Background
The world population of inhabitants of greater than 60 years of age has doubled since 1980 and is predicted to reach 2 billion by 2050 [1]. Trauma is the sixth leading cause of death in patients over 60 years of age [2]. Though this growing elderly population only comprises 12% of overall trauma patients, they consume considerable medical resources [3] and are more likely to require hospital admission [4]. An aggressive approach should be established throughout the management of the elderly trauma patient in order to reduce mortality and the incidence of permanent disability [5]. In the past decade, the overall mortality rate due to trauma decreased. However, in the elderly population (>65 years of age), the incidence of trauma-related mortality is still high, mostly secondary to falls [6]. Elderly patients have a higher mortality after trauma as well as a higher complication rate, specifically for pulmonary and infectious complications [7,8].
Trauma in the elderly clearly poses special challenges to the physician, with physiological changes of age impacting morbidity and mortality. Notwithstanding, little information is available regarding risk factors that aid in predicting increased mortality in this population. More so, there are significant findings in the literature showing that severely injured geriatric trauma patients who do survive their hospitalization have appreciable long-term survival and return to independent living [9-11].
Our study is a retrospective review of our experience with severely injured elderly patients. Our primary objectives were to describe the different pattern of injury among the elderly and define and analyze predictors of in-hospital mortality. Our secondary objective was to determine whether pre-existing co-morbidities had an adverse effect on outcome.
Methods
Hadassah University Hospital, Ein Kerem Campus, is a tertiary medical center and the only level I trauma center in the Jerusalem vicinity. Emergency medical services (EMS) in Israel are provided by a government funded national organization with regional control. The catchment area incorporates Jerusalem and nearby towns and villages and includes a population of approximately one million inhabitants.
Inclusion criteria to the study included all trauma patients ≥ 60 years of age who presented to our Level I Trauma Center with an injury severity score (ISS) ≥16 between January 2006 and December 2010. Patients who were pronounced dead at the trauma bay or had a do not resuscitate order were excluded from the study. Data was retrieved from medical records and the trauma registry database. The trauma registry is a prospectively collected database that is updated daily by dedicated personnel and has institutional review board (IRB) approval.
All charts were retrospectively reviewed for demographics, ISS, GCS (Glasgow Coma Scale) at presentation to the emergency department (ED), mechanism of injury (MOI), body regions injured, pre-existing co-morbidities, intensive care unit length of stay (ICU LOS), hospital LOS, surgical interventions, complications, and in-hospital mortality. Patients were divided into 3 age groups: 60-69 years, 70-79 and ≥80. The main outcome measure was in-hospital mortality. This was defined as death which occurred at the trauma center. In order to avoid missing late deaths which were directly related to the trauma, we chose to include patients who were discharged from the hospital but died within 30 days of the traumatic insult regardless of patient location at time of death. Co-morbidities were defined as presented in Table 1.
Table 1.
Definition of co-morbidities
| Cardiac disease |
Known history of ischemic heart disease, previous cardiac interventions for ischemic heart disease |
| Malignancy |
Currently under oncological follow up for active oncological disease |
| Diabetes mellitus |
Patient requiring insulin or oral hypoglycemic therapy |
| Neurological disease |
History of cerebrovascular accident, severe parkinsonism or antiepileptic therapy |
| Dementia |
A patient with an established diagnosis of dementia |
| Hypertension |
History of hypertension requiring medication |
| Chronic anticoagulation |
Patients currently on anticoagulation (low molecular weight heparin or Warfarin), and anti-platelet therapy (excluding aspirin) |
| Chronic renal failure |
Preexisting renal insufficiency on admission |
| Chronic pulmonary disease | Ongoing treatment for chronic obstructive pulmonary disease or asthma |
Statistical analysis
Data are presented as mean ± standard deviation. The Fisher's exact test was used to compare proportions and the Kruskal-Wallis test was used to compare continuous non-parametric variables between the three groups. The chi-squared test for trends was used to compare mortality between the different age groups. A logistic regression model was used to define predictors of death. In order to determine predictors of in-hospital death, parameters which were significant on univariate analysis were entered into a stepwise, forward regression model. A p value of 0.05 or less was considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.)
Results
Patient population
There were 417 trauma patients older than 60 years of age and with an ISS ≥16 who presented to our trauma unit during the study period and who met the inclusion criteria. One patient was excluded due to incomplete data. The mean age of the study cohort was 76.9 years (±9.6) and there were 232 males (55.6%). 174 patients (41.7%) were ≥ 80 years. Mean ISS for the whole cohort was 22.9 (±8.4). 230 patients (55.3%) had an ISS of 16 to 24 and 186 patients (44.7%) had an ISS ≥25.
The demographic and clinical characteristics of the patients according to the age groups are noted in Table 2. The rate of males declined significantly with age. Although ISS and the median number of regions injured decreased significantly with age (both p < 0.001), mortality increased significantly. The most common MOI for all patients was falls (n = 271, 65.1%) followed by pedestrian injuries (n = 71, 17.1%), motor vehicle collision (MVC) (n = 49, 11.8%), burns (n = 11, 2.6%), and other causes (assault, penetrating trauma, etc, n = 15, 3.6%). The MOI was different between the age groups. The rate of fall as a MOI increased significantly with age (p < 0.0001) while the rate of patients involved in MVC either as pedestrians or in a vehicle decreased significantly with age (p < 0.0001).
Table 2.
Univariate analysis of demographic and clinical data by age groups
| Age 60-69 (n = 105) | Age 70-79 (n = 137) | Age ≥ 80 (n = 174) | P value † | |
|---|---|---|---|---|
| Age, years |
64.2 ± 3.0 |
74.9 ± 2.9 |
86.1 ± 4.9 |
|
| Gender, males * |
71 (67.6) |
82 (59.9) |
79 (45.4) |
<0.0001 |
| Mechanism of Injury (fall) * |
42 (40.0) |
86 (62.8) |
143 (82.2) |
<0.0001 |
| ISS ≥ 25 * |
56 (53.3) |
58 (42.3) |
70 (40.2) |
0.04 |
| GCS upon arrival ≤8 * |
24 (22.9) |
23 (16.9) |
30 (17.2) |
NS |
| Head AIS ≥ 3 * |
58 (55.2) |
97 (70.8) |
152 (87.4) |
<0.0001 |
| Number of regions injured |
2.61 ± 1.5 |
2.09 ± 1.4 |
1.55 ± 0.9 |
<0.0001 |
| Intubation upon arrival * |
16 (15.2) |
16 (11.7) |
20 (11.5) |
NS |
| Required surgery * |
52 (49.5) |
52 (38.0) |
52 (29.9) |
0.0008 |
| ICU admission * |
71 (67.6) |
74 (54.0) |
81 (46.6) |
0.0009 |
| Complications * |
30 (28.6) |
24 (17.5) |
35 (20.1) |
NS |
| Mortality * | 10 (9.5) | 23 (16.8) | 41 (23.6) | 0.003 |
Data are presented as mean (and SD) or number of patients (and percentage points) *.
† Chi-squared test for trends.
ISS Injury severity score, GCS Glasgow coma scale, AIS Abbreviated injury scale, ICU Intensive care unit.
Types of injuries
Head and facial trauma (median AIS = 4, range 1-5) was the most common type of injury (339/416 patients, 81.5%). Thoracic injuries occurred in 39.7% (165/416) of the patients, with rib fractures and/or flail chest being the most common thoracic injuries (88/165, 53.3%). Cervical spine injuries were present in 9.6% (40/416) of patients. Thoracic, lumbar, and sacral spine injuries were present in 10.1% (42 of 416) of patients. Abdominal injuries were present in 8.9% (37/416) of patients. Pelvic fractures were present in 12.5% (52/ 416) of the patients and long bones fractures in 20.7% (86/416).
Figure 1 shows the injury patterns according to age groups. Head and facial injuries were significantly more common in the ≥80 age group compared with the other groups (p = 0.0006). Injuries to the torso, extremities and spine were significantly less common in the ≥80 age group.
Figure 1.
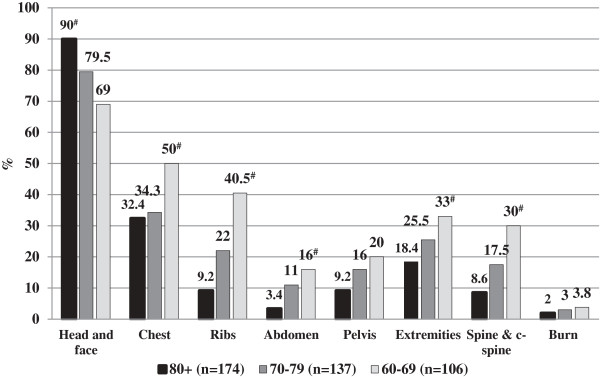
Injury patterns according to the different age groups (data shown as percentage points). # p < 0.05 Chi squared test for trends.
Co-morbidities
The impact of pre-existing co-morbidities on outcome was compared between patients who died and those who survived. On univariate analysis, only chronic renal failure (CRF) was associated with a poorer outcome (11 patients [14.9%] in the mortality group vs. 20 patients [4.8%] in the survival group, p = 0.013). Analysis of co-morbidities by the different age groups (60-69, 70-79 and ≥80) showed that hypertension (HTN) (16.2%, 43.1% and 49.4%, respectively, p = 0.035) and the chronic use of anti-coagulant treatment (4.8%, 9.5% and 12.6%, respectively, p = 0.018) were more common in the older age groups. Not surprisingly, the mean number of co-morbidities per patient increased significantly with age (0.77, 1.3, and 1.4, respectively, p = 0.023).
Complications
Eighty nine patients (21.4%) developed a total of 143 complications during the course of their hospital stay. Pulmonary complications were the most common and included pleural effusions (32, 7.7%), pneumonia (21, 5.0%) and atelectasis (20, 4.8%). Non-pulmonary complications included renal failure (11, 2.6%), septicemia (5, 1.2%) and wound infection (4, 1.0%). The total number of complications in the mortality group was significantly higher compared to the survival group (33 complications for 74 patients [44.6%] vs. 110 complications for 342 patients [32.2%], respectively, p = 0.044]. There were 62 patients (18.1%) who developed pulmonary complications and 24 patients (7.0%) who developed infectious complications in the survival group compared with 11 patients (14.9%) with pulmonary and 7 patients (9.5%) with infectious complications in the mortality group (differences not significant). The number of patients who developed complications was similar between the different age groups (30 patients [28.6%] with complications in the 60-69 group, 24 patients [17.5%] in the 70-79 group and 35 patients [20.1%] in the ≥80 group, p = 0.146) (Table 2).
In-hospital mortality
In-hospital mortality rate was 17.8% (74/416). One patient who died (1.4%) was discharged from the hospital but died within 30 days of the trauma and was therefore defined as hospital mortality. Thirty-three of the patients (5.5%) died within the first 24 hours of admission to our unit. Univariate analysis of clinical parameters is shown in Table 3. An increased mortality rate was observed in the ≥80 group compared with their younger counterparts and this was statistically significant (23.6% [41/174], vs. 16.8% in the 70-79 group [23/137], and 9.5% in 60-69 group [10/105], p = 0.003) (Table 2). MOI did not appear to affect mortality rate, with the exception of burns which had the highest mortality (7/11 patients, 64.6%). All patients with burns over ≥20% of body surface area died.
Table 3.
Univariate analysis of demographic and clinical parameters according to in-hospital outcome
| Mortality group (n = 74) | Survival group (n = 342) | P value | |
|---|---|---|---|
| Age, years |
79.8 ± 8.9 |
76.2 ± 9.7 |
0.003 |
| Gender, males * |
45 (60.8) |
187 (54.7) |
NS |
| ISS ≥ 25* |
62 (83.8) |
124 (36.3) |
<0.0001 |
| Mechanism of injury-fall * |
47 (63.5) |
224 (65.5) |
NS |
| Number of regions injured |
2.0 ± 1.5 |
1.99 ± 1.3 |
NS |
| Intubation upon arrival* |
26 (35.1) |
26 (7.6) |
<0.0001 |
| GCS upon arrival ≤8 * |
38 (51.4) |
40 (11.7) |
<0.0001 |
| Head AIS ≥ 3 * |
58 (78.4) |
250 (73.1) |
NS |
| Creatinine at arrival (mg %) |
136.1 ± 121.6 |
96.2 ± 52.3 |
<0.0001 |
| INR at arrival |
1.54 ± 0.9 |
1.18 ± 0.4 |
<0.0001 |
| Required surgery * |
30 (40.5) |
127 (37.1) |
NS |
| Required ICU stay * |
53 (71.6) |
173 (50.6) |
0.001 |
| Received blood products * |
50 (67.6) |
159 (46.5) |
0.001 |
| Complications * | 19 (25.7) | 70 (20.5) | NS |
Data shown as mean (and SD), or number of patients (and percentage points)*.
ISS Injury severity score, GCS Glasgow coma scale, AIS Abbreviated injury scale, INR International normalized ratio, ICU Intensive care unit.
Predictors of in-hospital mortality
Multivariate analysis was performed to analyze predictors of in-hospital death. Variables which were significant on univariate analysis (Table 3) were entered into a stepwise forward regression model. Variables entered included age, ISS, CRF, number of co-morbidities, intubation upon arrival at the trauma unit, GCS upon arrival, international normalized ratio (INR) at arrival, and the requirement for ICU and/or blood transfusion. Older age, CRF, low GCS, high INR, and the need for intubation were all found to be predictors of in-hospital mortality (Table 4). In order to underline the clinical relevance of our results, we applied well-established clinical cutoff points and categorized age (<80 and ≥80), INR (<1.2 and ≥1.2), and GCS (3-8, 9-13, and 14-15). Subsequently, age ≥ 80 (OR 2.29), GCS < 14 upon admission (OR 4.12), intubation in ED (OR 3.32), CRF (OR 3.65) and INR ≥ 1.2 (OR 3.53) were found to be significant predictors of in-hospital mortality.
Table 4.
Multivariate analysis of predictors of in-hospital mortality
| Adjusted OR | 95% CI | p value | |
|---|---|---|---|
| Age, years |
1.08 |
1.04-1.12 |
<0.0001 |
| GCS upon admission |
0.81 |
0.75-0.87 |
<0.0001 |
| Intubation in ED |
4.33 |
1.77-10.57 |
0.001 |
| CRF |
3.49 |
1.35-8.98 |
0.01 |
| INR | 2.38 | 1.45-3.91 | 0.001 |
OR Odds ratio, CI Confidence interval, GCS Glasgow coma scale, ED Emergency department, CRF Chronic renal failure, INR International normalized ratio.
Discussion
A six times greater mortality rate has been reported in elderly patients compared to younger trauma patients when taking into account the degree of injury [12]. We analyzed data on severely injured geriatric trauma patients treated at our level I trauma center. The major finding of this study is that pre-hospital parameters of age, and CRF, and initial in-hospital findings of a low GCS, the need for intubation, and an elevated INR can predict in-hospital mortality following severe trauma in an elderly population.
There is no consensus in the literature regarding the definition of a geriatric trauma patient and the age varies from 55 to 70 years old [13]. Some have defined geriatric trauma as patients over the age of 65 years corresponding to retirement policies. Furthermore, the rapidly increasing demographic changes in the elderly population over 80 years of age have led to a differentiation between old and the very old [14]. As previously been done, we divided our patients into 3 age categories: 60-69, 70-79 and ≥80. Our results show that the pattern of injury shifts gradually with these age groups.
The overall severity of the trauma load and its impact on the patient’s anatomy and physiology is usually expressed as an ISS of ≥ 16 [15]. Application of this score to an elderly population has been shown to be an inconsistent predictor of mortality [12,16]. A study by Tornetta et al [17] addressed the factors affecting morbidity and mortality in elderly trauma patients. The study included 326 elderly trauma patients over the age of 60 who had suffered from blunt trauma. Mean age of the patients in the study was 72, mean ISS was 19.7 and overall mortality was 18%. Perdue et al found that mortality in elderly patients was twice that of younger patients with comparable ISS [18]. In our study population, we found that on univariate analysis ISS was significantly higher in the non-survivor group (28.6 ± 10.9 vs. 21.7 ± 7.1, p < 0.0001). However, on multivariate analysis ISS was not a predictor of in-hospital mortality.
Traumatic brain injury in geriatric patients has been recognized to result in a worse outcome when compared to younger counterparts, with a low admission GCS commonly recognized as a poor prognostic indicator [19]. Head injury was predominant in all our age groups with a homogenous head AIS distribution. It was strongly associated with in-hospital mortality (p < 0.0001) and associated with other predictors of mortality: low GCS upon arrival and the need for pre-hospital intubation (both p < 0.0001). This finding was not surprising and is strongly supported in the literature [19-21]. It appears that in the elderly population, age and perhaps neurologic status upon arrival, as reflected in the need for intubation and GCS, are more consistent predictors of in-hospital mortality.
Blood pressure and heart rate are not consistently the most sensitive indicators of physiologic distress in an elderly trauma patient. Given that a history of HTN and beta blockade use in the elderly population is not uncommon, these parameters may be unreliable. More so, these classic physiologic parameters are less reliable in the pre-hospital evaluation of the elderly patient, and consequently, an occult shock state may go unrecognized resulting in under-triage and evacuation to a non-trauma center [22]. Thus, there is a need for additional clinical assessment tools in the elderly population to aid clinicians in diagnosis.
In the elderly, pre-existing co-morbidities can adversely affect a patient's recovery from a traumatic injury [23]. This can be attributed to physiological changes related to age as well as pre-existing co-morbidities and poly-pharmacy [24,25]. Hollis et al have demonstrated that pre-existing medical conditions and increased age are independent risk factors of mortality after trauma [26]. We examined co-morbidities which are well-known to affect survival. On univariate analysis only an elevated creatinine level and a previous diagnosis of CRF were associated with in-hospital mortality. Multivariate analysis showed CRF as a predictor of in-hospital mortality (OR 3.65, p = 0.005). It appears that other common medical conditions such as HTN, ischemic heart disease, and diabetes mellitus, or the number of co-morbidities, do not affect in-hospital mortality.
In major trauma, mortality in the elderly was found to be nearly double compared to mortality in the younger age group [27] and the complication death rate to be markedly higher, especially for pulmonary and infectious complications. It has been previously reported in orthopedic trauma patients with typical femoral fractures that pulmonary and infectious complications are predominant [28,29]. In our population, pulmonary and infectious complications did not appear to affect survival. However, the total number of complications was higher in non-survivors compared with survivors (p = 0.04).
Elderly trauma patients are often admitted to the ICU despite their potentially stable appearance because of their high propensity to deteriorate rapidly. Early transfer from the ED to the ICU allows the performance of thorough and continuous hemodynamic monitoring. In this setting, aggressive and targeted management can prevent hypoperfusion, reduce the incidence of multiple organ failure, improve survival, and allow a rapid diagnostic workup. As expected, we found that the requirement for ICU was significantly higher in the mortality group (71.6% vs. 50.6%, p = 0.001). Additionally, ICU admission was significantly higher in the 60-69 age group (67.6%), mainly due to more severe MOI, often MVC. However, on multivariate analysis, ICU stay was not a predictor of in-hospital mortality.
Low-energy falls have been reported to account for only 9–11% of injury-related deaths in the general population. However, in patients over the age of 65 they account for more than 50% of traumatic deaths [30-32]. Our results showed that MOI and distribution of injury varied between the age groups. Greater than 80% of trauma admissions in the ≥80 group were caused by falls resulting primarily in head trauma (90%). This may be due to the poor overall condition of the frail, elderly patient who stumbles and loses balance at home. Although fall as MOI was significantly more common with increasing age, it did not affect in-hospital mortality.
Limitations
Our analysis has several potential limitations. EMS crews in the Jerusalem district utilize age ≥ 60 as a criterion to transport patients to our level I trauma center, the only such center in the area. This study may have thus represented a population bias and therefore be limited in its ability to extrapolate our findings to other institutions. Patients were not analyzed based on hemodynamic status upon arrival, because criteria for hemodynamic instability are not clear and differ in age groups and individuals receiving medical treatment for pre-existing cardiovascular diseases. The presence of co-morbidities was based on data collection from the trauma registry with the intrinsic potential for error. Finally, this study was a retrospective review and is therefore susceptible to the inherent limitations.
Conclusions
Current trauma scoring systems are insufficient in directing management and predicting survival for elderly injured patients. We found that advanced age, especially age ≥80, low GCS, elevated INR, pre-existing CRF and the requirement for intubation on admission are the strongest independent predictors of mortality in elderly population following severe trauma. Further research comprising age and other medical-related parameters will help formulate more predictive trauma scores and advanced treatment algorithms to facilitate treatment.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MB: study conception, analysis and interpretation of data, drafting of manuscript. DW: study conception, analysis and interpretation of data, drafting of manuscript. DK: acquisition of data, analysis and interpretation of data. TBA: statistical analysis, analysis and interpretation of data. AIR: study conception, drafting of manuscript, critical revision. MAG: acquisition of data, analysis and interpretation of data. RE: statistical analysis, drafting of manuscript, critical revision. GA: study conception, analysis and interpretation of data, drafting of manuscript, critical revision. All authors read and approved the final manuscript.
Contributor Information
Miklosh Bala, Email: mikloshbala@gmail.com.
Dafna Willner, Email: dr.dafna@gmail.com.
Dima Klauzni, Email: dmitryk@hadassah.org.il.
Tali Bdolah-Abram, Email: taliba@savion.huji.ac.il.
Avraham I Rivkind, Email: avir@hadassah.org.il.
Mahmoud Abu Gazala, Email: mabugazala@hadassah.org.il.
Ram Elazary, Email: ramelazary@hadassah.org.il.
Gidon Almogy, Email: almogyg@yahoo.com.
References
- World health organization. 10 facts on ageing and the life course. http://www.who.int/features/factfiles/ageing/en/index.html Assessed August 2013.
- State of Israel. Ministry of health. Leading causes of death in Israel 2000-2010. http://www.health.gov.il/English/News_and_Events/Spokespersons_Messages/Pages/10032013_1.aspx. Ministry of health. Assessed Feb 2013.
- MacKenzie EJ, Morris JA, Smith GS, Fahey M. Acute hospital costs of trauma in the United States: implications for regionalized systems of care. J Trauma. 1990;21:1096–1103. doi: 10.1097/00005373-199009000-00005. [DOI] [PubMed] [Google Scholar]
- Court-Brown CM, Clement N. Four score years and ten: an analysis of the epidemiology of fractures in the very elderly. Injury. 2009;21:1111–1114. doi: 10.1016/j.injury.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Rushing AM, Scalea TM. Trauma resuscitation of the elderly patient. Clinics Geriatr. 2010;21:34–36. [Google Scholar]
- Kuhne CA, Ruchholtz S, Kaiser GM, Nast-Kolb D. Working group on multiple trauma of the German society of trauma. Mortality in severely injured elderly trauma patients–when does age become a risk factor? World J Surg. 2005;21:1476–1482. doi: 10.1007/s00268-005-7796-y. [DOI] [PubMed] [Google Scholar]
- Probst C, Zelle BA, Sittaro NA, Lohse R, Krettek C, Pape HC. Late death after multiple severe trauma: when does it occur and what are the causes? J Trauma. 2009;21:1212–1217. doi: 10.1097/TA.0b013e318197b97c. [DOI] [PubMed] [Google Scholar]
- Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA. 2011;21:1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- Grossman MD, Ofurum U, Stehly CD, Stoltzfus J. Long-term survival after major trauma in geriatric trauma patients: the glass is half full. J Trauma Acute Care Surg. 2012;21:1181–1185. doi: 10.1097/TA.0b013e31824d0e6d. [DOI] [PubMed] [Google Scholar]
- Clement ND, Tennant C, Muwanga C. Polytrauma in the elderly: predictors of the cause and time of death. Scand J Trauma Resusc Emerg Med. 2010;21:26. doi: 10.1186/1757-7241-18-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Aalst JA, Morris JA Jr, Yates HK, Miller RS, Bass SM. Severely injured geriatric patients return to independent living: a study of factors influencing function and independence. J Trauma. 1991;21:1096–1101. [PubMed] [Google Scholar]
- Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: injury patterns and outcome. J Trauma. 1984;21:565–572. doi: 10.1097/00005373-198407000-00003. [DOI] [PubMed] [Google Scholar]
- Jacobs DG, Plaisier BR, Barie PS, Hammond JS, Holevar MR, Sinclair KE, Scalea TM, Wahl W, EAST Practice Management Guidelines Work Group. Practice management guidelines for geriatric trauma: the EAST practice management guidelines work group. 2001. http://www.east.org/tpg/geriatric.pdf. Accessed 15 May 2013. [DOI] [PubMed]
- McMahon DJ, Shapiro MB, Kauder DR. The injured elderly in the trauma intensive care unit. Surg Clin North Am. 2000;21:1005–1019. doi: 10.1016/S0039-6109(05)70110-9. [DOI] [PubMed] [Google Scholar]
- Sikand M, Williams K, White C, Moran CG. The financial cost of treating polytrauma: implications for tertiary referral centres in the United Kingdom. Injury. 2005;21:733–737. doi: 10.1016/j.injury.2004.12.026. [DOI] [PubMed] [Google Scholar]
- Sharma OP, Oswanski MF, Sharma V, Stringfellow K, Raj SS. An appraisal of trauma in the elderly. Am Surg. 2007;21:354–358. [PubMed] [Google Scholar]
- Tornetta P 3rd, Mostafavi H, Riina J, Turen C, Reimer B, Levine R. et al. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;21:702–706. doi: 10.1097/00005373-199904000-00024. [DOI] [PubMed] [Google Scholar]
- Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: Geriatric status increases risk of delayed death. J Trauma. 1998;21:805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- Utomo WK, Gabbe BJ, Simpson PM, Cameron PA. Predictors of in-hospital mortality and 6-month functional outcomes in older adults after moderate to severe traumatic brain injury. Injury. 2009;21:973–977. doi: 10.1016/j.injury.2009.05.034. [DOI] [PubMed] [Google Scholar]
- Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;21:1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmons T, Menaker J. Traumatic brain injury in elderly. Clinics Geriatr. 2010;21:20–24. [Google Scholar]
- Salottolo KM, Mains CW, Offner PJ, Bourg PW, Bar-Or D. A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med. 2013;21:7. doi: 10.1186/1757-7241-21-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB. Centers for disease control and prevention (CDC). Guidelines for field triage of injured patients: recommendations of the national expert panel on field triage, 2011. MMWR Recomm Rep. 2012;21:1–20. [PubMed] [Google Scholar]
- Niven DJ, Kirkpatrick AW, Ball CG, Laupland KB. Effect of comorbid illness on the long-term outcome of adults suffering major traumatic injury: a population-based cohort study. Am J Surg. 2012;21:151–156. doi: 10.1016/j.amjsurg.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Heffernan DS, Thakkar RK, Monaghan SF, Ravindran R, Adams CA Jr, Kozloff MS, Gregg SC, Connolly MD, Machan JT, Cioffi WG. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;21:813–820. doi: 10.1097/TA.0b013e3181f41af8. [DOI] [PubMed] [Google Scholar]
- Hollis S, Lecky F, Yates DW, Woodford M. The effect of pre-existing medical conditions and age on mortality after injury. J Trauma. 2006;21:1255–1260. doi: 10.1097/01.ta.0000243889.07090.da. [DOI] [PubMed] [Google Scholar]
- Giannoudis PV, Harwood PJ, Court-Brown C, Pape HC. Severe and multiple trauma in older patients; incidence and mortality. Injury. 2009;21:362–367. doi: 10.1016/j.injury.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Liem IS, Kammerlander C, Raas C, Gosch M, Blauth M. Is there a difference in timing and cause of death after fractures in the elderly? Clin Orthop Relat Res. 2013;21:2846–2851. doi: 10.1007/s11999-013-2881-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan HB, MacDonald DA, Matthews SJ, Giannoudis PV. Incidence and causes of mortality following acute orthopaedic and trauma admissions. Ann R Coll Surg Engl. 2004;21:156–160. doi: 10.1308/003588404323043256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SP, Harvey AH. Fall injuries in the elderly. Clin Geriatr Med. 1985;21:501–512. [PubMed] [Google Scholar]
- Hogue CC. Injury in late life. Part I. Epidemiology. J Am Geriatr Soc. 1982;21:183–190. doi: 10.1111/j.1532-5415.1982.tb01302.x. [DOI] [PubMed] [Google Scholar]
- Shortt NL, Robinson CM. Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma. 2005;21:396–400. doi: 10.1097/01.bot.0000155311.04886.7e. [DOI] [PubMed] [Google Scholar]


