Abstract
Background and Purpose
Racial and geographic disparities in stroke mortality have been documented for over 50 years, and for those aged 45 to 64 are among the largest for any disease. The causes of the disparities have been mysterious; however, investments by NINDS, NHLBI and CDC are now providing insights into the causes.
Methods
Complementary study designs provide information on different aspects of the disparities. Vital statistics data track temporal patterns in stroke mortality, an objective index of the success in overcoming the disparities. Surveillance studies assess of the contributions of incidence versus case fatality to the disparities, a distinction critical to guide efforts to reduce the disparities. Finally, cohort studies give insights to the contribution of specific risk factors to disparities in either incidence or case fatality, allowing targeted interventions.
Results
While deaths from stroke mortality declined by a third in the most recent eleven years, there has been a 35% increase in the black-white disparity and little change in geographic disparities. Surveillance studies suggest that the black-white disparity is primarily attributable to differences in incidence, and also have potentially unmasked Hispanic-white differences in incidence that are not apparent in mortality trends. Longitudinal cohort studies are suggesting multiple targets for intervention such as a multi-dimensional impact of blood pressure on the black-white differences.
Conclusion
After suffering these disparities over a half-century, information is now emerging to allow us to better understand the underpinnings of the disparities and potentially enter a new era of targeted interventions to reduce these disparities.
Introduction
One of the two key goals of the Healthy People 2010 statement, the guiding document for the United States Department of Health and Human Services, was “is eliminate health disparities among different segments of the population” by the year 2010.1 The US Congress has by law directed NIH to specifically define health disparities to include the components:
Minority health research and related activities
Rural health research and related activities
Research and other activities related to the socioeconomically disadvantaged in the urban setting.2
For brevity, we focus on a review the magnitude of disparities in stroke of only the first two of these disparities, review progress in reducing these disparities, and assess barriers and opportunities to reduce these disparities.
Minority Health Research and Related Activities
Racial differences in stroke mortality are the most well-known and well-documented of the stroke disparities.3–5 Among non-Hispanics between the ages of 45 and 64, in 2009 there were 4,359 deaths from stroke and an age-adjusted death rate of 48.9/100,000 in blacks, while there were 9,994 deaths and a death rate of 16.3/100,000 in whites; this represents a three-fold difference in death rates.6 There would have been approximately 3000 fewer deaths for blacks in this 20-year age range had they the mortality rate of whites (4,359 * (16.3/48.9) = 1,424 projected deaths for a reduction of 2,935 deaths). If the case-fatality rate is 20%, then these 3000 deaths would have arisen from approximately 15,000 “extra” stroke events (3000 / 0.2 = 15,000) and a public health burden of the racial disparity in stroke is approximately $2.1 billion dollars annually (assuming a $140,000 cost of stroke7).
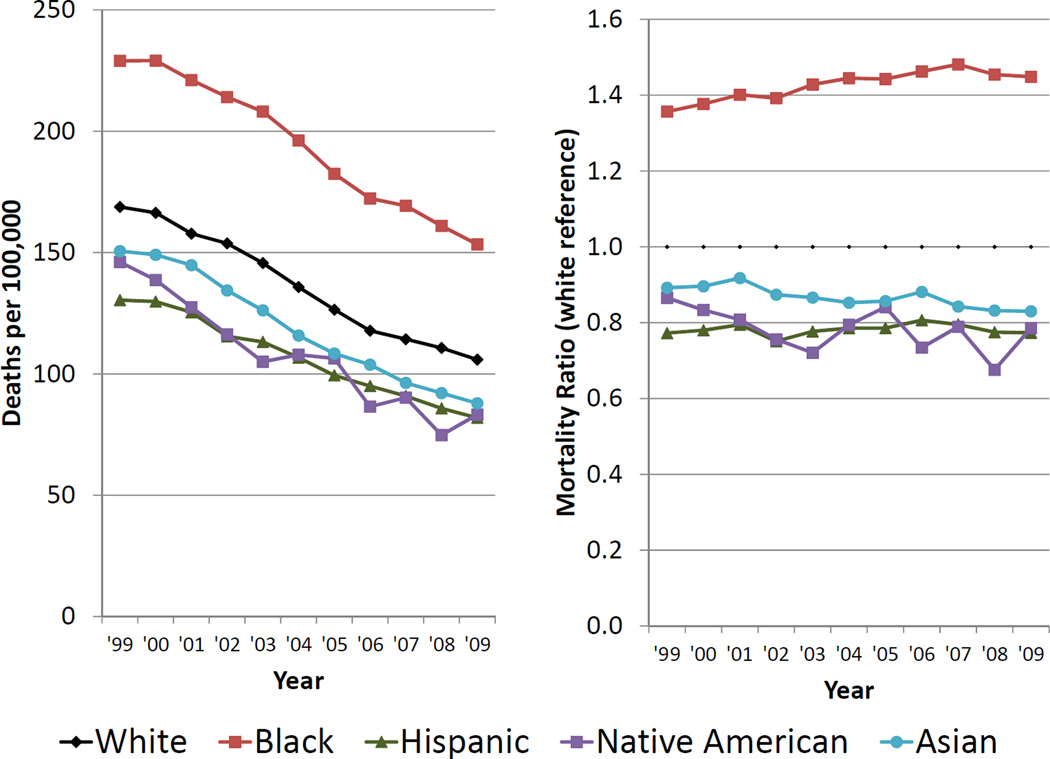
The racial disparity in stroke mortality has been remarkably persistent, where between 1949 and 1951 the nonwhite (primarily African American) to white stroke mortality ratio was 1.63 for men and 1.92 for women (reported in the very first volume of Stroke!).8 Using CDC Wonder,6 for ages 45 and over there was a remarkable 37% decline in the age-adjusted cerebrovascular disease mortality between 1999 and 2009 (1999: 173.2/100,000 → 2009: 108.6/100,000). While there was a decline for each race/ethnic group, the cerebrovascular disease death rates (ICD 10: I60 – I69) are strikingly higher for blacks than for whites, and marginally lower for Hispanics, Native Americans and Asians than for whites (Figure 1A). While the cerebrovascular death rates are falling for both whites and blacks, it is falling consistently faster for whites – resulting in an 26% increase in the black-to-white mortality ratio from 1.36 in 1999 to 1.45 in 2009 (Figure 1B); hence, while cerebrovascular deaths are falling for both blacks and whites, with the exception of the past two years (where there have been minor declines in the black-white disparity in stroke, the magnitude of the black-to-white disparity in stroke is consistently and rapidly growing. Relative to whites, declines in cerebrovascular deaths for Asians (1999 ratio of 0.89, 2009 ratio of 0.83) and Native Americans (1999 ratio of 0.87, 2009 ratio of 0.79) appear marginally faster than in whites, while declines for Hispanic (1999 ratio of 0.77, 2009 ratio of 0.77) are at approximate a similar magnitude as whites (Figure 1B).
Figure 1.
Race/ethnic differences in deaths from cerebrovascular disease (ICD 10: I60 – I69) for US residents aged 45 and above. Figure 1A (left) shows the age-adjusted (year 2000 standard) death rate per 100,000 for mutually exclusive race/ethnic strata: non-Hispanic whites (White), non-Hispanic blacks (Black), Hispanic (all races), non-Hispanic Native American/Alaska Natives (Native American), and non- Hispanic Asians (Asian). Figure 1B (right) shows the cerebrovascular disease mortality ratio for minority groups relative to non-Hispanic whites.
Over the past 15 years National Institute for Neurological Disorders and Stroke (NINDS) has funded observational epidemiological studies that have provided valuable insights to the causes of the racial disparities in stroke. Despite the racial disparity in stroke mortality being well-described in publications since the mid-1970’s, as late as the mid-1990’s it was not clear whether the higher mortality among blacks was attributable to a higher incidence of stroke or a worse case fatality from stroke. Stroke surveillance studies in racially-diverse communities addressed this knowledge gap when in 1998 the Northern Manhattan Stroke Study (NOMAS, or subsequently NOMAS) reported that the black-to-white stroke incidence ratio was 2.4,9 a finding supported by the an estimated 2.0 black-to-white incidence ratio in the 2004 report of Greater Cincinnati / Northern Kentucky Stroke Study (GCNKSS).10 These findings from specific communities have subsequently been supported by national data on black-white differences in stroke incidence.11 These data seem to suggest that it is critical to guide interventions to reduce the black-white disparities to primarily focus on incidence of incident stroke events through primary (or primordial) prevention, rather than efforts to reduce case fatality through improved stroke treatments. However, temporal increases in the magnitude of the black-white disparity may potentially be attributed a more rapid access by whites (and non-southerners) to acute stroke care units that shown to improve outcomes following stroke,12 and as such secondary attention could potentially be focused on stroke care to reduce the black excess in stroke mortality.
Simultaneously, NOMAS estimated the Hispanic-to-white stroke incidence ratio to be 2.0 for Hispanics in Manhattan,9 a finding supported for Mexican Americans in the Brain Attack Surveillance in Corpus Christi (BASIC) study estimating a Hispanic-to-white incidence ratio of 2.00 for ages 45–59, 1.57 for ages 60–74, and 1.13 for ages over age 75.13 The paradox of higher stroke incidence, but lower stroke mortality (see Figure 1B), among Hispanics is potentially related to misreporting of ethnicity in the vital statistics system; underscoring the importance of these targeted surveillance studies using more standard definition to identify disparities that might well otherwise go undetected. However, it has been suggested that reporting of Hispanic ethnicity in the vital statistics is “relatively good,”14 a finding supported by concordance (sensitivity, specificity and accuracy) in access of 95% between self-reported race and vital statistics among 480 deaths in the BASIC study,15 making it somewhat unlikely that misreporting totally explains this paradox. Alternatively, there is also the possibility that Hispanic-white ethnic differences in stroke mortality are also confounded with Hispanic-white geographic differences in stroke mortality. Specifically, between 2007 and 2009, there was a sufficient Hispanic population for the CDC to report smoothed Hispanic mortality rates in 635 of the 3,141 (20%) counties in the US, while they reported smoothed white mortality for 3115 of the 3141 (99%) of the counties (smoothing of rates making the reporting of county-level mortality more reliable).16 New York County (largely Manhattan, the location of the NOMAS Study) had a stroke mortality of 39.2/100,000 for Hispanics which was in the 9th percentile of counties reporting Hispanic mortality; however, the stroke mortality for whites was 36.7/100,000 the 5th lowest of the 3115 counties reported (i.e., in the 0th percentile of counties reporting white mortality). Hence, NOMAS was conducted in a county with a low relative Hispanic mortality compared to other regions, but New York County has even lower relative white stroke mortality (in fact, white stroke mortality in the City of New York has lowest white stroke mortality in the nation, with Kings County a rank of 1, Richmond County a rank of 2, Queens county a rank of 3, New York County a rank of 5, Bronx County a rank of 7 and Nassau county a rank of 15 of the 3115 counties reporting white mortality). Likewise, Nueces County, Texas (the location of the BASIC Study) has a Hispanic stroke mortality of 95.1/100,000 which is in the 88th percentile of counties reporting Hispanic mortality; while the white stroke mortality is 86.0/100,000 which is in the 53rd percentile of counties reporting white morality. Hence, another possible explanation of the paradox of high stroke incidence but low stroke mortality for Hispanics is that the NOMAS study is being conducted in a county with low Hispanic mortality but strikingly lower white stroke mortality, while the BASIC study is being conducted in a county with high Hispanic mortality but average white stroke mortality.
Because there are few sources on temporal changes in stroke incidence, the causes for the decline in stroke mortality, and impact of these declines on racial disparities, remains a mystery. Early reports from predominately white communities have suggested only a modest decline in stroke incidence that is likely insufficient to account for the dramatic declines in stroke mortality.17, 18 Recent reports from GCNKSS have fuelled this mystery with indications that stroke incidence rates appear to be falling for whites but not for blacks, potentially contributing to the 35% increase in the black-to-white mortality ratio between 1999 and 2007.19 The decline in stroke mortality was recognized as one of the “Ten Great Public Health Achievements” for the previous century;20 however, we cannot expect to sustain the decline in stroke mortality without understanding its cause, again underscoring the importance of the sustained funding for stroke surveillance studies.
While surveillance studies have provided insights to the changing pattern of stroke risk (incidence, case fatality and mortality), surveillance studies do not have data on risk factors prior to the stroke event, and as such are limited with respect to providing insights to guide interventions to reduce disparities in stroke incidence. Longitudinal cohort studies that are complementary to surveillance studies can address this knowledge gap, and include studies such as the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study,21 the longitudinal cohort in the NOMAS study, 22 the Atherosclerosis Risk in Communities (ARIC) study,23 the Cardiovascular Health Study (CHS),24 and the Multi-Ethnic Study of Atherosclerosis.25 As surveillance studies have shown the importance of racial disparities in stroke incidence, reducing the disparity in stroke must be through primary (or primordial) prevention efforts to reduce stroke incidence disparities, with treatment of stroke playing a secondary role in efforts to reduce racial disparities in stroke. While summarizing all findings from longitudinal studies focused on disparities in stroke incidence is beyond the scope of this report, some of the findings particularly pertinent to guiding interventions to reduce disparities is provided herein.
The National Health and Examination Survey (NHANES) study estimated approximately one-third of the black excess stroke incidence risk could be attributed to disparities in “traditional” risk factors (hypertension, diabetes, smoking, etc.).26 However, this effort was limited by a small number of blacks (1,362) and by the lack of physician adjudication of stroke events. The REGARDS study recently updated this effort,27 finding that the racial disparity in incidence is primarily below the age of 65, and in this age range approximately one-half of the racial disparity in stroke incidence is attributable to “traditional” risk factors (i.e., the those in the Framingham Stroke Risk Profile28).
There are major implications of this observation to guide interventions to reduce racial disparities. Specifically, because much of the disparity is attributable to disparities in the prevalence of these risk factors at the baseline visit, efforts to reduce the racial disparity through these risk factors must focus on reducing the disparities in risk factor prevalence (i.e., eliminating the excess prevalence of hypertension and diabetes in blacks) rather than improved treatment of prevalent risk factors. Noting that a higher prevalence is the product of some combination of a higher incidence or lower case fatality, it is almost certain that the racial disparities in risk factor prevalence are attributable to racial disparities in risk factor incidence, since: 1) the alternative explanation of a lower mortality of African Americans with the risk factors reducing the prevalence ratio seems unlikely, and 2) it has been shown that African Americans have a higher incidence of hypertension (the single most potent risk factor for stroke) than whites all ages up to 75 years.29 Hence, to reduce the black-to-white differences in risk factor prevalence we must reduce the black-to-white differences in the incidence of these traditional risk factors. Efforts to “go upstream” to address disparities in the incidence of stroke risk factors will be key to address the half of the disparity attributable to these traditional risk factors.
There is also the opportunity to reduce racial disparities in stroke incidence by a better understanding of pathways that do not involve these traditional risk factors. These pathways may include: 1) racial differences in the impact of risk factors (for example, that similar elevations of blood pressure may impart more risk in blacks than whites), 2) lack of adequate quantification of known risk factors (i.e., residual confounding), 3) nontraditional or “novel” risk factors, and 4) measurement error of the known risk factors.27 REGARDS and other studies are focusing efforts to advance the understanding of the potential role of each of these pathways – with very promising early findings to provide insights to target to reduce racial disparities. Examples of findings include: 1) documentation that blacks are actually more aware and more likely to be treated for hypertension, but that the treatment is much less likely to result in achieving blood pressure goals,30 2) the potential that risk factors may in fact be have a differential impact in blacks and whites, with (for example) elevated levels of SBP being associated with approximately a three-fold larger increase risk of stroke in blacks than whites,31 3) that after control for blood pressure levels, racial differences in duration of hypertension could be playing a substantial role in differential stroke risk,31 and 4) numerous “novel” risk factors could be contributing to racial disparities in stroke incidence including disparities in the prevalence of stroke symptoms,32 racial differences in awareness and treatment of atrial fibrillation,33 racial differences in stroke severity arising from population stratification introduced through a genetic differences in hypertension or other risk factors,34 differential impact of markers of inflammation including C-reactive protein (CRP),35 racial differences in the age of menopause,36 the role of diet, including differences in fish consumption,37 and systemic infections such as tooth loss.38 While much work remains, understanding these new pathways that potentially contribute to racial disparities in stroke incidence is a key first step to guiding the interventions to reduce this immense public health burden.
In conclusion regarding racial/ethnic disparities, while stroke mortality is declining, the magnitude of black-white disparity in stroke mortality is consistently and rapidly increasing. In the past 15 years, NINDS-funded surveillance studies have documented that the black-to-white disparity in stroke mortality is primarily attributable to disparities in stroke incidence, and have also documented substantial Hispanic-to-white disparities in stroke incidence (despite the lack of disparities in stroke mortality). NINDS-funded longitudinal cohort studies are rapidly accruing data and substantial contributions to the understanding of the black-to-white disparity in incidence are in process; however, continued investments in surveillance studies and newer cohort studies including Hispanics would help to clarify whether the Hispanic-to-white disparity in incidence remains.
Rural health research and related activities
Despite NIH explicitly defining rural health as a focus of disparities,2 and despite acknowledgement of opportunities for rural epidemiology of chronic diseases,39 to the knowledge of the author there are only a handful of papers contrasting stroke risk (mortality, incidence or prevalence) for the US in urban versus rural areas. A review of stroke in rural areas and small communities40 offered a single publication documenting a 1.45-times higher prevalence of stroke in rural over urban areas (the data was provided in a table, with no comment in the text).41 Recently, Sergeev reported a rural-to-urban mortality ratio of 1.37 for states outside the stroke belt between the years of 2000 to 2006.42 There appears to be no report of urban versus rural differences in stroke incidence.
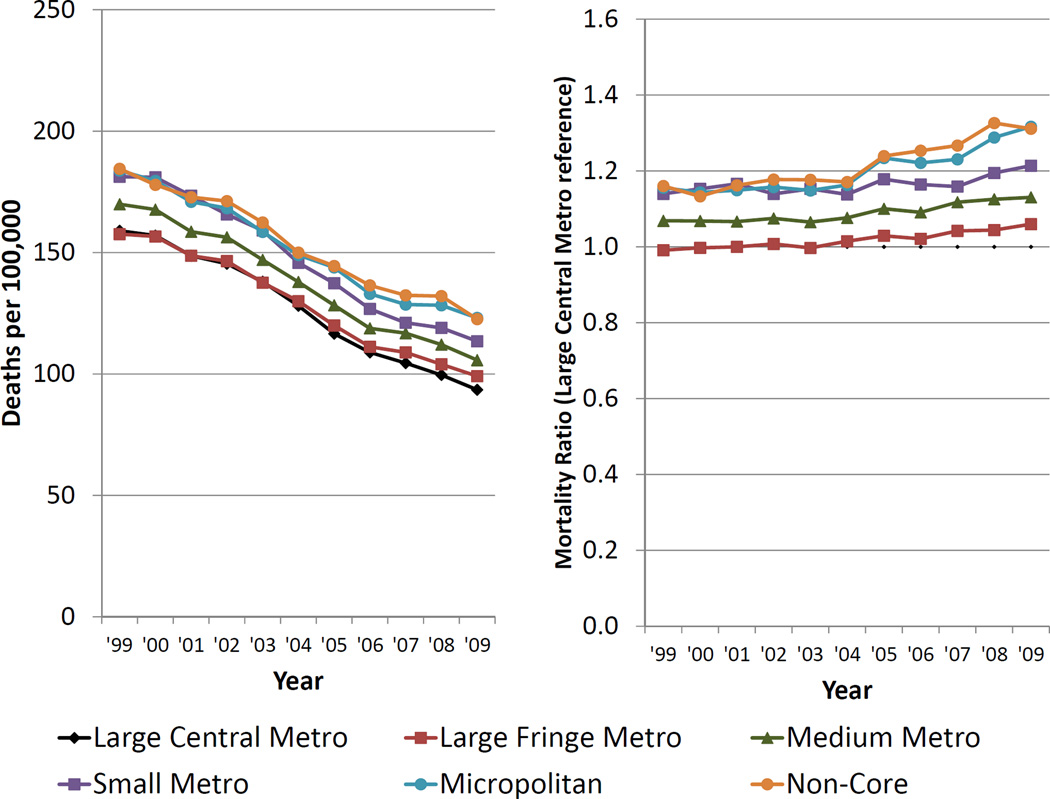
The CDC WONDER also provides the opportunity to assess urban-rural differences in stroke using the NCHS Urban-Rural Classification Scheme, which scales counties on a 6-point scale from Large Central Metro (most urban) to Non-Core (most rural).6 Estimates of stroke mortality for the non-Hispanic white (population restricted to avoid confounding with race) population over age 45 is shown in Figure 2, where for early years (1999–2003) there appears to be little differences in stroke mortality for the two most urban classifications (Large Central Metro and Large Fringe Metro); however, after this period there appears to be a less rapid decline in the Large Fringe Metro regions relative to the Large Central Metro regions resulting in approximately 5% increase in their relative risk. Over that same period 1999 to 2004 the Medium Metro areas showed pattern of a relatively constant 6%–7% excess risk relative to the Large Central Metro regions; however, since that time the relative risk in these regions also appears to be steadily increasing to a 13% excess. There was a similar pattern of increases for the three less rural classes (Small Metro, Micropolitan, and Non-Core) have a risk approximately 15% higher the Large Central Metro regions; but even larger increases to a 21% excess for the Small Metro regions, and to 31% excesses for the Micropolitan and Non-Core regions. Hence, while the magnitude of the higher stroke mortality in more rural regions was stable between 1999 and 2004, since that time the disparity appears to be growing with faster increases in the disparity the more rural the region. Secondary analysis including all race-ethnic groups showed similar patterns (data not shown). With the potential that rural-urban disparities in stroke potentially increasing, there is much work remaining in this area.
Figure 2.
Urban-rural differences in deaths from cerebrovascular disease (ICD 10: I60 – I69) for US non- Hispanic white residents aged 45 and above. Figure 2A (left) shows the age-adjusted (year 2000 standard) death rate per 100,000 by the NCHS Urban-Rural Classification Scheme for counties classified as large central metro (most urban), large fringe metro, medium metro, small metro, micropolitan, or non-core (most rural). Figure 2B (right) shows the cerebrovascular disease mortality ratio for urbanrural groups relative to large central metro.
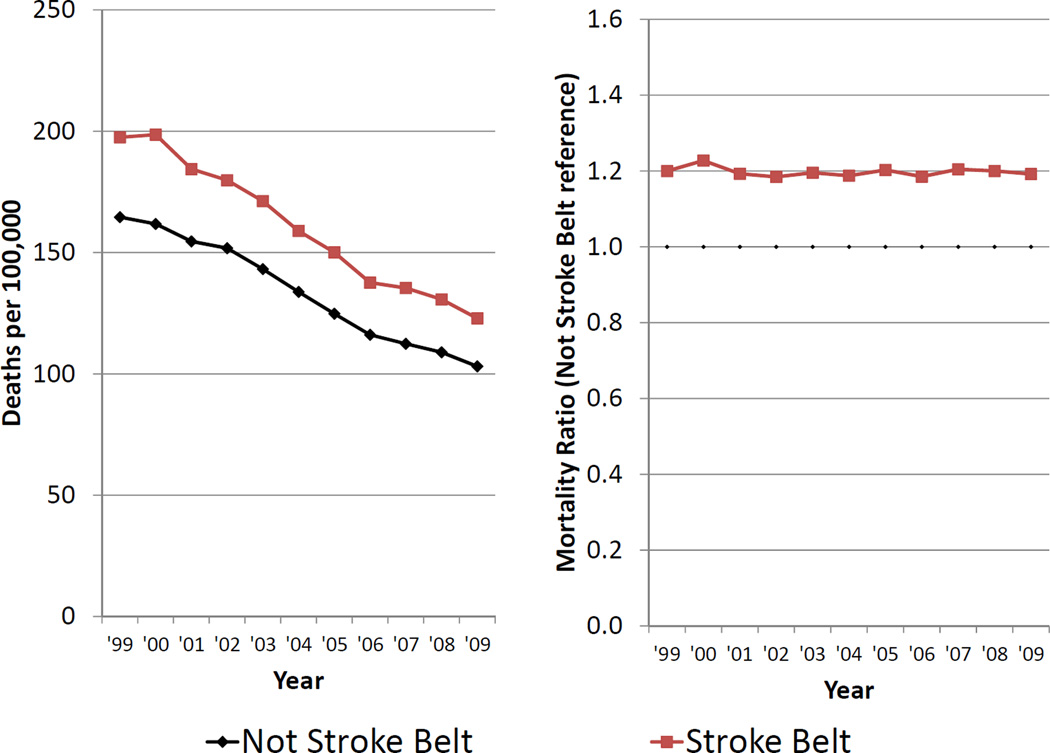
However, in a closely related area there has been a been a well-documented geographic disparity in stroke mortality, specifically a higher stroke mortality in the southeastern region of the US, that has been documented to exist for over a half-century.43 The average stroke mortality is approximately 20% to 25% higher in the stroke belt than the rest of the nation; however, there is substantial heterogeneity in stroke mortality risk both in and out of the region, and stroke mortality for specific regions (such as the “buckle of the stroke belt” along the coastal plain of North Carolina, South Carolina and Georgia) is as much as 300% higher than the lowest risk regions in the non-belt (New York City, Miami, etc.).44 The pattern of stroke mortality in the Stroke Belt and non-Stroke Belt is shown in Figure 3 for non-Hispanic whites (to avoid confounding with race). While there have been dramatic declines in stroke mortality in both regions, there the excess stroke mortality has been nearly constantly 20% higher in the stroke belt region over this entire observation period (data not shown).
Figure 3.
Stroke Belt versus non-Stroke Belt differences in deaths from cerebrovascular disease (ICD 10: I60 – I69) for non-Hispanic white US residents aged 45 and above. Figure 3A (left) shows the ageadjusted (year 2000 standard) death rate per 100,000 by the REGARDS defined stroke belt (states of North Carolina, South Carolina, Georgia, Tennessee, Alabama, Mississippi, Arkansas and Louisiana) and non-stroke belt regions (all states not included in the stroke belt). Figure 3B (right) shows the cerebrovascular disease mortality ratio for the stroke belt relative to the non-stroke belt.
The NINDS-funded REGARDS study has a co-primary focus on advancing the understanding of the causes of the stroke belt. Initial examination of regional differences (i.e. stroke belt versus non-stroke belt) in incidence were non-significant;11 however, additional analyses on a the county-level are needed to evaluate the relative contributions of regional differences in stroke incidence versus stroke case-fatality. REGARDS also documented that the Stroke Belt region also has a more rapid rate of cognitive decline, suggesting that more global measures of cerebrovascular health may also be affected by factors in the region.45 Prior to REGARDS, there were few data describing geographic disparities in the distribution of risk factor prevalence that may be contributing to the geographic disparities in incidence,46, 47 primarily reporting a higher prevalence of hypertension in the region.48, 49 Data from REGARDS confirmed the geographic disparity in hypertension, and noted a larger geographic disparity in the prevalence of diabetes; however, again the relatively small disparities in these traditional risk factors may not be sufficient to account for the disparities in incidence (suggesting other factors are playing a role).50 REGARDS is currently investigating potential causes of the geographic disparities in traditional and novel risk factors including less access to care,51 regional differences in the age of menopause (with the stroke belt having an average age of menopause 10 months earlier than the rest of the nation),36 a lack of smoking differences in whites and lower smoking exposure for blacks,52 lower intake of non-fried fish and higher intake of fried fish,37 a lower intake of fiber, potassium, magnesium, and calcium, but a higher intake of cholesterol, for men,53 and higher markers of inflammation and tooth loss due to gum disease;38 however, there was a 10% lower use of aspirin for prophylactic use in the region.54 As such, REGARDS is well underway in assessing geographic differences in prevalence of non-traditional risk factors, and is poised to perform mediation analysis to assess their role in the excess stroke risk in the region.
In summary of geographic disparities, while the NIH has focused on rural/urban differences in their definition of disparities, little work has been performed to assess such disparities in stroke. More work has been performed on the related geographic disparity of higher stroke in the Southeastern US. Data from REGARDS suggests a higher stroke incidence in the region that is contributing some, but not all, of the geographic disparity in stroke mortality. There are sizable differences in the distribution of traditional and novel risk factors, but additional work is required to assess the relationship of the geographic differences in risk factors to the geographic disparities in stroke risk.
Conclusion
While deaths from stroke are rapidly declining, the black-to-white disparity in stroke risk is increasing and geographic disparities in stroke appear to be stable or increasing. There is solid progress in understanding the causes of the racial disparity in stroke risk, and this information holds promise to guide interventions that may decrease the racial disparity. In addition, more work is certainly warranted to better understand the potential stroke disparities in the Hispanic population, the largest US minority group. The focus of NIH on geographic disparities has been on urban/rural differences, an interesting area that has largely not been investigated for stroke. However, substantial efforts are underway to better understand geographic disparities associated with the Stroke Belt. This disparity appears to be at least partially attributable to increased incidence of stroke in the region, with this increase only being partially attributable to “traditional” risk factors. More work is needed to better understand the role of non-traditional risk factors or other pathways that could contribute to this substantial disparity.
Acknowledgments
The research reported in this article was supported by cooperative agreement NS 041588 from the National Institute of Neurological Disorders and Stroke
Funding Sources: The author has NIH-NINDS grant support for the REasons for Geographic And Racial Differences in Stroke (REGARDS) study - NS 041588.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None.
References
- 1.Services USDoHaH. Health people 2010: Understanding and improving health. 2000 [Google Scholar]
- 2.Minority health and health disparities research and education act. 2000;106–525:2498. [Google Scholar]
- 3.Gillum RF. Stroke mortality in blacks. Disturbing trends. Stroke a journal of cerebral circulation. 1999;30:1711–1715. doi: 10.1161/01.str.30.8.1711. [DOI] [PubMed] [Google Scholar]
- 4.Howard G, Howard VJ, Geographic REf. Racial Differences in Stroke I. Ethnic disparities in stroke: The scope of the problem. Ethnicity & disease. 2001;11:761–768. [PubMed] [Google Scholar]
- 5.Cooper ES. Cardiovascular diseases and stroke in african americans: A call for action. Journal of the National Medical Association. 1993;85:97–100. [PMC free article] [PubMed] [Google Scholar]
- 6.Compressed mortality file 1999–2009. Cdc wonder online database, compiled from compressed mortality file 1999–2009 series 20 no. 2o. 2012 [Google Scholar]
- 7.Dicarlo A. Human and economic burden of stroke. Age Aging. 2009;38:4–5. doi: 10.1093/ageing/afn282. [DOI] [PubMed] [Google Scholar]
- 8.Wylie CM. Death statistics for cerebrovascular disease: A review of recent findings. Stroke a journal of cerebral circulation. 1970;1:184–193. doi: 10.1161/01.str.1.3.184. [DOI] [PubMed] [Google Scholar]
- 9.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and hispanic residents of an urban community: The northern manhattan stroke study. American journal of epidemiology. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 10.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, et al. Stroke in a biracial population: The excess burden of stroke among blacks. Stroke; a journal of cerebral circulation. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 11.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of neurology. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webster F, Saposnik G, Kapral MK, Fang J, O'Callaghan C, Hachinski V. Organized outpatient care: Stroke prevention clinic referrals are associated with reduced mortality after transient ischemic attack and ischemic stroke. Stroke a journal of cerebral circulation. 2011;42:3176–3182. doi: 10.1161/STROKEAHA.111.621524. [DOI] [PubMed] [Google Scholar]
- 13.Lisabeth LD, Smith MA, Sanchez BN, Brown DL. Ethnic disparities in stroke and hypertension among women: The basic project. American journal of hypertension. 2008;21:778–783. doi: 10.1038/ajh.2008.161. [DOI] [PubMed] [Google Scholar]
- 14.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and hispanic origin reporting on death certificates in the united states. Vital and health statistics. Series 2, Data evaluation and methods research. 2008:1–23. [PubMed] [Google Scholar]
- 15.Caveney AF, Smith MA, Morgenstern LB, Lisabeth LD. Use of death certificates to study ethnic-specific mortality. Public health reports. 2006;121:275–281. doi: 10.1177/003335490612100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Control CfD. Interactive atlas of heart disease and stroke tables. 2012;2012 [Google Scholar]
- 17.Broderick JP. Stroke trends in rochester, minnesota, during 1945 to 1984. Annals of epidemiology. 1993;3:476–479. doi: 10.1016/1047-2797(93)90099-p. [DOI] [PubMed] [Google Scholar]
- 18.Brown RD, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: Secular trends in rochester, minnesota, through 1989. Stroke; a journal of cerebral circulation. 1996;27:373–380. [PubMed] [Google Scholar]
- 19.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study. Stroke; a journal of cerebral circulation. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease C, Prevention. Ten great public health achievements--united states, 1900– 1999. MMWR. Morbidity and mortality weekly report. 1999;48:241–243. [PubMed] [Google Scholar]
- 21.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 22.Sacco RL, Khatri M, Rundek T, Xu Q, Gardener H, Boden-Albala B, et al. Improving global vascular risk prediction with behavioral and anthropometric factors. The multiethnic nomas (northern manhattan cohort study) Journal of the American College of Cardiology. 2009;54:2303–2311. doi: 10.1016/j.jacc.2009.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The atherosclerosis risk in communities (aric) study: Design and objectives. The aric investigators. American journal of epidemiology. 1989;129:687–702. [PubMed] [Google Scholar]
- 24.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The cardiovascular health study: Design and rationale. Annals of epidemiology. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 25.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: Objectives and design. American journal of epidemiology. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 26.Giles WH, Kittner SJ, Hebel JR, Losonczy KG, Sherwin RW. Determinants of black-white differences in the risk of cerebral infarction. The national health and nutrition examination survey epidemiologic follow-up study. Archives of internal medicine. 1995;155:1319–1324. [PubMed] [Google Scholar]
- 27.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half-full (empty?) glass. Stroke a journal of cerebral circulation. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the framingham study. Stroke; a journal of cerebral circulation. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 29.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: The multi-ethnic study of atherosclerosis. Hypertension. 2011;57:1101–1107. doi: 10.1161/HYPERTENSIONAHA.110.168005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: The reasons for geographic and racial differences in stroke study. Stroke; a journal of cerebral circulation. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 31.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. Archives of internal medicine. 2012:1–6. doi: 10.1001/2013.jamainternmed.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleindorfer D, Judd S, Howard VJ, McClure L, Safford MM, Cushman M, et al. Self-reported stroke symptoms without a prior diagnosis of stroke or transient ischemic attack: A powerful new risk factor for stroke. Stroke. 2011;42:3122–3126. doi: 10.1161/STROKEAHA.110.612937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meschia JF, Merrill P, Soliman EZ, Howard VJ, Barrett KM, Zakai NA, et al. Racial disparities in awareness and treatment of atrial fibrillation: The Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Stroke. 2010;41:581–587. doi: 10.1161/STROKEAHA.109.573907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson CD, Biffi A, Rost NS, Cortellini L, Furie KL, Rosand J. Chromosome 9p21 in ischemic stroke: Population structure and meta-analysis. Stroke. 2010;41:1123–1131. doi: 10.1161/STROKEAHA.110.580589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cushman M, McClure LA, Howard VJ, Jenny NS, Lakoski SG, Howard G. Implications of increased c-reactive protein for cardiovascular risk stratification in black and white men and women in the us. Clinical chemistry. 2009;55:1627–1636. doi: 10.1373/clinchem.2008.122093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKnight KK, Wellons MF, Sites CK, Roth DL, Szychowski JM, Halanych JH, et al. Racial and regional differences in age at menopause in the united states: Findings from the Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study. American journal of obstetrics and gynecology. 2011;205:e351–e358. doi: 10.1016/j.ajog.2011.05.014. 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nahab F, Le A, Judd S, Frankel MR, Ard J, Newby PK, et al. Racial and geographic differences in fish consumption: The regards study. Neurology. 2011;76:154–158. doi: 10.1212/WNL.0b013e3182061afb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.You Z, Cushman M, Jenny NS, Howard G. Regards. Tooth loss, systemic inflammation, and prevalent stroke among participants in the Reasons for Geographic And Racial Difference in Stroke (REGARDS) Study. Atherosclerosis. 2009;203:615–619. doi: 10.1016/j.atherosclerosis.2008.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pearson TA, Lewis C. Rural epidemiology: Insights from a rural population laboratory. American journal of epidemiology. 1998;148:949–957. doi: 10.1093/oxfordjournals.aje.a009571. [DOI] [PubMed] [Google Scholar]
- 40.Joubert J, Prentice LF, Moulin T, Liaw ST, Joubert LB, Preux PM, et al. Stroke in rural areas and small communities. Stroke. 2008;39:1920–1928. doi: 10.1161/STROKEAHA.107.501643. [DOI] [PubMed] [Google Scholar]
- 41.Adams PF, Hendershot GE, Marano MA. Centers for Disease C, Prevention/National Center for Health S. Current estimates from the national health interview survey, 1996. Vital and health statistics. Series 10, Data from the National Health Survey. 1999:1–203. [PubMed] [Google Scholar]
- 42.Sergeev AV. Racial and rural-urban disparities in stroke mortality outside the stroke belt. Ethnicity & disease. 2011;21:307–313. [PubMed] [Google Scholar]
- 43.Borhani NO. Changes and geographic distribution of mortality from cerebrovascular disease. American journal of public health and the nation's health. 1965;55:673–681. doi: 10.2105/ajph.55.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Casper ML BE, Williams GI, Jr, Halverson JA, Braham VE, Greenlund KJ. Atlas of stroke mortality: Racial, ethnic, and geographic disparities in the united states. 2003 [Google Scholar]
- 45.Wadley VG, Unverzagt FW, McGuire LC, Moy CS, Go R, Kissela B, et al. Incident cognitive impairment is elevated in the stroke belt: The regards study. Annals of neurology. 2011;70:229–236. doi: 10.1002/ana.22432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howard G. Why do we have a stroke belt in the southeastern united states? A review of unlikely and uninvestigated potential causes. The American journal of the medical sciences. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern united states. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 48.Hall WD, Ferrario CM, Moore MA, Hall JE, Flack JM, Cooper W, et al. Hypertension-related morbidity and mortality in the southeastern united states. The American journal of the medical sciences. 1997;313:195–209. doi: 10.1097/00000441-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Obisesan TO, Vargas CM, Gillum RF. Geographic variation in stroke risk in the united states. Region, urbanization, and hypertension in the third national health and nutrition examination survey. Stroke. 2000;31:19–25. doi: 10.1161/01.str.31.1.19. [DOI] [PubMed] [Google Scholar]
- 50.Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, et al. Estimated 10-year stroke risk by region and race in the united states: Geographic and racial differences in stroke risk. Annals of neurology. 2008;64:507–513. doi: 10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brown TM, Parmar G, Durant RW, Halanych JH, Hovater M, Prineas RJ, et al. Health professional shortage areas, insurance status, and cardiovascular disease prevention in the reasons for geographic and racial differences in stroke (regards) study. Journal of health care for the poor and underserved. 2011;22:1179–1189. doi: 10.1353/hpu.2011.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McClure LA, Murphy HL, Roseman J, Howard G, Malarcher A. Regional and racial differences in smoking and exposure to secondhand smoke: The reasons for geographic and racial differences in stroke (regards) study. Preventing chronic disease. 2011;8:A108. [PMC free article] [PubMed] [Google Scholar]
- 53.Newby PK, Noel SE, Grant R, Judd S, Shikany JM, Ard J. Race and region are associated with nutrient intakes among black and white men in the united states. The Journal of nutrition. 2011;141:296–303. doi: 10.3945/jn.110.130583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Glasser SP, Cushman M, Prineas R, Kleindorfer D, Prince V, You Z, et al. Does differential prophylactic aspirin use contribute to racial and geographic disparities in stroke and coronary heart disease (chd)? Preventive medicine. 2008;47:161–166. doi: 10.1016/j.ypmed.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]