Abstract
Francisella tularensis is a Gram-negative immune-evasive coccobacillus that causes tularemia in humans and animals. A safe and efficacious vaccine that is protective against multiple F. tularensis strains has yet to be developed. In this study, we tested a novel vaccine approach using artificial pathogens, synthetic nanoparticles made from catanionic surfactant vesicles that are functionalized by the incorporation of either F. tularensis type B live vaccine strain (F. tularensis LVS [LVS-V]) or F. tularensis type A Schu S4 strain (F. tularensis Schu S4 [Schu S4-V]) components. The immunization of C57BL/6 mice with “bare” vesicles, which did not express F. tularensis components, partially protected against F. tularensis LVS, presumably through activation of the innate immune response, and yet it failed to protect against the F. tularensis Schu S4 strain. In contrast, immunization with LVS-V fully protected mice against intraperitoneal (i.p.) F. tularensis LVS challenge, while immunization of mice with either LVS-V or Schu S4-V partially protected C57BL/6 mice against an intranasal (i.n.) F. tularensis Schu S4 challenge and significantly increased the mean time to death for nonsurvivors, particularly following the i.n. and heterologous (i.e., i.p./i.n.) routes of immunization. LVS-V immunization, but not immunization with empty vesicles, elicited high levels of IgG against nonlipopolysaccharide (non-LPS) epitopes that were increased after F. tularensis LVS challenge and significantly increased early cytokine production. Antisera from LVS-V-immunized mice conferred passive protection against challenge with F. tularensis LVS. Together, these data indicate that functionalized catanionic surfactant vesicles represent an important and novel tool for the development of a safe and effective F. tularensis subunit vaccine and may be applicable for use with other pathogens.
INTRODUCTION
Francisella tularensis is a Gram-negative coccobacillus that causes the potentially lethal disease tularemia, and it has a history of being used as a bioterrorism agent (reviewed in references 1 and 2). There are multiple subspecies of F. tularensis, including F. tularensis subsp. holarctica (type B) and F. tularensis subsp. tularensis (type A). Unlike F. tularensis subsp. novicida, both F. tularensis type A and B strains are significant causes of human infection. F. tularensis subsp. holarctica is found in North America, Europe, and Asia, while the more virulent F. tularensis subsp. tularensis is found primarily in North America (1). F. tularensis Schu S4 is a highly virulent prototypic type A strain, with a 50% lethal dose (LD50) of <10 CFU in mice for intranasal/aerosol infections (3).
A live attenuated strain of F. tularensis holarctica was developed initially in the former Soviet Union and further attenuated in the United States (i.e., F. tularensis live vaccine strain [LVS]) (4). While previous clinical studies demonstrated the effectiveness of this vaccine against more virulent strains (5), it has not been licensed in the United States (reviewed in reference 6) due to concerns about its unknown molecular basis of attenuation (7, 8), phenotypic inconsistencies (4, 9), frequency of reversion to virulence (6), and inability to completely protect against some strains of F. tularensis (5, 10, 11). While F. tularensis LVS is attenuated for humans, it causes a lethal tularemia-like disease in rodents when acquired by certain routes of infection, making it a valuable experimental model for tularemia (4, 12).
F. tularensis is able to infect many cell types, but it is preferentially recovered from macrophages (13). F. tularensis has developed multiple mechanisms of immune evasion (reviewed in reference 14). For example, unlike typical lipopolysaccharide (LPS) species from Gram-negative bacteria, F. tularensis has an unusual tetraacylated lipid A structure that precludes the activation of Toll-like receptor 4 (TLR4) (15–17). F. tularensis is phagocytosed by macrophages, but phagosomes are only transiently acidified (14). Ultimately, F. tularensis escapes from macrophage phagosomes to replicate in the cytoplasm (18, 19). In the late stages of infection, F. tularensis triggers the apoptosis and pyroptosis of macrophages, allowing its release for the next cycle of infection (reviewed in references 2, 20, and 21), as well as the release of endogenous TLR ligands, interleukin-1 beta (IL-1β), and the subsequent recruitment of neutrophils (reviewed in references 22 and 23). Endogenous danger signals released by dying cells may contribute to the “cytokine storm” and pathology associated with tularemia (24).
Intact F. tularensis activates proinflammatory gene expression through multiple host receptors and signaling pathways, including TLR2, the absent in melanoma 2 (AIM2) inflammasome, and an unknown intracellular receptor that leads to the induction of beta interferon (IFN-β) (25–28), although the F. tularensis ligands responsible for this activation have not yet been fully defined (27–30). Diverse strains of F. tularensis limit the efficiency of complement-mediated opsonization (31), and for the highly virulent F. tularensis Schu S4 strain, opsonization by antibodies is significantly reduced due to its ability to bind plasmin (32). Furthermore, F. tularensis alters the differentiation of macrophages from a state that is proinflammatory (classical activation) to one that is anti-inflammatory (i.e., alternative activation [33]), resulting in a lack of production of proinflammatory cytokines and increased bacterial burden. In addition, the early (<48 h) suppression of host inflammatory responses by F. tularensis has been reported in pulmonary infections (reviewed in reference 34). Each of these microbial strategies facilitates F. tularensis survival in the host. The treatment of mice with monophosphoryl lipid A (MPL), a weak TLR4 agonist, prior to or concurrent with infection resulted in significant antibody-independent protection from F. tularensis LVS and Schu S4 infection (29). This clearly indicates the importance of the innate proinflammatory response in controlling F. tularensis infection.
Although immunization with certain attenuated mutant strains of F. tularensis protects against subsequent challenge (35–37), they raise safety concerns due to the potential for reversion to full virulence. Therefore, subunit vaccines are generally considered to be safer than live attenuated vaccines (38). Immunization with purified F. tularensis LVS LPS just 2 days before challenge with live F. tularensis LVS protected mice against challenge with F. tularensis LVS (29, 39, 40). This protection was mediated by the production of IgM produced by B1a cells (25, 39, 41) in a process completely independent of T cell help (39). However, this same F. tularensis LVS LPS immunization regimen failed to protect mice against F. tularensis Schu S4 challenge (29). Effective protection against F. tularensis LVS challenge, but not Schu S4 challenge, was also elicited by immunization with a combination of several F. tularensis antigens (e.g., Tul4 and DnaK) plus an adjuvant (42 and data not shown). Immunization with liposomes containing recombinant F. tularensis outer membrane protein FopA protected mice against both intradermal and intranasal F. tularensis LVS challenges but not Schu S4 challenge (43). In short, while immunization with some live attenuated strains protects against challenge with the virulent Schu S4 strains (44–46), subunit vaccination success has largely been confined to protection against the less virulent F. tularensis LVS strain.
We therefore sought to combine the efficacious immune-stimulating capability of a live attenuated vaccine with the safety profile of a subunit vaccine. Nanoparticles are becoming increasingly popular as slow-release drug delivery systems (reviewed in reference 47); however, no work has been published using catanionic vesicles for vaccine delivery. Catanionic vesicles resemble liposomes structurally but are synthesized from matched pairs of cationic and anionic surfactants rather than phospholipids, which are used as the membrane-forming component (48). Surfactant vesicles have the advantages of being inexpensive to produce, having a long shelf life, demonstrating ease of vesicle production, and having higher stability than that of liposomes (48, 49). We hypothesized that surfactant vesicles would enable us to deliver F. tularensis nanoparticles that are capable of stimulating protective immunity without the safety concerns associated with live bacterial immunizations. Herein, we report our initial findings using a novel surfactant vesicle F. tularensis subunit vaccine approach to induce high titers of anti-F. tularensis IgG that fully protected mice against F. tularensis LVS challenge. Importantly, we also demonstrate significant partial protection afforded by a Schu S4-vesicle vaccine against intranasal challenge with the highly pathogenic F. tularensis Schu S4 in mice. This new approach shows high potential against this immune-evasive pathogen and potentially provides a vaccine platform that is amenable to use with many other agents.
MATERIALS AND METHODS
Vesicle preparation and purification.
The vesicle preparation method was adapted from a protocol developed by Kaler et al. (48) and refined by Thomas et al. (50). F. tularensis LVS (strain ATCC 29864) was the kind gift of Karen Elkins (FDA, Bethesda, MD). To prepare cultures for vaccine preparation, the stocks were grown to mid-log phase in Mueller-Hinton broth (MHB) (Becton, Dickinson Microbiology Systems), supplemented with 1% IsoVitaleX (Becton, Dickinson), 0.1% glucose (Sigma), and 0.025% ferric pyrophosphate (Sigma) at 37°C, while shaking. F. tularensis Schu S4 (FSC237; BEI Resources) was grown in Trypticase soy broth (TSB) (Becton, Dickinson Microbiology Systems) supplemented with 0.1% l-cysteine hydrochloride (Sigma), 0.1% glucose (Sigma), and 0.1% ferric pyrophosphate (Sigma) at 37°C, while shaking. To prepare 10 ml of vesicles, 25 ml (or 3 to 100 ml for experiments measuring the effects of protein loading on vesicle size and stability) of overnight F. tularensis cultures (optical density at 600 nm [OD600], 0.4 to 0.6) was pelleted by centrifugation and lysed in a 7.07-g/liter solution of the anionic surfactant sodium dodecylbenzenesulfonate (SDBS) (Tokyo Chemical Company, Ltd., Tokyo, Japan) in ultrapure endotoxin-free water (Sigma, St. Louis, MO). After 1 h, 30 mg of the ethanol-acetone recrystallized form of the cationic surfactant cetyltrimethylammonium tosylate (CTAT) (Sigma) per 10 ml of lysed bacteria was added, for a 3:1 molar ratio of SDBS to CTAT, and the vesicles were allowed to self-assemble overnight at room temperature with stirring. At this point, Schu S4-V preparations were plated on Mueller-Hinton blood plates and kept at 37°C to ensure the sterility of the vaccine preparations for safe removal from the biosafety level 3 (BSL-3) laboratory. No colonies were detected on any of the plates (data not shown). The vesicle preparations were stored at 4°C during this time. To separate the vesicles from free surfactants and cellular debris, the vesicle preparations were centrifuged to pellet large detritus, and the resulting supernatant was purified by size exclusion chromatography over a column composed of 10 ml of washed and packed Sephadex G-100 (Sigma). The vesicles remained stable at 4 to 25°C for ≥5 months (data not shown). The protein content in the vesicles was determined by a modified version of the detergent-compatible (DC) protein assay with Reagent S (Bio-Rad, Hercules, CA), using bovine serum albumin (BSA) as a standard (Pierce, Rockford, IL). The vesicles varied in size, with radii ranging from 70 to 105 nm in bare vesicles and 80 to 120 nm in vesicles containing F. tularensis components, as determined by dynamic light scattering (DLS) with an LS-DYNA (Livermore Software Technology Corporation) set to a 90° angle, utilizing PhotoCore 5.3.8 analysis software for cumulants algorithm (51). Zeta potential was measured with a Malvern Zetasizer Nano ZS90, using phosphate-buffered saline (PBS) as an electrolyte source (52). Zeta potential measures surface charge on the vesicles and has been found to correlate with the stability of vesicles (M. T. Hurley and P. DeShong, unpublished data).
Immunization protocol and F. tularensis challenge.
Wild-type 6- to 8-week-old female C57BL/6 mice were purchased from Jackson Laboratories (Bar Harbor, ME) and housed in a specific-pathogen-free facility at the University of Maryland Baltimore, MD, and in the animal BSL-3 (ABSL-3) suite at the University of Virginia. The mice were immunized with either the F. tularensis LVS (LVS-V) or the F. tularensis Schu S4 (S4-V) vesicles (35 μg protein) by either intraperitoneal (i.p.), intranasal (i.n.), or subcutaneous (s.c.) routes, as indicated, up to three times in 2-week intervals, with the last dose administered 14 days prior to live bacterial challenge. Where indicated, the resting period between the immunization and challenge was extended from 14 to 28 days. As a negative control, the mice received bare vesicles made in endotoxin-free water in the absence of bacterial pellets but purified identically to LVS-V and S4-V. For passive immunization experiments, the mice received 60 μl pooled serum samples from naive mice or from vesicle- or LVS-V-immunized animals by the intravenous (i.v.) route 1 day prior to challenge. The mice were challenged by the i.p. route with up to 100,000 CFU F. tularensis LVS or by the i.n. route with up to 50 CFU F. tularensis Schu S4. The challenge doses of F. tularensis LVS used in these studies were determined prior to each experiment to kill ≥80% of unimmunized mice.
The mice were checked twice daily for clinical symptoms of F. tularensis infection for 21 days following challenge. Clinical scores were assigned as follows: for mice infected with F. tularensis LVS, a score of 0 was assigned for healthy mice with normal behavior (exploring cage, feeding, alert), 1 for mild illness (usually marked by lower activity and weight loss), 2 for mild-moderate illness (mice showing symptoms of score 1 plus piloerection), 3 for moderate-severe illness (mice showing symptoms of score 2 plus assuming a hunched posture), 4 for severe illness (mice showing symptoms of score 3 and minimal activity or blepharitis [crustiness around the eye] involving one or both eyes), 4+ for moribund illness (mice showing symptoms of score 3 and were nonresponsive to stimulation [these mice were euthanized]), and 5 for mice found dead in their cage. Mice with scores of 4+ and 5 were reported on the day of death only and were excluded from analysis on subsequent days. The arithmetic means ± the standard errors of the means (SEM) of the clinical scores were reported. For mice infected with the F. tularensis Schu S4 strain, a score of 0 was assigned for healthy mice with normal mouse behavior (exploring cage, feeding, alert), 1 for mild illness (decreased movement), 2 for moderate illness (decreased motion, eye closure), 3 for severe illness (motionless, eye closure, increased respirations, ruffled fur), and 4 for mice that were moribund (no motion in response to external stimuli plus meeting the criteria in reference 3) or dead. The moribund mice were euthanized.
To measure the blood serum antibody titers in F. tularensis LVS-infected mice, ∼200 μl blood was collected at the indicated intervals. Each mouse was euthanized and bled at the termination of the experiments. All animal experiments were conducted with Institutional Animal Care and Use Committee approval.
ELISA, silver stain, and Western blots.
Enzyme-linked immunosorbent assays (ELISAs) were performed as previously described (41). Briefly, ELISA plates were coated with 2 μg/ml purified lipopolysaccharide from F. tularensis LVS (F. tularensis LVS LPS) or with 5 × 107 CFU/ml F. tularensis LVS. After washing, the plates were blocked with 10% fetal bovine serum (FBS). The serum samples were serially diluted in 10% FBS and 0.05% Tween 20 and were added to the coated plates for 90 min at 37°C. After extensive washing, horseradish peroxidase (HRP)-conjugated secondary antibodies (SouthernBiotech) were added to the wells at a 1:20,000 dilution. Detection was achieved using the 2,2′-azinobis(3-ethylbenzthiazolinesulfonic acid) (ABTS) system (Sigma) and the plates were read on a universal microplate reader, ELx800 (Bio-Tek Instruments, Inc.). The data were analyzed in MS Excel; the antibody titers were defined as the serum dilution corresponding to an average OD value of 3 standard deviations above the background OD values. The data for each mouse were graphed on a logarithmic scale, and the geometric mean was calculated for each group of mice at each time point. The geometric means were graphed separately in Fig. 2D for easier comparison.
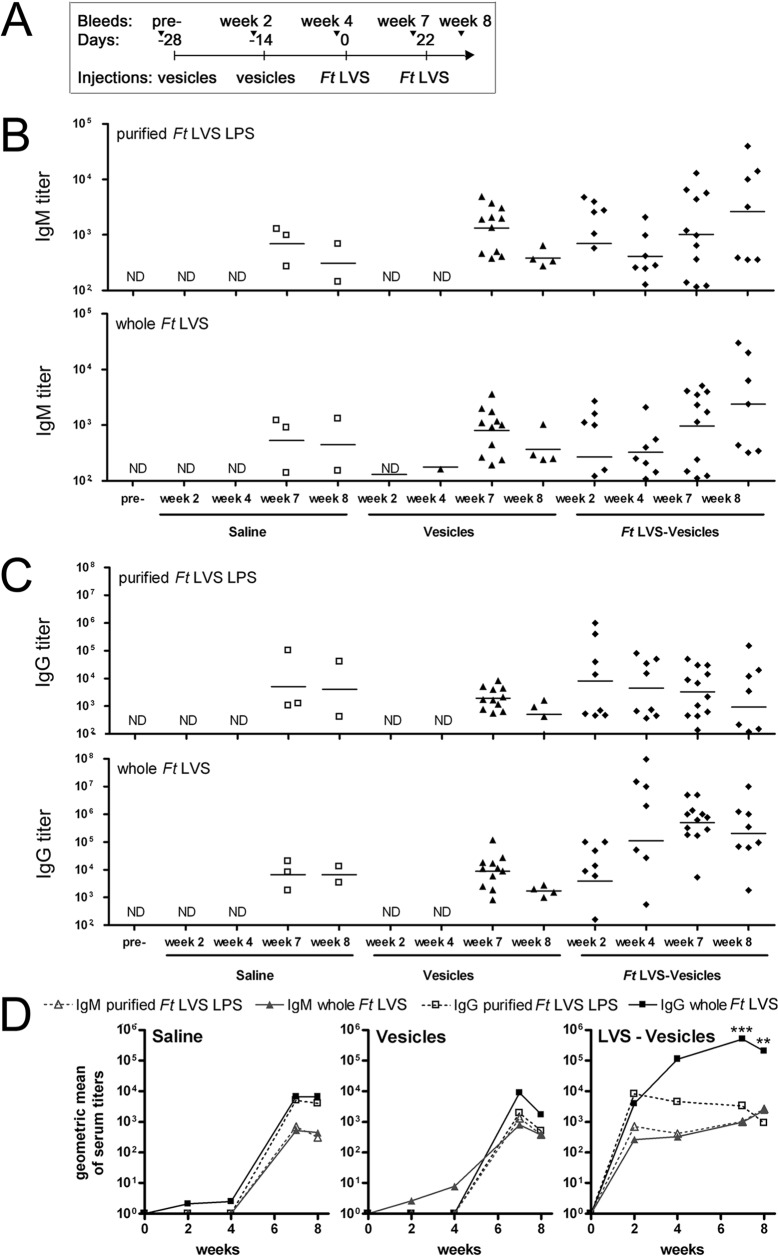
FIG 2.
LVS-V induce robust antibody responses where IgM is essentially all anti-LPS antibody and IgG is predominantly directed against non-LPS epitopes. (A) Schematic of immunization and bleeding schedule. The mice were immunized and challenged as described in Fig. 1. The mice were challenged again 22 days following the primary challenge to determine the effect on antibody responses. (B) ELISA data measuring F. tularensis-specific IgM. (C) ELISA data measuring F. tularensis-specific IgG (all subclasses). Microwell plates were coated with purified F. tularensis LVS LPS (top panels) or whole F. tularensis LVS bacteria (bottom panels) to distinguish between LPS-specific and overall anti-F. tularensis antibody levels. The titers are shown on a log scale. Each symbol represents one mouse. ND, none detected. (D) The geometric means of the ELISA titers detected in B and C were replotted for easier visual comparison between the antibody levels directed against whole F. tularensis LVS (filled symbols, solid lines) and those against purified F. tularensis LVS LPS (open symbols, dashed lines) in both IgG (■, black) and IgM (▲, gray) assays. **, P < 0.01; ***, P < 0.001.
Silver staining of membranes was performed as previously described (53). Briefly, vesicles and bacterial pellets were boiled in Laemmli sample buffer (with β-mercaptoethanol but without protease inhibitor cocktail) and separated by PAGE on Tris-glycine gels (12%, 10 to 20% gradient, or 4 to 20% gradient, as indicated) (Bio-Rad). The gels were fixed overnight in 40% ethanol, 0.5% glacial acetic acid, and washed for 5 min in 0.83% periodic acid (Sigma). After washing with water, the gels were stained with a basic solution of 0.8% silver nitrate (Sigma) for 15 min, washed extensively, and developed with 0.007% formaldehyde and 50 μg/ml citric acid for 10 min. The gels were washed with water, at which time they continued to develop and were scanned after 10 min.
For Western blots, vesicle and bacterial samples were boiled in Laemmli sample buffer and separated by PAGE as described above. The gels were transferred to an Immobilon-P membrane (Millipore) by wet transfer. The membranes were blocked in 5% milk in Tris-buffered saline-Tween 20 (TBST) (Bio-Rad). Pooled serum samples from LVS-V- or Schu S4-V-immunized mice were diluted 1:106 or 1:105, respectively, in 5% milk–TBST and incubated with the membranes overnight at 4°C or 2 h at room temperature (RT). The dilutions of anti-LVS-V or anti-Schu S4-V were based on preliminary experiments that optimized the detection of bands in the F. tularensis lysates. After washing, HRP-conjugated human adsorbed goat-anti-mouse IgG1, IgG2b, IgG2c, and IgG3 secondary antibodies (SouthernBiotech) were diluted 1:20,000 in 5% milk-TBST and incubated with the membranes for 60 min at RT. After extensive washing, the ECL Plus detection kit (GE Healthcare) was used to visualize the bands, which were recorded on BioMax MR film (Kodak). F. tularensis LPS-specific rabbit antibodies were kindly provided by Karen Elkins (FDA). Purified F. tularensis LVS DnaK and Tul4 were prepared as described previously (42).
Comparison of different F. tularensis strains by Western blot analysis.
F. tularensis strains Schu S4, MA00-2987, WY96-3418, KY99-3387, OR96-0246 (BEI Resources, Inc.) and F. tularensis LVS were grown in enriched TSB medium as described above. To estimate equal loading, each bacterial culture was grown overnight and was diluted to an OD600 of 0.300 prior to pelleting the bacteria and lysis in Laemmli sample buffer. PAGE, silver staining, and Western blot analysis were carried out as detailed above.
Real-time PCR.
To assess the initial inflammatory responses, each mouse was euthanized 4 h after the first i.p. immunization with saline, vesicles, or LVS-V. Total RNA was extracted from the liver samples, and real-time PCR analysis was performed as previously described (25). In this study, we report the relative gene expression normalized to the expression of mouse hypoxanthine phosphoribosyltransferase (HPRT). All primer pairs used in this study have been published (25). The cytokine protein levels were measured by the Cytokine Core Laboratory (University of Maryland Baltimore [UMB]).
Statistics.
The data were analyzed with GraphPad Prism 4 for Windows (GraphPad Software, Inc., San Diego, CA). Specific tests include Fisher's exact test for comparisons of survival at day 14 postchallenge, the log rank test for analysis of survival curves, the one-way analysis of variance (ANOVA), followed by a Tukey's post hoc test for analyses of multiple groups of data, and the Mann-Whitney test (nonparametric t test) for analyses of two groups of data.
RESULTS
Immunization with F. tularensis LVS LPS-V protects against F. tularensis LVS but not F. tularensis Schu S4 challenge.
We previously demonstrated that immunization with LPS from F. tularensis LVS (F. tularensis LVS LPS) only 2 days prior to live bacterial challenge fully protected mice against a lethal challenge with F. tularensis LVS (25, 29). This protection was attributable to B1a cell- and antibody-mediated responses (39). The same regimen did not protect against F. tularensis Schu S4 challenge (29), despite the fact that both F. tularensis LVS and F. tularensis Schu S4 share the same O antigen (54), and therefore, antibodies should be cross-protective. In an attempt to improve the effectiveness of F. tularensis LVS LPS as a vaccine, we initially incorporated the purified F. tularensis LVS LPS, with or without a promiscuous Th-cell epitope called PADRE (55), into catanionic vesicles that were used as a delivery system. PADRE was covalently modified at the N terminus with a C12 hydrophobic tail via amide linkage (C12-PADRE) to enable its coupling to the vesicles (see Supplemental Methods in the supplemental material for a detailed description of the chemical methods). Catanionic vesicles form when two surfactants with oppositely charged head groups and sufficiently long hydrophobic tails (≥C10) are combined in the appropriate ratio (i.e., a molar ratio of 3:1 is ideal for SDBS and CTAT) (48). Indeed, surfactant-based catanionic vesicles have been shown to be more stable than phospholipid-based vesicles (51, 56). Mice immunized with two doses of purified F. tularensis LVS LPS (as a positive control) or with catanionic vesicles functionalized with F. tularensis LVS LPS (±C12-PADRE), administered 2 weeks apart (see Fig. S1A in the supplemental material), survived i.p. challenge with F. tularensis LVS 2 weeks after final immunization (see Fig. S1B in the supplemental material; data not shown). However, no protection was seen when similarly immunized mice were i.n. challenged with F. tularensis Schu S4 (data not shown). A serum IgM anti-LPS antibody response was induced in immunized mice, which significantly increased following challenge, regardless of the immunogen used (see Fig. S1C in the supplemental material). The purified F. tularensis LVS LPS also induced a detectable serum IgG anti-LPS response (see Fig. S1C in the supplemental material). The levels of IgG1 antibodies were significantly reduced in the vesicle-immunized mice, and to a lesser extent, IgG3 levels were also reduced compared to the controls (see Fig. S1C in the supplemental material). Therefore, we sought a new approach that would lead to a subunit vaccine that would both increase the IgG response and protect against infection with F. tularensis Schu S4.
Immunization with F. tularensis LVS-vesicles elicits full protection against F. tularensis LVS challenge.
Since F. tularensis LVS LPS-V failed to protect against F. tularensis Schu S4 challenge, we next modified our catanionic vesicle system in an effort to develop an improved F. tularensis subunit vaccine. We hypothesized that immunization with a subunit vaccine that contained a diverse assortment of the F. tularensis ligands, including hydrophobic and amphiphilic bacterial molecules, as well as bacterial DNA, would enable concurrent engagement of multiple innate and adaptive signaling pathways. We theorized that a strong pathogen-specific inflammatory response, coupled with a specific high-titer IgG anti-F. tularensis antibody response, would protect not only against F. tularensis LVS challenge but also against F. tularensis Schu S4 challenge. To this end, we prepared control vesicles by combining anionic and cationic surfactants in endotoxin-free water (50). To prepare vesicles containing F. tularensis components, the anionic surfactant was first added to pelleted cultures of F. tularensis LVS or F. tularensis Schu S4 to lyse the bacteria, and then the cationic surfactant was added to produce vesicles that incorporated bacterial components from the bacterial lysates. The resulting F. tularensis nanoparticles are referred to as LVS-V and Schu S4-V, respectively. No living organisms grew on Mueller-Hinton blood plates after contact with anionic surfactant (data not shown). The vesicles were subsequently purified over a Sephadex G-100 column to separate free bacterial components and unincorporated surfactants from the vesicles prior to immunizing the mice.
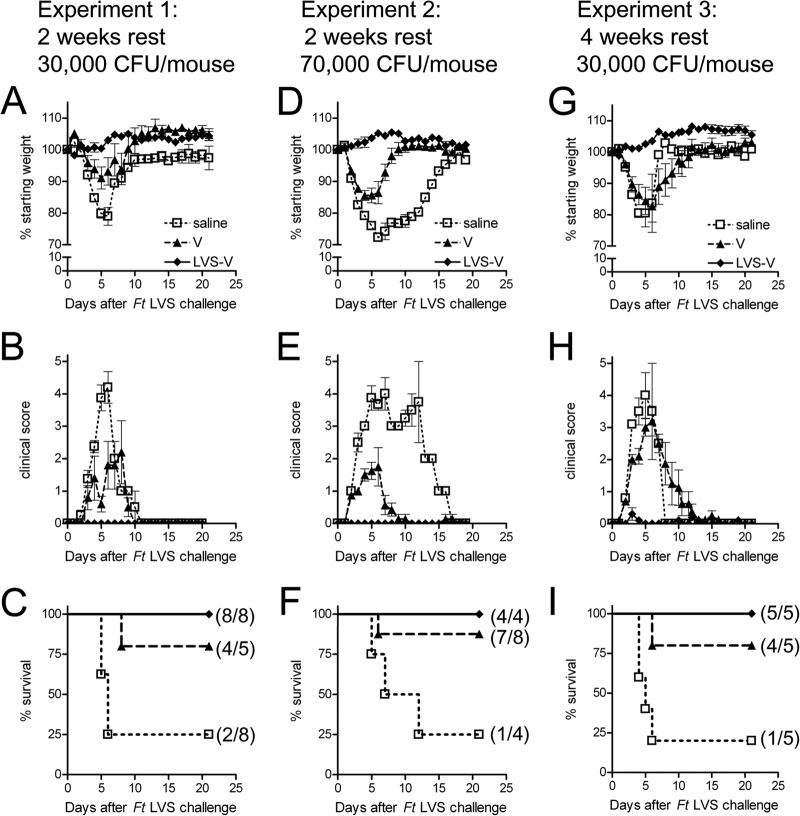
Initially, the mice were immunized twice by the i.p. route, 2 weeks apart, with sterile saline (as a control), LVS-V (35 μg protein), or an equivalent volume of bare vesicles as an additional control. Two weeks after the second immunization, all mice were challenged by the i.p. route with the indicated dose of F. tularensis LVS. Weight loss, clinical symptoms, and the survival of each mouse were monitored for 3 weeks. Figure 1 shows the results of two separate experiments at this immunization schedule, with challenge doses of 30,000 CFU F. tularensis LVS/mouse (Fig. 1A to C) or 70,000 CFU F. tularensis LVS/mouse (Fig. 1D to F). One experiment in which the resting period after immunization was extended to 4 weeks prior to challenge with 30,000 CFU F. tularensis LVS/mouse is also shown (Fig. 1G to I). In the saline-immunized groups, mice suffered rapid weight loss (Fig. 1A, D, and G) and exhibited infection-associated clinical symptoms (Fig. 1B, E, and H) starting on the second day after infection and either expired or started to recover 5 to 6 days after infection. Seventy-five to 80% of the mice immunized twice with saline and challenged with F. tularensis LVS died when challenged with 30,000 (Fig. 1C and I) or 70,000 CFU F. tularensis LVS (Fig. 1F). Immunization with LVS-V fully protected mice, as evidenced by the 100% survival rate at both challenge doses and the complete absence of weight loss and other clinical signs of disease, whether the resting time allowed between the final immunization and challenge was 2 weeks or 4 weeks (Fig. 1). Surprisingly, in both challenges carried out 2 weeks postimmunization, ≥80% of mice that were immunized with plain vesicles suffered only moderate weight loss during the peak infection period and survived F. tularensis LVS challenge (Fig. 1). Empty vesicle-immunized animals that were challenged 4 weeks after the second immunization exhibited more severe weight loss, similar to the saline controls (Fig. 1G), suggesting that the effect of bare vesicle immunization might wane by 4 weeks postimmunization, but in contrast to the saline controls, the majority of these animals recovered (Fig. 1I).
FIG 1.
LVS-V nanoparticles fully protect mice against F. tularensis (Ft) LVS challenge. (A to C) In experiment 1, mice were injected twice, 2 weeks apart (days −28 and −14), i.p. with sterile saline (◽, dotted line), LVS-V (35 μg protein) (◆, solid line), or the equivalent amount of vesicles (▲, dashed line). Two weeks after the second immunization, all mice were challenged i.p. with 30,000 CFU F. tularensis LVS per mouse. (D to F) In experiment 2, the challenge dose was increased to 70,000 CFU F. tularensis LVS per mouse. (G to I) In experiment 3, the time after final immunization was increased to 4 weeks. Everything else was kept the same as for experiment 1. In each experiment, the percent starting weight (A, D, and G), and the severity of tularemia symptoms (B, E, and H), ranging from 0 for healthy to 5 for dead (see Materials and Methods), and survival of the individual mice following challenge (C, F, and I) are shown.
LVS-V induced robust antibody responses, including isotype class switching.
To test whether immunization with LVS-V resulted in augmented humoral antibody responses, mice were immunized twice with saline, empty control vesicles, or LVS-V and challenged with 30,000 CFU F. tularensis LVS (challenge 1) by i.p. injection as described above, and then survivors, as well as a new group of saline-treated mice, were challenged i.p. with 50,000 CFU F. tularensis LVS (challenge 2) to determine if reexposure would boost antibody responses in mice previously exposed to F. tularensis antigens by immunization and/or by the first challenge. Blood serum samples were collected prior to each immunization and challenge, as well as 1 week following the second challenge (Fig. 2A), and the antibody titers were measured by ELISA. To assess the levels of serum antibody directed against LPS and non-LPS epitopes, ELISA plates were coated with either purified F. tularensis LVS LPS or whole F. tularensis LVS (Fig. 2B and C). Isotype-specific antibodies were detected with secondary antibodies against mouse IgM (Fig. 2B) or a cocktail of secondary antibodies against all four mouse IgG subclasses (Fig. 2C).
While no F. tularensis-specific IgM response was observed in mice immunized with saline or vesicles (weeks 2 and 4), a low but significant IgM titer followed live bacterial challenge (weeks 7 and 8). Only mice immunized with LVS-V produced detectable levels of F. tularensis-specific antibodies prior to live bacterial challenge: IgM titers were detected as early as 2 weeks after the first immunization and increased after challenge with live F. tularensis LVS (weeks 7 and 8). The IgM antibody titers were similar when assayed on plates coated with either purified F. tularensis LVS LPS or whole F. tularensis LVS (Fig. 2B), indicating that essentially all of the IgM produced was directed against the LPS.
Immunization with LVS-V, but not saline or bare vesicles, also induced antibody isotype switching to IgG. IgG titers were detectable 14 days after the first immunization, and were increased 2 weeks after the second immunization (Fig. 2C) when assayed by ELISA on plates coated with whole F. tularensis LVS. Notably, the prechallenge (week 4) antibody titers directed against whole bacteria exceeded anti-LPS IgG titers by >10-fold, indicating that the IgG responses were predominantly directed against non-LPS epitopes (Fig. 2D). Non-LPS-specific IgG antibodies remained strong and further increased to a titer of ∼106 following live bacterial challenge. Consistent with the responses to natural infections (12, 39), the antibody responses produced by immunization with saline or vesicles were detected only after live infection (week 7 and later) and were directed predominantly against the F. tularensis LPS. Thus, immunization of mice with LVS-V induces a strong IgG response to F. tularensis.
Passive immunization using serum samples from LVS-V-immunized mice protects against F. tularensis LVS challenge.
Since we observed high antibody titers following LVS-V immunization directed predominantly against non-LPS epitopes, we sought to test whether these antibodies would be protective in F. tularensis LVS challenge. Donor mice were immunized as described above with either saline, LVS-V, or vesicles. Two weeks following the second immunization, serum samples were harvested and pooled according to the immunogen the donor mice received. It is noteworthy that these mice were not challenged with F. tularensis LVS. F. tularensis-specific IgM and IgG titers were measured by ELISA. Similar to the data in Fig. 2, serum samples from LVS-V-immunized mice contained significantly elevated levels of F. tularensis-specific IgG when assayed by ELISA against whole organisms (Fig. 3A). Sixty microliters of each serum pool was administered to naive mice by i.v. injection. The recipient mice were challenged 24 h later with 100,000 CFU F. tularensis LVS per mouse by the i.p. route, and weight loss, clinical symptoms, and survival were recorded for each mouse over the course of 2 weeks. Mice that received serum from saline-immunized mice (control serum) expired in 4 to 6 days (Fig. 3D). Mice that received serum from LVS-V-immunized mice experienced essentially no weight loss and much less severe clinical symptoms than controls (Fig. 3B and C). Six of seven of these animals (86%) recovered in the second week following infection (Fig. 3C) (P = 0.0002 compared to control serum recipients). Mice that received serum from bare vesicle-immunized mice showed a slight delay in the onset of clinical symptoms (Fig. 3C) but mirrored the control serum recipients with respect to weight loss (Fig. 3B). Five of seven recipients of sera from empty vesicle-immunized donors died with the same kinetics as the control serum recipients (Fig. 3D). These data suggest that the survival in F. tularensis LVS challenge correlates with IgG anti-F. tularensis antibody titer. Despite protection against F. tularensis LVS challenge, serum from an LVS-V-immunized donor, transferred i.v., did not protect against an i.n. challenge with 50 CFU F. tularensis Schu S4 (data not shown).
FIG 3.
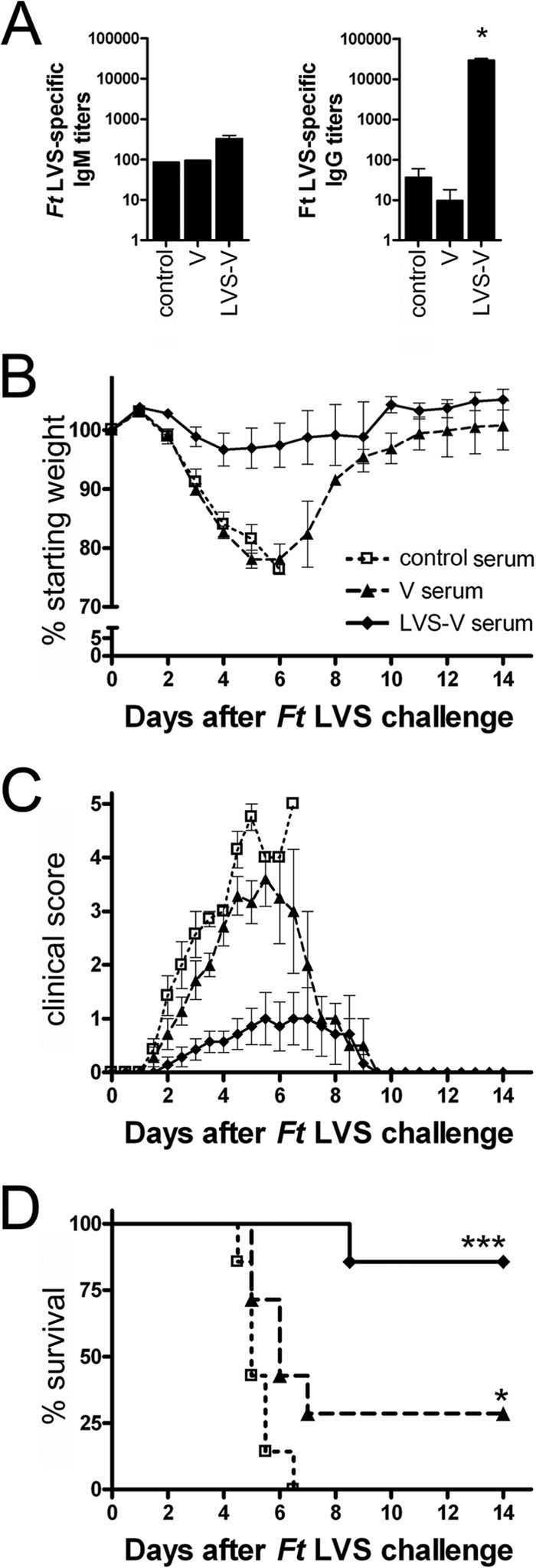
Passive immunization protects against F. tularensis LVS challenge. (A) IgM and IgG titers against whole F. tularensis LVS were measured by ELISA in pooled donor serum of saline-immunized mice (control serum) or of mice previously immunized twice i.p. with empty vesicles or LVS-V (x axis). *, P < 0.05 by Student t test. (B to D) Sixty microliters of serum was transferred to naive 6- to 8-week-old mice by tail vein injection 1 day prior to challenge with 100,000 CFU F. tularensis LVS. The percent starting weight (B), severity of clinical symptoms (C), and survival (D) were measured following challenge. The combined data from two independent experiments are shown (n = 7). The error bars represent the standard errors of the means (SEM). *, P < 0.05; ***, P < 0.001 by log rank test.
LVS-V induces cytokine gene and protein expression in vivo.
Because partial protection of mice that were immunized with empty vesicles was observed in response to lethal F. tularensis LVS challenge (Fig. 1), despite antibody responses that were no different than those of naive animals (Fig. 2), we sought to test the inflammatory potentials of the surfactant vesicles, as this is often a property of adjuvants (57). Mice were injected i.p. with either saline, bare vesicles, or LVS-V at the same dose as used for immunization. Four hours later, each mouse was bled and euthanized and the livers harvested for reverse transcription-quantitative PCR (qRT-PCR) analysis of proinflammatory gene expression. Compared to the saline controls, LVS-V induced significantly higher levels of the following genes: keratinocyte chemoattractant (KC), 58-fold (P = 0.0061); monocyte chemoattractant protein 1 (MCP-1), 5.7-fold (P = 0.0061); tumor necrosis factor alpha (TNF-α), 5.3-fold (P = 0.0061); and IL-1β, 4.6-fold (P = 0.0061) (Fig. 4A). IFN-β, IFN-γ, gamma interferon inducible protein 10 (IP-10), RANTES (data not shown), IL-6, and inducible nitric oxide synthase (iNOS) (Fig. 4A) were induced in only some of the LVS-V-treated mice by 4 h, and consequently, the mean induction values for these genes were not statistically significantly different compared to those of the saline controls. Only a few of these inflammatory genes were induced in the livers of mice treated with plain vesicles and to a much lower level than those induced by LVS-V (Fig. 4A). KC and IL-6 proteins were also detected in the serum samples of mice 4 h after immunization with LVS-V but decreased rapidly thereafter (Fig. 4B). No difference was observed in the Th2-inducing cytokines IL-4 and IL-13 (data not shown). Spleens were also harvested 4 h after injection and showed similar expression patterns but lower levels of induction of proinflammatory genes (data not shown).
FIG 4.
Comparison of cytokine gene and protein expression induced early after empty vesicle versus LVS-V administration. The mice were injected i.p. with saline, LVS-V (35 μg protein), or the equivalent amount of empty vesicles. (A) Four hours after vaccination, each mouse was euthanized and the liver harvested. Gene induction of iNOS and cytokine and chemokine genes representative of inflammatory responses was measured by qRT-PCR. Each symbol represents an individual mouse. (B) After immunization, mice were bled at the indicated time points and cytokine protein levels were measured in the serum samples of individual mice by the Luminex assay. The average serum concentrations ± the SEM of 5 mice are shown for KC and IL-6.
Reproducibility of size and stability of F. tularensis nanoparticles.
To optimize our immunization protocol, we tested whether the size or stability of the F. tularensis nanoparticles was affected by the protein content of the vesicles. F. tularensis LVS pellets containing increasing numbers of bacteria (from 1/8-fold below up to 4-fold above the standard input concentration of 25 ml of overnight culture) were processed into vesicles using the identical amounts of surfactants and water for each preparation, as described in Materials and Methods. Purified nanoparticles were analyzed for protein content and physical characteristics. Measurement of the zeta potential, a measure of vesicle stability (52), revealed that vesicles that incorporated more bacterial components (as evidenced by increased protein concentration of the purified vesicle preparations) exhibited lower surface charges (see Fig. S2A in the supplemental material). Lower surface charge is typically associated with the destabilization of vesicles (52), yet no differences in toxicity were observed between mice immunized with vesicles of low versus high surface charge (data not shown). The average vesicle size (∼80-nm radius) was also not significantly affected by the amount of bacterial starting material incorporated in the vesicles (see Fig. S2B in the supplemental material). Importantly, different batches of F. tularensis nanoparticles prepared from either F. tularensis LVS or F. tularensis Schu S4 using the standard protocol of 25 ml of overnight bacterial culture exhibited a high consistency of physical parameters, such as average radius and surface charge (see Fig. S2A and B in the supplemental material; also, data not shown).
F. tularensis LVS LPS and proteins, including epitopes recognized by immune mouse serum, are extracted into vesicles with a high degree of consistency.
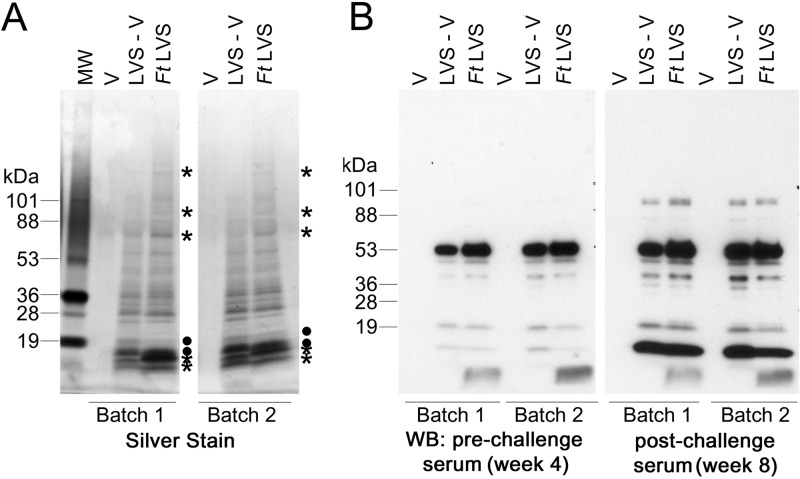
Figure 5A shows a silver-stained gel in which two independently prepared batches of empty vesicles and LVS-V (designated batch 1 and batch 2), as well as lysed samples of the F. tularensis LVS pellets from which the respective LVS-V batches were produced, were electrophoresed side by side. Silver staining revealed that there were no detectable bands in the bare vesicles, whereas most F. tularensis LVS proteins were consistently extracted into LVS-V preparations (Fig. 5A). Some bands, such as the one with an apparent molecular mass of ∼20 kDa, were enriched in the vesicles, while other proteins were less efficiently incorporated. Western analysis using a polyclonal anti-F. tularensis LPS antibody shows that F. tularensis LPS is also incorporated into LVS-V, as evidenced by the typical LPS ladder (see Fig. S3A in the supplemental material). Bands detected by Western analysis using serum samples from immunized mice before and after F. tularensis LVS challenge are also consistently incorporated into LVS-V (Fig. 5B). The vesicles that were made in the absence of F. tularensis LVS and served as control immunogens were also free from contamination, as evidenced by the absence of bands in the silver stain and Western analyses (Fig. 5). Similar batch-to-batch uniformity was observed in vesicles extracted from F. tularensis Schu S4 by silver stain and Western analysis (see Fig. S2C and D in the supplemental material).
FIG 5.
LVS-V are made with a high degree of consistency and are immunogenic. F. tularensis LVS molecules were incorporated into surfactant vesicles to form LVS vesicles. Lysates derived from a sampling of the F. tularensis bacterial pellets prior to the addition of surfactants (FtLVS) and empty control vesicles (V) were also included for comparison. (A) Samples were separated by SDS-PAGE on a 10 to 20% gradient gel and silver stained for total protein. Asterisks and filled circles mark bands that were extracted with low and high efficiency into vesicles, respectively. (B) The same samples were subjected to Western analysis (WB) with sera from mice that had been immunized twice with LVS-V (prechallenge) and challenged twice with F. tularensis LVS (postchallenge) as described in Fig. 2. The silver stain and serum blots are representative of 8 separate experiments.
Antibody epitope specificity matures following infection with live F. tularensis LVS.
Figure 5C also illustrates maturation of the IgG antibody response in mice that were immunized with F. tularensis nanoparticles, as evidenced by a comparison of the diversity of antigens detected by Western analysis in serum samples collected before and after challenge with F. tularensis LVS. Using serum samples collected immediately prior to challenge (two weeks after the second immunization with LVS-V) and a secondary anti-mouse IgG antibody, 5 prominent bands were detected in the LVS-V samples, one of which exhibited an apparent molecular mass of ∼55 kDa and was the predominant species detected by Western analysis. Minor bands with molecular masses of ∼50 kDa, ∼40 kDa, ∼20 kDa, and ∼12 kDa were also consistently detected at the same exposure. Immunoreactive bands of ∼95 kDa, ∼45 kDa, ∼37 kDa, ∼33 kDa, and ∼10 kDa were also present in LVS-V but were detected only after a long exposure (data not shown). A very low-molecular-weight species was detected exclusively in the F. tularensis LVS whole-cell lysates by Western analysis with both the anti-LPS antibody (see Fig. S3 in the supplemental material) and the LVS-V immune serum (Fig. 5B). Among the low-molecular-weight bands detected in silver staining, none were found that corresponded to the F. tularensis LVS lysate-specific band. In serum samples collected 1 week following a second F. tularensis LVS challenge, IgG responses to the minor band at ∼12 kDa were greatly enhanced to reveal a second immunodominant band. The responses to all other bands were also enhanced to various degrees, with the greatest increase seen at bands with apparent molecular masses of ∼95 kDa, ∼37 kDa, and ∼12 kDa. After the exposure to live bacteria, new minor bands with apparent molecular masses of ∼86 kDa, ∼67 kDa, and ∼22 kDa were detected. This same pattern was seen in both batches of LVS-V and F. tularensis LVS lysates. The same bands were detected regardless of whether LVS-V was produced in the absence or presence of protease inhibitors (see Fig. S3B and C in the supplemental material).
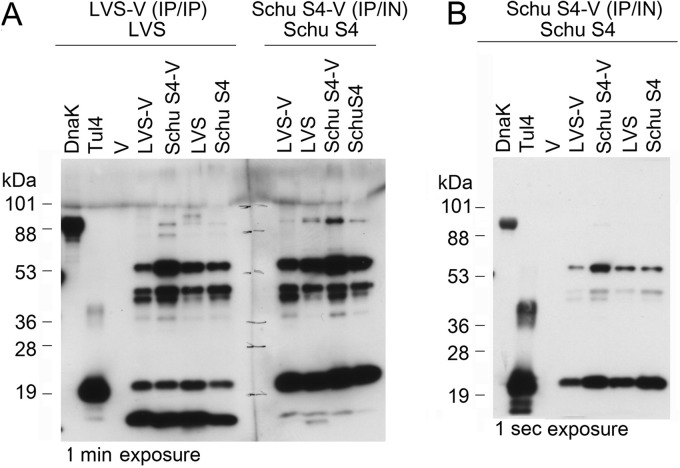
In the next series of experiments, blood serum samples were pooled from mice vaccinated with LVS-V (i.p./i.p.) and challenged with F. tularensis LVS (i.p.) and from mice vaccinated with Schu S4-V (i.p./i.n.) and challenged with F. tularensis Schu S4 (i.n.). In preliminary studies, we found that a 1:1,000,000 dilution of anti-LVS-V serum and a 1:100,000 dilution of the anti-Schu S4-V serum gave equivalent results in ELISA (data not shown). These dilutions were chosen for Western analysis, where they also detected several bands with the same intensity. A recent F. tularensis LVS subunit vaccine composed of Tul4 and DnaK successfully protected mice against intranasal challenge with F. tularensis LVS (42). Indeed, both purified Tul4 and DnaK preparations were detected with antisera from mice immunized and challenged homologously with either LVS-V and F. tularensis LVS or Schu S4-V and F. tularensis Schu S4 (Fig. 6A and B). The anti-Schu S4 serum reacted more strongly with Tul4 than the anti-LVS serum (note in Fig. 6B that these were exposed for only 1 s, because a longer exposure of the Tul4 protein detected by the anti-Schu S4-V antiserum was grossly overexposed). No bands were detected in bare vesicles with either antiserum preparation (Fig. 6A and B). Five predominant bands (including one that appears to be a doublet) were detected by the two antisera: the anti-LVS-V serum detected bands at molecular masses of ∼55 kDa, ∼40 kDa (doublet), ∼20 kDa, ∼12 kDa, and a faint band at ∼90 kDa (Fig. 6A). Interestingly, the anti-Schu S4-V antiserum detected the same bands but differed in the intensity of the bands. Specifically, the ∼12-kDa band was poorly detected, the ∼20-kDa species was more strongly detected, and the ∼90-kDa band, while still faint, was more apparent than in blots developed using the anti-LVS-V antiserum (Fig. 6A and B). Taken together, these data confirm our finding that the antibody response matures following exposure to live bacterial challenge (Fig. 5) and they extend it by showing that several immunodominant species are differentially detected by serum produced in response to LVS-V immunization/F. tularensis LVS challenge versus Schu S4-V immunization/F. tularensis Schu S4 challenge.
FIG 6.
Serum samples from mice immunized with LVS-V or Schu S4-V and challenged with live homologous bacteria detect similar bands by Western analysis but also exhibit differences in their binding specificities. (A) Mice were immunized either with LVS-V by two i.p. injections and challenged i.p. with F. tularensis LVS as described in Fig. 1 or immunized with Schu S4-V by i.p. and i.n. routes and challenged i.n. with F. tularensis Schu S4. Serum samples harvested 3 weeks postchallenge (LVS serum, 1:106; Schu S4 serum, 1:105) were used to probe Western blots (4 to 20% gradient gel) of vesicles (V, LVS-V, and Schu S4-V), whole-lysed bacteria (LVS and Schu S4), and purified recombinant F. tularensis proteins (DnaK and Tul4). (B) The same membrane at a lower (1-s) exposure to show DnaK and Tul4 detected by Schu S4-V-immunized/Schu S4-challenged survivor serum. Similar results were seen in two separate experiments.
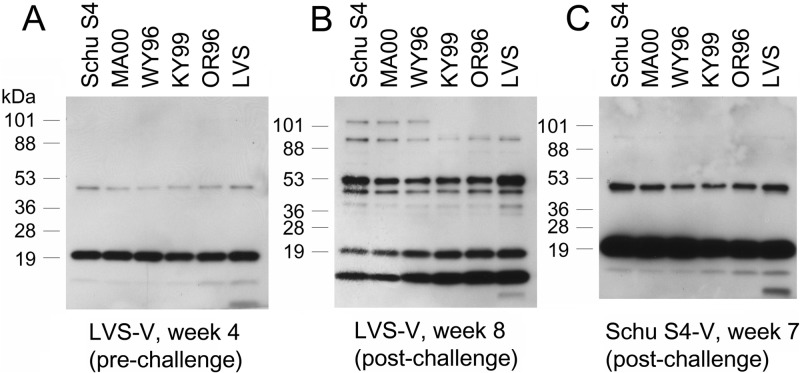
F. tularensis epitopes recognized by either LVS or Schu S4 antiserum are found in other F. tularensis strains as well.
We sought to test whether the epitopes recognized by the immune sera from LVS-V-immunized LVS-challenged mice and Schu S4-V-immunized Schu S4-challenged mice would be present in other strains, including some that are clinically relevant. F. tularensis strains MA00-2987 (A1 strain), WY96-3418 (A2 strain), and KY99-3387 and OR96-0246 (B strains) were grown in enriched TSB. The samples were subjected to Western analysis with the antisera described above. Approximately equal loading was confirmed by silver staining (data not shown). Prebleed serum failed to detect any bands by Western analysis (data not shown). Serum samples collected 2 weeks after the second immunization with LVS-V (i.p./i.p.) but prior to F. tularensis LVS challenge (week 4) (Fig. 7A), after i.p. challenge with F. tularensis LVS (week 8) (Fig. 7B), or after immunization (i.p./i.n.) with Schu S4-V and i.n. challenge with Schu S4 (Fig. 7C) each showed remarkable consistency in their binding patterns across different F. tularensis strains. Interestingly, antiserum from the LVS-V-immunized F. tularensis LVS challenge survivors recognized an additional high-molecular-weight band in the type A1 (Schu S4, MA00) and A2 (WY96) strains (molecular mass, ∼105 kDa) not detected in the type B strains (F. tularensis KY99, OR96, and LVS).
FIG 7.
Prominent F. tularensis epitopes detected in serum samples from vesicle-immunized mice are conserved across multiple strains of F. tularensis. F. tularensis from strains Schu S4, MA00-2987 (A1 strains), WY96-3418 (A2 strain), KY99-3387, OR96-0246, and LVS (B strains) were grown in enriched TSB as described in Materials and Methods and subjected to Western analysis (4 to 20% gradient gel) with the antisera used in Fig. 5 and 6. (A) Sera from LVS-V-immunized mice before challenge. (B) Sera from LVS-V-immunized mice after live LVS challenge. (C) Sera from Schu S4-immunized mice after live Schu S4 challenge.
LVS-V and Schu S4-V immunization partially protect against i.n. Schu S4 challenge.
The most pressing need for a Francisella vaccine is for the protection of populations in case of aerosol releases of virulent type A strains of F. tularensis. Since LVS-V appears to be proinflammatory early after immunization and induces robust anti-F. tularensis antibody titers, we sought to test whether the F. tularensis nanoparticles might also protect against F. tularensis Schu S4, the most extensively studied model strain of the type A clade. Initially, the mice were immunized as before (i.p./i.p., 2 weeks apart) with either sterile PBS, LVS-V, or the same volume of empty vesicles. Two weeks following the second immunization, all mice were challenged i.n. with ∼10 CFU F. tularensis Schu S4. The mice immunized with PBS rapidly developed tularemia, and all either died or had to be euthanized by the end of day 5 postchallenge. In contrast to LVS challenge, mice that had been immunized with empty vesicles were not protected against Schu S4 challenge and developed clinical symptoms with similar kinetics as the saline-immunized mice and exhibited a nonsignificant delay in time to death. However, in mice vaccinated with LVS-V, we observed a delay in the onset of clinical symptoms, and one of five mice survived (data not shown).
To improve on the partial protection gained by LVS-V immunization against Schu S4 challenge, the mice were next immunized with Schu S4-V rather than LVS-V. Utilizing the same immunization regimen as for LVS-V with Schu S4-V (i.p./i.p., 2 weeks apart), only one of 10 mice survived i.n. challenge with ∼20 CFU F. tularensis Schu S4. However, the onset of symptoms and time to death from tularemia were delayed by almost 2 days, which was significant by the Mann-Whitney test (nonparametric t test) compared to animals that had been immunized with vesicles only (Table 1).
TABLE 1.
Outcome of immunized mice after live intranasal F. tularensis Schu S4 challenge
| Immunization typea | Immunization routeb | Survival 14 days postchallenge |
Time to death postchallengec |
||
|---|---|---|---|---|---|
| No. of survivors/total no. (%) | Pd | Avg ± SD (days) | Pe | ||
| V (control) | i.p./i.p., i.p./i.n., i.n./i.p./i.n. | 0/34 (0) | 4.9 ± 0.3 | ||
| F. tularensis Schu S4-V | i.p. | 0/5 (0) | NS | 6.4 ± 0.9 | <0.01 |
| i.p./i.p. | 1/10 (10) | NS | 6.8 ± 1.0 | <0.001 | |
| i.p./i.n. | 7/35 (20) | 0.011 | 6.1 ± 0.9 | <0.001 | |
| i.n./i.p. | 2/8 (25) | 0.033 | 6.3 ± 1.0 | <0.01 | |
| i.n./i.p./i.n. | 2/9 (22) | 0.040 | 7.0 ± 0.8 | <0.001 | |
| i.n./i.n. | 0/11 (0) | NS | 5.5 ± 0.5 | NS | |
| i.n./i.n./i.n. | 3/15 (20) | 0.025 | 5.9 ± 0.8 | <0.001 | |
| s.c./i.p., s.c./i.n., s.c./s.c. | 0/30 (0) | NS | 5.7 ± 0.7 | <0.001 | |
Mice were immunized with control vesicles (V) or Schu S4-V at 2-week intervals by the indicated routes. Two weeks after the final immunization, all mice were challenged with ∼20 CFU (ranging from 3 to 49 CFU in different experiments) of F. tularensis Schu S4 by the intranasal route.
i.p., intraperitoneal; i.n., intranasal; s.c., subcutaneous.
Mean and standard deviation of time to death were calculated from only those animals that succumbed to infection.
Fisher's exact test, P value compared to that of control; NS, not significant.
One-way ANOVA, P value of Tukey posttest compared to that of control.
Heterologous routes of immunization with Schu S4-V result in improved protection against Schu S4 challenge.
Since the number of immunizations and the route of administration affect the strength and type of the subsequent immune response, we compared outcomes from Schu S4 challenge following immunization with either 2 or 3 doses, as well as by diverse administration routes. The results from 5 independent experiments are summarized in Table 1. In each experiment, the control group of mice was immunized with bare vesicles, and all of these mice died within 5 days (on average), even with a challenge dose as low as 3 CFU F. tularensis Schu S4 per mouse. All mice that received Schu S4-V by i.p. and/or by i.n. route displayed a delayed onset of symptoms and delayed time to death by >1 day. In mice immunized via the subcutaneous (s.c.) route, the time to death was delayed less but was still statistically significant. No mice survived challenge after two immunizations with Schu S4-V by combinations involving the s.c. route or i.n. route only. Improved partial protection was gained through heterologous prime-boost using i.p./i.n. and i.n./i.p. routes. In the single most effective experiment, four of six mice (66%) that were immunized with Schu S4-V i.p./i.n. survived challenge with ∼22 CFU live F. tularensis Schu S4 (data not shown). The clinical scores of a representative experiment are shown in Fig. S3 in the supplemental material and illustrate the effects of the various immunization regimens. The addition of a third i.n. immunization also improved the outcome of challenge, assessed by a slight improvement in the fraction of survivors and further delay in time to death in nonsurvivors (Table 1; see also Fig. S4A in the supplemental material). Systemic F. tularensis-specific IgG titers were also increased following a third i.n. immunization (see Fig. S4B in the supplemental material). Heterologous immunization routes (i.e., i.n. and i.p. administration, with two immunizations) showed similar titers compared to three doses administered solely through the i.n. route, and the administration of a third i.n. dose further increased IgG titers. Regardless of the route of immunization, the blood serum IgG levels of mice that survived Schu S4 i.n. challenge (bled 21 days postchallenge) were approximately 10-fold higher than those of nonsurvivors (bled 5 to 8 days postchallenge at the time of euthanasia) (i.e., average titers of ∼125,000 and ∼12,000, respectively). Together, these data show that significant partial protection against virulent type A challenge can be achieved with two doses as a heterologous (i.p./i.n.) prime-boost immunization or by three i.n. immunizations with Schu S4-V.
DISCUSSION
Vaccines for immune-evasive pathogens must effectively activate protective innate and adaptive immune responses in order to preclude the pathogens from creating a survival niche in their hosts. In the case of live vaccines, balancing the risks of overattenuation and reversion to pathogenicity presents significant regulatory hurdles, while the usually much safer subunit vaccines often lack efficacy. Therefore, new approaches are required to improve the efficacy of subunit vaccines. Herein, we describe the first use of functionalized catanionic vesicles, a nanoparticulate platform for vaccine delivery against the intracellular macrophage-tropic pathogen F. tularensis.
Catanionic surfactant vesicles are highly stable, with an overall slightly negative surface charge, due to the excess of anionic surfactant, which allows for the integration of bacterium-derived hydrophobic molecular regions similar to phospholipid bilayers. In contrast, other nanoparticles, e.g., immunostimulatory complexes (ISCOMs), utilize saponin mixed with cholesterol that segregates into distinct patches within phospholipid membranes that are nonfluid and usually do not accommodate transmembrane domains of proteins (58). The inclusion of saponin in an artificial vesicle has been associated with adjuvant activity (47). While ISCOMs have been used in vaccine candidates in animal models (reviewed in reference 59), their use was abandoned in small animal models due to toxicity (reviewed in reference 47). Liposomes are a related self-assembled structure composed entirely of artificial lipid membranes. However, unlike catanionic vesicles, liposomes are difficult to produce and fail to maintain their integrity due to oxidation aggregation under physiological conditions (47). The catanionic vesicle pair used herein is 3 parts SDBS and 1 part CTAT (by molar ratio), which is ideal for the formation of small distinct vesicles, rather than forming lamellar sheets (48). Purified catanionic vesicles are highly stable in water and saline and are generally well tolerated in mice at the concentrations required for effective immunization. Catanionic vesicle preparation for vaccines is also economically viable, as the reagents are (i) inexpensive, (ii) highly stable in vitro (unlike other vesicles), with shelf lives of >5 months at 4 to 25°C, and (iii) easily purified by size exclusion chromatography without the need for ultracentrifugation or other specialty equipment. The average size of bare and functionalized SDBS-to-CTAT catanionic vesicle preparations had a ∼70- to 120-nm radius, about the size of a virus, which is large enough to allow a multivalent presentation of antigens and innate stimuli, as well as efficient phagocytosis. Importantly, F. tularensis failed to survive exposure to the primary surfactant, SDBS, during the production of the immunogenic nanoparticles. However, the majority of bacterial components that can be detected by silver stain in whole-cell lysates were also detected in the resultant catanionic vesicle vaccine preparations (Fig. 5A; see also Fig. S2 in the supplemental material).
While we expect that hydrophobic and amphiphilic bacterial molecules (i.e., cell membrane and cell wall components) are inserted in the leaflet of catanionic vesicles, the spontaneous assembly into vesicles also permits the entrapment of hydrophilic bacterial components, as well as the capture of DNA across the array of negative charges on the surface of these vesicles. This allows for the simultaneous presentation of multiple antigens and innate immune stimulatory molecules to antigen-presenting cells. We have shown that the production of F. tularensis vaccines from catanionic vesicles is highly reproducible (Fig. 5; see also Fig. S2 and 3 in the supplemental material). These nanoparticles are also highly immunogenic, increasing the IgG antibody titers by >10-fold to titers that in some cases exceeded 106. Both morbidity and mortality were diminished in live F. tularensis LVS challenge experiments (Fig. 1), and the immunization regimen induced both cellular and humoral adaptive immune responses (Fig. 2 to 4). F. tularensis-specific antibody production was enhanced after vaccination with catanionic vesicles containing LVS particles (Fig. 2), while previous studies were unable to correlate F. tularensis-specific antibody production with protection (60, 61). T helper cells must be activated in our system, as most of the F. tularensis-specific antibodies produced in response to LVS-V-immunization are of the IgG isotype (Fig. 2), which is a T cell-dependent phenomenon. Moreover, we were able to reproduce the protection against live F. tularensis LVS challenge by passive immunization with the IgG-rich blood serum from LVS-V-immunized mice (Fig. 3). These data support previous findings that there exists an extracellular phase of F. tularensis infection that can be targeted by antibodies (62, 63).
The success of the passive immunization and the preservation of immunogenic epitopes across diverse clinical and laboratory strains of F. tularensis (Fig. 3 and 7) raise the question of which epitopes, or combination of epitopes, are essential for a protective response. With our method of lysing entire F. tularensis bacteria in surfactant for producing the immunogenic vesicles, we cannot currently provide a satisfactory answer to this question. However, in future studies, we will refine the catanionic F. tularensis vesicle vaccine by using deletion mutants of F. tularensis to identify important immunogens, as well as by identifying the immunogenic epitopes detected by Western analysis using mass spectrometry. Using catanionic vesicles as a vehicle for immunizing mice is an extremely flexible platform that will enable us to produce candidate vaccines for any F. tularensis mutant strain, including those that have been used as live attenuated vaccines. This modification of the approach also obviates problems related to safety during the preparation of vaccines and of reversion to virulence, while potentially providing protective antigenic epitopes.
It has been proposed that F. tularensis LVS may lack protective antigens that are necessary for protection against type A strains (64). Therefore, we produced nanoparticles that incorporate F. tularensis Schu S4 components. The sera from survivors of Schu S4 challenge recognized similar epitopes in LVS-V and Schu S4-V (Fig. 6). However, in lysates from type A strains, one band at ∼105 kDa was detected only using serum samples from LVS-V-immunized and F. tularensis LVS-challenged mice (Fig. 7B versus C). This protein may indeed represent a significant modification between the A and B subspecies of F. tularensis. Future studies will be required to identify this protein and to determine its molecular function. The present study demonstrated that multiple common immunoreactive species are present across diverse strains of F. tularensis, suggesting that it may be possible to protect against both type A and B strains using our approach.
One of the more surprising observations from this study is that the bare vesicles protected mice against challenge with F. tularensis LVS but not F. tularensis Schu S4. The mice immunized with bare vesicles survived F. tularensis LVS challenge despite no detectable antibody response and a relatively low induction of inflammatory cytokines early after immunization (Fig. 1, 2, and 4). However, the observed partial protection in weight loss, clinical score, and survival gained by immunization with vesicles, as shown in Fig. 1, were not replicated by passive immunization with serum samples from empty vesicle-immunized mice (Fig. 1 versus 3), indicating that the vesicles themselves may elicit a sufficient inflammatory response to overcome infection with a relatively weak strain of F. tularensis LVS. Inflammation has previously been shown to contribute significantly to the ability to form lasting immunity to F. tularensis. For example, IFN-γ−/− mice cannot be protected by immunization with live F. tularensis LVS vaccine (65), while even heat-killed F. tularensis LVS allowed for the development of protective immunity when coadministered with IL-12 (66), a strong inducer of IFN-γ (67). In IL-6−/− mice, susceptibility to F. tularensis LVS infection is enhanced (68). Moreover, live attenuated F. tularensis strains, such as the ΔclpB strain, elicit early inflammatory responses and induce immunity to F. tularensis LVS (35–37). Immunization with attenuated Schu S4 mutants capable of protecting mice against subsequent virulent Schu S4 challenge was shown to correlate with higher blood serum levels of TNF-α, IFN-γ, and MCP-1 within the first week postinfection than immunization with nonprotective mutants (60). The administration of F. tularensis components integrated into a catanionic vesicle also introduced F. tularensis antigens in an inflammatory context, as evidenced by an increase in inflammatory cytokines as early as 4 h after vaccination (Fig. 4). While the adjuvant effect of bare catanionic vesicles was insufficient to elicit protection against the more virulent type A F. tularensis, the catanionic vesicle platform used in this study is fully amenable to the insertion of known adjuvants (e.g., monophosphoryl lipid A [MPL]) to improve the adjuvanticity of the F. tularensis-specific vaccine. Consistent with this observation, we previously reported that the treatment of mice with MPL alone was sufficient to confer partial protection against F. tularensis Schu S4 (29). Perhaps the low level of cytokine production in response to immunization with bare vesicles was sufficient to result in macrophage activation and partial control of the F. tularensis LVS.
The main concern regarding a tularemia outbreak is infection via natural aerosol exposure or aerosolized intentional use because of the severity of symptoms associated with the pulmonary form of tularemia. Therefore, protection against i.n. challenge is highly relevant, particularly for F. tularensis type A strains. This type of protection has been notoriously difficult to achieve, even using live vaccines. Partial protection has been achieved previously with the live vaccine strain F. tularensis LVS (69), and several live attenuated vaccines have proven to be efficacious (38, 70); however, subunit vaccines have largely failed to protect against F. tularensis Schu S4 (70). Nonetheless, Schu S4-V was able to elicit partial protection in the F. tularensis Schu S4 challenge experiments; i.e., they elicited ≥20% survival and between one and 2 days delay in F. tularensis-associated symptoms and death in nonsurvivors compared to animals that received empty vesicles (Table 1). It should be noted that although C57BL/6 and BALB/c mice are approximately equally susceptible to F. tularensis LVS infection (4), differences in their genetic backgrounds make C57BL/6 mice more difficult to protect (37, 69, 71), and C57BL/6 mice were used in all of our experiments. Second, intrinsic differences between F. tularensis strains and their capacity to adapt to changing environments influence infection efficiency and disease progression. Growth conditions, such as the choice of medium and temperature, are known to influence expression patterns (72), and they have largely been kept the same for these experiments.
The highly virulent F. tularensis type A strain Schu S4 has additional immune-evasion strategies that are lacking from the F. tularensis type B strain, F. tularensis LVS, such as the ability to bind plasmin, which reduces the effectiveness of antibody opsonization (32). In our hands, i.p./i.n. heterologous immunization with Schu S4 vesicles elicited ∼10-fold-lower levels of F. tularensis-specific antibodies than i.p./i.p. immunization with F. tularensis LVS vesicles. Nonetheless, protection by the i.p./i.n. routes of immunization was generally more protective. This indicates that IgA, which is known to inhibit IgG-mediated phagocytosis (73), did not have a negative impact on vaccine protection in this model. Perhaps, the combination of lower antibody titers and plasmin-binding ability of F. tularensis Schu S4 contribute to its failure to elicit complete protection against intranasal F. tularensis Schu S4 challenge. We also speculate that the more potent infectious strains of F. tularensis are more efficient at inducing antiinflammatory signaling cascades in their host, such as the caspase-1-mediated feedback loop of the AIM2 inflammasome activation (74), and transcriptional downregulation of TLR2, phosphoinositide 3-kinase (PI3K), and Akt, which are important for sustained cytokine signaling, as well as downregulation of major histocompatibility complex class II (MHCII), which is important in T cell activation (75, 76). Nonetheless, our ability to consistently protect ∼25% of mice by various routes of immunization using Schu S4-V and to delay death significantly in those animals that did eventually succumb to F. tularensis Schu S4 infection shows that this work is an important step in the development of an efficacious subunit vaccine. Efficacy may be improved by incorporating additional proinflammatory stimuli or by incorporating adjuvants into the vesicle preparations. Future experiments will be required to test this approach.
In conclusion, in seeking an F. tularensis subunit vaccine that is safe and effective, we investigated the use of functionalized catanionic vesicles that represent an effective delivery system for antigens and proinflammatory molecules. While the protection achieved against challenge with the most dangerous form of F. tularensis, the pneumonic form of a type A strain, was only partial, our results indicate an important step in the right direction. Additionally, this nanoparticle methodology of antigen delivery via functionalized catanionic vesicles has the potential to be used as a vaccine vehicle against other immune-evasive pathogens.
Supplementary Material
ACKNOWLEDGMENTS
K.R. acknowledges the generous financial support of the National Institutes of Health (grant no. T32AI095190). S.N.V., E.M.B., and B.J.M. also acknowledge the generous financial support of the National Institutes of Health (grant no. AI157168). P.D. acknowledges the generous financial support from the National Science Foundation (grant no. CHE 1210804), the Maryland Industrial Partnership, and an unrestricted grant from DuPont and Company.
We declare no conflicts of interest.
We thank Karen Elkins for her generous gifts of F. tularensis LVS and antibodies. We also thank Wendy Lai, Tristan Dyson, Kari Ann Shirey, Mark Marohn, Christen Grassel, and Lindsey Zimmermann for their technical support.
Footnotes
Published ahead of print 18 December 2013
Supplemental material for this article may be found at http://dx.doi.org/10.1128/CVI.00738-13.
REFERENCES
- 1.Foley JE, Nieto NC. 2010. Tularemia. Vet. Microbiol. 140:332–338. 10.1016/j.vetmic.2009.07.017 [DOI] [PubMed] [Google Scholar]
- 2.Oyston PC, Sjostedt A, Titball RW. 2004. Tularaemia: bioterrorism defense renews interest in Francisella tularensis. Nat. Rev. Microbiol. 2:967–978. 10.1038/nrmicro1045 [DOI] [PubMed] [Google Scholar]
- 3.Conlan JW, Chen W, Bosio CM, Cowley SC, Elkins KL. 2011. Infection of mice with Francisella as an immunological model. Curr. Protoc. Immunol. Chapter 19:Unit 19.14. 10.1002/0471142735.im1914s93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eigelsbach HT, Braun W, Herring RD. 1951. Studies on the variation of Bacterium tularense. J. Bacteriol. 61:557–569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hornick RB, Eigelsbach HT. 1966. Aerogenic immunization of man with live Tularemia vaccine. Bacteriol. Rev. 30:532–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wayne Conlan J, Oyston PC. 2007. Vaccines against Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:325–350. 10.1196/annals.1409.012 [DOI] [PubMed] [Google Scholar]
- 7.Petrosino JF, Xiang Q, Karpathy SE, Jiang H, Yerrapragada S, Liu Y, Gioia J, Hemphill L, Gonzalez A, Raghavan TM, Uzman A, Fox GE, Highlander S, Reichard M, Morton RJ, Clinkenbeard KD, Weinstock GM. 2006. Chromosome rearrangement and diversification of Francisella tularensis revealed by the type B (OSU18) genome sequence. J. Bacteriol. 188:6977–6985. 10.1128/JB.00506-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Titball RW, Petrosino JF. 2007. Francisella tularensis genomics and proteomics. Ann. N. Y. Acad. Sci. 1105:98–121. 10.1196/annals.1409.015 [DOI] [PubMed] [Google Scholar]
- 9.Hartley G, Taylor R, Prior J, Newstead S, Hitchen PG, Morris HR, Dell A, Titball RW. 2006. Grey variants of the live vaccine strain of Francisella tularensis lack lipopolysaccharide O-antigen, show reduced ability to survive in macrophages and do not induce protective immunity in mice. Vaccine 24:989–996. 10.1016/j.vaccine.2005.08.075 [DOI] [PubMed] [Google Scholar]
- 10.McCrumb FR., Jr 1961. Aerosol infection of man with Pasteurella tularensis. Bacteriol. Rev. 25:262–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koskela P, Herva E. 1982. Cell-mediated and humoral immunity induced by a live Francisella tularensis vaccine. Infect. Immun. 36:983–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elkins KL, Cowley S, Bosio CM. 2003. Innate and adaptive immune responses to an intracellular bacterium, Francisella tularensis live vaccine strain. Microbes Infect. 5:135–142. 10.1016/S1286-4579(02)00084-9 [DOI] [PubMed] [Google Scholar]
- 13.KuoLee R, Harris G, Conlan JW, Chen W. 2011. Role of neutrophils and NADPH phagocyte oxidase in host defense against respiratory infection with virulent Francisella tularensis in mice. Microbes Infect. 13:447–456. 10.1016/j.micinf.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 14.Jones CL, Napier BA, Sampson TR, Llewellyn AC, Schroeder MR, Weiss DS. 2012. Subversion of host recognition and defense systems by Francisella spp. Microbiol. Mol. Biol. Rev. 76:383–404. 10.1128/MMBR.05027-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen W, KuoLee R, Shen H, Bùsa M, Conlan JW. 2004. Toll-like receptor 4 (TLR4) does not confer a resistance advantage on mice against low-dose aerosol infection with virulent type A Francisella tularensis. Microb. Pathog. 37:185–191. 10.1016/j.micpath.2004.06.010 [DOI] [PubMed] [Google Scholar]
- 16.Dueñas AI, Aceves M, Orduña A, Díaz R, Sánchez Crespo M, García-Rodríguez C. 2006. Francisella tularensis LPS induces the production of cytokines in human monocytes and signals via Toll-like receptor 4 with much lower potency than E. coli LPS. Int. Immunol. 18:785–795. 10.1093/intimm/dxl015 [DOI] [PubMed] [Google Scholar]
- 17.Hajjar AM, Harvey MD, Shaffer SA, Goodlett DR, Sjöstedt A, Edebro H, Forsman M, Byström M, Pelletier M, Wilson CB, Miller SI, Skerrett SJ, Ernst RK. 2006. Lack of in vitro and in vivo recognition of Francisella tularensis subspecies lipopolysaccharide by Toll-like receptors. Infect. Immun. 74:6730–6738. 10.1128/IAI.00934-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golovliov I, Baranov V, Krocova Z, Kovarova H, Sjöstedt A. 2003. An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect. Immun. 71:5940–5950. 10.1128/IAI.71.10.5940-5950.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clemens DL, Lee BY, Horwitz MA. 2004. Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect. Immun. 72:3204–3217. 10.1128/IAI.72.6.3204-3217.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alnemri ES. 2010. Sensing cytoplasmic danger signals by the inflammasome. J. Clin. Immunol. 30:512–519. 10.1007/s10875-010-9419-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Celli J, Zahrt TC. 2013. Mechanisms of Francisella tularensis intracellular pathogenesis. Cold Spring Harb. Perspect. Med. 3:a010314. 10.1101/cshperspect.a010314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergsbaken T, Fink SL, Cookson BT. 2009. Pyroptosis: host cell death and inflammation. Nat. Rev. Microbiol. 7:99–109. 10.1038/nrmicro2070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Denes A, Lopez-Castejon G, Brough D. 2012. Caspase-1: is IL-1 just the tip of the ICEberg? Cell Death Dis. 3:e338. 10.1038/cddis.2012.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mares CA, Ojeda SS, Morris EG, Li Q, Teale JM. 2008. Initial delay in the immune response to Francisella tularensis is followed by hypercytokinemia characteristic of severe sepsis and correlating with upregulation and release of damage-associated molecular patterns. Infect. Immun. 76:3001–3010. 10.1128/IAI.00215-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole LE, Elkins KL, Michalek SM, Qureshi N, Eaton LJ, Rallabhandi P, Cuesta N, Vogel SN. 2006. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 176:6888–6899 [DOI] [PubMed] [Google Scholar]
- 26.Cole LE, Santiago A, Barry E, Kang TJ, Shirey KA, Roberts ZJ, Elkins KL, Cross AS, Vogel SN. 2008. Macrophage proinflammatory response to Francisella tularensis live vaccine strain requires coordination of multiple signaling pathways. J. Immunol. 180:6885–6891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cole LE, Shirey KA, Barry E, Santiago A, Rallabhandi P, Elkins KL, Puche AC, Michalek SM, Vogel SN. 2007. Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect. Immun. 75:4127–4137. 10.1128/IAI.01868-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz J, Zhang P, Martin M, Vogel SN, Michalek SM. 2006. Toll-like receptor 2 is required for inflammatory responses to Francisella tularensis LVS. Infect. Immun. 74:2809–2816. 10.1128/IAI.74.5.2809-2816.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole LE, Mann BJ, Shirey KA, Richard K, Yang Y, Gearhart PJ, Chesko KL, Viscardi RM, Vogel SN. 2011. Role of TLR signaling in Francisella tularensis-LPS-induced, antibody-mediated protection against Francisella tularensis challenge. J. Leukoc. Biol. 90:787–797. 10.1189/jlb.0111014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henry T, Brotcke A, Weiss DS, Thompson LJ, Monack DM. 2007. Type I interferon signaling is required for activation of the inflammasome during Francisella infection. J. Exp. Med. 204:987–994. 10.1084/jem.20062665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clay CD, Soni S, Gunn JS, Schlesinger LS. 2008. Evasion of complement-mediated lysis and complement C3 deposition are regulated by Francisella tularensis lipopolysaccharide O antigen. J. Immunol. 181:5568–5578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crane DD, Warner SL, Bosio CM. 2009. A novel role for plasmin-mediated degradation of opsonizing antibody in evasion of host immunity by virulent, but not attenuated, Francisella tularensis. J. Immunol. 183:4593–4600. 10.4049/jimmunol.0901655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shirey KA, Cole LE, Keegan AD, Vogel SN. 2008. Francisella tularensis live vaccine strain induces macrophage alternative activation as a survival mechanism. J. Immunol. 181:4159–4167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cowley SC, Elkins KL. 2011. Immunity to Francisella. Front. Microbiol. 2:26. 10.3389/fmicb.2011.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barrigan LM, Tuladhar S, Brunton JC, Woolard MD, Chen CJ, Saini D, Frothingham R, Sempowski GD, Kawula TH, Frelinger JA. 2013. Infection with Francisella tularensis live vaccine strain clpB leads to an altered yet protective immune response. Infect. Immun. 81:2028–2042. 10.1128/IAI.00207-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conlan JW, Shen H, Golovliov I, Zingmark C, Oyston PC, Chen W, House RV, Sjöstedt A. 2010. Differential ability of novel attenuated targeted deletion mutants of Francisella tularensis subspecies tularensis strain SCHU S4 to protect mice against aerosol challenge with virulent bacteria: effects of host background and route of immunization. Vaccine 28:1824–1831. 10.1016/j.vaccine.2009.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Twine S, Shen H, Harris G, Chen W, Sjöstedt A, Ryden P, Conlan W. 2012. BALB/c mice, but not C57BL/6 mice immunized with a ΔclpB mutant of Francisella tularensis subspecies tularensis are protected against respiratory challenge with wild-type bacteria: association of protection with post-vaccination and post-challenge immune responses. Vaccine 30:3634–3645. 10.1016/j.vaccine.2012.03.036 [DOI] [PubMed] [Google Scholar]
- 38.Barry EM, Cole LE, Santiago AE. 2009. Vaccines against tularemia. Hum. Vaccin. 5:832–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cole LE, Yang Y, Elkins KL, Fernandez ET, Qureshi N, Shlomchik MJ, Herzenberg LA, Herzenberg LA, Vogel SN. 2009. Antigen-specific B-1a antibodies induced by Francisella tularensis LPS provide long-term protection against F. tularensis LVS challenge. Proc. Natl. Acad. Sci. U. S. A. 106:4343–4348. 10.1073/pnas.0813411106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kieffer TL, Cowley S, Nano FE, Elkins KL. 2003. Francisella novicida LPS has greater immunobiological activity in mice than F. tularensis LPS, and contributes to F. novicida murine pathogenesis. Microbes Infect. 5:397–403. 10.1016/S1286-4579(03)00052-2 [DOI] [PubMed] [Google Scholar]
- 41.Dreisenbach V, Cowley S, Elkins KL. 2000. Purified lipopolysaccharide from Francisella tularensis live vaccine strain (LVS) induces protective immunity against LVS infection that requires B cells and gamma interferon. Infect. Immun. 68:1988–1996. 10.1128/IAI.68.4.1988-1996.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ashtekar AR, Katz J, Xu Q, Michalek SM. 2012. A mucosal subunit vaccine protects against lethal respiratory infection with Francisella tularensis LVS. PLoS One 7:e50460. 10.1371/journal.pone.0050460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hickey AJ, Hazlett KR, Kirimanjeswara GS, Metzger DW. 2011. Identification of Francisella tularensis outer membrane protein A (FopA) as a protective antigen for tularemia. Vaccine 29:6941–6947. 10.1016/j.vaccine.2011.07.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rockx-Brouwer D, Chong A, Wehrly TD, Child R, Crane DD, Celli J, Bosio CM. 2012. Low dose vaccination with attenuated Francisella tularensis strain SchuS4 mutants protects against tularemia independent of the route of vaccination. PLoS One 7:e37752. 10.1371/journal.pone.0037752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jia Q, Lee BY, Bowen R, Dillon BJ, Som SM, Horwitz MA. 2010. A Francisella tularensis live vaccine strain (LVS) mutant with a deletion in capB, encoding a putative capsular biosynthesis protein, is significantly more attenuated than LVS yet induces potent protective immunity in mice against F. tularensis challenge. Infect. Immun. 78:4341–4355. 10.1128/IAI.00192-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mahawar M, Rabadi SM, Banik S, Catlett SV, Metzger DW, Malik M, Bakshi CS. 2013. Identification of a live attenuated vaccine candidate for tularemia prophylaxis. PLoS One 8:e61539. 10.1371/journal.pone.0061539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gregory AE, Titball R, Williamson D. 2013. Vaccine delivery using nanoparticles. Front. Microbiol. 3:13. 10.3389/fcimb.2013.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaler EW, Murthy AK, Rodriguez BE, Zasadzinski JA. 1989. Spontaneous vesicle formation in aqueous mixtures of single-tailed surfactants. Science 245:1371–1374. 10.1126/science.2781283 [DOI] [PubMed] [Google Scholar]
- 49.Šegota S, Težak D. 2006. Spontaneous formation of vesicles. Adv. Colloid Interface Sci. 121:51–75. 10.1016/j.cis.2006.01.002 [DOI] [PubMed] [Google Scholar]
- 50.Thomas GB, Rader LH, Park J, Abezgauz L, Danino D, DeShong P, English DS. 2009. Carbohydrate modified catanionic vesicles: probing multivalent binding at the bilayer interface. J. Am. Chem. Soc. 131:5471–5477. 10.1021/ja8076439 [DOI] [PubMed] [Google Scholar]
- 51.Danoff EJ, Wang X, Tung SH, Sinkov NA, Kemme AM, Raghavan SR, English DS. 2007. Surfactant vesicles for high-efficiency capture and separation of charged organic solutes. Langmuir 23:8965–8971. 10.1021/la070215n [DOI] [PubMed] [Google Scholar]
- 52.Ojogun VA, Lehmler HJ, Knutson BL. 2009. Cationic-anionic vesicle templating from fluorocarbon/fluorocarbon and hydrocarbon/fluorocarbon surfactants. J. Colloid Interface Sci. 338:82–91. 10.1016/j.jcis.2009.06.022 [DOI] [PubMed] [Google Scholar]
- 53.de Moreno MR, Smith JF, Smith RV. 1985. Silver staining of proteins in polyacrylamide gels: increased sensitivity through a combined Coomassie blue-silver stain procedure. Anal. Biochem. 151:466–470. 10.1016/0003-2697(85)90206-4 [DOI] [PubMed] [Google Scholar]
- 54.Prior JL, Prior RG, Hitchen PG, Diaper H, Griffin KF, Morris HR, Dell A, Titball RW. 2003. Characterization of the O antigen gene cluster and structural analysis of the O antigen of Francisella tularensis subsp. tularensis. J. Med. Microbiol. 52:845–851. 10.1099/jmm.0.05184-0 [DOI] [PubMed] [Google Scholar]
- 55.Alexander J, del Guercio MF, Maewal A, Qiao L, Fikes J, Chesnut RW, Paulson J, Bundle DR, DeFrees S, Sette A. 2000. Linear PADRE T helper epitope and carbohydrate B cell epitope conjugates induce specific high titer IgG antibody responses. J. Immunol. 164:1625–1633 [DOI] [PubMed] [Google Scholar]
- 56.Wang X, Danoff EJ, Sinkov NA, Lee JH, Raghavan SR, English DS. 2006. Highly efficient capture and long-term encapsulation of dye by catanionic surfactant vesicles. Langmuir 22:6461–6464. 10.1021/la0605135 [DOI] [PubMed] [Google Scholar]
- 57.Harris J, Sharp FA, Lavelle EC. 2010. The role of inflammasomes in the immunostimulatory effects of particulate vaccine adjuvants. Eur. J. Immunol. 40:634–638. 10.1002/eji.200940172 [DOI] [PubMed] [Google Scholar]
- 58.Kersten GF, Crommelin DJ. 2003. Liposomes and ISCOMs. Vaccine 21:915–920. 10.1016/S0264-410X(02)00540-6 [DOI] [PubMed] [Google Scholar]
- 59.Morein B, Hu KF, Abusugra I. 2004. Current status and potential application of ISCOMs in veterinary medicine. Adv. Drug Deliv. Rev. 56:1367–1382. 10.1016/j.addr.2004.02.004 [DOI] [PubMed] [Google Scholar]
- 60.Ryden P, Twine S, Shen H, Harris G, Chen W, Sjostedt A, Conlan W. 2013. Correlates of protection following vaccination of mice with gene deletion mutants of Francisella tularensis subspecies tularensis strain, SCHU S4 that elicit varying degrees of immunity to systemic and respiratory challenge with wild-type bacteria. Mol. Immunol. 54:58–67. 10.1016/j.molimm.2012.10.043 [DOI] [PubMed] [Google Scholar]
- 61.De Pascalis R, Chou AY, Bosio CM, Huang CY, Follmann DA, Elkins KL. 2012. Development of functional and molecular correlates of vaccine-induced protection for a model intracellular pathogen, F. tularensis LVS. PLoS Pathog. 8:e1002494. 10.1371/journal.ppat.1002494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Forestal CA, Malik M, Catlett SV, Savitt AG, Benach JL, Sellati TJ, Furie MB. 2007. Francisella tularensis has a significant extracellular phase in infected mice. J. Infect. Dis. 196:134–137. 10.1086/518611 [DOI] [PubMed] [Google Scholar]
- 63.Mara-Koosham G, Hutt JA, Lyons CR, Wu TH. 2011. Antibodies contribute to effective vaccination against respiratory infection by type A Francisella tularensis strains. Infect. Immun. 79:1770–1778. 10.1128/IAI.00605-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hubálek M, Hernychová L, Havlasová J, Kasalová I, Neubauerová V, Stulík J, Macela A, Lundqvist M, Larsson P. 2003. Towards proteome database of Francisella tularensis. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 787:149–177. 10.1016/S1570-0232(02)00730-4 [DOI] [PubMed] [Google Scholar]
- 65.Elkins KL, Colombini SM, Meierovics AI, Chu MC, Chou AY, Cowley SC. 2010. Survival of secondary lethal systemic Francisella LVS challenge depends largely on interferon gamma. Microbes Infect. 12:28–36. 10.1016/j.micinf.2009.09.012 [DOI] [PubMed] [Google Scholar]
- 66.Baron SD, Singh R, Metzger DW. 2007. Inactivated Francisella tularensis live vaccine strain protects against respiratory tularemia by intranasal vaccination in an immunoglobulin A-dependent fashion. Infect. Immun. 75:2152–2162. 10.1128/IAI.01606-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Robinson DS, O'Garra A. 2002. Further checkpoints in Th1 development. Immunity 16:755–758. 10.1016/S1074-7613(02)00331-X [DOI] [PubMed] [Google Scholar]
- 68.Kurtz SL, Foreman O, Bosio CM, Anver MR, Elkins KL. 2013. Interleukin-6 is essential for primary resistance to Francisella tularensis live vaccine strain infection. Infect. Immun. 81:585–597. 10.1128/IAI.01249-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen W, Shen H, Webb A, KuoLee R, Conlan JW. 2003. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen: protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine 21:3690–3700. 10.1016/S0264-410X(03)00386-4 [DOI] [PubMed] [Google Scholar]
- 70.Mann BJ, Ark NM. 2009. Rationally designed tularemia vaccines. Expert Rev. Vaccines 8:877–885. 10.1586/erv.09.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. 2005. Intranasal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect. Immun. 73:2644–2654. 10.1128/IAI.73.5.2644-2654.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Singh A, Rahman T, Malik M, Hickey AJ, Leifer CA, Hazlett KR, Sellati TJ. 2013. Discordant results obtained with Francisella tularensis during in vitro and in vivo immunological studies are attributable to compromised bacterial structural integrity. PLoS One 8:e58513. 10.1371/journal.pone.0058513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wilton JM. 1978. Suppression by IgA of IgG-mediated phagocytosis by human polymorphonuclear leucocytes. Clin. Exp. Immunol. 34:423–428 [PMC free article] [PubMed] [Google Scholar]
- 74.Juruj C, Lelogeais V, Pierini R, Perret M, Py BF, Jamilloux Y, Broz P, Ader F, Faure M, Henry T. 2013. Caspase-1 activity affects AIM2 speck formation/stability through a negative feedback loop. Front. Cell. Infect. Microbiol. 3:14. 10.3389/fcimb.2013.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cremer TJ, Amer A, Tridandapani S, Butchar JP. 2009. Francisella tularensis regulates autophagy-related host cell signaling pathways. Autophagy 5:125–128. 10.4161/auto.5.1.7305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Asare R, Kwaik YA. 2010. Exploitation of host cell biology and evasion of immunity by Francisella tularensis. Front. Microbiol. 1:145. 10.3389/fmicb.2010.00145 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.