Abstract
Objective and Methods
ACTIVE Reasoning training data (n = 699) were examined to characterize change through five-year follow-up, associated with training, booster, adherence, and other characteristics.
Results
Training resulted in improved reasoning performance through year five. A significant third annual booster effect was one-half the size of the training effect. Training adherence resulted in greater training effects. Higher education, MMSE, better health and younger age related to higher baseline performance. Higher MMSE was related to larger training effects, larger linear slopes and smaller Booster effects. Significant functional outcomes included a training effect for Complex Reaction Time (CRT), and first annual booster effects for the CRT and Observed Tasks of Daily Living.
Discussion
Initial training gain was comparable to magnitude of age-related cognitive decline over 5 years with no training. Neither age nor gender predicted training or booster effects, indicating the generality of training effects across age (65 – 90 years).
Keywords: ACTIVE trial, aging, cognitive training, reasoning training, training adherence, transfer of training, intervention studies
The primary objective of the ACTIVE (Advanced Cognitive Training for Independent and Vital Elderly) randomized controlled trial was to test the effectiveness and durability of three distinct cognitive interventions in improving the performance of elderly persons on basic measures of cognition and on measures of cognitively demanding tasks of daily living (Jobe et al., 2001; S. L. Willis et al., 2006). Prior ACTIVE analyses have focused on comparison of training effects to performance of a no-contact control group(K. Ball et al., 2002; S. L. Willis et al., 2006). This article focuses on the reasoning training group only, examining the performance trajectory over five years and the effects of booster, training adherence, and covariates in greater detail.
Participants in ACTIVE were randomly assigned to one of four groups: training on verbal episodic memory, reasoning ability, speed of processing, or a no-contact control group. Participants were reassessed immediately after training and at 1st, 2nd, 3rd and 5th annual follow-up (Jobe et al., 2001). Prior to 1st and 3rd annual follow-up, a random subsample of each training group received booster training on the target ability. Significant training effects in comparison to the no-contact control have been found immediately after training and at all follow-up occasions, through the 5th annual (S. L. Willis et al., 2006). Immediately after training, 74 percent of reasoning, 86 percent of speed of processing, and 26 percent of memory participants showed reliable cognitive improvement (K. Ball et al., 2002). Booster training for reasoning and speed of processing training groups produced significantly better performance (net of initial training effect) on their targeted cognitive abilities(S. L. Willis et al., 2006).
The major aim of ACTIVE was to examine whether cognitive training was associated with maintenance of functioning on tasks of daily living. Both self-reported and performance-based measures of daily function were included in ACTIVE (Diehl et al., 2005). At the 5th annual follow-up, the reasoning training group reported significantly less difficulty in the instrumental activities of daily living than the control group(S. L. Willis et al., 2006). The booster training for the speed of processing group showed a significant effect on the performance-based functional measure of everyday speed of processing.
Reasoning, as well as memory and speed of processing were selected for the ACTIVE trial because prior research has shown them to be important basic abilities in cognitive functioning (K Schaie, 2005), and because of previous successful interventions on these abilities in smaller scale training studies (K. Ball, Edwards, & Ross, 2007; Kramer & Willis, 2002; Smith et al., 2009; Verhaeghen, Marcoen, & Goossens, 1992). Inductive reasoning ability has been identified as a component of executive functioning (Lezak, 1995) and has been shown to be closely related to working memory ability (Salthouse, Fristoe, McGuthry, & Hambrick, 1998). Reasoning is considered one of the primary markers of fluid intelligence and has been found in longitudinal research to exhibit relatively early age-related decline, beginning in the mid sixties (K Schaie, 2005). Prior research has shown reasoning ability to account for significant individual variability in both self-reported everyday functioning and in performance-based assessment of instrumental activities of daily living(Allaire & Marsiske, 2002; Diehl, Willis, & Schaie, 1995; M. Marsiske & Willis, 1995).
Earlier, smaller-scale training studies involving no contact controls had found training effects on reasoning ability similar to the findings of the ACTIVE trial. The early ADEPT studies (Blieszner, Willis, & Baltes, 1981) reported immediate training effects when rural elderly were trained on strategies associated with reasoning ability; follow-up of the ADEPT sample showed maintenance of effects seven years after training (S. Willis & Nesselroade, 1990). The training studies within the Seattle Longitudinal Study (SLS; (KW Schaie & Willis, 1986; S. Willis & Schaie, 1994)) indicated that both individuals showing prior longitudinal decline on reasoning and individuals with no prior decline could improve as a function of reasoning training; these training effects were replicated over three waves of training with successive adult birth cohorts (Willis & Schaie, 1994). Approximately one-half of SLS reasoning training participants showed significant pre-posttest improvement; after training, forty percent of those showing prior reasoning decline were performing at or above their level of performance 14 years prior to training. Training effects have also been found at both the level of individual reasoning measures and at the level of a reasoning ability factor, defined by confirmatory factor analyses (S. Willis & Schaie, 1994).
Reasoning training has focused on strategies associated with problem solving involving patterns or rules. Reasoning training participants had higher usage of strategies than a comparison group and higher strategy use was associated with reasoning training gain (Saczynski, Willis, & Schaie, 2002). Collaborative training of couples on reasoning ability has been shown to be effective; older adults using a self-directed training protocol can improve their reasoning ability without the presence of a trainer (Margrett & Willis, 2006; Saczynski, Margrett, & Willis, 2004). The magnitude of training effects has been found to vary with cognitive risk and dementia status (Boron, Willis, & Schaie, 2007). Although these prior training studies had demonstrated the efficacy of reasoning training, the findings of these earlier studies were limited by the lack of intent-to-treat analyses, by small and homogeneous samples, and in some cases incomplete random assignment (Stine-Morrow & Basak, 2011).
Given the ACTIVE findings of five-year durability of training effects and some transfer to everyday functioning, there has been considerable interest in further examination of the characteristics of individuals profiting from reasoning training and of issues of dosing, including adherence with training and added effects of booster training. Prior reports of findings of training effects from the ACTIVE trial (K. Ball et al., 2002; S. L. Willis et al., 2006) have compared each training intervention to the control group, using a repeated-measures, mixed-effects model. In this paper, we employ piecewise growth models from baseline to the 5th annual follow-up to examine the five-year trajectory separately for the reasoning training group. Although only the reasoning composite score was used in the prior articles to represent the proximal outcome of the reasoning training, this paper reports findings for both the composite and three individual reasoning tests (letter series, letter sets, word series; see (McArdle & Prindle, 2008)). Three major questions were addressed: 1) What are the trajectories for the reasoning training group through the 5th annual follow-up on both the cognitive and functional outcomes? 2) Does intervention dosing (i.e., adherence with training regimen and boosters) influence outcomes? and 3) Are covariates significant predictors of training effects?
Method
Participants
The sample used for this study included all individuals randomly assigned to reasoning training (N = 699; M = 162, F = 537) and included an analyses consistent with the intention-to-treat principle. At baseline, this sample ranged in age from 65 to 91 years (M = 73.53, SD = 5.76), with an average education of 13.50 years (SD = 2.69, range = 4 - 20 years), and mean baseline MMSE of 27.26 (range = 23 - 30; SD = 2.02). Demographic characteristics for those in the booster and no booster groups are presented in Table 1.
Table 1.
Demographic characteristics of Reasoning Training participants (N = 699).
| Booster (n = 370) |
No Booster (n= 329) |
||
|---|---|---|---|
| Age | Mean | 73.11 | 74.02 |
| Range | 65-88 | 65-91 | |
| Years of education | Mean | 13.46 | 13.55 |
| Range | 6-20 | 4-20 | |
| MMSE | Mean | 27.38 | 27.12 |
| Range | 23-30 | 23-30 | |
| Female | n | 283 | 254 |
| percentage | 76.5 | 77.2 | |
| Good health | n | 303 | 255 |
| percentage | 81.9 | 77.5 |
The attrition information for the ACTIVE sample is described in Willis et al. (2006). Based on the intent-to-treat design of a randomized clinical trial, 30 subjects (4.3%) randomized to reasoning training but who received no reasoning training are included in the 699 participants analyzed for this study. Of the 699 persons included in this study, 625 (89.4%) completed 8 out of 10 initial training sessions and were considered compliant with training. Approximately 60% of participants (n = 370) who were compliant with initial reasoning training were randomly assigned to reasoning booster training at Year 01. Of individuals participating in 1st annual booster training (n = 305), 98.6% (n = 301) completed 3 out of 4 booster sessions (i.e., were compliant); 66 persons assigned to booster training did not participate in Year 01 booster. Of individuals participating in Year 03 booster (n = 250), 97.2% (n = 243) were compliant; 121 originally assigned to booster training did not receive 3rd annual booster. At Year 05, 469 (67%) reasoning participants were assessed; 64 (9%) had died; 126 (18%) had withdrawn due to health, moving away, caregiving, etc; 40 (5.7%) had been administratively withdrawn due to loss to follow-up. The five-year retention rate for reason trained participants was comparable to the 67% retention rate for the total ACTIVE sample at five years.
Study design and protocol
The ACTIVE trial was a multi-site, single-blind randomized controlled clinical trial. The ACTIVE sample consisted of older adults aged 65 to 94 years living independently who were recruited from senior housing, community centers, hospitals and clinics in Birmingham, AL, Detroit, MI, Boston, MA, Indianapolis, IN, central PA, and Baltimore, MD (K. Ball et al., 2002; Jobe et al., 2001). Participants were excluded from the trial if there was evidence at the time of enrollment of substantial cognitive (MMSE score < 23 or a diagnosis of dementia), visual (self-report of excessive difficulty reading newspaper print or visual test resulting in a score worse than 20/50), or functional decline (difficulty with Activities of Daily Living; ADLs), or a diagnosis of certain medical conditions that would predispose one to possible functional decline or mortality, such as short-lived cancers or stroke. Study procedures were approved by the institutional review boards at the collaborating institutions, and all subjects gave informed consent to participate.
Procedure
Potential participants were first telephone-screened to determine eligibility. Eligible participants consented to three in-person baseline assessments (two individual and one group session) of cognitive, sensory, and functional abilities. Participants were also interviewed regarding their health, medication use, and everyday activities. After completing all eligibility and baseline assessments, participants were randomized to either a no-contact control group (n = 704), speed of processing training group (n = 712), memory training group (n = 712), or reasoning training group (n = 705). However, due to a protocol violation in randomization procedures, 30 participants (6 in reasoning training arm) were dropped from the analyses. This resulted in a total sample of 2802 persons with 699 assigned to reasoning training.
Participants received training according to standardized procedures across 10 sessions over five to six-week period. Regardless of training group assignment, all three interventions shared common design features: 1) equivalent intervention dosing; 2) small group settings with individual and group exercises by certified trainers; 3) ten 60-75 minute sessions; 4) focus on training of strategies relevant to the ability trained; 5) modeling of strategy use by trainer and practice by participants; 6) feedback on performance; 7) fostering self-efficacy regarding performance; 8) applying learned strategies to real-world tasks; and 9) social interaction. In reasoning training, the first five sessions focused on strategy instruction and exercises to practice the strategy, while the last five sessions provided additional practice exercises, but no new strategy training. Training was administered over six replicates or waves.
Immediately following training (< 10 days), participants completed a posttest assessment including 3 sessions similar to the baseline assessment. Follow-up assessments occurred again at approximately 1, 2, 3, and 5 years following training.
Just prior to the first annual assessment, booster training was offered to a 60% random sub-sample of compliant participants, who had completed at least 8 out of 10 initial training sessions. Booster training consisted of four 75-minute refresher classes designed to reinforce strategies learned during the initial training sessions in order to help participants enhance and maintain training gains; no new information was provided during booster sessions. Booster training was again offered to this same sub-sample just prior to the third annual assessment.
Measures
Dependent measures – cognitive outcome analysis
The dependent variables in this analysis were three reasoning measures and a composite score of the three measures. The Letter Series test requires participants to identify the pattern in a series of letters and circle the letter that comes next in the series (30 items; Time: 6 minutes; (Thurstone & Thurstone, 1949)). The Word Series test requires participants to identify the pattern in a series of words, such as the month or day of the week, and circle the word that comes next in the series (30 items; Time: 6 minutes; (Gonda & Schaie, 1985)). The Letter Sets test requires participants to identify which set of letters out of 4 letter sets does not follow the pattern of letters (15 items; 6 minutes; (Ekstrom, French, Harman, & Derman, 1976)). The scores for each test were transformed using the Blom transformation to reduce skewness (Blom, 1958). For the Reasoning Composite, each of the 3 reasoning measures was standardized to its baseline value, and an average of the equally weighted standardized scores was calculated.
Dependent measures – functional outcome analysis
The dependent variables in this analysis were two measures of everyday reasoning/problem-solving abilities --- the Everyday Problems Test (EPT; (M Marsiske & Willis, 1993)) and the Observed Tasks of Daily Living (OTDL; (Diehl et al., 2005)) --- and two measures of everyday speed of processing -- the Complex Reaction Time test (CRT; (K Ball, 2000)) and the Timed Instrumental Activities of Daily Living (TIADL; (Owsley, Sloane, McGwin, & Ball, 2002)). Lower scores on the CRT and TIADL reflected better performance. The scores for each test were transformed using the Blom transformation to reduce skewness (Blom, 1958).
Covariates
The covariates were: baseline Mini-Mental State Exam (MMSE), self rated health, age, education, and gender. The MMSE (Folstein, Folstein, & McHugh, 1975) assesses orientation, attention, language, memory and construction skills and is widely used as a measure of general mental status (Score: 0-30). Individuals with scores below 23 were excluded at baseline screening, resulting in a truncated range from 23 to 30 (M = 27.26, SD = 2.02). Participants completed the self-rated health item (“in general, would you say your health is”) of the SF-36 (Ware & Sherbourne, 1992) with a 5-point scale (1 = Excellent, 2 = Very Good, 3 = Good, 4 = Fair, 5 = Poor). For the analysis, health was coded dichotomously as 0 = excellent/very good/good, 1 = fair/poor, given the sample distribution. Gender was coded as 0 = male, 1 = female. Age, education, and MMSE were mean-centered.
Adherence Indicators
Participants were considered compliant with initial training if they participated in at least 80% of the training sessions (i.e., 8-10 sessions). Adherence with the booster training sessions at the1st annual and 3rd annual follow-up assessments was indicated by participation in at least three of the four sessions; participants not randomly assigned to booster training were given missing values for the booster adherence variables. Given that 90 percent of participants were compliant with initial training and 98 percent were compliant with 1st annual and 3rd annual boosters, adherence indicators were coded as 0 = compliant, 1 = non-compliant.
Reasoning Training Program
Reasoning training focused on improving the ability to solve problems that require linear thinking and that follow a serial pattern or sequence (Jobe et al., 2001; KW Schaie & Willis, 1986). Such problems involve identifying the pattern in a series of letters or words. Participants were taught strategies (e.g., underlining repeated letters, putting slashes between series, indicating skipped items in a series with tick marks) to identify the pattern or sequence involved in solving a problem; they used the pattern to determine the next item in the series. Participants practiced the strategies in both individual and group exercises. Exercises involved both abstract reasoning tasks (e.g., letter series) and reasoning problems related to activities of daily living (e.g., identifying medication dosing pattern).
Data Analysis
To examine the trajectory of performance on the outcome measures throughout the several phases of the ACTIVE training protocol that occurred between the baseline assessment and the 5th annual assessment, piecewise latent growth modeling was utilized (see, for example, (Raudenbush & Bryk, 2002) pp. 178-179). All analyses were conducted using Amos 7 (Arbuckle, 2006). Full information maximum likelihood (FML) was used to estimate the model parameters in order to utilize all available data in the total sample, even in the presence of some missing values on the variables.
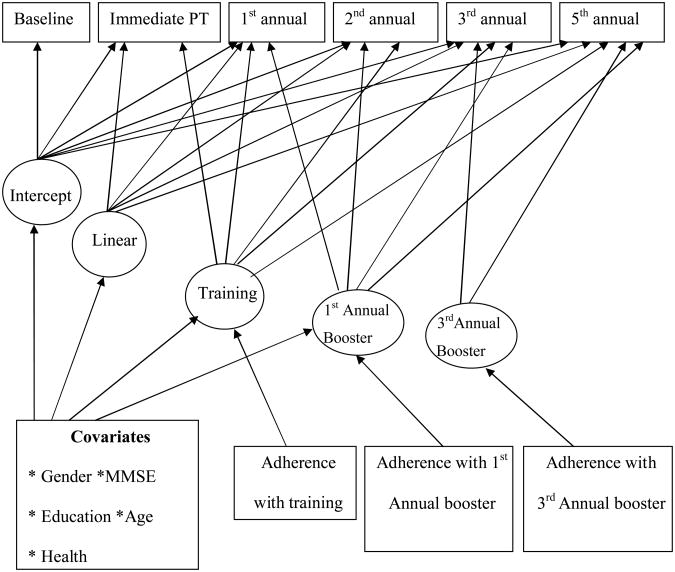
As shown in Figure 1, the growth model included an intercept and linear slope to indicate the average performance at baseline and linear change over time, without the influence of training or booster effects. All factor loadings from the intercept to the six observed timepoints were fixed to 1; for the linear slope factor, these paths were set to 0, .23, 1.23, 2.23, 3.23, and 5.23, representing amount of time in years since baseline. Thus, the mean linear slopes can be interpreted as the average rate of linear change over one year. Three additional latent factors were also included to represent: (1) the influence of training, (2) the influence of the booster training received at the 1st annual assessment, and (3) the influence of booster training received at the 3rd annual assessment. Each of these latent factors assessed the effect of that component of training and was operationalized in the model with loadings fixed to 0 for timepoints prior to the training component and loadings fixed to 1 for timepoints at or after that training component.
Figure 1.
Piecewise growth model with both demographic covariates and adherence indictors as predictors.
Unconditional (no-predictor) models
As our first step in the analyses, unconditional models (i.e., without predictors) were estimated for each outcome measure. As noted in Table 3, several of the models had one or more negative error variance estimates, most likely reflecting difficulty in estimating near-zero interindividual variability for the particular effect. In all cases, these variances were constrained to zero to allow for an admissible solution. Next, homogeneity of the measurement errors across time for each outcome was tested and retained for all of the cognitive outcomes and two of the functional outcomes (EPT and TIADL). As shown in Table 3, the final unconditional models for all outcomes showed very good fit to the data.
Table 3. Fit of the unconditional and conditional piecewise growth models (N = 699).
| Outcome | Chi-square | DF | p-value | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| Unconditional Models | ||||||
|
| ||||||
| Letter Series | 19.51 | 16 | .243 | 1.00 | 1.00 | .02 |
| Letter Sets | 22.36 | 17d | .171 | 1.00 | 1.00 | .02 |
| Word Series | 34.40 | 16 | .005 | 1.00 | 0.99 | .04 |
| Reasoning Composite | 27.70 | 16 | .035 | 1.00 | 1.00 | .03 |
| EPT | 25.98 | 18b,d | .100 | 1.00 | 1.00 | .03 |
| OTDL | 12.89 | 8d | .116 | 1.00 | 0.99 | .03 |
| TIADL | 18.25 | 19b,c,d | .148 | 1.00 | 1.00 | .02 |
| CRT | 28.85 | 13b,d | .007 | 1.00 | 0.99 | .04 |
|
| ||||||
| Conditional Models | ||||||
|
| ||||||
| Letter Series | 55.42 | 36 | .020 | 1.00 | .99 | .03 |
| Letter Sets | 50.43 | 37d | .069 | 1.00 | .99 | .02 |
| Word Series | 65.86 | 36 | .002 | 0.99 | .98 | .03 |
| Reasoning Composite | 58.00 | 36 | .011 | 1.00 | .99 | .03 |
| EPT | 48.76 | 38d | .113 | 1.00 | .99 | .02 |
| OTDL | 30.86 | 27a,d | .227 | 1.00 | .99 | .01 |
| TIADL | 56.32 | 39b,c,d | .036 | 0.99 | .98 | .03 |
| CRT | 53.54 | 33d | .013 | 0.99 | .98 | .03 |
Note. Measurement errors were constrained to equality for all proximal outcomes, for EPT, and for TIADL.
Variance for the linear slope was constrained to zero.
Variance for the training effect was constrained to zero.
Variance for the booster effect at the first annual assessment was constrained to zero.
Variance for the booster effect at the third annual assessment was constrained to zero.
Conditional models: Influence of adherence and demographic covariates
After finding a good fit for the unconditional models, the demographic covariates (i.e., age, education, MMSE, gender, and self-rated health) and three adherence indicators (training adherence, first annual booster adherence, and third annual booster adherence) were added to the models. These conditional models also showed good fit to the data, as shown in Table 3. The estimated means and variances for the piecewise growth model factors are given in Table 4. The three continuous covariates were mean-centered. Three predicted trajectories controlling for adherence and demographic variables are shown in Figure 2; specifically, the trajectory that would have been predicted without training is shown and is contrasted with the trajectories predicted for those who receive and complete only the initial training as well as those who had both the initial training and the booster training. Outcome variables were transformed to T-scores, with a mean of 50 and standard deviation of 10 at baseline.
Table 4.
Means and variances for the piecewise growth model factors with demographic covariates and adherence indicators included in the model.
| Intercept | Linear Slope | Training Effect | 1st Annual Booster Effect | 3rd Annual Booster Effect | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Mean | Variance | Mean | Variance | Mean | Variance | Mean | Variance | Mean | Variance |
| Letter Series | 50.36*** | 43.50*** | -1.09*** | 0.07 | 8.05*** | 6.70*** | 0.07 | 0.91 | 3.36*** | 2.04 |
| Letter Sets | 51.50*** | 41.27*** | -1.41*** | 0.05 | 4.43*** | 8.00*** | 0.19 | 1.29 | 3.07* | 0.00a |
| Word Series | 50.44*** | 44.67*** | -1.83*** | 0.39** | 7.94*** | 6.54*** | 1.41* | 0.36 | 2.96** | 1.95 |
| Reasoning Composite | 50.92*** | 48.26*** | -1.56*** | 0.24** | 7.65*** | 5.24*** | 0.58 | 1.37 | 3.64*** | 1.65 |
| EPT | 51.18*** | 42.58*** | -0.54* | 0.33*** | 0.56 | 0.00a | -0.36 | 1.55 | 0.61 | 0.00a |
| OTDL | 48.89*** | 26.83*** | 0.04 | 0.00a | --- | --- | 2.26* | 10.75*** | -0.32 | 0.00a |
| TIADL | 51.61*** | 34.24*** | 0.87* | 0.09 | -1.35 | 0.00a | -0.80 | 0.00a | -0.63 | 0.00a |
| CRT | 47.72*** | 62.44*** | 0.43 | 0.71*** | -1.76*** | 0.00a | -1.59* | 4.64* | -0.55 | 0.00a |
p < .05
p < .01
p < .001.
This variance was constrained to zero.
Figure 2.
Reasoning Composite: Predicted trajectories of participants with no training, complete initial training only, and both initial training and booster training.
Results
Results are presented for the three major questions addressed. Descriptive statistics for the cognitive and functional outcome measures across the six time points assessed are shown in Table 2 for the booster and no booster groups.
Table 2.
Descriptive statistics for the cognitive and functional outcomes across time by assignment to booster.
| Outcome | Group | Baseline | PT | 1st Annual | 2nd Annual | 3rd Annual | 5th Annual | |
|---|---|---|---|---|---|---|---|---|
| Letter Series | Booster | M | 50.25 | 58.65 | 58.38 | 57.11 | 60.38 | 57.94 |
| SD | 10.40 | 10.26 | 10.29 | 10.09 | 10.42 | 9.94 | ||
| n | 370 | 355 | 299 | 288 | 274 | 246 | ||
| No Booster | M | 49.78 | 57.96 | 56.04 | 55.67 | 57.03 | 56.72 | |
| SD | 9.64 | 10.22 | 9.52 | 10.31 | 9.99 | 9.69 | ||
| n | 328 | 268 | 208 | 199 | 193 | 156 | ||
| Letter Sets | Booster | M | 50.26 | 54.57 | 55.08 | 52.93 | 54.97 | 52.99 |
| SD | 10.15 | 10.36 | 10.13 | 10.63 | 9.80 | 10.27 | ||
| n | 368 | 355 | 298 | 285 | 273 | 245 | ||
| No Booster | M | 49.76 | 53.52 | 51.92 | 52.20 | 53.04 | 52.19 | |
| SD | 9.84 | 10.54 | 10.30 | 9.36 | 9.76 | 9.92 | ||
| n | 327 | 263 | 207 | 200 | 191 | 156 | ||
| Word Series | Booster | M | 50.36 | 58.18 | 58.12 | 57.36 | 59.64 | 56.89 |
| SD | 9.84 | 9.99 | 10.27 | 10.35 | 10.71 | 10.64 | ||
| n | 370 | 353 | 304 | 283 | 276 | 246 | ||
| No Booster | M | 49.60 | 56.95 | 55.98 | 55.92 | 56.84 | 54.80 | |
| SD | 10.25 | 10.66 | 10.00 | 11.15 | 11.11 | 11.24 | ||
| n | 328 | 270 | 212 | 206 | 194 | 160 | ||
| Reasoning Composite | Booster | M | 50.32 | 57.93 | 57.94 | 56.39 | 59.14 | 56.64 |
| SD | 10.15 | 10.46 | 10.36 | 10.52 | 10.48 | 10.54 | ||
| n | 370 | 357 | 305 | 290 | 280 | 246 | ||
| No Booster | M | 49.67 | 56.77 | 55.12 | 55.02 | 56.21 | 55.03 | |
| SD | 9.85 | 10.62 | 10.02 | 10.43 | 10.35 | 10.26 | ||
| n | 329 | 272 | 213 | 207 | 196 | 160 | ||
| TIADL | Booster | M | 49.65 | 48.34 | 48.73 | 48.90 | 49.46 | 50.01 |
| SD | 9.76 | 9.95 | 10.14 | 10.61 | 9.45 | 9.98 | ||
| n | 370 | 353 | 298 | 286 | 276 | 247 | ||
| No Booster | M | 50.42 | 50.16 | 48.91 | 48.32 | 49.31 | 49.35 | |
| SD | 10.16 | 10.12 | 10.22 | 9.53 | 9.99 | 9.46 | ||
| n | 329 | 270 | 210 | 201 | 193 | 157 |
1) What are the trajectories for the reasoning training group through the 5th annual follow-up on both the cognitive and functional outcomes?
Cognitive (reasoning) outcomes
Significant linear decline was observed in all reasoning measures without training. However, reasoning training resulted in a significant, positive training effect for all reasoning measures; training effects were found at immediate posttest and were maintained through fifth annual follow-up (Table 2; Figure 2). Given that our dependent variables were scaled in T-score metric (M = 50, SD = 10), the average training gains were equivalent to approximately 0.8 SD for Letter Series, Word Series, and the Reasoning Composite and approximately 0.4 SD for Letter Sets.
Functional outcomes
A significant training effect was observed for only one functional outcome, the CRT (Table 2;Table 4). Participants showed a significant decrease in reaction time on this measure. Given that our dependent variables were scaled in T-score metric (M = 50, SD = 10), the average training gain for CRT was equivalent to approximately 0.2 SD.
2) Does intervention dosing (i.e., adherence with training regimen and boosters) influence outcomes?
Adherence
With regard to cognitive (reasoning) outcomes, both training adherence and booster adherence had a positive effect. Training adherence (80%+ sessions) resulted in greater training effects for Letter Series (p < .001), Word Series (p < .001), and the reasoning composite (p < .001). Also, booster adherence (75%+sessions) resulted in a greater booster effect at the first annual booster for all cognitive outcomes.
With regard to functional outcomes, only booster adherence had an effect. In contrast to the positive effects of adherence for the cognitive measures, training adherence did not have a positive effect for any of the functional outcomes. However, booster adherence resulted in greater booster effects at first annual booster for the OTDL (p = .013), TIADL (p = .020), and CRT (p = .003), but in poorer booster effects at the third annual assessment for EPT (p = .013).
Booster
Only Word Series showed a significant effect from the first annual booster. However, at the third annual booster, all cognitive (reasoning) outcomes showed a significant positive effect (Tables 2 and 4; Figure 2). Regarding functional outcomes, at the first annual booster, both CRT and OTDL showed significant booster effects.
3) Are covariates significant predictors of training effects?
Predictors of baseline performance level and predictors of slope (training effect) were examined.
Predictors of cognitive outcomes
Predictors of higher baseline performance for all reasoning measures were: younger age, higher education, higher MMSE (at baseline), and better health . A higher MMSE at baseline was the only predictor of the training effect (slope; p = .006). In contrast, a higher baseline MMSE score was associated with smaller booster effects (slope; p = .001) at the first and third annual assessments. Finally, better health was related to a greater training effect (slope) for Letter Series (p = .047).
Predictors of functional outcomes
Predictors of higher baseline performance on all functional outcomes were: younger age, higher MMSE (at baseline), and better health (p < .001). Also, higher education was associated with higher baseline performance for EPT, OTDL, and TIADL (p < .001), and being female was associated with better TIADL performance (p < .001) but lower CRT performance (p = .005). Younger age was also related to a slower linear decline (without influence of training or booster effects) in TIADL (p = .013) and a larger training effect (slope) for EPT (p = .004) and CRT (p = .038). Poorer health showed an association with greater linear decline for OTDL (p = .021).
Discussion
This study addressed three major questions with regard to the reasoning training group within the ACTIVE trial. What was the impact of training on the trajectory of the reasoning trained group from baseline to five-year follow-up? Did adherence with training and booster sessions influence training outcomes? What covariates were significant predictors of training effects? We will first discuss these findings with regard to cognitive outcomes and then consider the more limited findings regarding functional outcomes.
The magnitude of age-related decline for reasoning ability over the five-year interval (without training) was found to be approximately 0.78 SD units for the Reasoning Composite (Table 4). The magnitude of the initial training effect was on the order of approximately 0.80 SD units for the Reasoning Composite. Thus, the magnitude of benefit derived from the initial training (10 sessions) was on the order of the magnitude of age-related decline over the five-year follow-up interval. The comparability of magnitude of training gain from initial training and magnitude of age-related decline over five years may contribute to our understanding of the maintenance of training effects. The descriptive statistics for reasoning performance (Table 2) indicate that, on average, participants were performing at least 0.50 SD units above baseline even 5 years after training, for the Reasoning Composite.
We can offer two hypotheses about why there might have been a lesser effect for the Letter Sets measure. First, less time in initial training and in booster sessions was focused on Letter Sets; this allocation of training time was based in part on prior factor analysis of markers of Inductive Reasoning and the finding that Letter Sets is a less salient marker of Inductive Reasoning ability. Second, although the strategies focused on during training do apply to Letter Sets problems, the application of the strategies to Letter Set problems is more complex and thus strategy training may have been less useful in solving Letter Set items.
The second major question of the study focused on dosing issues. Although the efficacy of cognitive training has been demonstrated in prior research, these smaller scale studies have given less attention to issues of dosing. How much training is needed for a certain level of effect? Do temporally spaced booster sessions significantly increase the training effect? These dosing issues are relevant to cost-benefit analyses of training and for the pragmatics of delivery of cognitive interventions. Amount of training required for a given effect also has implications for the diversity of elderly participants (e.g., frailty) who may be offered training. The ACTIVE trial is unique in its design and focus on addressing these issues. The study findings suggest that both adherence with training and added booster sessions can significantly enhance the training experience and increase the training effect. Training adherence for the initial training and for the booster sessions resulted in larger training effects for the Reasoning Composite and for the individual measures of Letter Series and Word Series. However, it should be noted that the majority of subjects were adherent to both initial and booster training; this high rate of compliance may be partly due to opportunities for make-up sessions and the rigorous monitoring of compliance by study personnel. That most subjects did adhere to study protocol may have limited the power to detect the effects of variability in adherence.
The findings regarding booster sessions indicate that a delayed booster, at three years after training, had significant added training benefit. The magnitude of the booster effect at 3rd Annual was approximately 0.30 SD units. The impact of the 3rd Annual booster was approximately one-half (48%) as great as the magnitude of initial training for the Reasoning Composite. The effect of the 3rd Annual booster was three times as large as the amount of age-related decline that would occur in one year with no training. Descriptive statistics, shown in Table 2 (also Figure 2), indicate that the highest performance for the boosted group across the five-year trajectory was immediately after the 3rd Annual booster training. In contrast, there was less improvement associated with the booster immediately before the first annual follow-up, with the exception of Word Series. It may be that, on average, many of the training participants were functioning at a high level after initial training and less able to benefit from the booster that so closely followed the initial training.
Level of reasoning scores at baseline (intercept) is associated with better functioning on a number of the covariates (younger age, higher education, higher MMSE, and better health). However, of note is that neither age nor gender were significant predictors of initial training effects (slope) or booster effects for any reasoning measures, indicating the generality of training gain across gender and the wide age range of participants from 65 to 90 years of age. In contrast, those with lower levels of education exhibited greater training effects for the Letter Series and Word Series. Likewise, participants with lower baseline MMSE showed greater booster effects for the Reasoning Composite; this is particularly noteworthy for booster effects occurring three years after training. Thus, additional booster interventions appear particularly useful for the cognitively less advantaged. The general self- report measure of health had little relationship with training or booster effects.
More limited effects of training were found for functional outcomes. Only one functional outcome (CRT) showed a training effect associated with initial training and the magnitude of training gain was only one-fourth (0.2 SD) the size of the cognitive training effect. CRT is a speed-based measure, while training focused on strategies for solving reasoning problems. The focus on strategies specific to reasoning may have contributed to reduced transfer to functional outcomes in two ways. First, a focus solely on reasoning per se may have reduced transfer; performance on reasoning accounted for a much smaller proportion of variability in performance on functional measures than on reasoning measures. Second, the focus on strategies may have emphasized to subjects the importance of accuracy over an emphasis on speed.
One of the more interesting findings is that both additional training (booster) and adherence to booster were associated with improvement on multiple functional measures (CRT, TIADL, OTDL) at third annual booster. Both the TIADL and OTDL focus on performance of instrumental tasks of daily living. The functional improvement associated with booster training and adherence may suggest that additional and more intensive training is needed to demonstrate a far transfer effect to tasks of daily living; the finding of the effect at third annual may suggest the importance of temporal spacing of interventions in order to allow for integration of cognitive effects. A younger age was the only predictor of training for functional outcomes.
In summary, the ACTIVE study is the first large-scale randomized trial to show that cognitive training improves cognitive functioning in well-functioning older adults, and that this improvement lasts up to 5 years follow up. Prior smaller intervention studies had documented significant immediate effects of training; the ACTIVE trial using intent-to-treat analyses replicated these findings. However, prior training research had not carefully examined issues of adherence with training and the effect of temporally-spaced booster sessions. Prior studies had seldom reported the proportion of participants compliant with the intervention or whether adherence enhanced the intervention effect. The significant effect of adherence indicates that the dosing of the intervention is an important factor in its effectiveness. The high proportion of participants who were compliant with training indicates that participants are willing and able to tolerate the intensity of intervention provided in ACTIVE. The finding that the three-year booster sessions resulted in an effect approximately half the size of the initial training is informative, given that the number of booster sessions was 60% of the intensity of the initial training and the participants were three years older, on average in their mid-to-late seventies. The efficacy of the delayed booster suggests that maintenance of training effects may indeed extend beyond the five-year follow-up, underscoring the importance of following this sample into old-old age.
Acknowledgments
Active is supported by grants from the National Institute on Aging and the National Institute of Nursing Research to Hebrew Senior Life (U01NR04507), Indiana University School of Medicine (U01NR04508), Johns Hopkins University (U01AG14260), New England Research Institutes (U01AG14282), Pennsylvania State University (U01AG14263), University of Alabama at Birmingham (U01AG14289), University of Florida (U01AG14276). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research, National Institute on Aging, or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data.
References
- Allaire JC, Marsiske M. Well- and ill-defined measures of everyday cognition: relationship to older adults' intellectual ability and functional status. Psychol Aging. 2002;17(1):101–115. doi: 10.1037/0882-7974.17.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle J. Amos 7.0 User's Guide. Chicago, IL: SPSS, Inc; 2006. [Google Scholar]
- Ball K. Increased mobility and reducing accidents of older drivers. In: Schaie K, Pietrucha M, editors. Mobility and Transportation in the Elderly. Vol. 5. New York, NY: Springer; 2000. [Google Scholar]
- Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. Jama. 2002;288(18):2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K, Edwards JD, Ross LA. The impact of speed of processing training on cognitive and everyday functions. J Gerontol B Psychol Sci Soc Sci. 2007;62 Spec No 1:19–31. doi: 10.1093/geronb/62.special_issue_1.19. [DOI] [PubMed] [Google Scholar]
- Blieszner R, Willis S, Baltes P. Training research in aging on the fluid ability of inductive reasoning. J Appl Dev Psychol. 1981;2:247–265. [Google Scholar]
- Blom G. Statistical Estimates and Transformed Beta-Variables. New York: Wiley; 1958. [Google Scholar]
- Boron JB, Willis SL, Schaie KW. Cognitive training gain as a predictor of mental status. J Gerontol B Psychol Sci Soc Sci. 2007;62(1):P45–52. doi: 10.1093/geronb/62.1.p45. [DOI] [PubMed] [Google Scholar]
- Diehl M, Marsiske M, Horgas AL, Rosenberg A, Saczynski JS, Willis SL. The Revised Observed Tasks of Daily Living: A Performance-Based Assessment of Everyday Problem Solving in Older Adults. J Appl Gerontol. 2005;24(3):211–230. doi: 10.1177/0733464804273772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Willis SL, Schaie KW. Everyday problem solving in older adults: observational assessment and cognitive correlates. Psychol Aging. 1995;10(3):478–491. doi: 10.1037//0882-7974.10.3.478. [DOI] [PubMed] [Google Scholar]
- Ekstrom R, French J, Harman H, Derman D. Kit of Factor-Referenced Cognitive Tests (Rev ed) Princeton, NJ: Educational Testing Service; 1976. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gonda J, Schaie K. Schaie-Thurstone Mental Abilities Test: Word Series Test. Palo Alto, CA: Consulting Psychologists Press; 1985. [Google Scholar]
- Jobe JB, Smith DM, Ball K, Tennstedt SL, Marsiske M, Willis SL, et al. ACTIVE: a cognitive intervention trial to promote independence in older adults. Control Clin Trials. 2001;22(4):453–479. doi: 10.1016/s0197-2456(01)00139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer AF, Willis SL. Enhancing the cognitive vitality of older adults. Curr Dir Psychol Sci. 2002;11(5):P173–177. [Google Scholar]
- Lezak M. Neuropsychological assessment. Oxford; Oxford University Press; 1995. [Google Scholar]
- Margrett J, Willis S. In-home cognitive training with older married couples: Individual versus collaborative learning. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2006;13(2):173–195. doi: 10.1080/138255890969285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsiske M, Willis S. Manual for the Everyday Problems Test. University Park: The Pennsylvania State University; 1993. [Google Scholar]
- Marsiske M, Willis SL. Dimensionality of everyday problem solving in older adults. Psychol Aging. 1995;10(2):269–283. doi: 10.1037//0882-7974.10.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle JJ, Prindle JJ. A latent change score analysis of a randomized clinical trial in reasoning training. Psychol Aging. 2008;23(4):702–719. doi: 10.1037/a0014349. [DOI] [PubMed] [Google Scholar]
- Owsley C, Sloane M, McGwin G, Jr, Ball K. Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology. 2002;48(4):254–265. doi: 10.1159/000058360. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical linear models: Applications and data analysis methods. 2nd. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- Saczynski J, Margrett J, Willis S. Older adults' strategic behavior: Effects of individual versus collaborative cognitive training. Educ Gerontol. 2004;30:587–610. [Google Scholar]
- Saczynski J, Willis S, Schaie K. Strategy use in reasoning training with older adults. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2002;9:48–60. [Google Scholar]
- Salthouse TA, Fristoe N, McGuthry KE, Hambrick DZ. Relation of task switching to speed, age, and fluid intelligence. Psychol Aging. 1998;13(3):445–461. doi: 10.1037/0882-7974.13.3.445. [DOI] [PubMed] [Google Scholar]
- Schaie K. Developmental Influences on Adult Intellectual Development: The Seattle Longitudinal Study. New York: Oxford University Press; 2005. [Google Scholar]
- Schaie K, Willis S. Can decline in adult intellectual functioning be reversed? Developmental Psychology. 1986;22:223–232. [Google Scholar]
- Smith GE, Housen P, Yaffe K, Ruff R, Kennison RF, Mahncke HW, et al. A cognitive training program based on principles of brain plasticity: results from the Improvement in Memory with Plasticity-based Adaptive Cognitive Training (IMPACT) study. J Am Geriatr Soc. 2009;57(4):594–603. doi: 10.1111/j.1532-5415.2008.02167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stine-Morrow E, Basak C. Cognitive intervention. In: Schaie K, Willis S, editors. Handbook of the psychology of aging. 7th. Amsterdam: Elsevier; 2011. pp. 153–171. [Google Scholar]
- Thurstone L, Thurstone T. Examiner Manual for the SRA Primary Mental Abilities Test (Form 10-14) Chicago: Science Research Associates; 1949. [Google Scholar]
- Verhaeghen P, Marcoen A, Goossens L. Improving memory performance in the aged through mnemonic training: a meta-analytic study. Psychol Aging. 1992;7(2):242–251. doi: 10.1037//0882-7974.7.2.242. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Willis S, Nesselroade C. Long term effects of fluid ability training in old-old age. Dev Psychol. 1990;26:905–910. [Google Scholar]
- Willis S, Schaie K. Cognitive training in the normal elderly. In: Forette F, Christen Y, Boller F, editors. Plasticité Cérébrale et Stimulation Cognitiv. Paris: Foundation National de Gérontologie; 1994. [Google Scholar]
- Willis SL, Tennstedt SL, Marsiske M, Ball K, Elias J, Koepke KM, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. Jama. 2006;296(23):2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]