Abstract
Purpose
Emergency endotracheal intubation (EEI) is a complex process that leads to various complications. Previous studies mainly demonstrated that the Medical Emergency Team (MET) intervention reduced the incidence of cardiac arrest, however, the impact of a MET on airway management has not been investigated in detail. Our purpose was to confirm the impact of a MET on airway management and compare the incidence of complications of EEI before and after MET intervention in a general ward.
Materials and Methods
We performed an observational study and reviewed 318 patients intubated by a MET in a general ward.
Results
The patients enrolled during the control (2007) and study (2009) periods were 103 and 215, respectively. Cardiopulmonary resuscitation requiring emergency intubation in a general ward was reduced after MET intervention at the Asan Medical Center (39.8% vs. 19.1%, p<0.001). Pre-intubation and post-intubation oxygen saturation levels were higher after MET intervention (pre-intubation, 80% before vs. 92% after MET, p<0.001; post-intubation, 95% before vs. 99% after MET, p<0.001). The use of vasopressors after intubation decreased as a result of MET intervention (62.1% before vs. 36.7% after MET, p<0.001). Hypotension was also reduced (34% before vs. 8.8% after MET, p<0.001).
Conclusion
Early interventions of a MET changed the causes of emergency intubation in a general ward from cardiopulmonary resuscitation to respiratory distress or shock and improved hypoxemia and hypotension related to emergency intubation. The MET intervention is safe and effective system for emergency intubation in a general ward.
Keywords: Emergency medical service, cardiopulmonary resuscitation, intubation, intratracheal, airway management
INTRODUCTION
Hospitalized patients are at risk for adverse events such as unexpected cardiac arrest or respiratory failure and admission to an Intensive Care Unit (ICU). Among these, critically ill patients often require emergency endotracheal intubation (EEI) for airway control due to respiratory distress, shock, or cardiac arrest,1 and they frequently have airway difficulties. In one prospective study, the most common reasons for intubation were a patient's inability to preserve their own airway (70%), the presence of brain injury (54%), and poor oxygenation with ventilation (26%).2 EEI is a complex process with many potential factors that lead to failure. Several studies reported that EEI in the ICU is associated with a high incidence of complications such as hypotension and severe hypoxemia ranging from 25 to 39%,1,3 and that EEI in general ward is associated with multiple (i.e., >2 intubations) insertion attempts and esophageal intubation occurring in 27% of cases.1,4,5 Furthermore, critically ill patients have limited or suboptimal responses to pre-oxygenation, and high susceptibility to hypotension and hypoxemia, and demonstrate a high incidence of difficult airways.1,6
The medical emergency team (MET) was established to facilitate emergency care for patients who may progress to respiratory distress or cardiac arrest. Several studies have suggested that early intervention by a MET is associated with improved patients' outcomes such as a reduced ICU admission rate, incidence of unexpected in-hospital cardiac arrest, and mortality rate.7-9 While the published studies thus far mainly demonstrated the positive effect of a MET intervention in reducing the incidence of cardiac arrest, the effect of a MET in airway management has not yet been investigated in detail.
We postulated that the MET intervention would decrease the incidence of complications related to EEI in a general ward. Our aims in this study were to compare the incidence of immediate complications of EEI before and after MET intervention and demonstrate an association between MET intervention and mortality.
MATERIALS AND METHODS
Study setting and population
The study was approved by our institutional review board which waived informed consent (IRB No. 2011-0616).
Of all patients who were admitted to the hospital ward during the control and study periods, adult patients 18 years or older who underwent EEI by a MET intervention were enrolled in the study. Any patients intubated in the ICU, operating room, and the emergency unit were excluded. We reviewed 318 patients enrolled from our hospital's electronic medical records and obtained relevant information regarding MET intervention in 2007 and 2009.
We performed an observational study to show the effects of a MET intervention. The data were collected retrospectively from March to August, 2007 (a six-month "before MET intervention" period) and prospectively from March to August, 2009 (a six-month "after MET intervention" period). A preparation and education period, from March to August, 2008, was excluded.
Hospital setting
The Asan Medical Center is a teaching hospital affiliated with the University of Ulsan and is a tertiary care hospital in Seoul. As of 2010, the hospital has 2680 beds, more than 10000 inpatients per day, approximately 904000 patient admissions per year, and 58000 surgical procedures performed annually, 5700 of them being highly difficult surgical procedures.
The Medical Emergency Team and protocol
The MET system was introduced in March, 2008 at the Asan Medical Center (named the Medical Alert Team, MAT). The MET was composed of pulmonary/critical care attending physicians and fellows, junior or senior residents, and critical care nurses. The MET was available 24 hours a day via pager and could be summoned by any member of the hospital staff who may be concerned about the management of critically ill patients in a general ward. A list of criteria for MET intervention was provided in all clinical units (Table 1).
Table 1.
Criteria for Calling Medical Emergency Team
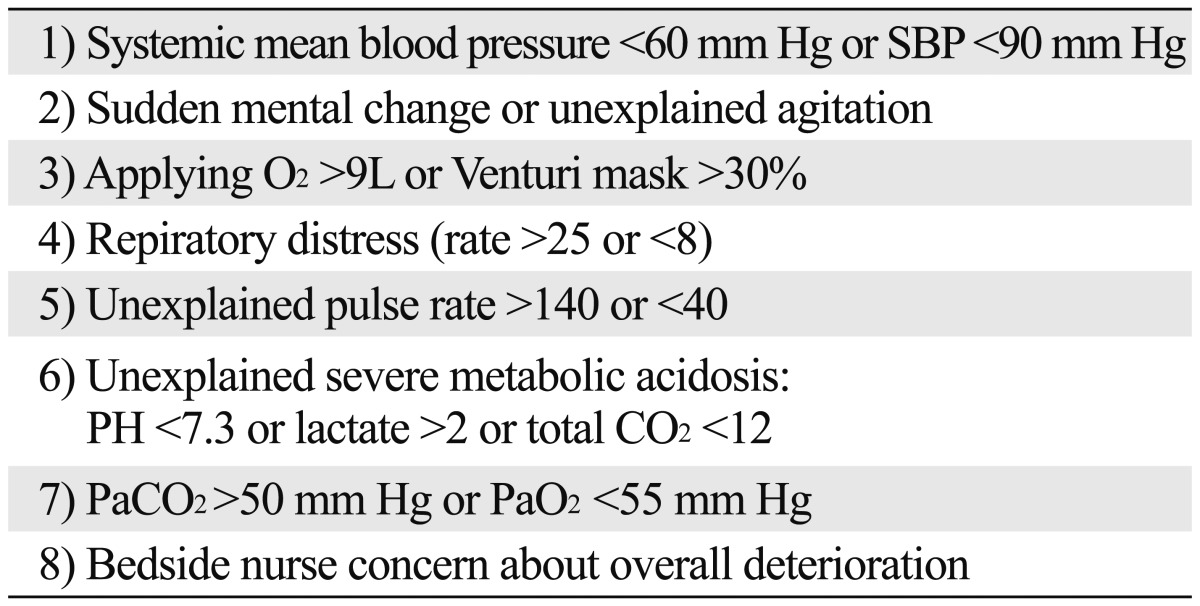
SBP, systolic blood pressure; PH, hydrogen ion concentration; CO2, carbon dioxide; PaCO2, arterial carbon dioxide tension; PaO2, partial pressure of oxygen in arterial blood.
Also, the MET nurses reviewed the Medical Alarm System (MAS), a screening system which presented predefined abnormalities of vital signs or clinical parameters, and recorded them on a computer in real time for 24 hours. The MET triggered by the MAS performed critical care intervention, and the MET staff reviewed the data in regular meetings.
Definitions and variables
Characteristics of patients
We collected information on the demographics and the clinical characteristics of the patients, such as age, gender, Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission, previous underlying disease, and admission department.
Procedure parameters
The MET nurses recorded the data prospectively, including the location of intubation, reasons for intubation, the number of intubation attempts, the use of adjuvant device, medications and complications during intubation. Also, data before and after MET intervention from the hospital's electronic medical records were recorded. The following parameters within 60 minutes of pre- and post-endotracheal intubation were documented: systolic blood pressure, oxygen saturation, partial pressure of oxygen in the arterial blood (PaO2), the fraction of inspired oxygen (FiO2), and the use of vasopressors.
We defined the reasons for EEI as respiratory distress (dyspnea with arterial desaturation <90%), shock (systolic blood pressure <90 mm Hg), cardiopulmonary resuscitation (CPR), and mental change. Clinical outcomes were defined as hospital mortality, ICU mortality, length of stay in the ICU, and the duration of mechanical ventilation.
Difficulty in airway management can be divided into difficult mask ventilation (DMV) and difficult tracheal intubation (DTI). DMV is defined as the inability of a trained anesthetist to maintain the oxygen saturation above 90% using face-mask ventilation. DTI is defined as the inability to place an endotracheal tube within 10 min or after three attempts.10 The MET used a modified rapid sequence intubation (RSI) process, which is called "Facilitated intubation", RSI refers to the use of a sedative only without neuromuscular blocker (NMB) to assist with intubation.11
We used the "LEMON" method for airway assessment that was composed of four "look" criteria, three "evaluate" criteria, Mallampati classification, the presence of airway obstruction, and neck mobility. In principle, the airway assessment score is 0-10 if Mallampati classification is recorded. But, because "Mallampati classification" is both difficult to assess and a poor predictor of intubation grade in an emergency situation, the airway assessment score is practically 0-9. The "look" criteria is composed of the presence of facial trauma, large incisors, beard or moustache, and large tongue. The "evaluate" criteria have the 3-3-2 rule which allows alignment of pharyngeal, laryngeal and oral axes. The 3-3-2 rule is composed of inter-incisor distance, hyoid mental distance, and thyroid to floor of mouth in fingers. The Mallampati classification is used for assessing the degree of hypopharynx visible. The Neck mobility is a vital requirement for successful intubation, and it is assessed easily by getting the patient to place their chin down onto their chest and then to extend their neck so they are looking towards the ceiling.
Immediate intubation-related complications
The immediate complications occurring within 30 minutes after endotracheal intubation were defined as hypotension (systolic blood pressure <90 mm Hg recorded at least once or persisting despite vascular loading or use of inotropics), esophageal intubation, tooth extraction (dental injury), bleeding, aspiration of gastric contents, and arrhythmia.
Statistical analysis
We used SPSS 18.0 program (SPSS Inc., Chicago, IL, USA) to analyze the data of 318 patients. Continuous variables were expressed in terms of the median (range) because they were not normally distributed. Categorical variables were expressed as numbers (percentages). Differences among the continuous groups were compared using the Student's t-tests or the Mann-Whitney U test, and thoses among the categorized groups were compared using either the chi-square test or Fisher's exact test. In statistical testing, two-sided p<0.05 was considered statistically significant.
RESULTS
In this study, there were 103 and 215 patients enrolled before and after MET intervention, respectively. The median patient ages were 67 (25-90) years and 64 (17-91) years, and there were 66 (64%) and 143 (67%) male patients before and after MET intervention, respectively. The APACHE II score and the number of patients with previous underlying diseases were similar in both groups (Table 2). The Admission Department for patients who experienced EEI varied. More patients were seen in the Internal Medicine (IM) Department after MET intervention than before it (72.6% after vs. 58.3% before MET, p=0.011).
Table 2.
Baseline Characteristics of Study Patients
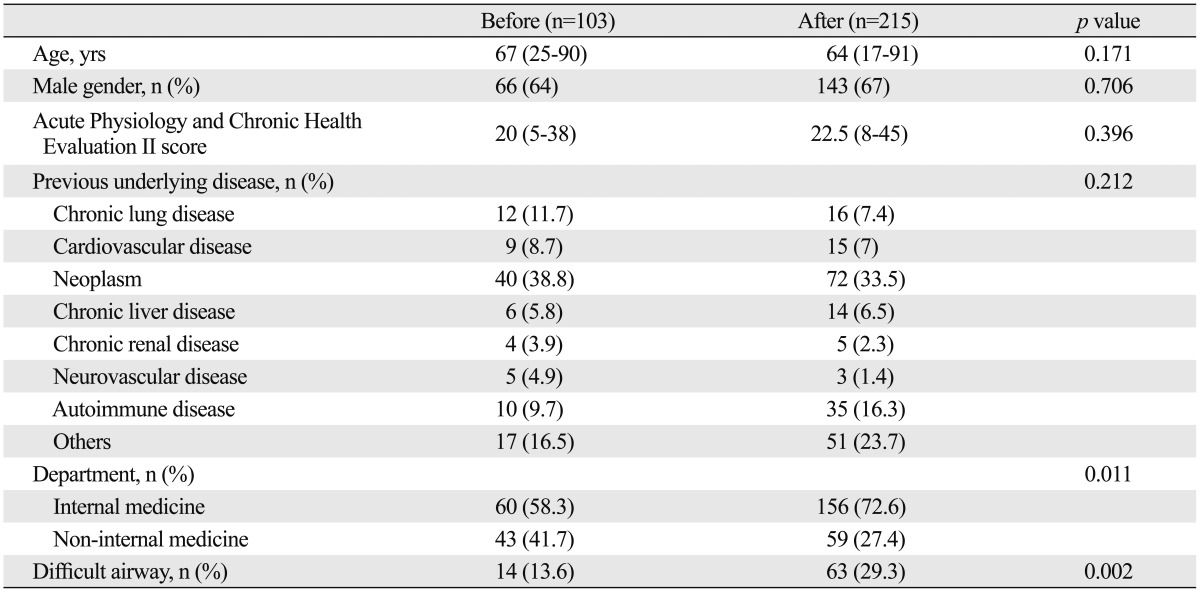
Values are presented as median (range) or number (%) unless otherwise indicated.
Pre-intubation and post-intubation oxygen saturation levels were higher after MET intervention than before it (pre-intubation, 80% before vs. 92% after MET, p<0.001; post-intubation, 95% before vs. 99% after MET, p<0.001). The use of vasopressors after intubation was decreased as a result of a MET intervention (62.1% before vs. 36.7% after MET, p<0.001) (Table 3).
Table 3.
Physiologic Parameters before- and after-Medical Emergency Team Intervention
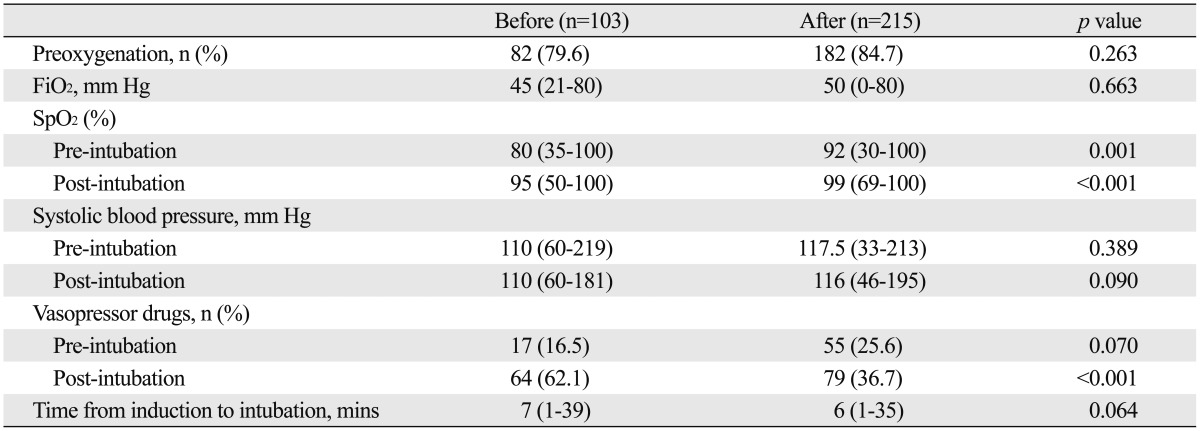
FiO2, fractional inspired oxygen concentration; SpO2, Pulse Oximeter Oxygen Saturation.
Values are presented as median (range) or number (%) unless otherwise indicated.
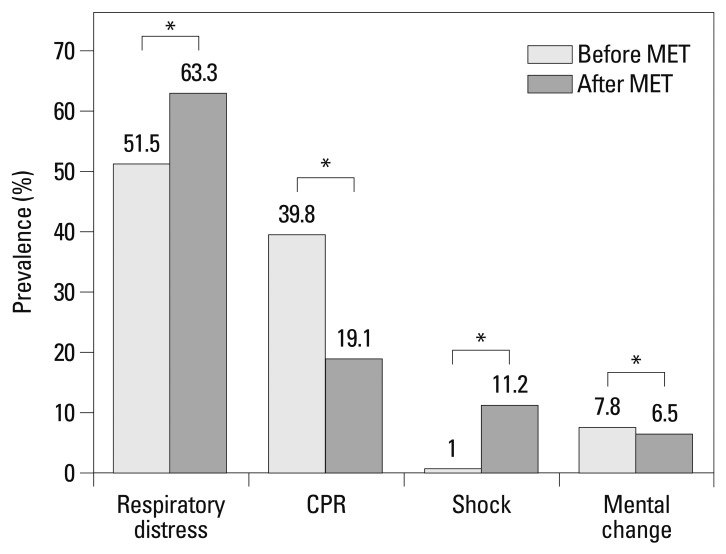
The presence of difficult airway, respiratory distress, and shock were higher after MET intervention than before it (difficult airway, 13.6% before vs. 29.3% after MET, p=0.002; respiratory distress, 51.5% before vs. 63.3% after MET, p< 0.001; shock, 1% before vs. 11.2% after MET, p<0.001). However, the incidence of CPR as a cause for EEI and complications caused by intubation diminished after MET intervention (CPR, 39.8% before vs. 19.1% after MET, p<0.001; complications, 41.7% before vs. 18.1% after MET, p<0.001) (Fig. 1). Also, the rate of immediate intubation-related complications was reduced after MET intervention (41.7% before vs. 18.1% after MET, p<0.001).
Fig. 1.
Reasons for emergency intubation by a MET (*p<0.001). The causes of emergency intubation in a general ward changed from CPR to respiratory distress or shock by early intervention of a MET. The incidence of CPR was reduced, whereas the incidence of respiratory distress or shock increased. MET, Medical Emergency Team; CPR, cardiopulmonary resuscitation.
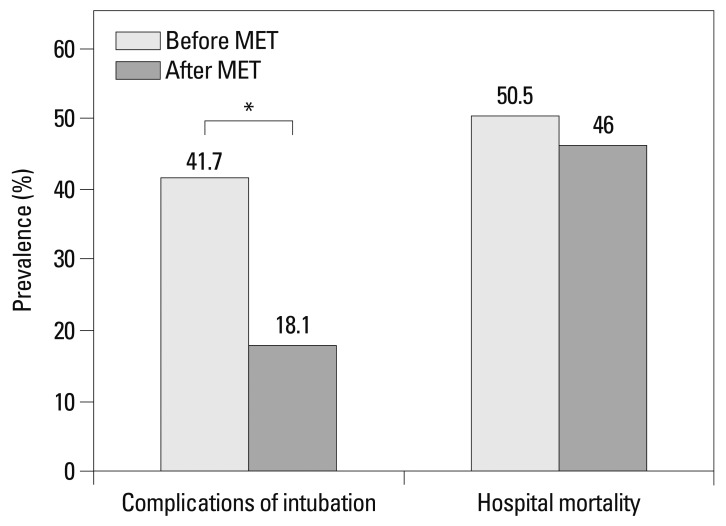
Although statistical significance was not shown, the time from induction to intubation was reduced after MET intervention (7 minutes before vs. 6 minutes after MET, p=0.064), whereas, in-hospital or ICU mortality rates were not affected by a MET intervention (Fig. 2).
Fig. 2.
Outcomes before and after MET intervention (*p<0.001). There were no statistically significant differences in outcomes such as complications of intubation and hospital mortality rate. MET, Medical Emergency Team.
DISCUSSION
In the present study, we showed that MET intervention along with a computerized screening program reduced the incidence of CPR as a cause of EEI and complications related to EEI. Early intervention by a MET detected critically ill patients suffering from respiratory distress or shock in its early stage and managed them before respiratory or cardiac arrest. As a result, the incidence of respiratory distress or shock decreased. Intubation-related complications, hypoxemia and hypotension were reduced after MET intervention. Critically ill patients who need EEI have little cardiopulmonary reserve, and need critical care intervention due to less effective pre-oxygenation. The MET provided preoxygenation by using devices such as noninvasive ventilation or high-flow nasal cannula and early intubation. Furthermore, the MET provided critically ill patients with early goal-direct therapy, and early intervention of a MET enabled hemodynamics to stabilize. As a result, the early intervention by a MET played an important role in airway management of critically ill patients in a general ward.
While a controversy exists as to whether MET improves outcomes, several studies have shown a favorable effect on patient outcomes after MET intervention.7-9 These studies reported that MET intervention was associated with a reduction in-hospital cardiac arrest and unplanned ICU admission. However, only a few studies advocated the MET intervention for airway management. One study showed that pediatric MET was associated with a significant decrease in the incidence of respiratory arrest in a general ward,12 and another study showed that intervention by the Medical Emergency Response Team, a part of the British Military's trauma system, and advanced airway management including RSI increased survival in the peri-evacuation phase.13 Moreover, our present study demonstrated an association with MET intervention and improvements of various physiologic parameters in critically ill adult patients during airway management.
First, the incidence of CPR requiring EEI in a general ward was reduced after MET intervention. The number of unexpected cardiac arrest occuring due to respiratory distress was reduced because a MET was able to identify patients undergoing respiratory distress or shock at an early stage and provided proper airway management.
Second, hypoxemia, a common intubation-related complication, was reduced after MET intervention both pre- and post-intubation. The MET provided early and tailored respiratory management such as diuretics, bronchodilators, application of noninvasive ventilation and high-flow nasal cannula to patients with respiratory distress. As a result, the baseline FiO2 and the percent of preoxygenation were not different between the two groups, however, the oxygen saturation of pre- and post-intubation was improved, and early intubation was achieved before an impending respiratory arrest. Furthermore, proper use of rescue devices such as Video Laryngoscope reduced hypoxemia in patients with difficult airway. In one study, the most common documented medical reason for intubation by a MET was respiratory distress.14 Critically ill patients have a lower threshold to tolerate the interruption of oxygen delivery.6,15 According to a study, the time up to de-saturation below 85% is shortened to 23 seconds in critically ill patients compared to 502 seconds in healthy adults.16 Mort's study showed that standard pre-oxygenation methods were ineffective in patients with cardiopulmonary failure before EEI, whereas pre-oxygenation in patients who required only EEI for airway protection was unproblematic.6,15
Third, hypotension, the most common intubation-related procomplication, was reduced after MET intervention. Although the use of inotropics in post-intubation decreased, it is important that the pre-and post-intubation systolic blood pressure showed no statistically significant difference between the two groups. The pre-emptive system of a MET paved the way for early detection and early intervention, as early goal-directed therapy could decrease the use of vasopressors.
Fourth, through a well-trained team approach and a systematized intubation protocol, our study allowed the intubation to be carried out under close supervision. Junior residents were under the supervision of senior residents. In our intubation protocol, critical care physicians backed junior or senior residents up in every condition that initial intubation failed. Jaber, et al.3 noted that the complication rate was lower when a junior and a senior resident were working together. The presence of acute respiratory distress and shock as an indication for EEI were independent risk factors for complications, whereas supervision by a senior resident showed a protective effect.3 Highly skilled airway management is necessary in order to avoid adverse outcomes of intubation such as esophageal intubation.17 Martin, et al.18 observed a 16.9% of complication rate in patients managed by junior residents when compared with a 4.2% of complication rate by senior residents, and emphasized that the experience of initial responder to emergency airway situations may be responsible for the outcomes.
Our study implemented a modified RSI protocol. Previous studies documented the utilization of NMB from 5 to 62% of intubation.3,4 In our study, with the exception of 5 (2.3%) patients, all EEIs were performed without NMB. One study showed that intubation without NMB was also sufficiently safe and had a high success rate of 76%.4,19 In our study, because the first intubation attempt was by residents in a general ward, the use of NMB should be avoided. In a study, the first attempt intubation success rate by Internal Medicine residents was found to be low compared with 83% for Emergency Medicine residents.20 Some researchers have advocated that the use of NMB may lead to catastrophic situations in which a difficult airway can be anticipated.11
Some limitations in our study are considered. First, it was a retrospective study performed in a single institution with a relatively short duration. The impact of MET intervention may not be noticed immediately and may take up to years in order to achieve a cultural change and decreased mortality at a single institution. Our data were extracted from only a six-month period of MET intervention and we enrolled relatively small patients for mortality. Several studies have noted that it was only in the fourth year of MET intervention that they were able to show a statistically significant reduction in the unexpected hospital mortality rate.21,22 Second, our study might have several biases. The number of patients in the non-IM Department decreased after MET intervention. The Mayo Clinic data showed that the survival rate of patients with post-operative cardiac arrest was higher than that of patients with an in-hospital cardiac arrest (34.5% post-operative vs. 23% in-hospital).23 Another bias includes our information bias. In our study, the incidence of patients with difficult airway after MET intervention was higher than before it. The data before MET intervention were collected by a chart review, which did not routinely evaluate difficult airway before intubation. On the contrary, however, prospective data collected after MET intervention were more accurate than those collected before it, and a MET used the "LEMON"24 method for airway assessment before intubation and provided proper advanced airway management. Finally, we could not comment on the presence of supervision by a senior resident before MET intervention. Before MET intervention, senior residents or critical care physicians' back up was not mandatory. Also, because the data before MET intervention were insufficient, it is impossible to identify whether senior residents or critical care attending physicians were a part of the initial responder and impacted on airway outcomes.
In conclusion, early interventions of a MET changed the causes of emergency intubation in a general ward from CPR to respiratory distress or shock.
Besides, early intervention and proper management of a MET improved hypoxemia and hypotension related to emergency intubation.
Therefore, MET intervention is a safe and effective system for emergency intubation in a general ward.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–376. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Hardcastle TC, Goff T. Trauma unit emergency doctor airway management. S Afr Med J. 2007;97:864–867. [PubMed] [Google Scholar]
- 3.Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34:2355–2361. doi: 10.1097/01.CCM.0000233879.58720.87. [DOI] [PubMed] [Google Scholar]
- 4.Benedetto WJ, Hess DR, Gettings E, Bigatello LM, Toon H, Hurford WE, et al. Urgent tracheal intubation in general hospital units: an observational study. J Clin Anesth. 2007;19:20–24. doi: 10.1016/j.jclinane.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: part II. J Intensive Care Med. 2007;22:208–215. doi: 10.1177/0885066607301359. [DOI] [PubMed] [Google Scholar]
- 6.Mort TC, Waberski BH, Clive J. Extending the preoxygenation period from 4 to 8 mins in critically ill patients undergoing emergency intubation. Crit Care Med. 2009;37:68–71. doi: 10.1097/CCM.0b013e318192845e. [DOI] [PubMed] [Google Scholar]
- 7.Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324:387–390. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, Opdam H, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003;179:283–287. doi: 10.5694/j.1326-5377.2003.tb05548.x. [DOI] [PubMed] [Google Scholar]
- 9.Dacey MJ, Mirza ER, Wilcox V, Doherty M, Mello J, Boyer A, et al. The effect of a rapid response team on major clinical outcome measures in a community hospital. Crit Care Med. 2007;35:2076–2082. doi: 10.1097/01.ccm.0000281518.17482.ee. [DOI] [PubMed] [Google Scholar]
- 10.Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 1993;78:597–602. [PubMed] [Google Scholar]
- 11.Mace SE. Challenges and advances in intubation: rapid sequence intubation. Emerg Med Clin North Am. 2008;26:1043–1068. doi: 10.1016/j.emc.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Hunt EA, Zimmer KP, Rinke ML, Shilkofski NA, Matlin C, Garger C, et al. Transition from a traditional code team to a medical emergency team and categorization of cardiopulmonary arrests in a children's center. Arch Pediatr Adolesc Med. 2008;162:117–122. doi: 10.1001/archpediatrics.2007.33. [DOI] [PubMed] [Google Scholar]
- 13.Haldane AG. Advanced airway management--a medical emergency response team perspective. J R Army Med Corps. 2010;156:159–161. doi: 10.1136/jramc-156-03-06. [DOI] [PubMed] [Google Scholar]
- 14.Jamieson E, Ferrell C, Rutledge DN. Medical emergency team implementation: experiences of a mentor hospital. Medsurg Nurs. 2008;17:312–316. 323. [PubMed] [Google Scholar]
- 15.Mort TC. Preoxygenation in critically ill patients requiring emergency tracheal intubation. Crit Care Med. 2005;33:2672–2675. doi: 10.1097/01.ccm.0000187131.67594.9e. [DOI] [PubMed] [Google Scholar]
- 16.Farmery AD, Roe PG. A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth. 1996;76:284–291. doi: 10.1093/bja/76.2.284. [DOI] [PubMed] [Google Scholar]
- 17.Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth. 1996;8:289–293. doi: 10.1016/0952-8180(96)00037-2. [DOI] [PubMed] [Google Scholar]
- 18.Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011;114:42–48. doi: 10.1097/ALN.0b013e318201c415. [DOI] [PubMed] [Google Scholar]
- 19.Atlas GM, Mort TC. Attempts at emergent tracheal intubation of inpatients: A retrospective practice analysis comparing adjunct sedation with or without neuromuscular blockade. Internet J Anesthesiol. 2003;7:40. [Google Scholar]
- 20.Sagarin MJ, Barton ED, Chng YM, Walls RM National Emergency Airway Registry Investigators. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46:328–336. doi: 10.1016/j.annemergmed.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Jones D, Opdam H, Egi M, Goldsmith D, Bates S, Gutteridge G, et al. Long-term effect of a Medical Emergency Team on mortality in a teaching hospital. Resuscitation. 2007;74:235–241. doi: 10.1016/j.resuscitation.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Santamaria J, Tobin A, Holmes J. Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. Crit Care Med. 2010;38:445–450. doi: 10.1097/CCM.0b013e3181cb0ff1. [DOI] [PubMed] [Google Scholar]
- 23.Dumot JA, Burval DJ, Sprung J, Waters JH, Mraovic B, Karafa MT, et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of "limited" resuscitations. Arch Intern Med. 2001;161:1751–1758. doi: 10.1001/archinte.161.14.1751. [DOI] [PubMed] [Google Scholar]
- 24.Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22:99–102. doi: 10.1136/emj.2003.008771. [DOI] [PMC free article] [PubMed] [Google Scholar]