Abstract
BACKGROUND AND OBJECTIVES:
Latino–white disparities in age at autism spectrum disorder (ASD) diagnosis may be modified by primary care pediatrician (PCP) practices and beliefs. The objectives of this study were to assess ASD and developmental screening practices, attitudes toward ASD identification in Latino children, and barriers to ASD identification for Latino children, in a sample of 267 California PCPs.
METHODS:
In mail-based PCP survey, we assessed rates of bilingual general developmental and ASD screening, perceptions of parent ASD knowledge in Latino and white families, reports of difficulty assessing for ASDs in Latino and white children, and perceptions of barriers to early ASD identification for Latinos.
RESULTS:
Although 81% of PCPs offered some form of developmental screening, 29% of PCPs offered Spanish ASD screening per American Academy of Pediatrics guidelines, and only 10% offered both Spanish general developmental and Spanish ASD screening per American Academy of Pediatrics guidelines. Most PCPs thought that Latino (English and Spanish primary family language) parents were less knowledgeable about ASDs than white parents. PCPs had more difficulty assessing ASD risk for Latino children with Spanish primary family language than for white children, even when the PCP conducted recommended ASD screening or had >25% Latino patients. The most frequent barrier to ASD identification in Latinos was access to developmental specialists.
CONCLUSIONS:
Multiple factors in the primary care setting may contribute to delayed ASD identification for Latinos. Promoting language-appropriate screening, disseminating culturally appropriate ASD materials to Latino families, improving the specialist workforce, and providing PCP support in screening and referral of Latino children may be important ways to reduce racial and ethnic differences in care.
Keywords: autism spectrum disorder, Hispanic Americans, pediatrics, health care disparities, child development, developmental disabilities, developmental screening
What’s Known on This Subject:
Latino children are diagnosed with autism spectrum disorders (ASDs) less often and later than white children. Primary care pediatricians (PCPs) may play an important role in early ASD identification for Latinos.
What This Study Adds:
PCPs find it more difficult to assess for ASDs in Latinos with Spanish primary language, view Latino parents as less knowledgeable about ASDs, and experience frequent barriers to ASD diagnosis in Latino patients. Many PCPs do not offer recommended screenings in Spanish.
Autism spectrum disorders (ASDs) are common childhood developmental conditions, and early ASD identification is associated with improved long-term prognosis and family coping with disease.1 However, many children meeting ASD diagnostic criteria may be missed in diagnosis or diagnosed years after onset of symptoms,2,3,4,5 and studies have shown racial and ethnic differences in ASD diagnostic trends.6–8 Latino families face particular difficulty obtaining ASD diagnoses: Latino children are diagnosed with ASDs 2.5 years later than white children9 and have more severe symptoms at time of diagnosis.8 Similar delays have been reported for Latino children with other emotional, behavioral, or developmental conditions.4,10,11
Reasons for low rates of ASD diagnosis and diagnostic delay among Latino children are poorly understood. Delays may reflect family factors, including ethnic differences in parent knowledge, beliefs, and concerns about overall child development and developmental delay.5,12,13 Latino families may also have poorer overall healthcare access14 and less access to information about ASDs.15 Quality of provider interaction may also mediate ASD identification: Studies show that families of Latino children with ASDs experience poorer health care quality16 and lower-quality provider communication17 than white families. However, no studies have assessed specific provider beliefs and behaviors related to ASDs in Latino children.
Given their regular, early contact with families, PCPs play a critical role in early ASD identification. In addition to developmental surveillance at well-child visits, the American Academy of Pediatrics (AAP) recommends that PCPs perform developmental screening at 9, 18, and 24 to 30 months and autism-specific screening at 18 and 24 to 30 months.1 PCPs also refer children to developmental specialists capable of ASD diagnosis and therapists providing ASD treatment services. Therefore, PCP views and behaviors regarding ASD identification among Latino children may contribute to diagnostic and treatment disparities.
In this study, we surveyed a representative sample of PCPs about ASD identification in Latinos. We set the study in California because it has the highest population of Latino children, with recent census estimates suggesting that Latino children represent the majority.18 Our primary research questions were: (1) What proportion of PCPs offer recommended general developmental and ASD screening, including Spanish-language screening? (2) How confident are PCPs in assessing ASD risk among Latino children? (3) Do PCPs perceive racial or ethnic differences in family knowledge about ASDs? (4) What are PCPs’ perceptions of barriers to ASD care for Latino children? We hypothesized that a minority of PCPs offer guideline-based developmental and ASD screening in Spanish, that PCPs feel less confident assessing ASD risk in Latino children, and that PCPs view Latino parents as less informed about ASDs. Finally, we hypothesized that PCPs would cite frequent language, cultural, communication, and health care access barriers to ASD care for Latino children.
Methods
Survey Administration
We mailed a self-administered survey to a random sample of California pediatricians obtained from the American Medical Association Masterfile.19 A sample size of 500 (with 60% responding) gave adequate power to detect barriers to ASD care ranging from 10% to 75% prevalence with +/−5% precision. Pediatricians were eligible for the sample if they practiced clinic-based general pediatrics in California, were board-certified, and spent >50% of their time providing clinical care. Responses were collected from August 2011 to March 2012. Survey response rate was calculated using the American Association of Public Opinion Research algorithm.20 The Oregon Health & Science University institutional review board approved the study. The Supplemental Information shows the full survey.
Survey Content
Developmental and Autism Screening
To assess general developmental screening, the survey asked PCPs whether they “use general developmental screening tools at one or more well-child visits for patients under age three” and provided examples of validated tools. PCPs who screened were asked which tool they used, at which well visits they screened, and whether they offered Spanish-language screening for families with Spanish preference.
To assess ASD screening, pediatricians were asked whether they used “a screening tool specifically to assess for ASDs at one or more well child visits for patients under age three” and provided the Modified Checklist for Autism in Toddlers as an example. PCPs who screened for ASDs were asked which tool they used, at which visits they screened, and whether they offered Spanish-language screening for families with Spanish preference.
ASD Attitudes
PCPs used a 4-part scale to compare ASD knowledge among parents of white, Latino/English primary family language (PFL), Latino/Spanish PFL, and African American children and to rate the difficulty of recognizing signs and symptoms of ASDs among white, Latino/English PFL, Latino/Spanish PFL, and African American children.
Barriers to ASD Care
PCPs used a scale to rate frequency of experiencing 10 possible barriers to ASD care for Latinos, subdivided into two domains. Access barriers included access to primary care, access to developmental and behavioral specialists, availability of reliable screening tools, and logistical issues such as location of services or clinic hours. Language, cultural, and communication barriers included parent trust or willingness to communicate with provider, parent beliefs about normal child development, parent understanding about the importance of early ASD diagnosis and treatment, and availability of interpreter services.
Demographic Characteristics
The survey asked PCPs to report Spanish proficiency, practice size, Latino providers in practice, percentage Latino patients, and knowledge about ASDs. Years since medical school graduation, gender, and region of California were obtained from American Medical Association Masterfile data (Table 1). PCP race and ethnicity data were obtained from the California Medical Board, which collects these data via self-report.
TABLE 1.
Characteristics of PCPs and Their Practices (n = 267)
| Characteristic | n | % |
|---|---|---|
| Personal Characteristics | ||
| Gendera | ||
| Male | 108 | 40.6% |
| Female | 158 | 59.4% |
| Years since medical school graduationa | ||
| >20 y | 143 | 53.6% |
| ≤20 y | 124 | 46.4% |
| Race or ethnicityb | ||
| White only | 55 | 22.5% |
| Black only | 4 | 1.6% |
| Hispanic/Latino | 11 | 4.5% |
| Asian/Pacific Islander | 30 | 12.3% |
| Other | 6 | 2.4% |
| Declined to disclose | 138 | 56.6% |
| Spanish fluencyc | ||
| None, poor, or fair | 183 | 69.6% |
| Good or excellent | 80 | 30.4% |
| Practice Characteristics | ||
| Practice sizec | ||
| Solo or small group (1–3 providers) | 75 | 28.9% |
| Medium group (4–9 providers) | 114 | 43.8% |
| Large group (≥10 providers) | 71 | 27.3% |
| Practice regiona,d | ||
| Bay Area | 78 | 29.2% |
| Central/Southern Farm | 23 | 8.6% |
| Central Valley | 26 | 9.7% |
| Los Angeles | 58 | 21.7% |
| North and Mountain | 3 | 1.1% |
| Southern California without Los Angeles | 79 | 29.6% |
| Any Latino provider in practicec | ||
| Yes | 112 | 42.9% |
| No | 149 | 57.1% |
| Percentage Latino patients in practicec | ||
| ≥25% | 132 | 50.8% |
| <25% | 128 | 49.2% |
Data obtained from the American Medical Association Masterfile.
Data obtained from the California Medical Board.
Data obtained from survey.
Based on California Department of Social Services/Data Analysis and Publications Branch regional grouping.
Data Analysis
Analysis of Developmental and Autism Screening
We assessed screening in 4 categories. PCPs performing developmental or ASD screening at any routine visit, using any tool, were coded as “performs any type of developmental screening at any routine visit.” PCPs performing general developmental screening at the 9-, 18-, and 24- or 30-month visits using a validated tool21 were coded as “performs general developmental screening per AAP Bright Futures Periodicity Guidelines.”22 PCPs performing ASD-specific screening at the 18- and 24- or 30-month visit with a validated tool1 were coded as “performs ASD screening per AAP Bright Futures Periodicity Guidelines.”21,22 PCPs who performed both recommended screenings per guidelines were coded as “performs both types of screening per AAP Bright Futures Periodicity Guidelines.” We calculated percentage of PCPs offering each type of screening as and both screenings, in English and Spanish. We then dichotomized PCPs according to those with ≥25% vs <25% Latino patients in their practice (50.8% vs 49.2% of sample) and compared screening rates between these groups using χ2 tests (Table 2).
TABLE 2.
Screening Practices of PCPs and Percentage Latino Patients
| All PCPs (%, n) (n = 267) | PCPs With >25% Latino Patients in Practice (%, n) (n = 128) | PCPs With ≤25% Latino Patients in Practice (%, n) (n = 132) | Pa | |
|---|---|---|---|---|
| PCP performs any kind of developmental screening at any routine visit | 80.5% (215) | 76.6% (98) | 84.1% (111) | .13 |
| PCP performs general developmental screening per AAP Bright Futures Periodicity Guidelines | 30.4% (81) | 27.2% (34) | 33.3% (44) | .29 |
| PCP performs ASD screening per AAP Bright Futures Periodicity Guidelines | 42.9% (112) | 43.0% (55) | 42.8% (56) | .97 |
| PCP performs both types of screening per AAP Bright Futures Periodicity Guidelines | 15.2% (39) | 15.2% (19) | 15.3% (20) | .98 |
| PCP offers general developmental screening in Spanish per AAP Bright Futures Periodicity Guidelines | 17.7% (46) | 21.8% (27) | 13.7% (18) | .09 |
| PCP offers ASD screening in Spanish per AAP Bright Futures Periodicity Guidelines | 28.7% (74) | 40.6% (52) | 16.9% (22) | .001 |
| PCP offers both types of screening in Spanish per AAP Bright Futures Periodicity Guidelines | 10.3% (26) | 12.9% (16) | 7.8% (10) | .18 |
Percentages reflect the proportion of subjects with valid responses for each variable.
χ2 test P value comparing PCPs with >25% Latino patients to PCPs with ≤25% Latino patients.
Analysis of ASD Attitudes
To assess PCP perceptions of parent knowledge about ASDs, we dichotomized knowledge about ASDs into “not at all” or “not very” knowledgeable versus “somewhat” or “very knowledgeable.” We used McNemar’s test to compare the proportion of PCPs reporting that families of white children were “not at all/not very knowledgeable” compared with the proportion reporting that families of Latino/English PFL, Latino/Spanish PFL, and African American children were “not at all/not very knowledgeable” (Table 3). Because PCP perceptions of parent knowledge might vary according to practice or personal characteristics, we performed subgroup analyses for 4 practice characteristics (PCP performs general developmental screening per AAP Bright Futures Periodicity Guidelines, PCP performs ASD screening per AAP Bright Futures Periodicity Guidelines, Latino provider in practice, and >25% of patients are Latino) and 2 personal characteristics (PCP rates Spanish as good or excellent, PCP self-reports very knowledgeable about autism). We used McNemar’s test to compare racial and ethnic perceptions among PCPs in each subgroup and χ2 tests to compare perceptions across PCP subgroups. Finally, in the Latino/English PFL and Latino/Spanish PFL groups only, we used logistic regression to assess the association of each PCP personal or practice characteristic with knowledge about ASDs, adjusting for sociodemographic differences. We used similar statistical procedures to compare PCPs’ reports of difficulty identifying signs and symptoms of ASDs in white, Latino/English PFL, Latino/Spanish PFL, and African American children (Table 4).
TABLE 3.
PCPs’ Perceptions of Parent Knowledge About ASDs, by Racial or Ethnic Group
| “How Knowledgeable About ASD Are Parents in Each Group?” | ||||
|---|---|---|---|---|
| Percentage of PCPs Reporting Parents “Not at All” or “Not Very” Knowledgeable About ASD | ||||
| Subgroup (n) | Parents of Non-Latino White Children | Parents of Latino Children/English PFL | Parents of Latino Children/Spanish PFL | Parents of African American Children |
| All PCPs (267) | 20.4% | 32.2%a | 73.9%a | 49.6%a |
| PCP Practice Characteristic Subgroups | ||||
| PCP performs general developmental screening per AAP Bright Futures Periodicity Guidelines | ||||
| Yes (81) | 23.1% | 31.9%a | 69.1%a | 44.9%a |
| No (183) | 19.5% | 32.9%a | 76.7%a | 52.6%a |
| PCP performs ASD screening per AAP Bright Futures Periodicity Guidelines | ||||
| Yes (112) | 15.9% | 27.2%a | 68.7%a | 43.5%a |
| No (154) | 23.1% | 35.5%a | 77.6%a | 53.4%a |
| Latino provider in practice | ||||
| Yes (112) | 15.7% | 27.9%a | 74.5%a | 50.0%a |
| No (149) | 22.5% | 33.8%a | 72.4%a | 48.8%a |
| >25% Latino patients in practice | ||||
| Yes (128) | 25.4% | 33.3%a | 75.2%a | 49.6%a |
| No (132) | 14.8%b | 30.8%a | 71.6%a | 49.6%a |
| PCP Practice Characteristic Subgroups | ||||
| PCP rates Spanish as good or excellent | ||||
| Yes (80) | 19.2% | 31.6%a | 72.7%a | 52.1%a |
| No (183) | 20.1% | 31.9%a | 74.0%a | 48.7%a |
| PCP self-reports very knowledgeable about ASD | ||||
| Yes (138) | 12.9% | 24.8%a | 63.0%a | 40.2%a |
| No (125) | 28.3%b | 40.4%a,b | 84.8%a,b | 59.4%a,b |
Significantly different by parent racial or ethnic and language group (P < .05 compared with parents of non-Latino white children on McNemar’s test).
Significantly different by PCP subgroup (“yes” versus “no” P < .05 on χ2 test).
TABLE 4.
PCPs’ Perceived Ability to Identify ASD by Racial or Ethnic Group
| “How Difficult Is It for You to Recognize the Signs and Symptoms of ASD in Each Group?” | ||||
|---|---|---|---|---|
| Percentage of PCPs Reporting “Somewhat or Very Difficult” | ||||
| Subgroup (n) | Parents of Non-Latino White Children | Parents of Latino Children/English PFL | Parents of Latino Children/Spanish PFL | Parents of African American Children |
| All PCPs (267) | 33.2% | 34.8% | 60.4%a | 37.6%a |
| PCP Practice Characteristic Subgroups | ||||
| PCP performs general developmental screening per AAP Bright Futures Periodicity Guidelines | ||||
| Yes (81) | 35.8% | 37.0% | 58.4%a | 41.0% |
| No (183) | 31.8% | 33.5% | 61.4%a | 35.2% |
| PCP performs ASD screening per AAP Bright Futures Periodicity Guidelines | ||||
| Yes (112) | 29.4% | 31.2% | 58.6%a | 34.3% |
| No (154) | 35.5% | 36.9% | 61.4%a | 39.4%a |
| Latino provider in practice | ||||
| Yes (112) | 26.1%b | 27.9% | 49.6%a | 30.1% |
| No (149) | 38.6% | 40.1%b | 69.9%a,b | 43.4%b |
| >25% Latino patients in practice | ||||
| Yes (128) | 27.2%b | 30.4% | 46.0%a | 32.2% |
| No (132) | 40.0% | 40.1% | 76.5%a,b | 43.1% |
| PCP Personal Characteristic Subgroups | ||||
| PCP rates Spanish as good or excellent | ||||
| Yes (80) | 32.9% | 35.4% | 48.1%a | 35.6% |
| No (183) | 34.1% | 35.2% | 67.1%a,b | 39.3%a |
| PCP self-reports very knowledgeable about ASD | ||||
| Yes (138) | 25.6%b | 27.9%b | 55.6%a | 29.9% |
| No (125) | 41.5% | 42.2% | 66.1%a | 45.7%b |
Significantly different by parent racial or ethnic and language group (P < .05 compared with parents of non-Latino white Children on McNemar's test).
Significantly different by PCP subgroup (“yes” versus “no” P < .05 on χ2 test).
Analysis of Barriers to ASD Care
We considered an item as a barrier if a PCP reported experiencing the item often or frequently (versus never, rarely, or sometimes). We used descriptive statistics to rank barriers experienced by the most PCPs and to calculate median and interquartile range of barriers experienced. We used logistic regression to assess whether PCP personal characteristics, practice characteristics, ratings of parent knowledge, and difficulty identifying ASDs were associated with having an above-median number of barriers to ASD care.
Results
Respondent Characteristics
In all, 267/500 PCPs returned the survey; 53 providers were ineligible because of invalid contact information, not being PCPs, retired, or moved out of California. The overall response rate was 62.9%. Respondent characteristics are shown in Table 1; responders and nonresponders did not differ by gender, race, or region of California. However, responders were more likely to have been in practice <20 years (66.3% of responders vs 55.0% of nonresponders; P = .02).
Developmental and ASD Screening Rates
Most PCPs offered some type of routine developmental screening (Table 2). However, a minority offered general developmental (30.4%) or ASD screening (42.9%) per AAP guidelines, and a smaller proportion offered both recommended screenings (15.2%) per AAP guidelines. Spanish-language screening rates were even lower: 17.7% of PCPs offered general screening, and 28.7% offered ASD screening in Spanish. Only 10.3% of PCPs offered both ASD screening and general developmental screening in Spanish per AAP guidelines (Table 2).
A minority of both PCPs with >25% Latino patients and PCPs with ≤ 25% Latino patients offered Spanish-language screening; however, PCPs with more Latino patients were more likely to offer Spanish-language ASD screening. There was a nonsignificant trend toward higher rates of offering Spanish-language general developmental screening and performing both types of Spanish-language screening among PCPs with more Latino patients (Table 2).
Perceptions of Parent Knowledge About ASDs
Most PCPs reported that parents of Latino and African American children had lower levels of ASD knowledge than parents of white children (Table 3). The largest difference was between parents of Latino/Spanish PFL children and parents of white children. PCPs who performed developmental or ASD screening rated parental ASD knowledge similarly to other PCPs (Table 3). Spanish proficiency, having a Latino provider in the practice, or having >25% Latino patients in the practice did not modify perceived ASD knowledge among parents of Latino children; however, PCPs with >25% Latino patients in their practice were more likely to report that white parents also had low ASD knowledge. PCPs who self-reported as “very knowledgeable about autism” were more likely to report parents of all races and ethnicities as knowledgeable about autism; however, they still noted significant knowledge differences between parents of Latino or African American children and parents of white children (Table 3). After multivariate adjustment, only PCP self-reported ASD knowledge was associated with higher odds of reporting that Latino/Spanish PFL parents (adjusted odds ratio [aOR] 3.51; confidence interval [CI] 1.81–6.84) or Latino/English PFL parents (aOR 2.08 [CI 1.16–3.73]) were somewhat or very knowledgeable about ASDs.
Ability to Identify Signs and Symptoms of ASDs
When PCPs were asked to compare how difficult it was to “recognize the signs and symptoms of ASD” in white, Latino/English PFL, Latino/Spanish PFL, and African American children, more PCPs had difficulty identifying ASD signs and symptoms in Latino/Spanish PFL children and African American children than in white children (Table 4). PCPs with higher Spanish proficiency, a Latino provider in their practice, or >25% Latino patients were less likely to have difficulty identifying ASD signs and symptoms in Latino/Spanish PFL children than other PCPs; however, even these groups of PCPs reported significantly more difficulty assessing ASD risk in Latino/Spanish PFL children than in white children. PCPs who performed general developmental screening or ASD screening were as likely as other PCPs to report difficulty recognizing ASDs among Latinos (Table 4). After multivariate adjustment, having a Latino provider in the practice (aOR 1.85 [CI 1.03–3.31]) and having >25% Latino patients (aOR 3.43 [CI: 1.88–6.26]) were associated with easier identification of ASDs among Latino/Spanish PFL children. PCP self-reported autism knowledge was the only factor associated with easier identification of ASDs among Latino/English PFL children (aOR 2.15 [CI: 1.24–3.75]).
Barriers to ASD Identification
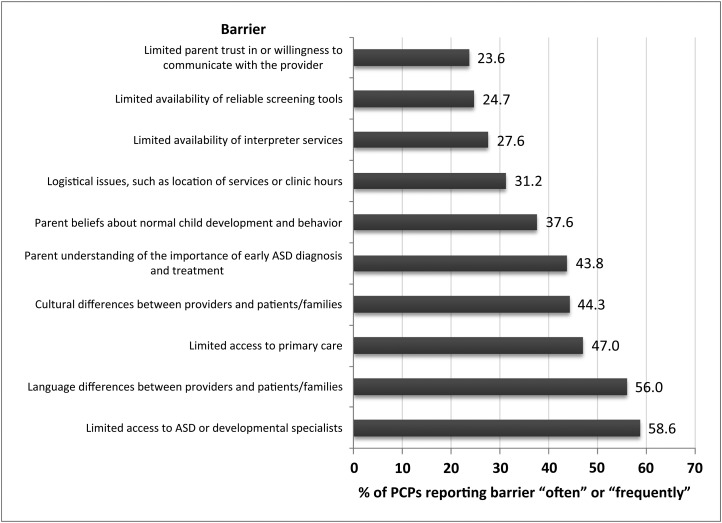
A total of 74.5% of PCPs experienced ≥1 barriers to ASD diagnosis in Latino children; 60.7% experienced ≥1 access barrier, and 68.2% experienced ≥1 language, cultural, or communication barrier. The most frequent barriers were “limited access to ASD or developmental specialists,” “language differences between providers and patients/families,” and “limited access to primary care” (Fig 1). Of PCPs experiencing ≥1 barrier, the median number experienced was 4 (interquartile range 3). PCPs who viewed Latino/Spanish PFL parents as less knowledgeable about ASDs were more likely to report >4 barriers to ASD care than PCPs who viewed Latino/Spanish PFL parents as more knowledgeable (aOR 6.67 [CI 2.88–15.54]). Likewise, PCPs who reported that recognizing ASDs in Latino/Spanish PFL families was difficult were more likely to report >4 barriers than PCPs who found ASDs easier to recognize (aOR 2.13 [CI 1.15–3.93]). PCP personal or practice characteristics had no significant associations with experiencing >4 barriers to ASD diagnosis.
FIGURE 1.
Barriers to ASD care for Latino children.
Discussion
Latino children are diagnosed with ASDs at low rates, and this investigation found several provider-related factors that might explain these disparities. First, most providers do not offer guideline-based developmental and ASD screening. Rates were particularly low for Spanish-language screening, which disproportionately affects ASD identification in Latinos. Additionally, most PCPs experienced difficulty recognizing signs and symptoms of ASDs in Latino/Spanish PFL children, even if they performed recommended ASD screening or had >25% Latinos in their practice. PCPs thought that parents of Latino children (especially those with Spanish PFL) had less ASD knowledge. Finally, 3 in 4 PCPs cited access, communication, or cultural barriers to ASD care for Latino children, and PCPs experiencing these barriers found ASDs particularly difficult to identify.
These findings have important policy implications. First, rates of Spanish-language developmental and ASD screening need targeted improvement: When only 1 in 5 California PCPs offers recommended Spanish-language ASD screening, and only 1 in 10 offers both Spanish-language ASD and general developmental screening, it is unlikely for a Latino/Spanish PFL child to have ASD identified via routine screening. Although the survey did not assess why many PCPs did not offer Spanish-language screening, limited availability of screening tools (barrier cited by 24.7% of PCPs) may be one problem. Although the Modified Checklist for Autism in Toddlers is publicly available in Spanish,23 most recommended developmental screening tools are not publicly available, and Spanish materials cost more.24–26 Cost of tools may explain the particularly low rates of Spanish-language general developmental screening we found. Developing and promoting free or low-cost screening resources could improve early identification and reduce language-based disparities. However, because most PCPs who did screen still experienced difficulty identifying ASDs in Latinos, additional resources are needed. PCPs may also need information about bilingualism and language development, accurate interpretation of screening results in less-acculturated Latinos, or strategies for discussing this difficult topic with parents from a different culture.
The finding that PCPs viewed Latino parents as less knowledgeable about ASDs merits additional investigation. Although we do not know whether PCPs’ views were accurate, Latino parents have lower average health literacy27,28 and less access to ASD-specific information,15 which could contribute to knowledge deficits about ASDs. Differences in PCP education and anticipatory guidance provision to Latino parents29,30 may also contribute to these deficits. Our findings suggest that PCPs should discuss ASD signs and symptoms with Latino parents because they may have less information. Increasing the availability of culturally appropriate, bilingual parent–oriented ASD materials might augment such discussions. Because many providers noted cultural barriers to ASD identification, efforts to spread information about ASDs outside the primary care setting may also be helpful. A promising example of such an effort is the Centers for Disease Control’s “Learn the Signs. Act Early” campaign, which has publicly available, parent-focused Spanish-language materials.31
PCPs cited access to primary care and ASD specialty care as prevalent barriers to ASD diagnosis for Latino children. Latino children may be at particular risk for having poor health care access because they are more likely to be uninsured or underinsured than other children.14,32 Geographic disparities in child mental health services for Latinos may reduce service accessibility.33 This may be more likely in California, where regionalization in developmental disability services may impose geographic and logistical challenges. Increasing accessibility and number of providers, particularly Latino providers or providers experienced with Latino families, may reduce access barriers and improve quality.
The study had limitations. We studied PCPs rather than family practitioners or allied health professionals. We chose this group because PCPs generally have more children in their practices and therefore might have more established views on developmental screening and ASDs. However, PCPs may be more likely to follow developmental screening practice guidelines than other providers,34 so our results may overestimate screening rates. We set the study in California to sample PCPs who interact regularly with Latino patients; rates of Spanish-language screening and attitudes toward Latino families may differ in areas with fewer Latinos. In survey items where PCPs compared language groups of Latinos, we used PFL instead of English proficiency. However, studies show that English proficiency is perhaps a better marker of health care access35 that many PCPs are able to assess.36 By choosing to use PFL instead of English proficiency, our study probably minimized differences between the Latino/Spanish group and other groups.
We did not directly ask PCPs their reasons for not screening, nor did we ask PCPs where or how they obtained knowledge about ASD. There were significant gaps in data for PCP race and ethnicity because we relied on data from the California Medical Board. As a result, we were unable to examine PCP racial and ethnic subgroups or family–PCP racial or ethnic concordance. Our analysis may be subject to type I and type II errors: We made multiple comparisons, which increases the likelihood of finding a significant result by chance. However, because we powered the study around barriers to ASD care only, it is also possible that significant differences went undetected because of lack of power.
Strengths of the study include a random sample design and a strong response rate. We used a rigorous definition of developmental screening that adhered more closely to AAP guidelines than prior studies.37 Although this probably resulted in lower estimates of screening rates, estimates may more accurately reflect adherence to practice guidelines.
Conclusions
To our knowledge, this is the first study investigating PCP perspectives on disparities in ASD identification. This study points to modifiable provider-related factors that may contribute to ASD diagnostic delays among Latinos. The data may help inform future interventions to reduce racial and ethnic differences in ASD care.
Supplementary Material
Acknowledgments
We thank Richard LeDonne, Jean Su and Yassar Arain for their assistance with data collection.
Glossary
- AAP
American Academy of Pediatrics
- aOR
adjusted odds ratio
- ASD
autism spectrum disorder
- CI
confidence interval
- PCP
primary care pediatrician
- PFL
primary family language
Footnotes
Dr Zuckerman conceptualized and designed the project, oversaw data acquisition, performed data analysis, and drafted the article; Ms Mattox and Dr Donelan made substantial contributions to conceptualization and design of the project; Ms Mattox assisted with data acquisition and analysis; Dr Donelan assisted with data interpretation; Ms Baghaee made substantial contributions to data acquisition and assisted with drafting the manuscript; Ms Batbayar made substantial contributions to data acquisition and analysis and assisted with drafting the manuscript; Dr Bethell made substantial contributions to conceptualization and design of the project and assisted with data analysis and interpretation; Ms Mattox, Dr Donelan, Ms Baghaee, Ms Batbayar, and Dr Bethell revised the manuscript for important intellectual content; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This project was funded by an Academic Pediatric Association/Commonwealth Fund Young Investigator Award (principal investigator, Dr Zuckerman). Dr Zuckerman’s effort was partially funded by grant 1K23MH095828 from the National Institute of Mental Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Johnson CP, Myers SM, American Academy of Pediatrics Council on Children With Disabilities . Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215 [DOI] [PubMed] [Google Scholar]
- 2.Mandell DS, Ittenbach RF, Levy SE, Pinto-Martin JA. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism & Developmental Disorders. 2007;37(9):1795–1802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. American J of Public Health. 2009;99(3):493–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555 [DOI] [PubMed] [Google Scholar]
- 5.Bornstein MH, Cote LR. “Who is sitting across from me?” Immigrant mothers’ knowledge of parenting and children’s development. Pediatrics. 2004;114(5). Available at: www.pediatrics.org/cgi/content/full/114/5/e557 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) . Mental health in the United States: parental report of diagnosed autism in children aged 4–17 years—United States, 2003–2004. MMWR Morb Mortal Wkly Rep. 2006;55(17):481–486 [PubMed] [Google Scholar]
- 7.Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders: Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012;61:1–19 [PubMed] [Google Scholar]
- 8.Liptak GS, Benzoni LB, Mruzek DW, et al. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. J Dev Behav Pediatr. 2008;29(3):152–160 [DOI] [PubMed] [Google Scholar]
- 9.Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among Medicaid-eligible children with autism. J Am Acad Child Adolesc Psychiatry. 2002;41(12):1447–1453 [DOI] [PubMed] [Google Scholar]
- 10.Rowland AS, Umbach DM, Stallone L, Naftel AJ, Bohlig EM, Sandler DP. Prevalence of medication treatment for attention deficit–hyperactivity disorder among elementary school children in Johnston County, North Carolina. Am J Public Health. 2002;92(2):231–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller TW, Nigg JT, Miller RL. Attention deficit hyperactivity disorder in African American children: what can be concluded from the past ten years? Clin Psychol Rev. 2009;29(1):77–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pachter LM, Dworkin PH. Maternal expectations about normal child development in 4 cultural groups. Arch Pediatr Adolesc Med. 1997;151(11):1144–1150 [DOI] [PubMed] [Google Scholar]
- 13.Keels M. Ethnic group differences in Early Head Start parents’ parenting beliefs and practices and links to children’s early cognitive development. Early Child Res Q. 2009;24:381–397 [Google Scholar]
- 14.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2). Available at: www.pediatrics.org/cgi/content/full/121/2/e286 [DOI] [PubMed] [Google Scholar]
- 15.Magaña S, Lopez K, Aguinaga A, Morton H. Access to diagnosis and treatment services among Latino children with autism spectrum disorders. Intellect Dev Disabil. 2013;51(3):141–153 [DOI] [PubMed] [Google Scholar]
- 16.Magaña S, Parish SL, Rose RA, Timberlake M, Swaine JG. Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellect Dev Disabil. 2012;50(4):287–299 [DOI] [PubMed] [Google Scholar]
- 17.Parish S, Magaña S, Rose R, Timberlake M, Swaine JG. Health care of Latino children with autism and other developmental disabilities: quality of provider interaction mediates utilization. Am J Intellect Dev Disabil. 2012;117(4):304–315 [DOI] [PubMed] [Google Scholar]
- 18.National Council of La Raza. Toward a more vibrant and youthful nation: Latino children in the 2010 Census. Available at: www.nclr.org/index.php/publications/toward_a_more_vibrant_and_youthful_nation_latino_children_in_the_2010_census/. Accessed October 15, 2012
- 19.American Medical Association Physician Masterfile. Available at: www.ama-assn.org/ama/pub/about-ama/physician-data-resources/physician-masterfile.shtml. Accessed March 20, 2013
- 20.American Association for Public Opinion Research. Response rate: An overview. Available at: www.AAPpor.org/Response_Rates_An_Overview1.htm. Accessed September 14, 2012
- 21.Council on Children With Disabilities. Section on Developmental Behavioral Pediatrics. Bright Futures Steering Committee. Medical Home Initiatives for Children With Special Needs Project Advisory Committee . Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118(1):405–420 [DOI] [PubMed] [Google Scholar]
- 22.Duncan P. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed Elk Grove Village, IL: American Academy of Pediatrics; 2008 [Google Scholar]
- 23.Robbins DL. M-CHAT information. Available at: http://www2.gsu.edu/∼psydlr/Diana_L._Robins,_Ph.D.html. Accessed December 1, 2012
- 24.Squires J. Ages and Stages Questionnaire. 3rd ed. Available at: http://agesandstages.com/. Accessed December 1, 2012
- 25.Denver Developmental Materials. Denver II. Available at: http://denverii.com/. Accessed December 1, 2012
- 26.Glascoe FP. Parents’ Evaluation of Developmental Status. Available at: www.pedstest.com/. Accessed December 1, 2012
- 27.Yin HS, Sanders LM, Rothman RL, et al. Assessment of health literacy and numeracy among Spanish-speaking parents of young children: validation of the Spanish Parental Health Literacy Activities Test (PHLAT Spanish). Acad Pediatr. 2012;12(1):68–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(suppl 3):82–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bethell C, Reuland CH, Halfon N, Schor EL. Measuring the quality of preventive and developmental services for young children: national estimates and patterns of clinicians’ performance. Pediatrics. 2004;113(6 suppl):1973–1983 [PubMed] [Google Scholar]
- 30.Guerrero AD, Chen J, Inkelas M, Rodriguez HP, Ortega AN. Racial and ethnic disparities in pediatric experiences of family-centered care. Med Care. 2010;48(4):388–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC). Learn the signs. Act early. Available at: www.cdc.gov/ncbddd/actearly/index.html. Accessed June 5, 2013
- 32.Flores G, Abreu M, Tomany-Korman SC. Why are Latinos the most uninsured racial/ethnic group of US children? A community-based study of risk factors for and consequences of being an uninsured Latino child. Pediatrics. 2006;118(3). Available at: www.pediatrics.org/cgi/content/full/118/3/e730 [DOI] [PubMed] [Google Scholar]
- 33.Sturm R, Ringel JS, Andreyeva T. Geographic disparities in children’s mental health care. Pediatrics. 2003;112(4). Available at: www.pediatrics.org/cgi/content/full/112/4/e308 [DOI] [PubMed] [Google Scholar]
- 34.Sices L, Feudtner C, McLaughlin J, Drotar D, Williams M. How do primary care physicians manage children with possible developmental delays? A national survey with an experimental design. Pediatrics. 2004;113(2):274–282 [DOI] [PubMed] [Google Scholar]
- 35.Flores G, Abreu M, Tomany-Korman SC. Limited English proficiency, primary language at home, and disparities in children’s health care: how language barriers are measured matters. Public Health Rep. 2005;120(4):418–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuo DZ, O’Connor KG, Flores G, Minkovitz CS. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119(4). Available at: www.pediatrics.org/cgi/content/full/119/4/e920 [DOI] [PubMed] [Google Scholar]
- 37.Radecki L, Sand-Loud N, O’Connor KG, Sharp S, Olson LM. Trends in the use of standardized tools for developmental screening in early childhood: 2002–2009. Pediatrics. 2011;128(1):14–19 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.