Abstract
The field of epigenetics has expanded rapidly to reveal multiple new targets for drug discovery. The functional elements of the epigenomic machinery can be catagorized as writers, erasers and readers, and together these elements control cellular gene expression and homeostasis. It is increasingly clear that aberrations in the epigenome can underly a variety of diseases, and thus discovery of small molecules that modulate the epigenome in a specific manner is a viable approach to the discovery of new therapeutic agents. In this Digest, the components of epigenetic control of gene expression will be briefly summarized, and efforts to identify small molecules that modulate epigenetic processes will be described.
Keywords: Histone, epigenetic, methyllysine, methylarginine, acetyllysine
1. Introduction
The term epigenetics refers to the study of heritable changes in gene expression and/or phenotype that are mediated by processes that do not involve alterations in the primary sequence of DNA. Epigenetic changes occur either by covalent modification of histone proteins or by methylation of DNA, usually at CpG island sites near specific gene promoters. Specific epigenetic modifications allow the cell to solve the fundamental problem of storing approximately 2 meters of DNA in a cell nucleus with an average diameter of 6 μm, while retaining the ability to control the expression of specific gene products. Prior to 2004, the field of epigenetics was focused on two primary processes, histone acetylation/deacetylation1, 2 and DNA methylation.3 Histone proteins occur as octamers that consist of one H3-H4 tetramer and two H2A-H2B dimers,4 and these structures are directed to DNA because of their predominating positive charges.5 Histone protein tails contain residues that interact with the negative charges on the DNA backbone, and interact with double stranded DNA in such a way that a section of DNA is wrapped around the histone octamer, forming a structure known as a nucleosome. As part of this structure, histone lysine tails protrude through the DNA strand and become sites for post-translational modifications (PTMs) of chromatin, allowing alteration of higher order nucleosome structure.1 The acetylation status of histones is controlled by a balance between two enzymes that functionalize specific histone lysines: histone acetyltransferase (HAT), which promotes histone hyperacetylation, and the histone deacetylases (HDACs), which catalyze acetyl group cleavage.2, 6 Normal mammalian cells efficiently control chromatin architechture in part by maintaining a balance between HAT and HDAC activity. Both the zinc-dependent 7, 8 and sirtuin9, 10 classes of histone deacetylases have been regarded as validated drug targets for a number of years, and two HDAC inhibitors have reached the market, with several other drug candidates in Phase II or III trials. Aberrant methylation of DNA is also an important event in epigenetic silencing.11 In many forms of cancer, cells exhibit a global loss of methylcytosine (hypomethylation) in the gene body, while simultaneously exhibiting hypermethylation at CpG islands in the promoter region.12 Like HDAC inhibitors, DNA methyltransferase inhibitors are well known epigenetic modulators that have been used extensively in cancer chemotherapy.13, 14 Because these topics have been thoroughly reviewed, they will not be considered in this digest. This article will focus on druggable epigenetic targets that have come to light in the last decade, with a particular emphasis on recent developments.
2. Components of the Epigenome
Conceptually, elements of the epigenome machinery can be divided into three categories that are commonly termed writers, erasers and readers.1, 15 In addition to DNA methylation, the epigenetic code is set by the formation and breakdown of specific PTMs at histone lysine (acetylation, methylation, ubiquitination, sumoylation, crotonylation, butyrylation and propionylation) and arginine (methylation, citrullination and ADP-ribosylation) residues, as well as phosphorylation of serine, tyrosine and threonine.16–18 Taken together, modifications at these residues make up an epigenetic “landscape” whereby cellular gene expression can be tightly and accurately controlled. From a drug discovery standpoint, the most important of these PTMs to date are lysine acetylation/deacetylation and lysine or arginine methylation/demethylation. The discussion below will focus on drug development efforts targeting epigenetic writers, erasers and readers; a deeper discussion of the biology underlying their function can be found in recent comprehensive reviews.16, 19 To limit the scope of this review, emphasis was given to novel compounds described in primary journal references. Information concerning epigenetic modulators disclosed in the patent literature has been presented elsewhere.7, 13, 20, 21
3. Epigenetic writers
3.1. Inhibitors of histone acetyltransferases
As stated above, histone lysines can be post-translationally modified by the addition of acetyl groups to lysine, or by the addition of methyl groups to both lysine and arginine. These reactions are carried out by HATs or one of several histone methyltransferases, respectively. In the case of lysine acetylation, formation of an amide with the terminal amino group serves two functions. Acetylation of the ε-amino groups of lysine residues cancels the positive charge, promoting the formation of a relaxed form of DNA (euchromatin).1, 2 This allows greater access to DNA by transcription factors and RNA polymerase, and promotes the expression of various transcriptional products. It follows that removal of the acetyl group from histone lysine residues by HDACs restores the positive charge at ε-amino group, resulting in a densely packed form of chromatin (heterochromatin) that is transcriptionally inactive. As described below, acetylated lysine residues also serve as recognition and binding sites for specific histone readers such as bromodomain-containing proteins.22, 23 The association of these reader proteins with an acetylated lysine on the histone tail also promotes transcription.
Nuclear-localized HATs are more correctly referred to as lysine acetyltransferases, since they are also known to acetylate a variety of non-histone lysine residues.24 These enzymes are classified into 5 families based on structural homology and catalytic mechanism,25, 26 but three of these constitute the major classes that are involved in chromatin remodeling: the Gcn5-related N-acetyltransferases or GNAT family (tGcn5, PCAF and ELP3), the p300/CBP family (p300 and cyclic AMP-responsive element (CREB binding protein) and the MYST family (Tip60 and MYST 1–4).27–29 The effects of these acetyltransferases can be gene-specific or global, depending on their structure and they may participate in a multisubunit protein complex that determines substrate specificity. All of these enzymes require acetyl CoA as a co-substrate, and despite having low sequence homology, they all exhibit a conserved acetyl CoA binding pocket.25 The p300/CBP and GNAT family acetyltransferases appear to play a role in cancer, and elevated HAT activity has been observed in asthma and chronic obstructive pulmonary disease (COPD).30 The levels of the acetyltransferase p300 have been suggested as biomarkers for prognosis in both lung and prostate cancer.31, 32
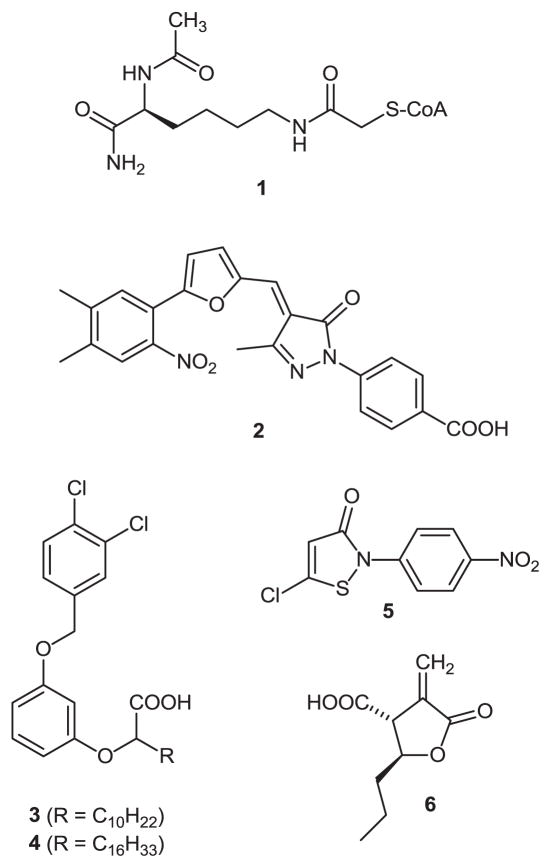
Only a handful of HAT inhibitors have been identified to date (Figure 1), and these compounds were useful in delineating the enzyme mechanism and identifying the role of HAT in cancer. These inhibitors are classified as bisubstrate analogues, natural products or synthetic small molecules.33 Lau et al. described the synthesis and application of compound 1, an adduct between lysine and acetyl CoA, a potent (IC50 = 500 nM) and selective (~200-fold) bisubstrate inhibitor of p300 that displayed an unusual hit-and-run (Theorell-Chance) catalytic mechanism.34 Interestingly, addition of a 20-mer peptide analogous to the sequence of the H3 lysine tail produces a compound that is selective for tGcn5 (IC50 = 300 nM) and PCAF over p300.35 Olhava et al. performed a virtual screen of about 500,000 small molecules against the p300 HAT bisubstrate inhibitor binding site and identified compound 2, which displayed an IC50 of 400 nM in an in vitro assay.36 Treatment with 2 reduces histone H3 and H4 acetylation levels and abrogates TSA-induced acetylation in cultured cells. In addition, a dose-dependent growth inhibitory effects were observed when tested against melanoma, lung and brain cancer cells.36 A number of natural products such as curcumin, garcinol, plumbagin, EGCG, gambogic acid and anacardic acid act as micromolar inhibitors of HATs,30 and these findings led to the design of small molecule synthetic analogues. The most notable derivatives of anacardic acid, compounds 3 and 4, reported by Eliseeva et al. produced HAT inhibition that correlates with its antiproliferative effects, and caused H4 hypoacetylation in MCF7 cells in vitro.37 In addition, isothiazolone derivatives such as 5 reported by Stimson et al. have been shown to inhibit the GNAT family acetyltransferase PCAF,38 while α-methylene-γ-butyrolactone 6 described by Biel et al. have been shown to inhibit GNC5, a GNAT family HAT.39
Figure 1.
Known inhibitors of histone acetyltransferases.
3.2. Inhibitors of histone methylation
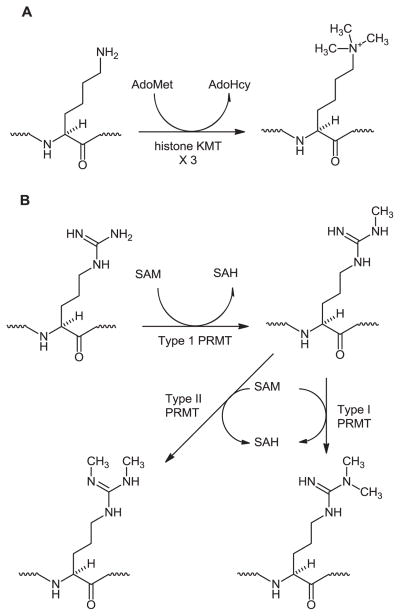
N-terminal histone tails undergo methylation at specific histone lysine and arginine chromatin marks.2, 40 To date, 17 lysine residues and 7 arginine residues on histone proteins have been shown to undergo methylation38 catalyzed by 28 lysine methyltransferases (KMTs) 41, 42 and 9 protein arginine methyltransferases (PRMTs).40, 43 All of these enzymes require S-adenosylmethionine (SAM) as methyl donor, and produce the by-product S-adenosylhomocysteine (SAH), which is recycled through salvage pathways. Histone KMTs generally target a specific lysine residue, and can promote or repress transcription, depending on the lysine residue involved.42, 44, 45 There are 8 classes of histone KMTs: 7 SET1 domain KMTs, 5 SET2 domain KMTs, 6 KMTs in the SUV39 group, EZH1 and 2, 3 KMTs in the PRDM group, 4 KMTs in the other-SET group and 1 non-SET domain KMT.46 Except for the non-SET KMT hDOT1L, all histone KMTs contain a conserved SET (SU(VAR)3–9, enhancer-of-Zeste, Trihorax) domain that is responsible for the methylation activity.47 As shown in Figure 2A, histone KMTs catalyze the stepwise conversion of unmethylated histone lysines to the mono-, di- and trimethylated forms. There are also 2 separate groups of PRMTs, 5 Type I PRMTs and 4 Type II PRMTs. Type I PRMTs methylate arginine to produce N-monomethyl arginine (Figure 2B). From there, a second methyl group can be added to the same carbon to form gem-N,N-dimethylarginine, or a Type II PRMT can methylate the second arginine nitrogen. All histone KMTs and PRMTs require S-adenosylmethionine as a methyl group donor. Importantly, aberrant methylation of histone arginines and lysines is linked to carcinogenesis,48, 49 and possibly to coronary disease.50
Figure 2.
Methylation reactions catalyzed by histone KMTs (Panel A) and histone PRMTs (Panel B). S-adenosylmethionine (SAM), S-adenosylhomocysteine (SAH).
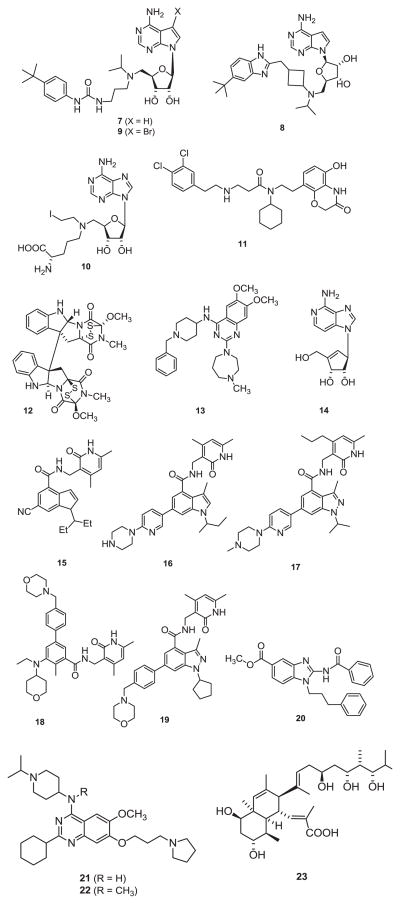
Although efforts to identify histone KMT and PRMT inhibitors are in early stages, a number of promising compounds have been discovered. Most of these histone methyltransferase inhibitors compete with either SAM or the histone substrate. This section describes the key inhibitors of the KMTs DOT1L, SMYD2, Su(var)3–9, G9a, EZH2, SetD8 and SET9 (Figure 3).
Figure 3.
Inhibitors of histone KMTs that act as epigenetic modulators.
A large number of inhibitors of DOT1L has been reported by Epizyme, 36, 51 of which the most noteworthy is compound 7 (EPZ04777) reported by Daigle et al., a potent, SAM-competitive inhibitor (IC50 = 0.4 nM) that selectively inhibits H3K79 methylation and blocks expression of leukemogenic genes in MLL cells in vitro.52 In an attempt to improve the pharmacokinetic properties of 7, the same group synthesized compound 8 (EPZ-5676), a conformationally rigid analog of 7 that displayed improved potency (Ki < 0.08 nM) and selectivity for H3K79 (>37,000-fold).53 A phase I clinical trial has been initiated for 8 where it is being evaluated as a therapy for acute leukemia bearing MLL-rearrangements. In an attempt to elucidate the mechanism, Yu et al. derivatized 7 and found out that the 7-brominated analogue of 7, compound 9 (IC50 = 0.3 nM; 100-fold selective) reduces H3K79 dimethylation and selectively kills MLL cancer cells. 54 A series of inhibitors that resemble SAH were reported from Song’s laboratory, and one of the most potent inhibitors, compound 10 (IC50 = 38 nM) reported by Yao et al. showed weak/no activity against other KMTs or PRMTs.55
Ferguson et al. discovered compound 11 (AZ505; IC50 = 0.12 μM), a potent and selective inhibitor of SMYD2, an oncogenic protein that represses the functional activities of tumor suppressors such as p53 and Rb.56 A co-crystal of SMYD2 with AZ505 showed that it is a substrate competitive inhibitor of the enzyme. The mycotoxin chaetocin 12 reported by Greiner et al. inhibits the KMT Su(var)3–9 from Drosophila (IC50 = 0.8 μM), and produces antitumor effects in vivo.57 More recently, it was demonstrated that chaetocin causes a 25-fold induction of latent HIV-1 expression without activation of T-cells, suggesting that it may be useful in clearing latent HIV from infected cells.58 The compound BIX-01294 13, reported by Kubicek et al. inhibits the G9a KMT and produces a reduction in histone H3 lysine 9 (H3K9) dimethylation (but not mono- or trimethylation) in several cell lines.59 Compound 13 and its homologues also exhibit potent antimalarial activity in both chloroquine-sensitive and -resistant strains, an effect that is mediated through histone KMT inhibition.60
The significance of EZH2 in a multitude of cancers such as prostate, breast and bladder fueled the discovery of specific inhibitors. One of the most widely studied EZH2 inhibitors is 3- deazaneplanocin A, 14, which depletes EZH2 levels while inhibiting the formation of K3K27me3 in AML cells.61 Fiskus et al. reported an enhancement in depletion of EZH2 activity in cultured AML cells when 14 was combined with panobinostat, a pan-HDAC inhibitor.61 It was also reported that 14 as a single agent is growth-inhibitory through induction of a G1 cell cycle arrest in non-small cell lung carcinoma in vitro.62 Qi et al. carried out high-throughput screening against a recombinant PCR2 protein complex containing EZH2 that eventually resulted in the design of compound 15 (El1). Compound 15 elicited potent inhibitory activity against both wild-type (IC50 = 15 nM) and Y641F mutant enzymes (IC50 = 13 nM).63 In addition to being highly selective for EZH2 when compared with EZH1 (90-fold selectivity) or other HMTs (10,000-fold selectivity), 15 inhibits H3K27 methylation, reduces cell proliferation, and initiates cell cycle arrest and apoptosis.
Based on a combination of high-throughput screening and subsequent lead optimization, McCabe et al. identified a series of novel indole-based EZH2 inhibitors.64 The representative compound 16 (GSK-126) inhibited both wild-type and mutant EZH2 with similar potencies (Kiapp = 0.5–3.0 nM) and displayed 1000-fold selectivity over other methyltransferases and 150-fold selective over EZH1.64 In addition, 16 inhibited the proliferation of EZH2 mutants in both diffuse large B-cell lymphoma (DLBCL) cell lines and xenografts. Subsequent design by Verma et al. resulted in 17 (GSK-343; Kiapp = 1.2 nM), in which an indazole moiety is substituted for the indole in 16.65 Both compounds 16 and 17 decreased H3K27me3 levels in a dose-dependent manner. Despite 17 being more potent, it was precluded from advancement to clinical studies due to high clearance as suggested by rat pharmacokinetic studies.65
Researchers at Epizyme recently presented the most interesting data to date regarding EZH2 inhibitors. Knutson et al. carried out a combination of screening and iterative medicinal chemistry that resulted in a novel class of pyridine-based EZH2 inhibitors. The representative compound 18 (EPZ6438) a SAM-competitive inhibitor displayed a Ki value of 2.5 nM and a selectivity index of 35-fold over EZH1 and >4500-fold over other PMTs.66 Compound 18 inhibited H3K27me3 levels leading to specific killing of lymphoma cell lines. Epizyme recently initiated a Phase I/II clinical trial where compound 18 is being evaluated for the treatment of non-Hodgkin lymphoma in patients with EZH2 SET domain mutants.
Two additional novel classes of EZH2 inhibitors worth mentioning are the 2,2,6,6-tetramethypiperidinyl analogues reported by Albrecht et al. and the 2-pyridones reported by Knight et al.67, 68 These drug-like inhibitors displayed low micromolar EZH2 inhibition, but their detailed anticancer effects were not disclosed. An orally available chemical probe, compound 19 (UNC 1999), was recently disclosed by Konze et al. This compound, which combines the structural features of key EZH2 inhibitors such as EPZ005687 and GSK-126, is highly potent against EZH2 (IC50=2.0 nM) and is about 22-fold and 1000-fold selective for EZH2 when compared against EZH1 and other PMTs, respectively.69 Compound 19, in addition to being orally bioavailable in mice, reduced transcriptionally repressive H3K27me3 marks and killed EZH2 mutant DLBCL cells with an EC50 of 633 nM. Finally, decreasing EZH2 activity by altering its endogenous expression levels using small molecules such as 3,3′-indolylmethane, 6-hydroxycleroda-3,13-dien-15,16-olide and all-trans retinoic acid have also been reported.70
Yuan et al. reported the discovery of compound 20 (BRD4770), a probe molecule that inhibits the histone KMT G9a, and induces senescence in pancreatic adenocarcinoma cells in vitro.71 Vedadi et al. performed structure-based optimization and iterative medicinal chemistry of 13 that led to the discovery of compound 21 (UNC0638; R=H), a potent [IC50 15 nM (G9a) and 19 nM (GLP)] inhibitor of histone KMTs G9a and GLP with excellent selectivity over a variety of epigenetic and non-epigenetic targets.72 Interestingly, conversion 21 to 22 (UNC0737, R = CH3) resulted in significantly decreased inhibition, suggesting that H-bonding between Asp 1083 of G9a and the aminoquinazoline moiety in 21 is crucial for inhibition. Finally, nahouic acid 23, a polyketide produced by a marine strain of Streptomyces, is the first known selective SAM-competitive inhibitor of SETD8.73
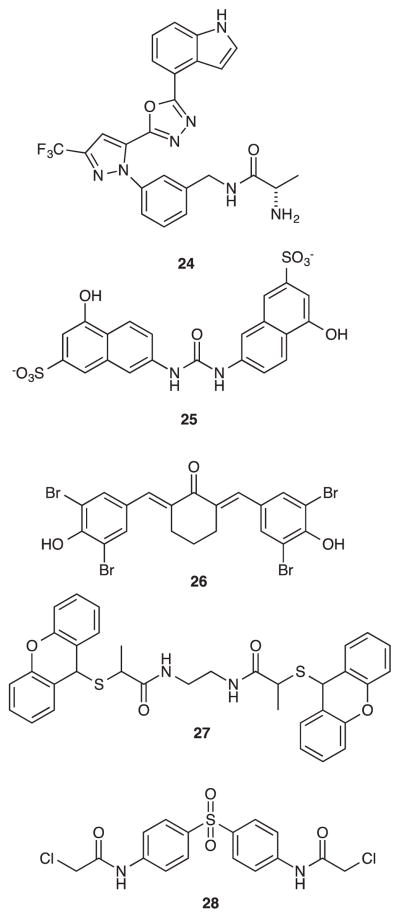
Some progress has also been made in the search for selective histone PRMT inhibitors (Figure 4). Sack et al. carried out a high-throughput screen using full-length co-activator-associated arginine methyltransferase 1 (CARM1), followed by iterative medicinal chemistry optimization, resulting in compound 24 (IC50 30 nM).74 A random screen of a compound library carried out by Cheng afforded nine PRMT inhibitors with structures related to compound 25, also known as AMI-1, (IC50=8.81 μM).75 Further studies have shown that 25 is selective for PRMT over KMT and produced an in vivo effect on methylation.75 Subsequent studies revealed structure-optimized analogues with increased potency against PRMT1 and PRMT4 that modulated T-helper cell cytokine production.76 Analogues of 25 bearing 2- bromo- and 2,6-dibromophenol moieties linked through unsaturated cyclic spacers, such as 26, equally inhibited PRMTs, HKMT, HAT, and SIRTs, thus behaving as multiple ligands for these epigenetic targets.77 A related series of linear and cyclic urea analogues produced modest inhibition of PRMT1 and PRMT5.78 Using a combination of pharmacophore-based virtual screening methods and radioactive methylation assays, Wang et al. identified compounds A9 and A36, which disrupted PRMT1 function by directly targeting the substrate H4, and that were more effective than AMI-1.79 Dillon et al. used a high-throughput screening approach to identify 2 novel inhibitors selective for PRMT1 over other S-adenosylmethionine-requiring protein methyltransferases.80 Spannhoff et al. conducted a focused virtual screening of 9000 compounds and a subsequent optimization of a hit molecule that resulted in compound 27 (RM-65). This compound inhibited PRMTs RmtA (IC50 = 46 μM) and PRMT1 (IC50 = 55 μM) without affecting lysine methyltransferase SET7/9. In silico docking experiments suggested that that 27 acts as a bisubstrate mimic occupying both the arginine and SAM binding pockets.81 Acylated derivatives of p-aminobenzenesulfonamides and the antileprosy drug dapsone also act as inhibitors of PRMT1.82 The (bis)chloroacetyl amide of dapsone, compound 28, selectively inhibited human PRMT1 (IC50 1.5 μM) and was selective for PRMT1 over the arginine methyltransferase CARM1 and the lysine methyltransferase Set7/9.82 It also showed anticancer activity in MCF7a and LNCaP cells in vitro, and blocked androgen-dependent transcription specifically in a reporter gene system.
Figure 4.
Inhibitors of histone PRMTs that act as epigenetic modulators.
Whereas the activity of the PRMT inhibitors is in μM range, very potent and selective KMT inhibitors have been discovered, many of which are active in cells as well as in animal models. However, improved pharmacokinetic attributes (including metabolic stability) and a deeper understanding of mechanistic rationale are required to minimize off-target effects. Additional optimization studies are being conducted to address these concerns.
4. Epigenetic erasers
4.1. Histone deacetylases
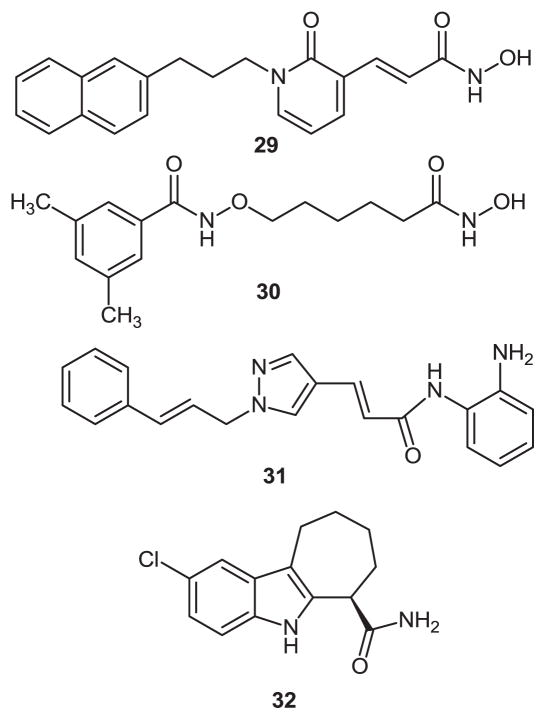
As was mentioned above, a review of histone deacetylase drug discovery research is beyond the scope of this article. However, a brief synopsis of selected research published in the past 6 months is sufficient to demonstrate the direction the field is taking. Cho et al. synthesized a series of pyridone-based hydroxamic acids and evaluated the HDAC inhibition profile of the resulting compounds.83 The most promising of these analogues, compound 29 (Figure 5), exhibited the highest level of HDAC inhibition (IC50 0.07 μM), and was highly selective for the class I HDAC1 and the class II HDAC6 enzymes. Using the conventional HDAC pharmacophore model, Marek et al. designed compound 30 (LMK235; IC50 = 0.65 μM), which had comparable activity to vorinostat (IC50 = 0.53 μM) against global cellular HDACs while being more cytotoxic to the human cancer cell lines A2780, Cal27, Kyse510, and MDA-MB231.84 This effect was increased when 30 was combined with cisplatin. Further HDAC profiling revealed that 30 exhibited a novel HDAC isoform selectivity profile, and produced nanomolar inhibition of HDAC4 (IC50 = 12 nM) and HDAC5 (IC50 = 4 nM). It was also metabolically stable in mouse liver microsomes, and produced growth inhibition of various cancer cell lines.
Figure 5.
Recently discovered HDAC inhibitors.
It is increasingly clear that HDAC inhibitors can be of benefit in a variety of non-cancer disease states. By way of example, the HDAC3-selective inhibitor 31 (RGFP966; IC50 = 80 nM) recently disclosed by Malvaez et al. was found to promote extinction of cocaine-seeking behavior in a persistent manner.85 HDAC inhibitors cause increases in glucocerebrosidase activity in Gaucher’s disease by modulating the levels of molecular chaperones. Other treatment applications for HDAC inhibitors include liver and kidney fibrosis,86 encephalomyelitis,87 stroke and neuroprotection,88 Huntington’s disease89 and a host of other applications. The NAD+-dependent deacetylase SIRT1 regulates transcription via deacetylation of transcription factors such as PPARγ, NFκB, and the tumor suppressor protein p53. In the 2.5 Å crystal structure of the SIRT1 catalytic domain (residues 241–516) bound to NAD+, compound 32 (IC50 = 98 nM) binds deep in the catalytic cleft, where it displaces NAD+ and forces it into an extended conformation that sterically prevents substrate binding,90 thus defining a novel mechanism of histone deacetylase inhibition.
4.2. Lysine demethylases
Methylation of lysines and arginines on histone tails are not static modifications, a fact that was first validated by the discovery that removal of methyl groups from histone 3 lysine 4 (H3K4) mono- and dimethyllysines was catalyzed by lysine specific demethylase 1 (LSD1, aka BHC110 and KDM1A) in a complex where it is associated with the CoREST protein.91 Since histone 3 dimethyllysine 4 (H3K4me2) is a key chromatin mark found associated with promoters of active genes,92, 93 oxidative demethylation of histone 3 methyllysine 4 (H3K4me1) and H3K4me2 by LSD1 is associated with transcriptional repression. Excessive demethylation of this mark by overexpression of LSD1 may prevent expression of tumor suppressor genes important in human cancer.94 Thus, LSD1 is an important new target for the development of specific inhibitors as a new class of antitumor drugs.95 Interestingly, when LSD1 associates with the androgen receptor rather than CoREST, it becomes a specific demethylase for H3K9me and H3K9me2.96 A distinct form of LSD1, which was termed LSD2 or KDM1B,97, 98 has the same substrate specificity, but does not bind to CoREST, because it lacks the requisite tower domain necessary for CoREST binding. LSD2 appears to play a distinct epigenetic role from LSD1.
Subsequent to the discovery of LSD1 in 2004, a number of additional histone lysine demethylases (KDMs) have been identified. The histone demethylases can be classified in one of six families termed KDM1 – KDM6. A discussion of the histone lysine substrate specificity, the effect they have on gene expression and the roles they play in cancer and other diseases is beyond the scope of this Digest, and have recently been reviewed.99 Briefly, the KDM1 family, consisting of LSD1 and 2, are flavin-dependent amine oxidases that show specificity for either H3K4 or H3K9. Because the catalytic mechanism for demethylation by LSD1 and 2 requires a protonated nitrogen moiety, they are only capable of demethylating monomethyl- and dimethyllysines. By contrast, histone demethylases in classes KDM2-KDM6 are all members of the Fe(II)/2-oxoglutarate-dependent oxygenase superfamily.100 The 2-oxoglutarate-dependent histone demethylases are members of the Jumonji family, so named because they contain the JmjC (Jumonji) protein domain within their structure.101 Because the mechanism of Fe(II)/2-oxoglutarate-dependent KDMs does not require a protonated nitrogen on the substrate, they are able to demethylate mono-, di- and trimethylated lysines on the histone tail. KDMs in classes 2–6 belong to six subfamilies termed JMJD1, JMJD2, JARID1, UTX/Y-JMJD3, PHF and FXBL. Depending on the specific KDM involved, Fe(II)/2-oxoglutarate-dependent KDMs can demethylate the mono-, di- and trimethylated forms of lysines H3K4, H3K9, H3K27, H3K36 and H1K26.
Because multiple research groups have been involved in the isolation and characterization of KDMs, the nomenclature for these enzymes is at times confusing; however, a brief summary of the known Fe(II)/2-oxoglutarate-dependent KDMs follows. The KDM2 subfamily is comprised of 2 histone demethylases, KDM2A (JHDM1A; FBXL11)102 and KDM2B (JHDM1B, FBXL10),103 both of which are specific for H3K36me and H3K36me2, recognize unmethylated GpG island DNA and target the polycomb repression system. The KDM3 subfamily contains 3 KDMs, KDM3A (JMJD1A, JH-DM2A, TSGA),104 KDM3B (JMJD1B, JHDM2B, 5qNCA)105 and KDM3C (JMJD1C, JHDM2C, TRIP8).106 The KDM3 subfamilies are specific for H3K9me and H3K9me2, and act as transcriptional activators. The KDM4 subfamily is comprised of KDM4A (JMJD2A, JHDM3A),107 KDM4B (JMJD2B, JHDM3B)108 and KDM4C (JMJD2C, JHDM3C, GASC1).109 KDM4s candemethylate H3K9me2 and H3K9me3, leading to activation of transcription, or H3K36me2 and H3K36me3, leading to transcriptional repression. The KDM5s KDM5A, B, C and D demethylate H3K4me2 and H3K4me3, leading to transcriptional repression, while KDM6A and B demethylate H3K27me2 and H3K27me3, promoting transcriptional activation.
4.3. Inhibitors of LSD1
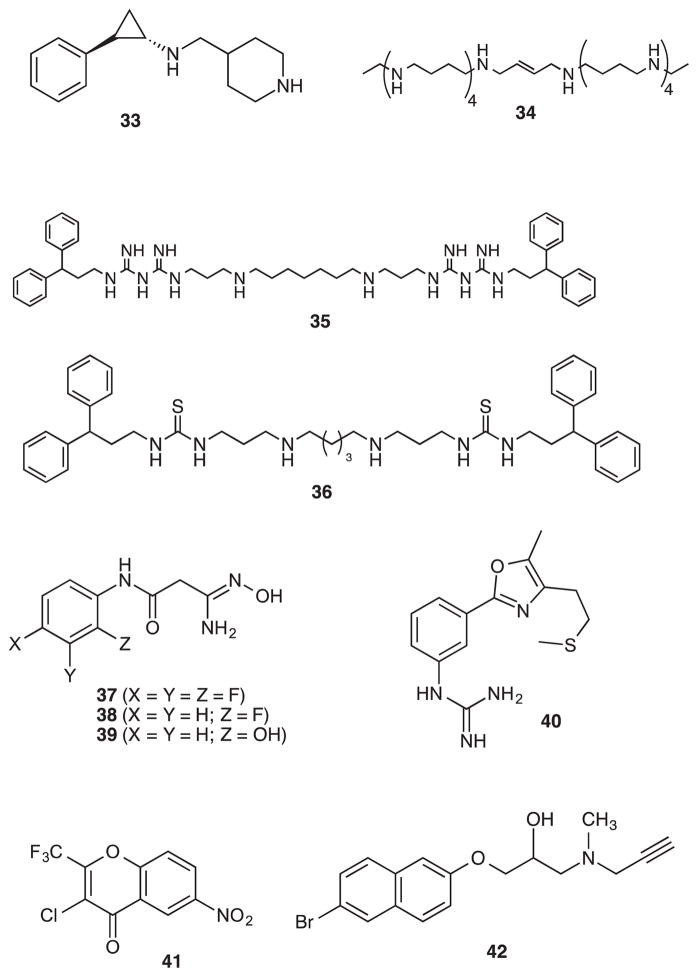
A large body of evidence suggesting that LSD1 is one of the drivers in cancer progression has generated considerable interest in the design and development of novel LSD1 inhibitors for a possible clinical outcome. These inhibitors (Figure 6) could be broadly classified into at least six classes: (i) peptide-based; (ii) monoamine oxidase (MAO) inhibitor-based; (iii) oligoamines-based; (iv) amidoximes; (v) natural polyphenols; (vi) other inhibitors such as phenyl oxazole derivatives and namoline. Dancy et al. reported a number of peptide-based inhibitors that exhibited good LSD1 inhibition.110 While these analogues acted as efficient probes to unravel the mechanism of LSD1, their poor bioavailability precluded their potential for further advancement.110 Because of the homology between LSD1 and MAOs, classical MAO inhibitors such as pargyline and tranylcyproamine were among the first small molecule LSD1 inhibitors that were tested and reported in the literature. Inhibitors in this class has been extensively reviewed elsewhere.111 Recently, Johnson et al. disclosed novel LSD1 inhibitors containing piperidinyl analogues of phenyl cyclopropylamine.112 Representative compound 33 has been shown to be highly potent against LSD1 (mean pIC50 = 8.3) and very selective against MAO-B (pIC50 = 4.1), however, the epigenetic effects of these compounds were not disclosed.
Figure 6.
Small-molecule LSD1 inhibitors.
The similarity between LSD1 and the polyamine oxidases known as acetylpolyamine oxidase (APAO) and spermine oxidase (SMO) led to the evaluation a series of (bis)guanidines and (bis)biguanides that were originally designed as antiparasitic agents.113 The synthesis, recombinant LSD1 inhibition, kinetics, ability to increase the transcriptionally active epigenetic marks such as H3K4me and H3K4me2 and the ability to induce re-expression of tumor suppressors (SFRP1, SFRP4, SFRP5, and GATA5) of these compounds has been described elsewhere.114 Interestingly, when oligoamines 34 and 35 were co-administered with the DNA methyltransferase inhibitor 5-azacytidine (5-AC) in an HCT 116 nude mouse xenograft study, a synergistic re-expression of aberrantly silenced genes was observed. Both 34 and 35 in combination with 5-AC, but not as single agents, dramatically reduced tumor growth over a 38 day period without any significant changes in animal weight.115
A number of functionalized oligoamines have been shown to act as potent epigenetic modulators through inhibition of LSD1, including one of the first small-molecule inhibitors of the enzyme, verlindamycin 35.116 Because of the promising epigenetic activity of oligoamines containing various linker sizes as LSD1 inhibitors,116–118 Pachaiyappan et al. synthesized and tested novel (bis)urea/(bis)thiourea-based oligoamines containing central carbon chains of varying linker length. Structure/activity studies revealed that the 3-5-3 carbon backbone architecture coupled with terminal diphenylalkyl moieties produced the most potent inhibition of LSD1. Three out of nine compounds with the 3-5-3 backbone produced >95% inhibition of the enzyme at 10 μM in a fluorimetric assay. Compound 36 displayed potent LSD1 activity (IC50 = 5.5 μM), and produced significant cytotoxicity in an MTS reduction assay (IC50 = 4 μM). Compound 36 induced significant re-expression of aberrantly silenced tumor suppressors such as SFRP2, HCAD, GATA4 and p16 in Calu6 lung adenocarcinoma cells (unpublished observations). Importantly, 36 was also found to be an effective growth inhibitor of the MCF7 estrogen receptor-positive breast tumor cell line (IC50 = 5.6 μM) and the estrogen receptor negative MDA-MB-231 breast tumor line (IC50 = 9.2 μM) in vitro, but was less effective against the MCF10A breast epithelial cell line (IC50 = 19 μM) (unpublished observations). The effect of compound 36 was also additive with 5-AC. In the MDA-MB-231 cell line, 1.25 μM 36 reduced the IC50 of tamoxifen from 7.5 to 4.5 μM, and this effect was accompanied by a dose-dependent increase in estrogen receptor content.
As part of an effort to identify novel LSD1 inhibitor scaffolds, Hazeldine et al. carried out virtual screening of the Maybridge Hitfinder 5 compound library and identified amidoxime 37 as a potential LSD1 inhibitor.119 In this model, 37 contained a hydrophilic moiety that appeared to be situated near the FAD cofactor, and a hydrophobic substituent that was bound in the hydrophobic pocket. Compound 37 was a weak inhibitor of LSD1 (11.4% at 10 μM), and promoted a 1.6-fold increase in global H3K4me2 levels in the Calu-6 lung tumor cell line. Optimization studies led to the identification of the ortho fluoro derivative 38, which was a modest inhibitor of LSD1, but produced a 12.4-fold increase in global H3K4 methylation at 10 μM, and then to 39 and related analogues. Compounds in this series served as epigenetic modulators that produced increases in H3K4 methylation as high as 3700-fold, including compound 39 (39% inhibition of LSD1 at 10 μM with an accompanying 837- fold increase in global H3K4me2 levels). Under the same conditions, tranylcypromine and pargyline at 10 μM produced an 18.4% and 69.8% inhibition of LSD1.
Recently, Abdulla et al. reported that various natural polyphenols such as resveratrol, curcumin and quercetin were identified as LSD1 inhibitors in a fluorimetric assay.120 Inhibition of LSD1 by resveratrol and curcumin has been shown to inhibit myogenesis in cell culture by inhibition of myogenic gene expression. Interestingly, the inhibitory activity of these compounds was found to be independent of their antioxidant properties suggesting that the natural polyphenols have a novel mechanism and hence may be worthy for further medicinal chemistry pursuits.
By combining the key ligand attributes of oligoamines related to 36, MAO inhibitors and a methionine-based LSD1 peptide inhibitor,121 Dulla et al. reported a small series of phenyl oxazoles containing either amine or guanidine moiety.122 When assayed for LSD1 activity, they found that the representative compound 40 displayed a good inhibition profile (in vitro IC50 of 9.5 μM; cellular IC50 = 1.3 μM in an MDA-MB-231 cell viability assay) and induced apoptosis in zebrafish embryos, suggesting the therapeutic potential of these compounds. The γ-pyrone derivative namoline (41), identified by Willmann et al., was shown to inhibit LSD1 (IC50 = 51 μM) but not MAO-A and B.123 Namoline caused increases in H3K4me2 and H3K4me, and silenced androgen receptor-mediated gene expression, leading to reduced proliferation of LnCAP prostate tumor cells in vitro and in vivo.
Schmitt and coworkers recently desribed a series of nonpeptidic propargylamines typified by compound 42.124 These warhead-containing compounds were only modestly potent IC50 = 22.2 μM for 42), and produced increases in H3K4me2 in MCF7 cells (1.6–1.7-fold) only at concentrations of ≥100 μM. Interestingly, although these compounds contain a propargyl moiety that is present in previously described inactivators of LSD1, no enzyme kinetic data was presented.
4.4 Inhibitors of JmjC domain-containing histone demethylases
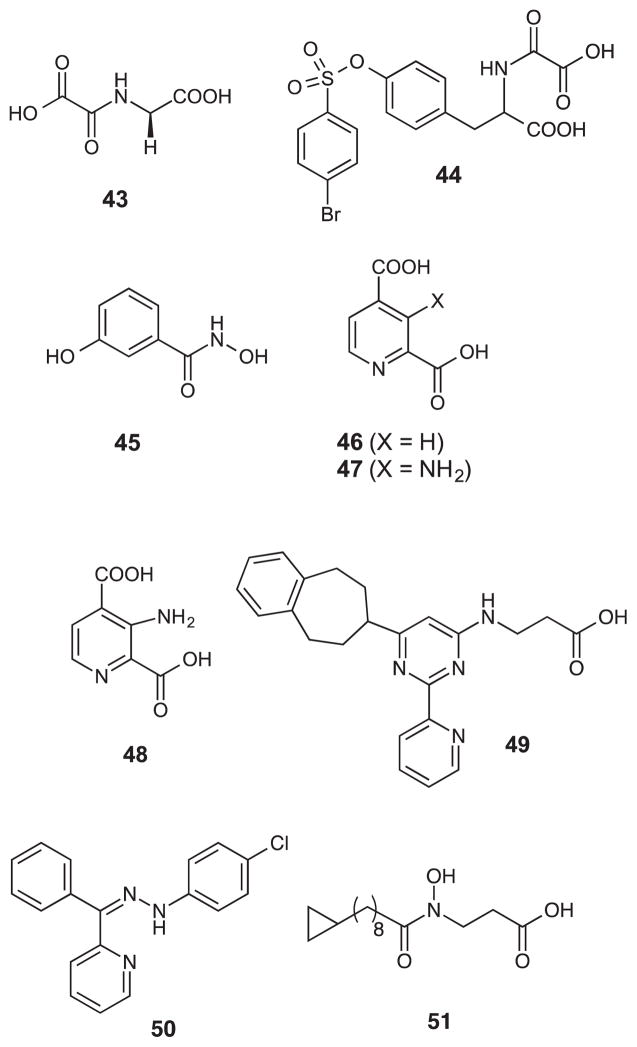
Considering the importance of JmjC domain-containing demethylases in various cancers, intense inhibitor-design efforts were pursued to identify optimal compounds that elicit good activity and selectivity. These inhibitors (Figure 7) are classified into at least four categories: (i) oxalyl derivatives; (ii) hydroxamic acids; (iii) pyridyl analogues; (iv) flavanoids/catechols. Rose et al. identified a series of inhibitor scaffolds that mimic the 2-oxoglutarate cofactor in Fe(II)-2- oxoglutarate-dependent histone demethylases.125 Compound 43 (N-oxalyl glycine; R = H) displayed an IC50 of 78 μM when tested against JMJD2E. Interestingly, the IC50 dropped to 24 μM with 30 min preincubation. Several other derivatives of N-oxalylated D-amino acids were synthesized, the most active being compound 44 (IC50 = 5.4 μM) containing a p-bromobenzene sulfonyl substituent.
Figure 7.
Inhibitors of JmjC domain-containing histone demethylases.
It has been hypothesized that compounds that coordinate with Zn2+ (present in HDACs) may also coordinate with Fe2+ (present in JmjC demethylases). However, when the known HDAC inhibitor SAHA was tested against JMJD2E, a weak inhibition was observed (IC50 = 540 μM) suggesting that was not the case.125 As before, when SAHA was pre-incubated, the IC50 went as low as 14 μM. One of the potent potent hydroxamic acids inhibitors of JMJD2E reported so far is 45 (IC50 = 28 μM; 4.8 μM with pre-incubation). It has been hypothesized that compounds that coordinate with Zn2+ (present in HDACs) may also coordinate with Fe2+ (present in JmjC demethylases). However, when the known HDAC inhibitor SAHA was tested against JMJD2E, a weak inhibition was observed (IC50 = 540 μM) suggesting that was not the case.125 Interestingly, when SAHA was pre-incubated, the IC50 went as low as 14 μM. One of the potent potent hydroxamic acids inhibitors of JMJD2E reported so far is 45 (IC50 = 28 μM; 4.8 μM with pre-incubation). Thalhammer et al. tested the JMJD2E inhibition of pyridyl carboxylates that are known to interact with Fe2+ in collagen/Hypoxia-Inducible Factor (HIF). Compound 46 emerged as a good inhibitor with IC50 value of 1.4 μM. Continuing studies produced additional analogues such as 47 and 48, with IC50 values of 0.11 and 2.5 μM, respectively, against JMJD2E.126
Kruidenier et al. reported one of the most potent JMJD3 (KDM6) inhibitors thus far.127, 128 Based on a structure-based and chemoproteomics approach, they synthesized a series of beta-alanine derivatives containing 2-(pyridinyl)-4-pyrimidine moiety. One of the potent inhibitors in the series, compound 49, is highly active against JMJD3 (IC50 = 60 nM), shows no activity against a panel of other family members, and reduces lipopolysaccharide-induced proinflammatory cytokine (TNF-α) production by human macrophages, a process regulated by JMJD3 and UTX. Compound 50, also known as JIB-04, specifically inhibits the activity of the Jumonji family of histone demethylases in vitro, in cancer cells, and in tumours in vivo. Interestingly, it is not a competitive inhibitor of α-ketoglutarate. Studies show that 50 alters transcriptional pathways, thus blocking cell viability, reducing tumour burden and prolonging survival. Compound 51 was found to be a potent inhibitor of KDM2A (IC50 = 6.8 μM), KDM7A (IC50 = 0.2 μM) and KDM7B (IC50 = 1.2 μM), but only produced modest increases in H3K27me2.129 However, these analogues showed antiproliferative activity against the KYSE150 esophageal squamous cell carcinoma line.
Sakurai et al. designed and implemented a robust and miniaturized high-throughput kinetic assay to identify JMJD2E inhibitors.130 Naturally occurring flavenoids such as myricetin, baicalein and β-lapachone, and catechols such as dopamine, (S)-carbidopa and fenoldopam were identified as hits with IC50 values ranging from 2 to 10 μM.
The demethylases have emerged as attractive targets in cancer drug discovery because of the identification of several active and structurally diverse classes of inhibitors described above. Whereas some of the compounds are active both in vitro and in cell studies, very few are active in animal models, a pre-requisite to enter into clinical trials. Several X-ray crystal structures of both LSD1 and JmjC-domain demethylases are available today and it is expected from medicinal chemists to deliver better clinical candidates in the near future. Nevertheless, these inhibitors act as good starting points.
5. Epigenetic readers
Histone post-translational modifications (PTMs) can only exert their effects on gene expression in the presence of specific reader proteins that are able to recruit or stabilize various components of the transcriptional machinery. As might be expected, there are at least 26 families of reader proteins that function to interpret signals from methylated lysines and arginines, acetylated lysines, phosphorylated serines and threonines and even unmodified histones. A complete discussion of these reader proteins, their specificities for histone PTMs and their effects on transcription is beyond the scope of this digest, and is the subject of an excellent review.16 Specific histone readers have been identified for methyllysines (e.g. ADD, chromodomain, plant homeodomain or PHD, Tudor, WD40), methylarginines (e.g. ADD, Tudor, WD40) and acetyllysine (e.g. bromodomain, double bromodomain or DBD, double PHD finger or DPF), as well as for unmodified histone residues. The methyllysine readers are the best characterized group of reader proteins, but with regard to drug discovery, bromodomain targets have received the most attention.131 There are 8 families of bromodomains, and to date, 61 bromodomains have been identified as components of 46 large, multidomain proteins (bromodomain-containing proteins or BCPs). Within BCP reader proteins, bromodomains fold to form a highly conserved four-helix bundle structure, creating a deep hydrophobic cavity that recognizes and binds acetyllysine. Acetylated lysine makes several contacts with these hydrophobic residues, and the complex is stabilized by a hydrogen bond with a highly conserved asparagine. Lysine acetylation recruits transcriptional coactivators such as p300 and the bromodomain-containing cyclic AMP-responsive element (CREB) binding protein (PCAF).22, 23 The bromodomain found in PCAF is one of 3 known protein domains that act as acetylated lysine-binding elements (the other two are DPF and double pleckstrin homology (PH) domains).131 These coactivators have inherent autocatalytic acetyltransferase activity, and also recruit transcription factors into a complex that promotes active gene transcription.2, 132 Aberrant HDAC overexpression results in reduction of acetylated lysine and the loss of bromodomain-containing proteins, leading to transcriptional repression. HDAC inhibitors have been shown to synergize with p300 autoacetylation to restore acetyl lysine levels and the binding of bromodomain-containing transcription factors, activating transcription.19 This series of events promotes the expression of various transcriptional products. Based on these facts, it is clear that small molecule inhibitors of the interaction of bromodomains with acetyllysines could serve as epigenetic modulators with therapeutic value.
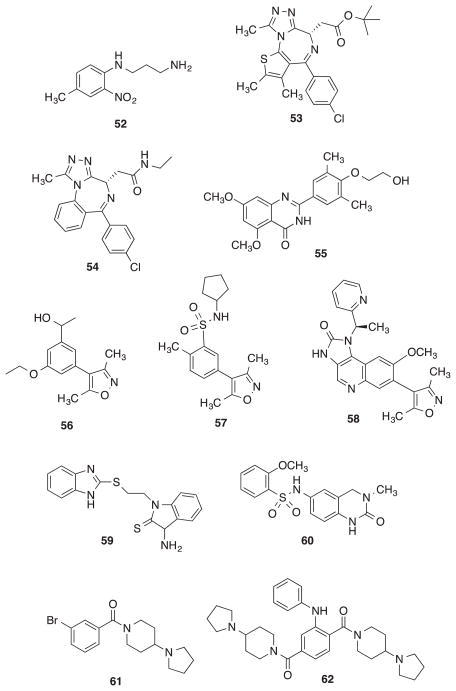
Mujtaba et al utilized an NMR-based screening approach to identify small molecules that could bind to PCAF bromodomain and disrupt its function.133 Although 52 (IC50 = 1.6 μM) fulfilled this role, it was found to bind to PCAF in the peptide binding groove, and not at the acetyllysine site.
Subsequent efforts to design small molecule bromodomain inhibitors have focused largely on the BET family of bromodomains. Using structure-based design techniques, Filippakopoulos et al. reported an optically active (+)JQ1 or compound 53 containing thienodiazepine moiety that binds to BET bromodomain and disrupts the binding of acetyllysine to the BRD4 bromodomain causing cellular differentiation and growth inhibition in a NUT midline carcinoma cell line.134 Nicoteme et al. utilized a screening approach to identify molecules that has the ability to up-regulate ApoA1 reporter gene activity and discovered compound 54 (GSK525768A), a potent inhibitor containing the benzodiazepine moiety that binds to the tandem bromodomains of BET with high affinity (Kd = 50.5 – 61.3 nM).135 Compound 54 offers protection against LPS-induced endotoxic shock and bacteria- induced sepis. Currently, 54 is in clinical trials where its efficacy is evaluated for patients with NUT midline carcinoma and other cancers. The observation that the triazolodiazepine nucleus in 53 and 54 was a common structural feature led to the discovery that clinically approved benzodiazepines, most notably alprazolam, had low micromolar affinity for the BRD4 bromodomain. In addition to 54, there are a couple of other bromodomain inhibitors that made it to the clinical trials. Compound 55 (RVX-208), an orally acting bromodomain inhibitor produced by Resverlogix Corporation removes atherosclerotic plaque via reverse cholesterol transport, and is currently in Phase IIb trials.136 Lastly, OTX-015, a novel orally acting BET bromodomain inhibitor produced by OncoEthix, induces potent anti-proliferative effects that are associated with cell cycle arrest, cellular senescence or apoptosis and is currently in Phase I clinical trials where it is evaluated against acute leukemia and other hematological malignancies.137
Additional bromodomain inhibitors that exhibited various therapeutic properties have been reported. Hewings et al. used X-ray crystallographic studies to design the 3,5-dimethylisoxazole 56,138 which had an IC50 of 4.8 μM against BRD4, and 1.6 μM against BRD2. A similar analogue, 57, was identified through focused fragment screening by Bamborough et al.139 Compound 57 exhibited enhanced water solubility, and IC50 values of 0.5 μM against BRD2, BRD3 and BRD4. This molecule has been shown to possess anti-inflammatory activity in a cellular assay system. Dawson et al. reported IBET-151 or compound 58 that inhibits transcription in MLL-fusion leukemia cells by inhibition of BRD3 (KD = 20 nM) and BRD4 (KD = 100 nM) binding to acetyllysine.140 The benzamidizole analogue 59 reported by Ito et al. was found to inhibit the association of BRD2 with acetylated H3K12 with a dissociation constant of 28 μM.141 Based on a combination of structure-based fragment assessment and optimization, Fish et al. discovered compound 60, a novel, small-molecule chemical probe for BET family.142 Wagner et al. pursued structure-based drug design strategy and reported the discovery of UNC669 or compound 61 (IC50 = 6 μM), a potent L3MBTL1 inhibitor that displayed 5-fold increase in binding affinity compared to the native peptide H4K20me1. The same group also discovered compound 62 (UNC1215), the first potent L3BMTL3 antagonist (Kd = 120 nM) that is selective against other members of the MBT family as well as against other reader domains.143, 144 Collectively, these studies indicate that specific inhibitors of bromodomain binding have promise for use as biological probes of bromodomain function, and for development as novel therapeutic agents.
5. Conclusion
It should be clear from the emerging complexity of the epigenetic landscape that these processes are only beginning to be understood, and that multiple targets are being identified for the discovery of new agents that have therapeutic activity based in modulation of aberrant epigenetic processes. Although much of the epigenetic drug discovery effort to date has been in the cancer arena, it is certain that aberrant epigenetic processes can be identified in a variety of diseases. As such, the potential for development of highly effective agents that modulate the epigenome is apparent. It is highly likely that this potential will be realized in the near future, as disease- and epigenetic process-specific modulators of the epigenome continue to be identified.
Figure 8.
Recently identified small-molecule inhibitors of bromodomain binding to acetyllysine.
Acknowledgments
A portion of the research described in this Digest was supported by NIH/NCI grant RO1 CA149095 (PMW).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and Notes
- 1.Jenuwein T, Allis CD. Science. 2001;293:1074. doi: 10.1126/science.1063127. [DOI] [PubMed] [Google Scholar]
- 2.Johnstone RW. Nat Rev Drug Disc. 2002;1:287. doi: 10.1038/nrd772. [DOI] [PubMed] [Google Scholar]
- 3.He XJ, Chen T, Zhu JK. Cell Res. 2011;21:442. doi: 10.1038/cr.2011.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marks PA, Miller T, Richon VM. Curr Opin Pharmacol. 2003;3:344. doi: 10.1016/s1471-4892(03)00084-5. [DOI] [PubMed] [Google Scholar]
- 5.Luger K, Mader AW, Richmond RK, Sargent DF, Richmond TJ. Nature. 1997;389:251. doi: 10.1038/38444. [DOI] [PubMed] [Google Scholar]
- 6.Marks PA, Richon VM, Miller T, Kelly WK. Adv Cancer Res. 2004;91:137. doi: 10.1016/S0065-230X(04)91004-4. [DOI] [PubMed] [Google Scholar]
- 7.Carafa V, Miceli M, Altucci L, Nebbioso A. Expert Opin Ther Pat. 2013;23:1. doi: 10.1517/13543776.2013.736493. [DOI] [PubMed] [Google Scholar]
- 8.Li J, Li G, Xu W. Curr Med Chem. 2012 [Google Scholar]
- 9.Chen L. Curr Med Chem. 2011;18:1936. doi: 10.2174/092986711795590057. [DOI] [PubMed] [Google Scholar]
- 10.Stunkel W, Campbell RM. J Biomol Screen. 2011;16:1153. doi: 10.1177/1087057111422103. [DOI] [PubMed] [Google Scholar]
- 11.Jones PA, Baylin SB. Cell. 2007;128:683. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsai HC, Baylin SB. Cell Res. 2011;21:502. doi: 10.1038/cr.2011.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fahy J, Jeltsch A, Arimondo PB. Expert Opin Ther Pat. 2012;22:1427. doi: 10.1517/13543776.2012.729579. [DOI] [PubMed] [Google Scholar]
- 14.Gros C, Fahy J, Halby L, Dufau I, Erdmann A, Gregoire JM, Ausseil F, Vispe S, Arimondo PB. Biochimie. 2012;94:2280. doi: 10.1016/j.biochi.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 15.Ruthenburg AJ, Allis CD, Wysocka J. Mol Cell. 2007;25:15. doi: 10.1016/j.molcel.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 16.Musselman CA, Lalonde ME, Cote J, Kutateladze TG. Nat Struct Mol Biol. 2012;19:1218. doi: 10.1038/nsmb.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Portela A, Esteller M. Nat Biotechnol. 2010;28:1057. doi: 10.1038/nbt.1685. [DOI] [PubMed] [Google Scholar]
- 18.Rossetto D, Avvakumov N, Cote J. Epigenetics. 2012;7:1098. doi: 10.4161/epi.21975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arrowsmith CH, Bountra C, Fish PV, Lee K, Schapira M. Nature Reviews. 2012;11:384. doi: 10.1038/nrd3674. [DOI] [PubMed] [Google Scholar]
- 20.Quattrocelli M, Thorrez L, Sampaolesi M. Recent patents on drug delivery & formulation. 2013;7:18. doi: 10.2174/187221113804805883. [DOI] [PubMed] [Google Scholar]
- 21.Robles-Fernandez I, Rodriguez-Serrano F, Alvarez PJ, Ortiz R, Rama AR, Prados J, Melguizo C, Alvarez-Manzaneda E, Aranega A. Recent patents on anti-cancer drug discovery. 2013;8:203. doi: 10.2174/1574891x113089990034. [DOI] [PubMed] [Google Scholar]
- 22.Chen J, Ghazawi FM, Li Q. Epigenetics. 2010;5:509. doi: 10.4161/epi.5.6.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stiehl DP, Fath DM, Liang D, Jiang Y, Sang N. Cancer Res. 2007;67:2256. doi: 10.1158/0008-5472.CAN-06-3985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allis CD, Berger SL, Cote J, Dent S, Jenuwien T, Kouzarides T, Pillus L, Reinberg D, Shi Y, Shiekhattar R, Shilatifard A, Workman J, Zhang Y. Cell. 2007;131:633. doi: 10.1016/j.cell.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 25.Furdas SD, Kannan S, Sippl W, Jung M. Arch Pharm (Weinheim) 2012;345:7. doi: 10.1002/ardp.201100209. [DOI] [PubMed] [Google Scholar]
- 26.Roth SY, Denu JM, Allis CD. Annu Rev Biochem. 2001;70:81. doi: 10.1146/annurev.biochem.70.1.81. [DOI] [PubMed] [Google Scholar]
- 27.Kouzarides T. Cell. 2007;128:693. doi: 10.1016/j.cell.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Hodawadekar SC, Marmorstein R. Oncogene. 2007;26:5528. doi: 10.1038/sj.onc.1210619. [DOI] [PubMed] [Google Scholar]
- 29.Trievel RC, Rojas JR, Sterner DE, Venkataramani RN, Wang L, Zhou J, Allis CD, Berger SL, Marmorstein R. Proc Natl Acad Sci U S A. 1999;96:8931. doi: 10.1073/pnas.96.16.8931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dekker FJ, Haisma HJ. Drug discovery today. 2009;14:942. doi: 10.1016/j.drudis.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 31.Isharwal S, Miller MC, Marlow C, Makarov DV, Partin AW, Veltri RW. Prostate. 2008;68:1097. doi: 10.1002/pros.20772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu Y, Mayo MW, Nagji AS, Hall EH, Shock LS, Xiao A, Stelow EB, Jones DR. Cancer Res. 2012;73:1308. doi: 10.1158/0008-5472.CAN-12-2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manzo F, Tambaro FP, Mai A, Altucci L. Expert Opin Ther Pat. 2009;19:761. doi: 10.1517/13543770902895727. [DOI] [PubMed] [Google Scholar]
- 34.Lau OD, Kundu TK, Soccio RE, Ait-Si-Ali S, Khalil EM, Vassilev A, Wolffe AP, Nakatani Y, Roeder RG, Cole PA. Mol Cell. 2000;5:589. doi: 10.1016/s1097-2765(00)80452-9. [DOI] [PubMed] [Google Scholar]
- 35.Zheng Y, Thompson PR, Cebrat M, Wang L, Devlin MK, Alani RM, Cole PA. Methods Enzymol. 2004;376:188. doi: 10.1016/S0076-6879(03)76012-1. [DOI] [PubMed] [Google Scholar]
- 36.Olhava EJ, Chesworth R, Kuntz KW, Richon VM, Pollock RM, Daigle SR. WO 2011/US6331
- 37.Eliseeva ED, Valkov V, Jung M, Jung MO. Mol Cancer Ther. 2007;6:2391. doi: 10.1158/1535-7163.MCT-07-0159. [DOI] [PubMed] [Google Scholar]
- 38.Stimson L, Rowlands MG, Newbatt YM, Smith NF, Raynaud FI, Rogers P, Bavetsias V, Gorsuch S, Jarman M, Bannister A, Kouzarides T, McDonald E, Workman P, Aherne GW. Mol Cancer Ther. 2005;4:1521. doi: 10.1158/1535-7163.MCT-05-0135. [DOI] [PubMed] [Google Scholar]
- 39.Biel M, Kretsovali A, Karatzali E, Papamatheakis J, Giannis A. Angew Chem Int Ed. 2004;43:3974. doi: 10.1002/anie.200453879. [DOI] [PubMed] [Google Scholar]
- 40.Smith BC, Denu JM. Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms. 2009;1789:45. doi: 10.1016/j.bbagrm.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feng Q, Wang H, Ng HH, Erdjument-Bromage H, Tempst P, Struhl K, Zhang Y. Current Biology. 2002;12:1052. doi: 10.1016/s0960-9822(02)00901-6. [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y, Reinberg D. Genes Dev. 2001;15:2343. doi: 10.1101/gad.927301. [DOI] [PubMed] [Google Scholar]
- 43.Krause CD, Yang ZH, Kim YS, Lee JH, Cook JR, Pestka S. Pharmacology & Therapeutics. 2007;113:50. doi: 10.1016/j.pharmthera.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 44.Kouzarides T. Curr Opin Genet Dev. 2002;12:198. doi: 10.1016/s0959-437x(02)00287-3. [DOI] [PubMed] [Google Scholar]
- 45.Martin C, Zhang Y. Nat Rev Mol Cell Biol. 2005;6:838. doi: 10.1038/nrm1761. [DOI] [PubMed] [Google Scholar]
- 46.Li KK, Luo C, Wang D, Jiang H, Zheng YG. Medicinal Res Rev. 2012;32:815–867. doi: 10.1002/mrr.20228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jenuwein T. Trends Cell Biol. 2001;11:266. doi: 10.1016/s0962-8924(01)02001-3. [DOI] [PubMed] [Google Scholar]
- 48.Schneider R, Bannister AJ, Kouzarides T. Trends Biochem Sci. 2002;27:396. doi: 10.1016/s0968-0004(02)02141-2. [DOI] [PubMed] [Google Scholar]
- 49.Spannhoff A, Hauser AT, Heinke R, Sippl W, Jung M. ChemMedChem. 2009;4:1568. doi: 10.1002/cmdc.200900301. [DOI] [PubMed] [Google Scholar]
- 50.Chen X, Niroomand F, Liu Z, Zankl A, Katus HA, Jahn L, Tiefenbacher CP. Basic Res Cardiol. 2006;101:346. doi: 10.1007/s00395-006-0592-5. [DOI] [PubMed] [Google Scholar]
- 51.Chesworth B, Kuntz KW, Olhava EJ, Patane MA. WO2011-US63309. 2012
- 52.Daigle SR, Olhava EJ, Therkelsen CA, Majer CR, Sneeringer CJ, Song J, Johnston LD, Scott MP, Smith JJ, Xiao Y, Jin L, Kuntz KW, Chesworth R, Moyer MP, Bernt KM, Tseng JC, Kung AL, Armstrong SA, Copeland RA, Richon VM, Pollock RM. Cancer Cell. 2011;20:53. doi: 10.1016/j.ccr.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Daigle SR, Olhava EJ, Therkelsen CA, Basavapathruni A, Jin L, Boriack-Sjodin PA, Allain CJ, Klaus CR, Raimondi A, Scott MP, Waters NJ, Chesworth R, Moyer MP, Copeland RA, Richon VM, Pollock RM. Blood. 2013;122:1017. doi: 10.1182/blood-2013-04-497644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu W, Chory EJ, Wernimont AK, Tempel W, Scopton A, Federation A, Marineau JJ, Qi J, Barsyte-Lovejoy D, Yi J, Marcellus R, Iacob RE, Engen JR, Griffin C, Aman A, Wienholds E, Li F, Pineda J, Estiu G, Shatseva T, Hajian T, Al-Awar R, Dick JE, Vedadi M, Brown PJ, Arrowsmith CH, Bradner JE, Schapira M. Nature Comm. 2012;3:1288. doi: 10.1038/ncomms2304. [DOI] [PubMed] [Google Scholar]
- 55.Yao Y, Chen P, Diao J, Cheng G, Deng L, Anglin JL, Prasad BV, Song Y. Journal of the American Chemical Society. 2011;133:16746. doi: 10.1021/ja206312b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferguson AD, Larsen NA, Howard T, Pollard H, Green I, Grande C, Cheung T, Garcia-Arenas R, Cowen S, Wu J, Godin R, Chen H, Keen N. Structure. 2011;19:1262. doi: 10.1016/j.str.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 57.Greiner D, Bonaldi T, Eskeland R, Roemer E, Imhof A. Nat Chem Biol. 2005;1:143. doi: 10.1038/nchembio721. [DOI] [PubMed] [Google Scholar]
- 58.Bernhard W, Barreto K, Saunders A, Dahabieh MS, Johnson P, Sadowski I. FEBS Lett. 2011;585:3549. doi: 10.1016/j.febslet.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 59.Kubicek S, O’Sullivan RJ, August EM, Hickey ER, Zhang Q, Teodoro ML, Rea S, Mechtler K, Kowalski JA, Homon CA, Kelly TA, Jenuwein T. Mol Cell. 2007;25:473. doi: 10.1016/j.molcel.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 60.Malmquist NA, Moss TA, Mecheri S, Scherf A, Fuchter MJ. Proc Natl Acad Sci U S A. 2012;109:16708. doi: 10.1073/pnas.1205414109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fiskus W, Wang Y, Sreekumar A, Buckley KM, Shi H, Jillella A, Ustun C, Rao R, Fernandez P, Chen J, Balusu R, Koul S, Atadja P, Marquez VE, Bhalla KN. Blood. 2009;114:2733. doi: 10.1182/blood-2009-03-213496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kikuchi J, Takashina T, Kinoshita I, Kikuchi E, Shimizu Y, Sakakibara-Konishi J, Oizumi S, Marquez VE, Nishimura M, Dosaka-Akita H. Lung Cancer. 2012;78:138. doi: 10.1016/j.lungcan.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qi W, Chan H, Teng L, Li L, Chuai S, Zhang R, Zeng J, Li M, Fan H, Lin Y, Gu J, Ardayfio O, Zhang JH, Yan X, Fang J, Mi Y, Zhang M, Zhou T, Feng G, Chen Z, Li G, Yang T, Zhao K, Liu X, Yu Z, Lu CX, Atadja P, Li E. Proc Natl Acad Sci U S A. 2012;109:21360. doi: 10.1073/pnas.1210371110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McCabe MT, Ott HM, Ganji G, Korenchuk S, Thompson C, Van Aller GS, Liu Y, Graves AP, Della Pietra A, 3rd, Diaz E, LaFrance LV, Mellinger M, Duquenne C, Tian X, Kruger RG, McHugh CF, Brandt M, Miller WH, Dhanak D, Verma SK, Tummino PJ, Creasy CL. Nature. 2012;492:108. doi: 10.1038/nature11606. [DOI] [PubMed] [Google Scholar]
- 65.Verma SK, Tian X, LaFrance L, Duquenne C, Suarez DP, Newlander KA, Romeril SP, Burgess JL, Grant SW, Brackley JA, Graves AP, Scherzer DA, Shu A, Thompson C, Ott HM, Van Aller GS, Machutta CA, Diaz E, Jiang Y, Johnson NW, Knight SD, Kruger RG, McCabe MT, Dhanak D, Tummino PJ, Creasy CL, Miller WH. ACS Med Chem Lett. 2012;3:1091. doi: 10.1021/ml3003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Knutson SK, Warholic NM, Wigle TJ, Klaus CR, Allain CJ, Raimondi A, Porter Scott M, Chesworth R, Moyer MP, Copeland RA, Richon VM, Pollock RM, Kuntz KW, Keilhack H. Proc Natl Acad Sci U S A. 2013;110:7922. doi: 10.1073/pnas.1303800110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Albrecht BK, Audia JE, Gagnon A, Harmange JC, Nasveschuk C. WO/2012/068589
- 68.Knight SD, Miller WH, Newlander KA, Verma SK. WO/2012/075080
- 69.Konze KD, Ma A, Li F, Barsyte-Lovejoy D, Parton T, Macnevin CJ, Liu F, Gao C, Huang XP, Kuznetsova E, Rougie M, Jiang A, Pattenden SG, Norris JL, James LI, Roth BL, Brown PJ, Frye SV, Arrowsmith CH, Hahn KM, Wang GG, Vedadi M, Jin J. ACS Chem Biol. 2013 doi: 10.1021/cb400133j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yang YA, Yu J. Protein & Cell. 2013;4:331. doi: 10.1007/s13238-013-2093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuan Y, Wang Q, Paulk J, Kubicek S, Kemp MM, Adams DJ, Shamji AF, Wagner BK, Schreiber SL. ACS Chem Biol. 2012;7:1152. doi: 10.1021/cb300139y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vedadi M, Barsyte-Lovejoy D, Liu F, Rival-Gervier S, Allali-Hassani A, Labrie V, Wigle TJ, Dimaggio PA, Wasney GA, Siarheyeva A, Dong A, Tempel W, Wang SC, Chen X, Chau I, Mangano TJ, Huang XP, Simpson CD, Pattenden SG, Norris JL, Kireev DB, Tripathy A, Edwards A, Roth BL, Janzen WP, Garcia BA, Petronis A, Ellis J, Brown PJ, Frye SV, Arrowsmith CH, Jin J. Nat Chem Biol. 2011;7:566. doi: 10.1038/nchembio.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Williams DE, Dalisay DS, Li F, Amphlett J, Maneerat W, Chavez MA, Wang YA, Matainaho T, Yu W, Brown PJ, Arrowsmith CH, Vedadi M, Andersen RJ. Org Lett. 2013;15:414. doi: 10.1021/ol303416k. [DOI] [PubMed] [Google Scholar]
- 74.Sack JS, Thieffine S, Bandiera T, Fasolini M, Duke GJ, Jayaraman L, Kish KF, Klei HE, Purandare AV, Rosettani P, Troiani S, Xie D, Bertrand JA. Biochem J. 2011;436:331. doi: 10.1042/BJ20102161. [DOI] [PubMed] [Google Scholar]
- 75.Cheng D, Yadav N, King RW, Swanson MS, Weinstein EJ, Bedford MT. J Biol Chem. 2004;279:23892. doi: 10.1074/jbc.M401853200. [DOI] [PubMed] [Google Scholar]
- 76.Bonham K, Hemmers S, Lim YH, Hill DM, Finn MG, Mowen KA. FEBS J. 2010;277:2096. doi: 10.1111/j.1742-4658.2010.07623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mai A, Cheng D, Bedford MT, Valente S, Nebbioso A, Perrone A, Brosch G, Sbardella G, De Bellis F, Miceli M, Altucci L. J Med Chem. 2008;51:2279. doi: 10.1021/jm701595q. [DOI] [PubMed] [Google Scholar]
- 78.Fontan N, Garcia-Dominguez P, Alvarez R, de Lera AR. Bioorg Med Chem. 2013;21:2056. doi: 10.1016/j.bmc.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 79.Wang J, Chen L, Sinha SH, Liang Z, Chai H, Muniyan S, Chou YW, Yang C, Yan L, Feng Y, Li KK, Lin MF, Jiang H, Zheng YG, Luo C. J Med Chem. 2012;55:7978. doi: 10.1021/jm300521m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dillon MB, Bachovchin DA, Brown SJ, Finn MG, Rosen H, Cravatt BF, Mowen KA. ACS Chem Biol. 2012;7:1198. doi: 10.1021/cb300024c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Spannhoff A, Machmur R, Heinke R, Trojer P, Bauer I, Brosch G, Schule R, Hanefeld W, Sippl W, Jung M. Bioorg Med Chem Lett. 2007;17:4150. doi: 10.1016/j.bmcl.2007.05.088. [DOI] [PubMed] [Google Scholar]
- 82.Bissinger EM, Heinke R, Spannhoff A, Eberlin A, Metzger E, Cura V, Hassenboehler P, Cavarelli J, Schule R, Bedford MT, Sippl W, Jung M. Bioorg Med Chem. 2011;19:3717. doi: 10.1016/j.bmc.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 83.Cho M, Choi E, Yang JS, Lee C, Seo JJ, Kim BS, Oh SJ, Kim HM, Lee K, Park SK, Kwon HJ, Han G. ChemMedChem. 2013;8:272. doi: 10.1002/cmdc.201200529. [DOI] [PubMed] [Google Scholar]
- 84.Marek L, Hamacher A, Hansen FK, Kuna K, Gohlke H, Kassack MU, Kurz T. J Med Chem. 2013;56:427. doi: 10.1021/jm301254q. [DOI] [PubMed] [Google Scholar]
- 85.Malvaez M, McQuown SC, Rogge GA, Astarabadi M, Jacques V, Carreiro S, Rusche JR, Wood MA. Proc Natl Acad Sci U S A. 2013;110:2647. doi: 10.1073/pnas.1213364110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Van Beneden K, Mannaerts I, Pauwels M, Van den Branden C, van Grunsven LA. Fibrogenesis & Tissue Repair. 2013;6:1. doi: 10.1186/1755-1536-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ge Z, Da Y, Xue Z, Zhang K, Zhuang H, Peng M, Li Y, Li W, Simard A, Hao J, Yao Z, Zhang R. Exp Neurol. 2012;241C:56. doi: 10.1016/j.expneurol.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 88.Chen YT, Zang XF, Pan J, Zhu XL, Chen F, Chen ZB, Xu Y. Clin Exp Pharmacol Physiol. 2012;39:751. doi: 10.1111/j.1440-1681.2012.05729.x. [DOI] [PubMed] [Google Scholar]
- 89.Jia H, Pallos J, Jacques V, Lau A, Tang B, Cooper A, Syed A, Purcell J, Chen Y, Sharma S, Sangrey GR, Darnell SB, Plasterer H, Sadri-Vakili G, Gottesfeld JM, Thompson LM, Rusche JR, Marsh JL, Thomas EA. Neurobiol Dis. 2012;46:351. doi: 10.1016/j.nbd.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao X, Allison D, Condon B, Zhang F, Gheyi T, Zhang A, Ashok S, Russell M, Macewan I, Qian Y, Jamison JA, Luz JG. J Med Chem. 2013;56:963. doi: 10.1021/jm301431y. [DOI] [PubMed] [Google Scholar]
- 91.Shi Y, Lan F, Matson C, Mulligan P, Whetstine JR, Cole PA, Casero RA, Shi Y. Cell. 2004;119:941. doi: 10.1016/j.cell.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 92.Liang G, Lin JC, Wei V, Yoo C, Cheng JC, Nguyen CT, Weisenberger DJ, Egger G, Takai D, Gonzales FA, Jones PA. Proc Natl Acad Sci U S A. 2004;101:7357. doi: 10.1073/pnas.0401866101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schneider R, Bannister AJ, Myers FA, Thorne AW, Crane-Robinson C, Kouzarides T. Nat Cell Biol. 2004;6:73. doi: 10.1038/ncb1076. [DOI] [PubMed] [Google Scholar]
- 94.Huang Y, Greene E, Murray Stewart T, Goodwin AC, Baylin SB, Woster PM, Casero RA., Jr Proc Natl Acad Sci U S A. 2007;104:8023. doi: 10.1073/pnas.0700720104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Stavropoulos P, Hoelz A. Exp Opin Ther Targets. 2007;11:809. doi: 10.1517/14728222.11.6.809. [DOI] [PubMed] [Google Scholar]
- 96.Metzger E, Wissmann M, Yin N, Muller JM, Schneider R, Peters AH, Gunther T, Buettner R, Schule R. Nature. 2005;437:436. doi: 10.1038/nature04020. [DOI] [PubMed] [Google Scholar]
- 97.Hou H, Yu H. Current Opinion in Structural Biology. 2010;20:739. doi: 10.1016/j.sbi.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Karytinos A, Forneris F, Profumo A, Ciossani G, Battaglioli E, Binda C, Mattevi A. J Biol Chem. 2009;284:17775. doi: 10.1074/jbc.M109.003087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rotili D, Mai A. Genes & cancer. 2011;2:663. doi: 10.1177/1947601911417976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Loenarz C, Schofield CJ. Nat Chem Biol. 2008;4:152. doi: 10.1038/nchembio0308-152. [DOI] [PubMed] [Google Scholar]
- 101.Takeuchi T, Yamazaki Y, Katoh-Fukui Y, Tsuchiya R, Kondo S, Motoyama J, Higashinakagawa T. Genes Dev. 1995;9:1211. doi: 10.1101/gad.9.10.1211. [DOI] [PubMed] [Google Scholar]
- 102.Zhou JC, Blackledge NP, Farcas AM, Klose RJ. Mol Cell Biol. 2012;32:479. doi: 10.1128/MCB.06332-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Farcas AM, Blackledge NP, Sudbery I, Long HK, McGouran JF, Rose NR, Lee S, Sims D, Cerase A, Sheahan TW, Koseki H, Brockdorff N, Ponting CP, Kessler BM, Klose RJ. eLife. 2012;1:e00205. doi: 10.7554/eLife.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yamada D, Kobayashi S, Yamamoto H, Tomimaru Y, Noda T, Uemura M, Wada H, Marubashi S, Eguchi H, Tanemura M, Doki Y, Mori M, Nagano H. Ann Surg Oncol. 2012;19(Suppl 3):S355. doi: 10.1245/s10434-011-1797-x. [DOI] [PubMed] [Google Scholar]
- 105.Kim JY, Kim KB, Eom GH, Choe N, Kee HJ, Son HJ, Oh ST, Kim DW, Pak JH, Baek HJ, Kook H, Hahn Y, Kook H, Chakravarti D, Seo SB. Mol Cell Biol. 2012;32:2917. doi: 10.1128/MCB.00133-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jin G, Sun J, Kim ST, Feng J, Wang Z, Tao S, Chen Z, Purcell L, Smith S, Isaacs WB, Rittmaster RS, Zheng SL, Condreay LD, Xu J. Hum Mol Genet. 2012;21:5222. doi: 10.1093/hmg/dds361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Berry WL, Shin S, Lightfoot SA, Janknecht R. Int J Oncol. 2012;41:1701. doi: 10.3892/ijo.2012.1618. [DOI] [PubMed] [Google Scholar]
- 108.Antony J, Oback F, Chamley LW, Oback B, Laible G. Molec Cell Biol. 2012;33:974. doi: 10.1128/MCB.01014-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Berdel B, Nieminen K, Soini Y, Tengstrom M, Malinen M, Kosma VM, Palvimo JJ, Mannermaa A. BMC Cancer. 2012;12:516. doi: 10.1186/1471-2407-12-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Dancy BC, Ming SA, Papazyan R, Jelinek CA, Majumdar A, Sun Y, Dancy BM, Drury WJ, 3rd, Cotter RJ, Taverna SD, Cole PA. J Am Chem Soc. 2012;134:5138. doi: 10.1021/ja209574z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Suzuki T, Miyata N. J Med Chem. 2011;54:8236. doi: 10.1021/jm201048w. [DOI] [PubMed] [Google Scholar]
- 112.Johnson NW, Kasparec J, Miller WH, Rouse MB, Suarez DP, Tian X. WO/2012/135113A2. 2012
- 113.Bi X, Lopez C, Bacchi CJ, Rattendi D, Woster PM. Bioorg Med Chem Lett. 2006;16:3229. doi: 10.1016/j.bmcl.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 114.Sharma SK, Hazeldine S, Crowley ML, Hanson A, Beattie R, Varghese S, Senanayake TM, Hirata A, Hirata F, Huang Y, Wu Y, Steinbergs N, Murray-Stewart T, Bytheway I, Casero RA, Jr, Woster PM. MedChemComm. 2012;3:14. doi: 10.1039/C1MD00220A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Huang Y, Murray-Stewart T, Wu Y, Baylin SB, Marton LJ, Woster PM, Casero JRA. Cancer Chemo Pharmacol. 2009;15:7217. doi: 10.1158/1078-0432.CCR-09-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Huang Y, Greene E, Stewart TM, Goodwin AC, Baylin SB, Woster PM, Casero RA. Proc Natl Acad Sci USA. 2007;104:8023. doi: 10.1073/pnas.0700720104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Huang Y, Stewart TM, Wu Y, Baylin SB, Marton LJ, Perkins B, Jones RJ, Woster PM, Casero RA., Jr Clin Cancer Res. 2009;15:7217. doi: 10.1158/1078-0432.CCR-09-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sharma S, Wu Y, Steinbergs N, Crowley M, Hanson A, Casero RAJ, Woster P. J Med Chem. 2010;53:5197. doi: 10.1021/jm100217a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hazeldine S, Pachaiyappan B, Steinbergs N, Nowotarski S, Hanson AS, Casero RA, Jr, Woster PM. J Med Chem. 2012;55:7378. doi: 10.1021/jm3002845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Abdulla A, Zhao X, Yang F. J Biochem Pharm Res. 2013;1:56. [PMC free article] [PubMed] [Google Scholar]
- 121.Forneris F, Binda C, Adamo A, Battaglioli E, Mattevi A. J Biol Chem. 2007;282:20070. doi: 10.1074/jbc.C700100200. [DOI] [PubMed] [Google Scholar]
- 122.Dulla B, Kirla KT, Rathore V, Deora GS, Kavela S, Maddika S, Chatti K, Reiser O, Iqbal J, Pal M. Org Biomolec Chem. 2013;11:3103. doi: 10.1039/c3ob40217g. [DOI] [PubMed] [Google Scholar]
- 123.Willmann D, Lim S, Wetzel S, Metzger E, Jandausch A, Wilk W, Jung M, Forne I, Imhof A, Janzer A, Kirfel J, Waldmann H, Schule R, Buettner R. Int J Cancer. 2012;131:2704. doi: 10.1002/ijc.27555. [DOI] [PubMed] [Google Scholar]
- 124.Schmitt ML, Hauser AT, Carlino L, Pippel M, Schulz-Fincke J, Metzger E, Willmann D, Yiu T, Barton M, Schule R, Sippl W, Jung M. J Med Chem. 2013;56:7334. doi: 10.1021/jm400792m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rose NR, Ng SS, Mecinovic J, Lienard BM, Bello SH, Sun Z, McDonough MA, Oppermann U, Schofield CJ. J Med Chem. 2008;51:7053. doi: 10.1021/jm800936s. [DOI] [PubMed] [Google Scholar]
- 126.Thalhammer A, Mecinovic J, Loenarz C, Tumber A, Rose NR, Heightman TD, Schofield CJ. Org Biomolec Chem. 2011;9:127. doi: 10.1039/c0ob00592d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kruidenier L, Chung CW, Cheng Z, Liddle J, Che K, Joberty G, Bantscheff M, Bountra C, Bridges A, Diallo H, Eberhard D, Hutchinson S, Jones E, Katso R, Leveridge M, Mander PK, Mosley J, Ramirez-Molina C, Rowland P, Schofield CJ, Sheppard RJ, Smith JE, Swales C, Tanner R, Thomas P, Tumber A, Drewes G, Oppermann U, Patel DJ, Lee K, Wilson DM. Nature. 2012;488:404. doi: 10.1038/nature11262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.ATKINSON SJ, Barker MD, CAMPBELL M, HUMPHREYS P, Liddle J, Sheppard RJ, Wilson DM. WO/2012/052390
- 129.Suzuki T, Ozasa H, Itoh Y, Zhan P, Sawada H, Mino K, Walport L, Ohkubo R, Kawamura A, Yonezawa M, Tsukada Y, Tumber A, Nakagawa H, Hasegawa M, Sasaki R, Mizukami T, Schofield CJ, Miyata N. J Med Chem. 2013;56:7222. doi: 10.1021/jm400624b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sakurai M, Rose NR, Schultz L, Quinn AM, Jadhav A, Ng SS, Oppermann U, Schofield CJ, Simeonov A. Molec Biosys. 2010;6:357. doi: 10.1039/b912993f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sanchez R, Zhou MM. Curr Opin Drug Discov Devel. 2009;12:659. [PMC free article] [PubMed] [Google Scholar]
- 132.Yang XJ. BioEssays. 2004;26:1076. doi: 10.1002/bies.20104. [DOI] [PubMed] [Google Scholar]
- 133.Mujtaba S, He Y, Zeng L, Farooq A, Carlson JE, Ott M, Verdin E, Zhou MM. Mol Cell. 2002;9:575. doi: 10.1016/s1097-2765(02)00483-5. [DOI] [PubMed] [Google Scholar]
- 134.Filippakopoulos P, Qi J, Picaud S, Shen Y, Smith WB, Fedorov O, Morse EM, Keates T, Hickman TT, Felletar I, Philpott M, Munro S, McKeown MR, Wang Y, Christie AL, West N, Cameron MJ, Schwartz B, Heightman TD, La Thangue N, French CA, Wiest O, Kung AL, Knapp S, Bradner JE. Nature. 2010;468:1067. doi: 10.1038/nature09504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nicodeme E, Jeffrey KL, Schaefer U, Beinke S, Dewell S, Chung CW, Chandwani R, Marazzi I, Wilson P, Coste H, White J, Kirilovsky J, Rice CM, Lora JM, Prinjha RK, Lee K, Tarakhovsky A. Nature. 2010;468:1119. doi: 10.1038/nature09589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nicholls SJ, Gordon A, Johannson J, Ballantyne CM, Barter PJ, Brewer HB, Kastelein JJ, Wong NC, Borgman MR, Nissen SE. Cardiovascular drugs and therapy / sponsored by the International Society of Cardiovascular Pharmacotherapy. 2012;26:181. doi: 10.1007/s10557-012-6373-5. [DOI] [PubMed] [Google Scholar]
- 137.Bonetti P, Boi M, Ponzoni M, Tibiletti M, Stahis A, Inghirami G, Noel K, Zucca E, Bertoni F. 54th ASH Annual Meeting and Exposition; Atlanta, GA. December 8–11, 2012; 2012. [Google Scholar]
- 138.Hewings DS, Wang M, Philpott M, Fedorov O, Uttarkar S, Filippakopoulos P, Picaud S, Vuppusetty C, Marsden B, Knapp S, Conway SJ, Heightman TD. J Med Chem. 2011;54:6761. doi: 10.1021/jm200640v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bamborough P, Diallo H, Goodacre JD, Gordon L, Lewis A, Seal JT, Wilson DM, Woodrow MD, Chung CW. J Med Chem. 2012;55:587. doi: 10.1021/jm201283q. [DOI] [PubMed] [Google Scholar]
- 140.Dawson MA, Prinjha RK, Dittmann A, Giotopoulos G, Bantscheff M, Chan WI, Robson SC, Chung CW, Hopf C, Savitski MM, Huthmacher C, Gudgin E, Lugo D, Beinke S, Chapman TD, Roberts EJ, Soden PE, Auger KR, Mirguet O, Doehner K, Delwel R, Burnett AK, Jeffrey P, Drewes G, Lee K, Huntly BJ, Kouzarides T. Nature. 2011;478:529. doi: 10.1038/nature10509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ito T, Umehara T, Sasaki K, Nakamura Y, Nishino N, Terada T, Shirouzu M, Padmanabhan B, Yokoyama S, Ito A, Yoshida M. Chem Biol. 2011;18:495. doi: 10.1016/j.chembiol.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 142.Fish PV, Filippakopoulos P, Bish G, Brennan PE, Bunnage ME, Cook AS, Federov O, Gerstenberger BS, Jones H, Knapp S, Marsden B, Nocka K, Owen DR, Philpott M, Picaud S, Primiano MJ, Ralph MJ, Sciammetta N, Trzupek JD. J Med Chem. 2012;55:9831. doi: 10.1021/jm3010515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.James LI, Barsyte-Lovejoy D, Zhong N, Krichevsky L, Korboukh VK, Herold JM, MacNevin CJ, Norris JL, Sagum CA, Tempel W, Marcon E, Guo H, Gao C, Huang XP, Duan S, Emili A, Greenblatt JF, Kireev DB, Jin J, Janzen WP, Brown PJ, Bedford MT, Arrowsmith CH, Frye SV. Nat Chem Biol. 2013;9:184. doi: 10.1038/nchembio.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.James LI, Korboukh VK, Krichevsky L, Baughman BM, Herold JM, Norris JL, Jin J, Kireev DB, Janzen WP, Arrowsmith CH, Frye SV. J Med Chem. 2013;56:7358. doi: 10.1021/jm400919p. [DOI] [PMC free article] [PubMed] [Google Scholar]