Abstract
Study Objectives:
Mexican immigrants to the United States report longer sleep duration and fewer sleep complaints than their US-born counterparts. To investigate whether this effect extends to other immigrant groups, we examined whether the prevalence of self-reported sleep complaints is higher among US-born Hispanic/Latina, Chinese, and Japanese immigrant women compared to their first-generation immigrant ethnic counterparts as well as to US-born whites. We examined whether these associations persisted after adjusting for sociodemographic and health characteristics and whether acculturation mediated the effects.
Design:
Cross-sectional observational study.
Setting:
Multisite study in Oakland, CA; Los Angeles, CA; and Newark, NJ.
Participants:
Hispanic/Latina (n = 196), Chinese (n = 228), Japanese (n = 271) and non-Hispanic white (n = 485) women (mean age = 46 y, range 42-52 y) participating in the Study of Women's Health Across the Nation (SWAN); 410 or 59.0% of the nonwhites were first-generation immigrants.
Interventions:
None.
Measurements and Results:
Questionnaires were used to assess sleep complaints, race/ethnicity, immigrant status, language acculturation (use of English language), and sociodemographic and health variables. Approximately 25% of first-generation immigrant women reported sleep complaints compared to 37% of those who were US-born nonwhites and 42% of US-born whites. Multivariable adjusted logistic regression analyses showed that US-born nonwhites had higher odds of reporting any sleep complaints (odds ratio = 2.1, 95% confidence interval [CI] 1.5-3.0), compared to first-generation immigrants. Women with higher levels of language acculturation had greater odds of reporting any sleep complaint compared to those with less language acculturation. Adjustment for language acculturation mediated 40.4% (95% CI 28.5-69.8) of the association between immigrant status and any sleep complaint. When results were stratified by race/ethnicity, significant mediation effects of acculturation were only found for Hispanic/Latina and Japanese women, but not for Chinese women.
Conclusion:
US-born Hispanic/Latina, Chinese, and Japanese immigrants were more likely to report sleep complaints than their first-generation ethnic counterparts, a finding largely explained by language acculturation and unmeasured factors associated with language acculturation.
Citation:
Hale L; Troxel WM; Kravitz HM; Hall MH; Matthews KA. Acculturation and sleep among a multiethnic sample of women: the Study of Women's Health Across the Nation (SWAN). SLEEP 2014;37(2):309-317.
Keywords: Sleep, immigrant, acculturation, women
INTRODUCTION
Both objective and subjective reports of sleep reveal racial and ethnic differences in sleep duration and quality.1–3 Generally, African Americans and Hispanics have more sleep complaints in comparison with non-Hispanic whites, whereas Asians have fewer sleep complaints in comparison with non-Hispanic whites in the United States.2,3 Among Hispanics, US-born Hispanics have more sleep complaints than do first-generation immigrants, suggesting that acculturation in the United States is associated with worse sleep.4,5 To our knowledge, relationships between immigrant status and sleep have not been evaluated in other racial/ethnic groups in the United States. In this manuscript, we investigated whether US-born Hispanic/Latina, Chinese, and Japanese women reported more sleep complaints in comparison with first-generation immigrant women of the same racial/ethnic group and US-born whites. We further sought to understand whether such advantages may be attributable to differences in sociodemographic, health, and/or language acculturation.
Immigration and Health
On average, US immigrants have better health outcomes and behaviors than their nonimmigrant counterparts.6,7 This immigrant health advantage is observed for all-cause mortality rates, in addition to prevalence of increased body weight and obesity, heart and circulatory disease, diabetes, cancer, infectious disease, and injuries.6 The data are mixed with regard to mental health and self-assessed general health.6 Given the numerous associations between sleep (both quality and duration) and mental health, morbidity, and mortality outcomes,8–12 an emerging area of research on immigrant health seeks to understand sleep patterns of immigrant populations. To date, however, most of this research has focused on the sleep patterns of Hispanic/Latino populations. For example, using data from the National Health Interview Survey, a nationally representative study that includes self-reported data on sleep duration, Hale and Rivero-Fuentes5 found that Mexican-born immigrants were less likely to be short sleepers than US-born Mexican-Americans. After adjustment for health and well-being variables (i.e., smoking, overweight/obesity, and stress), the association was not statistically significant, suggesting that part of the protective sleep patterns of immigrant populations may be driven by the adoption of other health behaviors that may be detrimental to sleep. In two separate studies, researchers examined the sleep patterns of Mexican-born immigrants in two waves of the National Health and Nutrition Examination Survey (NHANES): the 2005-200613 and the 2007-20084 waves. Both studies showed similar results; Mexican-born immigrants to the US had lower odds of short sleeping and fewer insomnia symptoms compared to individuals born in the US.
Only a handful of studies have looked specifically at the association between measures of acculturation and sleep disturbances. Heilemann et al. found positive associations between acculturation and self-reported sleep disturbances in a sample of around 300 women of Mexican descent in an urban Northern California community. Women who preferred to speak English and had earlier socialization to the US were more likely to report sleep disturbances. Kachikis and Breitkopf15 also found that among a subsample of Hispanic/Latina women (n = 1,966), higher acculturation scores (based on language) were associated with worse self-reported sleep quality. These findings raise the possibility that first-generation immigrants who are less acculturated are the ones who maintain better sleep. The literature regarding sleep among immigrants of ethnic populations other than Hispanics immigrating to America is more limited. Two international studies investigated the quality of sleep of Moroccan and Portuguese immigrants in Germany, and found that adoption of a Western lifestyle was associated with increased reports of poor sleep quality.16,17 These studies suggest that the experience of poor sleep among more acculturated individuals might generalize to other ethnic populations beyond Hispanics/Latinos.
Social Factors and Sleep
In prior studies focusing on the social determinants of sleep patterns, sociodemographic factors (such as unemployment and low education) that are associated with increased psychosocial stress are adversely associated with both high-risk sleep durations and low-quality sleep in both children and adults.1,18–24 Because immigrant populations may experience greater levels of psychosocial stress than others, one might hypothesize that foreign-born immigrants are likely to be vulnerable to sleep difficulties as they adapt to life in the United States. However, given the variety of literature on better health behaviors and health outcomes among immigrants, we expected to find that sleep quality will be comparatively better among the foreign-born immigrants, even after accounting for differences in sociodemographic and health factors.
The current analysis expands on the research on sleep in immigrants by investigating a sample that includes immigrant women from three race/ethnic categories, Hispanic/Latina, Japanese, and Chinese, and comparing their sleep patterns to their US-born ethnic counterparts and to US-born whites. Based on prior research, we expected that US-born women (both nonwhite and white) would report more sleep complaints compared to first-generation immigrants from three racial/ ethnic populations (Hispanic/Latina, Japanese, and Chinese) (Hypothesis 1). In addition, supported by prior evidence among Mexican Americans and insomnia symptoms, we hypothesized that this increased association with sleep complaints would persist after adjustment for socioeconomic and health characteristics known to be associated with sleep (Hypothesis 2). Finally, we hypothesized that language acculturation would mediate the association between immigrant status and sleep complaints (Hypothesis 3).
METHODS
Data
We used data from the Study of Women's Health Across the Nation (SWAN), a multisite, multiethnic, community-based study. The purpose of this national study was to characterize biologic and psychosocial changes occurring during the menopausal transition conducted at seven sites within the United States: Los Angeles, CA; Oakland, CA; Chicago, IL; Detroit, MI; Pittsburgh, PA; Newark, NY; and Boston, MA. We used the three sites at which there was representation of the three racial/ethnic groups of interest to this report (Oakland, Los Angeles, and Newark). Additional details about the study design and recruitment procedures of the SWAN study have been reported previously.25 Briefly, at each of the study sites, investigators recruited a sample that comprised both Caucasian women and one minority group (African-Americans in Boston, Chicago, Detroit, and Pittsburgh; Chinese in Oakland, Japanese in Los Angeles, and Hispanics/Latinas in Newark). All sites and researchers received approval from and adhered to the appropriate Institutional Review Board's guidelines for conducting human research. All participants provided written informed consent. Of the women who were contacted, 73% of them provided sufficient information to determine study eligibility. The eligibility criteria at baseline were: age 42-52 y, menses within the previous 3 mo, not pregnant or breast feeding, an intact uterus and at least one ovary, and no use of oral contraceptives or hormone replacement therapy within the 3 mo preceding the interview. Of eligible women, 51% (n = 3,302) enrolled in the SWAN study. Of these, 1,383 were at one of the three sites used in this analysis: Newark, Oakland, and Los Angeles. Out of this sample, we excluded 41 white women who were not born in the United States and 162 for having missing data. We compared the nonwhite women (n = 112) who were excluded due to missing data from the 695 nonwhite women included in the sample and found that there were differences in some of the covariate categories. Specifically, those with missing data were less educated and less likely to have a job, but there was no difference by age or likelihood of reporting any sleep problem.
Many of the individuals in our sample completed the survey in another language: Spanish, Japanese, or Cantonese. Professional translators at each site both forward-translated and back-translated all questions, with resolution of discrepancies through conversation with the professional translators. In the case of Spanish language translation, the professional translators used the most “universally” used linguistic translations, despite that fact that there is a range of usages across the heterogeneous countries of origin for the Hispanic women in the sample.
Outcome Variable: Sleep Complaints
The baseline interview asked four questions about sleep complaints that were adapted from the Women's Health Initiative Insomnia Rating Scale.26,27 The scale asked about difficulty falling asleep (“Did you have trouble falling asleep?”), awakenings (“Did you wake up several times a night?”), difficulty returning to sleep (“Did you wake up earlier than you had planned to, and were unable to fall asleep again?”), and typical sleep quality (“Overall, How was your typical night sleep during the past 2 weeks:”). For the first three items, participants were asked about the frequency with which they had experienced any of these complaints in the preceding 2 weeks, ranging from (1) no, not in the past 2 weeks to (5) yes, five or more times per week. Each item was dichotomized to 1 if it occurred three or more times per week, consistent with prior studies on insomnia.28,29 The question on “typical night's” sleep quality was scored on a scale from (1) very restful to (5) very restless. Participants who coded sleep as either a (4) restless or (5) very restless, were coded as 1, and the remainder were coded as 0. We then created a dichotomous variable for any sleep complaint, if any of the sleep complaints were coded as 1 (i.e., difficulty falling asleep, awakenings, inability to return to sleep, or poor typical sleep quality). Consistent with insomnia criteria, women who scored a 1 on any of the symptoms were coded as having a significant sleep complaint, whereas others were coded as not having a sleep complaint. We also analyzed the data in which each sleep complaint was assessed separately.
Primary Focal Variable: Immigrant Status
Our immigrant status variable was composed of three categories: first-generation immigrant, US-born nonwhite, and US-born white. The question, “Were you born in the United States?” was asked in an interviewer-administered questionnaire, and followed with a question about where the participants were born and their age when they immigrated. The mean age of immigration of the first-generation immigrants in this sample is 25.8 y.
Mediating Variable: Acculturation
To measure acculturation, we used four questions about language competence acculturation from the Marin acculturation scale.30 Although the Marin acculturation scale was developed and validated for use in Hispanic/Latino populations,30 the Marin acculturation scale's assessment of language competence among Asian Americans is also useful. It is a stronger predictor of psychosocial adjustment than other domains of acculturation.31 Language acculturation scales have been deemed valid and reliable in multiple immigrant populations, including those with both Hispanic and Asian origins.14,15,32,33 The four questions asked were: (1) In general, what language do you read and speak, (2) In what language do you usually think? (3) What language do you usually speak with your friends? and (4) What is/are the language(s) of the radio or TV programs you prefer to watch? For each question, there was a range of five options relevant for the participants' other language (Japanese, Chinese, or Spanish). For example, for Chinese women, the person's “other language” answer options read: “Only English (1),” “English more often than Chinese (2),” “Both Chinese and English equally (3),” “Chinese more often than English (4),” or “Only Chinese (5).” The answers were reverse coded and summed and coded such that there was a range of 4-20, with 20 being the most acculturated. For example, if the participant answered “Only English (1)” for all four questions regarding language acculturation, she was considered to be fully acculturated. If she answered “Only Chinese (5)” for all four questions regarding language acculturation, she was considered to have no language acculturation. A review article of acculturation measures describes this scale as having “good psychometric properties, covering multiple domains, and being frequently used.”34
Other Covariates
We included covariates for sociodemographic factors (menopausal status and education level [less than high school, high school, and more than high school]), employment (a dichotomous variable for employed or not), number of live children ever born (a continuous variable), whether the woman lives alone, and geographic location. Menopausal status was divided into two categories, premenopausal and early perimenopausal, with those in the perimenopausal group reporting that compared to one year ago, the number of days between the start of one menstrual period and the start of the next one had become less predictable. We also included indices of mental health (depressive symptoms), physical health (body mass index [BMI]), and health behaviors (smoking status, active living index, daily caffeine consumption, use of sleep medication, and use of folk medicine). Depression was measured using a continuous scale created from 19 items from the 20-item Center for Epidemiologic Studies of Depression (CES-D) scale.35 We subtracted the response to the item, “My sleep was restless”, from the sum of the remaining 19 items to avoid overadjustment for sleep problems, so the total score ranged from 0 to 57. BMI was calculated using measured weight in kilograms divided by measured height in meters squared, and was treated as a continuous variable. The active living index was created based on the average of two questions, during the past year, ‘Did you watch television?’ on a reverse coded scale of 1-5 where 1 is never or less than 1 h per week and 5 is more than 4 h per day, and “Did you walk or bike to and from work, school or errands?” on a scale of 1 to 5, where 1 is never or less than 5 min per day and 5 is more than 45 min per day. Smoking status was measured dichotomously and daily dietary caffeine intake was measured continuously (in milligrams) and was estimated from a food frequency questionnaire. As for sleep medication, we combined all reported medications that could plausibly be used for sleep (over-the-counter sleep medication, using medication for a “nervous condition,” and using barbiturates) into a dichotomous variable (yes/no to any one of these medication categories). Folk medicine was treated as a dichotomous variable in response to the question, “In the past 12 mo, have you used any of the following for any reason, folk medicine or traditional Chinese medicine?”
We did not include age as a covariate because it was collinear with other covariates (the variance inflation factor was > 10). Similarly, indices of physical activity, social functioning, emotional functioning, and social support36 were highly collinear with other covariates, so we did not include them.
Data Analysis
First we characterized the sample by providing the mean values for all individual variables for the total sample, and then for each variable stratified by immigrant status. We then used Pearson chi-square tests for categorical variables and analysis of variance for continuous variables to compare whether means varied by immigrant status.
We estimated a series of nested logistic regressions that predicted the outcome of “any sleep complaint.” Model 1 adjusted only for sociodemographic variables (education, racial/ethnic category, and menopausal status). Model 2 added adjustment for health and well-being variables (active living index, caffeine intake, employment status, live-alone status, number of children, BMI, smoking, depression, use of folk medicine, and sleep medication) variables. Model 3 added the language acculturation variable. We then used the MedEff module37,38 in Stata 12.0 to statistically test the extent to which language acculturation may mediate the association between immigrant status and sleep complaints. In ancillary analyses not shown, we repeated all aforementioned analyses with each sleep complaint as a separate outcome to determine if a specific sleep complaint was driving the effect. In addition, we tested for an interaction between race/ethnic category and immigrant status, but we failed to find a significant interaction, P values > 0.10. Specifically, the P values on the interaction terms with immigration status were P = 0.68 and P = 0.54 with Japanese and Hispanic/Latina women, respectively, compared to Chinese women. Thus, there were no statistically significant differences by race/ethnicity, but the stratified results are presented in the following paragraphs.
We used Stata 12.0 to conduct all analyses. P values < 0.05 were considered significant. We tested for collinearity after estimating all models using the variance inflation factor command available in Stata 12.0, and excluded the variables (e.g., social support and age) that were highly collinear with other variables.
RESULTS
Table 1 reveals that of the 695 first-generation and US-born women of Hispanic/Latina, Chinese, and Japanese races/ethnicities and 485 US-born white women at the three sites, the mean age of the analytic sample was 45.8 y (standard deviation = 2.7). The total number of first-generation immigrants was 410, 35% of the analytic sample. Among the nonwhites, the sample was 28% Hispanic/Latina, 33% Chinese, and 39% Japanese.
Table 1.
Descriptive statistics of the sample total and stratified by immigrant status (n = 1,180) (presented as percentages for dichotomous variables and as means with standard deviations in parentheses for continuous variables)
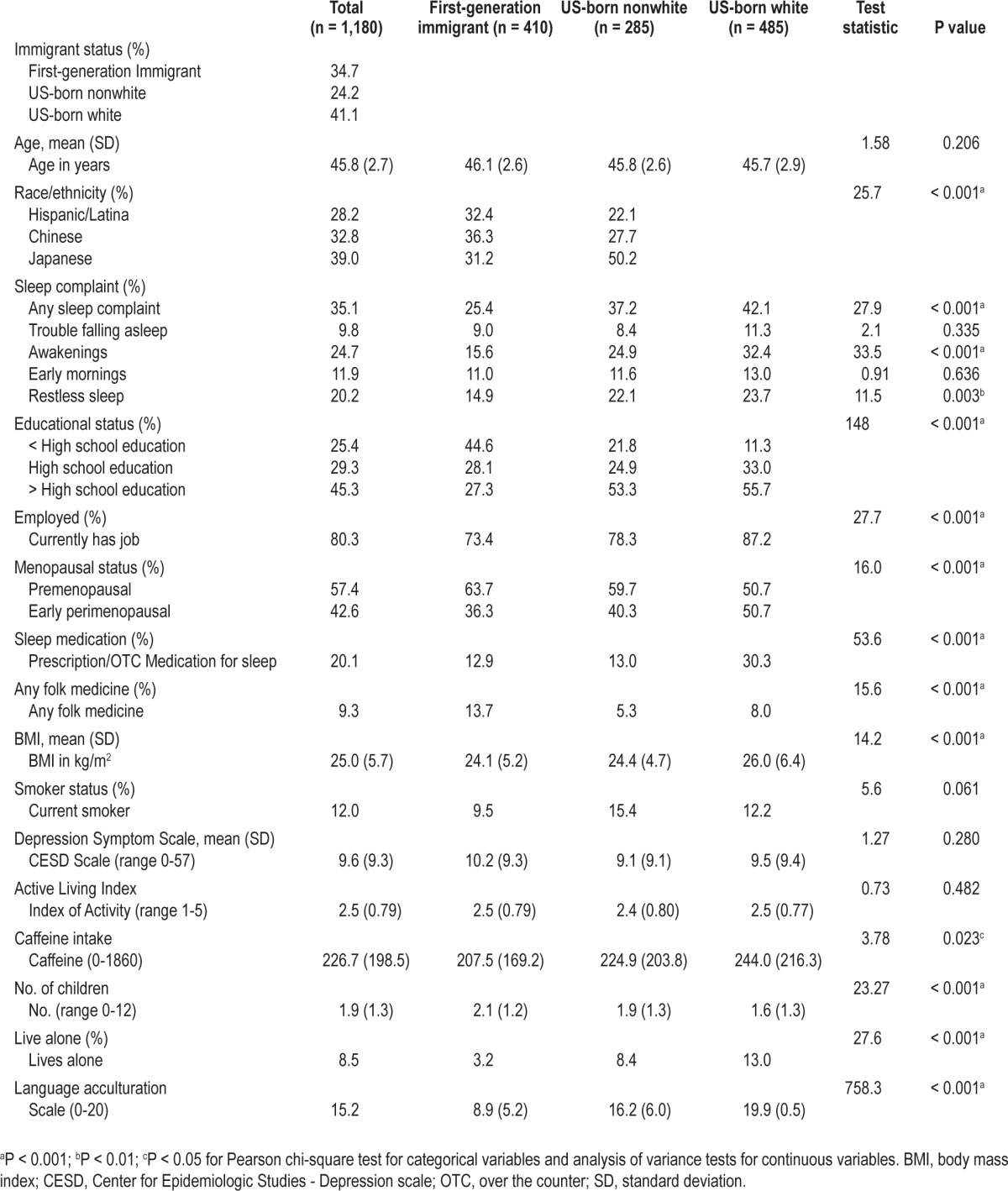
Approximately 25% of the first-generation immigrants reported any sleep complaint, compared to 37% of the US-born nonwhite women and 42% of the US-born white women (P < 0.001). Across the sample, nocturnal awakenings were the most common sleep complaint (25%); US-born white women were most likely to report nocturnal awakenings (32%), with US-born nonwhite respondents more likely to report nocturnal awakenings (25%) than first-generation immigrants (16%) (P < 0.001). Approximately 20% of the sample reported that their typical night's sleep was restless or very restless, with US-born white respondents reporting the highest prevalence (24%), followed by the US-born nonwhites (22%), followed by the first-generation immigrants (15%) (P < 0.01).
Approximately 45% of the sample had more than a high-school education, with a disproportionate number of the more highly educated being US-born (53%-56%) as compared with first-generation immigrants (27%) (P < 0.001). Approximately 13% of the nonwhite sample reported using any medication that affects sleep, with 30% of the US-born whites reporting use of such medications (P < 0.001). There were also statistically significant differences by immigrant status by menopausal status, employment status, BMI, caffeine intake, use of folk medicine, number of live children ever born, and whether the respondent lives alone.
The acculturation scale revealed that the first-generation immigrants were the least acculturated (with a score of 8.9 out of 20); the US-born nonwhites were more acculturated with a score of 16.2, and not surprisingly, the US-born whites had mean acculturation score of 19.9, with only 10 of the 485 US-born white respondents reporting anything other than full English language usage.
As demonstrated in Table 2, we observed that both US-born nonwhites and US-born whites had increased odds of reporting any sleep complaint (OR = 2.1, 95% CI 1.5-3.0 and OR = 2.6, 95% CI 1.9-3.6) compared to first-generation immigrants with adjustment for sociodemographic characteristics (Model 1). These associations changed slightly after adjustment for additional social and health variables (OR = 2.2, 95% CI 1.5-3.2 and OR = 2.3, 95% CI 1.6-3.4, respectively) (Model 2). With the addition of the language acculturation variable (in Model 3), we found significant attenuation of the ORs (OR = 1.6, 95% CI of 1.0-2.5 and OR = 1.5, 95% CI 0.9-2.4, respectively). Results of the MedEff command in Stata show that language acculturation or unmeasured factors associated with language acculturation mediated 40.4% (95% CI 28.5%-69.8%) of the association between immigrant status and any sleep complaint.
Table 2.
Results of logistic regression models predicting any sleep complaint in the past 2 weeks (n = 1,180)
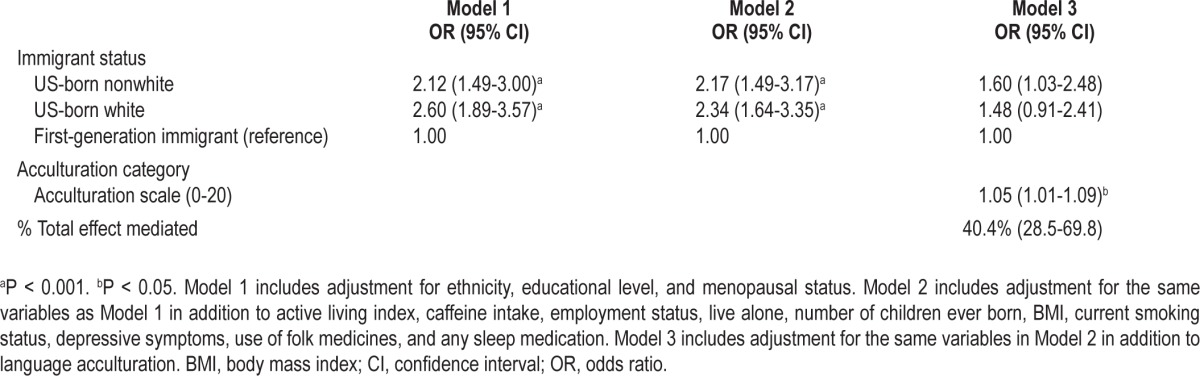
In separate analyses for each sleep complaint (trouble falling asleep, awakenings, waking too early and not being able to fall asleep, and restless or very restless typical night sleep), we found that immigrant status was significantly associated with two of the sleep complaints, awakenings, and restless typical night sleep (not shown). Both US-born white women and US-born nonwhite women were significantly more likely, by approximately 64%-90% increased odds, to report restless or very restless sleep and regular awakenings in the night compared to first-generation immigrants, even after adjustment for all variables included in the full model.
Several of the covariates were associated with increased sleep complaints. BMI and depressive symptoms were positively associated with reporting any sleep complaints, whereas being premenopausal was associated with fewer sleep complaints compared with being early perimenopausal.
In Table 3 we show the results of the analyses stratified by race/ethnicity, in which, again, among all three nonwhite groups, the US-born women were more likely to report sleep complaints than their first-generation immigrant counterparts. For both Hispanics and Japanese patients, substantial attenuation occurred with the addition of the acculturation scale. For Chinese women, we did not see attenuation with the addition of the acculturation variable.
Table 3.
Results of logistic regression models predicting any sleep complaint in the past 2 weeks, stratified by race/ethnicity.
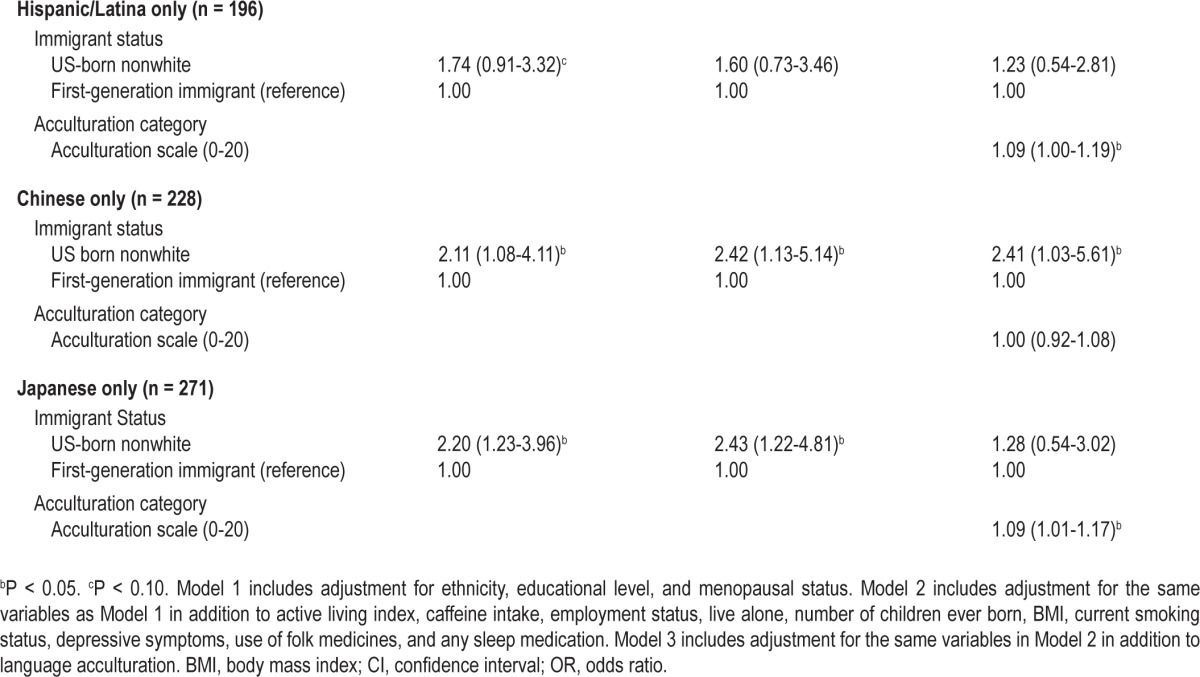
DISCUSSION
The results of this analysis confirmed our primary hypothesis and prior research that US-born whites and nonwhites have higher rates of sleep complaints than first-generation immigrants. This research builds on the extant literature by including additional races/ethnicities, Chinese and Japanese, compared to prior US research primarily conducted with Hispanics/Latinos. The magnitude of the association we observed was substantial, with an approximately twofold increased odds of the US-born women reporting a sleep complaint for the three race/ethnic groups (P < 0.001) in comparison with first-generation immigrants. There was no statistically significant interaction with race/ethnicity. The effect size was smaller and not significant for Hispanics (the smallest population) (OR = 1.74, 95% CI 0.91-3.32), whereas the effect sizes for Chinese and Japanese women were each significant (OR = 2.11, 95% CI 1.0-4.11 and OR = 2.20, 95% CI 1.23-3.96, respectively). Although our results counter the possible expectation that the stress of being a first-generation immigrant may interfere with sleep quality, this finding is consistent with prior research on health behaviors6,7 and specifically sleep4,5,13 among Hispanic/Latina immigrant populations. The two sleep complaints that appear to be driving the association between immigrant status and any sleep complaint are multiple awakenings and reporting a typical night's sleep as restless or very restless, which are also the most common sleep complaints and also differ significantly between immigrant groups.
As stated in our second research hypothesis, we expected that the association between immigrant status and sleep complaints would persist after adjustment for sociodemographic and health variables. Whereas a prior analysis of sleep patterns in Mexican-American populations found that adjusting for health behaviors accounted for differences in sleep duration between first-generation and US-born Mexican Americans, no such attenuation was found in these models. As expected, BMI and depressive symptoms were directly associated with increased odds of having any sleep complaints; however, they did not explain the differences in reporting sleep complaints by immigrant status. Some investigators suggest that immigrants as a group may be healthier than those who remain in their country of origin (labeled the healthy immigrant effect). Perhaps motivation for emigration includes the promise of a better life in the United States, with expectations of better neighborhoods and environments in which to live, work, and sleep. Thus, first-generation immigrants may be less likely to recognize a variety of minor symptoms, including sleep complaints, compared to those who are later- generation immigrants who have adapted to the United States. Although differences in attitudes and beliefs among immigrants and nonimmigrants may exist, we do not think the healthy immigrant effect accounts for all of our results, given that we adjusted for multiple health behaviors, depression, and health-relevant outcomes.
Our third research hypothesis posited that language acculturation would mediate the association between immigrant status and reduced sleep complaints. Four conditions39,40 have been met that support the hypothesis that language acculturation mediates the association between immigrant status and sleep complaints. First, immigrant status was associated with sleep complaints (Model 1). Second, immigrant status was associated with language acculturation (Table 1). Third, language acculturation was associated with sleep complaints after controlling for immigrant status (Model 3). Finally, after we adjusted for language acculturation in Model 3, we found partial attenuation of the association between immigrant status and sleep complaints when all of the race/ethnicities were aggregated. These results, along with the percentage of total effect-mediated results, were consistent with mediation such that being more acculturated may be pertinent to understanding why US-born immigrants are more likely than first-generation immigrants to report sleep complaints. When the analyses were stratified by race/ethnicity (and consequently lower power), we found significant mediation for Hispanic and Japanese women but not for Chinese women. The lack of mediation by acculturation among the Chinese sample probably reflects that the underlying sources of the association between immigrant status and sleep complaints in the Chinese women is different from that of the Hispanic and Japanese women.
The current analysis was unable to address the causal association between immigrant status, acculturation, and sleep complaints. Future research should thus investigate how sleep complaints change from the time an immigrant arrives in the United States throughout their acculturation process to understand the temporal sequencing of the onset of sleep complaints (i.e., before or after) in relation to becoming fully acculturated. Another important limitation is that the data on sleep complaints were self-reported and thus may be influenced by expectations about what constitutes trouble sleeping; the lack of a rigorous definition of sleep quality presents significant challenges.41 Differences in expectations may be affected by cultural norms about sleep quality and by language acculturation directly, due to variation in the interpretation of questions by language of the respondent. There is also the potential for misclassification of the acculturation variable, which might affect the results, especially if the misclassification is differential by immigrant status. Given the validation studies of the scale we used, we do not have reason to suspect high levels of misclassification.34 A related concern is that the question about the use of sleep medications (both prescription and over-the-counter) may not be interpreted by some to include folk remedies. To address this concern, we included a variable for those who reported taking any folk medicine (to treat sleep or other ailments).
Although we have no evidence to support misreporting on the immigrant variable (and the majority of our nonwhite sample reported being first-generation immigrants), there is a concern that participants were anxious about reporting their country of birth if they were not legal. The study did not verify country of birth (or ask about legal status). Further, even though we adjusted for a range of relevant confounders, there are likely unmeasured confounders that could be driving the observed associations.
We acknowledge that the category of Hispanics/Latinas is a very heterogeneous one, as seen in our sample. Although we have information on where the individuals (and their parents) were born, we do not have a large enough sample size to conduct statistical analyses by country of origin. For example, of the 196 Hispanic/Latina women in the sample, the largest representation are from Colombia (30), Cuba (32), Dominican Republic (38), Puerto Rico (35), and Ecuador (19), with multiple other countries represented (Argentina, Chile, El Salvador, Honduras, Italy, Peru, Mexico, Guatemala, and Spain). Given the wide range of countries of origin, the women in the sample are unlikely to have a similar cultural heritage, even though they have all been self-classified as Hispanic/Latina. Future research should seek to understand if the sleep complaints vary by country of origin within the category of Hispanic/Latina.
A further limitation is that these analyses were conducted on data from women with a very limited age range, and we do not know if the findings generalize to men.
To date, very limited research has been conducted comparing cultural differences in sleep patterns around the world. One study, which surveyed more than 35,000 people from 10 countries (but not the United States) found that reports of poor sleep vary dramatically by country.42 Based on the respondent's self-assessments, approximately 32% of them had insomnia, but this varied by country with a range from 17.4% in Germany to 79.8% in Brazil based on the countries studied.42 There were also national differences in how residents managed the sleep problems, with low rates of medication reported in Japan (15.3%) and Austria (9.8%) and much higher rates in Portugal (45.7%) and South Africa (52.8%). As noted previously, we found that US-born whites were more than twice as likely to report sleep medication use compared to the three racial/ethnic groups included in these analyses. The relatively low number of participants reporting use of a sleep medication among the three racial/ethnic groups included in this study may reflect more limited access to health care in these populations or different methods of coping with insomnia symptoms.
The consistent finding that immigrants (from three racial/ ethnic populations) to the United States have fewer sleep complaints than their US-born counterparts raises questions about the contextual and cultural causes of poor sleep. On the one hand, we know that there are individual factors (i.e., education, ethnicity, employment)1,18 that may affect sleep quality and duration; on the other hand, we are less clear about the factors that may affect sleep at a contextual level (e.g., neighborhood noise, light, sense of safety/security, or cultural influences). Although there is growing evidence that neighborhood context is important for sleep quality,43–45 we have only a limited understanding of the cultural dimensions of sleep. Studying first-generation immigrant populations and comparing their sleep to their US-born counterparts (white and nonwhite) may provide a key into understanding the high prevalence of sleep complaints in the United States. It may help explain dimensions of the root causes of sleep complaints and thus lead to opportunities to improve both sleep and sleep's downstream effects on health and functioning. These findings also have clinical implications by encouraging healthcare practitioners to pay attention to the sleep health of racial/ethnic minority populations, especially as they become more acculturated and may develop heightened risk of sleep complaints. Finally, these analyses hold implications for the larger literature on immigrant health and acculturation. Sleep, like many other health behaviors, appears to be better among first-generation immigrants than among more acculturated ones. Although socioeconomic opportunities may draw immigrants to the United States, numerous studies indicate that as immigrants acculturate into an American lifestyle, they often take on undesirable health profiles, including poorer quality sleep.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The Study of Women's Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women's Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495). Wendy Troxel is supported by K award HL093220. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH.
Clinical Centers: University of Michigan, Ann Arbor – Siobán Harlow, PI 2011-present, MaryFran Sowers, PI 1994-2011; Massachusetts General Hospital, Boston, MA – Joel Finkelstein, PI 1999-present; Robert Neer, PI 1994-1999; Rush University, Rush University Medical Center, Chicago, IL – Howard Kravitz, PI 2009-present; Lynda Powell, PI 1994-2009; University of California, Davis/Kaiser – Ellen Gold, PI; University of California, Los Angeles – Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011-present, Rachel Wildman, PI 2010-2011; Nanette Santoro, PI 2004-2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994-2004; and the University of Pittsburgh, Pittsburgh, PA – Karen Matthews, PI.
NIH Program Office: National Institute on Aging, Bethesda, MD – Winifred Rossi 2012-present; Sherry Sherman 1994-2012; Marcia Ory 1994-2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center: University of Pittsburgh, Pittsburgh, PA – Maria Mori Brooks, PI 2012-present; Kim Sutton-Tyrrell, PI 2001-2012; New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995-2001.
Steering Committee: Susan Johnson, Current Chair; Chris Gallagher, Former Chair The authors thank the study staff at each site and all the women who participated in SWAN.
REFERENCES
- 1.Hale L, Do DP. Racial differences in self-report of sleep duration in a population-based study. Sleep. 2007;30:1092–9. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 3.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 4.Hale L, Do DP, Rivero-Fuentes E. What do we know about Mexican immigration and Sleep? A population-based study and future directions. Hispanic Health Care International. 2010;8:199–208. [Google Scholar]
- 5.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2011;13:402–7. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 6.Argeseanu Cunningham S, Ruben JD, Narayan KM. Health of foreign-born people in the United States: a review. Health Place. 2008;14:623–35. doi: 10.1016/j.healthplace.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 9.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 10.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 11.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 12.Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48:904–11. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- 13.Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic Paradox. Sleep. 2011;34:1021–31. doi: 10.5665/SLEEP.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heilemann MV, Choudhury SM, Kury FS, Lee KA. Factors associated with sleep disturbance in women of Mexican descent. J Adv Nurs. 2012;68:2256–66. doi: 10.1111/j.1365-2648.2011.05918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kachikis AB, Breitkopf CR. Predictors of sleep characteristics among women in southeast Texas. Womens Health Issues. 2012;22:e99–109. doi: 10.1016/j.whi.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Voss U, Tuin I. Integration of immigrants into a new culture is related to poor sleep quality. Health Qual Life Outcomes. 2008;6:61. doi: 10.1186/1477-7525-6-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voss U, Tuin I. Relationship of sleep quality with coping and life styles in female Moroccan immigrants in Germany. Womens Health Issues. 2008;18:210–6. doi: 10.1016/j.whi.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27:205–11. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 19.Kageyama T, Kabuto M, Nitta H, et al. A population study on risk factors for insomnia among adult Japanese women: a possible effect of road traffic volume. Sleep. 1997;20:963–71. [PubMed] [Google Scholar]
- 20.Kappler C, Hohagen F. Psychosocial aspects of insomnia. Results of a study in general practice. Eur Arch Psychiatry Clin Neurosci. 2003;253:49–52. doi: 10.1007/s00406-003-0406-9. [DOI] [PubMed] [Google Scholar]
- 21.McLaughlin Crabtree V, Korhonen JB, Montgomery-Downs HE, Jones VF, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6:319–24. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Nordin M, Knutsson A, Sundbom E. Is disturbed sleep a mediator in the association between social support and myocardial infarction? J Health Psychol. 2008;13:55–64. doi: 10.1177/1359105307084312. [DOI] [PubMed] [Google Scholar]
- 23.Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner HL, Redline S. Effects of the home environment on school-aged children's sleep. Sleep. 2005;28:1419–27. doi: 10.1093/sleep/28.11.1419. [DOI] [PubMed] [Google Scholar]
- 24.Williams SJ. Sleep and society: sociological ventures into the (un)known. London, England: Routledge, Taylor and Francis Group; 2005. [Google Scholar]
- 25.Sowers MF, Crawford MP, Sternfeld B. SWAN: A multi-center, multi-ethnic, community-based cohort study of women and the menopausal transition. In: Lobo R, Marcus R, Kelsey J, editors. Menopause. New York: Academic Press; 2000. [Google Scholar]
- 26.Levine DW, Kripke DF, Kaplan RM, et al. Reliability and validity of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15:137–48. doi: 10.1037/1040-3590.15.2.137. [DOI] [PubMed] [Google Scholar]
- 27.Levine DW, Kaplan RM, Kripke DF, Bowen DJ, Naughton MJ, Shumaker SA. Factor structure and measurement invariance of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15:123–36. doi: 10.1037/1040-3590.15.2.123. [DOI] [PubMed] [Google Scholar]
- 28.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 29.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 30.Marin G, Sabogal F, Marin BV, Oterosabogal R, Perezstable EJ. Development of a Short Acculturation Scale for Hispanics. Hispanic J Behav Sci. 1987;9:183–205. [Google Scholar]
- 31.Kang SM. Measurement of acculturation, scale formats, and language competence - Their implications for adjustment. J Cross Cult Psychol. 2006;37:669–93. [Google Scholar]
- 32.Deyo RA, Diehl AK, Hazuda H, Stern MP. A simple language-based acculturation scale for Mexican Americans: validation and application to health care research. Am J Public Health. 1985;75:51–5. doi: 10.2105/ajph.75.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tran TV. Language acculturation among older Vietnamese refugee adults. Gerontologist. 1990;30:94–9. doi: 10.1093/geront/30.1.94. [DOI] [PubMed] [Google Scholar]
- 34.Celenk O, Van de Vijver F. Assessment of acculturation: issues and overview of measures. Online Readings in Psychology and Culture. 2011;8(1) http://dx.doi.org/10.9707/2307-0919.1105. [Google Scholar]
- 35.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:384–401. [Google Scholar]
- 36.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 37.Hicks R, Tingley D. Mediation: Stata module for causal mediation analysis and sensitivity analysis. 2012. http://econpapers.repec.org/software/bocbocode/s457294.htm.
- 38.Hicks R, Tingley D. Causal mediation analysis. Stata J. 2011;11:1–15. [Google Scholar]
- 39.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 40.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9(Suppl 1):S10–7. doi: 10.1016/S1389-9457(08)70011-X. [DOI] [PubMed] [Google Scholar]
- 42.Soldatos CR, Allaert FA, Ohta T, Dikeos DG. How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med. 2005;6:5–13. doi: 10.1016/j.sleep.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 43.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51:275–8. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 44.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: Testing a model of structural amplification. Health Place. 2009;15:1006–13. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 45.Hale L, Hill TD, Friedman E, et al. Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]


