK priming–induced hyperalgesia was unaffected in Epac1+/– mice.
The important question arises as to whether the priming phenomenon occurs in humans. A recent experimental study in humans showed that pre-exposure to a mild inflammatory stimulus (low-dose endotoxin) increased the hyperalgesic response to subsequent intradermal injection of capsaicin (59). Clinically, there is evidence that repeat surgery for recurring inguinal hernia increases the risk of chronic postoperative pain (9, 60, 61). In addition, gastrointestinal infection is a risk factor for irritable bowel disorder, a condition in which, for example, ingestion of food can induce a pain response (62). These observations indicate that in humans, previous exposure to tissue damage and/or inflammation may also sensitize (prime) the pain response to subsequent challenge, reminiscent of hyperalgesic priming. Increasing EPAC1 or decreasing GRK2 prevented the development of persistent hyperalgesia in mice primed by transient local inflammation. Therefore, we propose that targeting GRK2/EPAC1 prior to repeat surgery or in patients with irritable bowel disorder may help prevent or treat persistent pain in these situations that resemble hyperalgesic priming. Perhaps more importantly, we also showed that targeting GRK2/EPAC1 inhibited CFA-induced hyperalgesia, a model of persistent inflammatory pain. On the basis of these results, we propose that patients with chronic pain associated with chronic inflammation (e.g., arthritic pain) could benefit from therapies targeting GRK2/EPAC1. This may be especially relevant for patients that continue to experience pain after apparently successful reduction of joint inflammation in response to treatment (63, 64). Preclinical studies should be performed to further examine these possibilities.
Local application of HSV is regarded as an ideal platform for novel therapies of chronic pain because HSV has a natural ability to infect the sensory nerve via peripheral inoculation. With a single inoculation, the virus may provide long-term therapy in restricted appropriate regions of the body (65, 66). Recently, results from a phase I clinical trial using a similar replication-deficient HSV amplicon to overexpress preproenkephalin reported no adverse effects in patients (67). Notably, a recent study in rats indicates that HSV amplicons can also be used for the targeted delivery of asODNs (68), and thus would provide a tool to locally reduce EPAC1 expression as well. These and our present findings clearly indicate that it may ultimately be feasible to use a similar approach in humans to deliver GRK2 by local administration of HSV-GRK2 or EPAC1 antisense DNA in humans to prevent and treat chronic pain.
Methods
Animals.
Female C57BL/6 mice as well as Epac1+/– (36) and littermate WT mice aged 12–14 weeks were used. All experiments were performed in a blinded setup.
Mechanical hyperalgesia.
Before experiments, mice were exposed to the equipment without any nociceptive stimulation for 1–2 h/d for 2 days. On day 3, mice were placed in the test environment 15–20 minutes before testing. Baseline responses were determined on 3 different days using von Frey hairs, and the 50% paw withdrawal threshold was calculated using the up-and-down method (25, 69). In brief, animals were placed on a wire grid bottom through which the von Frey hairs were applied (bending force range, 0.02–1.4 g, starting with 0.16 g; Stoelting). The hair force was increased or decreased according to the response. Clear paw withdrawal, shaking, or licking were considered as nociceptive-like responses. Ambulation was considered an ambiguous response, and the stimulus was repeated in such cases.
Hyperalgesic priming and CFA models.
To induce hyperalgesic priming, 5 μl carrageenan (1% in saline; Sigma-Aldrich) or 5 μl ΨεRACK (1 μg in saline; obtained from the W.M. Keck Facility of Yale University) (15) was intraplantarly injected into the hind paw. Control mice received 5 μl saline.
3–14 days later, mice received an intraplantar injection of 2.5 μl PGE2 (40 μg/ml; Sigma-Aldrich), epinephrine (4 μg/ml; Sigma-Aldrich), 8-pCPT (5.04 μg/ml; Biolog LifeScience Institute), or 5 μl recombinant mouse IL-1β (200 ng/ml; R&D Systems) per paw. For the CFA model, 20 μl CFA (Sigma-Aldrich) was injected intraplantarly.
Immunohistochemical staining of GRK2.
Mice were deeply anesthetized with sodium pentobarbital (50 mg/kg i.p.) and transcardially perfused with PBS followed by 4% paraformaldehyde, after which DRG (lumbar [L3–L5] and thoracic [T6–T10]) and sciatic nerves were collected. Tissues were postfixed, cryoprotected in sucrose, embedded in OCT compound, and frozen at –80°C. Frozen sections of DRG and sciatic nerve (10 μm) were stained with biotinylated IB4 (10 μg/ml; Vector Laboratories) and rabbit anti-GRK2 (1:100; Santa Cruz Biotechnology). Primary anti-GRK2 antibody blocked with a GRK2 blocking peptide (Santa Cruz Biotechnology) was used as a control. Staining was visualized with Alexa Fluor 488–conjugated streptavidin (1:200; Invitrogen) and Alexa Fluor 594–conjugated goat anti-rabbit antibody (1:200; Invitrogen) and photographed with an EVOS fl (AMG Life Technologies) using identical exposure times for all slides. GRK2 levels in IB4+ and IB4– small-diameter DRG neurons (<23 μm diameter; ref. 70) and in sciatic nerve fibers were analyzed with NIH ImageJ.
The average background fluorescence for specific subsets of DRG neurons or sciatic nerves (primary GRK2 antibody plus GRK2 blocking peptide) were subtracted before calculation of the percent change in GRK2 staining. Stainings were done in parallel for samples from carrageenan-, ΨεRACK-, or CFA-treated mice and their respective saline-treated controls.
Western blotting.
Lumbar and thoracic DRG were frozen in liquid nitrogen and homogenized in ice-cold 50 mM Tris-HCl (pH 8), 5 mM EDTA, 150 mM NaCl, 1% NP-40, 0.5% deoxycholic acid, 0.1% SDS containing protease inhibitor mix (Sigma-Aldrich), 100 mM PMSF, 10 mM β-glycerolphosphate, 1 mM NaVO3, and 20 mM NaF.
Proteins were separated by 7.5% SDS-PAGE and transferred to polyvinylidene difluoride membranes (Millipore). Blots were stained with mouse anti-EPAC1 (Cell Signaling Technology), mouse anti-EPAC2 (Cell Signaling Technology), and goat anti-actin (Santa Cruz Biotechnology) followed by peroxidase-conjugated goat anti-mouse IgG plus IgM (heavy and light chain) (Jackson Immunoresearch) or peroxidase-conjugated donkey anti-goat IgG (Santa Cruz Biotechnology) and developed by enhanced chemiluminescence (GE Healthcare). Band density was determined using a GS-700 Imaging Densitometer (Bio-Rad).
HSV-mediated GRK2 and GFP gene expression.
We generated a bicistronic HSV construct into which we cloned bovine GRK2 or GRK2K220R under control of the α4 promotor and in which GFP expression is driven by the α22 promoter (34). Both are immediate early gene promoters and have similar kinetics of expression, so the reporter can reliably be used as an indicator of transgene expression (71, 72). Control HSV-GFP contains GFP under control of the α22 promoter only. Mice were inoculated intraplantarly twice with 2.5 μl of 1.4 × 107 pfu/ml. To control for GRK2 and/or GFP expression, the unfixed skin of hind paws was isolated and frozen at day 3 after the last inoculation. In addition, fixed DRG and sciatic nerve tissues were prepared as described above.
Frozen sections of skin (14 μm) were fixed in acetone and stained with rabbit anti-GFP (1:100; GeneTex) for 60 hours and overnight at 4°C. Frozen sections of skin, DRG and sciatic nerve (10 μm) were incubated with rabbit anti-GFP (1:100; GeneTex) for 60 hours. Skin was stained with mouse anti-peripherin (1:100; Sigma-Aldrich); DRG and sciatic nerve was stained with IB4 (10 μg/ml; Vector Laboratories). We used Alexa Fluor 594–conjugated streptavidin (Invitrogen) and Alexa Fluor 488–conjugated donkey anti-rabbit antibody (Invitrogen) in the second step.
Epac1 and mismatch asODNs.
The Epac1 asODN sequence (5′-AACTCTCCACCCTCTCCCA-3′) is directed against a unique sequence of mouse Epac1 mRNA; mismatch asODN (5′-ACATTCCACCCTCCTCCAC-3′) was used as a control. 10 μg Epac1 asODNs or mismatch asODNs in 5 μl saline were injected intrathecally between the fifth and sixth lumbar vertebrate under isoflurane anesthesia.
In situ hybridization.
In situ hybridization for Epac1 mRNA was performed on paraformaldehyde-fixed, paraffin-embedded tissue sections (4 μm). Sections were digested with 2 μg/ml proteinase K (Exiqon) for 5 minutes at room temperature and loaded onto Ventana Discovery Ultra for in situ hybridization analysis. Slides were incubated with double digoxigenin–labeled mercury LNA RNA probe specific for Epac1 (5DigN/TGGAGCGGTATGAGTGTGAGT/3DigN; Exiqon) for 2 hours at 50°C. Slides were developed using a polyclonal anti-digoxegenin antibody and alkaline phosphatase–conjugated secondary antibody (Ventana) with NBT-BCIP as the substrate. A double digoxigenin–labeled probe specific for U6 small nuclear RNA (Exiqon) was used as positive control, and a double digoxigenin–labeled negative control probe (catalog no. 99004-15; Exiqon) was used as a negative control.
Statistics.
Data are expressed as mean ± SEM. Statistical analysis was carried out using 2-tailed Student’s t test or 2-way ANOVA followed by Bonferroni analysis. A P value less than 0.05 was considered significant.
Study approval.
Mice were maintained in the animal facility of the University of Utrecht. All experiments were performed in accordance with international guidelines and approved by the University Medical Center Utrecht experimental animal committee.
Supplementary Material
Acknowledgments
The authors are indebted to Robert Sapolsky (Stanford University and Stanford University School of Medicine, Stanford, California, USA) for contributing to preparation of the HSV construct and scientific editor Jeanie F. Woodruff for expert editorial assistance. Research reported here was supported by the National Institute of Neurological Diseases and Stroke, NIH (award nos. RO1NS073939 and RO1NS074999). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This research was also supported by a STARS grant of the University of Texas System to A. Kavelaars.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2013;123(12):5023–5034. doi:10.1172/JCI66241.
References
- 1.Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. National Research Council. Washington, DC, USA: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Stein C, et al. Peripheral mechanisms of pain and analgesia. Brain Res Rev. 2009;60(1):90–113. doi: 10.1016/j.brainresrev.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gold MS, Gebhart GF. Nociceptor sensitization in pain pathogenesis. Nat Med. 2010;16(11):1248–1257. doi: 10.1038/nm.2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139(2):267–284. doi: 10.1016/j.cell.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woolf CJ. What is this thing called pain? J Clin Invest. 2010;120(11):3742–3744. doi: 10.1172/JCI45178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marchand F, Perretti M, McMahon SB. Role of the immune system in chronic pain. Nat Rev Neurosci. 2005;6(7):521–532. doi: 10.1038/nrn1700. [DOI] [PubMed] [Google Scholar]
- 8.Wallace MS, Irving G, Cowles VE. Gabapentin extended-release tablets for the treatment of patients with postherpetic neuralgia: a randomized, double-blind, placebo-controlled, multicentre study. Clin Drug Investig. 2010;30(11):765–776. doi: 10.2165/11539520-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005;95(1):69–76. doi: 10.1093/bja/aei019. [DOI] [PubMed] [Google Scholar]
- 10.Asiedu MN, et al. Spinal protein kinase M zeta underlies the maintenance mechanism of persistent nociceptive sensitization. J Neurosci. 2011;31(18):6646–6653. doi: 10.1523/JNEUROSCI.6286-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melemedjian OK, et al. IL-6- and NGF-induced rapid control of protein synthesis and nociceptive plasticity via convergent signaling to the eIF4F complex. J Neurosci. 2010;30(45):15113–15123. doi: 10.1523/JNEUROSCI.3947-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geranton SM, et al. A rapamycin-sensitive signaling pathway is essential for the full expression of persistent pain states. J Neurosci. 2009;29(47):15017–15027. doi: 10.1523/JNEUROSCI.3451-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jimenez-Diaz L, et al. Local translation in primary afferent fibers regulates nociception. PLoS One. 2008;3(4):e1961. doi: 10.1371/journal.pone.0001961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obara I, Geranton SM, Hunt SP. Axonal protein synthesis: a potential target for pain relief? Curr Opin Pharmacol. 2012;12(1):42–48. doi: 10.1016/j.coph.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Aley KO, Messing RO, Mochly-Rosen D, Levine JD. Chronic hypersensitivity for inflammatory nociceptor sensitization mediated by the epsilon isozyme of protein kinase C. J Neurosci. 2000;20(12):4680–4685. doi: 10.1523/JNEUROSCI.20-12-04680.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph EK, Parada CA, Levine JD. Hyperalgesic priming in the rat demonstrates marked sexual dimorphism. Pain. 2003;105(1–2):143–150. doi: 10.1016/S0304-3959(03)00175-1. [DOI] [PubMed] [Google Scholar]
- 17.Reichling DB, Levine JD. Critical role of nociceptor plasticity in chronic pain. Trends Neurosci. 2009;32(12):611–618. doi: 10.1016/j.tins.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gloerich M, Bos JL. Epac: defining a new mechanism for cAMP action. Annu Rev Pharmacol Toxicol. 2010;50:355–375. doi: 10.1146/annurev.pharmtox.010909.105714. [DOI] [PubMed] [Google Scholar]
- 19.Kawasaki H, et al. A family of cAMP-binding proteins that directly activate Rap1. Science. 1998;282(5397):2275–2279. doi: 10.1126/science.282.5397.2275. [DOI] [PubMed] [Google Scholar]
- 20.Hucho TB, Dina OA, Levine JD. Epac mediates a cAMP-to-PKC signaling in inflammatory pain: an isolectin B4(+) neuron-specific mechanism. J Neurosci. 2005;25(26):6119–6126. doi: 10.1523/JNEUROSCI.0285-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eijkelkamp N, et al. GRK2: a novel cell-specific regulator of severity and duration of inflammatory pain. J Neurosci. 2010;30(6):2138–2149. doi: 10.1523/JNEUROSCI.5752-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eijkelkamp N, et al. Low nociceptor GRK2 prolongs prostaglandin E2 hyperalgesia via biased cAMP signaling to Epac/Rap1, protein kinase Cepsilon, and MEK/ERK. J Neurosci. 2010;30(38):12806–12815. doi: 10.1523/JNEUROSCI.3142-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kavelaars A, Eijkelkamp N, Willemen HL, Wang H, Carbajal AG, Heijnen CJ. Microglial GRK2: a novel regulator of transition from acute to chronic pain. Brain Behav Immun. 2011;25(6):1055–1060. doi: 10.1016/j.bbi.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 24.Kleibeuker W, et al. A role for G protein-coupled receptor kinase 2 in mechanical allodynia. Eur J Neurosci. 2007;25(6):1696–1704. doi: 10.1111/j.1460-9568.2007.05423.x. [DOI] [PubMed] [Google Scholar]
- 25.Wang H, et al. GRK2 in sensory neurons regulates epinephrine-induced signalling and duration of mechanical hyperalgesia. Pain. 2011;152(7):1649–1658. doi: 10.1016/j.pain.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 26.Willemen HL, et al. Microglial/macrophage GRK2 determines duration of peripheral IL-1beta-induced hyperalgesia: contribution of spinal cord CX3CR1, p38 and IL-1 signaling. Pain. 2010;150(3):550–560. doi: 10.1016/j.pain.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Willemen HL, Huo XJ, Mao-Ying QL, Zijlstra J, Heijnen CJ, Kavelaars A. MicroRNA-124 as a novel treatment for persistent hyperalgesia. J Neuroinflammation. 2012;9:143. doi: 10.1186/1742-2094-9-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evron T, Daigle TL, Caron MG. GRK2: multiple roles beyond G protein-coupled receptor desensitization. Trends Pharmacol Sci. 2012;33(3):154–164. doi: 10.1016/j.tips.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jimenez-Sainz MC, et al. G protein-coupled receptor kinase 2 negatively regulates chemokine signaling at a level downstream from G protein subunits. Mol Biol Cell. 2006;17(1):25–31. doi: 10.1091/mbc.E05-05-0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peregrin S, et al. Phosphorylation of p38 by GRK2 at the docking groove unveils a novel mechanism for inactivating p38MAPK. Curr Biol. 2006;16(20):2042–2047. doi: 10.1016/j.cub.2006.08.083. [DOI] [PubMed] [Google Scholar]
- 31.Ferrari LF, Bogen O, Alessandri-Haber N, Levine E, Gear RW, Levine JD. Transient decrease in nociceptor GRK2 expression produces long-term enhancement in inflammatory pain. Neuroscience. 2012;222:392–403. doi: 10.1016/j.neuroscience.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferrari LF, Bogen O, Levine JD. Nociceptor subpopulations involved in hyperalgesic priming. Neuroscience. 2010;165(3):896–901. doi: 10.1016/j.neuroscience.2009.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joseph EK, Levine JD. Hyperalgesic priming is restricted to isolectin B4-positive nociceptors. Neuroscience. 2010;169(1):431–435. doi: 10.1016/j.neuroscience.2010.04.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao H, Yenari MA, Sapolsky RM, Steinberg GK. Mild postischemic hypothermia prolongs the time window for gene therapy by inhibiting cytochrome C release. Stroke. 2004;35(2):572–577. doi: 10.1161/01.STR.0000110787.42083.58. [DOI] [PubMed] [Google Scholar]
- 35.Sallese M, Mariggio S, D’Urbano E, Iacovelli L, De Blasi A. Selective regulation of Gq signaling by G protein-coupled receptor kinase 2: direct interaction of kinase N terminus with activated galphaq. Mol Pharmacol. 2000;57(4):826–831. [PubMed] [Google Scholar]
- 36.Suzuki S, et al. Differential roles of Epac in regulating cell death in neuronal and myocardial cells. J Biol Chem. 2010;285(31):24248–24259. doi: 10.1074/jbc.M109.094581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang C, Gu Y, Li GW, Huang LY. A critical role of the cAMP sensor Epac in switching protein kinase signalling in prostaglandin E2-induced potentiation of P2X3 receptor currents in inflamed rats. J Physiol. 2007;584(pt 1):191–203. doi: 10.1113/jphysiol.2007.135616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eijkelkamp N, et al. A role for Piezo2 in EPAC1-dependent mechanical allodynia. Nat Commun. 2013;4:1682. doi: 10.1038/ncomms2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferrari LF, Bogen O, Chu C, Levine JD. Peripheral administration of translation inhibitors reverses increased hyperalgesia in a model of chronic pain in the rat. J Pain. 2013;14(7):731–738. doi: 10.1016/j.jpain.2013.01.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Misra UK, Pizzo SV. Upregulation of mTORC2 activation by the selective agonist of EPAC, 8-CPT-2Me-cAMP, in prostate cancer cells: assembly of a multiprotein signaling complex. J Cell Biochem. 2012;113(5):1488–1500. doi: 10.1002/jcb.24018. [DOI] [PubMed] [Google Scholar]
- 41.Misra UK, Pizzo SV. Epac1-induced cellular proliferation in prostate cancer cells is mediated by B-Raf/ERK and mTOR signaling cascades. J Cell Biochem. 2009;108(4):998–1011. doi: 10.1002/jcb.22333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lombardi MS, et al. Decreased expression and activity of G-protein-coupled receptor kinases in peripheral blood mononuclear cells of patients with rheumatoid arthritis. FASEB J. 1999;13(6):715–725. doi: 10.1096/fasebj.13.6.715. [DOI] [PubMed] [Google Scholar]
- 43.Vroon A, et al. G protein-coupled receptor kinase 2 in multiple sclerosis and experimental autoimmune encephalomyelitis. J Immunol. 2005;174(7):4400–4406. doi: 10.4049/jimmunol.174.7.4400. [DOI] [PubMed] [Google Scholar]
- 44.Lombardi MS, Kavelaars A, Cobelens PM, Schmidt RE, Schedlowski M, Heijnen CJ. Adjuvant arthritis induces down-regulation of G protein-coupled receptor kinases in the immune system. J Immunol. 2001;166(3):1635–1640. doi: 10.4049/jimmunol.166.3.1635. [DOI] [PubMed] [Google Scholar]
- 45.Vroon A, Lombardi MS, Kavelaars A, Heijnen CJ. Changes in the G-protein-coupled receptor desensitization machinery during relapsing-progressive experimental allergic encephalomyelitis. J Neuroimmunol. 2003;137(1–2):79–86. doi: 10.1016/S0165-5728(03)00050-X. [DOI] [PubMed] [Google Scholar]
- 46.Gerke MB, Plenderleith MB. Binding sites for the plant lectin Bandeiraea simplicifolia I-isolectin B(4) are expressed by nociceptive primary sensory neurones. Brain Res. 2001;911(1):101–104. doi: 10.1016/S0006-8993(01)02750-0. [DOI] [PubMed] [Google Scholar]
- 47.Lagerstrom MC, et al. A sensory subpopulation depends on vesicular glutamate transporter 2 for mechanical pain, and together with substance P, inflammatory pain. Proc Natl Acad Sci U S A. 2011;108(14):5789–5794. doi: 10.1073/pnas.1013602108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Minett MS, et al. Distinct Nav1.7-dependent pain sensations require different sets of sensory and sympathetic neurons. Nat Commun. 2012;3:791. doi: 10.1038/ncomms1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wood JN, Eijkelkamp N. Noxious mechanosensation — molecules and circuits. Curr Opin Pharmacol. 2012;12(1):4–8. doi: 10.1016/j.coph.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 50.Breese NM, George AC, Pauers LE, Stucky CL. Peripheral inflammation selectively increases TRPV1 function in IB4-positive sensory neurons from adult mouse. Pain. 2005;115(1–2):37–49. doi: 10.1016/j.pain.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 51.Stemkowski PL, Smith PA. Long-term IL-1beta exposure causes subpopulation-dependent alterations in rat dorsal root ganglion neuron excitability. J Neurophysiol. 2012;107(6):1586–1597. doi: 10.1152/jn.00587.2011. [DOI] [PubMed] [Google Scholar]
- 52.Abrahamsen B, et al. The cell and molecular basis of mechanical, cold, and inflammatory pain. Science. 2008;321(5889):702–705. doi: 10.1126/science.1156916. [DOI] [PubMed] [Google Scholar]
- 53.Henken DB, Martin JR. Herpes simplex virus infection in populations of mouse dorsal root ganglion neurons: effects of inoculation route and virus strain. J Neurol Sci. 1991;105(1):29–36. doi: 10.1016/0022-510X(91)90114-M. [DOI] [PubMed] [Google Scholar]
- 54.Chuang TT, Sallese M, Ambrosini G, Parruti G, De Blasi A. High expression of beta-adrenergic receptor kinase in human peripheral blood leukocytes. Isoproterenol and platelet activating factor can induce kinase translocation. J Biol Chem. 1992;267(10):6886–6892. [PubMed] [Google Scholar]
- 55.Grange-Midroit M, Garcia-Sevilla JA, Ferrer-Alcon M, La Harpe R, Walzer C, Guimon J. G protein-coupled receptor kinases, beta-arrestin-2 and associated regulatory proteins in the human brain: postmortem changes, effect of age and subcellular distribution. Brain Res Mol Brain Res. 2002;101(1–2):39–51. doi: 10.1016/S0169-328X(02)00144-4. [DOI] [PubMed] [Google Scholar]
- 56.Monto F, et al. Different expression of adrenoceptors and GRKs in the human myocardium depends on heart failure etiology and correlates to clinical variables. Am J Physiol Heart Circ Physiol. 2012;303(3):H368–H376. doi: 10.1152/ajpheart.01061.2011. [DOI] [PubMed] [Google Scholar]
- 57.Harris DM, Cohn HI, Pesant S, Eckhart AD. GPCR signalling in hypertension: role of GRKs. Clin Sci (Lond). 2008;115(3):79–89. doi: 10.1042/CS20070442. [DOI] [PubMed] [Google Scholar]
- 58.Premont RT, Gainetdinov RR. Physiological roles of G protein-coupled receptor kinases and arrestins. Annu Rev Physiol. 2007;69:511–534. doi: 10.1146/annurev.physiol.69.022405.154731. [DOI] [PubMed] [Google Scholar]
- 59.Hutchinson MR, et al. Low-dose endotoxin potentiates capsaicin-induced pain in man: evidence for a pain neuroimmune connection. Brain Behav Immun. 2013;30:3–11. doi: 10.1016/j.bbi.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 60.Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg. 2001;88(8):1122–1126. doi: 10.1046/j.0007-1323.2001.01828.x. [DOI] [PubMed] [Google Scholar]
- 61.Callesen T, Bech K, Kehlet H. Prospective study of chronic pain after groin hernia repair. Br J Surg. 1999;86(12):1528–1531. doi: 10.1046/j.1365-2168.1999.01320.x. [DOI] [PubMed] [Google Scholar]
- 62.Dai C, Jiang M. The incidence and risk factors of post-infectious irritable bowel syndrome: a meta-analysis. Hepatogastroenterology. 2012;59(113):67–72. doi: 10.5754/hge10796. [DOI] [PubMed] [Google Scholar]
- 63.Lomholt JJ, Thastum M, Herlin T. Pain experience in children with juvenile idiopathic arthritis treated with anti-TNF agents compared to non-biologic standard treatment. Pediatr Rheumatol Online J. 2013;11(1):21. doi: 10.1186/1546-0096-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kimura Y, Walco GA. Treatment of chronic pain in pediatric rheumatic disease. Nat Clin Pract Rheumatol. 2007;3(4):210–218. doi: 10.1038/ncprheum0458. [DOI] [PubMed] [Google Scholar]
- 65.Wolfe D, Mata M, Fink DJ. Targeted drug delivery to the peripheral nervous system using gene therapy. Neurosci Lett. 2012;527(2):85–89. doi: 10.1016/j.neulet.2012.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Goins WF, Cohen JB, Glorioso JC. Gene therapy for the treatment of chronic peripheral nervous system pain. Neurobiol Dis. 2012;48(2):255–270. doi: 10.1016/j.nbd.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fink DJ, et al. Gene therapy for pain: results of a phase I clinical trial. Ann Neurol. 2011;70(2):207–212. doi: 10.1002/ana.22446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cheli VT, et al. Gene transfer of NMDAR1 subunit sequences to the rat CNS using herpes simplex virus vectors interfered with habituation. Cell Mol Neurobiol. 2002;22(3):303–314. doi: 10.1023/A:1020720001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53(1):55–63. doi: 10.1016/0165-0270(94)90144-9. [DOI] [PubMed] [Google Scholar]
- 70.Fang X, et al. Intense isolectin-B4 binding in rat dorsal root ganglion neurons distinguishes C-fiber nociceptors with broad action potentials and high Nav1.9 expression. J Neurosci. 2006;26(27):7281–7292. doi: 10.1523/JNEUROSCI.1072-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fink SL, Chang LK, Ho DY, Sapolsky RM. Defective herpes simplex virus vectors expressing the rat brain stress-inducible heat shock protein 72 protect cultured neurons from severe heat shock. J Neurochem. 1997;68(3):961–969. doi: 10.1046/j.1471-4159.1997.68030961.x. [DOI] [PubMed] [Google Scholar]
- 72.Yenari MA, et al. Gene therapy with HSP72 is neuroprotective in rat models of stroke and epilepsy. Ann Neurol. 1998;44(4):584–591. doi: 10.1002/ana.410440403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.