Abstract
Restricted, repetitive and stereotyped patterns of behavior, interests and activities (RRBs) are among the core symptoms of autism spectrum disorders (ASD). Previous studies have indicated that RRBs differentiate ASD from other developmental disorders and from typical development. This study examined the presentation of RRBs as reported on the Repetitive Behavior Scale-Revised (Bodfish, Symons, Parker & Lewis, 2000), a caregiver report, in children with ASD (separated into autism and Pervasive Developmental Disorder-Not Otherwise Specified groups) compared to children with non-spectrum developmental delays or typical development. We examined the role of age, cognitive functioning, sex and social communication impairment as they relate to RRBs. The stability of RRBs in children with autism was also examined over the course of two years. Results of the study confirmed that the amount and type of RRBs differs by diagnosis. Age, cognitive functioning, sex and social-communication impairment were not significant correlates. Among children with autism, RRBs remained stable over time.
Keywords: Autism spectrum disorders, repetitive behaviors
Introduction
Restricted, repetitive and stereotyped patterns of behavior, interests and activities (RRBs) are among the core features of autism spectrum disorders (ASD) as outlined by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV-TR; APA, 2000). The DSM-IV-TR includes descriptions of four symptoms of RRBs: preoccupation(s) with stereotyped and restricted patterns of interests, adherence to nonfunctional routines, stereotyped and repetitive motor movements, and preoccupation with parts of objects.
RRBs are not specific to ASD; these behaviors are observed in typically developing children (Arnott et al. 2010; Barber, Wether by, & Chambers, 2012; Evans, 1997) and among individuals with other developmental and psychiatric disorders, but it is the degree of excess and resulting impairment that appears specific to ASD. Studies have found that ASD can be differentiated from other disorders based on the type and severity of the RRBs presented (Bodfish, Symons, Parker, & Lewis, 2000; Mandy, Charman, Gilmour, & Skuse, 2011). In addition, the presence of RRBs has been shown to increase the accuracy of early diagnosis of ASD (Kim & Lord, 2010).
Measurement of RRBs
Several methods of measuring RRBs in ASD are used clinically, including caregiver interview, caregiver questionnaires, and observational methods. The Autism Diagnostic Interview-Revised (ADI-R, Rutter, LeCouteur, & Lord, 2003) is a semi-structured caregiver interview that measures the current presentation of RRBs as well as the behaviors at their worst. Several caregiver questionnaires are also commonly used to measure RRBs, including the Repetitive Behavior Scale-Revised (RBS-R; Bodfish et al., 2000) and the Repetitive Behavior Questionnaire (RBQ; Turner 1995). These parent report measures are among the most commonly used to understand the factor structure of RRBs in ASD; observational measures have thus far not been used widely.
RRB Subtypes
Evidence exists for distinct subtypes of RRBs, and several classification systems have been proposed. Turner (1999) provided one of the first categorical descriptions of RRBs, classifying RRBs as either higher order (preoccupation with restricted interests and adherence to nonfunctional routines) or lower order (repetitive motor movements and preoccupation with parts of objects). A factor analysis conducted on the RRB questions of the ADI-R (Rutter et al.,2003) indicated that a two factor model best fit the data, resulting in identifiable RRB subtypes characterized as repetitive sensory motor and resistance to change (Cuccaro et al., 2003). Repetitive sensory motor (RSM) behaviors included repetitive motor mannerisms and repetitive use of objects (termed lower order by others), while the resistance to change behaviors included adherence to routines and rituals, characterized by insistence of sameness (IS; termed higher order by others). Other analyses using the RRB items of the ADI-R have also supported a two factor model of RRBs (Mooney et al., 2009; Richler et al., 2010). However, Lam et al. (2008) found evidence for a three factor model: RSM, IS, and circumscribed interests. Differences in the study samples may explain the variation in RRB factor structures of the ADI-R. For instance, some of the studies finding two factors used samples that included young children with either Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) or non-ASD developmental delays (Mooney et al., 2009), as well as children with autism, typical development and non-ASD developmental delays (Richler et al., 2007). The study that found three factors used a wide age range (spanning from 20 months to 29 years), all diagnosed with autism (Lam et al., 2008).
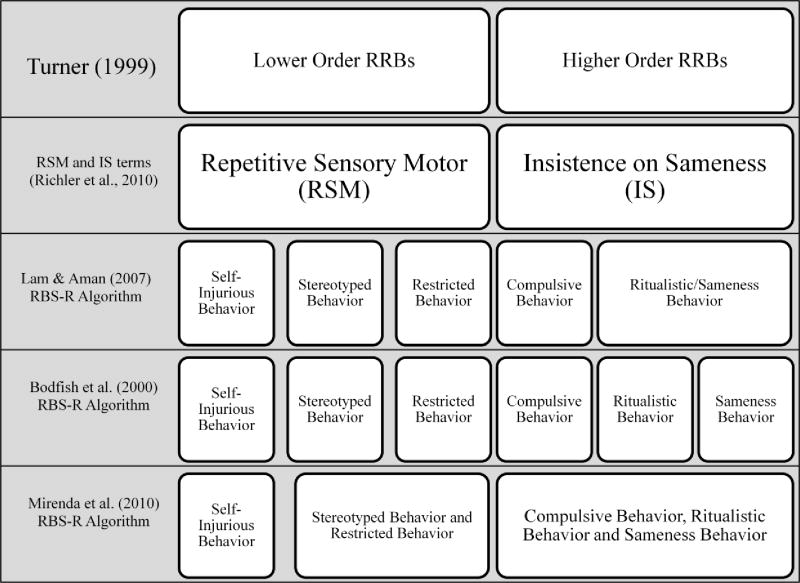
The structure of repetitive behaviors has also been examined in a widely used parent-rated scale of RRBs, the RBS-R (Bodfish et al., 2000). In a sample of children and adults with ASD, a factor analysis partially confirmed the original RBS-R structure, retaining stereotypic behavior, compulsive behavior, self-injurious behavior, and restricted behavior, but combining into one factor ritualistic and sameness behavior (Lam & Aman, 2007). Most recently, Bishop et al. (2012) conducted a factor analysis of the RBS-R in a sample of children and adolescents with ASD; their study also partially confirmed this five factor model of the measure. In a sample of young children with ASD, Mirenda et al. (2010) confirmed that several factor models of RRBs could be supported by the RBS-R; a five-factor model, similar to the Lam and Aman (2007) model, and a three-factor model that categorized stereotyped and restricted behaviors (analogous to the RSM behaviors mentioned above), compulsive, ritualistic and insistence on sameness behaviors (i.e., IS behaviors), and self injurious behaviors (SIB) as 3 distinct factors. See Figure 1 for the conceptualization of the RBS-R subscales.
Figure 1. Relationship of RBS-R scoring algorithms to conceptualizations of repetitive behaviors.
Note: The RBS-R (Bodfish et al, 2000) subscales consist of 43 items. The Lam and Aman scoring algorithm consists of 38 items and merges items from the Ritualistic and Sameness Behavior subscales (Lam & Aman, 2007). The conceptualization set forth by Mirenda and colleagues (2010) includes all 43 items with the Stereotyped and Restricted Behavior scales merged and the Compulsive, Ritualistic and Sameness Behavior scales merged. In a review of RRBs, Turner (1999) considered stereotyped behaviors “lower order” and compulsive behaviors “higher order.”
Associations of RRBs within ASD
Within the autism spectrum, RRBs have been shown to be associated with type of ASD diagnosis, cognitive functioning, age and sex (Bishop et al., 2012; Lam & Aman, 2007; Mandy et al., 2012; Richler, Huerta, Bishop, & Lord, 2010). The severity and frequency of RRBs have differentiated PDD-NOS from autism. As defined by the DSM-IV-R (APA, 2000), RRBs are not necessary for a diagnosis of PDD-NOS. Research has suggested that children with PDD-NOS engage in less severe RRBs than children with a diagnosis of autism; at least two types of RRBs, sensory interests and adherence to routines, are reported to occur less frequently among individuals with PDD-NOS than among individuals with autism (Mandy, Charman, Gilmour, & Skuse, 2011).
Owing to its differential association with various forms of RRBs, cognitive functioning has been used to classify subtypes of these behaviors. Higher-order RRBs, such as circumscribed interests, have been observed more frequently among individuals with higher cognitive functioning (Bishop, Richler & Lord, 2006). Conversely, Richler et al. (2010) reported that higher cognitive functioning at the age of 2 years was associated with less severe repetitive sensorimotor behaviors. Lower-order RRBs, such as repetitive sensorimotor activities, have also been found to be more severe in individuals with lower cognitive ability (Bishop et al., 2012; Cuccaro et al., 2003; Lam, Bodfish, & Piven, 2008).
Although several sources suggest that age affects the expression of RRBs in ASD, findings are somewhat mixed. Some data suggest that older individuals engage in more repetitive sensorimotor behaviors, stereotyped behaviors, insistence on sameness, and circumscribed interests than younger people (Lam & Aman, 2007). Conflicting evidence has been observed for the association of age and compulsive behavior; for example, Bishop et al. (2006) found that older children had more compulsions than younger children, while Richler et al. (2007) found no age difference. Findings from another cross-sectional study indicated that overall, repetitive behaviors were observed less frequently in adults than in children (Esbensen, Seltzer, Lam & Bodfish, 2009).
Given the sex difference in ASD prevalence, the role of sex in the presentation of RRBs has been explored. Mandy et al. (2012) found that male children and adolescents (3-18 years) presented with more and qualitatively different RRBs than females, including repetitive play with objects (lining up toys) and circumscribed interests. In a sample of toddlers (17 to 36 months) with ASD, females with average cognitive functioning were reported to have fewer RRBs than both males and females with low to average cognitive functioning (Sipes, Matson, Worley & Kozlowski, 2011).
Trajectory of RRBs
Although the diagnostic stability of autism is high (Gotham, Pickles & Lord, 2012; Lord et al., 2006; Stone et al., 1999), changes in the presentation of symptoms of the disorder are observed over time (Charman et al., 2005). Despite wide recognition of this phenomenon, there are few data on specific trajectories of RRBs. Moore and Goodson (2003) reported that at the age of 2 years, repetitive play with objects and unusual sensory interests were more prominent than compulsions and rituals, and at the age of 4 years, an increase in all behaviors was reported. Repetitive use of objects has also been found to be less frequent in older children (Bishop et al.,2006). When considering these data, it is important to recognize the limitations of cross-sectional data, insofar as between-subjects data are not useful in establishing longitudinal trends.
Richler et al. (2010) conducted one of the few longitudinal studies of RRBs. Scores on RSM and IS subscales of the ADI-R were tracked over seven years in children with ASD and children with non-spectrum developmental delays. There was a negative correlation between Nonverbal IQ (NVIQ) and the presentation of RRBs; as NVIQ increased, sensory and motor behaviors decreased over time. The severity of IS behaviors, however, was reported to increase over time for this subgroup of children. In addition, the social affect domain score (SA) of the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000), which assesses social communication impairments, was negatively related to IS scores, such that children with more impairment in social communication at the age of 2 years had fewer IS behaviors, compared to children with lower SA scores.
Current Study
Elucidation of the subtypes of RRB, has led to more precise categorization of children with ASD, and may eventually lead to the development of more targeted therapeutic interventions. However, the dearth of longitudinal data on RRBs precludes any firm conclusions about prognosis. The current study addresses this gap in the literature by examining RRBs as measured by the RBS-R (Bodfish et al., 2000), one of few caregiver-report measures that focus solely on RRBs. This study is the first to examine the RBS-R over time in an ASD sample. Based on the available literature, it was hypothesized that children with ASD (autism or PDD-NOS) would have significantly higher scores on the RBS-R than comparison groups of non-spectrum developmental delay and typical development. Differences based on demographic and phenotypic characteristics also were expected. Females were expected to present with fewer RRBs; and younger children were expected to engage in more severe RSM behaviors. Lower cognitive ability was expected to be associated with less IS behaviors and more RSM. Finally, we hypothesized that children with fewer social communication deficits would engage in fewer RRBs. The stability of the RBS-R over 2 years was evaluated in a subsample of children with autism; although some data suggest that age and attendant improvements in cognitive ability are associated with changes in RRB, no changes were expected in the relatively short timeframe used in this study.
Methods
Participants
Participants were 277 children aged 2 to 11 years who were assessed as part of either a protocol that included a diagnostic evaluation (cross-sectional cohort), or a longitudinal phenotyping protocol (longitudinal cohort) in the Pediatrics and Developmental Neuroscience Branch of the National Institute of Mental Health. Participants in the cross-sectional cohort included 128 children diagnosed with autism (AUT; mean age = 4.14 ± 1.57), 46 children diagnosed with pervasive developmental disorder-not otherwise specified (PDD-NOS; mean age=4.07 ± 1.88),44 children with non-spectrum developmental delay (DD; mean age = 3.85 ± 1.55) and 59 typically developing children (TD; mean age = 3.71 ± 1.46). A diagnosis of cerebral palsy or a significant neurological condition that would prohibit testing were exclusions for all groups, and for the TD group only, a history of extremely low birth weight (due to prematurity or intrauterine growth failure) was exclusionary.
The DD group was selected for a nonverbal developmental quotient (NVDQ) less than 80, with ASD ruled out by scores on the ADI-R or ADOS, or clinical judgment. Inclusionary criteria for the TD group included NVDQ of 85 or above, and no personal or family history of developmental delay. The DD group was not significantly different from the AUT group on NVDQ, though both differed from TD; all groups were matched on chronological age. As this was an observational study, participants in the AUT, PDD-NOS, and DD groups were receiving variable rates and types of interventions. The longitudinal sample was a subset of children from the AUT group (n=39), aged 2 to 7 years at the initial visit (mean age 4.03±1.20). Participant characteristics are summarized in Table 1.
Table 1.
Sample Description
| AUT | PDD-NOS | DD | TYP | AUT (Visit 2) | AUT (Visit 3) | |
|---|---|---|---|---|---|---|
| Cross-sectional Cohort | Longitudinal Cohort | |||||
| N | 128 | 46 | 44 | 59 | 39 | 39 |
| Age in years (SD) | 4.14 (1.57)a | 4.07 (1.88) a | 3.85 (1.55) a | 3.71 (1.46) a | 5.35 (1.32) | 6.23 (1.25) |
| Male (n, %) | 108 (84.4) | 41 (89.1) | 35 (79.5) | 44 (74.6) | 36 (92.3) | 36 (92.3) |
| NVDQ (SD) | 59.13 (19.73) a | 80.37 (17.60) b | 61.62 (17.02) a | 109.18 (14.40) c | 55.08 (16.62) a | 56.75 (25.82) a |
| VDQ (SD) | 40.47 (19.35) a | 69.80 (23.39) b | 57.75 (19.10) b,c | 107.85 (15.53) d | 42.58 (21.56) a | 42.70 (26.62) a |
| ADOS Module (n, %) 1 | ||||||
| Toddler | 6 (4.7) | 2 (4.3) | 1 (2.3) | 2 (3.4) | ||
| Module 1 | 110 (85.9) | 20 (43.5) | 24 (54.5) | 8 (13.6) | 29 (74.4) | 28 (71.8) |
| Module 2 | 10 (7.8) | 16 (34.8) | 16 (36.4) | 28 (47.5) | 9 (23.1) | 9 (23.1) |
| Module 3 | 2 (1.6) | 8 (17.4) | 2 (4.5) | 21 (35.6) | 1 (2.5) | 2 (5.1) |
Note. AUT=autism; PDD-NOS=pervasive developmental disorder-not otherwise specified; DD=non spectrum developmental delay; TD=typical development. NVDQ=nonverbal developmental quotient; VDQ=verbal developmental quotient; ADOS=Autism Diagnostic Observation Schedule.
Differing superscripts in the same row denote means that differ significantly at p < 0.05
One subject in the DD group was unable to complete an ADOS at the initial visit.
Procedures
An Institutional Review Board at the National Institutes of Health approved this research. Children in the AUT and PDD-NOS groups were recruited specifically due to concerns about ASD; some children in the DD group enrolled due to concerns about ASD and some enrolled due to concerns about non-spectrum developmental delays. At the initial visit, participants in all groups received a cognitive assessment and an assessment of ASD symptoms (including the ADOS). At this visit, parent-report measures of adaptive functioning and repetitive behaviors were completed by a primary caregiver, including the RBS-R. While the ADI-R was administered to children in the AUT, PDD-NOS and DD groups, parent report of ASD symptoms for participants in the TD group was obtained with the Social Communication Questionnaire (Rutter, Bailey & Lord, 2003). The ADI-R and the ADOS were administered by doctoral-level research reliable clinicians. Diagnoses of autism and PDD-NOS were made based on the ADI-R, ADOS, and clinical judgment to assess DSM-IV criteria. Children in the AUT group met the DSM-IV diagnostic criteria for autism, and children in the PDD-NOS group did not meet criteria for autism, but at least one criterion was met for a qualitative impairment in social interaction, as well as multiple symptoms in the domains of communication and restricted repetitive and stereotyped patterns of behavior.
Children in the longitudinal sample were evaluated at two additional time points approximately one year apart (Time 2, 12.82 ± 1.94 months after Time 1; Time 3, 25.26 ± 2.11 months after Time 1). At each of these time points, the cognitive assessment, the ADOS, and parent report of repetitive behaviors (RBS-R) were repeated.
Measures
Repetitive behaviors
The Repetitive Behavior Scale-Revised (RBS-R; Bodfish, Symons, Parker, & Lewis, 2000), is a 43-item caregiver report questionnaire that assesses repetitive behaviors in individuals. Items are scored on a 4- point Likert-type scale with a score of 0 indicating “behavior does not occur” and a score of 3 indicating “behavior occurs and is a severe problem.” The RBS-R was originally developed with six subscales: Ritualistic Behavior, Sameness Behavior, Self-Injurious Behavior, Stereotyped Behavior, Compulsive Behavior and Restricted Behavior. In a sample of children and adults with ASD (3 to 48 years), a 5-factor solution was judged to be more clinically meaningful (Lam & Aman, 2007). Additionally, only 38 of the 43 items loaded on the six subscales; the items not included on the algorithm were on the Compulsive Behavior (1 item), Ritualistic Behavior (3 items) and Sameness Behavior (1 item) subscales. The resulting algorithm contains 38 items and condenses the Ritualistic Behavior and Sameness Behavior subscales into one subscale (Rituals/Sameness). Both the older and newer algorithms were validated in ASD samples (Bodfish et al., 2000; Lam & Aman, 2007). The Lam and Aman (2007) 5-factor algorithm was used in the current study. Additionally, based on the factor analysis by Mirenda et al. (2010), which further validated use of the measure in young children with ASD (2 to 5 years), a 3-factor algorithm was calculated and included: Stereotyped Behavior and Restricted Interests (RSM); Compulsive Behavior, Ritualistic Behavior and Sameness Behavior (IS); and Self Injurious Behaviors (SIB). Since the Mirenda et al. (2010) SIB subscale was identical to the Lam & Aman (2007) Self-Injurious Behavior subscale, it is not referenced separately when the original Self Injurious Behavior subscale is discussed. We chose to use both scoring algorithms because there is no consensus in the field on which algorithm is superior, and by using both, we facilitate comparison to other studies.
Autism diagnostic measures
The Autism Diagnostic Interview-Revised (ADI-R; Rutter et al., 2003) is a semi-structured standardized interview that surveys both current and past functioning. Items are placed onto an algorithm that varies by language ability and can be used to aid in the diagnosis of ASD. For children younger than 4 years, the Toddler version of the ADI-R was used (Kim & Lord, 2012). This version contains an additional 32 questions which include an assessment of the age of onset of autism symptoms.
The Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000) was administered to directly assess ASD symptoms. The ADOS is a semi-structured instrument wherein the examiner attempts to engage the child with a series of social presses, and rates the child’s social affect and restricted and repetitive behaviors, according to recently published algorithms (Gotham et al., 2009). Scores on the Social Affect domain (SA) of this algorithm, which assesses social and communication impairments, were compared in this study.
Verbal and nonverbal cognitive/developmental abilities
The Mullen Scales of Early Learning (Mullen, 1995) is a test of development that consists of five scales: Gross Motor, Visual Reception, Fine Motor, Receptive Language, and Expressive Language. The Mullen was standardized for children from birth to 5 years, 8 months. Although some participants in the current study were outside of this prescribed age range, many were unable to complete a cognitive test more appropriate for their age, therefore instead of an intelligence quotient, which is norm based and therefore requires that the child be within the age range of the given test, a developmental quotient (DQ) was used (age equivalent, or mental age, divided by chronological age, multiplied by 100). For the Mullen, the average of the Fine Motor and Visual Reception scales was used to calculate NVDQ; verbal DQ (VDQ) was calculated from the average of the Receptive and Expressive Language scales.
The Differential Ability Scales, 2nd Edition (DAS-II; Elliott, 2007) is a cognitive assessment standardized for children from 2:6 through 17:11 years of age. The measure provides assessment of nonverbal and verbal cognitive skills, which together provide a full scale IQ. In order to facilitate comparison to the Mullen scores, NVDQ and VDQ were also calculated from the standardized NVIQ and VIQ from the DAS-II. The average of the Special Nonverbal Composite (Picture Similarities, Pattern Construction, Matrices, and Copying subtests) was computed for NVDQ; the average of the Verbal Composite (Verbal Comprehension and Naming Vocabulary subtests) was computed for VDQ.
Statistical Analysis
Cross-sectional data
Descriptive statistics were calculated for both the Lam & Aman (2007) and Mirenda et al. (2010) RBS-R algorithms. Differences by diagnostic group were evaluated using analysis of variance (ANOVA) and Tukey HSD post-hoc tests. Cohen’s d effect size was used to quantify the differences between groups; d between 0.2 and 0.5 is considered small, 0.5-0.8 medium, and above 0.8 large (Cohen, 1988).
Within the autism group only, specific variables identified by other studies as related to RRBs (age, sex, NVDQ, and ADOS SA) were correlated with each of the RBS-R subscales. To determine if relationships among variables were unique to the autism group, diagnosis was tested as a moderator in the whole sample. By testing the interaction between diagnosis and correlate (age, sex, NVDQ, and ADOS SA) a significant interaction would suggest that the slope of the relationship between the correlate and RBS-R score differed significantly among diagnostic groups.
Given that the Lam and Aman (2007) and Mirenda et al. (2010) algorithms were highly correlated, in order to limit the number of analyses and thereby control Type I error, one set was selected. In light of the validation of the Mirenda et al. (2010) algorithm in a younger sample of children with ASD, this set was included in the remaining analyses. The univariate general linear model used for these analyses allowed the simultaneous use of ANOVA and regression; categorical variables (diagnosis and sex) were entered as fixed factors and continuous correlates were entered as covariates (age, sex, NVDQ, and ADOS SA). To increase the interpretability of the interaction coefficients, all variables were standardized prior to analysis.
Longitudinal data
Within the longitudinal AUT sample (n = 39), change over time in the scores of the Mirenda et al. (2010) algorithm was tested using linear mixed models. Correlates of RRBs identified by other studies (age, sex, initial NVDQ, and ADOS SA) were evaluated as predictors of change where change was observed.
All statistical analyses were completed in the Statistical Package for the Social Sciences, Version 19.0 (SPSS Inc., 2010). Statistical significance was set at p < 0.01.
Results
Cross-Sectional Data
Means and standard deviations for the RBS-R subscales from both the Lam & Aman (2007) and Mirenda et al. (2010) algorithms are presented in Table 2. Using ANOVA, omnibus effects of diagnosis were observed on each of the RBS-R subscales. With respect to the Lam & Aman (2007) algorithm, the AUT group did not differ from PDD-NOS on any subscale, and both groups received significantly higher ratings than the TD group on all subscales [AUT versus TD ranged from d=0.67 (Self-Injurious Behavior) to d=2.05 (Stereotyped Behavior); PDD-NOS versus TD ranged from d=0.73 (Self-Injurious Behavior) to d=1.77 (Stereotyped Behaviors)]. Both AUT and PDD-NOS groups received significantly higher scores than the DD group on Compulsive Behavior (dAUT=0.55, dPDD=0.80), and Restricted Interests (dAUT=0.51, dPDD=0.77);on Stereotyped Behavior the AUT group received significantly higher scores than the DD group (d =0.92), but there was no significant difference between PDD-NOS and DD (d=0.55). There were no significant differences between the AUT and PDD-NOS groups and the DD group on the Self-Injurious Behavior and Ritualistic/Sameness subscales.
Table 2.
Mean Scores on the RBS-R Subscales and Factor Scores by Diagnostic Group for Cross-sectional Cohort
| AUT (n = 128) |
PDD-NOS (n = 46) |
DD (n = 44) |
TD (n = 59) |
F1 | |
|---|---|---|---|---|---|
| Lam & Aman (2007) Algorithm | |||||
| Stereotyped Behavior M ± SD | 8.90±4.94a | 7.33±5.80 a,b | 4.36±5.09b | 0.47±1.10c | 48.26 |
| Range (Min, Max) | (0, 23) | (0, 23) | (0, 26) | (0, 5) | |
| Self-Injurious Behavior M ± SD | 2.40±3.24a | 2.24±3.11a | 1.41±2.29a,b | 0.51±1.60b | 6.80 |
| Range (Min, Max) | (0, 16) | (0, 16) | (0, 10) | (0, 11) | |
| Compulsive Behavior M ± SD | 2.98±3.26a | 3.65±3.45a | 1.32±2.29b | 0.49±1.21b | 15.67 |
| Range (Min, Max) | (0, 15) | (0, 14) | (0, 10) | (0, 7) | |
| Ritualistic/Sameness Behavior M ± SD | 4.91±4.99a | 6.80±5.48a | 3.75±5.10a,b | 1.07±2.22b | 14.85 |
| Range (Min, Max) | (0, 23) | (0, 23) | (0, 21) | (0, 11) | |
| Restricted Behavior M ± SD | 2.95±2.55a | 3.37±2.32a | 1.73±1.97b | 0.54±0.90b | 21.43 |
| Range (Min, Max) | (0, 9) | (0, 8) | (0, 9) | (0, 4) | |
| Mirenda et al. (2010) Algorithm | |||||
| Repetitive Sensory Motor (RSM) M ± SD | 10.08±5.45a | 9.06±6.40a | 5.20±5.63a | 0.78±1.37b | 49.14 |
| Range (Min, Max) | (1, 25) | (1, 24) | (0, 29) | (0, 5) | |
|
| |||||
| Insistence on Sameness (IS) M ± SD | 12.63±10.85a,b | 15.59±11.13a | 7.64±10.31b,c | 2.81±4.33c | 19.45 |
| Range (Min, Max) | (0, 55) | (0, 55) | (0, 45) | (0, 19) | |
Note. AUT=autism; PDD-NOS=pervasive developmental disorder-not otherwise specified; DD=non spectrum developmental delay; TD=typical development. Superscripts denote means that differ significantly at p < 0.01.
The Mirenda et al. (2010) SIB subscale is identical to the Lam & Aman (2007) Self Injurious Behavior subscale and was therefore excluded.
Overall mean differs significantly at p < 0.01.
With respect to the Mirenda et al. (2010) algorithm, no differences were observed between AUT and PDD-NOS on the RSM (d=0.18) and IS subscales (d=-0.27); however, both groups had significantly higher scores than the TD group (RSM: dAUT=2.04, dPDD=1.92; IS: dAUT=1.06, dPDD=1.60). On the IS subscale, while the PDD-NOS group had significantly higher scores than the DD group (d=0.75), there were no significant differences between the AUT and DD groups (d=0.47).
The correlation matrix of RBS-R subscales with specific demographic variables found that within the AUT group only, the Ritualistic/Sameness and Restricted Behavior subscales and the RSM and IS subscales had small but significant positive correlations with age. No other correlations were significant (Table 3).
Table 3.
Correlates of RBS-R Subscale Scores, Autism Group Only (n = 128)
| Age, r(p) | Sex, t(1,126), p | NVDQ, r(p) | ADOS Social Affect, r(p) | |
|---|---|---|---|---|
| Lam & Aman (2007) Subscales | ||||
| Stereotyped Behavior | 0.22 (0.02) | 1.54, 0.13 | -0.21 (0.02) | 0.01 (0.92) |
| Self-Injurious Behavior | 0.20 (0.03) | 1.20, 0.23 | -0.08 (0.35) | -0.02 (0.85) |
| Compulsive Behavior | 0.09 (0.32) | 0.86, 0.39 | 0.17 (0.06) | -0.17 (0.052) |
| Ritualistic/Sameness | 0.29 (0.001)* | 0.69, 0.49 | -0.05 (0.59) | -0.13 (0.13) |
| Restricted Behavior | 0.23 (0.008)* | 0.75, 0.45 | -0.07 (0.45) | -0.17 (0.057) |
| Mirenda et al. (2010) Subscales | ||||
| RSM | 0.23 (0.009)* | 1.97, 0.05 | -0.19 (0.031) | -0.03 (0.73) |
| IS | 0.25 (0.004)* | 0.64, 0.52 | 0.03 (0.72) | -0.18 (0.049) |
p<0.01
Note: RSM = Repetitive Sensory Motor, IS = Insistence on Sameness, SIB = Self Injurious Behavior, NVDQ = Nonverbal Developmental Quotient, ADOS = Autism Diagnostic Observation Schedule.
The Mirenda et al. (2010) SIB subscale is identical to the Lam & Aman (2007) Self Injurious Behavior subscale and was therefore excluded.
Univariate GLM was used to test diagnosis as a moderator of the relationship among the putative correlates (age, sex, NVDQ, and ADOS SA) and the RSM, IS and SIB subscales. The goal was to determine if the relationship, or lack thereof, between a given variable and the subscales differed by diagnostic group. No significant interactions were observed; thus, diagnosis did not moderate the relationship between age, sex, NVDQ, or ADOS SA and the RBS-R subscale scores (Table 4).
Table 4.
Diagnosis as a Moderator of Relationship between Correlates and Mirenda et al. (2010) RBS-R Subscales
| Dependent Variable | Correlate | Correlate × Diagnosis Interaction F1 (p) |
|---|---|---|
| RSM | NVDQ | 0.61 (0.61) |
| Age | 2.52 (0.06) | |
| ADOS Social Affect | 0.75 (0.52) | |
| Sex | 2.38 (0.07) | |
| IS | NVDQ | 0.15 (0.93) |
| Age | 1.87 (0.14) | |
| ADOS Social Affect | 0.59 (0.62) | |
| Sex | 2.68 (0.05) | |
| SIB | NVDQ | 0.02 (0.99) |
| Age | 1.68 (0.17) | |
| ADOS Social Affect | 0.31 (0.82) | |
| Sex | 3.41 (0.02) |
Degrees of freedom associated with the F test for each of the correlates are as follows: NVDQ (3,277); Age (3,277); ADOS Social Affect (3,276); Sex (3, 277).
RSM = Repetitive Sensory Motor, IS = Insistence on Sameness, SIB = Self Injurious Behavior, NVDQ = Nonverbal Developmental Quotient, ADOS = Autism Diagnostic Observation Schedule.
Longitudinal Data
Using linear mixed-models, RBS-R subscale scores (RSM, IS, and SIB) were tested for change over time within the longitudinal AUT group (n = 39). Comparisons after two years (between Time 1 and 3), as well as comparisons between Time 1 and Time 2, and Time 2 and Time 3 were analyzed. No significant changes were observed between any of these time points. Table 5 provides means and standard deviations. Although analyses were planned to explore correlates of change, the stability in scores precluded this exercise.
Table 5.
Stability of RBS-R (Mirenda et al., 2010) over 2 years in AUT longitudinal cohort (n = 39)
| RBS-R Subscale | Visit 1 | Visit 2 | Visit 3 | F | p |
|---|---|---|---|---|---|
| RSM, M ± SD | 9.90 ± (4.22) | 9.10 ± (5.05) | 9.05 ± (5.34) | 0.60 | 0.55 |
| IS, M ± SD | 9.79 ± (6.61) | 9.82 ± (8.06) | 9.74 ± (8.54) | 0.002 | 1.00 |
| SIB, M ± SD | 1.82 ± (2.91) | 1.54 ± (2.80) | 2.00 ± (2.94) | 1.53 | 0.22 |
Note: RSM = Repetitive Sensory Motor, IS = Insistence on Sameness, SIB = Self Injurious Behavior.
Discussion
In the current study, we utilized two different algorithms of the RBS-R to analyze differences among diagnostic groups, and explored correlates and stability of RRBs in children. The goals of this study were to provide further validation that multiple domains of RRBs differentiate children with ASD from children with other developmental delays and typical development, and to explore implicated modifiers relative to particular aspects of RRBs both cross-sectionally and longitudinally. We hypothesized that children with ASD would have significantly higher scores than both non-spectrum developmentally delayed and typically developing children and that the correlates of gender, age, and cognitive ability would affect the presentation of RRBs. Additionally it was expected that children with fewer social-communication impairments would present with fewer RRBs. Finally, in our small sample of young children with autism, we expected that RRB s would remain stable over the course of two years. The purpose was not to evaluate the psychometric properties of the proposed RBS-R algorithms; thus, two proposed and validated algorithms, those of Lam and Aman (2007) and Mirenda et al. (2010) are discussed.
RRBs and Diagnosis
Consistent with prior research on RRBs (Kim & Lord, 2010; Honey et al, 2008), compared to typically developing children, children with ASD had significantly more RRBs as measured by the RBS-R. Interestingly, contrary to research that has found RRBs to be significantly different in children with autism compared to those with PDD-NOS (Mandy et al., 2011; Matson, Dempsey & Fodstad, 2009), none of the types of RRBs measured by the RBS-R distinguished these groups in the present sample. This may, in part, relate to the relatively small sample sizes of PDD-NOS groups that may be quite heterogeneous with respect to symptom profiles. For example, in the Mandy et al. study (2011), very few participants with PDD-NOS had RRBs, while the majority of participants had social and communication impairments. In the current sample, children in the PDD-NOS group met criteria for at least one symptom of RRB that are described in the autism criteria of the DSM-IV-TR (APA, 2000).
Some differences in RRBs were observed between the ASD and non-spectrum developmentally delayed groups. However, mean score differences depended upon the type of RRB as well as the particular diagnosis (autism or PDD-NOS). When considering the Lam and Aman (2007) subscales in our entire sample, only two of the five subscales, Compulsive Behavior and Restricted Behavior, differentiated children with autism or PDD-NOS from non-spectrum developmentally delayed children. While children with PDD-NOS did not differ from those with non-spectrum developmental delays on the Stereotyped Behavior subscale, children with autism did.
In the current sample, mean scores for children with ASD appear to be less severe on all subscales of the RBS-R than scores previously reported for children 3-12 years old with ASD in the Lam and Aman (2007) study. The only exception was on the Stereotyped Behavior subscale. Comparing the current results to the Bishop et al. (2012) study, mean scores for Self-Injurious behavior and Restricted Interests were similar. However, in the current study, scores on the Stereotyped Behavior subscale were more severe than the Sensory Motor scores (which included the items on the Stereotyped Behavior subscale and one item from the Restricted Interests subscale) in the Bishop et al. (2012) study.
With respect to the Mirenda et al. (2010) subscales, while autism and PDD-NOS groups were reported to both have significantly higher RSM (stereotyped and restricted behaviors) than typically developing children, they did not differ from one another. The IS subscale (compulsive, ritualistic and sameness behaviors) also did not differ between autism and PDD-NOS groups. On the IS subscale, the PDD-NOS group (but not the autism group) differed significantly from the non-spectrum developmental delay group; both ASD groups had significantly higher scores than typically developing peers. Given this pattern of group differences across the subtypes of RRB, past research indicating diagnostic specificity of RRBs is partially supported (Kim & Lord, 2010; Bodfish et al.,2000). In this study, as it has been for past research, the relationship between IS behaviors and their specificity to ASD versus to general cognitive ability was difficult to disentangle. A relationship between the role of cognitive functioning and some types of IS behaviors have been reported (Bishop et al, 2006), however some types of RRBs conceptualized as IS behaviors in this and other studies have not been found to be strongly associated with cognitive functioning (Bishop et al, 2012). The ways in which these behaviors are conceptualized on different measures may play a role in the associations found with other variables.
Correlates and Influence of Demographic Factors
Unlike other studies, we were unable to substantiate relationships between RRBs and NVDQ, age, social communication, or sex in our autism sample. The roles of NVDQ and age in other studies compared to the current study are important to address. While the Stereotyped Behavior subscale scores in the current sample were more severe compared to Bishop et al. (2012), it is of note that the current sample had a mean NVDQ that was approximately 20 points lower. Given that stereotyped behaviors have consistently been shown to correlate with lower NVDQ (Bishop et al., 2012; Richler et al., 2010; Cuccaro et al., 2003), it is possible that the reduced range of NVDQ in this study contributed to the failure to find a relationship between NVDQ and stereotyped behaviors in this study. Gabriels et al. (2005) found that sameness behaviors on the RBS-R were inversely related with cognitive function, which was not supported in the current study. However, the dichotomization of NVIQ (NVIQ ≥ 97 versus NVIQ ≤ 56) and the very small sample size (n = 14) do limit the interpretation and generalization of the Gabriels et al. (2005) results.
Findings regarding age have differed across studies; this may depend on several factors including the age range studies have used and the age at assessment. This cohort had a purposefully restricted age range (2-11 years), with 80% of the sample between the ages of 2 and 4 years. Previous studies that have found relationships between RRBs and age have had a wider distribution of age: 4 to 18 years (Bishop et al., 2012), 3 to 43 years (Lam & Aman, 2007), and 2 to 62 years (Esbensen et al., 2009). In the Lam and Aman (2007) study, scores on the Ritualistic/Sameness Behavior subscale were appreciably higher than in the current sample, with mean scores in that cohort ranging from 10.2 in their 6-12 year age group to 11.4 in their 3-5 year age group. Similarly, scores on this subscale were also lower in the current study than for children in the samples reported by Esbensen et al. (2009) and in the sample reported by Bishop et al. (2012). In both the Richler et al. (2010) and Bishop et al. (2012) studies, these behaviors were reported to increase with age.
The Ritualistic/Sameness Behavior subscale includes behaviors that are considered “higher order” RRBs. The studies that have found relationships with age (Bishop et al., 2012; Lam & Aman, 2007) included older children, which may have contributed to the differences in scores on this subscale. In the Lam and Aman (2007) study, approximately 10% of the sample was under the age of 5 years, while in the current sample, 76% of the sample was under 5 years. While RRBs are observed in typically developing 2 year olds (Leekam et al., 2007), findings from the present cohort suggest that for children with ASD, these specific types of Ritualistic/Sameness behaviors may not present as frequently in younger children. Interestingly, in a sample of toddlers (younger than 12 months to 56 months), Kim and Lord (2010) found RRBs to be independent of age for children with ASD. These differences highlight that RRBs may have a different presentation in young children compared to older children. The short-term trajectory among young children with ASD may also differ in younger children.
Previous studies have substantiated the effect of sex on RRBs in young children (Lord & Kim, 2010; Mandy et al., 2012) and in adults (Hattier et al., 2011). Like other correlates, sex has not been determined to be a stand-alone construct in predicting and explaining RRBs. Other data do suggest that NVIQ is related to sex differences in RRBs (Sipes et al, 2011), so the effect of sex on RRB presentation may be complex and beyond the scope of the current study.
RRBs Over Time
The results of the longitudinal portion of this study suggest that a broad range of repetitive behaviors are stable over a relatively short time period in children with autism between the ages of 2 and 7. These findings are consistent with Kim and Lord (2010), who also found that RRBs, as measured by the ADOS, were stable in young children. However, other studies have suggested somewhat less stability over time. Honey et al. (2008) found that in young children (24 -48 months), ADI-R RRB algorithm scores were stable over 1 year; however, when all available ADI-R RRB items were analyzed, RRBs improved (decreased) across time. In another study, Richler et al. (2010) found that RSM decreased and IS increased over time (a period of 7 years). Several factors may account for these discrepant findings, such as the measure(s) used to examine RRBs, differences in samples (age, diagnostic groups, etc.), and differences in the length of time RRBs were measured. Furthermore, there is evidence suggesting that different trajectories exist for children within ASD. A recent study by Gotham et al. (2012), examining the course of ASD symptoms over 10 years in children suggests that while some children exhibited worsening symptoms, others showed a more stable pattern or improvement over time.
Limitations
We examined the relationship among previously reported associated factors and RRBs in children with ASD, including the impact of NVDQ. Without knowing more about the nature of change in RRBs in typically developing children, we determined it made best sense to use chronologically age-matched typically developing controls. This resulted in a significant difference in NVDQ between the ASD and TD groups. We thus used a non-spectrum developmentally delayed group as an NVDQ control group in an attempt to understand the presentation of RRBs without the effect of NVDQ. This study design does provide information on how these behaviors present in children with delays, but as our age-matched TD group had significantly higher NVDQ, the paper does not address the presentation of RRBs in typically developing children with similar nonverbal mental ages.
This study is one of few to assess the trajectory of RRBs in children with autism; however, due to the relatively small sample size of those included in the longitudinal analysis, generalizability is limited. Further, the length of this study may have been insufficient to observe change in RRBs; as noted above, one of the studies that did report change over time in RRBs utilized observations over 7 years (Richler et al., 2010). To further understand the trajectory of RRBs in children with autism, it will be important to understand how these behaviors change in non-spectrum developmentally delayed children, as well as in typically developing children, over the preschool-age period. Future studies using this measure should examine these behaviors at regular intervals over a longer period of time in ASD and in children with non-spectrum developmental delays as well as typically developing children.
Conclusions
The current study adds to the growing literature on the importance of RRBs as a core feature of ASD that differentiates children with ASD, even from children who are similarly cognitively delayed, at young ages. This study failed to replicate relationships among some phenotypic variables and RRBs that have been found in other studies; importantly, this study points to the usefulness of the RBS-R in distinguishing some types of RRBs in young children with ASD compared to children with non-spectrum developmental delays. Future research in larger samples will be important in clarifying these findings. The same is true for the study of change in RRBs over time; larger samples followed over longer periods of time will help to contextualize the current findings in the field.
Acknowledgments
This research was supported by the Intramural Program of the National Institute of Mental Health (NIMH). The views expressed in this article do not necessarily represent the views of the NIMH, NIH, HHS, or the United Stated Government. The authors extend our gratitude for the children and their families who volunteered their time and efforts during this research.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Arnott B, McConachie H, Meins E, Fernyhough C, Couteur AL, Turner M, Leekam S, et al. The frequency of restricted and repetitive behaviors in a community sample of 15-month-old infants. Journal of Developmental and Behavioral Pediatrics. 2010;31(3):223–229. doi: 10.1097/DBP.0b013e3181d5a2ad. [DOI] [PubMed] [Google Scholar]
- Barber AB, Wetherby AM, Chambers NW. Brief report: Repetitive behaviors in young children with autism spectrum disorder and developmentally similar peers: A follow up to Watt et al. (2008) Journal of Autism and Developmental Disorders. 2012;42(9):2006–2012. doi: 10.1007/s10803-011-1434-3. [DOI] [PubMed] [Google Scholar]
- Bishop SL, Hus V, Duncan A, Huerta M, Gotham K, Pickles A, Kreiger A, Buja A, Lund S, Lord C. Subcategories of restricted and repetitive behaviors in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012 doi: 10.1007/s10803-012-1671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SL, Richler J, Lord C. Association between restricted and repetitive behaviors and nonverbal IQ in children with autism spectrum disorders. Child Neuropsychology. 2006;12(4-5):247–267. doi: 10.1080/09297040600630288. [DOI] [PubMed] [Google Scholar]
- Bodfish JW, Symons FJ, Parker DE, Lewis MH. Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of Autism and Developmental Disorders. 2000;30(3):237–243. doi: 10.1023/a:1005596502855. [DOI] [PubMed] [Google Scholar]
- Charman T, Taylor E, Drew A, Cockerill H, Brown JA, Baird G. Outcome at 7 years of children diagnosed with autism at age 2: predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry. 2005;46(5):500–513. doi: 10.1111/j.1469-7610.2004.00377.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Erlbaum; 1988. [Google Scholar]
- Cuccaro ML, Shao Y, Grubber J, Slifer M, Wolpert CM, Donnelly SL, Pericak-Vance MA, et al. Factor analysis of restricted and repetitive behaviors in autism using the Autism Diagnostic Interview-R. Child Psychiatry and Human Development. 2003;34(1):3–17. doi: 10.1023/a:1025321707947. [DOI] [PubMed] [Google Scholar]
- Elliott C. Differential Ability Scales. 2. San Antonio: Harcourt Assessment; 2007. [Google Scholar]
- Esbensen AJ, Seltzer MM, Lam KS, Bodfish JW. Age-related differences in restricted repetitive behaviors in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(1):57–66. doi: 10.1007/s10803-008-0599-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DW, Leckman JF, Carter A, Reznick JS, Henshaw D, King RA, Pauls D. Ritual, habit, and perfectionism: the prevalence and development of compulsive-like behavior in normal young children. Child Development. 1997;68(1):58–68. [PubMed] [Google Scholar]
- Gabriels RL, Cuccaro ML, Hill DE, Ivers BJ, Goldson E. Repetitive behaviors in autism: Relationships with associated clinical features. Research in Developmental Disabilities. 2005;26(2):169–181. doi: 10.1016/j.ridd.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(5):693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Pickles A, Lord C. Trajectories of autism severity in children using standardized ADOS scores. Pediatrics. 2012;130(5):1278–1284. doi: 10.1542/peds.2011-3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattier MA, Matson JL, Tureck K, Horovitz M. The effects of gender and age on repetitive and/or restricted behaviors and interests in adults with autism spectrum disorders and disability. Research in Developmental Disabilities. 2011;32(6):2346–2351. doi: 10.1016/j.ridd.2011.07.028. [DOI] [PubMed] [Google Scholar]
- Honey E, McConachie H, Randle V, Shearer H, Couteur AS. One-year change in repetitive behaviours in young children with communication disorders including autism. Journal of Autism and Developmental Disorders. 2008;38(8):1439–1450. doi: 10.1007/s10803-006-0191-1. [DOI] [PubMed] [Google Scholar]
- Kim SH, Lord C. Restricted and repetitive behaviors in toddlers and preschoolers with autism spectrum disorders based on the Autism Diagnostic Observation Schedule (ADOS) Autism Research. 2010;3(4):162–173. doi: 10.1002/aur.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Lord C. New autism diagnostic interview-revised algorithms for toddlers and young preschoolers from 12 to 47 months of age. Journal of Autism and Developmental Disorders. 2012;42(1):82–93. doi: 10.1007/s10803-011-1213-1. [DOI] [PubMed] [Google Scholar]
- Lam KS, Aman MG. The Repetitive Behavior Scale-Revised: independent validation in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37(5):855–866. doi: 10.1007/s10803-006-0213-z. [DOI] [PubMed] [Google Scholar]
- Lam KS, Bodfish JW, Piven J. Evidence for three subtypes of repetitive behavior in autism that differ in familiality and association with other symptoms. Journal of Child Psychology and Psychiatry. 2008;49(11):1193–1200. doi: 10.1111/j.1469-7610.2008.01944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leekam S, Tandos J, McConachie H, Meins E, Parkinson K, Wright C, Le Couteur A, et al. Repetitive behaviours in typically developing 2-year-olds. Journal of Child Psychology and Psychiatry. 2007;48(11):1131–1138. doi: 10.1111/j.1469-7610.2007.01778.x. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Archives of General Psychiatry. 2006;63(6):694–701. doi: 10.1001/archpsyc.63.6.694. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Rutter M, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Mandy W, Charman T, Gilmour J, Skuse D. Toward specifying pervasive developmental disorder-not otherwise specified. Autism Research. 2011;4(2):121–131. doi: 10.1002/aur.178. [DOI] [PubMed] [Google Scholar]
- Mandy W, Chilvers R, Chowdhury U, Salter G, Seigal A, Skuse D. Sex differences in autism spectrum disorder: evidence from a large sample of children and adolescents. Journal of Autism and Developmental Disorders. 2012;42(7):1304–1313. doi: 10.1007/s10803-011-1356-0. [DOI] [PubMed] [Google Scholar]
- Matson JL, Dempsey T, Fodstad JC. Stereotypies and repetitive/restrictive behaviours in infants with autism and pervasive developmental disorder. Developmental Neurorehabilitation. 2009;12(3):122–7. doi: 10.1080/17518420902936730. [DOI] [PubMed] [Google Scholar]
- Mirenda P, Smith IM, Vaillancourt T, Georgiades S, Duku E, Szatmari P, Zwaigenbaum L, et al. Validating the Repetitive Behavior Scale-revised in young children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2010;40(12):1521–1530. doi: 10.1007/s10803-010-1012-0. [DOI] [PubMed] [Google Scholar]
- Mooney EL, Gray KM, Tonge BJ, Sweeney DJ, Taffe JR. Factor analytic study of repetitive behaviours in young children with Pervasive Developmental Disorders. Journal of Autism and Developmental Disorders. 2009;39(5):765–774. doi: 10.1007/s10803-008-0680-5. [DOI] [PubMed] [Google Scholar]
- Moore V, Goodson S. How well does early diagnosis of autism stand the test of time? Follow-up study of children assessed for autism at age 2 and development of an early diagnostic service. Autism. 2003;7(1):47–63. doi: 10.1177/1362361303007001005. [DOI] [PubMed] [Google Scholar]
- Mullen E. Mullen scales of early learning. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- Richler J, Bishop SL, Kleinke JR, Lord C. Restricted and repetitive behaviors in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37(1):73–85. doi: 10.1007/s10803-006-0332-6. [DOI] [PubMed] [Google Scholar]
- Richler J, Huerta M, Bishop SL, Lord C. Developmental trajectories of restricted and repetitive behaviors and interests in children with autism spectrum disorders. Developmental Psychopathology. 2010;22(1):55–69. doi: 10.1017/S0954579409990265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. Manual for the Social Communication Questionnaire. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Rutter M, LeCouteur A, Lord C. Autism Diagnostic Interview Revised WPS. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Sipes M, Matson JL, Worley JA, Kozlowski AM. Gender differences in symptoms of Autism Spectrum Disorders in toddlers. Research in Autism Spectrum Disorders. 2011;5:1465–1470. [Google Scholar]
- SPSS Inc. SPSS Version 19. 0 for Windows. Chicago: SPSS Inc; 2010. [Google Scholar]
- Stone WL, Lee EB, Ashford L, Brissie J, Hepburn SL, Coonrod EE, Weiss BH. Can autism be diagnosed accurately in children under 3 years? Journal of Child Psychology and Psychiatry. 1999;40(2):219–226. [PubMed] [Google Scholar]
- Turner M. Unpublished doctoral thesis. University of Cambridge; UK: 1995. Repetitive behaviour and cognitive functioning in autism. [Google Scholar]
- Turner M. Annotation: Repetitive behaviour in autism: a review of psychological research. Journal of Child Psychology and Psychiatry. 1999;40(6):839–849. [PubMed] [Google Scholar]