Abstract
Purpose
Although the occurrence and progression of AIS has been linked to low bone mineral density (BMD), the relationships between spinal curvature and bilateral differences in proximal femur BMD are controversial. Few correlation studies have stratified patients by curve type. The purpose of this study was to evaluate the relationships between spinal coronal profile and bilateral differences in proximal femur BMD in patients with adolescent idiopathic scoliosis (AIS).
Methods
This study included 67 patients with AIS who underwent posterior correction and fusion surgery between January 2009 and October 2011. The mean age at the time of surgery was 17.4 ± 4.1 years. Bilateral proximal femur BMD was measured before surgery by dual-energy X-ray absorptiometry. We compared the proximal femur BMDs by determining the bilateral BMD ratio (left proximal femur BMD divided by that of the right). We evaluated correlations between coronal parameters, obtained from preoperative radiographs, and the BMD ratio using Pearson’s correlation analysis.
Results
Patients with Lenke type 1 curve (48; all with a right convex curve) had a mean bilateral proximal femur BMD ratio of 1.00 ± 0.04. Patients with Lenke type 5 curve (19; all with a left convex curve) had a mean bilateral proximal femur BMD ratio of 0.94 ± 0.04, indicating that the BMD in the proximal femur on the right side (concave) was greater than that in the left (convex). Coronal balance was significantly correlated with the BMD ratio in both the Lenke type 1 and type 5 groups, with a correlation coefficient of 0.46 and 0.50, respectively.
Conclusions
The bilateral proximal femur BMD ratio was significantly correlated with the coronal balance in AIS patients. When the C7 plumb line was shifted toward one side, the BMD was greater in the contralateral proximal femur.
Keywords: Adolescent idiopathic scoliosis, Bone mineral density, Proximal femur
Introduction
In 1982, Burner et al. reported that patients with adolescent idiopathic scoliosis (AIS) had low bone mineral density (BMD) as assessed by the Singh index [1]. Other studies have also reported an association between low BMD and the occurrence of AIS [2–7]. The prevalence of low BMD in AIS is 20–38 %, with low BMD being defined as a BMD value more than 2 SD below the mean value in age-matched, healthy control subjects [2–6]. Hung et al. identified low BMD in the proximal femur on the concave side as a risk factor in predicting AIS curve progression [8]. However, the relationships between spinal curvature and proximal femur BMD in AIS have been controversial. Some authors have reported differences in the proximal femur BMD in the right and left limb [8, 9], which might be attributable to asymmetrical mechanical loading due to spinal deformity. However, with the aid of a weight-bearing pattern analyzer, Hoppenfeld et al. [10] determined that spinal curvature is not associated with the amount of load borne by each foot. Some studies have found no significant relationship between spinal curvature and bilateral differences in femur BMD [1, 4, 6, 11, 12]. However, few studies have grouped subjects by curve type when evaluating correlations with BMD, which may account for these discrepancies.
Since relationships between the spinal coronal profile, especially the coronal balance, and bilateral proximal femur BMD have not yet been clarified, this study was conducted to evaluate correlations between the spinal coronal profile and bilateral differences in proximal femur BMD in AIS patients stratified by curve type.
Materials and methods
In this study, we reviewed the radiographs of 67 consecutive AIS patients (3 male, 64 female) with Lenke type 1 (48 patients) or type 5 curve [13] (19 patients) who underwent posterior correction and fusion surgery between January 2009 and October 2011. The mean age at the time of surgery was 17.4 ± 4.4 years (range 11.6–31.8 years) for all patients, and 17.7 ± 4.4 years (range 11.6–31.8 years) in the Lenke type 1 group and 16.6 ± 3.2 years (range 12.7–24.5 years) in the Lenke type 5 group. Although there are six Lenke curve types, we evaluated the two most common single-curve types to simplify the analysis. All patients in the Lenke type 1 group had a right convex thoracic curve, and in the Lenke type 5 group, all patients had a left convex thoracolumbar or lumbar curve.
Bilateral proximal femur BMD was measured prior to surgery using dual-energy X-ray absorptiometry (DEXA) (Lunar Prodigy Advance Encore 10X, GE Healthcare, Madison, WI, USA). To measure the femoral neck in anterior–posterior position, a foot support was used to maintain a 20° inward rotation of the legs to compensate for femoral neck anteversion and to minimize the effect of the pelvic rotation on the measurement results which might occur in scoliosis patients. Quality assurance was performed daily using the standard phantom provided by the manufacturer. We used the total proximal femur BMD and femoral neck BMD values for this study, since the reported precision error in BMD measurements of the total proximal femur (0.6–1.0 %) [14, 15] and femoral neck (1.2–2.1 %) [14, 15] is low compared with that in Ward’s triangle (1.6–3.9 %) [16–18] or the greater trochanter (1.5–3.7 %) [16–18].
We evaluated correlations between coronal parameters and bilateral differences in the proximal femur BMD, and between the coronal balance and pelvic obliquity. This study was approved by the medical ethics committee of Keio University Hospital.
Radiographic measurements
The following measurements were obtained from preoperative standing X-rays: the Cobb angles of the proximal thoracic, main thoracic, and thoracolumbar/lumbar curves; the apical vertebral translation, defined as the distance between the apex of the main thoracic curve and the C7 plumb line (C7PL) in Lenke type 1 patients or the distance between the apex of the main thoracolumbar/lumbar curve and the central sacral vertebral line (CSVL) in Lenke type 5 patients; and the coronal balance, defined as the distance between the CSVL and the C7PL. The value of the coronal balance was defined as negative when the C7PL was to the left side of the CSVL. We also measured pelvic obliquity and leg length discrepancy, using the method reported by O’Brien [19]. The angle of pelvic obliquity was defined as having a positive value if the sulcus of the S1 ala was higher on the left than on the right side. Similarly, the leg length discrepancy was defined as having a positive value if the left femoral head was higher than the right femoral head. All measurements were performed by the first author of the present study (RC); all radiographic parameters were measured with the CIS-Image/Viewer digital measurement software (Ver. 2.11.31, IBM, Japan).
Correlations between the BMD ratio and coronal parameters
Differences in bilateral proximal femur BMD values were compared by the BMD ratio, defined as the proximal femur BMD on the left side divided by that on the right. Correlations between the BMD ratio and coronal parameters obtained from radiographs were evaluated separately for the Lenke type 1 and type 5 groups.
Statistical analysis
SPSS software version 19.0 (IBM, New York) was used for statistical analysis of the data. Statistical significance was defined as a P value less than 0.05. Differences in BMD values between the right and left femur were evaluated by a paired t test. Correlations between BMD ratios and radiographic parameters, and between coronal balance and pelvic obliquity, were evaluated using Pearson’s correlation analysis.
Results
BMD and radiographic parameters
In the Lenke type 1 group, the mean total BMD in the femoral neck and in the total proximal femur did not differ between the left and right sides (Table 1), with mean total BMD ratios of 1.00 ± 0.06 and 1.00 ± 0.04, respectively. The mean coronal balance was 1.1 ± 12.3 mm (Table 2), and the mean pelvic obliquity was -1.4 ± 3.0° with a mean length discrepancy of 1.5 ± 3.5 mm. However, in the Lenke type 5 group, the mean total BMD in the femoral neck and the total proximal femur was significantly higher on the right than on the left side (Table 1), with mean BMD ratios of 0.97 ± 0.05 and 0.94 ± 0.04, respectively. The mean coronal balance was −20.2 ± 13.3 mm, and the mean pelvic obliquity was −4.6 ± 2.9° (Table 2). The mean discrepancy in length between the right and left leg was quite small (0.5 ± 10.6 mm).
Table 1.
BMD values and BMD ratios
| Type 1 | Type 5 | |||||
|---|---|---|---|---|---|---|
| Mean ± SD (g/cm2) | Range | P value* | Mean ± SD (g/cm2) | Range | P value* | |
| Femoral neck | ||||||
| Left | 0.93 ± 0.14 | 0.67–1.25 | 0.930 | 0.95 ± 0.11 | 0.72–1.14 | 0.007 |
| Right | 0.93 ± 0.14 | 0.64–1.25 | 0.99 ± 0.11 | 0.72–1.19 | ||
| BMD ratio | 1.00 ± 0.06 | 0.89–1.17 | 0.97 ± 0.05 | 0.86–1.05 | ||
| Total proximal femur | ||||||
| Left | 0.94 ± 0.12 | 0.63–1.17 | 0.517 | 0.94 ± 0.11 | 0.73–1.09 | 0.001 |
| Right | 0.94 ± 0.13 | 0.65–1.23 | 1.00 ± 0.11 | 0.75–1.19 | ||
| BMD ratio | 1.00 ± 0.04 | 0.94–1.12 | 0.94 ± 0.04 | 0.84–1 | ||
* Evaluation between left BMD and right BMD using paired t test
Table 2.
Radiographic parameters
| Type 1 | Type 5 | |||
|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | |
| Proximal thoracic Cobb angle (°) | 24.2 ± 5.4 | 4.9–32.6 | 9.2 ± 8.3 | 3.3–15.0 |
| Main thoracic Cobb angle (°) | 53.9 ± 7.3 | 42.4–70.5 | 25.4 ± 6.0 | 14.5–36.0 |
| Thoracolumbar/Lumbar Cobb angle (°) | 31.2 ± 9.1 | 13.7–48.5 | 45.2 ± 6.8 | 32.5–60.1 |
| Coronal balance (mm) | 1.1 ± 12.3 | −26.4–33.1 | −20.2 ± 13.3 | −44.3–6.5 |
| Apical translation (mm) | 50.5 ± 10.9 | 29.4–80.2 | −44.0 ± 26.6 | −63.7–59.5 |
| Pelvic obliquity (°) | −1.4 ± 3.0 | −9.4–7.5 | −4.6 ± 2.9 | −10.9–1.2 |
| Leg length discrepancy (mm) | 1.5 ± 3.5 | −5.0–10.6 | 0.5 ± 4.8 | −8.5–10.3 |
Pelvic obliquity was significantly correlated with coronal balance in the Lenke type 1 group, with a correlation coefficient of 0.406 (P = 0.004). However, no significant correlation was seen in the Lenke type 5 group (P = 0.806).
Correlation analysis
The coronal balance was significantly correlated with the bilateral BMD ratio, both in the femoral neck and the total proximal femur, in both the Lenke type 1 and type 5 groups; correlation coefficients ranged between 0.402 and 0.498 (Table 3). Pelvic obliquity was significantly correlated with the bilateral total proximal femur BMD ratio in the Lenke type 1 group, with a correlation coefficient of 0.446. However, the proximal femur BMD ratio was not correlated with the Cobb angle of the main curve, the apical translation, or the leg length discrepancy.
Table 3.
Correlation between radiographic parameters and BMD ratios
| Main curve Cobb angle | Apical translation | Coronal balance | Pelvic obliquity | Leg length discrepancy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| R | P value | R | P value | R | P value | R | P value | R | P value | |
| Femoral neck | ||||||||||
| Type1 | 0.013 | 0.932 | −0.060 | 0.684 | 0.402 | 0.005* | 0.275 | 0.058 | 0.037 | 0.804 |
| Type5 | 0.329 | 0.169 | −0.043 | 0.862 | 0.478 | 0.038* | 0.165 | 0.499 | 0.293 | 0.223 |
| Total proximal femur | ||||||||||
| Type1 | 0.011 | 0.939 | −0.048 | 0.747 | 0.464 | 0.001* | 0.446 | 0.001* | 0.155 | 0.297 |
| Type5 | 0.307 | 0.201 | 0.231 | 0.342 | 0.498 | 0.030* | 0.062 | 0.800 | 0.153 | 0.531 |
Bold values indicate statistical significance at (P < 0.05)
R correlation coefficient
* Significant correlation by Pearson correlation analysis
Discussion
We found that the mean BMD of the femoral neck and the total proximal femur was significantly higher on the concave than on the convex side of the curve in the Lenke type 5 group; however, no significant difference was observed in the Lenke type 1 group. Thus, the type of curve should be considered when discussing differences in bilateral proximal femur BMD values. In a study of 318 patients with AIS, Hung et al. [8] found that the mean BMD in the femoral neck on the concave side of the curve was significantly larger than that on the convex side, and Hans et al. [20] reported that 15 females with structural lumbar scoliosis had lower femoral neck BMD on the convex side of the curve. However, other authors found no significant differences in bilateral proximal femur BMD values [1, 4, 6, 11, 12], Previous studies have not grouped subjects by spinal curvature using a validated classification such as the Lenke [13] or King [21] system, which may account for some of these discrepancies.
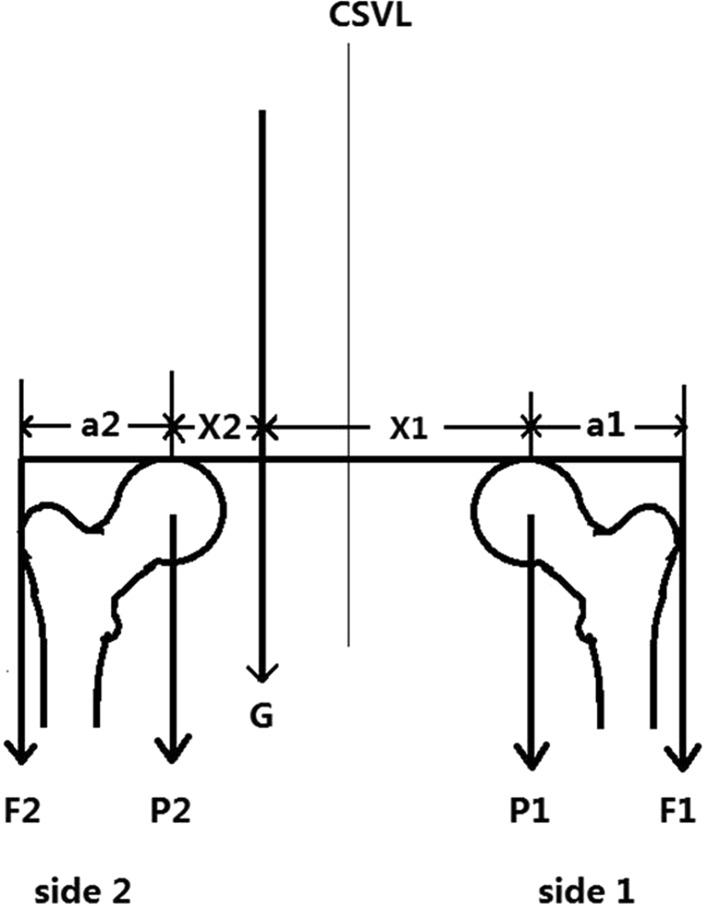
Regarding coronal parameters, patients in the Lenke type 1 group were well balanced on the coronal plane. The left and right pelvis were almost parallel, and the average leg length discrepancy was minimal. In patients in the Lenke type 5 group, the trunk was shifted to the left side (mean coronal balance −20.2 ± 13.3 mm), and the left pelvis was lower than the right (mean pelvic obliquity: −4.6 ± 2.9°) on average. Meanwhile, the mean total BMD in the femoral neck and in the total proximal femur did not differ between the left and right sides in the Lenke type 1 group, but the mean BMD values were significantly higher on the right than on the left side in the Lenke type 5 group. Since these results indicated that coronal parameters might influence differences in bilateral proximal femur BMD, we evaluated possible relationships and found that coronal balance was significantly correlated with the BMD ratio in both the Lenke type 1 and type 5 groups. Interestingly, the proximal femur BMD was higher in the side opposite to the direction of the C7PL shift away from the CSVL (Fig. 1), contrary to our expectation that a C7PL shift would cause BMD to increase in the proximal femur on the same side. This may be explained by the hip joint biomechanics described by Denham [22] (Fig. 2), in which the load on the proximal femur head on side 1 is equal to the sum of the force of gravity (G) and gluteal force (F1) (P1 = G+F1) (Fig. 2). If the C7PL, which can be used to indicate gravity (G), shifts toward side 2, G gains a longer force arm on the femur head on side 1 (X1 > X2), and F1 consequently increases. Finally, these forces would increase with any load added on side 1. Since BMD increases under mechanical stress, the femur BMD on side 1 would increase. However, we have neither demonstrated that the gravity line was identical with C7PL nor the changes of the moments at hips joints. Further evaluation using gait analysis system and stabilometry is required to elucidate the biomechanical background of the result in this study.
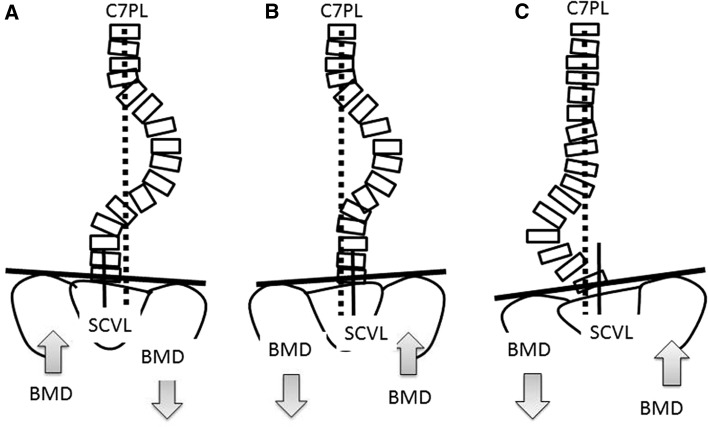
Fig. 1.
Relationships between coronal balance, pelvic obliquity, and proximal femur BMD In Lenke type 1 the pelvis and the proximal femur BMD were raised (a) on the concave side with a C7PL shift to the convex side, and (b) on the convex side if C7PL shifted to the concave side. In Lenke type 5, C7PL generally shifted to the convex side, with (c) BMD raised on the concave side and the pelvis raised on the concave side
Fig. 2.
Hip joint biomechanics Pressure on femoral head (P) = gravity (G) + gluteal force (F); a distance between femoral head and greater trochanter, X: distance between femoral head and gravity. If G shifts to side 2, G will gain a longer force arm on side 1 (X1 > X2). Consequently, F1 will increase. Finally, P1 will be larger than P2
Pelvic obliquity was significantly correlated with the BMD ratio for the total proximal femur only in the Lenke type 1 group (Table 3), possibly because pelvic obliquity was significantly correlated with coronal balance only in this group. In Lenke type 1 curve, if the C7PL shifts to one side, the contralateral pelvis elevates (Fig. 1a and b). In patients with Lenke type 5 curve, however, pelvic obliquity may relate to the lumbar curvature rather than the coronal balance, so the pelvis is usually higher on the concave than on the convex side (Fig. 1c).
In conclusion, bilateral difference in the proximal femur BMD was significantly correlated with coronal imbalance in both the Lenke type 1 and type 5 groups, where the C7PL shifted toward one side, the proximal femur BMD was greater on the opposite side. This conclusion should be tested by further biomechanical studies.
Acknowledgments
This study was supported in part by the Japan–China Sasakawa Medical Fellowship.
Conflict of interest
None.
References
- 1.Burner WL, 3rd, Badger VM, Sherman FC. Osteoporosis and acquired back deformities. J Pediatr Orthop. 1982;2:383–385. doi: 10.1097/01241398-198210000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Cheng JC, Guo X, Sher AH. Persistent osteopenia in adolescent idiopathic scoliosis. A longitudinal follow up study. Spine (Phila Pa 1976) 1999;24:1218–1222. doi: 10.1097/00007632-199906150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Cheng JC, Hung VW, Lee WT, Yeung HY, Lam TP, Ng BK, Guo X, Qin L. Persistent osteopenia in adolescent idiopathic scoliosis–longitudinal monitoring of bone mineral density until skeletal maturity. Stud Health Technol Inform. 2006;123:47–51. [PubMed] [Google Scholar]
- 4.Cheng JC, Qin L, Cheung CS, Sher AH, Lee KM, Ng SW, Guo X. Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis. J Bone Miner Res. 2000;15:1587–1595. doi: 10.1359/jbmr.2000.15.8.1587. [DOI] [PubMed] [Google Scholar]
- 5.Cheung CS, Lee WT, Tse YK, Lee KM, Guo X, Qin L, Cheng JC. Generalized osteopenia in adolescent idiopathic scoliosis–association with abnormal pubertal growth, bone turnover, and calcium intake? Spine (Phila Pa 1976) 2006;31:330–338. doi: 10.1097/01.brs.0000197410.92525.10. [DOI] [PubMed] [Google Scholar]
- 6.Cook SD, Harding AF, Morgan EL, Nicholson RJ, Thomas KA, Whitecloud TS, Ratner ES. Trabecular bone mineral density in idiopathic scoliosis. J Pediatr Orthop. 1987;7:168–174. doi: 10.1097/01241398-198703000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Suh KT, Eun IS, Lee JS. Polymorphism in vitamin D receptor is associated with bone mineral density in patients with adolescent idiopathic scoliosis. Eur Spine J. 2010;19:1545–1550. doi: 10.1007/s00586-010-1385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hung VW, Qin L, Cheung CS, Lam TP, Ng BK, Tse YK, Guo X, Lee KM, Cheng JC. Osteopenia: a new prognostic factor of curve progression in adolescent idiopathic scoliosis. J Bone Jt Surg Am. 2005;87:2709–2716. doi: 10.2106/JBJS.D.02782. [DOI] [PubMed] [Google Scholar]
- 9.Lee WT, Cheung CS, Tse YK, Guo X, Qin L, Lam TP, Ng BK, Cheng JC. Association of osteopenia with curve severity in adolescent idiopathic scoliosis: a study of 919 girls. Osteoporos Int. 2005;16:1924–1932. doi: 10.1007/s00198-005-1964-7. [DOI] [PubMed] [Google Scholar]
- 10.Hoppenfeld S, Lopez RA, Molnar G. Plantar weight-bearing pattern in idiopathic scoliosis. Spine (Phila Pa 1976) 1991;16:757–760. doi: 10.1097/00007632-199107000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Cheng JC, Guo X. Osteopenia in adolescent idiopathic scoliosis. A primary problem or secondary to the spinal deformity? Spine (Phila Pa 1976) 1997;22:1716–1721. doi: 10.1097/00007632-199708010-00006. [DOI] [PubMed] [Google Scholar]
- 12.Thomas KA, Cook SD, Skalley TC, Renshaw SV, Makuch RS, Gross M, Whitecloud TS, 3rd, Bennett JT. Lumbar spine and femoral neck bone mineral density in idiopathic scoliosis: a follow-up study. J Pediatr Orthop. 1992;12:235–240. doi: 10.1097/01241398-199203000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 14.Shepherd JA, Fan B, Lu Y, Lewiecki EM, Miller P, Genant HK. Comparison of BMD precision for Prodigy and Delphi spine and femur scans. Osteoporos Int. 2006;17:1303–1308. doi: 10.1007/s00198-006-0127-9. [DOI] [PubMed] [Google Scholar]
- 15.Krueger D, Vallarta-Ast N, Checovich M, Gemar D, Binkley N. BMD measurement and precision: a comparison of GE Lunar Prodigy and iDXA densitometers. J Clin Densitom. 2012;15:21–25. doi: 10.1016/j.jocd.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazess R, Chesnut CH, 3rd, McClung M, Genant H. Enhanced precision with dual-energy X-ray absorptiometry. Calcif Tissue Int. 1992;51:14–17. doi: 10.1007/BF00296209. [DOI] [PubMed] [Google Scholar]
- 17.Williams-Russo P, Healey JH, Szatrowski TP, Schneider R, Paget S, Ales K, Schwartzberg P. Clinical reproducibility of dual energy x-ray absorptiometry. J Orthop Res. 1995;13:250–257. doi: 10.1002/jor.1100130213. [DOI] [PubMed] [Google Scholar]
- 18.Leib ES, Lewiecki EM, Binkley N, Hamdy RC. Official positions of the International Society for Clinical Densitometry. J Clin Densitom. 2004;7:1–6 . doi: 10.1385/JCD:7:1:1. [DOI] [PubMed] [Google Scholar]
- 19.O’Brien M, Kuklo T, Blanke K, Lenke L, Group(SDSG). SDS (2004) Radiographic measurement manual. Medtronic Sofamor Danek USA, Memphis, Tennessee
- 20.Hans D, Biot B, Schott AM, Meunier PJ. No diffuse osteoporosis in lumbar scoliosis but lower femoral bone density on the convexity. Bone. 1996;18:15–17 . doi: 10.1016/8756-3282(95)00421-1. [DOI] [PubMed] [Google Scholar]
- 21.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Jt Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 22.Denham RA. Hip mechanics. J Bone Joint Surg Br. 1959;41-B:550–557. doi: 10.1302/0301-620X.41B3.550. [DOI] [PubMed] [Google Scholar]