Abstract
Low levels of 25-hydroxyvitamin D have been documented among inhabitants of the wider Middle East and North African countries. Sunlight has long been recognized as a major provider of vitamin D. In this study we aimed to determine the optimum time for sun exposure in the Central region of Riyadh, Saudi Arabia. Ampoules containing 7-dehydrocholesterol in ethanol were exposed to sunlight every hour starting from sunrise until sunset in July and December. Our results demonstrated that the time of the day has a major influence in vitamin D production. In this study, summer production of previtamin D3 was observed to occur between 8:00 PM to 4:00 PM with peak hours between 10:00 AM to 12:00 PM. During wintertime however, the conversion began later at around 9:30 AM and ended sooner at 2:00 PM, with peak hours at 10:00 AM to 12 noon. In conclusion, the optimum time to get sun exposure for vitamin D3 production in Riyadh, during summer is from 9:00 AM and before 10:30 AM, as well as after 2:00 PM until 3:00 PM, while during winter it’s from 10:00 AM until 2:00 PM. These times are important on a public health perspective, as it’s free, relatively safe and the most enjoyable. This strategy is a highly efficacious way for improving the vitamin D status for children and adults and preventing vitamin D deficiency.
Keywords: Vitamin D; sun; exposure; time; Riyadh, Saudi
Introduction
There is growing evidence that vitamin D sufficiency is required for optimal health. The role of vitamin D in both calcium absorption and metabolism for bone health is well known.1 Furthermore, the presence of vitamin D receptors (VDR) in other tissues and organs suggest that vitamin D function extends beyond bone homeostasis.1 Additionally, the enzyme responsible for conversion of 25-hydroxyvitamin D [25(OH)D] to its biologically active form 1,25-dihydroxyvitamin D [1,25(OH)2D] has been identified in other tissues aside from the kidneys.2,3 Research during the past two decades has illustrated the importance of vitamin D in reducing the risk of cancer,4-6 multiple sclerosis7,8 and type 1 diabetes mellitus.9
Globally, vitamin D deficiency has been noted in many countries. A high number of otherwise apparently healthy children, adolescents, pregnant women, and adults are vitamin D deficient.10-15 Even in sunny areas like Saudi Arabia, vitamin D deficiency is very prevalent.15-17 The major source of vitamin D for most humans is causal sun exposure and to a lesser extent from dietary intake. Even so, the natural diets that most humans consume contain little vitamin D, with exception of wild-caught, oily fish, cod liver oil and sun exposed mushroom.18
When human skin is exposed to sunlight, the solar UVB (290 to 315 nm) photons penetrate into the epidermis and are absorbed by 7-dehydrocholesterol, which is present in the plasma membrane.19-22The absorption of these energies transform 7-dehydrocholesterol into previtamin D3. Because this photochemical process occurs in the plasma membrane, only the cis-cis conformer of previtamin D3 is formed, which, being thermodynamically unstable, is rapidly isomerized to vitamin D3.23 Once formed, vitamin D3 is ejected out of the plasma membrane into the extracellular space where it is drawn into the dermal capillary bed by the vitamin D–binding protein.24 Excessive exposure to sunlight will not cause vitamin D intoxication because sunlight degrades any excess previtamin D3 and vitamin D3.29
Factors that affect cutaneous production of vitamin D3 include latitude, season, time of day, air pollution, cloud cover, melanin content of the skin, use of sunblock, age and the extent of clothing covering the body.20 When the sun is low on the horizon, the atmospheric ozone, clouds and particulate air pollution absorb UVB radiation, limiting the amount that reach the surface of the Earth. The zenith angle of the sun plays a critical role in vitamin D3 production. When the zenith angle is more oblique, the path length through the stratospheric ozone layer is increased and hence, fewer UVB photons are able to reach the earth’s surface. Therefore, cutaneous vitamin D3 production is effectively absent early and late in the day and for the entire day during several winter months at latitudes > 35°.25-27
Results
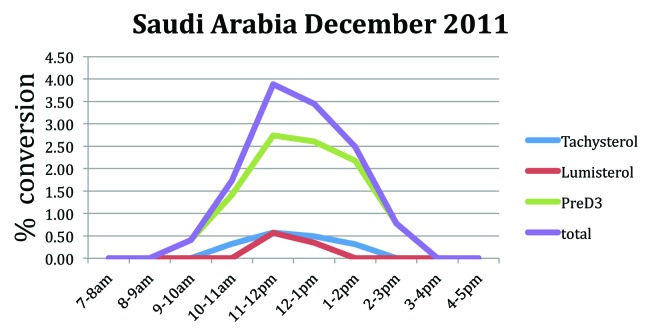
The conversion of 7-dehydrocholesterol to previtamin D3 in the ampules is the most sensitive indicator for the cutaneous production of vitamin D3 from sun exposure. Using this method we observe that although the sun was shining brightly beginning at 6:00 AM in July, no previtamin D3 production was detected before 8 AM. Previtamin D3 was detected in the ampule exposed to sunlight between 8–9:00 AM and gradually increased and was maximal between 11:00 AM and 1:00 PM. Previtamin D3 production gradually declined and no previtamin D3 was observed in ampules exposed to sunlight after 5:00 PM (Fig. 1).
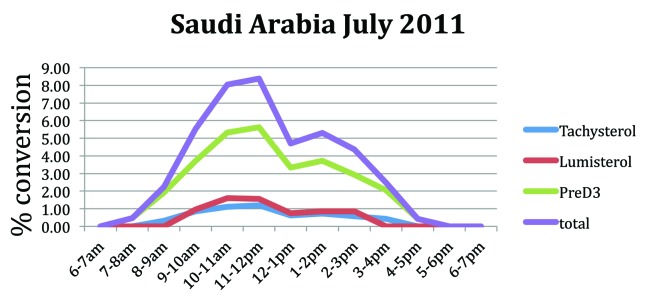
Figure 1. Conversion of 7-dehydrocholesterol (7-DHC) to previtamin D3, lumisterol and tachysterol at various times throughout the day in July on a sunny day in Saudi Arabia.
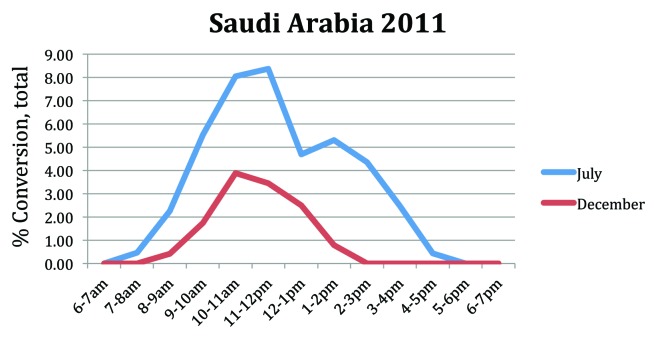
Even though it remains sunny in Saudi Arabia in December and the sun rises before 7:00 AM there was no detectable previtamin D3 production in the ampules until 9:00 AM. Previtamin D3 gradually increased and was maximally produced between the hours of 11:00 AM and 2:00 PM and rapidly declined with no further production after 3:00 PM (Fig. 2). The effect of the season was evaluated in our study that showed reduction by 50% of conversion of 7-dehydrocholesterol to previtamin D3 during winter. (Fig. 3)
Figure 2. Conversion of 7-dehydrocholesterol (7-DHC) to previtamin D3, lumisterol and tachysterol at various times throughout the day in December on a sunny day in Saudi Arabia.
Figure 3. influence of season on the synthesis of previtamin D3 and its photoproducts (% total).
Tachysterol and lumisterol were observed in ampules exposed to sunlight between 10:00 AM and 3:00 PM in July and 11:00 AM and 2:00 PM in December demonstrating that enough sunlight was available to convert previtamin D3 to these 2 photoproducts and thus beginning to establish a photoequilibrium.
Discussion
It is ironic that residents of Saudi Arabia, and the Middle East in general, suffer from vitamin D deficiency despite abundant sunlight year-round. A number of factors may affect serum vitamin D3 production in skin such as skin color, season, altitude, time of the day, and amount of sun exposure. Our results demonstrated that the time of the day has a major influence in vitamin D3 production. In this study, summer production of previtamin D3 was observed to be increased between 9:00 AM to 3:00 PM with peak hours between 10:00 AM to 12:00 PM. During wintertime however, the conversion begins later at around 9:30 AM until 2:00 PM, with peak hour around 11:00 AM. It is important to know whether that time is feasible for sun exposure without harming the skin. Maximum UVB time, believed to be responsible for both sun burning and skin cancer was previously recorded at 10:30 AM to 2:00 PM, during the summer months of Riyadh.28 Taking this into consideration, the optimum time for sun exposure therefore is from 9:00 AM and before 10:30 AM, as well as after 2:00 PM until 3:00 PM.
Similarly, Holick et al., have reported previtamin D3 production in Boston (latitude 42° N) was significant between hours of 10:00 AM and 4:00 PM during June.29 The effect of the season was evaluated in the same study that showed reduction by 80% in the conversion of 7-dehydrocholesterol to previtamin D3 at noon time between June and October.30
The production of vitamin D3 from sun exposure vs. oral supplementation has been evaluated in several studies. Data from Australian and New Zealand31 has demonstrated that whole body exposure of mid-day sun in summer for 10–15 min is comparable to taking 15 000 IU of vitamin D3 orally. Based on this, exposure of hands, face and arms (around 15% of body surface) should produce about 1000 IU of vitamin D3.29
Al-Daghri and colleagues have recently documented the counterintuitive effect of season in vitamin D levels among Saudis. Because summer season confer lesser outdoor activities secondary to extreme temperature elevations, it was suggested to increase dietary intake of food products fortified with vitamin D and encourage vitamin D supplements.30 From our study however we suggest a cost and reasonably risk-free alternative to restore vitamin D levels which is sun exposure between 9:00 AM and after 2:00 PM for 10–15 min during summer months.
Our study has a few limitations. The study was done in two seasons only. Further studies are needed to determine the effect of change in the season throughout the year on skin production of pro vitamin D3. In addition, the study was conducted in the central region (Riyadh) only, and different optimum sun exposure times might not be the same from other geographical regions in the country secondary to differences in weather and altitude. Moreover the study was done in cloudless day.
In summary, the optimum time to get sun exposure for vitamin D production in Riyadh, during summer time is from 9:00 AM and before 10:30 AM, as well as after 2:00 PM until 3:00 PM.while during winter time it’s from 10:00 AM until 2:00 PM. These timings are important on a public health perspective, as it’s free, safe and enjoyable. Furthermore it’s a highly efficacious way for management and prevention of vitamin D deficiency.
Objectives
To determine the optimum time for sun exposure and evaluate of previtamin D3 production during summer and winter in the central region of Riyadh, Saudi Arabia (latitude and altitude are 24° N, 620 min respectively).
Methods and Materials
7-dehydrocholesterol in ethanol was sealed under Argon in borosilicate ampoules, placed outside in direct sunlight on a cloudless day for 1 h intervals beginning from sunrise until sunset. The samples were stored in the dark and evaluated by high-performance liquid chromatography (HPLC) for the conversion of 7-dehydrocholesterol to previtamin D3 and its photoproducts (tachysterol and lumisterol) as previously described.21,23
Acknowledgments
The authors wishes to express sincere appreciation to The Prince Mutaib Chair for Biomarkers on Osteoporosis, Dr. Nasser Al Daghri, Lorrie Butler and Kelly Persons for their support during the performance of this study and Ahmed Alabdli for his contributions.
Disclosure of Potential Conflicts of Interest
This work was supported by small grant from the faculty of medicine, King Fahad Medical city, Riyadh, Saudi Arabia.
Footnotes
Previously published online: www.landesbioscience.com/journals/dermatoendocrinology/article/23351
References
- 1.DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80(Suppl):1689S–96S. doi: 10.1093/ajcn/80.6.1689S. [DOI] [PubMed] [Google Scholar]
- 2.Mawer EB, Hayes ME, Heys SE, Davies M, White A, Stewart MF, et al. Constitutive synthesis of 1,25-dihydroxyvitamin D3 by a human small cell lung cancer cell line. J Clin Endocrinol Metab. 1994;79:554–60. doi: 10.1210/jc.79.2.554. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz GG, Whitlatch LW, Chen TC, Lokeshwar BL, Holick MF. Human prostate cells synthesize 1,25-dihydroxyvitamin D3 from 25-hydroxyvitamin D3. Cancer Epidemiol Biomarkers Prev. 1998;7:391–5. [PubMed] [Google Scholar]
- 4.Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer? Int J Epidemiol. 1980;9:227–31. doi: 10.1093/ije/9.3.227. [DOI] [PubMed] [Google Scholar]
- 5.Garland C, Shekelle RB, Barrett-Connor E, Criqui MH, Rossof AH, Paul O. Dietary vitamin D and calcium and risk of colorectal cancer: a 19-year prospective study in men. Lancet. 1985;1:307–9. doi: 10.1016/S0140-6736(85)91082-7. [DOI] [PubMed] [Google Scholar]
- 6.Grant WB. An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer. 2002;94:1867–75. doi: 10.1002/cncr.10427. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg P, Fleming MC, Picard EH. Multiple sclerosis: decreased relapse rate through dietary supplementation with calcium, magnesium and vitamin D. Med Hypotheses. 1986;21:193–200. doi: 10.1016/0306-9877(86)90010-1. [DOI] [PubMed] [Google Scholar]
- 8.Hayes CE, Cantorna MT, DeLuca HF. Vitamin D and multiple sclerosis. Proc Soc Exp Biol Med. 1997;216:21–7. doi: 10.3181/00379727-216-44153a. [DOI] [PubMed] [Google Scholar]
- 9.Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001;358:1500–3. doi: 10.1016/S0140-6736(01)06580-1. [DOI] [PubMed] [Google Scholar]
- 10.Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercberg S, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int. 1997;7:439–43. doi: 10.1007/s001980050030. [DOI] [PubMed] [Google Scholar]
- 11.Rucker D, Allan JA, Fick GH, Hanley DA. Vitamin D insufficiency in a population of healthy western Canadians. CMAJ. 2002;166:1517–24. [PMC free article] [PubMed] [Google Scholar]
- 12.Roth DE, Martz P, Yeo R, Prosser C, Bell M, Jones AB. Are national vitamin D guidelines sufficient to maintain adequate blood levels in children? Can J Public Health. 2005;96:443–9. doi: 10.1007/BF03405185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. Prevalence of vitamin D deficiency among healthy adolescents. Arch Pediatr Adolesc Med. 2004;158:531–7. doi: 10.1001/archpedi.158.6.531. [DOI] [PubMed] [Google Scholar]
- 14.Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM. High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J Nutr. 2007;137:447–52. doi: 10.1093/jn/137.2.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bener A, Al-Ali M, Hoffmann GF. High prevalence of vitamin D deficiency in young children in a highly sunny humid country: a global health problem. Minerva Pediatr. 2009;61:15–22. [PubMed] [Google Scholar]
- 16.Ardawi MS, Sibiany AM, Bakhsh TM, Qari MH, Maimani AA. High prevalence of vitamin D deficiency among healthy Saudi Arabian men: relationship to bone mineral density, parathyroid hormone, bone turnover markers, and lifestyle factors. Osteoporos Int. 2012;23:675–86. doi: 10.1007/s00198-011-1606-1. [DOI] [PubMed] [Google Scholar]
- 17.Elsammak MY, Al-Wosaibi AA, Al-Howeish A, Alsaeed J. Vitamin d deficiency in Saudi Arabs. Horm Metab Res. 2010;42:364–8. doi: 10.1055/s-0030-1248296. [DOI] [PubMed] [Google Scholar]
- 18.Cannell JJ, Hollis BW, Zasloff M, Heaney RP. Diagnosis and treatment of vitamin D deficiency. Expert Opin Pharmacother. 2008;9:107–18. doi: 10.1517/14656566.9.1.107. [DOI] [PubMed] [Google Scholar]
- 19.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clinic proceedings. Mayo Clinic. 2006;81:353–73. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 20.Holick MF. Photosynthesis of vitamin D in the skin: effect of environmental and life-style variables. Fed Proc. 1987;46:1876–82. [PubMed] [Google Scholar]
- 21.Holick MF, MacLaughlin JA, Clark MB, Holick SA, Potts JT, Jr., Anderson RR, et al. Photosynthesis of previtamin D3 in human skin and the physiologic consequences. Science. 1980;210:203–5. doi: 10.1126/science.6251551. [DOI] [PubMed] [Google Scholar]
- 22.Holick MF. Vitamin D: A millenium perspective. J Cell Biochem. 2003;88:296–307. doi: 10.1002/jcb.10338. [DOI] [PubMed] [Google Scholar]
- 23.Holick MF, Tian XQ, Allen M. Evolutionary importance for the membrane enhancement of the production of vitamin D3 in the skin of poikilothermic animals. Proc Natl Acad Sci U S A. 1995;92:3124–6. doi: 10.1073/pnas.92.8.3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whyte MP, Haddad JG, Jr., Walters DD, Stamp TC. Vitamin D bioavailability: serum 25-hydroxyvitamin D levels in man after oral, subcutaneous, intramuscular, and intravenous vitamin D administration. J Clin Endocrinol Metab. 1979;48:906–11. doi: 10.1210/jcem-48-6-906. [DOI] [PubMed] [Google Scholar]
- 25.Chen TC. Photobiology of Vitamin D in “Vitamin D”. Humana press, 1998: 17-37. [Google Scholar]
- 26.Giacomoni PU. Spectral intensity of natural UVR and its dependence on various parameters. In: Urbach F, editor. The Biologic Effects of Ultraviolet Radiation. Oxford and New York. Pergamon Press, 1969: 351-8. [Google Scholar]
- 27.Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373–8. doi: 10.1210/jcem-67-2-373. [DOI] [PubMed] [Google Scholar]
- 28.Hannan MA, Paul M, Amer MH, Al-Watban FH. Study of ultraviolet radiation and genotoxic effects of natural sunlight in relation to skin cancer in Saudi Arabia. Cancer Res. 1984;44:2192–7. [PubMed] [Google Scholar]
- 29.Holick MF, Chen TC, Lu Z, Sauter E. Vitamin D and skin physiology: a D-lightful story. J Bone Miner Res. 2007;22(Suppl 2):V28–33. doi: 10.1359/jbmr.07s211. [DOI] [PubMed] [Google Scholar]
- 30.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, El-Kholie E, Yousef M, et al. Increased vitamin D supplementation recommended during summer season in the gulf region: a counterintuitive seasonal effect in vitamin D levels in adult, overweight and obese Middle Eastern residents. Clin Endocrinol (Oxf) 2012;76:346–50. doi: 10.1111/j.1365-2265.2011.04219.x. [DOI] [PubMed] [Google Scholar]
- 31.Holick MF. McCollum Award Lecture, 1994: vitamin D--new horizons for the 21st century. Am J Clin Nutr. 1994;60:619–30. doi: 10.1093/ajcn/60.4.619. [DOI] [PubMed] [Google Scholar]