Abstract
Background: Recent studies have shown inconsistent effects of sodium reduction, potassium intake, and the ratio of sodium to potassium (Na/K ratio) on hypertension and other cardiovascular diseases. Major gaps exist in knowledge regarding these issues in China.
Objective: We analyzed the patterns and trends of dietary sodium intake, potassium intake, and the Na/K ratio and their relations with incident hypertension in China.
Design: The China Health and Nutrition Survey cohort includes 16,869 adults aged 20–60 y from 1991 to 2009. Three consecutive 24-h dietary recalls and condiment and food weights provided detailed dietary data. Multinomial logistic regression models determined trends and patterns of sodium and potassium intake and the Na/K ratio. Models for survival-time data estimated the hazard of incident hypertension.
Results: Sodium intake is decreasing but remains double the Institute of Medicine recommendations. Most sodium comes from added condiments. Adults in the central provinces have the highest sodium intake and the most rapid increase in hypertension. Potassium intake has increased slightly but is below half of the recommended amount. The Na/K ratio is significantly higher than the recommended amounts. Recent measurements of high sodium intake, low potassium intake, and high Na/K ratio have strong independent dose-response associations with incident hypertension.
Conclusions: Reducing sodium in processed foods, the major public health strategy in Western countries, may be less effective in China, where salt intake remains high. Replacing sodium with potassium in salt to control and prevent hypertension in China should be considered along with other public health and clinical prevention options.
INTRODUCTION
Cardiovascular disease is the leading cause of death in China, and hypertension is the key modifiable risk factor (1, 2). Reducing the burden of diseases associated with hypertension has been identified as a global public health priority (3). High sodium intakes and low potassium intakes are among the key risk factors for hypertension (4–8). Sodium-reduction strategies have been shown to be low cost and effective, and studies have shown significant estimates of their benefits across low- and high-income countries (9–11). However, many recent studies suggest that there are insufficient data to support sodium reduction in the general population. Furthermore, limited research suggests that low sodium intake (<1.5 g/d) may worsen health outcomes (12–15), although this relation has engendered considerable controversy (15–22).
Potassium has long been recognized as a protective factor for hypertension (23). Recent studies have focused additional attention on diets deficient in potassium as a major component of hypertension campaigns (24). Recent Chinese studies have shown the significant positive effects of sodium replacement with potassium on blood pressure (25, 26).
Studies on sodium intake and potassium intake in China are limited. International Study of Electrolyte Excretion and Blood Pressure conducted a study in the late 1980s in 2 communities in the North (one near a military hospital in Beijing and the other in a village in Tianjin) and one in the South (at a medical college in Nanning) (27). International Population Study on Macronutrients and Blood Pressure conducted another study in the late 1990s in 3 counties (2 in the North and one in the South) (28). Both studies showed that sodium intake was higher in the North than in the South. Neither of these studies included subsamples from central China.
Despite the importance of potassium and the potential to reduce blood pressure and affect the burden of disease, few studies in China or elsewhere have explored systematically the sources and trends of sodium and potassium intake and their health effects in large populations in cross-sectional or longitudinal studies. Using unique in-depth measurements of sodium and potassium consumption based on added salt, soy sauce, and monosodium glutamate (MSG)4 and consumption of processed foods, we present the results of research on patterns and trends of sodium and potassium intakes and their relations with incident hypertension from 1991 to 2009 in 9 Chinese provinces representing 47% of the overall Chinese population according to recent census data.
SUBJECTS AND METHODS
Study design and subjects
We used data from 16,869 adults aged 20–60 y at enrollment in the China Health and Nutrition Survey (CHNS), an ongoing open-cohort study initiated in 1989 and followed up in 1991, 1993, 1997, 2000, 2004, 2006, and 2009. We used a multistage, random-cluster process to draw the sample surveyed in each of the following provinces from northeast to southwest: Heilongjiang, Liaoning, Jiangsu, Shandong, Henan, Hubei, Hunan, Guizhou, and Guangxi. We randomly selected 2 cities and 4 counties, stratified by income, in each province based on their income levels reported by the State Statistical Bureau in 1988. We randomly selected 4 communities in each city or county and 20 households in each community and interviewed all household members. The design, sampling, and response rates are reported elsewhere (29). Overall response rates, based on those who participated in previous surveys and remained in the current survey, were ∼88% at the individual level and 90% at the household level (29).
The institutional review committees of the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention, approved the survey protocols and instruments and the process for obtaining informed consent for this study. Participants provided their written informed consent.
Diet measurement
We collected diet data at the household level and at the individual level using weighing methods in combination with 3 consecutive 24-h dietary recalls (30, 31). All foods and condiments in the home inventory, purchased from markets, and picked from gardens were carefully recorded and measured with Chinese balance scales (graduation: 10 g) before 2004 and with digital diet and kitchen scales (graduation: 1 g) thereafter at the start of the first 24-h dietary recall and at the end of the last 24-h dietary recall in each survey. In addition, all mixed dishes were disaggregated by measuring all components of the recipe to allow accurate measurement at the household level (32). The days of 24-h dietary recalls were selected randomly from Monday to Sunday in each community. All interviewers participated in at least one 7-d training session and passed a comprehensive test before collecting any data.
We allocated proportions of foods and condiments consumed at the household level to each individual based on the proportion of a specific food or condiment that he or she consumed (31). In Chinese cuisine, condiments are added to food during cooking and preparation. To determine which foods and recipes encountered in our study used salt, soy sauce, and MSG, we conducted detailed interviews with Chinese chefs, housewives, nutritionists, and dietitians. From these interviews we determined that salt is added to all cooked dishes except rice and steamed flour products, soy sauce is added to noodles and meat dishes, and MSG is added to cooked vegetables and meat dishes. We calculated sodium intake (ie, sodium from all foods and condiments, including added salt) and potassium intake based on their compositions in the Chinese food-composition table (FCT), which includes sodium and potassium in >2500 foods measured with the Perkin-Elmer Analyst 800 (33). The sodium and potassium compositions of a few foods imported or unavailable in Chinese markets were adopted from the FCTs of Hong Kong, Taiwan, Japan, or the USDA.
Validation of sodium and potassium intake
We weighed intakes of salt, soy sauce, and MSG at the household level directly and accurately, and we estimated sodium and potassium intake based on consumption of all foods and condiments. A validation study evaluated the accuracy of estimated sodium and potassium intakes at the individual level in one of our survey provinces (but not with CHNS participants) by measuring urinary sodium and potassium excretions from 24-h urine samples collected for 3 consecutive days and by using p-aminobenzoic acid as a marker of completeness of 24-h urine samples. The correlation coefficients between dietary sodium and potassium intakes estimated by weighing with 24-h dietary recalls and by urinary sodium and potassium excretions measured from 24-h urine samples were 0.58 and 0.59, respectively (P = 0.005). In an independent validation of MSG intake, the correlation coefficient between individual MSG intakes estimated by weighing with 24-h dietary recalls and by using a urinary riboflavin marker was 0.82 (P < 0.010) (34).
In a previous study, the diet protocol for measurement of total energy intake was validated by using the doubly labeled water method, with all assays undertaken in the Human Nutrition Research Center, Tufts University. The correlation coefficient between the 2 methods was 0.56 for men and 0.60 for women (35).
Blood pressure measurement
Experienced physicians who attended a 7-d data-collection training session and passed a comprehensive reliability test measured blood pressure with the participant in the sitting position after 5 min of rest. Standard mercury sphygmomanometers with regular adult cuffs were used as indicated in the manufacturer's guidelines. The cuff was placed on the participant's right arm (the lower edge ∼25 mm above the elbow) and inflated until the cuff pressure was 30 mm Hg above the level at which the pulse disappeared. Diastolic blood pressures (DBPs) were determined by using the fifth phase of the Korotkoff method. Three measurements were obtained with a 30-s interval between cuff inflations if the first measure was normal. Otherwise, participants were requested to take 10–30 min of rest before a second measurement was taken. We defined hypertension as having a mean systolic blood pressure (SBP) of ≥140 mm Hg, a mean DBP of ≥90 mm Hg, currently undergoing treatment with antihypertensive medication, or previously diagnosed by a physician (36).
Statistical methods
For continuous variables, we applied general linear regression models and t tests to test differences between groups and trends. We tested categorical variables by using chi-square tests. We divided inflation-adjusted per capita household income into tertiles (low-, middle-, and high-income levels) and resident locations into 3 areas based on geographic location: North (Heilongjiang and Liaoning), central (Shandong, Jiangsu, and Henan), and South (Hubei, Hunan, Guangxi, and Guizhou). We grouped communities in large cities and county capital cities into urban areas and communities in suburban and rural villages into rural areas. We divided education levels into 2 categories: below high school and high school or higher. We defined smokers as those who ever smoked and alcohol drinkers as those who drank any alcoholic beverage at least once a month in the past year. We represented the prevalence of hypertension as the raw rate, age-specified rate, and standardized rate using the population in 1991.
Because dependent variables and independent variables were contemporaneously correlated among the error terms, we used seemingly unrelated regression models (37, 38) that correct for error term correlations between each of the 4 regressions (added salt, soy sauce, MSG, and processed foods) to determine the dynamic trends of sodium consumption. We included age, sex, education, income, residence location (urban or rural), region (North/central/South), and survey year in the models.
We used multinomial logit analysis, which generalizes logistic regression by allowing >2 discrete outcomes, to examine the demographic and economic factors associated with various categories of sodium, potassium, and ratio of sodium to potassium (Na/K ratio) in the study population (39, 40). We categorized 5 levels of sodium intake (<1.5, 1.5–2.2, 2.3–3.9, 4.0–5.9, and ≥6.0 g/d), 4 levels of potassium intake (<1.6, 1.6–1.9, 2.0–2.9, and ≥3.0 g/d), and 3 levels of the Na/K ratio (<1.0, 1.0–1.9, and ≥2.0) based on the levels recommended by the Institute of Medicine (IOM) and WHO (3, 41). Results are represented as adjusted probabilities of each respondent falling into one of these categories.
To examine the effects of sodium intake, potassium intake, and the Na/K ratio on incident hypertension, we conducted a subanalysis that included all subjects free of hypertension at baseline and with at least one wave of dietary data complete before the event or censoring. We used flexible parametric models for survival-time data and selected the odds scale and 3 splines (from 0 to 5 available) based on the lowest Akaike Information Criterion (42). We defined baseline as the first available measure and considered the event to happen between the wave of the first hypertension measurement and the previous wave. We compared 3 ways of including dietary data from the repeated measures (the measure closest to the baseline, the mean of all available values during follow-up, and the most current measure closest to the event or censoring) but present the results only for the most recent, because this one had stronger estimates. We built models for sodium quintiles, potassium quintiles (adjusted for sodium intake), and Na/K ratio quintiles separately. All models were adjusted by baseline covariates: age, sex, education, income, region, BMI, physical activity, smoking status, alcohol intake, and energy intake. Interactions with geographic region were assessed with a likelihood ratio test between the models with and without interaction terms. We used the macro %EMICM in SAS version 9.2 (SAS Institute) to compute the survival curves for interval-censored data. We cleaned, managed, and analyzed all the data with SAS software version 9.2 and STATA version 11 (StataCorp).
RESULTS
The average sample age at baseline was 37.4 y. Of the participants, 52.0% were women, 82.5% did not have a high school education, and 32.1% lived in an urban area. The average SBP, DBP, and prevalence of hypertension at baseline were 112.2 mm Hg, 73.5 mm Hg (Table 1), and 10.4%, respectively.
TABLE 1.
Characteristics of participants, 1991–20091
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | |
| No. of subjects | 7337 | 6958 | 7241 | 7940 | 7250 | 6826 | 6932 |
| Sample participated previously (%)2 | 85.0 | 60.5 | 78.4 | 78.6 | 88.2 | 77.7 | |
| Replenishment sample (%) | 15.0 | 39.5 | 21.6 | 21.4 | 11.8 | 22.3 | |
| Age (y) | 37.4 ± 11.03 | 37.9 ± 10.9 | 38.8 ± 10.8 | 40.1 ± 10.5 | 42.3 ± 10.4 | 43.3 ± 10.2 | 43.5 ± 10.6 |
| 20–29 y (%) | 32.2 | 28.8 | 26.0 | 20.7 | 15.0 | 12.0 | 13.6 |
| 30–39 y (%) | 28.9 | 29.2 | 26.9 | 28.8 | 25.8 | 24.9 | 22.3 |
| 40–49 y (%) | 22.6 | 25.3 | 28.6 | 29.7 | 30.3 | 30.9 | 31.0 |
| 50–60 y (%) | 16.4 | 16.7 | 18.5 | 20.8 | 29.0 | 32.2 | 33.2 |
| Female (%) | 52.0 | 52.0 | 51.0 | 51.2 | 52.2 | 52.5 | 52.0 |
| Rural areas (%) | 67.9 | 71.8 | 71.0 | 71.4 | 71.7 | 71.8 | 70.7 |
| Less than high school education (%) | 82.5 | 81.4 | 78.8 | 75.1 | 73.3 | 70.5 | 71.7 |
| Adjusted household income4 | 12.0 ± 8.8 | 13.8 ± 11.9 | 16.2 ± 13.3 | 20.0 ± 20.1 | 24.2 ± 24.4 | 28.5 ± 36.8 | 39.9 ± 46.6 |
| Smoker (%) | 32.4 | 31.3 | 33.4 | 29.2 | 32.2 | 31.2 | 31.5 |
| Men | 64.0 | 61.6 | 64.4 | 56.4 | 64.3 | 63.1 | 62.7 |
| Women | 3.3 | 3.4 | 3.5 | 3.2 | 2.9 | 2.4 | 2.6 |
| Alcohol drinker (%) | 35.5 | 33.6 | 37.9 | 32.6 | 34.2 | 33.8 | 36.3 |
| Men | 60.6 | 58.0 | 66.5 | 57.4 | 62.2 | 62.7 | 65.0 |
| Women | 12.3 | 11.1 | 10.3 | 8.8 | 8.7 | 7.7 | 9.7 |
| Weight (kg) | 55.8 ± 9.0 | 56.2 ± 9.0 | 57.8 ± 9.8 | 59.7 ± 10.3 | 60.5 ± 10.6 | 61.1 ± 10.7 | 61.8 ± 11.0 |
| Men | 59.2 ± 8.6 | 59.9 ± 8.5 | 61.5 ± 8.6 | 63.8 ± 10.2 | 64.8 ± 10.5 | 65.6 ± 10.6 | 66.5 ± 11.0 |
| Women | 52.7 ± 8.2 | 53.0 ± 8.2 | 54.4 ± 9.8 | 56.1 ± 8.9 | 56.7 ± 9.1 | 57.0 ± 8.9 | 57.6 ± 9.2 |
| BMI (kg/m2) | 21.7 ± 2.8 | 21.9 ± 2.7 | 22.3 ± 3.0 | 22.9 ± 3.1 | 23.1 ± 3.2 | 23.3 ± 3.2 | 23.4 ± 3.4 |
| Men | 21.5 ± 2.5 | 21.7 ± 2.5 | 22.2 ± 2.8 | 22.8 ± 3.0 | 23.1 ± 3.1 | 23.3 ± 3.1 | 23.5 ± 3.3 |
| Women | 22.0 ± 2.9 | 22.0 ± 2.9 | 22.5 ± 3.1 | 23.0 ± 3.2 | 23.2 ± 3.3 | 23.2 ± 3.3 | 23.3 ± 3.4 |
| SBP (mm Hg) | 112.2 ± 15.6 | 112.7 ± 14.9 | 116.1 ± 15.6 | 116.9 ± 15.5 | 119.1 ± 16.0 | 118.6 ± 15.7 | 120.8 ± 16.6 |
| Men | 114.7 ± 14.8 | 115.0 ± 13.7 | 118.2 ± 14.3 | 119.2 ± 14.2 | 121.5 ± 14.9 | 121.0 ± 14.6 | 122.9 ± 15.1 |
| Women | 109.9 ± 15.9 | 110.7 ± 15.6 | 114.1 ± 16.5 | 114.8 ± 16.2 | 116.9 ± 16.7 | 116.5 ± 16.2 | 118.8 ± 17.6 |
| DBP (mm Hg) | 73.5 ± 10.7 | 74.6 ± 10.3 | 76.2 ± 10.4 | 76.9 ± 10.5 | 78.1 ± 10.9 | 78.3 ± 10.5 | 79.8 ± 11.0 |
| Men | 75.2 ± 10.5 | 76.2 ± 10.0 | 77.8 ± 10.2 | 78.7 ± 10.1 | 79.9 ± 10.5 | 80.3 ± 10.3 | 81.8 ± 10.6 |
| Women | 72.0 ± 10.8 | 73.2 ± 10.4 | 74.8 ± 10.5 | 75.3 ± 10.7 | 76.5 ± 10.9 | 76.4 ± 10.4 | 78.0 ± 11.0 |
Age, weight, BMI, SBP, and DBP were significantly greater in 2009 than in any earlier year (P-trend < 0.01, general linear regression models). Percentage of participants aged ≥50 y who lived in urban areas and who achieved higher education were greater in 2009 than in earlier years (P-trend < 0.01, chi-square tests). Percentage of females, alcohol drinkers, and smokers did not significantly change over time (P-trend > 0.05, chi-square tests). DBP, diastolic blood pressure; SBP, systolic blood pressure.
The percentage of participants who participated previously is different from the follow-up rate, because participants younger than 20 y or older than 60 y were excluded from the analysis.
Mean ± SD (all such values).
Adjusted to Chinese yuan value in 2009 (per 1000 yuan).
Dietary sodium intake, potassium intake, and Na/K ratio
Sodium intake decreased from 6.6 g/d in 1991 to 4.7 g/d in 2009. Unadjusted results in 2009 show lower intakes for women than for men (4.5 g/d compared with 4.9 g/d; P = 0.0035), for younger age groups (4.6 g/d in those aged <50 y and 4.9 g/d in those aged ≥50 y; P-trend = 0.0001), and for urban than for rural residents (4.6 g/d compared with 4.7 g/d; P = 0.0150). Sodium intakes in southern (4.4 g/d) and northern (4.3 g/d) China were not significantly different (P = 0.7900); both were much lower than that in central China (5.3 g/d; P < 0.0001) (Table 2; also see Supplemental Table S1 under “Supplemental data” in the online issue).
TABLE 2.
Sodium intake, potassium intake, and Na/K ratio by region in China, 1991–20091
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | |
| Sodium intake (g/d) | |||||||
| Average | 6.6 ± 3.4 | 6.6 ± 3.4 | 6.2 ± 3.5 | 6.0 ± 3.2 | 5.2 ± 2.7 | 5.0 ± 2.8 | 4.7 ± 2.6 |
| North | 6.8 ± 3.5 | 5.6 ± 2.7 | 5.1 ± 3.3 | 5.1 ± 2.9 | 4.6 ± 2.6 | 4.5 ± 2.5 | 4.3 ± 2.6 |
| Central | 7.0 ± 3.4 | 7.5 ± 3.5 | 6.8 ± 3.7 | 6.9 ± 3.4 | 5.7 ± 3.0 | 5.3 ± 2.8 | 5.3 ± 2.8 |
| South | 6.3 ± 3.3 | 6.1 ± 3.3 | 5.9 ± 3.2 | 5.8 ± 3.1 | 5.0 ± 2.6 | 5.0 ± 2.9 | 4.4 ± 2.4 |
| Potassium intake (g/d) | |||||||
| Average | 1.5 ± 0.5 | 1.6 ± 0.6 | 1.8 ± 0.6 | 1.8 ± 0.7 | 1.8 ± 0.7 | 1.8 ± 0.7 | 1.8 ± 0.7 |
| North | 1.5 ± 0.5 | 1.5 ± 0.6 | 1.8 ± 0.6 | 1.7 ± 0.6 | 1.6 ± 0.6 | 1.9 ± 0.7 | 1.9 ± 0.7 |
| Central | 1.6 ± 0.6 | 1.6 ± 0.6 | 1.8 ± 0.6 | 1.9 ± 0.7 | 1.8 ± 0.7 | 1.8 ± 0.6 | 1.9 ± 0.7 |
| South | 1.5 ± 0.5 | 1.5 ± 0.6 | 1.8 ± 0.7 | 1.8 ± 0.7 | 1.8 ± 0.8 | 1.8 ± 0.7 | 1.8 ± 0.6 |
| Na/K ratio | |||||||
| Average | 4.9 ± 3.4 | 4.7 ± 3.2 | 3.7 ± 2.7 | 3.7 ± 2.2 | 3.2 ± 2.0 | 3.0 ± 1.8 | 2.8 ± 1.8 |
| North | 5.2 ± 4.3 | 4.1 ± 2.4 | 3.0 ± 2.1 | 3.3 ± 1.9 | 3.1 ± 2.2 | 2.6 ± 1.6 | 2.5 ± 1.9 |
| Central | 4.9 ± 3.1 | 5.2 ± 3.3 | 4.0 ± 2.3 | 4.0 ± 2.4 | 3.6 ± 2.3 | 3.1 ± 1.8 | 3.1 ± 1.7 |
| South | 4.7 ± 3.4 | 4.5 ± 3.3 | 3.7 ± 3.1 | 3.6 ± 2.0 | 3.0 ± 1.7 | 3.1 ± 1.9 | 2.7 ± 1.8 |
All values are means ± SDs. Sodium intake and the Na/K ratio significantly decreased and potassium intake increased over time (P-trend < 0.001, general linear regression models). In 2009, sodium intake and the Na/K ratio were greater in central China than in the North or in the South (P < 0.001, general linear regression models); potassium intake significantly but slightly differed between regions (P < 0.050, general linear regression models). Na/K ratio, ratio of sodium to potassium.
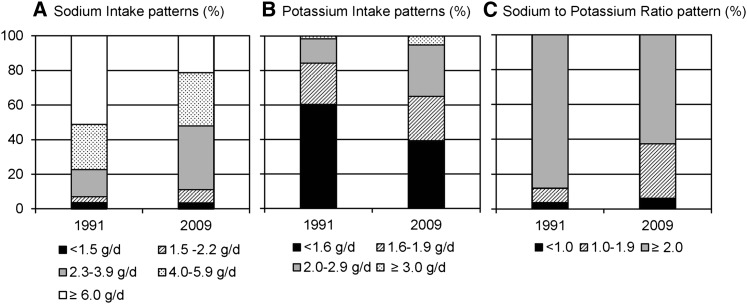
The proportion of the participants who consumed 2.3–6.0 g Na/d increased rapidly during our study period. Approximately 3.5% of the participants consumed <1.5 g Na/d in each survey, and ∼52.0% of adults consumed ≥4.0 g/d in 2009 (Figure 1A).
FIGURE 1.
Patterns of sodium intake (A), potassium intake (B), and Na/K ratio (C) in China, 1991–2009. Percentages of participants with a sodium intake <2.3 g/d, a potassium intake ≥3.0 g/d, and an Na/K ratio <1.0 were greater in 2009 than in 1991 (P-trend < 0.001, chi-square tests). Na/K ratio, the ratio of sodium to potassium.
Potassium intake increased from 1.5 g/d in 1991 to 1.8 g/d in 2009. Potassium intake was lower in women (P < 0.0001), in the low-income group (P < 0.0001), and in the lower-education group (P = 0.0100). Although statistically significant, the variations between groups were only 0.1–0.2 g/d. Major regional differences did not exist, nor did they exist by age or urban or rural residence (P = 0.3000) (Table 2; also see Supplemental Table S2 under “Supplemental data” in the online issue). Few subjects had a potassium intake ≥3.0 g/d in 2009 (Figure 1B). In 2009, 60.8% had a potassium intake ≥1.6 g/d, up from 39.6% in 1991.
The average Na/K ratio was 2.8 in 2009. The Na/K ratio was higher in the low-income group (P < 0.0001), in the lower-education group (P = 0.0009), and in the group aged ≥50 y (P = 0.0003). Subjects in central China had the highest ratio (P = 0.0070). On average, 6.1% of subjects had an Na/K ratio <1.0 (up from 3.6% in 1991), whereas 62.5% had an Na/K ratio ≥2.0 (down from 88.1% in 1991) (Figure 1C; also see Supplemental Table S3 under “Supplemental data” in the online issue).
It is important to note that whereas mean sodium intake decreased, potassium intake increased and the Na/K ratio decreased over the time period studied; approximately one-third to one-half of the sample moved in the opposite direction between each survey year. The distribution of those with increasing and decreasing sodium and potassium intakes and Na/K ratio between survey years is provided elsewhere (see Supplemental Table S4 under “Supplemental data” in the online issue).
Sources of dietary sodium and potassium
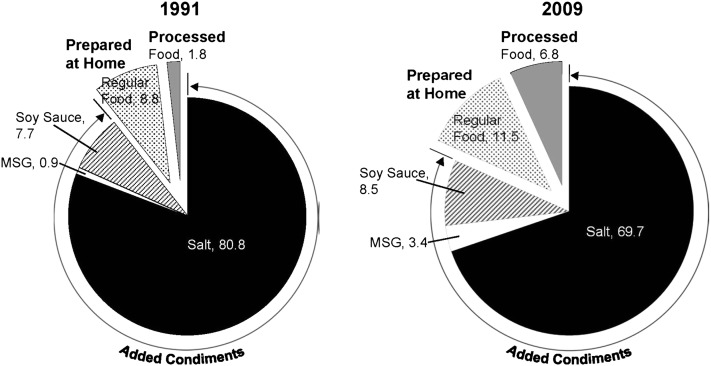
The major source of dietary sodium was added salt, followed by soy sauce, processed foods, and MSG. In 2009, the average salt intake was 8.3 g/d, accounting for 69.7% of total sodium intake. The average soy sauce intake was 6.9 g/d, accounting for 8.5% of total sodium intake. The average processed food intake was 244.7 g/d, which represented 20.8% of all food consumed and accounted for 6.8% of total sodium intake. The average MSG intake was 1.5 g/d, accounting for 3.4% of total sodium intake (Figure 2; also see Supplemental Table S5 under “Supplemental data” in the online issue).
FIGURE 2.
Sources of dietary sodium intake in China, 1991–2009. Dietary sodium intake was primarily from salt added during cooking. Sodium from processed food consumption was still low but was increasing rapidly. MSG, monosodium glutamate.
We examined over time the sociodemographic correlates of key food sources of sodium, and salt consumption was much higher in central China (see Supplemental Table S6 under “Supplemental data” in the online issue). We also examined the 10 major foods that were sources of potassium and found little change in major food sources. However, we found that the proportion of potassium provided by the 10 major foods decreased significantly from 57.7% in 1991 to 43.5% in 2009 (see Supplemental Table S7 under “Supplemental data” in the online issue), which indicated that the current diet is more diversified than the diet of 20 y ago.
Dynamics of dietary sodium and potassium trends
Between 1991 and 2009, sodium intake in the Chinese population in our study decreased. Sodium intake from added salt decreased from 5.3 g/d in 1991 to 3.3 g/d in 2009, and the proportion of sodium intake from added salt decreased from 80.8% to 69.7% during the same time period. Processed foods were not a major source of dietary sodium in 1991, representing <0.1 g Na/d (1.8% of sodium intake), which tripled to 0.3 g/d (or 6.8%) in 2009. Sodium from MSG was still low in 2009, but the rapid increase from 0.9% to 3.4% of sodium intake should not be overlooked (Figure 2).
During the same time period, potassium intake increased slightly from 1.5 g/d in 1991 to 1.8 g/d in 1997 and remained at the same level thereafter (Table 2). Using results of multinomial logistic regressions (see Supplemental Tables S8–S10 under “Supplemental data” in the online issue), we provided adjusted differential sodium and potassium intakes and the Na/K ratio by region while controlling for age, sex, education, income, urban or rural area, and survey years. Residents of the central region of China were significantly more likely to consume higher amounts of sodium (≥6.0 g/d) and to have a higher Na/K ratio (2.0), but their consumption of potassium was also slightly higher (≥3.0 g/d) (see Supplemental Figure S1 under “Supplemental data” in the online issue).
Prevalence of hypertension
SBP increased by 8.6 mm Hg, from 112.2 mm Hg in 1991 to 120.8 mm Hg in 2009. DBP increased by 6.3 mm Hg, from 73.5 mm Hg in 1991 to 79.8 mm Hg in 2009 (Table 1). The prevalence of hypertension more than doubled from 10.4% of the study population in 1991 to 22.7% in 2009 (16.7% when adjusted to the 1991 study population). Hypertension prevalence was lower in rural areas in 1991 but increased much more rapidly in rural than in urban areas to reach comparable levels by 2009. Similarly, northern residents had a much higher prevalence in 1991 and have had increases since. The most rapid changes have occurred in central China (Table 3). In 2009 among the proportion of the study population we diagnosed as being hypertensive, 7.5% had been diagnosed and 5.4% were being treated with medication.
TABLE 3.
Prevalence of hypertension in China, 1991–2009
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | |
| Unadjusted prevalence (%) | 10.4 | 11.5 | 15.2 | 16.2 | 18.1 | 17.6 | 22.7 |
| Adjusted prevalence (%)1 | 10.4 | 10.9 | 13.6 | 13.8 | 13.8 | 12.8 | 16.6 |
| Diagnosed hypertension (%)2 | 2.4 | 2.3 | 2.4 | 3.9 | 5.2 | 5.8 | 7.5 |
| Treated hypertension (%)3 | 1.3 | 1.1 | 1.4 | 2.4 | 3.6 | 4.1 | 5.4 |
| Age group (%) | |||||||
| 20–29 y | 3.2 | 4.3 | 6.8 | 5.4 | 4.9 | 3.7 | 5.9 |
| 30–39 y | 6.8 | 7.6 | 9.0 | 9.8 | 9.9 | 9.3 | 11.9 |
| 40–49 y | 12.4 | 13.8 | 17.7 | 17.9 | 18.8 | 17.6 | 23.4 |
| 50–60 y | 26.5 | 25.8 | 30.0 | 31.0 | 30.5 | 28.2 | 35.4 |
| Sex (%) | |||||||
| Men | 12.0 | 13.4 | 17.9 | 18.5 | 21.8 | 20.9 | 26.5 |
| Women | 9.0 | 9.9 | 12.7 | 14.1 | 14.9 | 14.7 | 19.2 |
| Education (%) | |||||||
| <High school | 10.6 | 12.0 | 15.9 | 16.5 | 18.6 | 18.8 | 24.3 |
| ≥High school | 9.0 | 9.3 | 12.7 | 15.3 | 16.8 | 14.8 | 18.6 |
| Income (%) | |||||||
| Low | 8.7 | 10.4 | 16.1 | 15.2 | 17.6 | 17.3 | 24.5 |
| Middle | 10.4 | 11.8 | 13.4 | 16.4 | 18.4 | 18.3 | 22.9 |
| High | 12.0 | 12.4 | 16.1 | 17.0 | 18.6 | 17.3 | 20.7 |
| Rural/urban (%) | |||||||
| Rural | 8.6 | 10.0 | 14.4 | 15.7 | 18.0 | 17.2 | 22.5 |
| Urban | 14.0 | 15.4 | 17.2 | 17.3 | 18.5 | 18.6 | 23.1 |
| Region (%) | |||||||
| North | 20.0 | 19.3 | 22.4 | 19.0 | 24.6 | 20.4 | 29.5 |
| Central | 10.7 | 12.3 | 18.2 | 19.1 | 19.8 | 20.2 | 24.9 |
| South | 7.8 | 9.2 | 10.9 | 12.3 | 13.5 | 14.4 | 17.4 |
Adjusted to the 1991 population.
Self-reported prevalence of hypertension diagnosed by physicians.
Percentage of patients with hypertension who were using antihypertension medications.
Sodium intake, potassium intake, Na/K ratio, and incident hypertension
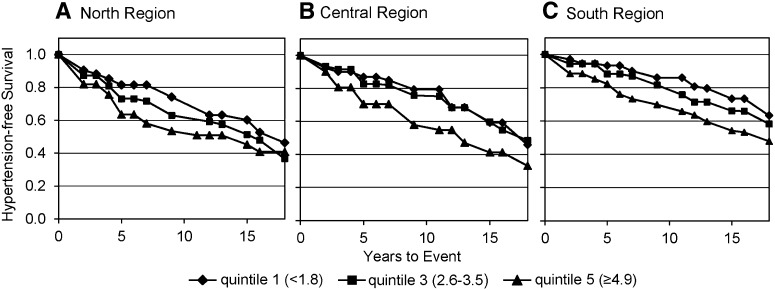
Of the 3 sodium and potassium intake measurements, the most recent lagged intakes had higher and more significant HRs. Compared with the lowest group, recent intakes of sodium had strong dose-response associations with incident hypertension for the third to fifth quintiles. The second to fifth quintiles of potassium intake had a significantly lower HR adjusted for baseline covariates. The results show no evidence of a regional interaction with sodium or potassium intake. In contrast, we found that region had a significant interaction with the effect of the Na/K ratio on the risk of hypertension, with significant effects in both the overall sample and in each region. In the central and southern regions, the HR for the fourth and fifth quintiles of Na/K ratio were significantly different from the first quintile, and in all regions the fifth quintile was significantly different from the first quintile (Figure 3); a higher risk was found in the southern region (Table 4).
FIGURE 3.
Hypertension-free survival probability by quintiles of Na/K ratio in the north (A), central (B), and south (C) regions in China, 1991–2009. Survival probabilities were adjusted by sodium intake, energy intake, age, sex, education, income, region, BMI, physical activity, smoking status, and alcohol consumption. The macro %EMICM in SAS 9.2 (SAS Institute) was used to compute the survival curves. Region had a significant interaction with the effect of the Na/K ratio on the risk of hypertension, with significant effects in both the overall sample and each region. In the third through the fifth quintiles of the Na/K ratio, there was a significantly higher HR for hypertension than for the lowest ratio quintile (P < 0.001 by flexible parametric models). Na/K ratio, the ratio of sodium to potassium.
TABLE 4.
HRs for incident hypertension by quintiles of sodium intake, potassium intake, and Na/K ratio1
| Quintiles of intake |
|||||
| Lowest | Second | Third | Fourth | Highest | |
| Sodium intake | |||||
| Range (g/d) | <3.2 | 3.2–4.3 | 4.4–5.52 | 5.6–7.52 | ≥7.62 |
| HR (95% CI)3 | 1.00 | 0.99 (0.84, 1.18) | 1.20 (1.01, 1.42)2 | 1.37 (1.16, 1.62)2 | 1.84 (1.56, 2.16)2 |
| Potassium intake | |||||
| Range (g/d) | <1.2 | 1.2–1.4 | 1.5–1.7 | 1.8–2.12 | ≥ 2.22 |
| HR (95% CI)3 | 1.00 | 0.83 (0.71, 0.97)2 | 0.94 (0.80, 1.10) | 0.74 (0.63, 0.87)2 | 0.66 (0.56, 0.78)2 |
| Na/K ratio | |||||
| Range | <1.8 | 1.8–2.5 | 2.6–3.4 | 3.5–4.8 | ≥4.9 |
| Average [HR (95% CI)] | 1.00 | 1.12 (0.93, 1.35) | 1.27 (1.06, 1.53)2 | 1.64 (1.37, 1.97)2 | 2.14 (1.79, 2.55)2 |
| North [HR (95% CI)]4 | 1.00 | 1.27 (0.88, 1.85) | 1.74 (1.17, 2.58)2 | 1.31 (0.89, 1.93) | 2.08 (1.40, 3.08)2 |
| Central [HR (95% CI)]4 | 1.00 | 1.18 (0.85, 1.63) | 1.05 (0.76, 1.46) | 1.59 (1.16, 2.17)2 | 1.90 (1.41, 2.56)2 |
| South [HR (95% CI)]4 | 1.00 | 1.00 (0.75, 1.32) | 1.28 (0.97, 1.69) | 1.82 (1.39, 2.40)2 | 2.37 (1.81, 3.12)2 |
HRs were adjusted for energy intake, age, sex, education, income, region, BMI, physical activity, smoking status, and alcohol consumption. Flexible parametric models for survival-time data and the macro %EMICM in SAS 9.2 (SAS Institute) were used to compute HRs and the survival curves. Na/K ratio, ratio of sodium to potassium.
Significant result.
HRs were additionally adjusted for sodium intake.
Estimates are linear combinations of coefficients from a model including Na/K ratio quintiles by region interaction terms, likelihood ratio test (model with compared with without the interaction term, P = 0.08).
DISCUSSION
Overall, among Chinese adults, the prevalence of hypertension—particularly untreated hypertension—is high. Unlike the trends in the United States, where sodium intake was stable between 1957 and 2003 (43), sodium intake decreased from 6.6 to 4.7 g/d in China between 1991 and 2009 (P-trend < 0.01) among adults aged 20–60 y as a result of the rapid nutrition transition in recent decades. Nevertheless, it remains high. Potassium intake increased slightly from 1.5 to 1.8 g/d (P-trend < 0.01) between 1991 and 2009, and the Na/K ratio declined from 4.9 to 2.8 (P-trend < 0.01). The key current sources of sodium are condiments, but the contribution of processed foods is expected to increase greatly in the future. Potassium sources, in contrast, are remarkably varied. A high sodium intake, a low potassium intake, and a high Na/K ratio all have significant effects on incident hypertension.
Sodium intakes in China remain double those recommended by the IOM and the WHO (15, 41, 44, 45). In our sample population, 62.5% consumed ≥6.0 g/d of added salt, and 92.7% consumed ≥2.0 g Na/d; the highest intake was in the central Chinese provinces. Added salt remains the major source of sodium intake, and sodium from processed foods remains low. This situation is similar to that in South Korea, where added condiments are the major sources of sodium in the diet (46).
Several small studies established the current thinking about sodium intake in China, namely, that sodium intake is a major problem in North China. The INTERSALT 3-neighborhood study (the CHNS has 228 neighborhoods) found that 24-h urinary sodium excretion was between 3.9 and 5.6 g/d (27). The INTERMAP 3-county rural follow-up study found an intake of 3.2 to 6.3 g/d (47), with an average of 3.6 g/d in the North and 2.5 g/d in the South (28). These 2 studies were conducted over 30 and 20 y ago, respectively, and did not include samples from central China. With a much larger and more representative sample, our results show that sodium intake was higher in the central and southern parts of China than in the northern areas (except in our baseline year, 1991). Our sources of sodium differed from those in other studies, because we measured both sodium in added salt and other condiments and sodium in processed foods. Thus, we found a lower proportion of sodium from added salt (69.7% in 2009) than in other studies (48). Furthermore, we used 3 d of measurement.
Ours was the first study to include a large number of communities across all regions of China. The larger more diverse sample shows that the highest sodium intake occurred in central China, most likely related to the 2 popular cuisines in this area: Huaiyang and Lu. Both cuisines use salt and large amounts of soy sauce during cooking and preparation to make the dishes colorful and to enhance overall taste and presentation. This region also has reported high levels of stomach cancer related to high consumption of fermented products and salty preserved fish (49). There are possible reasons other than the scope and size of this study that are responsible for differences with earlier research. The Chinese food environment is rapidly changing. In the past, fresh vegetables and meats were rarely available in the North, particularly in the winter. Thus, many salty and pickled foods were consumed for a great portion of the year. Marked advancements in the transportation of food have occurred; therefore, pickled food consumption in the North has declined significantly (50). As a result, added salt intake has decreased faster in the North than in the South.
Another important development is the decline in sodium intake and the slow shift toward increased intake of processed foods among all sociodemographic subpopulations. Sodium intake from processed foods and MSG, which are more expensive than salt, is increasing rapidly. Furthermore, the major food preservative was salt when food supplies in China were limited. Modernization has reduced the need for food preservation in traditional ways (50, 51). Refrigerator ownership has increased from 16.6% in 1991 to 63.7% in 2009. Concomitant shifts in diet have been linked with rapid modernization and urbanization in China (52). In the past 15 y, the Chinese government, under the leadership of the Chinese Nutrition Society and the National Institute of Nutrition and Food Safety, has launched national campaigns and studies focusing on salt reduction along with more localized actions. In some areas the government distributed a small spoon to each household for salt measurement to encourage restricting the amount of salt added during cooking and food preparation (53). Evaluations of the effects of these efforts are not reported.
To the best of our knowledge, this was the first study on potassium intake and the Na/K ratio and hypertension in China. During our study period, potassium intake increased slightly. Similarly, the proportion of participants achieving the potassium intake levels recommended by the Chinese Nutrition Society increased from 40% in 1991 to 60% in 2009, but few met the level recommended by the IOM (41). On average, potassium intake in China was much lower than the adequate intake level recommended by the IOM (4.7 g/d for all adults) (45) or by the WHO (2.7–3.1 g/d) (44) but was within the range recommended by China (1.6–2.0 g/d for all adults) (54). We showed that an increased potassium intake among the lowest 40% of consumers or a reduced Na/K ratio among 60% would reduce incident hypertension, which indicates a need for increased potassium intake. This suggests that Chinese authorities should reconsider their potassium dietary guidelines.
Some of the research does not corroborates our results, ie, that increased potassium intake reduces the risk of hypertension. Our study found that potassium intake was negatively associated with incident hypertension. Compared with the lowest quintile (intake <1.2 g/d), incident hypertension decreased by 26% in the fourth quintile (intake: 1.8–2.2 g/d: HR: 0.74; 95% CI: 0.63, 0.87) and by 34% in the highest quintile (intake: ≥2.2 g/d: HR: 0.66; 95% CI: 0.56, 0.78). A recent meta-analysis reported that an increased potassium intake had no statistically significant effect on blood pressure (55), and other meta-analyses reported that an increased potassium intake lowered blood pressure in both patients with or without hypertension (56–58). A study sponsored by the WHO shows an added complexity of potassium. That study found that potassium intake negatively associated with both SBP and DBP in Tibetan subjects but was positively associated with SBP and DBP in Han subjects—the majority ethnicity in China (59). The WHO study focused on older people aged 48–56 y with a small sample from 4 communities (n = 800), which may account for the discrepancies between those results and ours.
Sodium intake has declined, whereas rates of hypertension have steadily increased across the country. Although sodium intake is decreasing, the average intake is still as high as 4.7 g/d and affects the risk of hypertension, particularly the most recent lagged measure of sodium intake (60). In addition, although we found that sodium intake is declining, the large increases in many other risk factors more than offset these small sodium reductions (61, 62). In particular, increases in weight and BMI have significantly affected hypertension rates in China (63–66). Our results echo those of earlier studies in China (27, 67).
We found that the Na/K ratio has a stronger association with incident hypertension than does sodium or potassium intake solely; this result is consistent with that of previous studies. Furthermore, the interaction between region of residence and Na/K ratio is significant. A study that used 2 cross-sectional population surveys (n = 2068) in one large city in China reported that potassium intake did not increase the risk of hypertension among men and women, whereas the Na/K ratio increased the risk by 10% among men and by ∼20% among women (68). Our data show that the risk of incident hypertension more than doubled in the highest quintile of the Na/K ratio (≥4.9) compared with the lowest quintile (ratio <1.8) (HR: 2.14; 95% CI: 1.79, 2.55), whereas potassium intake solely in the highest quintile decreased the risk by 34%, as mentioned above. The extent of the association between the Na/K ratio and incident hypertension differs by region, with a slightly weaker but significant HR in the central region. We found that sodium intake is higher in central China and that the prevalence of hypertension has increased more in this region. This may be because blood pressure reduction from potassium intake depends on concurrent levels of sodium intake and vice versa. Potassium intake lowers blood pressure to a larger extent when sodium intake is high (69).
This study had several limitations. Past studies might have overestimated salt intake, whereas we might underestimate it. During periods of heavy salting and preservation, the excessive salt solution that was discarded was not measured. In contrast, eating away from home is rapidly increasing (1, 43, 44), as is the consumption of packaged, processed foods (70, 71). As in all other countries, national FCTs and dietary intake surveys do not accurately capture the varying sodium content of these foods (72). Another limitation was the lack of urine collection and analysis of 24-h urinary sodium excretion—the preferred method of obtaining sodium intake data in a population survey (73).
Sodium intake in China was twice the international recommended intake and varied by geographic region, with the highest intake occurring in central China among older populations and among men. Potassium intake was low. Few adults in our study reached the level recommended by the IOM. Potassium intake did not vary by geographic region, income, sex, or age group in China. The Na/K ratio was 3 times higher than the level recommended by the WHO or 6 times higher than that recommended by the IOM, although it decreased during our study period. Sodium intake from processed foods and restaurant foods, although underestimated, is increasing rapidly. We also noted important targeting issues. Rural populations still rely on added salt, so sodium replacement and salt substitution might be feasible and have been found to be acceptable. Similarly, the dynamics of the Chinese economy and food environment suggest that programs and policies to address processed and away-from-home foods will be needed (70). The prevalence of hypertension is high among the Chinese population, and cardiovascular disease is a major burden to social, economic, and health resources, particularly in rural areas, where the burden is great. Reducing sodium intake is a public health priority. Replacing sodium in salt with potassium is an option with the potential to improve the health and quality of life of the Chinese population. The results of this study have spearheaded the development of a salt reduction campaign in Shandong, one of the central provinces, sponsored by the Chinese Center for Disease Control and Prevention and the US CDC.
Supplementary Material
Acknowledgments
We thank Frances Dancy, Carolina Population Center, for her helpful administrative assistance; Jim Terry and Dan Blanchette for programming and technical support; and Tom Swasey for graphic support.
The authors’ responsibilities were as follows—SD and BMP: designed and conducted the research, wrote the manuscript, and had primary responsibility for the final content of the manuscript; SD and CB: performed the data analysis; SD and BZ: conducted the validation study of the sodium and potassium intake measurement; AN, HW, BZ, and JZ: critically revised the manuscript; and HW, BZ, and JZ: conducted the research in the field. The authors declared that they had no conflicts of interest.
Footnotes
Abbreviations used: CHNS, China Health and Nutrition Survey; DBP, diastolic blood pressure; FCT, food-composition table; IOM, Institute of Medicine; MSG, monosodium glutamate; Na/K ratio, ratio of sodium to potassium; SBP, systolic blood pressure.
REFERENCES
- 1.Yan S, Li J, Li S, Zhang B, Du S, Gordon-Larsen P, Adair L, Popkin B. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev 2012;13:810–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, Wang J, Chen CS, Chen J, Wildman RP, Klag MJ, Whelton PK. Major causes of death among men and women in China. N Engl J Med 2005;353:1124–34. [DOI] [PubMed] [Google Scholar]
- 3.WHO. WHO Forum on Reducing Salt Intake in Populations Report of a WHO forum and technical meeting, 5–7 October 2006, Paris, France. Geneva, Switzerland: World Health Organization, 2007.
- 4.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6:e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Midgley JP, Matthew AG, Greenwood CM, Logan AG. Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomized controlled trials. JAMA 1996;275:1590–7. [DOI] [PubMed] [Google Scholar]
- 6.Rodgers A, Ezzati M, Vander Hoorn S, Lopez AD, Lin RB, Murray CJ. Distribution of major health risks: findings from the Global Burden of Disease study. PLoS Med 2004;1:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elliott P, Walker LL, Little MP, Blair-West JR, Shade RE, Lee DR, Rouquet P, Leroy E, Jeunemaitre X, Ardaillou R, et al. Change in salt intake affects blood pressure of chimpanzees: implications for human populations. Circulation 2007;116:1563–8. [DOI] [PubMed] [Google Scholar]
- 8.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ, Comparative Risk Assessment Collaborating G. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347–60. [DOI] [PubMed] [Google Scholar]
- 9.Palar K, Sturm R. Potential societal savings from reduced sodium consumption in the U.S. adult population. Am J Health Promot 2009;24:49–57. [DOI] [PubMed] [Google Scholar]
- 10.Smith-Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med 2010;152:481-7, W170-3. [DOI] [PubMed] [Google Scholar]
- 11.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 2007;370:2044–53. [DOI] [PubMed] [Google Scholar]
- 12.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens 2012;25:1–15.. [DOI] [PubMed] [Google Scholar]
- 13.O'Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, Sleight P, Sharma AM, Dans A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA 2011;306:2229–38. [DOI] [PubMed] [Google Scholar]
- 14.McCarron DA. Dietary sodium and cardiovascular and renal disease risk factors: dark horse or phantom entry? Nephrol Dial Transplant 2008;23:2133–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strom BL, Yaktine AL, Oria M. eds. Sodium intake in populations: assessment of evidence. Washington, DC: The National Academies Press, 2013. [PubMed] [Google Scholar]
- 16.Appel LJ, Whelton PK. Flawed evidence should not derail sound policy: the case remains strong for population-wide sodium reduction. Am J Hypertens 2013;26:1183–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clapp JE, Curtis CJ, Kansagra SM, Farley TA. Getting the message right: reducing sodium intake saves lives. Am J Hypertens 2013;26:1181–2. [DOI] [PubMed] [Google Scholar]
- 18.Gunn JP, Barron JL, Bowman BA, Merritt RK, Cogswell ME, Angell SY, Bauer UE, Frieden TR. Sodium reduction is a public health priority: reflections on the Institute of Medicine's Report, Sodium Intake in Populations: Assessment of Evidence. Am J Hypertens 2013;26:1178–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heaney RP. Sodium: How and how not to set a nutrient intake recommendation. Am J Hypertens 2013;26:1194–7. [DOI] [PubMed] [Google Scholar]
- 20.Kotchen TA. The salt discourse in 2013. Am J Hypertens 2013;26:1177. [DOI] [PubMed] [Google Scholar]
- 21.McCarron DA. Physiology, not policy, drives sodium intake. Am J Hypertens 2013;26:1191–3. [DOI] [PubMed] [Google Scholar]
- 22.Mente A, O'Donnell MJ, Yusuf S. Extreme sodium reductions for the entire population: zealotry or evidence based? Am J Hypertens 2013;26:1187–90. [DOI] [PubMed] [Google Scholar]
- 23.Addison WL. The use of sodium chloride, potassium chloride, sodium bromide, and potassium bromide in cases of arterial hypertension which are amenable to potassium chloride. Can Med Assoc J 1928;18:281–5. [PMC free article] [PubMed] [Google Scholar]
- 24.van Mierlo LA, Greyling A, Zock PL, Kok FJ, Geleijnse JM. Suboptimal potassium intake and potential impact on population blood pressure. Arch Intern Med 2010;170:1501–2. [DOI] [PubMed] [Google Scholar]
- 25.Zhou X, Liu JX, Shi R, Yang N, Song DL, Pang W, Li YM. Compound ion salt, a novel low-sodium salt substitute: from animal study to community-based population trial. Am J Hypertens 2009;22:934–42. [DOI] [PubMed] [Google Scholar]
- 26.Mu J, Liu Z, Liu F, Xu X, Liang Y, Zhu D. Family-based randomized trial to detect effects on blood pressure of a salt substitute containing potassium and calcium in hypertensive adolescents. Am J Hypertens 2009;22:943–7. [DOI] [PubMed] [Google Scholar]
- 27.Stamler R, Liu LS, Nichols R, Huang DX, Long ZP, Xie JX, Elliott P. Blood pressure and life style in the People's Republic of China: three samples in the INTERSALT Study. J Hum Hypertens 1993;7:429–35. [PubMed] [Google Scholar]
- 28.Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, Ueshima H, Kesteloot H, Miura K, Curb JD, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc 2010;110:736–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol 2010;39:1435–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhai F, Guo X, Popkin BM, Ma L, Wang Q, Yu W, Jin S, Ge K. Evaluation of the 24-hour individual recall method in China. Food Nutr Bull 1996;17:154–61. [Google Scholar]
- 31.Du S, Mroz TA, Zhai F, Popkin BM. Rapid income growth adversely affects diet quality in China–particularly for the poor! Soc Sci Med 2004;59:1505–15. [DOI] [PubMed] [Google Scholar]
- 32.Popkin BM, Lu B, Zhai F. Understanding the nutrition transition: measuring rapid dietary changes in transitional countries. Public Health Nutr 2002;5:947–53. [DOI] [PubMed] [Google Scholar]
- 33.Yang Y, Wang G, Pan X. China food composition 2002. Beijing, China: Peking University Medical Press, 2002. [Google Scholar]
- 34.He K, Du S, Xun P, Sharma S, Wang H, Zhai F, Popkin B. Consumption of monosodium glutamate in relation to incidence of overweight in Chinese adults: China Health and Nutrition Survey (CHNS). Am J Clin Nutr 2011;93:1328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao M, Lichtenstein AH, Roberts SB, Ma G, Gao S, Tucker KL, McCrory MA. Relative influence of diet and physical activity on cardiovascular risk factors in urban Chinese adults. Int J Obes Relat Metab Disord 2003;27:920–32. [DOI] [PubMed] [Google Scholar]
- 36.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:e21–181. [DOI] [PubMed] [Google Scholar]
- 37.Greene WH. 7th ed. New York, NY: Prentice Hall, 2011. [Google Scholar]
- 38.Kmenta J. Gilbert, Roy F. Small sample properties of alternative estimators of seemingly unrelated regressions. J Am Stat Assoc 1968;63:1180–200. [Google Scholar]
- 39.Hausman JaM. D. Specification tests for the multinomial logit model. Econometrica 1984;52:1219–40. [Google Scholar]
- 40.Jones A, O'Donnell OA. Econometric analysis of health data. New York, NY: Wiley, 2002.
- 41.Institute of Medicine, Food and Nutrition Board. Strategies to reduce sodium intake in the United States. Washington, DC: National Academy Press, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Royston P. Flexible parametric alternatives to the Cox model, and more. Stata J 2001;1:1–28. [Google Scholar]
- 43.Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957-2003: a systematic review. Am J Clin Nutr 2010;92:1172–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.WHO/FAO. Diet, nutrition and the prevention of chronic diseases. Report of a joint WHO/FAO expert consultation. World Health Organ Tech Rep Ser 2003;916. [PubMed]
- 45.Institute of Medicine. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: The National Academies Press, 2005. [Google Scholar]
- 46.Lee HS, Duffey KJ, Popkin BM. Sodium and potassium intake patterns and trends in South Korea. J Hum Hypertens 2013;27:298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao L, Stamler J, Yan LL, Zhou B, Wu Y, Liu K, Daviglus ML, Dennis BH, Elliott P, Ueshima H, et al. Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension 2004;43:1332–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang JG, Zhang B, Wang ZH, Wang HJ, Zhai FY. [The status of dietary sodium intake of Chinese population in nine provinces (autonomous region) from 1991 to 2006.] Zhonghua Yu Fang Yi Xue Za Zhi 2011;45:310–2 (in Chinese). [PubMed] [Google Scholar]
- 49.WCRF/AICR. Policy and action for cancer prevention: food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: World Cancer Research Fund/American Institute for Cancer Research, 2009. [Google Scholar]
- 50.Hu D, Reardon T, Rozelle S, Timmer P, Wang H. The emergence of supermarkets with Chinese characteristics: challenges and opportunities for China's agricultural development. Dev Policy Rev 2004;22:557–86. [Google Scholar]
- 51.Reardon T, Timmer C, Barrett C, Berdegue J. The rise of supermarkets in Africa, Asia, and Latin America. Am J Agric Econ 2003;85:1140–6. [Google Scholar]
- 52.Du S, Lu B, Zhai F, Popkin BM. A new stage of the nutrition transition in China. Public Health Nutr 2002;5:169–74. [DOI] [PubMed] [Google Scholar]
- 53.World Action on Salt & Health. China: salt action summary. Available from: http://www.worldactiononsalt.com/worldaction/asia/53714.html (cited 27 June 2013).
- 54.Chinese Nutrition Society. Chinese DRIs. Beijing, China: China Light Industry Press, 2000. [Google Scholar]
- 55.Dickinson HO, Nicolson DJ, Campbell F, Beyer FR, Mason J. Potassium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 2006;CD004641.. [DOI] [PubMed] [Google Scholar]
- 56.Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, Klag MJ. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA 1997;277:1624–32. [DOI] [PubMed] [Google Scholar]
- 57.D'Elia L, Barba G, Cappuccio FP, Strazzullo P. Potassium intake, stroke, and cardiovascular disease a meta-analysis of prospective studies. J Am Coll Cardiol 2011;57:1210–9. [DOI] [PubMed] [Google Scholar]
- 58.Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013;346:f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu L, Ding Y, Huang Z, He B, Sun S, Zhao G, Zhang H, Miki T, Mizushima S, Ikeda K, et al. Ethnic and environmental differences in various markers of dietary intake and blood pressure among Chinese Han and three other minority peoples of China: results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) Study. Hypertens Res 2001;24:315–22. [DOI] [PubMed] [Google Scholar]
- 60.Batis C, Gordon-Larsen P, Cole SR, Du S, Zhang B, Popkin B. Sodium intake from various time frames and incident hypertension among Chinese adults. Epidemiology 2013;24:410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bell AC, Adair LS, Popkin BM. Understanding the role of mediating risk factors and proxy effects in the association between socio-economic status and untreated hypertension. Soc Sci Med 2004;59:275–83. [DOI] [PubMed] [Google Scholar]
- 62.Dearth-Wesley T, Wang H, Popkin BM. Under- and overnutrition dynamics in Chinese children and adults (1991-2004). Eur J Clin Nutr 2008;62:1302–7. [DOI] [PubMed] [Google Scholar]
- 63.Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, Koplan JP. Emergence of chronic non-communicable diseases in China. Lancet 2008;372:1697–705. [DOI] [PubMed] [Google Scholar]
- 64.Nguyen TT, Adair LS, He K, Popkin BM. Optimal cutoff values for overweight: using body mass index to predict incidence of hypertension in 18- to 65-year-old Chinese adults. J Nutr 2008;138:1377–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Colin Bell A, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol 2002;155:346–53. [DOI] [PubMed] [Google Scholar]
- 66.Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr 2010;13:639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, Woodward M, Li X, Chalmers J, Gao R, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679–86. [DOI] [PubMed] [Google Scholar]
- 68.Hu G, Tian H. A comparison of dietary and non-dietary factors of hypertension and normal blood pressure in a Chinese population. J Hum Hypertens 2001;15:487–93. [DOI] [PubMed] [Google Scholar]
- 69.Appel LJ, American Society of Hypertension Writing Group, Giles TD, Black HR, Izzo JL Jr, Materson BJ, Oparil S, Weber MA. ASH position paper: dietary approaches to lower blood pressure. J Clin Hypertens (Greenwich) 2009;11:358–68. [DOI] [PMC free article] [PubMed]
- 70.Zhai F, Du S, Wang Z, Zhang J, Du W, Popkin BM. Dynamics of the Chinese diet and the role of urbanization, 1991–2011. Obes Rev 2014;15(suppl 1):16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reardon T, Timmer CP, Minten B. Supermarket revolution in Asia and emerging development strategies to include small farmers. Proc Natl Acad Sci USA 2012;109:12332–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Slining MM, Ng SW, Popkin B. An approach for evaluating food companies’ calorie-reduction pledge to improve the U.S. diet. Am J Prev Med 2013;44:174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol 2009;38:791–813. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.