Two general approaches to the treatment of type 2 diabetes mellitus (T2DM) have been advocated. 1) A “guideline” approach that advocates sequential addition of antidiabetes agents with “more established use” (1); this approach more appropriately should be called the “treat to failure” approach, and deficiencies with this approach have been discussed (2). And 2) a “pathophysiologic” approach using initial combination therapy with agents known to correct established pathophysiologic defects in T2DM (3). Within the pathophysiologic approach, choice of antidiabetes agents should take into account the patient’s general health status and associated medical disorders. This individualized approach, which we refer to as the ABCD(E) of diabetes treatment (4), has been incorporated into the updated American Diabetes Association (ADA) guidelines (5).
A = Age
B = Body weight
C = Complications (microvascular and macrovascular)
D = Duration of diabetes
E = Life Expectancy
E = Expense
Even though physicians must be cognizant of these associated conditions (ABCDE) when initiating therapy in newly diagnosed T2DM patients, we believe that the most important consideration is to select antidiabetes agents that correct specific pathophysiologic disturbances present in T2DM and that have complementary mechanisms of action. Although it has been argued that the pathogenesis of T2DM differs in different ethnic groups (6), evidence to support this is weak. Although the relative contributions of β-cell failure and insulin resistance to development of glucose intolerance may differ in different ethnic groups (6), the core defects of insulin resistance in muscle/liver/adipocytes and progressive β-cell failure (3) are present in virtually all T2DM patients and must be treated aggressively to prevent the relentless rise in HbA1c that is characteristic of T2DM.
In subsequent sections, we provide a review of the natural history of T2DM, specific pathophysiologic abnormalities responsible for T2DM, currently available antidiabetes agents and their mechanism of action, recommended glycemic goals, and use of combination therapy based upon reversal of pathophysiologic defects present in T2DM. We will not address expense but recognize that this is an important consideration in choosing any antidiabetes regimen.
Overview of T2DM: pathophysiology and general therapeutic approach
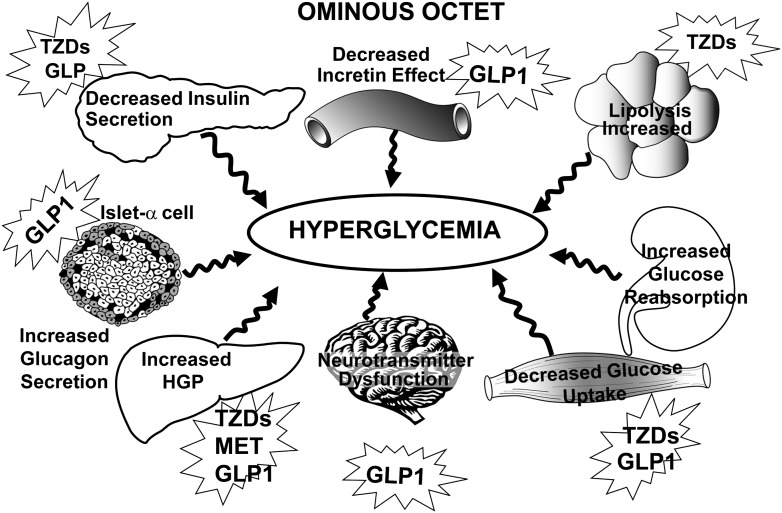
T2DM is a complex metabolic/cardiovascular disorder with multiple pathophysiologic abnormalities. Insulin resistance in muscle/liver and β-cell failure represent the core defects (7,8). β-Cell failure occurs much earlier in the natural history of T2DM and is more severe than previously thought (9–12). Subjects in the upper tertile of impaired glucose tolerance (IGT) are maximally/near-maximally insulin resistant and have lost >80% of their β-cell function. In addition to muscle, liver, and β-cells (“triumvirate”) (7), adipocytes (accelerated lipolysis), gastrointestinal tract (incretin deficiency/resistance), α-cells (hyperglucagonemia), kidney (increased glucose reabsorption), and brain (insulin resistance and neurotransmitter dysregulation) play important roles in development of glucose intolerance in T2DM individuals (3). Collectively, these eight players comprise the “ominous octet” (Fig. 1) and dictate that 1) multiple drugs used in combination will be required to correct the multiple pathophysiological defects, 2) treatment should be based upon reversal of known pathogenic abnormalities and not simply on reducing HbA1c, and 3) therapy must be started early to prevent/slow progressive β-cell failure that is well established in IGT subjects. A treatment paradigm shift is recommended in which combination therapy is initiated with agents that correct known pathogenic defects in T2DM and produce durable reduction in HbA1c rather than just focusing on the glucose-lowering ability of the drug.
Figure 1.
The ominous octet (3) depicting the mechanism and site of action of antidiabetes medications based upon the pathophysiologic disturbances present in T2DM.
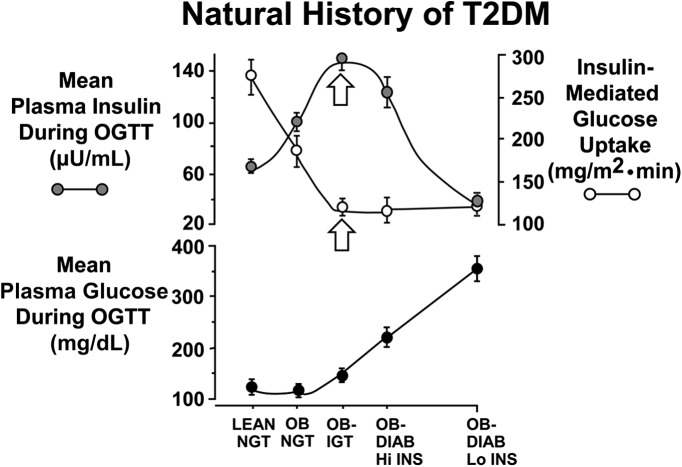
Natural history of T2DM
Individuals destined to develop T2DM inherit genes that make their tissues resistant to insulin (2,8,13–15). In liver, insulin resistance is manifested by glucose overproduction during the basal state despite fasting hyperinsulinemia (16) and impaired suppression of hepatic glucose production (HGP) by insulin (17), as occurs following a meal (18). In muscle (17,19,20), insulin resistance is manifest by impaired glucose uptake after carbohydrate ingestion, resulting in postprandial hyperglycemia (18). Although the origins of insulin resistance can be traced to their genetic background (8,14,15), the current diabetes epidemic is related to the epidemic of obesity and physical inactivity (21), which are insulin-resistant states (22) and place stress on pancreatic β-cells to augment insulin secretion to offset insulin resistance (2,3,8). As long as β-cells augment insulin secretion sufficiently to offset the insulin resistance, glucose tolerance remains normal (2,3,8,23–29). However, with time β-cells begin to fail, and initially postprandial plasma glucose levels and subsequently fasting plasma glucose begin to rise, leading to overt diabetes (2,3,8). Thus, it is progressive β-cell failure that determines the rate of disease progression. The natural history of T2DM described above (2,3) is depicted by a prospective study carried out by DeFronzo (3); Jallut, Golay, and Munger (30); and Felber et al. (31) (Fig. 2).
Figure 2.
Natural history of T2DM. The plasma insulin response depicts the classic Starling’s Curve of the Pancreas. See text for a detailed explanation (7). Upper panel: Insulin-mediated glucose disposal (insulin clamp technique) and mean plasma insulin concentration during OGTT. Lower panel: Mean plasma glucose concentration during OGTT. DIAB, T2DM; Hi, high; Lo, low; OB, obese.
β-Cell function
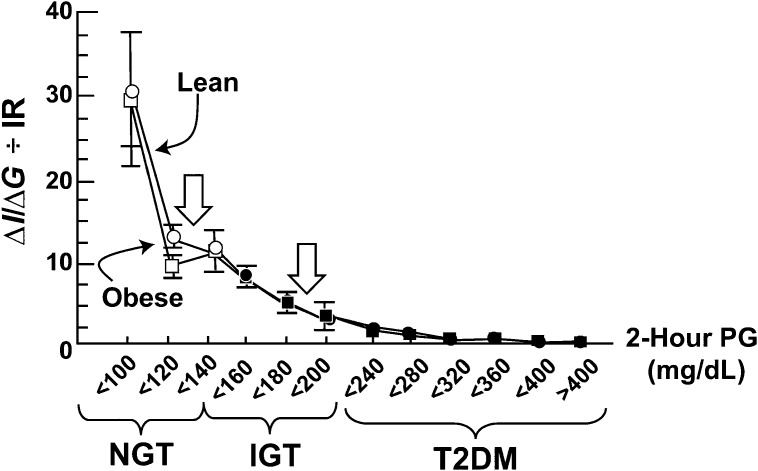
Although the plasma insulin response to insulin resistance is increased early in the natural history of T2DM (Fig. 2), this does not mean that β-cells are functioning normally (3). Simply measuring the plasma insulin response to a glucose challenge does not provide a valid index of β-cell function (32). β-Cells respond to an increment in glucose (ΔG) with an increment in insulin (ΔI). Thus, a better measure of β-cell function is ΔI/ΔG. However, β-cells also increase insulin section to offset insulin resistance and maintain normoglycemia (9,10,12,23,32,33). Thus, the gold standard measure of β-cell function in vivo in man is the insulin secretion/insulin resistance (disposition) index (ΔI/ΔG ÷ IR).
Figure 3 depicts the insulin secretion/insulin resistance index in normal glucose tolerant (NGT), IGT, and T2DM subjects as a function of 2-h plasma glucose during oral glucose tolerance test (OGTT) (2,9,10,12). Subjects in the upper tertile of NGT (2-h plasma glucose 120–139 mg/dL) have lost >50% of β-cell function, while subjects in upper tertile of IGT (2-h plasma glucose 180–199 mg/dL) have lost ∼80% of β-cell function (Fig. 3). Similar conclusions are evident from other publications (24,27,34,35). The therapeutic implications of these findings are obvious. When the diagnosis of diabetes is made, the patient has lost ∼80% of their β-cell function, and it is essential that physicians intervene with therapies known to correct established pathophysiological disturbances in β-cell function. Even more ominous are observations of Butler et al. (36), who demonstrated that as individuals progress from NGT to IFG, there is significant loss of β-cell mass that continues with progression to diabetes. Similar results have been published by others (37,38) and indicate that significant loss of β-cells occurs long before onset of T2DM, according to current diagnostic criteria (1).
Figure 3.
Insulin secretion/insulin resistance (disposition) index (ΔI/ΔG ÷ IR) during OGTT in individuals with NGT, IGT, and T2DM as a function of the 2-h plasma glucose (PG) concentration in lean and obese subjects (9–12).
In summary, although insulin resistance in liver/muscle is well established early in the natural history of T2DM, overt diabetes does not occur in the absence of progressive β-cell failure.
Insulin resistance
The liver and muscle are severely resistant to insulin in T2DM (rev. in 2,3,8).
Liver.
After an overnight fast, the liver produces glucose at ∼2 mg/kg/min (2,16). In T2DM, the rate of basal HGP is increased, averaging ∼2.5 mg/kg/min (2,16). This amounts to addition of an extra 25–30 g glucose to the systemic circulation nightly and is responsible for the increased fasting plasma glucose concentration. This hepatic overproduction of glucose occurs despite fasting insulin levels that are increased two- to threefold, indicating severe hepatic insulin resistance.
Muscle.
With use of the euglycemic insulin clamp with limb catheterization (2,3,17,19,20,39,40), it has conclusively been demonstrated that lean, as well as obese, T2DM individuals are severely resistant to insulin and that the primary site of insulin resistance resides in muscle. Multiple intramyocellular defects in insulin action have been documented in T2DM (rev. in 2,3,8,40), including impaired glucose transport/phosphorylation (17), reduced glycogen synthesis (39), and decreased glucose oxidation (17). However, more proximal insulin signaling defects play a paramount role in muscle insulin resistance (3,40–42).
Ominous octet
In addition to the triumvirate (β-cell failure and insulin resistance in muscle and liver), at least five other pathophysiologic abnormalities contribute to glucose intolerance in T2DM (3) (Fig. 1): 1) adipocyte resistance to insulin’s antilipolytic effect, leading to increased plasma FFA concentration and elevated intracellular levels of toxic lipid metabolites in liver/muscle and β-cells that cause insulin resistance and β-cell failure/apoptosis (17); 2) decreased incretin (glucagon-like peptide [GLP]-1/glucose-dependent insulinotropic polypeptide [GIP]) effect resulting from impaired GLP-1 secretion (43) but, more importantly, severe β-cell resistance to the stimulatory effect of GLP-1 and GIP (44,45); 3) increased glucagon secretion by α-cells and enhanced hepatic sensitivity to glucagon, leading to increased basal HGP and impaired HGP suppression by insulin (46,47); 4) enhanced renal glucose reabsorption contributing to maintenance of elevated plasma glucose levels (48,49); and 5) central nervous system resistance to the anorectic effect of insulin and altered neurosynaptic hormone secretion contributing to appetite dysregulation, weight gain, and insulin resistance in muscle/liver (50–52).
Implications for therapy
The preceding review of pathophysiology has important therapeutic implications: 1) effective treatment will require multiple drugs in combination to correct the multiple pathophysiological defects, 2) treatment should be based upon established pathogenic abnormalities and not simply on HbA1c reduction, and 3) therapy must be started early in the natural history of T2DM to prevent progressive β-cell failure.
Figure 1 displays therapeutic options as they relate to key pathophysiological derangements in T2DM (Fig. 1). In liver, both metformin (53–55) and thiazolidinediones (TZDs) (56–62) are potent insulin sensitizers and inhibit the increased rate of HGP. In muscle, TZDs are potent insulin sensitizers (56–58,61,63), whereas metformin is, at best, a weak insulin sensitizer (53,55,64). Since TZDs work through the insulin signaling pathway (65), whereas metformin works through the AMP kinase pathway (66), combination TZD/metformin therapy gives a completely additive effect to reduce HbA1c (67–72). Further, hypoglycemia is not encountered because these drugs are insulin sensitizers and do not augment insulin secretion. In adipocytes, TZDs are excellent insulin sensitizers and potent inhibitors of lipolysis (73). TZDs also mobilize fat out of muscle, liver, and β-cells, thereby ameliorating lipotoxicity (57,62,63,74–76).
Although weight loss has the potential to improve both the defects in insulin sensitivity and insulin secretion (77), two meta-analyses involving 46 published studies demonstrated that the ability to maintain the initial weight loss is difficult (78,79). In the following sections, we will focus on pharmacologic agents—as monotherapy and combination therapy—that have been proven to reverse pathophysiologic abnormalities in T2DM.
In the β-cell, sulfonylureas and glinides augment insulin secretion (80), but only TZDs (81–83) and GLP-1 analogs (84–86) improve and preserve β-cell function and demonstrate durability of glycemic control (70,82–85,87–93). Importantly, TZDs and GLP-1 analogs cause durable HbA1c reduction for up to 5 and 3.5 years, respectively (82,93). Although dipeptidyl peptidase inhibitors (DPP4i) augment insulin secretion (94), their β-cell effect is weak compared with GLP1 analogs and they begin to lose efficacy (manifested by rising HbA1c) within 2 years after initiation of therapy (95,96). Despite the potent effects of TZDs and GLP-1 agonists on β-cells, the two most commonly prescribed drugs in the U.S. and worldwide are sulfonylureas and metformin, neither of which exerts any β-cell protective effect. This is a major concern, since progressive β-cell failure is the primary pathogenic abnormality responsible for development of T2DM and progressive HbA1c rise (Fig. 3).
GLP-1 analogs augment and preserve β-cell function for at least 3 years (84). This protective effect has its onset within 24 h (86) and persists as long as GLP-1 therapy is continued (84,85,93). Further, both exenatide and liraglutide promote weight loss, inhibit glucagon secretion, and delay gastric emptying, reducing postprandial hyperglycemia (45,93,97–99). Weight loss depletes lipid from muscle and liver, improving muscle and hepatic insulin sensitivity (84,85). GLP-1 analogs also correct multiple cardiovascular risk factors (rev. in 100) and, thus, have the potential to reduce cardiovascular events (101,102). Although DPP4i share some characteristics with GLP-1 analogs, they do not raise plasma GLP-1 levels sufficiently to offset β-cell resistance to GLP-1 (103). Not surprisingly, their ability to augment insulin secretion and reduce HbA1c is considerably less than GLP-1 analogs (94,104,105), and they do not promote weight loss (94). In a 1-year study involving 665 metformin-treated T2DM patients, HbA1c reduction with sitagliptin (0.9%) was significantly less than liraglutide dosed at 1.2 mg/day (ΔHbA1c = 1.2%) or 1.8 mg/day (ΔHbA1c = 1.8%) (105). In a short-term, mechanism-of-action, crossover study, exenatide was far superior to sitagliptin in reducing glucose area under the curve and 2-h glucose after a meal, increasing insulin secretion, inhibiting glucagon secretion, and promoting weight loss (104). Metformin increases GLP-1 secretion by intestinal L-cells (106–108), and the combination of metformin plus DPP4i may exert a more durable effect on β-cell function. The major mechanism of action of DPP4i to improve glycemic control is mediated via inhibition of glucagon secretion with subsequent decline in HGP (109)
Although not yet approved by U.S. regulatory agencies, sodium glucose transporter 2 inhibitors (approved in Europe) demonstrate modest efficacy in reducing HbA1c, promote weight loss, reduce blood pressure, and can be added to any antidiabetes agent (48,110).
Instituting therapy in newly diagnosed T2DM patients
When initiating therapy in newly diagnosed T2DM patients, the following considerations are of paramount importance:
Therapy should have the ability to achieve the desired level of glycemic control, based upon starting HbA1c. According to the ADA, European Association for the Study of Diabetes (EASD), and American Association of Clinical Endocrinologists (AACE), the desired HbA1c is 6.5% (EASD and AACE) or 7.0% (ADA) (5,111). However, we believe that in newly diagnosed diabetic patients without cardiovascular disease, the optimal HbA1c should be ≤6.0%, while avoiding adverse events, primarily hypoglycemia. This is consistent with the expanded ADA/EASD statement (5).
In most newly diagnosed diabetic patients, monotherapy will not reduce HbA1c <6.5–7.0% or, most optimally, <6.0%, and combination therapy will be required.
Importantly, medications used in combination therapy should have an additive effect, and individual drugs should correct established pathophysiologic disturbances in T2DM. If antidiabetes medications do not correct underlying pathogenic abnormalities, long-term durable glycemic control cannot be achieved.
Progressive β-cell failure is responsible for progressive HbA1c rise in T2DM (3). Therefore, medications used to treat T2DM should preserve or improve β-cell function to ensure durable glycemic control.
Because insulin resistance is a core defect in T2DM and exacerbates the decline in β-cell function, medications also should ameliorate insulin resistance in muscle/liver.
T2DM is associated with an increased incidence of atherosclerotic cardiovascular complications. Therefore, it is desirable that drugs exert beneficial effects on cardiovascular risk factors and decrease cardiovascular events.
Since obesity is a major problem in diabetic individuals, combination therapy should be weight neutral and, if possible, promote weight loss.
Combination therapy should be safe and not exacerbate underlying medical conditions.
No single antidiabetes agent can correct all of the pathophysiologic disturbances present in T2DM, and multiple agents, used in combination, will be required for optimal glycemic control. Further, the HbA1c decrease produced by a single antidiabetes agent, e.g., metformin, sulfonylurea, TZD, GLP-1 analog, is in the range of 1.0–1.5% depending upon the starting HbA1c (5). Thus, in newly diagnosed T2DM with HbA1c >8.0–8.5%, a single agent is unlikely to achieve HbA1c goal <6.5–7.0%, and virtually no one will achieve HbA1c <6.0%. When maximal-dose metformin, sulfonylurea, or TZD is initiated as monotherapy, <40% of newly diagnosed T2DM subjects can be expected to achieve HbA1c <6.5–7.0%. Thus, most patients with HbA1c >8.0–8.5% will require initial combination therapy to reach HbA1c <6.5–7.0%. Moreover, because different agents lower plasma glucose via different mechanisms, combination therapy will have an additive effect to reduce HbA1c compared with each agent alone. Simultaneous correction of the β-cell defect and insulin resistance is more likely to cause durable HbA1c reduction. Lastly, combination therapy allows use of submaximal doses of each antidiabetes agent, resulting in fewer side effects (112).
In summary, initiating therapy with multiple antidiabetes agents in newly diagnosed T2DM patients, especially those with HbA1c >8.0–8.5%, represents a rational approach to achieve the target HbA1c level while minimizing side effects. Indeed, AACE recommends starting newly diagnosed diabetic subjects with HbA1c >7.5% on multiple antidiabetes agents (111).
“Treat to fail” algorithm
The 2009 ADA/EASD algorithm (1) recommended initiation of therapy with metformin to achieve HbA1c <7.0%, followed by, importantly, sequential addition of a sulfonylurea. If sulfonylurea addition failed to reduce HbA1c <7.0%, addition of basal insulin was recommended. Although the revised 2012 ADA/EASD algorithm (5) includes newer antidiabetes agents (GLP-1 receptor agonists, DPP4i, and TZDs) as potential choices if metformin fails, the initial box in the treatment algorithm still depicts sequential addition of sulfonylurea and then insulin to maintain HbA1c <7.0%. This algorithm has little basis in pathophysiology and more appropriately should be called the treat to fail algorithm. Moreover, it does not consider the starting HbA1c or need for initial combination therapy in most newly diagnosed T2DM patients, especially if HbA1c goal <6.0–6.5% is desired, as suggested by us (4) and by the 2012 ADA/EASD consensus statement (5). Because β-cell failure is progressive (9–12,24–30,34,35,113,114) and results in loss of β-cell mass (36–38), it is essential to intervene with agents that normalize HbA1c and halt the progressive β-cell demise (Fig. 3). Failure to do so will result in the majority of T2DM patients progressing to insulin therapy, as demonstrated in the UK Prospective Diabetes Study (UKPDS) (113,114).
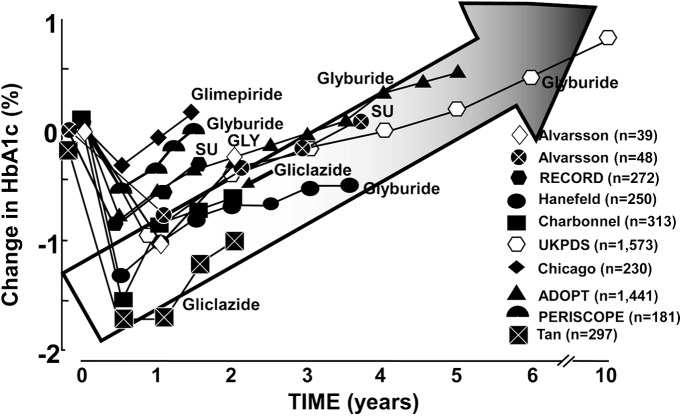
Sulfonylureas/glinides: the treat to fail approach.
Until recently (5), sulfonylureas have been considered the drug of choice for add-on therapy to metformin (1). In large part, this is attributed to their low cost and rapid onset of hypoglycemic effect. However, they lack “glycemic durability” and within 1–2 years lose their efficacy, resulting in steady HbA1c rise to or above pretreatment levels (107,108) (Figs. 4 and 5). Although long-term studies examining glycemic durability with glinides (nateglinide, repaglinide) in T2DM are not available, nateglinide failed to prevent prediabetic (IGT) patients from progressing to T2DM (115). In a 2-year study in newly diagnosed T2DM subjects, durability of netaglinide plus metformin was comparable with glyburide plus metformin (116) and both groups experienced a small but progressive HbA1c rise after the first year. Since deterioration in glycemic control is largely accounted for by progressive β-cell failure (3), it is clear that both sulfonylureas and glinides fail to prevent the progressive decline in β-cell function characteristic of T2DM. Consistent with this, in vitro studies have demonstrated a proapoptotic β-cell effect of sulfonylureas and glinides (117–120).
Figure 4.
The effect of sulfonylurea (glibenclamide = glyburide) and metformin therapy on the plasma HbA1c concentration in newly diagnosed T2DM subjects in UKPDS. Conventionally treated diabetic subjects received diet plus exercise therapy (113,114).
Figure 5.
Durability of glycemic control with sulfonylureas. Summary of studies examining the effect of sulfonylurea treatment versus placebo or versus active comparator on HbA1c in T2DM. See text for a more detailed discussion (70,82,87–92,113,114,124–127,131,132).
UKPDS conclusively demonstrated that sulfonylureas exerted no β-cell protective effect in newly diagnosed T2DM patients (starting HbA1c = 7.0%) over a 15-year follow-up (113,114). After an initial HbA1c drop, sulfonylurea-treated patients experienced progressive deterioration in glycemic control that paralleled HbA1c rise in conventionally treated individuals (Fig. 4). Moreover, some studies have suggested that sulfonylureas may accelerate atherogenesis (121,122). Similarly, metformin-treated patients in UKPDS, after initial HbA1c decline (secondary to inhibition of HGP), also experienced progressive deterioration in glycemic control (123) (Fig. 4). With use of homeostasis model assessment of β-cell function, it was shown that the relentless HbA1c rise observed with sulfonylureas and metformin resulted from progressive decline in β-cell function and that within 3–5 years, ∼50% of diabetic patients required an additional pharmacologic agent to maintain HbA1c <7.0% (114,124–127). Although there is in vitro evidence that metformin may improve β-cell function (128,129), in vivo data from UKPDS and other studies (130) fail to support any role for metformin in preservation of β-cell function in humans. Metformin did reduce macrovascular events in UKPDS (123), although by today’s standards the number of metformin-treated subjects (n = 342) would be considered inadequate to justify any conclusions about cardiovascular protection. Other than its effect to reduce the elevated rate of basal and postprandial HGP (53,55,64), metformin does not correct any other component of the ominous octet (Fig. 1), and even its muscle insulin-sensitizing effect is difficult to demonstrate in absence of weight loss (53,55,64).
UKPDS was designed as a monotherapy study. However, after 3 years it became evident that monotherapy with neither metformin nor sulfonylureas could prevent progressive β-cell failure and stabilize HbA1c at its starting level (113,114,123–127). Therefore, study protocol was altered to allow metformin addition to sulfonylurea and sulfonylurea addition to metformin. Although addition of a second antidiabetes agent initially improved glycemic control, progressive β-cell failure continued and HbA1c rose progressively.
Numerous long-term (>1.5 years) active-comparator or placebo-controlled studies have demonstrated inability of sulfonylureas to produce durable HbA1c reduction in T2DM patients. These studies (70,83,87–92,113,131–133) showed that after initial HbA1c decline, sulfonylureas (glyburide, glimepiride, and gliclazide) were associated with progressive decline in β-cell function with accompanying loss of glycemic control (Fig. 5). There are no exceptions to this consistent loss of glycemic control with sulfonylureas after the initial 18 months of therapy. Thus, evidence-based medicine demonstrates that the glucose-lowering effect of sulfonylureas is not durable and that loss of glycemic control is associated with progressive β-cell failure.
Sulfonylurea treatment does not correct any pathophysiologic component of the ominous octet (3) (Fig. 1) and is associated with significant weight gain and hypoglycemia (89,90). Although no study has clearly implicated sulfonylureas with an increased incidence of cardiovascular events, a deleterious effect of glibenclamide (glyburide) on the cardioprotective process of ischemic preconditioning has been demonstrated (134), while some (121,122,135–142) but not all (143,144) studies have suggested a possible association between sulfonylureas and adverse cardiovascular outcomes. Since metformin was the comparator in many of these studies (121,122,137,138,140–142), it is difficult to determine whether sulfonylureas increased or metformin decreased cardiovascular morbidity/mortality. In the study by Sillars et al. (143) the increased cardiovascular mortality/morbidity disappeared after adjusting for confounding variables, and failure to do so in other sulfonylurea studies may have clouded their interpretation. Among the sulfonylurea studies, the older sulfonylureas (i.e., glibenclamide) more commonly have been associated with increased adverse cardiovascular outcomes than the newer sulfonylurea agents (i.e., gliclazide and glimeperide) (139,144–146).
In summary, we believe that currently available insulin secretagogues (sulfonylureas and glinides) represent a poor option as add-on therapy to metformin. However, in many countries newer antidiabetes agents are not available or are expensive (ABCDE) (4). In such circumstances, sulfonylureas may be the only option.
Antidiabetes agents known to reverse pathophysiologic defects
Pioglitazone: unique benefits, unique side effects.
Rosiglitazone has been removed from the market or its use severely restricted because of cardiovascular safety concerns (147). Therefore, pioglitazone is the only representative TZD. Pioglitazone is unique in that it both exerts β-cell protective effects (81) and is a powerful insulin sensitizer in muscle and liver (56–61,65,74–76) Thus, it is the only antidiabetes agent that corrects the core defects of insulin resistance and β-cell failure in T2DM. Not surprisingly, it has a durable effect to reduce HbA1c with low risk of hypoglycemia.
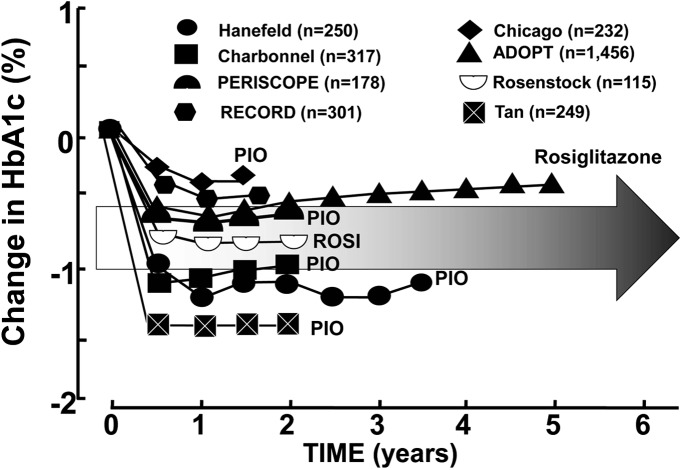
Eight long-term (>1.5 years) studies with TZDs (70,82,81–92) (Fig. 6) have demonstrated that, after initial decline in HbA1c, durability of glycemic control is maintained because of preservation of β-cell function in T2DM patients. Further, five studies demonstrate that TZDs prevent progression of IGT to T2DM (148–152). All five studies showed that, in addition to their insulin-sensitizing effect, TZDs had a major action to preserve β-cell function. In Actos Now for Prevention of Diabetes (ACT NOW), improved insulin secretion/insulin resistance (disposition) index was shown both with OGTT and frequently sampled intravenous glucose tolerance test. Similar results were documented in Troglitazone in Prevention of Diabetes (TRIPOD) and Pioglitazone in Prevention of Diabetes (PIPOD) (148,151). Many in vivo and in vitro studies with human and rodent islets have demonstrated that TZDs exert a β-cell–protective effect (153–157).
Figure 6.
Durability of glycemic control with TZDs. Summary of studies examining the effect of TZDs versus placebo or versus active comparator on HbA1c in T2DM subjects. See text for a more detailed discussion (70,82,87–92). Pio, pioglitazone; Rosi, rosiglitazone.
Pioglitazone has additional beneficial pleiotropic properties, including increased HDL cholesterol, reduced plasma triglyceride, decreased blood pressure, improved endothelial dysfunction, anti-inflammatory effects (76,158–161), and amelioration of nonalcoholic steatohepatitis (75). In addition to reduced cardiovascular events in PROactive and U.S. phase 3 trials (162,163), pioglitazone slows progression of carotid intimal-media thickness (87,152) and reduces coronary atheroma volume (88).
Physicians must be cognizant of side effects associated with TZDs including weight gain (81,164), fluid retention (162,165), bone fractures (166), and possibly bladder cancer (162,167,168) (see article on peroxisome proliferator–activated receptors in this supplement [169]). The preferred starting dose of pioglitazone is 15 mg/day titrated to 30 mg/day, which provides 70–80% of the glycemic efficacy with minimal side effects (170–174); titrating to 45 mg/day is not recommended. HbA1c lowering has been observed with a pioglitazone dose of 7.5 mg/day with minimal side effects. In a 26-week study (172) involving a Caucasian population, 7.5 mg/day pioglitazone reduced the HbA1c by 0.9% compared with placebo (P = 0.14), while 15 mg/day reduced the HbA1c by 1.3% vs. placebo (P < 0.05). Similar HbA1c reduction with pioglitazone, 7.5 mg/day, has been observed in an Asian population (173,174).
In combination with metformin (inhibits hepatic gluconeogenesis), pioglitazone (improves insulin sensitivity in liver/muscle and preserves β-cell function) offers an effective, durable, and additive therapy that retards progressive β-cell failure with little risk of hypoglycemia. In a 6-month trial comparing fixed-dose combination with pioglitazone (30 mg)/metformin (1,700 mg) in 600 drug-naïve T2DM patients, HbA1c declined by 1.8% (from baseline HbA1c 8.6%) and was significantly greater than the 1.0% reduction observed with metformin alone or pioglitazone alone (175). Similar results were reported by Rosenstock et al. (176) using initial combination therapy with rosiglitazone (8 mg)/metformin (2,000 mg).
Combining pioglitazone with GLP-1 analog curbs weight gain associated with the TZD (177). Further, the natriuretic effect of GLP-1 analogs (178) mitigates against fluid retention observed with TZDs. Therefore, we advocate combined GLP-1 analog/pioglitazone therapy with or without metformin in newly diagnosed T2DM patients (3).
Intensive therapy with insulin plus metformin: reversal of metabolic decompensation.
Newly diagnosed T2DM patients who present in poor metabolic control are markedly resistant to insulin and have severely impaired β-cell function. Glucotoxicity (8), lipotoxicity (8,42,62), and multiple metabolic abnormalities (3) play an important role in the insulin resistance and β-cell dysfunction. Institution of intensive insulin therapy with or without other antidiabetes agents to correct these many metabolic abnormalities, therefore, represents a rational approach to therapy based upon pathophysiology. After a period of sustained metabolic control, the insulin therapy can be continued or the patient can be switched to a noninsulin therapeutic regimen. This approach has recently been examined by Harrison et al. (179). Fifty-eight newly diagnosed T2DM patients in poor metabolic control (HbA1c 10.8%) initially were treated for 3 months with metformin plus insulin to reduce the HbA1c to 5.9%. Subjects then were randomized to continued therapy with insulin-metformin combination therapy with pioglitazone/metformin/glyburide. During 3 years of follow-up, both groups maintained the reduction in HbA1c, but the insulin dose had to be increased, indicating that, despite excellent glycemic control, β-cell failure continued in this group. Further, glycemic control in both groups was achieved at the expense of a relatively high rate of hypoglycemia and weight gain in the insulin/metformin group, consistent with multiple studies demonstrating a high incidence of hypoglycemia in sulfonylurea-treated and insulin-treated subjects.
Metformin plus GLP-1 analog plus pioglitazone: a pathophysiologic option that offers robust glycemic control and weight loss.
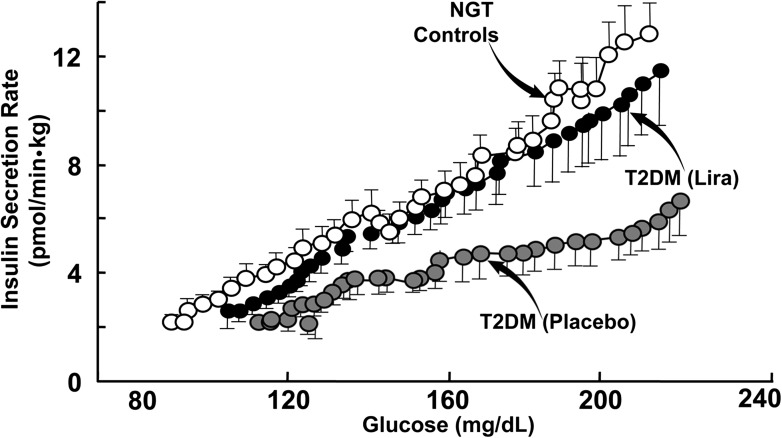
The combination of biguanide (metformin), TZD (pioglitazone), and GLP-1 analog offers a rational treatment choice, targeting multiple pathophysiologic abnormalities in T2DM: muscle insulin resistance (pioglitazone), adipocyte insulin resistance (pioglitazone), pancreatic β-cell failure (GLP-1 analog, pioglitazone), hepatic insulin resistance (metformin, pioglitazone, and GLP-1 analog), and excessive glucagon secretion (GLP-1 analog) (3) with weight loss (GLP-1 analog) and low risk of hypoglycemia (93,97). Studies with exenatide have demonstrated durable glycemic control for 3 years (84,93). β-Cells in T2DM are blind to glucose, and GLP-1 analogs have the unique ability to restore β-cell glucose sensitivity (84–86) (Fig. 7) by augmenting glucose transport, activating glucokinase, increasing Pdx, and replenishing β-cell insulin stores (180,181). Because pharmacologic GLP-1 levels (∼80–90 pmol/L) are achieved with GLP-1 analogs, they overcome β-cell incretin resistance and augment insulin secretion. Increased insulin and inhibited glucagon secretion reduce basal HGP, reducing fasting plasma glucose concentration and enhancing HGP suppression after a meal (98,99). Although GLP-1 analogs do not have a direct insulin-sensitizing effect, they augment insulin-mediated glucose disposal secondary to weight loss (97). The combination of pioglitazone plus exenatide reduces hepatic fat content and markers of liver damage in T2DM (182). In T2DM patients treated with rosiglitazone, exenatide, or both (as add-on to metformin), improved β-cell function and insulin sensitivity were noted, with weight loss in all exenatide-treated groups (177). Similar results have been reported by others (182–185) with combined GLP-1 analog/TZD therapy.
Figure 7.
A single dose of liraglutide (Lira) (7.5 μg/kg or 0.75 mg for 100-kg person) administered acutely completely restores β-cell sensitivity to glucose using the graded glucose infusion technique to evaluate β-cell function (86).
In an ongoing study, we compared triple combination therapy with pioglitazone/metformin/exenatide with the standard ADA approach (metformin followed by sequential addition of sulfonylurea and then basal insulin) in 134 newly diagnosed T2DM patients with starting HbA1c 8.7% (186). After 2 years, HbA1c reduction was greater in the triple therapy versus sequential ADA group (2.7 vs. 2.2%, P < 0.01), triple therapy subjects lost 1.5 vs. 4.1 kg weight gain with the ADA approach, and hypoglycemia incidence was 13.5-fold higher in the sequential ADA group. These preliminary results indicate that a triple combination approach focused on reversing underlying insulin resistance and β-cell dysfunction is superior to sequential therapy (metformin, add sulfonylurea, add basal insulin) with agents that do not correct core pathophysiologic defects in T2DM.
DPP4i: weak but easy alternative to GLP-1 analogs.
DPP4i have gained widespread use in combination with metformin because of their weight neutrality, modest efficacy, and safety (187,188). Metformin has a modest effect to increase GLP-1 secretion (107,189). Thus, combination metformin/DPP4i therapy may result in increased GLP-1 levels (190) and an additive glucose-lowering effect (191,192). When used in triple combination with metformin plus pioglitazone (30 mg/day), alogliptin resulted in better glycemic control and fewer pioglitazone dose-dependent side effects (edema, weight gain) compared with metformin with a higher pioglitazone dose (45 mg/day) (172). Because they correct multiple components of the ominous octet, have superior glucose-lowering efficacy, promote weight loss, and preserve β-cell function, we favor GLP-1 analogs over DPP4i in the triple therapy approach. Nonetheless, because of their ease of administration and safety, DPP4i represent a reasonable alternative.
Conclusions and recommendations
T2DM is a multifactorial, multiorgan disease, and antidiabetes medications should address underlying pathogenic mechanisms rather than solely reducing the blood glucose concentration. Emphasis should be placed on medications that ameliorate insulin resistance and prevent β-cell failure if durable HbA1c reduction is to be achieved. Further, the long-practiced glucocentric paradigm has become antiquated. Diabetic patients are at high risk for cardiovascular events, and comprehensive evaluation/treatment of all cardiovascular risk factors is essential. Simply focusing on glycemic control will not have a major impact to reduce cardiovascular risk (113,123). Therefore, we favor a therapeutic approach based not only on the drug’s glucose-lowering efficacy/durability but also on its effect on weight, blood pressure, lipids, cardiovascular protection, and side effect profile, especially hypoglycemia.
Initial therapy in newly diagnosed T2DM patients without cardiovascular disease should be capable of achieving the desired glycemic goal, which should be as close to normal as possible: HbA1c ≤6.0%. This will require combination therapy in the majority of T2DM patients (3) (Fig. 1). While we favor the pathophysiologic approach, physicians must be cognizant of the ABCDE of diabetes management (4). An approach that emphasizes pathophysiology but allows for individualized therapy will provide optimal results. Evidence-based medicine (UPKDS) has taught us that sequential therapy with metformin followed by sulfonylurea addition with subsequent insulin addition represents the treat to fail approach, and we do not recommend this approach unless cost is the overriding concern.
Acknowledgments
R.A.D. is a member of the Bristol-Myers Squibb, Janssen, Amylin, Takeda, Novo Nordisk, and Lexicon advisory boards; has received grants from Takeda, Amylin, and Bristol-Myers Squibb; and is a member of the following speakers bureaus: Bristol-Myers Squibb, Novo Nordisk, Janssen, and Takeda. No other potential conflicts of interest relevant to this article were reported.
R.A.D. wrote the initial draft of the manuscript. R.E. and M.A.-G. revised the manuscript. R.A.D. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This publication is based on the presentations from the 4th World Congress on Controversies to Consensus in Diabetes, Obesity and Hypertension (CODHy). The Congress and the publication of this supplement were made possible in part by unrestricted educational grants from Abbott, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Ethicon Endo-Surgery, Janssen, Medtronic, Novo Nordisk, Sanofi, and Takeda.
See accompanying article, p. S139.
References
- 1.Nathan DM, Buse JB, Davidson MB, et al. American Diabetes Association. European Association for Study of Diabetes Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009;32:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schernthaner G, Barnett AH, Betteridge DJ, et al. Is the ADA/EASD algorithm for the management of type 2 diabetes (January 2009) based on evidence or opinion? A critical analysis. Diabetologia 2010;53:1258–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pozzilli P, Leslie RD, Chan J, et al. The A1C and ABCD of glycaemia management in type 2 diabetes: a physician’s personalized approach. Diabetes Metab Res Rev 2010;26:239–244 [DOI] [PubMed] [Google Scholar]
- 5.Inzucchi SE, Bergenstal RM, Buse JB, et al. American Diabetes Association (ADA) European Association for the Study of Diabetes (EASD) Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdul-Ghani MA, Matsuda M, Sabbah M, Jenkinson C, Richardson DK, DeFronzo RA. The relative contribution of insulin resistance and beta cell failure to the transition from normal to impaired glucose tolerance varies in different ethnic groups. Diab Metab Syndr 2007;1:105–112
- 7.DeFronzo RA. Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 1988;37:667–687 [DOI] [PubMed] [Google Scholar]
- 8.DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Res 1997;5:177–269 [Google Scholar]
- 9.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, DeFronzo RA, San Antonio metabolism study Beta-cell dysfunction and glucose intolerance: results from the San Antonio metabolism (SAM) study. Diabetologia 2004;47:31–39 [DOI] [PubMed] [Google Scholar]
- 10.Ferrannini E, Gastaldelli A, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA. beta-Cell function in subjects spanning the range from normal glucose tolerance to overt diabetes: a new analysis. J Clin Endocrinol Metab 2005;90:493–500 [DOI] [PubMed] [Google Scholar]
- 11.Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 2006;29:1130–1139 [DOI] [PubMed] [Google Scholar]
- 12.Abdul-Ghani MA, Jenkinson CP, Richardson DK, Tripathy D, DeFronzo RA. Insulin secretion and action in subjects with impaired fasting glucose and impaired glucose tolerance: results from the Veterans Administration Genetic Epidemiology Study. Diabetes 2006;55:1430–1435 [DOI] [PubMed] [Google Scholar]
- 13.Eriksson J, Franssila-Kallunki A, Ekstrand A, et al. Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus. N Engl J Med 1989;321:337–343 [DOI] [PubMed] [Google Scholar]
- 14.Groop L, Lyssenko V. Genes and type 2 diabetes mellitus. Curr Diab Rep 2008;8:192–197 [DOI] [PubMed] [Google Scholar]
- 15.Ahlqvist E, Ahluwalia TS, Groop L. Genetics of type 2 diabetes. Clin Chem 2011;57:241–254 [DOI] [PubMed] [Google Scholar]
- 16.DeFronzo RA, Ferrannini E, Simonson DC. Fasting hyperglycemia in non-insulin-dependent diabetes mellitus: contributions of excessive hepatic glucose production and impaired tissue glucose uptake. Metabolism 1989;38:387–395 [DOI] [PubMed] [Google Scholar]
- 17.Groop LC, Bonadonna RC, DelPrato S, et al. Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J Clin Invest 1989;84:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrannini E, Simonson DC, Katz LD, et al. The disposal of an oral glucose load in patients with non-insulin-dependent diabetes. Metabolism 1988;37:79–85 [DOI] [PubMed] [Google Scholar]
- 19.DeFronzo RA, Gunnarsson R, Björkman O, Olsson M, Wahren J. Effects of insulin on peripheral and splanchnic glucose metabolism in noninsulin-dependent (type II) diabetes mellitus. J Clin Invest 1985;76:149–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pendergrass M, Bertoldo A, Bonadonna R, et al. Muscle glucose transport and phosphorylation in type 2 diabetic, obese nondiabetic, and genetically predisposed individuals. Am J Physiol Endocrinol Metab 2007;292:E92–E100 [DOI] [PubMed] [Google Scholar]
- 21.James WP. The fundamental drivers of the obesity epidemic. Obes Rev 2008;9(Suppl 1):6–13 [DOI] [PubMed] [Google Scholar]
- 22.DeFronzo RA, Soman V, Sherwin RS, Hendler R, Felig P. Insulin binding to monocytes and insulin action in human obesity, starvation, and refeeding. J Clin Invest 1978;62:204–213 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Diamond MP, Thornton K, Connolly-Diamond M, Sherwin RS, DeFronzo RA. Reciprocal variations in insulin-stimulated glucose uptake and pancreatic insulin secretion in women with normal glucose tolerance. J Soc Gynecol Investig 1995;2:708–715 [DOI] [PubMed] [Google Scholar]
- 24.Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott DM, Bennett PH. Sequential changes in serum insulin concentration during development of non-insulin-dependent diabetes. Lancet 1989;1:1356–1359 [DOI] [PubMed] [Google Scholar]
- 25.Lillioja S, Mott DM, Howard BV, et al. Impaired glucose tolerance as a disorder of insulin action. Longitudinal and cross-sectional studies in Pima Indians. N Engl J Med 1988;318:1217–1225 [DOI] [PubMed] [Google Scholar]
- 26.Lillioja S, Mott DM, Spraul M, et al. Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. Prospective studies of Pima Indians. N Engl J Med 1993;329:1988–1992 [DOI] [PubMed] [Google Scholar]
- 27.Weyer C, Tataranni PA, Bogardus C, Pratley RE. Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care 2001;24:89–94 [DOI] [PubMed] [Google Scholar]
- 28.Levy J, Atkinson AB, Bell PM, McCance DR, Hadden DR. Beta-cell deterioration determines the onset and rate of progression of secondary dietary failure in type 2 diabetes mellitus: the 10-year follow-up of the Belfast Diet Study. Diabet Med 1998;15:290–296 [DOI] [PubMed] [Google Scholar]
- 29.Bergman RN, Finegood DT, Kahn SE. The evolution of beta-cell dysfunction and insulin resistance in type 2 diabetes. Eur J Clin Invest 2002;32(Suppl. 3):35–45 [DOI] [PubMed] [Google Scholar]
- 30.Jallut D, Golay A, Munger R, et al. Impaired glucose tolerance and diabetes in obesity: a 6-year follow-up study of glucose metabolism. Metabolism 1990;39:1068–1075 [DOI] [PubMed] [Google Scholar]
- 31.Felber JP, Golay A, Jéquier E, et al. The metabolic consequences of long-term human obesity. Int J Obes 1988;12:377–389 [PubMed] [Google Scholar]
- 32.Ahren B, Taborsky GJ. Beta-cell function and insulin secretion. In Ellenberg and Rifkin’s Diabetes Mellitus Porte D, Sherin RS, Baron A, Eds. New York, McGraw Hill, 2003, p. 43–65 [Google Scholar]
- 33.Bergman RN. Lilly lecture 1989. Toward physiological understanding of glucose tolerance. Minimal-model approach. Diabetes 1989;38:1512–1527 [DOI] [PubMed] [Google Scholar]
- 34.Zimmet P, Whitehouse S, Alford F, Chisholm D. The relationship of insulin response to a glucose stimulus over a wide range of glucose tolerance. Diabetologia 1978;15:23–27 [DOI] [PubMed] [Google Scholar]
- 35.Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott DM, Bennett PH. The natural history of impaired glucose tolerance in the Pima Indians. N Engl J Med 1988;319:1500–1506 [DOI] [PubMed] [Google Scholar]
- 36.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003;52:102–110 [DOI] [PubMed] [Google Scholar]
- 37.Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab 2008;10(Suppl. 4):32–42 [DOI] [PubMed] [Google Scholar]
- 38.Stefan Y, Orci L, Malaisse-Lagae F, Perrelet A, Patel Y, Unger RH. Quantitation of endocrine cell content in the pancreas of nondiabetic and diabetic humans. Diabetes 1982;31:694–700 [DOI] [PubMed] [Google Scholar]
- 39.Shulman GI, Rothman DL, Smith D, et al. Mechanism of liver glycogen repletion in vivo by nuclear magnetic resonance spectroscopy. J Clin Invest 1985;76:1229–1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bajaj M, Defronzo RA. Metabolic and molecular basis of insulin resistance. J Nucl Cardiol 2003;10:311–323 [DOI] [PubMed] [Google Scholar]
- 41.Cusi K, Maezono K, Osman A, et al. Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J Clin Invest 2000;105:311–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeFronzo RA. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009. Diabetologia 2010;53:1270–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nauck MA, Vardarli I, Deacon CF, Holst JJ, Meier JJ. Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes: what is up, what is down? Diabetologia 2011;54:10–18 [DOI] [PubMed] [Google Scholar]
- 44.Knop FK, Vilsbøll T, Højberg PV, et al. Reduced incretin effect in type 2 diabetes: cause or consequence of the diabetic state? Diabetes 2007;56:1951–1959 [DOI] [PubMed] [Google Scholar]
- 45.Holst JJ. Glucagon-like peptide-1: from extract to agent. The Claude Bernard Lecture, 2005. Diabetologia 2006;49:253–260 [DOI] [PubMed] [Google Scholar]
- 46.Baron AD, Schaeffer L, Shragg P, Kolterman OG. Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type II diabetics. Diabetes 1987;36:274–283 [DOI] [PubMed] [Google Scholar]
- 47.Matsuda M, Defronzo RA, Glass L, et al. Glucagon dose-response curve for hepatic glucose production and glucose disposal in type 2 diabetic patients and normal individuals. Metabolism 2002;51:1111–1119 [DOI] [PubMed] [Google Scholar]
- 48.Abdul-Ghani MA, Norton L, Defronzo RA. Role of sodium-glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetes. Endocr Rev 2011;32:515–531 [DOI] [PubMed] [Google Scholar]
- 49.Mogensen CE. Maximum tubular reabsorption capacity for glucose and renal hemodynamcis during rapid hypertonic glucose infusion in normal and diabetic subjects. Scand J Clin Lab Invest 1971;28:101–109 [DOI] [PubMed] [Google Scholar]
- 50.Matsuda M, Liu Y, Mahankali S, et al. Altered hypothalamic function in response to glucose ingestion in obese humans. Diabetes 1999;48:1801–1806 [DOI] [PubMed] [Google Scholar]
- 51.Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci 2002;5:566–572 [DOI] [PubMed] [Google Scholar]
- 52.Obici S, Feng Z, Tan J, Liu L, Karkanias G, Rossetti L. Central melanocortin receptors regulate insulin action. J Clin Invest 2001;108:1079–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cusi K, Consoli A, DeFronzo RA. Metabolic effects of metformin on glucose and lactate metabolism in NIDDM. J Clin Endocrinol Metab 1996;81:4059–4067 [DOI] [PubMed] [Google Scholar]
- 54.DeFronzo RA, Goodman AM, The Multicenter Metformin Study Group Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 1995;333:541–549 [DOI] [PubMed] [Google Scholar]
- 55.Cusi K, DeFronzo RA. Metformin: a review of its metabolic effects. Diabetes Res 1998;6:89–131 [Google Scholar]
- 56.Miyazaki Y, Mahankali A, Matsuda M, et al. Improved glycemic control and enhanced insulin sensitivity in type 2 diabetic subjects treated with pioglitazone. Diabetes Care 2001;24:710–719 [DOI] [PubMed] [Google Scholar]
- 57.Miyazaki Y, Mahankali A, Matsuda M, et al. Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab 2002;87:2784–2791 [DOI] [PubMed] [Google Scholar]
- 58.Bajaj M, Suraamornkul S, Hardies LJ, Pratipanawatr T, DeFronzo RA. Plasma resistin concentration, hepatic fat content, and hepatic and peripheral insulin resistance in pioglitazone-treated type II diabetic patients. Int J Obes Relat Metab Disord 2004;28:783–789 [DOI] [PubMed] [Google Scholar]
- 59.Gastaldelli A, Miyazaki Y, Mahankali A, et al. The effect of pioglitazone on the liver: role of adiponectin. Diabetes Care 2006;29:2275–2281 [DOI] [PubMed] [Google Scholar]
- 60.Gastaldelli A, Miyazaki Y, Pettiti M, et al. The effect of rosiglitazone on the liver: decreased gluconeogenesis in patients with type 2 diabetes. J Clin Endocrinol Metab 2006;91:806–812 [DOI] [PubMed] [Google Scholar]
- 61.Miyazaki Y, DeFronzo RA. Rosiglitazone and pioglitazone similarly improve insulin sensitivity and secretion, glucose tolerance and adipocytokines in type 2 diabetic patients. Diabetes Obes Metab 2008;10:1204–1211 [DOI] [PubMed] [Google Scholar]
- 62.Bays H, Mandarino L, DeFronzo RA. Role of the adipocyte, free fatty acids, and ectopic fat in pathogenesis of type 2 diabetes mellitus: peroxisomal proliferator-activated receptor agonists provide a rational therapeutic approach. J Clin Endocrinol Metab 2004;89:463–478 [DOI] [PubMed] [Google Scholar]
- 63.Bajaj M, Baig R, Suraamornkul S, et al. Effect of pioglitazone on intramocellular fat metabolism in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 2010;95:1916–1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Natali A, Ferrannini E. Effects of metformin and thiazolidinediones on suppression of hepatic glucose production and stimulation of glucose uptake in type 2 diabetes: a systematic review. Diabetologia 2006;49:434–441 [DOI] [PubMed] [Google Scholar]
- 65.Miyazaki Y, He H, Mandarino LJ, DeFronzo RA. Rosiglitazone improves downstream insulin receptor signaling in type 2 diabetic patients. Diabetes 2003;52:1943–1950 [DOI] [PubMed] [Google Scholar]
- 66.Musi N, Hirshman MF, Nygren J, et al. Metformin increases AMP-activated protein kinase activity in skeletal muscle of subjects with type 2 diabetes. Diabetes 2002;51:2074–2081 [DOI] [PubMed] [Google Scholar]
- 67.Einhorn D, Rendell M, Rosenzweig J, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride in combination with metformin in the treatment of type 2 diabetes mellitus: a randomized, placebo-controlled study. The Pioglitazone 027 Study Group. Clin Ther 2000;22:1395–1409 [DOI] [PubMed] [Google Scholar]
- 68.Fonseca V, Rosenstock J, Patwardhan R, Salzman A. Effect of metformin and rosiglitazone combination therapy in patients with type 2 diabetes mellitus: a randomized controlled trial. JAMA 2000;283:1695–1702 [DOI] [PubMed] [Google Scholar]
- 69.Matthews DR, Charbonnel BH, Hanefeld M, Brunetti P, Schernthaner G. Long-term therapy with addition of pioglitazone to metformin compared with the addition of gliclazide to metformin in patients with type 2 diabetes: a randomized, comparative study. Diabetes Metab Res Rev 2005;21:167–174 [DOI] [PubMed]
- 70.Charbonnel B, Schernthaner G, Brunetti P, et al. Long-term efficacy and tolerability of add-on pioglitazone therapy to failing monotherapy compared with addition of gliclazide or metformin in patients with type 2 diabetes. Diabetologia 2005;48:1093–1104 [DOI] [PubMed] [Google Scholar]
- 71.Inzucchi SE, Maggs DG, Spollett GR, et al. Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N Engl J Med 1998;338:867–872 [DOI] [PubMed] [Google Scholar]
- 72.Bajaj M, DeFronzo RA. Combination therapy in type 2 diabetes. In International Textbook of Diabetes Mellitus 3rd ed. DeFronzo RA, Ferrannini E, Keen H, Zimmet P, Eds. Hoboken, NJ, John Wiley & Sons, 2004, p. 915–950 [Google Scholar]
- 73.Miyazaki Y, Glass L, Triplitt C, et al. Effect of rosiglitazone on glucose and non-esterified fatty acid metabolism in Type II diabetic patients. Diabetologia 2001;44:2210–2219 [DOI] [PubMed] [Google Scholar]
- 74.Bajaj M, Suraamornkul S, Pratipanawatr T, et al. Pioglitazone reduces hepatic fat content and augments splanchnic glucose uptake in patients with type 2 diabetes. Diabetes 2003;52:1364–1370 [DOI] [PubMed] [Google Scholar]
- 75.Belfort R, Harrison SA, Brown K, et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med 2006;355:2297–2307 [DOI] [PubMed] [Google Scholar]
- 76.Yki-Järvinen H. Thiazolidinediones. N Engl J Med 2004;351:1106–1118 [DOI] [PubMed] [Google Scholar]
- 77.Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011;54:2506–2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 2001;74:579–584 [DOI] [PubMed] [Google Scholar]
- 79.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med 2007;147:41–50 [DOI] [PubMed] [Google Scholar]
- 80.DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med 1999;131:281–303 [DOI] [PubMed] [Google Scholar]
- 81.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA. Thiazolidinediones improve beta-cell function in type 2 diabetic patients. Am J Physiol Endocrinol Metab 2007;292:E871–E883 [DOI] [PubMed] [Google Scholar]
- 82.Kahn SE, Haffner SM, Heise MA, et al. ADOPT Study Group Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427–2443 [DOI] [PubMed] [Google Scholar]
- 83.Kahn SE, Lachin JM, Zinman B, et al. ADOPT Study Group Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes 2011;60:1552–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bunck MC, Cornér A, Eliasson B, et al. Effects of exenatide on measures of β-cell function after 3 years in metformin-treated patients with type 2 diabetes. Diabetes Care 2011;34:2041–2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bunck MC, Diamant M, Cornér A, et al. One-year treatment with exenatide improves beta-cell function, compared with insulin glargine, in metformin-treated type 2 diabetic patients: a randomized, controlled trial. Diabetes Care 2009;32:762–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chang AM, Jakobsen G, Sturis J, et al. The GLP-1 derivative NN2211 restores beta-cell sensitivity to glucose in type 2 diabetic patients after a single dose. Diabetes 2003;52:1786–1791 [DOI] [PubMed] [Google Scholar]
- 87.Mazzone T, Meyer PM, Feinstein SB, et al. Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial. JAMA 2006;296:2572–2581 [DOI] [PubMed] [Google Scholar]
- 88.Nissen SE, Nicholls SJ, Wolski K, et al. PERISCOPE Investigators Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA 2008;299:1561–1573 [DOI] [PubMed] [Google Scholar]
- 89.Hanefeld M, Pfützner A, Forst T, Lübben G. Glycemic control and treatment failure with pioglitazone versus glibenclamide in type 2 diabetes mellitus: a 42-month, open-label, observational, primary care study. Curr Med Res Opin 2006;22:1211–1215 [DOI] [PubMed] [Google Scholar]
- 90.Tan MH, Baksi A, Krahulec B, et al. GLAL Study Group Comparison of pioglitazone and gliclazide in sustaining glycemic control over 2 years in patients with type 2 diabetes. Diabetes Care 2005;28:544–550 [DOI] [PubMed] [Google Scholar]
- 91.Rosenstock J, Goldstein BJ, Vinik AI, et al. RESULT Study Group Effect of early addition of rosiglitazone to sulphonylurea therapy in older type 2 diabetes patients (>60 years): the Rosiglitazone Early vs. SULphonylurea Titration (RESULT) study. Diabetes Obes Metab 2006;8:49–57 [DOI] [PubMed] [Google Scholar]
- 92.Home PD, Jones NP, Pocock SJ, et al. RECORD Study Group Rosiglitazone RECORD study: glucose control outcomes at 18 months. Diabet Med 2007;24:626–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Klonoff DC, Buse JB, Nielsen LL, et al. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr Med Res Opin 2008;24:275–286 [DOI] [PubMed] [Google Scholar]
- 94.Bergenstal RM, Wysham C, Macconell L, et al. DURATION-2 Study Group Efficacy and safety of exenatide once weekly versus sitagliptin or pioglitazone as an adjunct to metformin for treatment of type 2 diabetes (DURATION-2): a randomised trial. Lancet 2010;376:431–439 [DOI] [PubMed] [Google Scholar]
- 95.Matthews DR, Dejager S, Ahren B, et al. Vildagliptin add-on to metformin produces similar efficacy and reduced hypoglycaemic risk compared with glimepiride, with no weight gain: results from a 2-year study. Diabetes Obes Metab 2010;12:780–789 [DOI] [PubMed] [Google Scholar]
- 96.Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet 2012;380:475–483 [DOI] [PubMed] [Google Scholar]
- 97.Astrup A, Carraro R, Finer N, et al. NN8022-1807 Investigators Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond) 2012;36:843–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cervera A, Wajcberg E, Sriwijitkamol A, et al. Mechanism of action of exenatide to reduce postprandial hyperglycemia in type 2 diabetes. Am J Physiol Endocrinol Metab 2008;294:E846–E852 [DOI] [PubMed] [Google Scholar]
- 99.Cersosimo E, Gastaldelli A, Cervera A, et al. Effect of exenatide on splanchnic and peripheral glucose metabolism in type 2 diabetic subjects. J Clin Endocrinol Metab 2011;96:1763–1770 [DOI] [PubMed] [Google Scholar]
- 100.Chilton R, Wyatt J, Nandish S, Oliveros R, Lujan M. Cardiovascular comorbidities of type 2 diabetes mellitus: defining the potential of glucagonlike peptide-1-based therapies. Am J Med 2011;124(Suppl.):S35–S53 [DOI] [PubMed] [Google Scholar]
- 101.Jenkins AJ, Krishnamurthy B, Best JD, et al. Evaluation of an algorithm to guide patients with type 1 diabetes treated with continuous subcutaneous insulin infusion on how to respond to real-time continuous glucose levels: a randomized controlled trial. Diabetes Care 2010;33:1242–1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marso SP, Lindsey JB, Stolker JM, et al. Cardiovascular safety of liraglutide assessed in a patient-level pooled analysis of phase 2: 3 liraglutide clinical development studies. Diab Vasc Dis Res 2011;8:237–240 [DOI] [PubMed] [Google Scholar]
- 103.Herman GA, Bergman A, Stevens C, et al. Effect of single oral doses of sitagliptin, a dipeptidyl peptidase-4 inhibitor, on incretin and plasma glucose levels after an oral glucose tolerance test in patients with type 2 diabetes. J Clin Endocrinol Metab 2006;91:4612–4619 [DOI] [PubMed] [Google Scholar]
- 104.DeFronzo RA, Okerson T, Viswanathan P, Guan X, Holcombe JH, MacConell L. Effects of exenatide versus sitagliptin on postprandial glucose, insulin and glucagon secretion, gastric emptying, and caloric intake: a randomized, cross-over study. Curr Med Res Opin 2008;24:2943–2952 [DOI] [PubMed] [Google Scholar]
- 105.Pratley RE, Nauck M, Bailey T, et al. 1860-LIRA-DPP-4 Study Group Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet 2010;375:1447–1456 [DOI] [PubMed] [Google Scholar]
- 106.Mulherin AJ, Oh AH, Kim H, Grieco A, Lauffer LM, Brubaker PL. Mechanisms underlying metformin-induced secretion of glucagon-like peptide-1 from the intestinal L cell. Endocrinology 2011;152:4610–4619 [DOI] [PubMed] [Google Scholar]
- 107.Mannucci E, Ognibene A, Cremasco F, et al. Effect of metformin on glucagon-like peptide 1 (GLP-1) and leptin levels in obese nondiabetic subjects. Diabetes Care 2001;24:489–494 [DOI] [PubMed] [Google Scholar]
- 108.Migoya EM, Bergeron R, Miller JL, et al. Dipeptidyl peptidase-4 inhibitors administered in combination with metformin result in an additive increase in the plasma concentration of active GLP-1. Clin Pharmacol Ther 2010;88:801–808 [DOI] [PubMed] [Google Scholar]
- 109.Ahrén B, Landin-Olsson M, Jansson PA, Svensson M, Holmes D, Schweizer A. Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, and reduces glucagon levels in type 2 diabetes. J Clin Endocrinol Metab 2004;89:2078–2084 [DOI] [PubMed] [Google Scholar]
- 110.DeFronzo RA, Davidson JA, Del Prato S. The role of the kidneys in glucose homeostasis: a new path towards normalizing glycaemia. Diabetes Obes Metab 2012;14:5–14 [DOI] [PubMed] [Google Scholar]
- 111.Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract 2009;15:540–559 [DOI] [PubMed] [Google Scholar]
- 112.Zinman B, Harris SB, Neuman J, et al. Low-dose combination therapy with rosiglitazone and metformin to prevent type 2 diabetes mellitus (CANOE trial): a double-blind randomised controlled study. Lancet 2010;376:103–111 [DOI] [PubMed] [Google Scholar]
- 113.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 114.Turner RC, Cull CA, Frighi V, Holman RR, UK Prospective Diabetes Study (UKPDS) Group Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). JAMA 1999;281:2005–2012 [DOI] [PubMed] [Google Scholar]
- 115.Holman RR, Haffner SM, McMurray JJ, et al. NAVIGATOR Study Group Effect of nateglinide on the incidence of diabetes and cardiovascular events. N Engl J Med 2010;362:1463–1476 [DOI] [PubMed] [Google Scholar]
- 116.Gerich J, Raskin P, Jean-Louis L, Purkayastha D, Baron MA. PRESERVE-beta: two-year efficacy and safety of initial combination therapy with nateglinide or glyburide plus metformin. Diabetes Care 2005;28:2093–2099 [DOI] [PubMed] [Google Scholar]
- 117.Takahashi A, Nagashima K, Hamasaki A, et al. Sulfonylurea and glinide reduce insulin content, functional expression of K(ATP) channels, and accelerate apoptotic beta-cell death in the chronic phase. Diabetes Res Clin Pract 2007;77:343–350 [DOI] [PubMed] [Google Scholar]
- 118.Hambrock A, de Oliveira Franz CB, Hiller S, Osswald H. Glibenclamide-induced apoptosis is specifically enhanced by expression of the sulfonylurea receptor isoform SUR1 but not by expression of SUR2B or the mutant SUR1(M1289T). J Pharmacol Exp Ther 2006;316:1031–1037 [DOI] [PubMed] [Google Scholar]
- 119.Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab 2005;90:501–506 [DOI] [PubMed] [Google Scholar]
- 120.Kim JY, Lim DM, Park HS, et al. Exendin-4 protects against sulfonylurea-induced β-cell apoptosis. J Pharmacol Sci 2012;118:65–74 [DOI] [PubMed] [Google Scholar]
- 121.Johnson JA, Majumdar SR, Simpson SH, Toth EL. Decreased mortality associated with the use of metformin compared with sulfonylurea monotherapy in type 2 diabetes. Diabetes Care 2002;25:2244–2248 [DOI] [PubMed] [Google Scholar]
- 122.Evans JM, Ogston SA, Emslie-Smith A, Morris AD. Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 2006;49:930–936 [DOI] [PubMed] [Google Scholar]
- 123.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865 [PubMed] [Google Scholar]
- 124.U.K. Prospective Diabetes Study Group UKPDS 28: a randomized trial of efficacy of early addition of metformin in sulfonylurea-treated type 2 diabetes. Diabetes Care 1998;21:87–92 [DOI] [PubMed] [Google Scholar]
- 125.Wright A, Burden AC, Paisey RB, Cull CA, Holman RR, U.K. Prospective Diabetes Study Group Sulfonylurea inadequacy: efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the U.K. Prospective Diabetes Study (UKPDS 57). Diabetes Care 2002;25:330–336 [DOI] [PubMed] [Google Scholar]
- 126.Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC, UK Prospective Diabetes Study (UKPDS) Group UKPDS 26: Sulphonylurea failure in non-insulin-dependent diabetic patients over six years. Diabet Med 1998;15:297–303 [DOI] [PubMed] [Google Scholar]
- 127.U.K. Prospective Diabetes Study Group U.K. prospective diabetes study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995;44:1249–1258 [PubMed] [Google Scholar]
- 128.Lupi R, Del Guerra S, Tellini C, et al. The biguanide compound metformin prevents desensitization of human pancreatic islets induced by high glucose. Eur J Pharmacol 1999;364:205–209 [DOI] [PubMed] [Google Scholar]
- 129.Lupi R, Del Guerra S, Fierabracci V, et al. Lipotoxicity in human pancreatic islets and the protective effect of metformin. Diabetes 2002;51(Suppl. 1):S134–S137 [DOI] [PubMed] [Google Scholar]
- 130.Brown JB, Conner C, Nichols GA. Secondary failure of metformin monotherapy in clinical practice. Diabetes Care 2010;33:501–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Alvarsson M, Berntorp K, Fernqvist-Forbes E, et al. Effects of insulin versus sulphonylurea on beta-cell secretion in recently diagnosed type 2 diabetes patients: a 6-year follow-up study. Rev Diabet Stud 2010;7:225–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Alvarsson M, Sundkvist G, Lager I, et al. Effects of insulin vs. glibenclamide in recently diagnosed patients with type 2 diabetes: a 4-year follow-up. Diabetes Obes Metab 2008;10:421–429 [DOI] [PubMed] [Google Scholar]
- 133.Gallwitz B, Guzman J, Dotta F, et al. Exenatide twice daily versus glimepiride for prevention of glycaemic deterioration in patients with type 2 diabetes with metformin failure (EUREXA): an open-label, randomised controlled trial. Lancet 2012;379:2270–2278 [DOI] [PubMed] [Google Scholar]
- 134.Nieszner E, Posa I, Kocsis E, Pogátsa G, Préda I, Koltai MZ. Influence of diabetic state and that of different sulfonylureas on the size of myocardial infarction with and without ischemic preconditioning in rabbits. Exp Clin Endocrinol Diabetes 2002;110:212–218 [DOI] [PubMed] [Google Scholar]
- 135.Panicker GK, Karnad DR, Salvi V, Kothari S. Cardiovascular risk of oral antidiabetic drugs: current evidence and regulatory requirements for new drugs. J Assoc Physicians India 2012;60:56–61 [PubMed] [Google Scholar]
- 136.Garratt KN, Brady PA, Hassinger NL, Grill DE, Terzic A, Holmes DR., Jr Sulfonylurea drugs increase early mortality in patients with diabetes mellitus after direct angioplasty for acute myocardial infarction. J Am Coll Cardiol 1999;33:119–124 [DOI] [PubMed] [Google Scholar]
- 137.Simpson SH, Majumdar SR, Tsuyuki RT, Eurich DT, Johnson JA. Dose-response relation between sulfonylurea drugs and mortality in type 2 diabetes mellitus: a population-based cohort study. CMAJ 2006;174:169–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schramm TK, Gislason GH, Vaag A, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study. Eur Heart J 2011;32:1900–1908 [DOI] [PubMed] [Google Scholar]
- 139.Johnsen SP, Monster TB, Olsen ML, et al. Risk and short-term prognosis of myocardial infarction among users of antidiabetic drugs. Am J Ther 2006;13:134–140 [DOI] [PubMed] [Google Scholar]
- 140.Selvin E, Bolen S, Yeh HC, et al. Cardiovascular outcomes in trials of oral diabetes medications: a systematic review. Arch Intern Med 2008;168:2070–2080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rao AD, Kuhadiya N, Reynolds K, Fonseca VA. Is the combination of sulfonylureas and metformin associated with an increased risk of cardiovascular disease or all-cause mortality?: a meta-analysis of observational studies. Diabetes Care 2008;31:1672–1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Roumie CL, Hung AM, Greevy RA, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann Intern Med 2012;157:601–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sillars B, Davis WA, Hirsch IB, Davis TM. Sulphonylurea-metformin combination therapy, cardiovascular disease and all-cause mortality: the Fremantle Diabetes Study. Diabetes Obes Metab 2010;12:757–765 [DOI] [PubMed] [Google Scholar]
- 144.Pantalone KM, Kattan MW, Yu C, et al. The risk of overall mortality in patients with type 2 diabetes receiving glipizide, glyburide, or glimepiride monotherapy: a retrospective analysis. Diabetes Care 2010;33:1224–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Khalangot M, Tronko M, Kravchenko V, Kovtun V. Glibenclamide-related excess in total and cardiovascular mortality risks: data from large Ukrainian observational cohort study. Diabetes Res Clin Pract 2009;86:247–253 [DOI] [PubMed] [Google Scholar]
- 146.Monami M, Balzi D, Lamanna C, et al. Are sulphonylureas all the same? A cohort study on cardiovascular and cancer-related mortality. Diabetes Metab Res Rev 2007;23:479–484 [DOI] [PubMed] [Google Scholar]
- 147.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 2007;356:2457–2471 [DOI] [PubMed] [Google Scholar]
- 148.Xiang AH, Peters RK, Kjos SL, et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 2006;55:517–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gerstein HC, Yusuf S, Bosch J, et al. DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 2006;368:1096–1105 [DOI] [PubMed] [Google Scholar]
- 150.Knowler WC, Hamman RF, Edelstein SL, et al. Diabetes Prevention Program Research Group Prevention of type 2 diabetes with troglitazone in the Diabetes Prevention Program. Diabetes 2005;54:1150–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic women. Diabetes 2002;51:2796–2803 [DOI] [PubMed] [Google Scholar]
- 152.DeFronzo RA, Tripathy D, Schwenke DC, et al. ACT NOW Study Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med 2011;364:1104–1115 [DOI] [PubMed] [Google Scholar]
- 153.Lupi R, Del Guerra S, Marselli L, et al. Rosiglitazone prevents the impairment of human islet function induced by fatty acids: evidence for a role of PPARgamma2 in the modulation of insulin secretion. Am J Physiol Endocrinol Metab 2004;286:E560–E567 [DOI] [PubMed]
- 154.Finegood DT, McArthur MD, Kojwang D, et al. Beta-cell mass dynamics in Zucker diabetic fatty rats. Rosiglitazone prevents the rise in net cell death. Diabetes 2001;50:1021–1029 [DOI] [PubMed] [Google Scholar]
- 155.Kim HI, Cha JY, Kim SY, et al. Peroxisomal proliferator-activated receptor-gamma upregulates glucokinase gene expression in beta-cells. Diabetes 2002;51:676–685 [DOI] [PubMed] [Google Scholar]
- 156.Santini E, Fallahi P, Ferrari SM, Masoni A, Antonelli A, Ferrannini E. Effect of PPAR-gamma activation and inhibition on glucose-stimulated insulin release in INS-1e cells. Diabetes 2004;53(Suppl. 3):S79–S83 [DOI] [PubMed] [Google Scholar]
- 157.Masuda K, Okamoto Y, Tsuura Y, et al. Effects of Troglitazone (CS-045) on insulin secretion in isolated rat pancreatic islets and HIT cells: an insulinotropic mechanism distinct from glibenclamide. Diabetologia 1995;38:24–30 [DOI] [PubMed] [Google Scholar]
- 158.Betteridge DJ, DeFronzo RA, Chilton RJ. PROactive: time for a critical appraisal. Eur Heart J 2008;29:969–983 [DOI] [PubMed] [Google Scholar]
- 159.Patrono C, Bachmann F, Baigent C, et al. European Society of Cardiology Expert consensus document on the use of antiplatelet agents. The task force on the use of antiplatelet agents in patients with atherosclerotic cardiovascular disease of the European society of cardiology. Eur Heart J 2004;25:166–181 [DOI] [PubMed] [Google Scholar]
- 160.Bajaj M, Suraamornkul S, Hardies LJ, Glass L, Musi N, DeFronzo RA. Effects of peroxisome proliferator-activated receptor (PPAR)-alpha and PPAR-gamma agonists on glucose and lipid metabolism in patients with type 2 diabetes mellitus. Diabetologia 2007;50:1723–1731 [DOI] [PubMed] [Google Scholar]
- 161.Betteridge DJ. Effects of pioglitazone on lipid and lipoprotein metabolism. Diabetes Obes Metab 2007;9:640–647 [DOI] [PubMed] [Google Scholar]
- 162.Dormandy JA, Charbonnel B, Eckland DJ, et al. PROactive investigators Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279–1289 [DOI] [PubMed] [Google Scholar]
- 163.Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA 2007;298:1180–1188 [DOI] [PubMed] [Google Scholar]
- 164.Miyazaki M, De Filippis E, Bajaj M, et al. Predictors of improved glycaemic control with rosiglitazone therapy in type 2 diabetic patients: a practical approach for the primary care physician. Br J Diabetes Vasc Dis 2005;5:28–35 [Google Scholar]
- 165.Singh S, Loke YK, Furberg CD. Thiazolidinediones and heart failure: a teleo-analysis. Diabetes Care 2007;30:2148–2153 [DOI] [PubMed] [Google Scholar]
- 166.Bodmer M, Meier C, Kraenzlin ME, Meier CR. Risk of fractures with glitazones: a critical review of the evidence to date. Drug Saf 2009;32:539–547 [DOI] [PubMed] [Google Scholar]
- 167.Lewis JD, Ferrara A, Peng T, et al. Risk of bladder cancer among diabetic patients treated with pioglitazone: interim report of a longitudinal cohort study. Diabetes Care 2011;34:916–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cohort study of pioglitazone and bladder cancer in patients with type II diabetes [article online], 2013. Available from http://clinicaltrials.gov/ct2/show/results/NCT01637935?sect=X6015#outcome1 Accessed 4 February 2013
- 169.Eldor R, DeFronzo RA, Abdul-Ghani M. In vivo actions of peroxisome proliferator–activated receptors: glycemic control, insulin sensitivity, and insulin secretion. Diabetes Care 2013;36(Suppl. 2):S162–S174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Aronoff S, Rosenblatt S, Braithwaite S, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride monotherapy improves glycemic control in the treatment of patients with type 2 diabetes: a 6-month randomized placebo-controlled dose-response study. The Pioglitazone 001 Study Group. Diabetes Care 2000;23:1605–1611 [DOI] [PubMed] [Google Scholar]
- 171.Miyazaki Y, Matsuda M, DeFronzo RA. Dose-response effect of pioglitazone on insulin sensitivity and insulin secretion in type 2 diabetes. Diabetes Care 2002;25:517–523 [DOI] [PubMed] [Google Scholar]
- 172.DeFronzo RA, Burant CF, Fleck P, Wilson C, Mekki Q, Pratley RE. Efficacy and tolerability of the DPP-4 inhibitor alogliptin combined with pioglitazone, in metformin-treated patients with type 2 diabetes. J Clin Endocrinol Metab 2012;97:1615–1622 [DOI] [PubMed] [Google Scholar]
- 173.Yokoyama J, Sutoh N, Higuma T, et al. Efficacy and safety of low-dose pioglitazone after primary coronary angioplasty with the use of bare metal stent in patients with acute myocardial infarction and with type 2 diabetes mellitus or impaired glucose tolerance. Heart Vessels 2007;22:146–151 [DOI] [PubMed] [Google Scholar]
- 174.Aso Y, Hara K, Ozeki N, et al. Low-dose pioglitazone increases serum high molecular weight adiponectin and improves glycemic control in Japanese patients with poorly controlled type 2 diabetes. Diabetes Res Clin Pract 2009;85:147–152 [DOI] [PubMed] [Google Scholar]
- 175.Perez A, Zhao Z, Jacks R, Spanheimer R. Efficacy and safety of pioglitazone/metformin fixed-dose combination therapy compared with pioglitazone and metformin monotherapy in treating patients with T2DM. Curr Med Res Opin 2009;25:2915–2923 [DOI] [PubMed] [Google Scholar]
- 176.Rosenstock J, Rood J, Cobitz A, Biswas N, Chou H, Garber A. Initial treatment with rosiglitazone/metformin fixed-dose combination therapy compared with monotherapy with either rosiglitazone or metformin in patients with uncontrolled type 2 diabetes. Diabetes Obes Metab 2006;8:650–660 [DOI] [PubMed] [Google Scholar]
- 177.DeFronzo RA, Triplitt C, Qu Y, Lewis MS, Maggs D, Glass LC. Effects of exenatide plus rosiglitazone on beta-cell function and insulin sensitivity in subjects with type 2 diabetes on metformin. Diabetes Care 2010;33:951–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gutzwiller JP, Tschopp S, Bock A, et al. Glucagon-like peptide 1 induces natriuresis in healthy subjects and in insulin-resistant obese men. J Clin Endocrinol Metab 2004;89:3055–3061 [DOI] [PubMed] [Google Scholar]
- 179.Harrison LB, Adams-Huet B, Raskin P, Lingvay I. β-cell function preservation after 3.5 years of intensive diabetes therapy. Diabetes Care 2012;35:1406–1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 2007;87:1409–1439 [DOI] [PubMed] [Google Scholar]
- 181.Yusta B, Baggio LL, Estall JL, et al. GLP-1 receptor activation improves beta cell function and survival following induction of endoplasmic reticulum stress. Cell Metab 2006;4:391–406 [DOI] [PubMed] [Google Scholar]
- 182.Sathyanarayana P, Jogi M, Muthupillai R, Krishnamurthy R, Samson SL, Bajaj M. Effects of combined exenatide and pioglitazone therapy on hepatic fat content in type 2 diabetes. Obesity (Silver Spring) 2011;19:2310–2315 [DOI] [PubMed] [Google Scholar]
- 183.Zinman B, Hoogwerf BJ, Durán García S, et al. The effect of adding exenatide to a thiazolidinedione in suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2007;146:477–485 [DOI] [PubMed] [Google Scholar]
- 184.Liutkus J, Rosas Guzman J, Norwood P, et al. A placebo-controlled trial of exenatide twice-daily added to thiazolidinediones alone or in combination with metformin. Diabetes Obes Metab 2010;12:1058–1065 [DOI] [PubMed] [Google Scholar]
- 185.Zinman B, Gerich J, Buse J, et al. LEAD-4 Study Investigators Efficacy and safety of the human GLP-1 analog liraglutide in combination with metformin and TZD in patients with type 2 diabetes mellitus (LEAD-4 Met+TZD). Diabetes Care 2009;32:1224–1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Abdul-Ghani MA, Puckett C, Adams J, et al. Initial triple combination therapy is superior to stepwise add-on conventional therapy in newly diagnosed T2DM (Abstract). Diabetes 2013;62(Suppl. 1):A97
- 187.Deacon CF. Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: a comparative review. Diabetes Obes Metab 2011;13:7–18 [DOI] [PubMed] [Google Scholar]
- 188.Raz I, Hanefeld M, Xu L, Caria C, Williams-Herman D, Khatami H, Sitagliptin Study 023 Group Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. Diabetologia 2006;49:2564–2571 [DOI] [PubMed] [Google Scholar]
- 189.Yasuda N, Inoue T, Nagakura T, et al. Enhanced secretion of glucagon-like peptide 1 by biguanide compounds. Biochem Biophys Res Commun 2002;298:779–784 [DOI] [PubMed] [Google Scholar]
- 190.Mathieu C, Degrande E. Vildagliptin: a new oral treatment for type 2 diabetes mellitus. Vasc Health Risk Manag 2008;4:1349–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Karyekar C, Donovan M, Allen E, Fleming D, Ravichandran S, Chen R. Efficacy and safety of saxagliptin combination therapy in US patients with type 2 diabetes. Postgrad Med 2011;123:63–70 [DOI] [PubMed] [Google Scholar]
- 192.Goldstein BJ, Feinglos MN, Lunceford JK, Johnson J, Williams-Herman DE, Sitagliptin 036 Study Group Effect of initial combination therapy with sitagliptin, a dipeptidyl peptidase-4 inhibitor, and metformin on glycemic control in patients with type 2 diabetes. Diabetes Care 2007;30:1979–1987 [DOI] [PubMed] [Google Scholar]