Results of the study suggest that direct optical entry technique reduced entry time and blood loss with trends to slightly decrease the occurrence of minor vascular and bowel injuries in obese women.
Keywords: Complications, Direct optical access, Direct trocar insertion, Laparoscopic entry, Laparoscopy, Obesity, Open Hasson technique, Pneumoperitoneum, Veress needle
Abstract
Background:
Recently, we have shown advantages of a direct optical entry (DOE) using a bladeless trocar in comparison with the open Hasson technique (OHT) in older reproductive-age women with previous operations, as well as in comparison with Veress needle entry in reproductive-age and postmenopausal women.
Objectives:
A prospective multicenter randomized study to determine whether the DOE is feasible for establishing safe and rapid entry into the abdomen in comparison with those of the OHT in reproductive-age obese women.
Methods:
Two types of surgical techniques were blindly applied in 224 obese reproductive-age women with benign neoplastic diseases of ovary and uterus. Namely, laparoscopic entry into the abdomen in 108 patients was performed by DOE and in 116 women by OHT. Following parameters (entry time in seconds needed to establish the intra-abdominal vision after pneumoperitoneum, blood loss, occurrence of vascular and/or bowel injuries) were compared during surgery as main outcomes.
Results:
Main baseline characteristics of patients, including age (36.1 ± 4.5 vs 35.7 ± 5.8), body mass index (34.9 ± 5.1 vs 35.1 ± 4.9 kg/m2), and parity (2.1 ± 0.4 vs 1.9 ± 0.9), were not significantly different between the DOE and OHT groups (P > .05). While intraoperative parameters such as the entry time (71.9 ± 3.7 vs 215.1 ± 6.2 seconds) and blood loss value (9.7 ± 6.1 vs 12.2 ± 2.9 mL) were significantly reduced in the DOE group in comparison with those of OHT group (respectively, P < .0001 and < .01), there were also trends to slight decrease of the occurrence of the minor injuries, manifested as omental small vessels rupture (0 of 108 vs 4 of 116) and punctures and pinches of jejunal serosa (0 of 108 vs 3 of 116) in patients of the DOE group in comparison with those of OHT group (respectively, P = .0515 and = .0925).
Conclusions:
DOE reduced entry time and blood loss with trends to slightly decrease of the occurrence of the minor vascular and bowel injuries, thus enabling a possible alternative to OHT in obese women; however, further larger trials need to confirm the possible additional benefits of a DOE.
INTRODUCTION
Fifty percent of complications are associated with laparoscopy due to the abdominal entry.1 There is a concern that rare but life-threatening complications can occur, including severe bleeding due to damages of major abdominal vessels, as well as other injuries related to bowel and bladder trauma, subcutaneous emphysema, and postsurgical infections.1,2 A consensus concerning the optimal laparoscopy entry technique does not exist; therefore, surgeons have applied a wide spectrum of instruments and have developed different entry techniques. Of the techniques currently being used, none has been identified as being safe enough to prevent complications associated with laparoscopic entry.3
This potential for complications is seemingly infinite in obese patients with a body mass index (BMI) >30 kg/m2. Difficulties of entry into the abdomen in obese patients are associated with the expanded thick fatty layer of the abdominal wall, especially with translocation of the umbilicus, which is more caudal to the normal umbilical site and just below the aortic bifurcation.4,5 Therefore, manipulations during entry with grasping the abdominal wall are difficult because of abdominal wall thickness as well as a large-vessel trauma timidity.
Over the years, we have been researching abdominal entry with comparative studies of direct optical entry (DOE) using a bladeless trocar versus a blind closed access by Veress needle entry (VNE) in young women without previous surgery,6 in postmenopausal women,7 as well as comparison of DOE with open laparoscopy by open Hasson technique (OHT) in women with previous abdominopelvic surgery.8
A significantly reduced DOE abdominal entry time in seconds has been demonstrated in 93 women compared with that of VNE in 101 patients (62.8 ± 7.5 vs 180.4 ± 11.8 seconds) of the same age-groups (26.4 ± 5.8 vs 27.3 ± 6.0 years) with the absence of any considerable differences in main intraoperative parameters of entry, such as blood loss and occurrence of vascular and/or bowel injury, between these techniques, independently of BMI sizeable values (24.8 ± 2.8 vs 25.1 ± 4.9 kg/m2), between patients of these 2 groups.6 Likewise in postmenopausal women, time for abdominal entry was significantly reduced in the DOA group (65.7 ± 11.9 vs 192.8 ± 5.6 seconds) compared with that of the VNE group in the absence of significant differences concerning blood loss value (8.4 ± 7.2 vs 9.3 ± 5.5 mL) and minor vascular (1 of 89 vs 3 of 97) and major vascular as well as minor bowel injuries.7
Furthermore, a comparative study of DOE with OHT was fulfilled in women with previous abdominopelvic surgery with the same age-groups (42.3 ± 2.5 vs 41.8 ± 3.3 years), BMI values (28.3 ± 6.2 vs 27.9 ± 5.9 kg/m2), and parity (2.3 ± 0.7 vs 2.1 ± 0.9). It was shown that all main intrasurgical outcome parameters including entry time of both umbilical access (45.8 ± 2.9 vs 225.4 ± 5.7 seconds) and periumbilical access (38.4 ± 3.5 vs 210.7 ± 2.4 seconds) as well as blood loss values (7.6 ± 3.9 vs 11.7 ± 5.3 mL) were significantly reduced in the DOE group compared with those of the OHT group, with the total number of major and minor vascular and bowel injuries occurring, respectively, in 1 of 86 and 10 of 82 patients.8,9
In consideration of the foregoing data, in the current study we presumed that the main parameters of abdominal entry, such as time required for entry into abdomen, blood loss, and occurrence of vascular and bowel injury would be improved by using DOE in reproductive-age obese women compared with those parameters for OHT.
MATERIALS AND METHODS
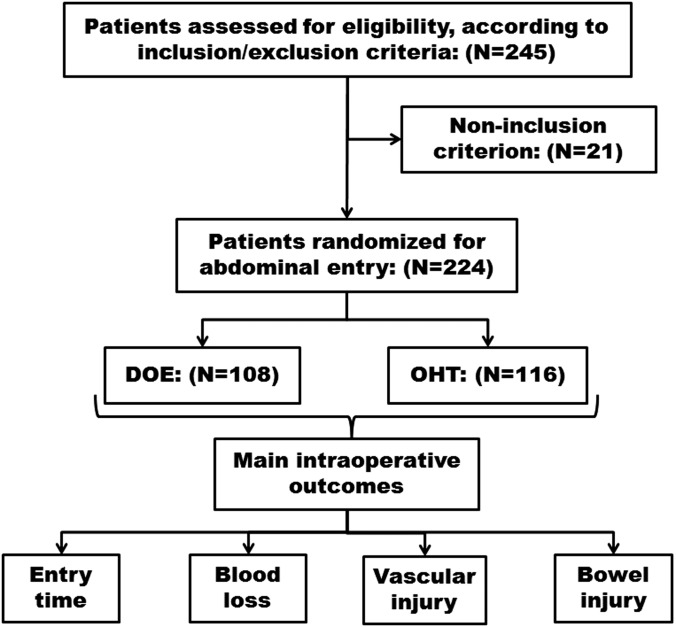
Between January 2006 and December 2010, 245 reproductive-age obese women with a benign pelvic mass (utero-ovarian origin) were assessed for eligibility according to the study design. The patients were from the departments of obstetrics and gynecology of the university-affiliated hospitals that participated in this research (Figure 1).
Figure 1.
Study design. DOE, direct optical entry; OHT, open Hasson technique.
All procedures used in the present study were in accordance with guidelines of the Helsinki Declaration on human experimentation. Approval was received by ethics committees of the all the university-affiliated hospitals in this study in accord with a previous general study design of application of different abdominal entry techniques in our patients. Teams, which included experienced surgeons and mature residents who had done at least 300 laparoscopic procedures in the past, were formed. All the surgical procedures of the current study were done by members of these teams. Inclusion criteria included reproductive-age (between 30 and 40 years) patients with a BMI (between 30 and 40 kg/m2), defined as obesity of class I to II10 with the presence of benign pelvic mass of uterine and/or ovarian origin. Initial exclusion criteria included postmenopausal age due to differing physiological characteristics8 and previous abdominal and pelvic surgeries because of scar tissue and postsurgical adhesions. Noninclusion criteria during the perioperative examination included a pelvic mass >10 cm in diameter. Twenty-one patients were not included because they had a >10-cm-diameter pelvic mass; subsequently, 224 patients agreed and were included in this prospective multicenter randomized study.
Patients provided written informed consent for each procedure and permission to use anonymously their health information for research purposes.
Surgical procedures for benign uterine or ovarian pathologies were randomly performed via abdominal entry by either DOE or OHT. The method of allocation was controlled by the statistician who assigned patients to surgery with a 1:1 randomization ratio by the use of sealed numbered containers, and surgeons received the container in the operating room with patient. To avoid confounding factors, there was consensus between the surgeons in this study that when they received a container they would not abandon the entry technique determined by the statistician in favor of others, and they agreed not do more than 2 attempts at entry during the procedure.
All surgical procedures were performed under general anesthesia with endotracheal intubations and insertion of an orogastric tube by a technique described in our previous studies,8–10 and all patients received a prophylactic dose of intravenous antibiotic (cefazolin, 2 g), as requested by the hospital administrations in the protocol for management of obese patients.
Laparoscopic procedures were performed by means of routinely used standard laparoscopic equipment: 108 patients underwent abdominal entry via DOE and 116 patients via OHT.
The DOE access was performed using an optical bladeless trocar with an optical viewing port (Endopath or Endopath Xcel; Ethicon Endo-Surgery, Cincinnati, Ohio) according to the steps described previously,9 but will be briefly recapped here. A 10-mm intraumbilical vertical incision was made with a size 15 blade through the skin down to the fascia. The fascia was then gently lifted upward by the hands of the operators (Figure 2) or, alternatively, with 2 Kocher forceps in case of difficulty, to prevent it from sliding and slipping away from the skin at the trocar entry site (Figure 3). Then the point of entry was elevated by the surgeons prior to trocar insertion, taking into account that elevation can distort anatomical features of the abdominal wall. The fascia at the umbilicus was not closed by stitches at the completion of the case because the bladeless trocar was 10 mm in diameter. The optical bladeless trocar, with a 0°illuminated laparoscope, was gently inserted directly into the abdominal cavity using clockwise and counterclockwise rotation under constant axial force (Figure 4). The peritoneum was perpendicularly penetrated under direct vision, enabling identification of the fused abdominal layers at umbilical site, avoiding trocar angulations. Then an obturator was removed, and the insufflation tube was connected to the trocar for the creation of required CO2 pneumoperitoneum, with a 10-L/min CO2 flow rate.
Figure 2.
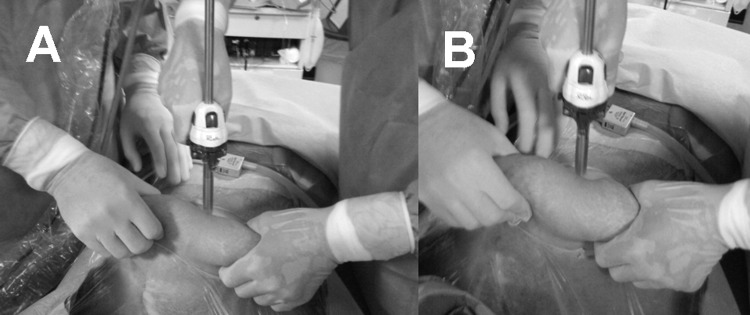
After umbilical incision and trocar lighted-tip positioning on umbilical cutting (A), both surgeons grab and elevate the abdomen, and the first surgeon grasps the handle of the trocar and introduces it into the umbilical incision (B).
Figure 3.

Alternatively, in cases of difficulty, the surgeons grab and elevate the abdomen with 2 Kocher forceps to prevent it from sliding and slipping away from the skin at the trocar entry site.
Figure 4.
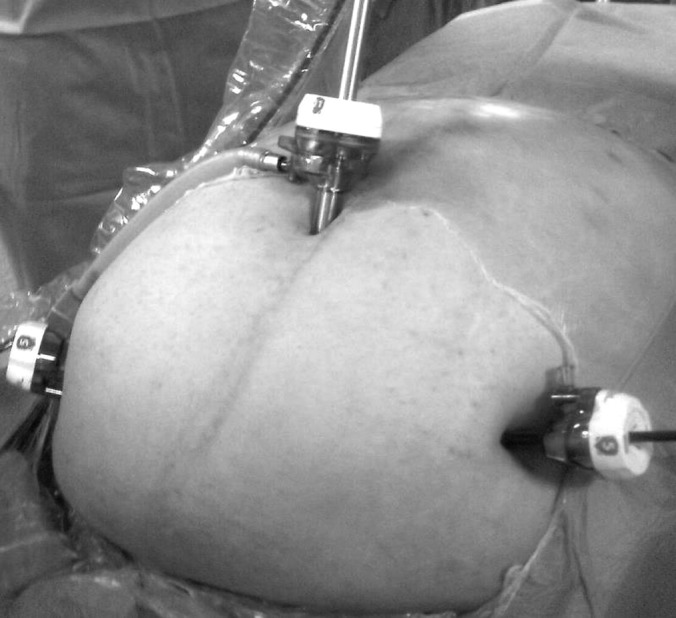
After peritoneal overcoming and abdominal entry, the 0° laparoscope without the obturator is reinserted to check proper position of the trocar cannula and pneumoperitoneum is immediately performed. The entry site and adjacent viscera are inspected promptly for continuing the operation and positioning the ancillary trocars (the photo displays an obese women with a BMI of 36 kg/m2 with positioned ancillary trocars).
In the OHT group, the Hasson trocar (Ethicon Endo-Surgery, Cincinnati, Ohio) was applied by a routinely applicable technique.10 Briefly, the umbilical skin was vertically incised and the subcutaneous fat was dissected down until the upper sheet of the rectal fascia was visualized. Following midline fascial dissection, the peritoneum was incised with a scalpel and bluntly divided with the index fingers. Then the abdominal wall was grasped and lifted at points lateral to the incision; the trocar was inserted under continuous visualization; and it was fixed to the abdominal wall/rectal fascia by 2 stitches, following insufflation of the abdominal cavity through the trocar and the insertion of a prewarmed laparoscope. At the start of OHT, for security reasons, the fascia was identified and fixed by 2 stitches to close at the end of procedure.
The laparoscopic entry techniques were compared by analysis of the following criteria: entry time in seconds was defined as the time from incision of the subumbilical skin to the visualization of the intra-abdominal cavity; the occurrence of major and minor vascular or bowel injuries; blood loss during the access; and number of attempts.
The entry time in seconds was registered under a leading surgeon's control. The operating room personnel turned on the timer (a stopwatch) when the surgeon started the abdominal entry and turned off the timer when the surgeon entered into the abdominal cavity and visualized the intra-abdominal cavity. The blood loss of skin and layer bleeding was measured by the weight of swabs in grams.
A calculation of sample size and power analysis proved that 107 patients in each group would be necessary to detect a difference with an alpha error level of 5% and a beta error of 80%. Based on the previously published papers,6–9 we expected the mean blood loss to be 15 mL/kg per operation with a standard deviation of 75%. We were able to detect a difference of at least 50% between the 2 groups. We chose an a value of 0.05 and a b value of 0.2 (power of 80%).
The power analysis of the secondary outcomes is ∼60%; a higher powered analysis of blood loss should be reached by a larger group of women, even if it could be justified with a larger time need to recruit patients.
Statistical analysis was performed using the Statistical Program/STATVIEW 5.1 for Macintosh (Abacus Concepts, Inc, Berkeley, California). One-way analysis of variance was used to perform the table statistics. The Levene test for homogeneity of the variation was used to screen for violations of the assumptions of the analysis of variance. Comparisons between these 2 groups with homogeneity of variability were performed by the 2-tailed unpaired Student t test (P < .01). Alternatively, comparisons between groups with abnormality and heterogeneity of variability were performed by Welch t test. Discrete variables were analyzed using the Fisher exact test. A P value of < .05 was considered statistically significant. There was no need to make the analysis based on the “intention to treat” because all patients enrolled concluded the study.
RESULTS
Main baseline characteristics of patients (Table 1) including age (36.1 ± 4.5 vs 35.7 ± 5.8 years), BMI (34.9 ± 5.1 vs 35.1 ± 4.9 kg/m2), and parity (2.1 ± 0.4 vs 1.9 ± 0.9) were not significantly different between the DOE and OHT groups (P > .05). However, intraoperative parameters (Table 2) such as the entry time (71.9 ± 3.7 vs 215.1 ± 6.2 seconds) and blood loss value (9.7 ± 6.1 vs 12.2 ± 2.9 mL) were significantly reduced in the DOE group compared with those of the OHT group (respectively, P < .0001 and < .01). There were also trends toward slight decreases of the occurrence of the minor injuries, manifested as omental small vessels rupture (0 of 108 vs 4 of 116) and punctures and pinches of jejunal serosa (0 of 108 vs 3 of 116) in patients of the DOE group compared with those of OHT group (respectively, P = .0515 and = .0925).
Table 1.
Baseline Homogeneous Characteristics of the Participants in the Studya
| Characteristics | DOE Group (n = 108) | OL Access Group (n = 116) | P Value |
|---|---|---|---|
| Age, y | 36.1 ± 4.5 | 35.7 ± 5.8 | P = .923 |
| NS | |||
| BMI, kg/m2 | 34.9 ± 5.1 | 35.1 ± 4.9 | P = .765 |
| NS | |||
| Parity | 2.1 ± 0.4 | 1.9 ± 0.9 | P = .035 |
| (P < .01) NS |
Data are expressed as mean ± standard deviation. Statistical analysis was performed by means of an unpaired Student t test.
BMI, body mass index; DOE, direct optical entry; NS, not significant; OL, open laparoscopy.
Table 2.
Difference and Complications During First Access Among the 2 Groups
| Variables | DOE Group (n = 108) | OL Access Group (n = 116) | P Value |
|---|---|---|---|
| Duration of entry, mean ± SD, s | 71.9 ± 3.7 | 215.1 ± 6.2 | P < .0001a |
| Blood loss, mean ± SD, ml | 9.7 ± 6.1 | 12.2 ± 2.9 | P < .01b |
| Major vascular injuries | 0 | 0 | — |
| Minor vascular injuries | 0 | 4 | P = .0515c |
| Minor bowel injuries | 0 | 3 | P = .0925c |
For statistical analysis, unpaired t test with Welch correction was used.
For statistical analysis, unpaired Student t test was used.
For statistical analysis, Fisher exact test was used.
Abbreviations as in Table 1.
To evaluate whether a possible danger originates from entry-induced injuries, we spent <5 minutes on the entry and no entry complications required additional treatments. Then all surgical procedures were completed without major or further complications.
In addition, the DOE was successful in 103 of 108 patients on the first attempt and in 5 of 108 (4.6%) patients on the second attempt, while all OHT was done by the first attempt.
Postoperative 4- to 6-week follow-up did not reveal any problems, not even in women with small vascular and bowel injuries at entry.
DISCUSSION
A wide diversity of abdominal entry techniques have developed since laparoscopy became a surgical approach. Recently Ahmad et al3 identified 13 different laparoscopic-entry techniques from 28 randomized controlled studies. Indeed numbers of entry techniques are multiplying even faster in consideration of the state-of-the-art updates, which are consistently retooling operating theaters, and surgical technique modifications, but abdominal entry is always hazardous when obese patients are in the surgical room.
According to the literature, abdominal entry times are wide-ranging. Intriguingly, in obese patients, Bernante et al11 reached an average entry time of ∼20 seconds (range 10–50), independently of high BMI rate of 48 kg/m2 (range 40–62), and they concluded that BMI did not affect the entry time. Although the investigators reported successful fast entry without intrasurgical vascular and hollow viscous injuries, there was a notice concerning trocar insertion inside the bursa omentalis through the gastrocolic ligament in 5 cases. In those cases, the trocar was relocated into the correct position without complications for those patients.11
In 327 gastric bypass procedures, Berch et al12 used DOE without trocar-related bowel or vascular injuries in the entry sites, and only in 10 patients did they register entry times that were ∼28.0 ± 1.2 seconds. Subsequently, they concluded that DOE could provide a safe and rapid technique for placement of the initial trocar.
It seems that there are study design shortcomings of these reports concerning abdominal entry times registered by Bernante et al11 in 70 patients, whereas there were complications reviewed in 200 patients. Furthermore, Berch et al12 evaluated only 10 cases from 327 patients. Therefore, it is difficult to consider the beneficial conclusions concerning entry time in these studies. A longer abdominal entry time was reached by Hallfeldt et al,13 who applied DOE in 200 patients undergoing laparoscopic cholecystectomy, appendectomy, or herniorrhaphy as an alternative to VNE and minilaparotomy and reached an average entry time of ∼4 minutes (range 2.30–11.0 minutes).
The results of these observations are contradictory and probably why wide ranges of entry times are related with the registration of this criterion. In our studies, entry time in seconds was defined as the time from incision of the subumbilical skin to the visualization of the intra-abdominal cavity.
Subsequently, we presumed that the main parameters of abdominal entry such as entry time, blood loss, and occurrence of vascular and bowel injuries would be improved by using DOE in reproductive-age obese women compared with those of OHT. Despite such limitations as small numbers of patients in the groups and restricted age-groups and BMI, in this prospective multicenter randomized study we showed the advantages of DOE versus OHT concerning the entry times (71.9 ± 3.7 vs 215.1 ± 6.2 seconds) and blood loss values (9.7 ± 6.1 vs 12.2 ± 2.9 mL) that were significantly reduced with trends to slight decreases of the occurrence of the minor vascular (0 of 108 vs 4 of 116) and bowel injuries (0 of 108 vs 3 of 116) in this particular population (ie, reproductive-age obese women). The advantages of our study are the well-organized study design incorporating a restricted population by reproductive age (between 30 and 40 years) and BMI (between 30 and 40), the absence of previous surgery in the abdominal cavity, and size limit of benign pelvic masses to <10 cm in diameter. Furthermore, this research was carried out by teams with experienced leading surgeons and mature residents in university-affiliated hospitals.
The results of current study accorded with our previous comparisons of these techniques in women with previous abdominopelvic surgery.8 In some instances, our results agreed with the results of comparative studies of DOE and VNE in reproductive-age women without previous surgery6 and in postmenopausal women.7 Furthermore, our results concurred with entry times by other teams14 who applied DOE as an alternative to VNE in 650 laparoscopic procedures and who analyzed the site, the duration of entry, and any complications. String et al 14 demonstrated varied mean entry times in seconds with SD values depending on the trocar entry sites: 114 ± 30 at the back site, 92 ± 45 at the umbilical site, and 77 ± 35 at remaining sites, including right/left/midline upper and right/left lower quadrants, with 2 serious complications such as small-bowel and gallbladder injuries.
Alternatively, manifold intraoperative abdominal entry complications in obese patients are not always registered and described. A distinguishing characteristic of obese patients for abdominal entry is a caudally displaced umbilical position due to increased BMI,15 but the cephalocaudal relationship between the aortic bifurcation and umbilicus varies widely, and it is not related to BMI in anesthetized patients.16
However, when Sabeti et al17 applied DEO in 2207 obese patients undergoing to bariatric surgery, 4 cases of small-bowel mesenteric vascular injuries occurred in patients with prior abdominal surgery. Mesenteric vessel clipping was done in 3 cases via conversion to laparotomy and hemostasis in one case and was achieved by pressure in the retroperitoneal fat.17
In 844 bariatric laparoscopic procedures, Rosenthal et al18 applied DOE in obese patients with an average BMI of 53.2 kg/m2. They did not register any cases of intraoperative complications and did not evaluate entry time at all. Concerning the technical part of surgery, 2 trocar-site hernias developed, and although there were several cases of postoperative complications (eg, early: atelectasis, gastrointestinal bleeding, wound infection, anastomotic leak, and deep venous thrombosis, respectively, in 11.6%, 2.5%, 3.7%, 1.9%, and 0.8% of patients; late minor and major: marginal ulcer, anastomotic stricture, trocar-site hernia, small-bowel obstruction, respectively, in 1.4%, 1.4%, 6.3%, and 1.4% of patients), the investigators concluded that the DOE shows a trend toward reducing trocar-site hernias, decreasing bowel obstruction, and eliminating the need for time-consuming fascial closure.18
Whereas Schwartz et al19 described only one case of VNE-related injury of the transverse colon muscularis without penetration into the mucosa among 600 morbidly obese patients, there are different opinions concerning the superiority of particular abdominal entry access over other techniques. Ballem and Rudomanski20 compared the results of different abdominal entry techniques in 300 patients, took into account complications, including bowel laceration, and concluded that compared with VNE, OHT is the superior technique for quickly and safely obtaining pneumoperitoneum. However, Dunne et al21 comparatively analyzed the results of OHT and VNE, respectively, in 1200 and 1887 patients and demonstrated an absence of evidence to support as superior either of these 2 techniques. However, their report registered only such dangerous outcomes as a full thickness colonic perforation, a small-bowel perforation, and a left hepatic lobe injury, whereas abdominal entry times and minor complications were not presented.21
Analysis of the literature results indicated that restricted abdominal entry complications, such as blood loss and occurrence of vascular and/or bowel injuries, were not described in most studies designed to compare different techniques of abdominal entry. Correctly evaluating abdominal entry efficiency depends on study design and reviewed outcomes. Therefore, further investigations are required to identify correct evaluation criteria of abdominal entry techniques.
CONCLUSIONS
Using DOE reduced entry times and blood loss with trends to slightly decrease the occurrence of the minor vascular and bowel injuries, thus enabling a possible alternative to OHT in obese women. However, further larger trials need to confirm the possible additional benefits of DOE.
Contributor Information
Andrea Tinelli, Department of Obstetrics and Gynaecology, Vito Fazzi Hospital, Lecce, Italy..
Antonio Malvasi, Department of Obstetrics and Gynaecology, Santa Maria Hospital, Bari, Italy..
Ospan A. Mynbaev, Experimental Researches and Modeling Division, Moscow State University of Medicine and Dentistry, Moscow, Russia..
Daniel Alberto Tsin, Department of Gynecology, Division of Minimal Invasive Endoscopy, The Mount Sinai Hospital of Queens, New York, NY, USA..
Fausto Davila, Hospital Regional de Poza Rica, Sesver, Monterrey, Mexico..
Guillermo Dominguez, Fundaciòn Hospitalaria, Buenos Aires, Argentina..
Emanuele Perrone, Department of Gynecology and Obstetrics, University of Perugia, Perugia, Italy..
Farr R. Nezhat, Columbia University College of Physicians and Surgeons, New York, NY, USA.; Division of Gynecologic Oncology and the Department of Obstetrics and Gynecology, St. Luke's-Roosevelt Hospital Center, New York, NY, USA.
References:
- 1. Tinelli A, Malvasi A, Schneider AJ, et al. First abdominal access in gynecological laparoscopy: which method to utilize? [in Italian]. Minerva Ginecol. 2006;58(5):429–440 [PubMed] [Google Scholar]
- 2. Tinelli A. Laparoscopic Entry: Traditional Methods, New Insights and Novel Approaches. London, UK: Springer, 2012 [Google Scholar]
- 3. Ahmad G, O'Flynn H, Duffy JM, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2012;2:CD006583. [DOI] [PubMed] [Google Scholar]
- 4. Ambardar S, Cabot J, Cekic V, et al. Abdominal wall dimensions and umbilical position vary widely with BMI and should be taken into account when choosing port locations. Surg Endosc. 2009;23(9):1995–2000 [DOI] [PubMed] [Google Scholar]
- 5. Stany MP, Winter WE, 3rd, Dainty L, Lockrow E, Carlson JW. Laparoscopic exposure in obese high-risk patients with mechanical displacement of the abdominal wall. Obstet Gynecol. 2004;103(2):383–386 [DOI] [PubMed] [Google Scholar]
- 6. Tinelli A, Malvasi A, Istre O, Keckstein J, Stark M, Mettler L. Abdominal access in gynaecological laparoscopy: a comparison between direct optical and blind closed access by Verres needle. Eur J Obstet Gynaecol Reprod Biol. 2010;148(2):191–194 [DOI] [PubMed] [Google Scholar]
- 7. Tinelli A, Malvasi A, Guido M, Istre O, Keckstein J, Mettler L. Initial laparoscopic access in postmenopausal women: a preliminary prospective study. Menopause. 2009;16(5):966–970 [DOI] [PubMed] [Google Scholar]
- 8. Tinelli A, Malvasi A, Guido M, Tsin DA, Hudelist G, Stark M, Mettler L. Laparoscopy entry in patients with previous abdominal and pelvic surgery. Surg Innov. 2011;18(3):201–205 [DOI] [PubMed] [Google Scholar]
- 9. Tinelli A, Malvasi A, Hudelist G, Istre O, Keckstein J. Abdominal access in gynaecological laparoscopy: a comparison between direct optical and open access. J Laparoendosc Adv Surg Tech A. 2009;19(4):529–533 [DOI] [PubMed] [Google Scholar]
- 10. Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121(7):492–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bernante P, Foletto M, Toniato A. Creation of pneumoperitoneum using a bladed optical trocar in morbidly obese patients: technique and results. Obes Surg. 2008;18(8):1043–1046 [DOI] [PubMed] [Google Scholar]
- 12. Berch BR, Torquati A, Lutfi RE, Richards WO. Experience with the optical access trocar for safe and rapid entry in the performance of laparoscopic gastric bypass. Surg Endosc. 2006;20(8):1238–1241 [DOI] [PubMed] [Google Scholar]
- 13. Hallfeldt KK, Trupka A, Kalteis T, Stuetzle H. Safe creation of pneumoperitoneum using an optical trocar. Surg Endosc. 1999;13(3):306–307 [DOI] [PubMed] [Google Scholar]
- 14. String A, Berber E, Foroutani A, Macho JR, Pearl JM, Siperstein AE. Use of the optical access trocar for safe and rapid entry in various laparoscopic procedures. Surg Endosc. 2001;15(6):570–573 [DOI] [PubMed] [Google Scholar]
- 15. Ambardar S, Cabot J, Cekic V, et al. Abdominal wall dimensions and umbilical position vary widely with BMI and should be taken into account when choosing port locations. Surg Endosc. 2009;23(9):1995–2000 [DOI] [PubMed] [Google Scholar]
- 16. Nezhat F, Brill AI, Nezhat CH, Nezhat A, Seidman DS, Nezhat C. Laparoscopic appraisal of the anatomic relationship of the umbilicus to the aortic bifurcation. J Am Assoc Gynecol Laparosc. 1998;5(2):135–140 [DOI] [PubMed] [Google Scholar]
- 17. Sabeti N, Tarnoff M, Kim J, Shikora S. Primary midline peritoneal access with optical trocar is safe and effective in morbidly obese patients. Surg Obes Relat Dis. 2009;5(5):610–614 [DOI] [PubMed] [Google Scholar]
- 18. Rosenthal RJ, Szomstein S, Kennedy CI, Zundel N. Direct visual insertion of primary trocar and avoidance of fascial closure with laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21(1):124–128 [DOI] [PubMed] [Google Scholar]
- 19. Schwartz ML, Drew RL, Andersen JN. Induction of pneumoperitoneum in morbidly obese patients. Obes Surg. 2003;13(4):601–604 [DOI] [PubMed] [Google Scholar]
- 20. Ballem RV, Rudomanski J. Techniques of pneumoperitoneum. Surg Endosc. 1993;3(1):42–43 [PubMed] [Google Scholar]
- String A, Berber E, Foroutani A, Macho JR, Pearl JM, Siperstein AE. Use of the optical access trocar for safe and rapid entry in various laparoscopic procedures. Surg Endosc. 2001;15(6):570–573 [DOI] [PubMed] [Google Scholar]
- 21. Dunne N, Booth MI, Dehn TC. Establishing pneumoperitoneum: Verres or Hasson? The debate continues. Ann R Coll Surg Engl. 2011;93(1):22–24 [DOI] [PMC free article] [PubMed] [Google Scholar]