Abstract
Study Objectives:
To examine associations between specific parasomnias and psychotic experiences in childhood.
Design:
Birth cohort study. Information on the presence of frequent nightmares in children was obtained prospectively from mothers during multiple assessments conducted when children were aged between 2.5 and 9 y. Children were interviewed at age 12 y about nightmares, night terrors, sleepwalking, and psychotic experiences (delusions, hallucinations, and thought interference) occurring in the previous 6 mo.
Setting:
Assessments were completed in participants' homes or a University clinic within the UK.
Patients or Participants:
There were 6,796 children (3,462 girls, 50.9%) who completed the psychotic experiences interview.
Measurements and Results:
Children who were reported by their mothers as experiencing frequent nightmares between 2.5 and 9 y of age were more likely to report psychotic experiences at age 12 y, regardless of sex, family adversity, emotional or behavioral problems, IQ and potential neurological problems (odds ratio (OR) = 1.16, [95% confidence intervals (CI) = 1.00, 1.35], P = 0.049). Children reporting any of the parasomnias at age 12 y also had higher rates of concurrent psychotic experiences than those without such sleeping problems, when adjusting for all confounders (OR = 3.62 [95% CI = 2.57, 5.11], P < 0.001). Difficulty getting to sleep and night waking were not found to be associated with psychotic experiences at age 12 y when controlling for confounders.
Conclusion:
Nightmares and night terrors, but not other sleeping problems, in childhood were associated with psychotic experiences at age 12 years. These findings tentatively suggest that arousal and rapid eye movement forms of sleep disorder might be early indicators of susceptibility to psychotic experiences.
Citation:
Fisher HL; Lereya ST; Thompson A; Lewis G; Zammit S; Wolke D. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort. SLEEP 2014;37(3):475-482.
Keywords: ALSPAC, nightmares, night terrors, parasomnias, psychosis, sleepwalking
INTRODUCTION
Psychotic experiences are reported by a substantial minority of individuals in late childhood1,2 and include paranoid thoughts, hearing or seeing things that others do not, and believing that others can read one's mind or vice versa. These experiences are often distressing in their own right3 and have been shown to predict the development of schizophrenia and other psychiatric disorders in adulthood.4,5 The etiology of childhood psychotic experiences thus warrants investigation and may provide insight into how to identify children at increased risk of developing severe mental health problems in adulthood, in order to more effectively target preventive interventions.
One possible early indicator of susceptibility to psychosis is experience of parasomnias, which tend to occur most frequently during childhood.6–8 Historically, frequent nightmares have been postulated to be involved in the emergence of psychosis,9,10 often due to the similarities between dream states while asleep and daytime hallucinations.11,12 Indeed, nightmares have been shown to be associated with psychotic experiences and magical thinking in adults.13–20 For instance, Hartman et al.15 found that 12 individuals who suffered frequent nightmares scored higher on psychotic beliefs than 12 frequent dreamers and 12 individuals who had neither nightmares or vivid dreams. Moreover, Levin18 reported that 30 female college students who had frequent nightmares were more likely to experience illusions and have magical beliefs than 30 others who only rarely had nightmares. Nightmares have also been demonstrated to occur more commonly among individuals taking antipsychotic medications21 and those in whom psychotic disorders have been diagnosed.22
However, these existing studies have several methodological limitations, including small sample sizes recruited via convenience methods, reliance on self-report questionnaires of psychotic experiences, and cross-sectional assessments. Moreover, to our knowledge no studies have been conducted with children and, aside from one report exploring associations between night terrors, sleepwalking, and sleep-related hallucinations,23 there has been no investigation of the potential relationship between other parasomnias and psychotic experiences.
Therefore, we sought to investigate using a large birth cohort from the UK whether the common parasomnias, such as nightmares, night terrors, or sleepwalking, during childhood were associated with psychotic experiences when children were 12 y of age. This study extends previous research by examining associations between prospectively obtained information from mothers on their children's nightmares based on repeated assessments and psychotic experiences that were judged to be definitely present by clinicians using information elicited through semi-structured interviews with the children. Thus, this aspect of the study provides more rigorous measurement of the exposure and outcome as well as their temporal order compared to previous studies, and avoids the problems associated with shared method variance. We were also able to explore associations between other forms of parasomnia (night terrors and sleep walking) and psychotic experiences, though only in a concurrent manner. Additionally, in order to rule out the possibility that any psychotic experiences were associated with sleep, such as the child falling asleep (hypnagogic) or waking up (hypnopompic), analyses were also conducted for psychotic experiences excluding those attributed to sleep. Finally, we were able to control for emotional and behavioral problems along with diagnosable psychiatric disorders to rule out the potentially confounding effects of depression, anxiety, and attention deficit /hyperactivity disorder (ADHD), all of which have previously been linked to parasomnias24,25 and psychotic experiences.26,27
METHODS
Participants
The Avon Longitudinal Study of Parents and Children (ALSPAC) is a birth cohort study, set in the UK, examining the determinants of development, health and disease during childhood and beyond.28,29 Briefly, women who were residents in Avon while pregnant, and had an expected delivery date between April 1, 1991 and December 31, 1992 were approached to participate in the study, leading to 14,775 live births and 14,701 alive at 1 y of age. From the first trimester of pregnancy, parents completed postal questionnaires about themselves and the study child's health and development. Children were invited to attend annual assessment clinics, including face-to-face interviews and psychological and physical tests from age 7 y onward. Please note that the study website contains details of all of the data that is available through a fully searchable data dictionary: http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/. This analysis is based on 6,796 children who completed the Psychosis-Like Symptoms semistructured interview (PLIKSi) at approximately 12 y of age. Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees and informed consent was provided by all participants.
Outcome Variable
Psychotic experiences age 12 y: The Psychosis-Like Symptom interview (PLIKSi) is a semi-structured face-to-face interview conducted in private with each child when s/he was an average age of 12.9 y.30 The PLIKS interview consisted of 12 core questions eliciting key psychotic experiences covering hallucinations (visual and auditory), delusions (spied on, persecution, thoughts read, reference, control, grandiosity and other unspecified delusions), and experiences of thought interference (thought broadcasting, insertion, and withdrawal) over the previous 6 mo. For these core items, seven stem questions were derived from the Diagnostic Interview Schedule for Children-IV (DISC-IV)31 and five from the Schedules for Clinical Assessment in Neuropsychiatry version 2.0 (SCAN 2.0).32 Coding followed the glossary definitions and rating rules for SCAN and the items were assessed as not present, suspected, or definitely present with an average kappa value for interrater reliability of 0.72.30 Ambiguous descriptions of psychotic experiences were checked by clinicians to ensure validity. Two main PLIKSi outcomes are considered in this article: (1) ≥ 1 of the 12 PLIKSi experiences definitely present including those attributable to sleep, fever or substance use; (2) ≥ 1 of the 12 PLIKSi experiences definitely present and not attributable to sleep, fever, or substance use.
Predictor Variables
Sleep problems during preschool and school were derived from postal questionnaires completed by mothers when the children were age 2.5, 3.5, 4.75, 5.75, 6.75, and 9 y. Specifically, mothers were asked: “In the past year, has your child regularly had nightmares?” (nightmares); “In the past year, has your child regularly had difficulty going to sleep?” (sleep onset problems); “In the past year, has your child regularly woken in the night?” (night waking). The presence of nightmares at one time period, two time periods, and three or more time periods versus no nightmares was considered here in order to assess the persistence of nightmares during the preschool and school period. Children were excluded from the analysis if they did not have nightmare data available for at least three time periods. Identical definitions of persistence and missingness were used for sleep onset problems and night waking.
Sleep problems at 12 y were assessed via face-to-face semistructured interviews with the children when they were an average age of 12.9 y. The interviews were conducted by psychology graduates who were trained to a gold standard and attended a monthly clinic with the study's consultant psychiatrists to obtain consensus on difficult to rate cases. The children were asked a series of questions concerning nightmares, night terrors, and sleepwalking during the 6 mo prior to the interview based on the Diagnostic and Statistical Manual of Mental Disorders - IV (DSM-IV)33 criteria for sleep disorders (nightmares: “Since your 12th birthday have you had any dreams that woke you up? Were they frightening?”; night terrors: “Has anyone ever told you, since you were 12, that you scream out at night, sit up in bed, seem to fight or wrestle with unseen creatures or shout at them in your sleep?”; sleep-walking: “Has anyone ever told you, since you were 12, that you got out of bed and walked around while you were fast asleep?”). Positive responses were probed to obtain further information to distinguish between nightmares and night terrors (e.g., when they occurred at night, amnesia upon awakening, etc.).34 A full list of questions and response categories is provided in Table S1 in the supplemental material. An overall rating of not present (0), “suspected” (1), or “definitely” (2) present was then made for each type of parasomnia based on all the information obtained. “Definitely present” was rated when all criteria for a specific parasomnia were fulfilled and “suspected” when most but not all criteria were fulfilled after probing. The average kappa value for inter-rater reliability was 0.72. Sleeping problems coded overall as suspected or definitely present were used in the current analysis. Another variable was derived (any parasomnia) to reflect whether the children had reported any of these particular parasomnias (nightmare and/or night terror and/or sleepwalking) at 12 y of age.
Confounders
An abbreviated form of the Wechsler Intelligence Scale for Children-III (UK version)35 was used to derive an overall IQ (grand mean = 103.53, standard deviation [SD] = 21.14) for the children who attended the ALSPAC 8-y clinic.
In order to exclude potential neurological problems, motor ability was assessed at 7 y of age with the Movement Assessment Battery for Children (Movement ABC).36 For analysis, the total ABC score was dichotomized into the top 15th percentile (the cutoff normally used to identify those with or at risk of developmental coordination disorder) versus the rest.37 A total of 8.0% (n = 399) of the children in the sample were classified as being at risk for developmental coordination disorder.
Multiple family risk factors were assessed during pregnancy with the Family Adversity Index (FAI).38 The FAI consists of 17 items (e.g., financial difficulties, crime involvement, problematic partner relationships) taken from questionnaires administered throughout pregnancy. Adversity present in each item was rated as 1, and the scores were totaled across the 17 items (Grand Mean = 1.05, SD = 1.42).
DSM-IV33 psychiatric diagnoses were made at 7 y using the Development and Well-Being Assessment (DAWBA)39 based on parent and teacher reports. The presence of any Axis I diagnosis of ADHD, conduct disorder, oppositional defiant disorder, depression, or anxiety versus no diagnosis were considered. A total of 5.2% (n = 310) of the children in the sample had any of these Axis I diagnoses.
Assessment of internalizing/externalizing behavior was estimated using the sum of negative emotionality, hyperactivity, and conduct problems taken from the Strengths and Difficulties Questionnaire (SDQ)40 completed by parents at ages 4, 6.75, and 9.5 y (4 y grand mean = 7.38, SD = 3.89; 6.75 y grand mean = 6.32, SD = 3.99; 9.5 y grand mean = 5.54, SD = 3.97).
Statistical Analyses
Selective dropout was determined by comparing those who completed the PLIKS interview at age 12 y to those who did not, using binary logistic regression in the Statistical Package for the Social Sciences (SPSS) version 20 for Windows (IBM Corporation) and odds ratios (OR) are reported with 95% confidence intervals (CI) (Table 1). To assess whether persistence of nightmares during the preschool or school years or the specific parasomnias at age 12 y were associated with psychotic experiences at age 12 y, two sets of logistic regression analyses were conducted (Table 2). Model A shows unadjusted analyses. Model B controlled for sex, FAI, IQ, any risk for developmental coordination disorder (Movement ABC), any DSM-IV Axis I diagnosis (DAWBA), and internalizing/externalizing behavior at preschool or elementary school age (SDQ). In order to rule out the possibility that any psychotic experiences associated with the parasomnias were only those that occurred when a child was falling asleep (hypnagogic) or waking up (hypnopompic), analyses were also conducted for psychotic experiences excluding those attributed to sleep (or fever or substance misuse). Last, logistic regression was used to assess whether childhood nightmares increased the risk of later parasomnias at age 12 y (Table 3).
Table 1.
Dropout analysis with regard to availability of PLIKS interview
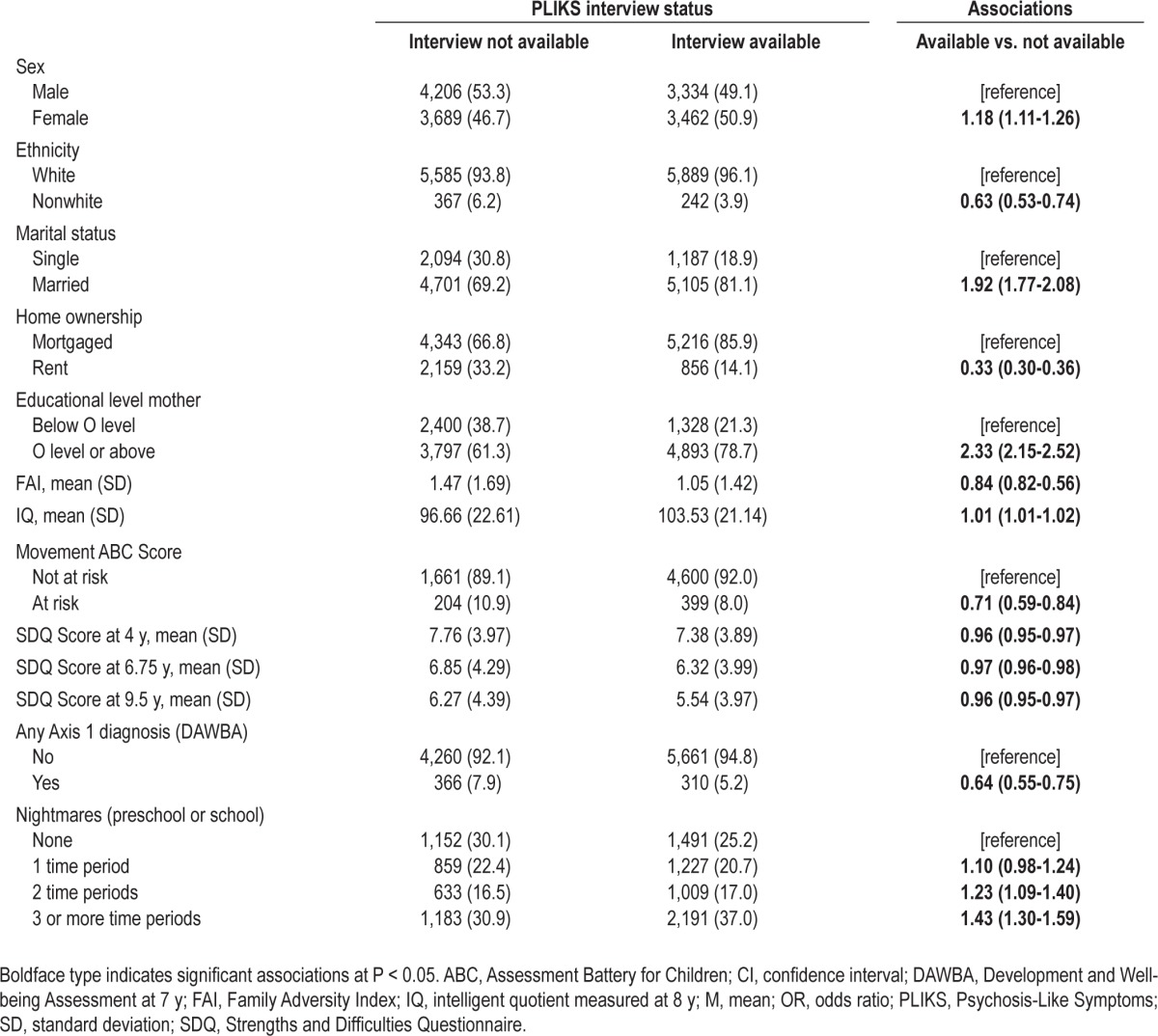
Table 2.
Childhood parasomnias and definite psychotic experiences at 12 y with or without attribution to sleep, fever or substance use Definite PE with attributes Definite PE without attributes Model Aa
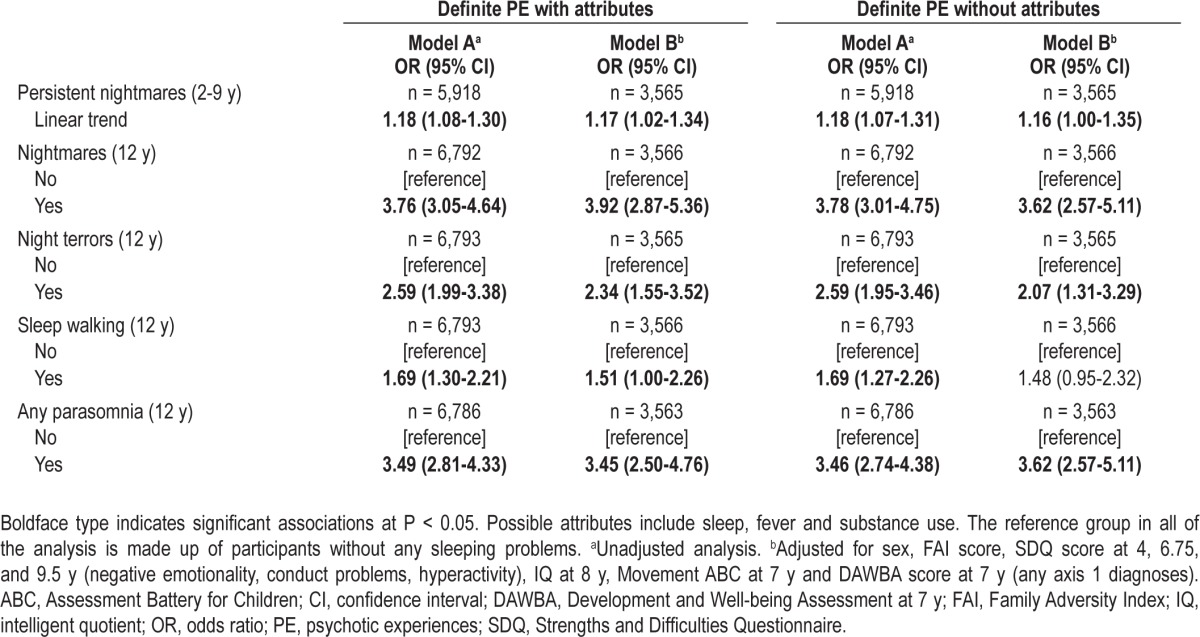
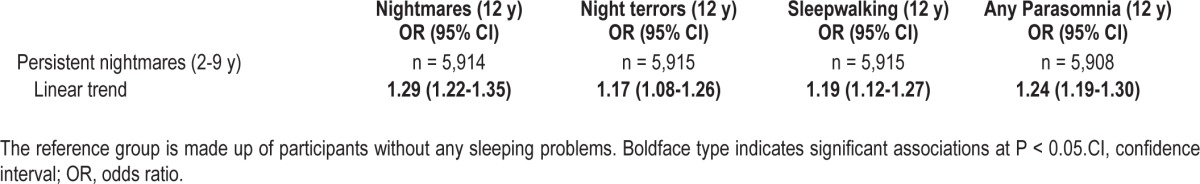
Table 3.
Persistence of nightmares during childhood and reports of parasomnias at age 12 y Nightmares (12 y)
As the childhood persistent nightmares variable involves four ordinal categories (0, not reported; 1, regular nightmares reported at one time period; 2, reports at two time periods; and 3, reports at three or more time periods), the results are presented as a linear trend across these categories with 0 (no nightmares) as the reference group. To obtain OR for each category, the OR for the linear trend is exponentiated using the category number (OR value to the power of 1, 2, or 3). Thus, if the linear trend OR was X, then for nightmares reported at one time period the OR = X1, for two time periods OR = X2, and for three or more time periods OR = X3. To assess the clinical meaningfulness of the findings regarding the association between the childhood persistent nightmares and psychotic experiences, a population attributable fraction was calculated for psychotic experiences without attributes with persistent nightmares dichotomized conservatively into reports at none, one, or two time periods versus three or more time periods using the ‘punaf’ command in Stata (v11.2; Stata Corporation, College Station, Texas). These were not calculated for parasomnias at age 12 y as these were cross-sectionally assessed.
RESULTS
Differences Between Participants With and Without PLIKSi
The frequencies of sociodemographic factors, family environment, and child characteristics are shown for ALSPAC participants with and without the PLIKS interview at 12 y in Table 1. Those who did not complete the PLIKS interview were more often nonwhite boys born to single mothers of lower education level, from families living in rented properties. These children were more likely to have a lower IQ at age 8 y; more behavioral problems during childhood and any DSM-IV psychiatric diagnosis at age 7 y. The non-completers were also more likely to be at risk for developmental coordination disorder and have more nightmares in the preschool or school period. In this study, we did not use any statistical method for imputing missing values but did repeat the analyses with data weighted to account for the selective dropout and did not find substantially different results. This study reports the results only for children who completed the PLIKS interview at 12 y of age (n = 6,796; 3,462 girls, 50.9%).
Prevalence of Sleep Problems and Psychotic Experiences
Mothers of 1,491 children (25.2%) did not report any nightmares, 1,227 (20.7%) reported children having regular nightmares at one time period, 1,009 (17.0%) reported children having nightmares at two time periods and 2,191 (37.0%) reported children having nightmares at three or more time periods. At age 12 y, 1,655 children (24.4%) reported having nightmares in the previous 6 mo, 633 (9.3%) reported having night terrors, and 853 (12.6%) reported sleepwalking during this period. Overall at age 12 y, 2,458 children (36.2%) reported experiencing at least one type of parasomnia.
At age 12 y, 384 children (5.7%) were judged to have one or more definite psychotic experiences, including those attributable to sleep, fever, or substance use, and 320 (4.7%) had definite psychotic experiences not attributable to any of these factors.
Parasomnias and Psychotic Experiences at Age 12 Y
Prospective associations between childhood nightmares and age 12 y psychotic experiences along with concurrent occurrence of specific parasomnias are presented in Table 2. Persistent nightmares during the preschool and school periods were associated with definite psychotic experiences, both including and excluding those attributable to sleep, fever, or substance use, even after controlling for potential confounders. The adjusted linear trend of 1.16 for nonattributable psychotic experiences equates to an OR of 1.16 (1.161) for regular nightmares reported at only one time period, an OR of 1.35 (1.162) for reports at two time periods and an OR of 1.56 (1.163) for three or more time periods, all compared to having no nightmares. Splitting the childhood nightmares conservatively into none, one, or two time periods versus reports at three or more time periods, yields a population attributable fraction of 12.9% (95% CI 3.4% to 21.5%) for definite psychotic experiences without attributes, suggesting that a small proportion of children with psychotic experiences would be prevented from developing them if persistent nightmares could be eliminated (assuming that a true and causal relationship exists between them). No associations were found between other persistent sleep problems during childhood (difficulty getting to sleep or night waking) and age 12 y psychotic experiences when adjustment was made for potential confounders (see Table S2 in the supplemental material).
Associations were evident between ‘any parasomnias’, nightmares and night terrors reported at age 12 y, and both definite psychotic experiences with or without attributes (Table 2). However, the associations between sleepwalking and definite psychotic experiences were weaker and the OR fell short of statistical significance when all the confounders were added to the model for definite psychotic experiences without attributes. When all three types of parasomnia were included in the model together, only concurrent nightmares and night terrors were independently associated with definite psychotic symptoms with (nightmares: OR = 3.43 [95% CI 2.77, 4.25], P < 0.001; night terrors: OR = 1.88 [95% CI 1.42, 2.48], P < 0.001) or without attributes (nightmares: OR = 3.44 [95% CI 2.73, 4.35], P < 0.001; night terrors: OR = 1.86 [95% CI 1.38, 2.52], P < 0.001), while no independent association was evident for sleepwalking (with attributes: OR = 1.25 [95% CI 0.95, 1.65], P = 0.112; without attributes: OR = 1.25 [95% CI 0.92, 1.68], P = 0.152).
Childhood Nightmares and Parasomnias at Age 12 Y
Within this sample it is only possible to explore prospectively the associations between frequent nightmares in childhood and age 12 y psychotic experiences. However, reports of persistent nightmares during the preschool and school periods were predictive of each type of parasomnia at age 12 y (see Table 3). These findings suggest that the prospective nightmare results might extrapolate to these other forms of parasomnia.
DISCUSSION
This large birth cohort study found that the persistence of nightmares during the preschool and school years (2.5 to 9 y of age) was associated prospectively with psychotic experiences at age 12 y. This association held regardless of family adversity, emotional or behavioral problems, IQ, and potential neurological problems. Twelve-y-old children who reported specific parasomnias (night terrors, nightmares, or sleepwalking) were also more likely to have concurrent psychotic experiences, although the association with sleepwalking was weaker and became nonsignificant for nonattributable psychotic experiences when other potentially confounding factors were taken into account. These findings extend those of previous studies in adults that mainly relied on cross-sectional assessments and self-report questionnaires of psychotic experiences.13–20 The specificity of these parasomnias rather than other sleeping problems to psychotic experiences (after adjustment for potential confounders) echoes the findings of Koffel and Watson,41 who reported associations between unusual sleeping problems and schizotypy (a broader concept of psychosis proneness), but not for other sleep disturbances.
Furthermore, the current study was able to demonstrate that associations were present for definite psychotic experiences at age 12 y that were not attributable to sleep, fever, or substance misuse, thus ruling out potential misclassification by excluding hypnagogic and hypnopompic hallucinations. These are often considered as within the range of ‘normal’ human experience and classified as symptoms of sleep disorders, such as narcolepsy,33 rather than as psychotic symptoms, though they have been shown to co-occur frequently with daytime hallucinations.42
Several possible mechanisms could account for the associations found here between parasomnias and psychotic experiences. First, Mahowald and Schenck43,44 hypothesized that the boundaries between being asleep and awake may be too flexible in some individuals, resulting in brief lapses into rapid eye movement (REM) sleep (within which nightmares are experienced) occurring while they are awake, resulting in the experience of hallucinations during the day. Similarly, slipping into a waking state while in nonrapid eye movement (NREM) sleep is postulated to account for the occurrence of night terrors and sleepwalking. This would seem to suggest that parasomnias would be related mainly to hypnagogic and hypnopompic hallucinations; however, in the current study, associations with psychotic experiences held even when these phenomena were excluded. Moreover, evidence of intrusions of REM sleep into waking states have not been found in patients with schizophrenia experiencing hallucinations,45 although some studies have found poor sleep/wake boundaries among individuals with psychotic symptoms.46,47
Another possible mechanism is exposure to stressful experiences in childhood. Exposure to sexual abuse48 or disasters49 during childhood have been linked to the occurrence of nightmares. Such early adverse experiences have also been shown to increase the likelihood of developing psychotic experiences in late childhood.50,51 Given the association found in the current study between nightmares and psychotic experiences at age 12 y, it is possible that exposure to such traumatic events in childhood could trigger the development of nightmares, which then in turn may lead to the emergence of psychotic experiences. This might occur through dissociative or posttraumatic phenomena arising from exposure to childhood trauma,52,53 both of which are discussed in detail in the next paragraph in relation to nightmares and psychotic experiences. Early trauma could also confound the association between parasomnias and psychotic experiences through its association with both. Further research is required to explore these potential pathways.
Finally, dissociation (separation of mental functions that are usually integrated) could underlie the association between parasomnias and psychotic experiences. Dissociative symptoms (e.g., feeling detached from oneself or reality, being unable to recall details about the self, etc.) have been shown to co-occur with psychotic experiences54 and have been linked with nightmares.17,41,55 Within the current sample, children reported on two dissociative symptoms at age 12 y (depersonalization and derealization) and adjusting for these items did not substantially alter the association between parasomnias and psychotic experiences (definite with attributes: adjusted OR = 3.09, [95% CI 2.48, 3.85], P < 0.001; definite without attributes: adjusted OR = 3.06, [95% CI 2.41, 3.89], P < 0.001), although further investigation with a full dissociation scale is warranted.
The findings should be considered in light of the following limitations. First, relevant data were not available for the entire ALSPAC cohort reducing statistical power and selective dropout may have biased the results. Nevertheless, empirical simulations demonstrate that even when dropout is correlated with predictor/confounder variables, the relationship between predictors and outcome is unlikely to be substantially altered by selective dropout processes.56 Indeed, weighting the data to account for the factors on which those included and not included in this analysis differed did not substantially alter the results, but the dropout rate may still limit the generalizability of the findings.
Second, of the parasomnias, only nightmares were assessed prospectively from preschool age. In addition, it is not possible from the data obtained to know how frequently the nightmares occurred at each assessment point because parents were asked simply if the children had ‘regular’ nightmares. Nonetheless, the definition of persistent nightmares was based on the reports obtained at different time periods during childhood, indicating that nightmares did at least persist over time even if the actual frequency of their occurrence was unknown. Parents also had no definition to distinguish between more prevalent nightmares and more rarely occurring night terrors, which are sometimes confused.34 This may partly explain the prediction of repeated nightmares to night terrors at 12 y of age and suggests that this study cannot definitively determine which of these two parasomnias are associated with psychotic experiences.
Third, reports of night terrors and sleepwalking were obtained at the same assessment time period as the psychotic experiences. Hence, it is not possible to ascertain whether these parasomnias occurred before or after the emergence of psychotic experiences, thus preventing any conclusions being drawn concerning cause and effect. There were, however, robust associations between persistent nightmares in childhood and the parasomnias reported at age 12 y, suggesting possible overlap between these parasomnias and that prospective associations with psychotic experiences could potentially be extrapolated to night terrors or sleepwalking. Nonetheless, it would be useful to extend these analyses in the future to explore associations between childhood parasomnias and psychotic experiences in young adulthood. This would also allow examination of the effect of childhood sleeping disorders on the persistence of psychotic experiences across adolescence. Persistent psychotic experiences are considered to be stronger predictors of transition to clinically relevant psychotic disorders than psychotic experiences only reported at one time point.57
The prevalence of night terrors (9.3%) and sleepwalking (12.6%) found in the current sample at age 12 y was also higher than has previously been reported for children of a similar age. These types of parasomnia tend to become less frequent by late childhood and a study conducted by Laberge et al.58 of a representative sample of children from Canada found that only 2.3% of them were still experiencing night terrors and only 6.8% were sleepwalking by 12 y of age. One possible reason for the discrepancy is that the current study used self-reports of sleeping difficulties, whereas the study by Laberge et al.58 used parental reports. This might have led to an overestimation of the true prevalence of these parasomnias in the full population. Therefore, the associations between night terrors, sleepwalking, and psychotic experiences at age 12 y should be interpreted cautiously in light of this limitation and future studies should have different informants reporting on the occurrence of parasomnias (e.g., parents) and psychotic experiences (e.g., child) to avoid the problems associated with shared method variance.
It is also possible that the findings could have been due to the presence of post-traumatic stress disorder (PTSD) in the children. Nightmares are common symptoms of PTSD59 and the psychotic experiences that the children reported could actually have been flashbacks of traumatic experiences incorrectly classified as psychotic experiences, or at least these experiences might co-occur with such PTSD symptoms.60 However, examination of the cohort revealed that PTSD was diagnosed in only one of the children by 12 y of age, and this individual did not report any psychotic experiences, thus ruling this out as an explanation for the results of this study. Another potential confounder is having an insufficient total amount of sleep, which has been associated with both parasomnias61 and psychotic experiences.62 Unfortunately, this was not measured across childhood in our sample so it remains a possible explanation for our findings.
In conclusion, this large birth cohort study found robust associations between prospectively assessed persistent nightmares occurring during childhood and definite psychotic experiences reported by children at 12 y of age that were not attributable to sleep or other factors. Several types of parasomnia (nightmares, night terrors and to a lesser extent sleepwalking) were also more commonly reported by 12-y-old children who had psychotic experiences than those who did not. These findings tentatively suggest that these REM and NREM arousal sleep disorders may be early indicators of psychotic experiences in late childhood/early adolescence. If replicated, this could have important implications for assisting clinicians in identifying children who were at most risk of having psychotic experiences. This could potentially lead to more effective targeting of sleep or psychological interventions to prevent the emergence of psychotic experiences among children or minimize the persistence of such experiences. The estimated population attributable fraction indicated that eliminating persistent nightmares might prevent approximately 13% of children with psychotic experiences from developing them. This level of attributable fraction appears small but is considerable when compared, for example, to being obese (body mass index > 30), which occurs in 15% of the population but accounts for only around 2.8% of myocardial infarctions.63 Nonetheless, this possibility of prevention should be considered with caution because it is not possible to say whether the association between nightmares and psychotic experiences is causal, and more research is required to ascertain whether nightmares can actually be prevented or successfully treated. The current findings also tentatively suggest that clinicians who encounter children who are still experiencing frequent nightmares, night terrors, or sleepwalking at 12 y of age might consider inquiring about the presence of concurrent psychotic experiences. This would allow affected children to access psychological help to deal with any associated distress and also potentially reduce the likelihood of developing severe psychopathology in adulthood.4
DISCLOSURE STATEMENT
This was not an industry supported study. The UK Medical Research Council (MRC) and the Wellcome Trust (grant 092731) and the University of Bristol provide core support for ALSPAC. Data collection was partly funded by an MRC grant (G0701503). Drs Wolke and Lereya's work on this study was supported by the Economic and Social Research Council (ESRC) grant ES/K003593/1. Dr Fisher is funded by an MRC Population Health Scientist fellowship (G1002366). Dr Zammit received support from a Clinician Scientist Award funded by the National Assembly for Wales. Dr Lewis is an NIHR Senior Investigator. None of the funding bodies had any further role in the collection, analysis or interpretation of data, the writing of this manuscript, or the decision to submit this manuscript for publication. This publication is the work of the authors, and Drs Fisher and Wolke serve as guarantors for the contents of this paper. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Drs Fisher and Lereya contributed equally to this work. The authors are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting the families, and the entire Avon Longitudinal Study of Parents and Children (ALSPAC) team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses.
ABBREVIATIONS
- ABC
Movement Assessment Battery for Children
- ALSPAC
Avon Longitudinal Study of Parents and Children
- CI
confidence interval
- DAWBA
Development and Well-being Assessment
- DISC-IV
Diagnostic Interview Schedule for Children 4th edition
- DSM-IV
Diagnostic and Statistical Manual for Mental Disorders 4th edition
- FAI
Family Adversity Index
- NREM
non-rapid eye movement
- OR
odds ratio
- PE
psychotic experiences
- PLIKSi
Psychosis-Like Symptoms semi-structured interview
- REM
rapid eye movement
- SCAN
Schedules for Clinical Assessment in Neuropsychiatry
- SD
standard deviation
- SDQ
Strengths and Difficulties Questionnaire
- SPSS
Statistical Package for the Social Sciences
SUPPLEMENTAL MATERIAL
Parasomnia questions from age 12 y interview with children
Childhood sleeping problems and psychotic experiences at 12 y with or without attribution to sleep, fever or substance use
REFERENCES
- 1.Laurens KR, Hodgins S, Maughan B, Murray RM, Rutter ML, Taylor EA. Community screening for psychotic-like experiences and other putative antecedents of schizophrenia in children aged 9-12 years. Schizophr Res. 2007;90:130–46. doi: 10.1016/j.schres.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta- analysis of population-based studies. Psychol Med. 2012;42:1857–63. doi: 10.1017/S0033291711002960. [DOI] [PubMed] [Google Scholar]
- 3.Armando M, Nelson B, Yung AR, et al. Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr Res. 2010;119:258–65. doi: 10.1016/j.schres.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Fisher HL, Caspi A, Poulton R, et al. Specificity of childhood psychotic symptoms for predicting schizophrenia by 38 years of age: a birth cohort study. Psychol Med. 2013;43:2077–86. doi: 10.1017/S0033291712003091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Werbeloff N, Drukker M, Dohrenwend BP, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. 2012;69:467–75. doi: 10.1001/archgenpsychiatry.2011.1580. [DOI] [PubMed] [Google Scholar]
- 6.DiMario FJ, Jr, Emery ES. The natural history of night terrors. Clin Pediatr (Phila) 1987;26:505–11. doi: 10.1177/000992288702601002. [DOI] [PubMed] [Google Scholar]
- 7.Klackenberg G. Somnambulism in childhood--prevalence, course and behavioral correlations. A prospective longitudinal study (6-16 years) Acta Paediatr Scand. 1982;71:495–9. doi: 10.1111/j.1651-2227.1982.tb09458.x. [DOI] [PubMed] [Google Scholar]
- 8.Yang L, Zuo C, Eaton LF. Research note: sleep problems of normal Chinese adolescents. J Child Psychol Psychiatry. 1987;28:167–72. doi: 10.1111/j.1469-7610.1987.tb00660.x. [DOI] [PubMed] [Google Scholar]
- 9.Detre TR, Jarecki HG, editors. Modern psychiatric treatment. New York, NY: JB Lippincott; 1971. [Google Scholar]
- 10.Mack JE. Nightmares and human conflict. Boston, MA: Little Brown; 1970. [Google Scholar]
- 11.Jung CG. On the psychogenesis of schizophrenia. J Ment Sci. 1939;85:999–1011. [Google Scholar]
- 12.West LJ. A general theory of hallucinations and dreams. In: West LJ, editor. Hallucinations. New York: Grune & Stratton; 1962. [Google Scholar]
- 13.Claridge G, Clark K, Davis C. Nightmares, dreams, and schizotypy. Br J Clin Psychol. 1997;36:377–86. doi: 10.1111/j.2044-8260.1997.tb01245.x. [DOI] [PubMed] [Google Scholar]
- 14.Fennig S, Salganik E, Chayat M. Psychotic episodes and nightmares: a case study. J Nerv Ment Dis. 1992;180:60. doi: 10.1097/00005053-199201000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Hartmann E, Russ D, Oldfield M, Sivan I, Cooper S. Who has nightmares? The personality of the lifelong nightmare sufferer. Arch Gen Psychiatry. 1987;44:49–56. doi: 10.1001/archpsyc.1987.01800130053008. [DOI] [PubMed] [Google Scholar]
- 16.Kales A, Soldatos CR, Caldwell AB, et al. Nightmares: clinical characteristics and personality patterns. Am J Psychiatry. 1980;137:1197–201. doi: 10.1176/ajp.137.10.1197. [DOI] [PubMed] [Google Scholar]
- 17.Knox JA. Context effects examined: imagination, sleep experiences, dissociation, and schizotypy. Dissertation Abstracts International. 2008;68:7B. (UMI No. 3274108) [Google Scholar]
- 18.Levin R. Nightmares and schizotypy. Psychiatry. 1998;61:206–16. doi: 10.1080/00332747.1998.11024832. [DOI] [PubMed] [Google Scholar]
- 19.Levin R, Fireman G. Nightmare prevalence, nightmare distress, and self-reported psychological disturbance. Sleep. 2002;25:205–12. [PubMed] [Google Scholar]
- 20.Levin R, Raulin ML. Preliminary evidence for the proposed relationship between frequent nightmares and schizotypal symptomatology. J Pers Disord. 1991;5:8–14. [Google Scholar]
- 21.Hublin C, Kaprio J, Partinen M, Koskenvuo M. Nightmares: familial aggregation and association with psychiatric disorders in a nationwide twin cohort. Am J Med Genet. 1999;88:329–36. doi: 10.1002/(sici)1096-8628(19990820)88:4<329::aid-ajmg8>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 22.Hartmann E, Russ D, van der Kolk B, Falke R, Oldfield M. A preliminary study of the personality of the nightmare sufferer: Relationship to schizophrenia and creativity? Am J Psychiatry. 1981;138:794–7. doi: 10.1176/ajp.138.6.794. [DOI] [PubMed] [Google Scholar]
- 23.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60:268–76. doi: 10.4088/jcp.v60n0413. [DOI] [PubMed] [Google Scholar]
- 24.Schredl M, Fricke-Oerkermann L, Mitschke A, Wiater A, Lehmkuhl G. Longitudinal study of nightmares in children: stability and effect of emotional symptoms. Child Psychiatry Hum Dev. 2009;40:439–49. doi: 10.1007/s10578-009-0136-y. [DOI] [PubMed] [Google Scholar]
- 25.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:E60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 26.Freeman D, Stahl D, McManus S, et al. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1195–203. doi: 10.1007/s00127-011-0433-1. [DOI] [PubMed] [Google Scholar]
- 27.Rubino IA, Frank E, Croce Nanni R, Pozzi D, Lanza di Scalea T, Siracusano A. A comparative study of axis I antecedents before age 18 of unipolar depression, bipolar disorder and schizophrenia. Psychopathology. 2009;42:325–32. doi: 10.1159/000232975. [DOI] [PubMed] [Google Scholar]
- 28.Boyd A, Golding J, Macleod J, et al. Cohort Profile: The ‘Children of the 90s’--the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–27. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fraser A, Macdonald-Wallis C, Tilling K, et al. Cohort Profile: The Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42:97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horwood J, Salvi G, Thomas K, et al. IQ and non-clinical psychotic symptoms in 12-year-olds: results from the ALSPAC birth cohort. Br J Psychiatry. 2008;193:185–91. doi: 10.1192/bjp.bp.108.051904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. Washington, DC: American Psychiatric Research; 1994. Schedules for Clinical Assessment in Neuropsychiatry. [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and statistical manual of mental health disorders. 4th ed. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 34.Wolke D. Feeding and sleeping across the lifespan. In: Rutter M, Hay D, editors. Development through life: a handbook for clinicians. Oxford: Blackwell Scientific Publications; 1994. pp. 517–57. [Google Scholar]
- 35.Weschsler D, Golombok S, Rust J, editors. WISC-III UK Wechsler Intelligence Scale for Children. Sidcup, England: Psychological Corporation; 1992. [Google Scholar]
- 36.Henderson SE, Sugden D, editors. The Movement Assessment Battery for Children. London, UK: The Psychological Corporation; 1992. [Google Scholar]
- 37.Livesey D, Coleman R, Piek J. Performance on the movement assessment battery for children by Australian 3- to 5-year-old children. Child Care Health Dev. 2007;33:713–9. doi: 10.1111/j.1365-2214.2007.00733.x. [DOI] [PubMed] [Google Scholar]
- 38.Bowen E, Heron J, Waylen A, Wolke D ALSPAC Study Team. Domestic violence risk during and after pregnancy: findings from a British longitudinal study. BJOG. 2005;112:1083–9. doi: 10.1111/j.1471-0528.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- 39.Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–55. [PubMed] [Google Scholar]
- 40.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 41.Koffel E, Watson D. Unusual sleep experiences, dissociation, and schizotypy: evidence for a common domain. Clin Psychol Rev. 2009;29:548–59. doi: 10.1016/j.cpr.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ohayon MM. Prevalence of hallucinations and their pathological associations in the general population. Psychiatry Res. 2000;97:153–64. doi: 10.1016/s0165-1781(00)00227-4. [DOI] [PubMed] [Google Scholar]
- 43.Mahowald MW, Schenck CH. Dissociated states of wakefulness and sleep. Neurol. 1992;42:44–52. [PubMed] [Google Scholar]
- 44.Mahowald MW, Schenck CH. Evolving concepts of human state dissociation. Arch Ital Biol. 2001;139:269–300. [PubMed] [Google Scholar]
- 45.Rechtschaffen A, Schulsinger F, Mednick SA. Schizophrenia and physiological indices of dreaming. Arch Gen Psychiatry. 1964;10:89–93. doi: 10.1001/archpsyc.1964.01720190091012. [DOI] [PubMed] [Google Scholar]
- 46.Howland RH. Sleep-onset rapid eye movement periods in neuropsychiatric disorders: implications for the pathophysiology of psychosis. J Nerv Ment Dis. 1997;185:730–8. doi: 10.1097/00005053-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Tandon R, Shipley JE, Taylor S, et al. Electroencephalographic sleep abnormalities in schizophrenia. Relationship to positive/negative symptoms and prior neuroleptic treatment. Arch Gen Psychiatry. 1992;49:185–94. doi: 10.1001/archpsyc.1992.01820030017003. [DOI] [PubMed] [Google Scholar]
- 48.Mannarino AP, Cohen JA. A clinical-demographic study of sexually abused children. Child Abuse Negl. 1986;10:17–23. doi: 10.1016/0145-2134(86)90027-x. [DOI] [PubMed] [Google Scholar]
- 49.Terr LC, Bloch DA, Michel BA, Shi H, Reinhardt JA, Metayer S. Children's symptoms in the wake of Challenger: A field study of distant-traumatic effects and an outline of related conditions. Am J Psychiatry. 1999;156:1536–44. doi: 10.1176/ajp.156.10.1536. [DOI] [PubMed] [Google Scholar]
- 50.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kar N. Psychological impact of disasters on children: review of assessment and interventions. World J Pediatr. 2009;5:5–11. doi: 10.1007/s12519-009-0001-x. [DOI] [PubMed] [Google Scholar]
- 52.Gershuny BS, Thayer JF. Relations among psychological trauma, dissociative phenomena, and trauma-related distress: A review and integration. Clin Psychol Rev. 1999;19:631–57. doi: 10.1016/s0272-7358(98)00103-2. [DOI] [PubMed] [Google Scholar]
- 53.Walker JL, Carey PD, Mohr N, Stein DJ, Seedat S. Gender differences in the prevalence of childhood sexual abuse and in the development of pediatric PTSD. Arch Womens Ment Health. 2004;7:111–21. doi: 10.1007/s00737-003-0039-z. [DOI] [PubMed] [Google Scholar]
- 54.Ross CA, Keyes B. Dissociation and schizophrenia. J Trauma Dissociation. 2004;5:69–83. [Google Scholar]
- 55.Watson D. Dissociations of the night: individual differences in sleep-related experiences and their relation to dissociation and schizotypy. J Abnorm Psychol. 2001;110:526–35. doi: 10.1037//0021-843x.110.4.526. [DOI] [PubMed] [Google Scholar]
- 56.Wolke D, Waylen A, Samara M, et al. Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. Br J Psychiatry. 2009;195:249–56. doi: 10.1192/bjp.bp.108.053751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dominguez M, Wichers M, Lieb R, Wittchen H-U, van Os J. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr Bull. 2011;37:84–93. doi: 10.1093/schbul/sbp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106:67–74. doi: 10.1542/peds.106.1.67. [DOI] [PubMed] [Google Scholar]
- 59.Lewis V, Creamer M, Failla S. Is poor sleep in veterans a function of post-traumatic stress disorder? Mil Med. 2009;174:948–51. doi: 10.7205/milmed-d-04-0208. [DOI] [PubMed] [Google Scholar]
- 60.Schafer I, Fisher HL. Childhood trauma and PTSD in patients with psychosis - clinical challenges and emerging treatments. Curr Opin Psychiatry. 2011;24:514–8. doi: 10.1097/YCO.0b013e32834b56c8. [DOI] [PubMed] [Google Scholar]
- 61.Wills L, Garcia J. Parasomnias: epidemiology and management. CNS Drugs. 2002;16:803–10. doi: 10.2165/00023210-200216120-00002. [DOI] [PubMed] [Google Scholar]
- 62.Oshima N, Nishida A, Fukushima M, et al. Psychotic-like experiences (PLEs) and mental health status in twin and singleton Japanese high school students. Early Interv Psychiatry. 2010;3:206–13. doi: 10.1111/j.1751-7893.2010.00186.x. [DOI] [PubMed] [Google Scholar]
- 63.Yusuf S, Hawken S, Ôunpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Parasomnia questions from age 12 y interview with children
Childhood sleeping problems and psychotic experiences at 12 y with or without attribution to sleep, fever or substance use


