Abstract
Background
Obsessive-compulsive disorder (OCD) is a heterogeneous and disabling condition; however, no studies have examined symptom categories or subtypes as predictors of long-term clinical course in adults with primary OCD.
Method
A total of 213 adults with DSM-IV OCD were recruited from several mental health treatment sites between July 2001 and February 2006 as part of the Brown Longitudinal Obsessive Compulsive Study, a prospective, naturalistic study of treatment-seeking adults with primary OCD. OCD symptoms were assessed annually over the 5-year follow-up period using the Longitudinal Interval Follow-Up Evaluation.
Results
Thirty-nine percent of participants experienced either a partial (22.1%) or a full (16.9%) remission. Two OCD symptom dimensions impacted remission. Participants with primary obsessions regarding overresponsibility for harm were nearly twice as likely to experience a remission (P < .05), whereas only 2 of 21 participants (9.5%) with primary hoarding achieved remission. Other predictors of increased remission were lower OCD severity (P < .0001) and shorter duration of illness (P < .0001). Fifty-nine percent of participants who remitted subsequently relapsed. Participants with obsessive-compulsive personality disorder were more than twice as likely to relapse (P < .005). Participants were also particularly vulnerable to relapse if they experienced partial remission versus full remission (70% vs 45%; P < .05).
Conclusions
The contributions of OCD symptom categories and comorbid obsessive-compulsive personality disorder are critically important to advancing our understanding of the prognosis and ultimately the successful treatment of OCD. Longer duration of illness was also found to be a significant predictor of course, highlighting the critical importance of early detection and treatment of OCD. Furthermore, having full remission as a treatment target is an important consideration for the prevention of relapse in this disorder.
Obsessive-compulsive disorder (OCD) is a common and frequently disabling psychiatric illness. Despite advances in the short-term treatment of OCD, a substantial number of individuals remain significantly impaired by their symptoms, and little is known about the long-term course of the disorder.1–5 Thus far, available course studies have not yielded consistent findings regarding rates of remission and relapse. Skoog and Skoog,6 in the longest follow-up study to date, reported data from a 40-year repeated-measures study of a cohort of 251 individuals treated for OCD in Sweden, prior to the recent era of improved treatments for OCD. Improvement was observed in 83% of the sample. However, fewer than half had “recovered” from OCD (20% no longer had symptoms and 28% had subclinical symptoms). More recent prospective observational studies in the era of efficacious short-term treatments for OCD have found surprisingly large differences in the probability of remission, ranging from .25 to .76.2,7–10 Rates of relapse were also variable in previous prospective studies, with probabilities of relapse ranging from .25 to .60.2,7,10 These previous investigations were all limited by small sample sizes, and the study with the largest sample size (N = 113)10 was composed of patients recruited for a primary anxiety disorder other than OCD and had a 32% attrition rate by 5 years.
Given the wide range of remission and relapse rates, it is critical to examine predictors of the variable outcome in OCD. Reported but inconsistent predictors of remission include both demographic and clinical features such as age at onset and symptom severity.6,7,9–12 In our previous report12 on the 2-year course of OCD, age at onset, symptom severity at intake, male gender, and obsessions regarding overresponsibility for harm were found to be significant predictors of remission. Of critical importance, there have been no course studies to date examining predictors of relapse in a primary OCD sample. The importance of subsyndromal symptoms and their association with overall course have been reported in other psychiatric disorders, notably mood disorders.13–15 It remains unknown what role OCD clinical features or the degree of clinical improvement may play in minimizing the risk of relapse.
Differences in reported rates of remission and relapse may, in part, be due to the heterogeneity of the disorder. Indeed, clinical features such as putative major symptom dimensions and subtypes of OCD have emerged as potentially important clinical predictors of treatment response and overall prognosis.12,16–18 Research has highlighted possible genetic variants as well as childhood vulnerabilities and risk factors as being linked to specific OCD subtypes and symptom dimensions.19,20 Examining the contribution of OCD subtypes, symptoms, and other clinical characteristics to the long-term course of OCD is key to advancing our understanding of etiology, prognosis, and treatment for this heterogeneous disorder.
We report here on the 5-year results of the Brown Longitudinal Obsessive Compulsive Study (BLOCS), the first prospective, observational study of a large clinical sample of individuals with primary OCD. The BLOCS uses gold-standard follow-up methodology to examine OCD-specific clinical features (eg, major symptom categories) as potential predictors of remission and relapse. On the basis of our 2-year findings,12 we predicted that having overresponsibility for harm would improve prognosis and that longer duration of OCD, greater severity of OCD symptoms at intake, male gender, and hoarding would continue to be associated with a lowered likelihood of remission. We also hypothesized that these predictors would be associated with relapse, as would degree of improvement, such that those achieving full remission would be less likely to relapse than those who achieved partial remission.
METHOD
Participants
Participants who were treatment-seeking within the past 5 years and identified OCD as the major psychiatric problem across their lifetime were recruited (July 2001–February 2006). The only exclusion criterion was having an organic mental disorder so that the person was unable to understand the nature of the study. Individuals with self- or referee-reported organic mental disorders were excluded from the study (n = 4). Participants were sequentially recruited from multiple psychiatric treatment settings; 71% were recruited from an outpatient OCD specialty clinic (consecutive admissions), 4% were from the inpatient units of a psychiatric hospital, and the remaining 25% were from community mental health centers, including 2 general outpatient psychiatric clinics, and the private practices of 3 experts in cognitive-behavioral therapy (CBT) for OCD. A total of 653 people were screened for inclusion in the BLOCS, with 127 refusing participation, 121 failing to meet initial inclusion criteria (eg, OCD not primary, no treatment in 5 years), 6 failing to meet inclusion criteria following the diagnostic intake assessment, and an additional 4 withdrawing after completing the intake assessment, for a total initial enrollment of 325 adults and 70 children. The BLOCS was approved by the institutional review boards at Butler Hospital and Brown University. All participants provided written informed consent.
This study reports on the 5-year course of 213 adult participants who met full criteria for OCD at intake (90% of the adult “in-episode” sample at intake) and had at least 3 years of follow-up data. The remaining 10% did not complete a 3-year follow-up assessment. There were no significant differences in demographics or course between those with and those without 3 or more years of follow-up. Table 1 shows demographic and clinical characteristics of the sample. Most of the sample (83%) was on treatment with a serotonin reuptake inhibitor (SRI) at study intake, and 90% reported SRI treatment during the first 5 years of the study. Of those who received SRI treatment, the mean number of weeks taking an SRI during the 5-year follow-up period was 201 (SD = 78). Slightly more than half of the participants (52%) received CBT during the study period. Of those who received CBT, 75% received at least 12 sessions (range, 1–277 sessions; mean = 47 sessions, SD = 46).
Table 1.
Clinical Characteristics of 213 Participants With Obsessive-Compulsive Disorder (OCD) at Intake
| Variable | Value |
|---|---|
| Female, n (%) | 120 (56.3) |
| White, n (%) | 207 (97.2) |
| Married, n (%) | 82 (38.5) |
| Employed, n (%) | 108 (50.9) |
| College educated, n (%) | 90 (42.3) |
| Age at intake, mean (SD), y | 39.8 (12.8) |
| Age at OCD onset, mean (SD), y | 17.9 (9.5) |
| Duration of OCD, mean (SD), y | 21.9 (13.6) |
| YBOCS total score (OCD severity), mean (SD) | 23.4 (5.7) |
| BABS total score (insight), mean (SD) | 7.0 (4.7) |
| GAF score, mean (SD) | 48.5 (9.5) |
| Principal obsession category, n (%)a | |
| Aggressive | 25 (11.7) |
| Overresponsibility for harm | 33 (15.5) |
| Contamination | 43 (20.2) |
| Sexual | 15 (7.0) |
| Hoarding | 21 (9.9) |
| Religious | 11 (5.2) |
| Symmetry | 26 (12.2) |
| Somatic | 14 (6.6) |
| Principal compulsion category, n (%)b | |
| Cleaning | 42 (19.9) |
| Checking | 46 (21.8) |
| Repeating | 27 (12.8) |
| Counting | 5 (2.4) |
| Ordering | 14 (6.6) |
| Hoarding | 21 (10.0) |
| Current Axis I comorbidity, n (%) | |
| Mood disorderc | 39 (18.3) |
| Psychotic disorder | 4 (1.9) |
| Other anxiety disorder | 88 (41.5) |
| Substance use disorder | 11 (5.2) |
| Eating disorder | 5 (2.4) |
| Somatoform disorder | 15 (7.0) |
| Tic disorder | 17 (8.0) |
| No. of Axis I disorders, mean (SD) | 2.2 (1.3) |
| OCPD, n (%) | 62 (29.1) |
n = 211 (2 did not endorse a primary obsession). Refers to the YBOCS Symptom Checklist category of the single obsession subject “Would most like to get rid of” (mutually exclusive categories).
n = 208 (2 missing and 3 did not endorse having primary compulsion). Refers to the YBOCS Symptom Checklist category of the single compulsion subject “Would most like to get rid of” (mutually exclusive categories).
Major depressive disorder, n = 36 (16.9%).
Abbreviations: BABS = Brown Assessment of Beliefs Scale, GAF = Global Assessment of Functioning, OCPD = obsessive-compulsive personality disorder, YBOCS = Yale-Brown Obsessive Compulsive Scale.
Assessments
The Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition21 and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders22 were used to establish diagnoses. Demographic and clinical information was collected using a semistructured rater-administered questionnaire, the Butler Hospital OCD Database.23 The Yale-Brown Obsessive Compulsive Scale (YBOCS) and Symptom Checklist (YBOCS-SC) were administered to assess severity of OCD symptoms and specific obsessions and compulsions.24,25 Primary obsession was defined as the obsession on the YBOCS-SC that the participants “would most like to get rid of.” Based on previous factor analytic research,26,27 an additional obsessions category was included, overresponsibility for harm, which was composed of 2 obsessions, fear of harming others if not careful enough and fear of being responsible for something terrible happening. Therefore, each endorsed primary obsession fell within 1 of the 8 obsession categories on the YBOCS-SC (aggressive, overresponsibility for harm, contamination, sexual obsessions, hoarding obsessions, religious obsessions, symmetry obsessions, and somatic obsession). We chose obsessions rather than compulsions because of their greater specificity to domains of symptom content. Compulsions tend to be nonspecific (eg, a checking ritual can relate to a fear of causing harm or a concern about having an illness). The Brown Assessment of Beliefs Scale (BABS)28 was administered to determine insight into OCD beliefs, with higher scores indicating poorer insight. The Global Assessment of Functioning29 was administered to assess overall severity of psychopathology and functional impairment in the worst week of the past month.
Participants underwent annual assessments during the study either in person or via a telephone interview. Each annual assessment included the Longitudinal Interval Follow-Up Evaluation (LIFE), a semistructured instrument used previously in longitudinal studies of psychiatric disorders.10,30 During the annual LIFE interview, the rater reviews each week of the previous year with the participant and codes a weekly psychiatric status rating (PSR) for each diagnosis based on symptom severity. The reliability and validity of the LIFE are reported elsewhere.31 For this study, the OCD PSR had 6 points based on OCD symptom severity and functional impairment. A PSR of 4 or greater represents full DSM-IV criteria for OCD, with 6 being the most severe and impaired. A PSR of 3 is assigned when OCD symptoms are present but not impairing and symptoms occupy less than an hour daily. A PSR of 2 indicates minimal symptoms and no impairment; a PSR of 1 indicates no symptoms. Full remission was defined as an OCD PSR of 1 or 2 for 8 consecutive weeks, and partial remission was defined as a PSR of 3 for 8 consecutive weeks. Having achieved either partial or full remission, participants were considered to have relapsed if their OCD PSR increased to 4, 5, or 6 for 4 consecutive weeks. These definitions mirror those used in other major longitudinal studies of psychiatric disorders.32–34 The LIFE was also used to collect data regarding pharmacologic and psychotherapy usage; the methodology for reporting treatments received is reported elsewhere.12
Interviewer Training
Details describing interviewer training are reported elsewhere.35 New raters were required to demonstrate interrater reliability with both trainers and senior raters (intraclass correlation coefficients > 0.85 for YBOCS total score and Structured Clinical Interview for DSM-IV/LIFE diagnoses). To prevent “rater drift,” assessment of interrater reliability was conducted periodically on random samples of taped interviews. Shrout-Fleiss interrater reliabilities were 0.95 for total YBOCS scores, 0.97 for OCD PSR ratings, and 0.97 for Global Assessment of Functioning scores.
Analyses
Descriptive analyses of course used Kaplan-Meier life tables for remission and relapse. Predictors of remission and relapse were determined using Cox proportional hazards regression.36 In the analysis of remission, all predictors were entered simultaneously; the a level was .05. Because of the smaller number of cases in the relapse analyses, however, a forward stepwise procedure was used with a P value to enter of .05 and a P value to stay of .10. On the basis of our 2-year course findings,12 we tested the following variables (assessed at intake) as predictors of remission and relapse: OCD severity (total YBOCS score), level of insight (BABS score), gender, number of current Axis I diagnoses, OCPD diagnosis, OCD duration, and binary indicator variables for whether the primary obsession was overresponsibility or hoarding (other primary obsession categories were tested in secondary analyses). Because only 2 participants with primary hoarding remitted, hoarding was omitted from the relapse analyses. Duration of illness, age at OCD onset, and age at intake were highly correlated. We chose to use duration of illness because this variable has been assessed in previous studies of the course of OCD.7,9,11
We conducted descriptive analyses of SRI and CBT treatments received. Effects of treatment in naturalistic studies are complicated by multiple factors including nonrandom assignment to treatment and variations in treatment implementation.37,38 Because of these potential biases, a comprehensive analysis of treatment effects is beyond the scope of this article.
RESULTS
Rates and Predictors of Remission
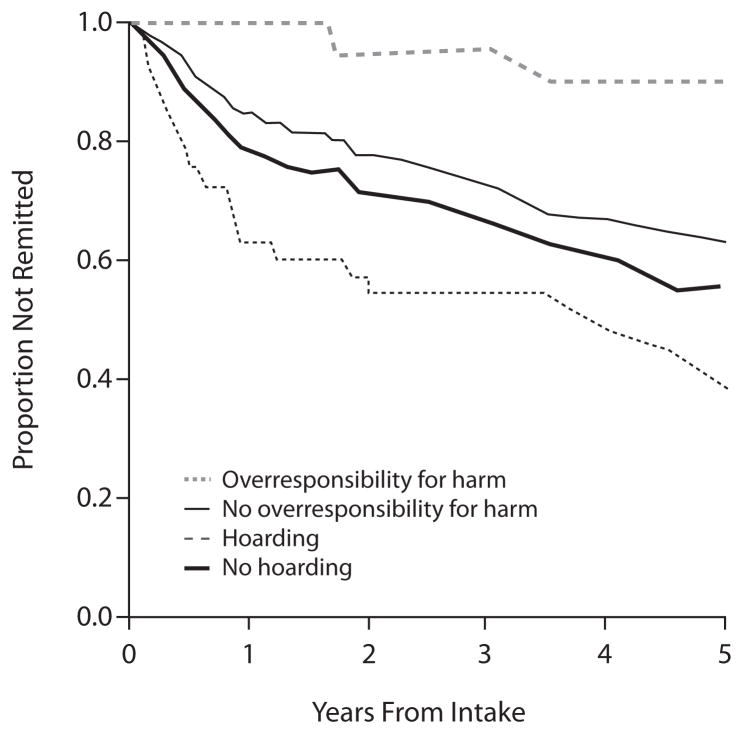
The cumulative rate of remission for OCD over 5 years was 38.9%. Of the 83 total remissions, 47 were partial remissions (22.1% of the sample), and 36 were full remissions (16.9% of the sample). Shorter duration of illness was associated with a higher rate of remission (Table 2). Lower severity of illness at intake, as measured by the YBOCS, was associated with a higher rate of remission. Participants who endorsed overresponsibility as their primary concern were more likely to remit as compared to participants who endorsed other obsessions as primary on the YBOCS-SC; 61% with overresponsibility remitted, versus 37% for those without overresponsibility (Figure 1). Although the finding did not reach statistical significance, it is notable that only 2 of 21 participants (9.5%) with primary hoarding remitted. Insight, gender, OCPD, and Axis I diagnostic comorbidity were not associated with the rate of remission. In secondary analyses, we tested the other primary obsession categories and found no additional significant predictors (all P values > .05).
Table 2.
Proportional Hazard Regression Testing Clinical Predictors of Remission and Relapse From Obsessive-Compulsive Disorder (OCD) Over 5 Years (N = 213)
| B (SE) | χ2 | Pa | Hazard Ratio | 95% CI | |
|---|---|---|---|---|---|
| Remission predictorsb | |||||
|
| |||||
| Duration of OCD (years) | −0.06 (0.02) | 26.14 | <.0001 | 0.95 | 0.92–0.97 |
| OCD severity (YBOCS total score) | −0.12 (0.02) | 30.56 | <.0001 | 0.88 | 0.85–0.92 |
| Insight (BABS total score) | 0.04 (0.03) | 2.72 | .10 | 1.04 | 0.99–1.10 |
| Overresponsibility for harm | 0.64 (0.27) | 5.41 | .02 | 1.89 | 1.11–3.22 |
| Gender | −0.34 (0.23) | 2.29 | .13 | 0.71 | 0.45–1.11 |
| Hoarding | −0.75 (0.73) | 1.05 | .31 | 0.47 | 0.11–1.98 |
| OCPD | −0.48 (0.30) | 2.62 | .11 | 0.62 | 0.34–1.11 |
| Axis I comorbidityc | 0.06 (0.10) | 0.33 | .57 | 1.06 | 0.87–1.29 |
|
| |||||
| Relapse predictorsd | |||||
|
| |||||
| Duration of OCD (years) | −0.01 (0.01) | 0.81 | .37 | 0.99 | 0.97–1.01 |
| OCD severity (YBOCS total score) | 0.02 (0.02) | 0.42 | .52 | 1.02 | 0.97–1.07 |
| Insight (BABS total score) | −0.71 (0.03) | 4.42 | .04e | 0.93 | 0.87–1.00 |
| Overresponsibility for harm | −0.73 (0.37) | 3.81 | .05f | 0.48 | 0.23–1.00 |
| Gender | 0.18 (0.29) | 0.40 | .53 | 1.20 | 0.68–2.11 |
| Hoardingg | … | … | … | … | … |
| OCPD | 0.94 (0.34) | 7.76 | <.005 | 2.56 | 1.32–4.96 |
| Axis I comorbidityb | 0.19 (0.14) | 1.89 | .17 | 1.21 | 0.92–1.58 |
Boldface indicates significance.
Predictors entered simultaneously. Wald χ28 = 38.18, P < .001.
Axis I comorbidity = number of current comorbid Axis I disorders at intake.
Predictors entered stepwise. Wald χ28 = 19.85, P < .01.
Regression artifact due to a suppression effect.
P = .051.
Hoarding was excluded from relapse analyses due to only 2 remissions among participants who identified hoarding as primary obsession category.
Abbreviations: BABS = Brown Assessment of Beliefs Scale, OCPD = obsessive-compulsive personality disorder, YBOCS = Yale-Brown Obsessive Compulsive Scale.
Figure 1.
Survival Curves for Remission of Obsessive-Compulsive Disorder Over Follow-Up According to Primary Obsessive Symptom
Rates and Predictors of Relapse
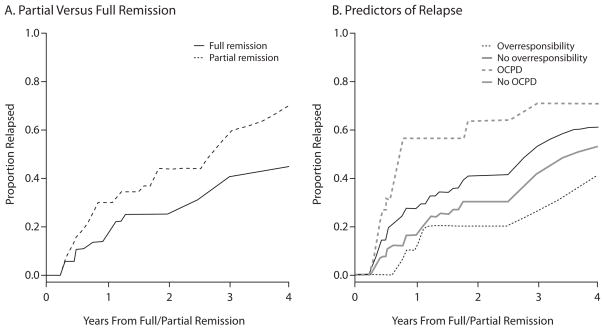
More than half of the participants who achieved full or partial remission (49/83, 59%) subsequently relapsed. As shown in Figure 2 and Table 2, participants with comorbid OCPD had a significantly higher rate of relapse. Overresponsibility for harm was marginally significant (hazard ratio [HR] = 0.48; 95% CI, 0.23–1.00; P = .051), and insight at intake (BABS score) was associated with time to relapse in our stepwise procedure (HR = 0.93; 95% CI, 0.87–1.00; P < .05). A secondary univariate analysis of the BABS revealed a nonsignificant trend in the opposite direction, leading us to conclude that the BABS finding was a regression artifact due to a suppression effect. Those who achieved only partial remission (subclinical noninterfering symptoms) were more likely to relapse compared to those who fully remitted (70% vs 45%; HR = 0.50; 95% CI, 0.29–0.84; P < .05). In secondary analyses, we tested the other primary obsession categories and found no additional significant predictors (all P values > .05).
Figure 2. Survival Curves for Relapse of Obsessive-Compulsive Disorder Over Follow-Up.
Abbreviation: OCPD = obsessive-compulsive personality disorder.
DISCUSSION
The primary aims of this study were to examine remission and relapse rates of OCD during 5 years of prospective follow-up and to determine predictors of course in a longitudinal study of 213 adults with primary OCD. Over one-third of the participants experienced substantial improvement of their OCD to the point of subclinical noninterfering symptoms. Other prospective follow-up studies of OCD have observed higher rates of remission.2,9 These rates of remission ranging as high as 76% may, in part, be accounted for by differences in the chronicity of OCD illness between samples. Indeed, duration of illness has been associated with poorer outcome in prior investigations9,39 and was a powerful predictor of remission in this study. Our sample of treatment-seeking adults with OCD was particularly chronic; participants had a mean duration of illness of nearly 22 years. The relationship between duration and course highlights the critical need for early detection and intervention, as the rate of remission declines as the illness persists.
While over one-third of the participants remitted, more than half of these participants subsequently relapsed. Our rates of relapse were high particularly in participants who continued to have subclinical symptoms; the likelihood of relapse was 25% higher for participants in partial remission compared with those subjects in full remission. These findings further underscore the importance of treating patients as early as possible after the onset of OCD and targeting full remission from OCD—rather than improvement of symptoms—as the treatment goal.
The current study is the first to explore primary obsessions as predictors of long-term course in adults with OCD, with hoarding and overresponsibility emerging as key variables impacting clinical course. Consistent with convergent brain imaging and treatment outcome data,40–42 only 2 of 21 participants with primary hoarding experienced a remission over 5 years. These results are also consistent with a recent longitudinal cohort study of pediatric OCD associating prominent hoarding symptoms with the persistence of OCD.43 Taken together, these findings support the current direction of distinguishing hoarding from OCD from a diagnostic perspective, as is being considered in DSM-5.44,45 In contrast to hoarding, overresponsibility for harm was associated with a significantly better prognosis in this investigation. Individuals with overresponsibility for harm as their principal obsession category were almost twice as likely to remit and almost half as likely to relapse, with the relapse finding approaching statistical significance. This finding of a distinct pattern of course supports the growing body of evidence suggesting that OCD symptom dimensions have distinct patterns in a number of domains including comorbidity, genetic transmission, neural substrates, and treatment response.46
OCPD was also found to be a significant risk factor for OCD relapse. While several studies have examined the relationship between OCPD and OCD, literature on longitudinal associations between the two disorders is sparse. One prior investigation examining the longitudinal course of personality disorders failed to find an association between the course of OCPD and OCD.47 However, this study was limited by its small sample size of OCD patients and did not investigate relapse specifically. The results of the current investigation lend support to the growing body of literature highlighting the deleterious effect of OCPD on OCD treatment outcome.48,49 Future work is needed to clarify the relationship between OCPD and OCD morbidity and to determine if OCPD comorbid with OCD constitutes a specific subtype of the disorder50,51 or is a marker of severity in OCD.52
Naturalistic investigations by design observe but do not manipulate treatments received. As a consequence, the causal path between treatment and symptom change is often ambiguous9,10,38 and subject to a treatment bias effect whereby individuals with greater symptom severity are more likely to receive treatment. Therefore, examining the impact of treatment on long-term course is beyond the scope of this study. Further, our finding that the vast majority of participants were continuously maintained on SRI treatment throughout the duration of the follow-up interval highlights the need for controlled maintenance and long-term safety studies of the SRIs for OCD. Future studies utilizing data analytic techniques developed to address treatment in naturalistic studies of psychiatric disorders are warranted to further disentangle the complex relationship between long-term treatment and outcome.
Contrary to our prediction, gender was not found to significantly predict course in this study. Of note, being male was a predictor in our 2-year course study.12 Although gender was not a significant predictor of remission in our 5-year analysis, inspection of the survival curves for gender indicate that women tended to remit earlier than men (as represented by the significant gender difference in our 2-year analysis), but by 5 years the rate of remission for men caught up to that of women, and hence the 2 rates were no longer significantly different.
The results of this study must be considered in light of several limitations. First, the participants in our sample were primarily white, were treatment-seeking, and had relatively chronic symptoms. Therefore, it is unclear how our results generalize to more diverse or non–treatment-seeking individuals in the community. Second, despite the use of well-validated assessment measures, data collected on treatments received and symptom severity over the follow-up interval are subject to retrospective recall bias. Finally, while the YBOCS represents the gold standard in OCD assessment, limited information is gained regarding specific obsessions. Future research including dimensional approaches to assessing OCD symptoms may provide additional clarity regarding the relationship between OCD symptoms and course.53–55 Despite these limitations, this study is the longest and largest prospective study of course in OCD using state of the art methodology. Further, it is the first study, to our knowledge, to assess the likelihood and predictors of relapse following prospectively observed remission and the first to explore OCD symptom categories and subtypes as predictors of clinical course.
In summary, 2 previously unreported findings emerged with regard to factors that influence course in OCD. First, an important distinction was found between those who experience partial versus full remission, with the former experiencing a much higher relapse rate. Second, our study highlights the heterogeneity of OCD, with different course patterns being uniquely associated with specific symptom categories. Taken together, these results highlight the critical need to develop more targeted treatments to address the variable outcome and treatment response in this disorder.
Clinical Points.
Clinicians should target full remission (minimal or no symptoms) of obsessive-compulsive disorder (OCD) to minimize the risk of relapse.
Comorbid obsessive-compulsive personality disorder is associated with a worse OCD course.
Primary obsessions regarding overresponsibility for harm are associated with better prognosis compared with other types of obsessions.
Acknowledgments
Funding/support: This study was supported by National Institute of Mental Health grants to Dr Rasmussen (R01 MH060218), Dr Pinto (K23 MH080221), and Dr Mancebo (K23 MH091032).
Footnotes
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside US Food and Drug Administration–approved labeling has been presented in this article.
Financial disclosure: Drs Eisen, Sibrava, Boisseau, Mancebo, Stout, Pinto, and Rasmussen have no personal affiliations or financial relationships with any commercial interest to disclose relative to the article.
Financial Disclosure
All individuals in a position to influence the content of this activity were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. In the past year, Alan J. Gelenberg, MD, Editor in Chief, has been a consultant for Allergan and Forest, has received grant/research support from Pfizer, and has been a stock shareholder of Healthcare Technology Systems. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears at the end of the article.
References
- 1.Foa EB, Liebowitz MR, Kozak MJ, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- 2.Eisen JL, Goodman WK, Keller MB, et al. Patterns of remission and relapse in obsessive-compulsive disorder: a 2-year prospective study. J Clin Psychiatry. 1999;60(5):346–351. doi: 10.4088/JCP.v60n0514. quiz 352. [DOI] [PubMed] [Google Scholar]
- 3.Fineberg NA, Craig KJ. Pharmacotherapy for obsessive-compulsive disorder. In: Stein DJ, Hollander E, Rothbaum BP, editors. Textbook of Anxiety Disorders. 2. Washington, DC: American Psychiatric Publishing, Inc; 2010. pp. 311–338. [Google Scholar]
- 4.Greist J, Chouinard G, DuBoff E, et al. Double-blind parallel comparison of three dosages of sertraline and placebo in outpatients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1995;52(4):289–295. doi: 10.1001/archpsyc.1995.03950160039008. [DOI] [PubMed] [Google Scholar]
- 5.van Oppen P, van Balkom AJ, de Haan E, et al. Cognitive therapy and exposure in vivo alone and in combination with fluvoxamine in obsessive-compulsive disorder: a 5-year follow-up. J Clin Psychiatry. 2005;66(11):1415–1422. doi: 10.4088/JCP.v66n1111. [DOI] [PubMed] [Google Scholar]
- 6.Skoog G, Skoog I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56(2):121–127. doi: 10.1001/archpsyc.56.2.121. [DOI] [PubMed] [Google Scholar]
- 7.Catapano F, Perris F, Masella M, et al. Obsessive-compulsive disorder: a 3-year prospective follow-up study of patients treated with serotonin reuptake inhibitors OCD follow-up study. J Psychiatr Res. 2006;40(6):502–510. doi: 10.1016/j.jpsychires.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Reddy YC, D’Souza SM, Shetti C, et al. An 11- to 13-year follow-up of 75 subjects with obsessive-compulsive disorder. J Clin Psychiatry. 2005;66(6):744–749. doi: 10.4088/JCP.v66n0611. [DOI] [PubMed] [Google Scholar]
- 9.Steketee G, Eisen J, Dyck I, et al. Predictors of course in obsessive-compulsive disorder. Psychiatry Res. 1999;89(3):229–238. doi: 10.1016/S0165-1781(99)00104-3. [DOI] [PubMed] [Google Scholar]
- 10.Marcks BA, Weisberg RB, Dyck I, et al. Longitudinal course of obsessive-compulsive disorder in patients with anxiety disorders: a 15-year prospective follow-up study. Compr Psychiatry. 2011;52(6):670–677. doi: 10.1016/j.comppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ravizza L, Maina G, Bogetto F. Episodic and chronic obsessive-compulsive disorder. Depress Anxiety. 1997;6(4):154–158. doi: 10.1002/(SICI)1520-6394(1997)6:4<154::AID-DA4>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 12.Eisen JL, Pinto A, Mancebo MC, et al. A 2-year prospective follow-up study of the course of obsessive-compulsive disorder. J Clin Psychiatry. 2010;71(8):1033–1039. doi: 10.4088/JCP.08m04806blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Judd LL, Schettler PJ, Akiskal HS, et al. Residual symptom recovery from major affective episodes in bipolar disorders and rapid episode relapse/ recurrence. Arch Gen Psychiatry. 2008;65(4):386–394. doi: 10.1001/archpsyc.65.4.386. [DOI] [PubMed] [Google Scholar]
- 14.Kiosses DN, Alexopoulos GS. The prognostic significance of subsyndromal symptoms emerging after remission of late-life depression. Psychol Med. 2012;21:1–10. doi: 10.1017/S0033291712000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grabovich A, Lu N, Tang W, et al. Outcomes of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2010;18(3):227–235. doi: 10.1097/JGP.0b013e3181cb87d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leckman JF, Denys D, Simpson HB, et al. Obsessive-compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V. Depress Anxiety. 2010;27(6):507–527. doi: 10.1002/da.20669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mataix-Cols D, Rauch SL, Manzo PA, et al. Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 1999;156(9):1409–1416. doi: 10.1176/ajp.156.9.1409. [DOI] [PubMed] [Google Scholar]
- 18.Steketee G, Frost RO. Compulsive hoarding: current status of the research. Clin Psychol Rev. 2003;23(7):905–927. doi: 10.1016/j.cpr.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Grisham JR, Fullana MA, Mataix-Cols D, et al. Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychol Med. 2011;15:1–12. doi: 10.1017/S0033291711000894. [DOI] [PubMed] [Google Scholar]
- 20.Iervolino AC, Rijsdijk FV, Cherkas L, et al. A multivariate twin study of obsessive-compulsive symptom dimensions. Arch Gen Psychiatry. 2011;68(6):637–644. doi: 10.1001/archgenpsychiatry.2011.54. [DOI] [PubMed] [Google Scholar]
- 21.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition (SCID/IP Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 22.First MB, Gibbon M, Spitzer RL, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 23.Rasmussen SA. Genetic studies of obsessive-compulsive disorder. Ann Clin Psychiatry. 1993;5(4):241–247. doi: 10.3109/10401239309148823. [DOI] [PubMed] [Google Scholar]
- 24.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale, 1: development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 25.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale, 2: validity. Arch Gen Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 26.Pinto A, Eisen JL, Mancebo MC, et al. Taboo thoughts and doubt/checking: a refinement of the factor structure for obsessive-compulsive disorder symptoms. Psychiatry Res. 2007;151(3):255–258. doi: 10.1016/j.psychres.2006.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinto A, Greenberg BD, Grados MA, et al. Further development of YBOCS dimensions in the OCD Collaborative Genetics study: symptoms vs categories. Psychiatry Res. 2008;160(1):83–93. doi: 10.1016/j.psychres.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eisen JL, Phillips KA, Baer L, et al. The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry. 1998;155(1):102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 30.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 31.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the Longitudinal Interval Follow-up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28(6):531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 32.Ansell EB, Pinto A, Edelen MO, et al. The association of personality disorders with the prospective 7-year course of anxiety disorders. Psychol Med. 2011;41(5):1019–1028. doi: 10.1017/S0033291710001777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bruce SE, Yonkers KA, Otto MW, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162(6):1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keller MB, Shapiro RW, Lavori PW, et al. Recovery in major depressive disorder: analysis with the life table and regression models. Arch Gen Psychiatry. 1982a;39(8):905–910. doi: 10.1001/archpsyc.1982.04290080025004. [DOI] [PubMed] [Google Scholar]
- 35.Pinto A, Mancebo MC, Eisen JL, et al. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. J Clin Psychiatry. 2006;67(5):703–711. doi: 10.4088/JCP.v67n0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cox DR. Regression models and life-tables. J R Stat Soc, B. 1972;34(2):187–220. [Google Scholar]
- 37.Rosenbaum PR, Rubin DB. The bias due to incomplete matching. Biometrics. 1985;41(1):103–116. doi: 10.2307/2530647. [DOI] [PubMed] [Google Scholar]
- 38.Leon AC. Evaluation of psychiatric interventions in an observational study: issues in design and analysis. Dialogues Clin Neurosci. 2011;13(2):191–198. doi: 10.31887/DCNS.2011.13.2/aleon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dell’Osso B, Buoli M, Hollander E, et al. Duration of untreated illness as a predictor of treatment response and remission in obsessive-compulsive disorder. World J Biol Psychiatry. 2010;11(1):59–65. doi: 10.3109/15622970903418544. [DOI] [PubMed] [Google Scholar]
- 40.Mataix-Cols D, Marks IM, Greist JH, et al. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychother Psychosom. 2002;71(5):255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- 41.Saxena S. Neurobiology and treatment of compulsive hoarding. CNS Spectr. 2008;13(suppl 14):29–36. doi: 10.1017/s1092852900026912. [DOI] [PubMed] [Google Scholar]
- 42.Saxena S, Brody AL, Maidment KM, et al. Cerebral glucose metabolism in obsessive-compulsive hoarding. Am J Psychiatry. 2004;161(6):1038–1048. doi: 10.1176/appi.ajp.161.6.1038. [DOI] [PubMed] [Google Scholar]
- 43.Bloch MH, Craiglow BG, Landeros-Weisenberger A, et al. Predictors of early adult outcomes in pediatric-onset obsessive-compulsive disorder. Pediatrics. 2009;124(4):1085–1093. doi: 10.1542/peds.2009-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pertusa A, Frost RO, Fullana MA, et al. Refining the diagnostic boundaries of compulsive hoarding: a critical review. Clin Psychol Rev. 2010;30(4):371–386. doi: 10.1016/j.cpr.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 45.Mataix-Cols D, Frost RO, Pertusa A, et al. Hoarding disorder: a new diagnosis for DSM-V? Depress Anxiety. 2010;27(6):556–572. doi: 10.1002/da.20693. [DOI] [PubMed] [Google Scholar]
- 46.Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry. 2005;162(2):228–238. doi: 10.1176/appi.ajp.162.2.228. [DOI] [PubMed] [Google Scholar]
- 47.Shea MT, Stout RL, Yen S, et al. Associations in the course of personality disorders and Axis I disorders over time. J Abnorm Psychol. 2004;113(4):499–508. doi: 10.1037/0021-843X.113.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cavedini P, Erzegovesi S, Ronchi P, et al. Predictive value of obsessive-compulsive personality disorder in antiobsessional pharmacological treatment. Eur Neuropsychopharmacol. 1997;7(1):45–49. doi: 10.1016/S0924-977X(96)00382-3. [DOI] [PubMed] [Google Scholar]
- 49.Pinto A, Liebowitz MR, Foa EB, et al. Obsessive compulsive personality disorder as a predictor of exposure and ritual prevention outcome for obsessive compulsive disorder. Behav Res Ther. 2011;49(8):453–458. doi: 10.1016/j.brat.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coles ME, Pinto A, Mancebo MC, et al. OCD with comorbid OCPD: a subtype of OCD? J Psychiatr Res. 2008;42(4):289–296. doi: 10.1016/j.jpsychires.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 51.Garyfallos G, Katsigiannopoulos K, Adamopoulou A, et al. Comorbidity of obsessive-compulsive disorder with obsessive-compulsive personality disorder: does it imply a specific subtype of obsessive-compulsive disorder? Psychiatry Res. 2010;177(1–2):156–160. doi: 10.1016/j.psychres.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 52.Lochner C, Serebro P, van der Merwe L, et al. Comorbid obsessive-compulsive personality disorder in obsessive-compulsive disorder (OCD): a marker of severity. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(4):1087–1092. doi: 10.1016/j.pnpbp.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Leckman JF, Rauch SL, Mataix-Cols D. Symptom dimensions in obsessive-compulsive disorder: implications for the DSM-V. CNS Spectr. 2007;12(5):376–387. 400. doi: 10.1017/s1092852900021179. [DOI] [PubMed] [Google Scholar]
- 54.Rosario-Campos MC, Miguel EC, Quatrano S, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11(5):495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- 55.Abramowitz JS, Deacon BJ, Olatunji BO, et al. Assessment of obsessive-compulsive symptom dimensions: development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psychol Assess. 2010;22(1):180–198. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]