Abstract
The causes of the current high prevalence of overweight and obesity among children are not clearly known. Schools have been implicated in the causal chain to high child obesity prevalence. Recent studies have compared school year versus summertime changes (herein called seasonal differences) in child adiposity or related phenomena. The most common seasonal pattern in six longitudinal descriptive studies was that overweight and obese children experienced accelerated gain in weight or some BMI indicator during the summer, whereas healthy weight children gained less or not at all. Four physical activity (PA) intervention studies demonstrated that school year fitness improvements were lost during the summer. One study showed that PA declined across the summer. Another study provided conflicting results of lower total energy expenditure in the summer, but no seasonal difference in total energy expenditure after adjusting for fat-free mass. This pattern of fairly rapid seasonal differences suggests that PA is the primary factor contributing to seasonal differences in weight or BMI, but the documented seasonal pattern in PA (i.e., higher in summer) does not support this relationship. Sleep duration has also been inversely related to child adiposity. Seasonal patterns in adiposity, PA, and sleep need to be clearly established separately for overweight and healthy weight children in further longitudinal research to provide a clear focus for national policy.
Introduction
Child obesity is a prevalent national health problem.1 Recently, a plateauing in prevalence of obesity was detected among children,2 but the levels are still quite high, placing many children at increased risk for serious health problems as they age.3 The causes of the high prevalence of obesity are likely multi-factorial, including biological, behavioral, psychosocial, and physical environmental levels of influence.4 At the behavioral-biological level, competing hypotheses have included energy imbalance,5 high fructose corn syrup,6 glycemic index and load,7 shorter sleep durations,8 chicken fat virus,9 chemicals found in plastics,10, 11 low physical activity (PA),12 high sedentary behavior,13 and other possible factors.14 Many genetic polymorphisms have been related to obesity,15 supported by the estimate that obesity is as high as 70% heritable.16
Schools17 and families18 have been implicated in causal pathways to child obesity. Schools have been castigated for providing unhealthy meals at lunch, offering unhealthy beverages and foods in vending machines, stores offering unhealthy foods, food carts rolled between classes, school-sanctioned, parent-provided treats for parties in classrooms, providing inadequate PA in physical education and recess, inadequate PA in after-school programs,19 and declines in walking to school.20 Recently, parents have received attention with concern that authoritarian, permissive, and neglectful parenting styles,21 as well as various aspects of food, PA, and screen media-use parenting practices, may contribute to child obesity.18
Within this complex web of many possible causes of child obesity, understanding the dominant influences may provide an effective focus for national prevention efforts. Several recent studies have addressed school versus home influences by analyzing summertime versus school year changes (herein called seasonal differences) in body composition.22–27 The small number of studies and large heterogeneity in designs, measures, and analyses, within and across types of studies, preclude a meta-analysis, but a narrative review is appropriate. This article briefly summarizes these findings and attempts to draw inferences for further research and practice.
Review of Descriptive Studies
In a six-cohort longitudinal study, each spanning 6 years, with 446 children weighed monthly in Japan, 68.4% of obese children increased their weight in the summer (nonschool) months, with only 9.0% of healthy weight children doing so.22 Healthy weight children tended to increase their weight in the fall, winter, or early spring and decrease weight during the summer. This was the same for boys and girls. The researchers attributed the summer weight gain to the advent of air conditioners, which, they suggested, reduced child outdoor PA.22
BMIs from 5380 children in the Early Childhood Longitudinal Study, Kindergarten Cohort (a nationally representative sample) were collected at the beginning and end of both kindergarten and first grade (1998–2000).23 BMI growth occurred during summer vacation in both overweight and healthy weight children, but occurred faster among ethnic minority (black, Hispanic) children and those already overweight at first assessment.23 Individual- and school-level variances in BMI change were also higher in summer.
Among Native American children in central Wyoming, BMI gain was obtained at several strategic transitions from 149 to 251 third to eighth graders (depending on study component).24 Significant summer BMI gains were detected in the third, fourth, and fifth grade, but not seventh grade, girl cohorts, and only the fourth-grade boy cohort,24 but the grade-level cohorts tended to be small (as few as n=13). Summer BMI (but not BMI z-score) gains were significant among the full sample of overweight and obese boys and girls, but not the healthy weight children.
Native American children (n=454; 48.4% female) attending kindergarten in South Dakota provided data four times: in the fall (near the beginning of the school year), again in the spring, and in the fall and spring of first grade.25 Analyses revealed significant increases in BMI z-score during the first grade, but not kindergarten or summer. Among the overweight and obese children, increases in BMI occurred in kindergarten and first grade, but not summer, whereas the healthy weight children's BMI increase occurred in first grade.25 The influence of a school obesity prevention intervention, the framework within which these data were collected, was not presented or explicitly statistically controlled for in the report.
Returning to Japan, BMIs were collected monthly from 148 boy and 113 girl 0 to 6 year olds followed for 6 years.26 Among overweight boys and girls in general, larger weight increases occurred in the summer during the last year of the study only, but among healthy weight children larger weight increases occurred in the fall. This suggests that the seasonal differences start at about 5 years of age, when children begin elementary school.
Most recently, 3588 ethnically diverse kindergartners in Texas had their height and weight assessed biannually in the fall and winter for 6 years.27 Averaging across the 6 years, BMI percentile decreased 1.5 percentile points during the school year and increased 5.2 percentile points during the summer. Children with healthy weight at baseline increased 0.4 percentile points during the school year and 6.2 percentile points during summer, whereas children who were overweight or obese at baseline decreased 7.9 and 3.7 percentile points during school and increased 4.2 and 1.8 percentile points during summer, respectively.27 The standard deviations for all mean percentile changes were quite high. An interaction term for ethnic group was not significant; differences were not reported by gender. More-detailed analyses revealed annual seasonal cycles in BMI z-score change over 5 years from first through fifth grades, but not in kindergarten (J. Moreno, personal communication), which is consistent with findings from Japan26 and Shanghai.28
Review of Intervention Studies
Among 73 initially overweight youth (10.5±2.8 years of age) in a pediatric weight control clinic in Canada, percent ideal body weight was measured every 2 months over 1 year.29 Children were not exposed to a diet or PA program, but did set goals to change their behavior. Average percent ideal body weight increased only in the July–August period, decreased in all other 2-month intervals, and the percent who lost weight was lowest in the July–August interval.29 The researchers indicated that participant self-monitoring record keeping of diet and PA was also lowest in this period (indicating a need for objective measures) and pointed to the need to better understand home influences on child behavior, especially in the summer.
As part of an evaluation of a 1-year school PA program with 17 overweight rural middle school children with starting BMI above the 95th percentile in Wisconsin,30 the 9-month school year improvements in percent body fat (as determined by DEXA), cardiovascular fitness, and fasting insulin were lost during the summer break.30
In a 3-year school cluster randomized fitness intervention with 206 third graders (at the start of the study; 47% male; 63% black) in Georgia,31 both percent body fat (as determined by DEXA) and fitness improved in the intervention group, in comparison to the control group, during the 3 school years and were lost during the summer months.31 No differences were reported by gender or ethnic groups.
A 3-year after-school program promoting PA starting in third grade in Georgia assessed percent body fat (from DEXA) and cardiovascular fitness on 574 children (32% white; 47% male) collected in the fall and spring of the sequential three grades.32 Average percent body fat decreased during the school years in the third and fourth, but not fifth, grades, and in the average, the positive outcomes were lost during the summer months.32 Fitness gains were detected in the third and fifth grades and also lost during the summer months.32
Seasonal Differences in Physical Activity
To test specifically whether energy expenditure differed between summer and school year, doubly labeled water was used in a cross-sectional study among 96 overweight or obese 6 to 13 year olds measured during the school year and 66 similar youth measured during the summer.33 Whereas total energy expenditure and BMI were higher during the school year, after statistically controlling for fat-free mass, total energy expenditure was no longer significant. Other, potentially confounding differences were detected between groups (e.g., resting metabolic rate and percent fat). Differences were not reported between genders or ethnic groups. The study design was not able to assess differences between overweight or obese with healthy weight youth or to relate energy expenditure to level of change (increases or decreases) in BMI across seasons.
To test changes over the summer only in BMI, diet, and PA, for thirty 9- to 11-year-old Minnesota children (19 male; ethnic groups not identified), data were collected at the end of one school year and again at the end of that summer.34 BMI and BMI percentile increased over the summer, whereas light and moderate PA declined [but not moderate-to-vigorous PA (MVPA) or vigorous PA] and sedentary behavior increased.34 No changes were detected in kilocalories or any macronutrient intake.
Two reviews have been published on seasonal patterns in PA among children.35,36 The more inclusive review across 35 studies from 12 countries reported that 83% of studies consistently detected a seasonality effect with more PA in the summer and least activity in the winter among 7- to 18-year-old children, but not younger children.35 Two studies revealed that rural youth were more active in the summer and urban youth more active in the winter. Differences by adiposity status were not reported.35 The more restrictive review (only studies using accelerometers to assess level of activity), which included seasonal differences in sedentary behavior, also reported that most studies found more PA in the summer and less in the winter.36 They reported conflicting results on seasonality of sedentary behavior and no report of differences by adiposity, gender, or ethnic groups.36
No studies, published since the reviews, investigated seasonal differences in PA by adiposity status. Among Canadian adolescents (n=547), PA declined across the school year primarily as the result of a decline in organized (sports) activities.37 Among English 9- to 10-year-old children (n=1029), quite different complex models were obtained predicting MVPA and sedentary behavior when including BMI versus not.38 In all analyses, MVPA was highest and sedentary behavior was lowest in the summer.38 Among Dutch preschoolers (n=347), BMI z-score was not related to PA.39 None of these analyses were designed to test whether the influence of season on child PA varied by BMI status.
Finally, seasonal differences in PA such as play were qualitatively investigated from a sociological perspective in a small sample of New Zealand families with children of unspecified age (n=20; 11 suburban and 9 inner city).40 Parents in suburban areas felt outside PA (e.g., roaming independently or biking) for children was a natural part of suburban life in summer and even in the winter (but less so). Parents living in a city identified many barriers to child PA. Sedentary behavior was perceived as more appropriate in the city for both summer and winter. Winter PA implied mostly winter sport teams, whereas summer activity emphasized activity-based play. Many parents (urban and suburban) perceived a need to protect their child by keeping them indoors in winter, especially in cold and inclement weather.40 The researchers reported that the parents did not perceive (and thereby did not act on) the opportunities for PA in the city in winter.40 This very-small-sample qualitative study needs to be interpreted with caution, but provocatively indicated highly nuanced parenting behavior in regard to child PA between seasons and between urban and suburban parents. The study did not address differences between healthy and overweight children.
Discussion
Diverse designs, methods, measures, and samples were employed to test related, but not identical, hypotheses about seasonal BMI or weight gain among school-age youth. The most common pattern without intervention was weight loss during the school year, and weight gain during the summer, for the overweight and obese, but less so among healthy weight children. This pattern was true of young children in Japan,22,26 kindergartners in the United States,23 9 to 11 year old Minnesotans,34 and kindergartners in Texas.27 Among Native Americans in central Wyoming, this pattern characterized the younger girls and one grade of young boys (fourth graders),24 but did not characterize early-elementary Native American children in South Dakota.25 The seasonal pattern may be inconsistent with the documented higher BMI increases among overweight and obese children during the winter holidays41 or may be consistent in that children are away from the structure within school at both times. Among several school fitness intervention evaluations that collected annual data in the fall and spring, the BMI and fitness improvements obtained during the school year were lost during the summer among middle schoolers in Wisconsin30 and twice among third through fifth graders in Georgia.31,32
Research on child maturation and growth mostly before the onset of the obesity epidemic indicated that most seasonal child weight gain was during the winter.42 More recently, among younger children in Shanghai, China (n=4128), weight or BMI gain was in the fall or winter.28 Whereas all children should put on weight over time, the seasonal differences between overweight and healthy weight children indicate that different influences are occurring. Both the large summertime increases, among the overweight, in BMI z-scores in Texas27 and the loss, during the summer, of fitness increases from intervention programs during the school year30–32 indicate that these are not healthy summertime changes for overweight or obese children.
Tests of these seasonal patterns in aspects of body composition need to be replicated in other countries, especially those varying in climatic zones. It may be, as suggested in Japan,22 that the extensive introduction of air conditioning decreased summer outdoor PA patterns.43 Because air conditioning is common and an accepted fact of life in the United States, to which it would be very difficult to randomize homes, it would be valuable to test this pattern in areas with less (e.g., northern temperate zones) and more air conditioning (e.g., southern temperate zones) as well as in homes with and without air conditioning (e.g., lower-income homes). Randomization to home air conditioning may be possible in other less economically developed countries.
This consistent pattern of fairly rapid seasonal change in BMI in most sites appears to reflect the influences of energy imbalance.44 In the areas in which the seasonal pattern has been clearly documented, a next first step needs to identify what energy-balance–related behaviors account for the summer/school year changes: caloric intake; caloric expenditure (including PA and sedentary behavior); or sleep.44 The summertime loss of school-time fitness–related increases (from PA interventions)30–32 suggests that differences in PA could account for the seasonal changes in BMI. This is supported by the documented summer decline in MVPA,34 and the lower total energy expenditure in summer,27 but not supported by the lack of summer/school year difference in total energy expenditure corrected for fat-free mass.27
The reviews indicating greater activity in the summer and less in the winter would appear to contradict the greater BMI gain in summer and decline in the winter among the overweight. It is possible that the seasonal pattern in PA characterizes the healthy weight children, but not the overweight children. Additional research needs to investigate overweight versus healthy weight group differences in patterns of BMI change and PA. The availability of structured PA programs during the school year (e.g., physical education,45 active commuting to school, recess,46 and sport teams47) may engage overweight or obese children, who may not have structured opportunities during the summer. The sociological study indicated that there were major suburban-urban differences in opportunities for child PA, and less activity was encouraged in winter. This seems inconsistent with the reported patterns in seasonal weight gain and loss among overweight children, except that the parents reported that winter sports were the primary winter PA opportunity. This study, however, also did not separate overweight from healthy weight children.40 Urban children attending summer camp (n=57), however, participated in more PA than those who stayed at home.48 Future research needs to address urban- versus suburban-located seasonal influences on PA and adiposity.
The amount of PA per day may be biologically regulated, such that bouts of extra PA early in a day are compensated with less activity later in the day,49 but this has been questioned.50 Obese children may not be compensating when exposed to structured PA at school (perhaps as a result of some impaired PA self-regulation mechanism), whereas healthy weight children are. Compensation effects can be assessed by comparing days with and without PA in the morning.
The seasonal BMI increase in summer and BMI loss or no increase during the school year was true of black and Hispanic, but not other, populations in the United States in one large sample study,23 but not another.27 Speculations on these findings have not been presented in the literature. Further research will need to address this important health-disparities–related issue. Similarities and differences in seasonal energy-balance–related practices between Japan and the United States may elucidate influences on the common patterns in these countries. Cross-cultural research would be valuable in this regard.
Unfortunately, assessment of dietary or caloric intake among children incorporates substantial error,51 which makes it difficult to detect patterns corresponding to the seasonal changes in BMI.34 One study with Greek children and adolescents reported average daily calorie intake was 344 kilojoules higher in the spring and summer than the fall and winter,52 but no explanations were provided. It is possible that more calories are consumed in the summer as a result of the possible greater home availability of child-preferred foods and more time available for eating. Whereas lower-income children might be expected to gain more access to calories during the school year (e.g., from free school breakfasts and lunches), these calories may come from healthier, more nutrient-dense foods, compared to more energy-dense, nutrient-poor foods available in their homes in the summer. It may also be valuable to assess factors associated with energy intake, which could be more reliably assessed (e.g., appetite, satiety, or food preferences).53 New objective measures of dietary intake54 may facilitate assessment of energy intake variables once these innovative procedures have been adapted to, and validated with, children. At that time, it would be valuable to document caloric intake while in school (e.g., food items from school sources, school breakfast, school lunch, vending machines, or parties) versus in the home and out of school, including snacks during travel to and from school, and while viewing screen media.55
Sleep duration has been inversely associated with child obesity56,57; however, little is known about seasonal variation in sleep duration among children. One study that objectively examined seasonal differences in child sleep duration with actigraphy58 found significant and clinically meaningful less sleep in the summer than during the school year. This was likely a result of children going to bed later in the summer. Though adolescents compensated during the school year for shorter weekday sleep with longer weekend sleep,59,60 this has not been consistently demonstrated for children, who may not compensate for later weekend bedtimes with later weekend wake times.58,61 Children who did not compensate for shorter weekday sleep duration and later bedtimes on weekends [odds ratio (OR), 2.59] or holidays (OR, 2.32) were more likely to be overweight or obese.62 Among 8- to 11-year-old children, experimentally manipulated sleep restriction for only 1 week (having the child go to bed 1 hour later than his or her typical bedtime) resulted in increased caloric intake and weight gain.63 Thus, shorter sleep duration over the summer than the school year may also contribute to seasonal changes in weight.
Whereas seasonal variation in energy-balance–related behaviors would appear to be the proximal cause of the patterns in seasonal BMI change, home influences may differentiate summer versus school-year changes. Food-related parenting practices are the behaviors that parents exert directly to influence child behavior and are thought to include nurturance, control, and structure components.64 It is not clear whether parenting practices are similarly employed between summer and winter, parents are more indulgent during the summer, or children who spend summertime away from home (e.g., summer camp, day care, or grandparents) do not benefit from structure at home and at school. The home physical environment (an aspect of parenting structure) influenced child PA.65 Parents who used more rules in general to govern child behavior, including sleep rules, had children who slept longer.66 Family risk moderated the effect of sleep deprivation on obesity.67 Increasing family routines decreased BMI.68 Further research should assess seasonal stability in the home PA environment, as well as sleep-related parenting practices (e.g., parenting structure or rules) and routines,68 and whether these accounted for the seasonal BMI differences.
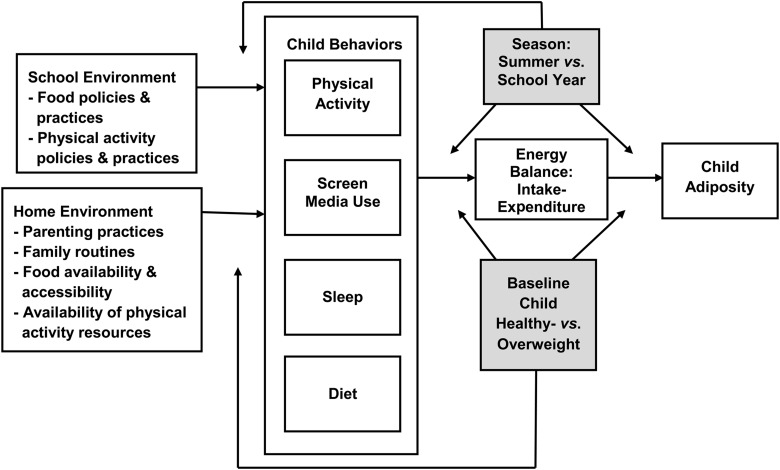
Figure 1 presents a graphic depiction of the factors likely involved in explaining the seasonal differences in weight gain. Following energy balance concepts, energy intake minus expenditure is the primary determinant of child BMI z-scores. As detailed in this article, physical activity, screen media use, sleep patterns, and diet likely contribute to energy imbalance. School food and physical activity (e.g., physical education, sports, and active commuting to school) policies and practices will influence these child behaviors primarily during the school year, whereas parenting practices and family routines will influence these behaviors throughout the year. Consistency in parenting practices between summer and winter is not known. Season (summer vs. school year) will moderate these relationships at the point of environment influencing behavior and perhaps further downstream as well. Child weight at baseline assessment will also likely be a moderator. This conceptual model is likely a simplification of possible influences, but should provide a reasonable representation of potential factors to consider to explain the seasonal differences in adiposity.
Figure 1.
Conceptual model of influences on seasonal differences in BMI (shaded boxes indicate possible moderating variables).
Conclusion
Although schools may not provide a perfect environment for encouraging healthy energy-balance–related behaviors, they appear to provide some obesity protection. Research is needed to clarify where, when, and why these differences occur, both to enhance the obesity protective influences in schools and to mitigate the obvious obesigenic influences outside of school.
Acknowledgments
This work was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (5R01DK091254). This work is also a publication of the USDA (USDA/ARS) Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine (Houston, TX) and had been funded, in part, with federal funds from the USDA/ARS under Cooperative Agreement No. 58-6250-6001. The contents of this publication do not necessarily reflect the views or policies of the USDA nor does mention of trade names, commercial products, or organizations imply endorsement from the US government.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief 2012;82:1–8 [PubMed] [Google Scholar]
- 3.Nadeau KJ, Maahs DM, Daniels SR, et al. Childhood obesity and cardiovascular disease: Links and prevention strategies. Nat Rev Cardiol 2011;8:513–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pate RR, O'Neill JR, Liese AD, et al. Factors associated with development of excessive fatness in children and adolescents: A review of prospective studies. Obes Rev 2013;14:645–658 [DOI] [PubMed] [Google Scholar]
- 5.Wang YC, Orleans CT, Gortmaker SL. Reaching the healthy people goals for reducing childhood obesity: Closing the energy gap. Am J Prev Med 2012;42:437–444 [DOI] [PubMed] [Google Scholar]
- 6.Wells JC, Siervo M. Obesity and energy balance: Is the tail wagging the dog? Eur J Clin Nutr 2011;65:1173–1189 [DOI] [PubMed] [Google Scholar]
- 7.Mirza NM, Palmer MG, Sinclair KB, et al. Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: A randomized controlled trial. Am J Clin Nutr 2013;97:276–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magee CA, Caputi P, Iverson DC. The longitudinal relationship between sleep duration and body mass index in children: A growth mixture modeling approach. J Dev Behav Pediatr 2013;34:165–173 [DOI] [PubMed] [Google Scholar]
- 9.Atkinson RL. Human adenovirus-36 and childhood obesity. Int J Pediatr Obes 2011;6(Suppl. 1):2–6 [DOI] [PubMed] [Google Scholar]
- 10.Trasande L, Spanier AJ, Sathyanarayana S, et al. Urinary phthalates and increased insulin resistance in adolescents. Pediatrics 2013;132:e646–e655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eng DS, Lee JM, Gebremariam A, et al. Bisphenol A and chronic disease risk factors in US children. Pediatrics 2013;132:e637–e645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rauner A, Mess F, Woll A. The relationship between physical activity, physical fitness and overweight in adolescents: A systematic review of studies published in or after 2000. BMC Pediatr 2013;13:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.te Velde SJ, van Nassau F, Uijtdewilligen L, et al. Energy balance-related behaviours associated with overweight and obesity in preschool children: A systematic review of prospective studies. Obes Rev 2012;13(Suppl. 1):56–74 [DOI] [PubMed] [Google Scholar]
- 14.McAllister EJ, Dhurandhar NV, Keith SW, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr 2009;49:868–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouchard C. The biological predisposition to obesity: Beyond the thrifty genotype scenario. Int J Obes (Lond) 2007;31:1337–1339 [DOI] [PubMed] [Google Scholar]
- 16.Min J, Chiu DT, Wang Y. Variation in the heritability of body mass index based on diverse twin studies: A systematic review. Obes Rev 2013;14:871–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baranowski T, Cerin E, Baranowski J. Steps in the design, development and formative evaluation of obesity prevention-related behavior change trials. Int J Behav Nutr Phys Act 2009;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vollmer R, Mobley AR. Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight. A review. Appetite 2013;71:232–241 [DOI] [PubMed] [Google Scholar]
- 19.Clarke J, Fletcher B, Lancashire E, et al. The views of stakeholders on the role of the primary school in preventing childhood obesity: A qualitative systematic review. Obes Rev 2013July12 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Tudor-Locke C, Ainsworth BE, Popkin BM. Active commuting to school: An overlooked source of childrens' physical activity? Sports Med 2001;31:309–313 [DOI] [PubMed] [Google Scholar]
- 21.Rhee KE, Lumeng JC, Appugliese DP, et al. Parenting styles and overweight status in first grade. Pediatrics 2006;117:2047–2054 [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi M, Kobayashi M. The relationship between obesity and seasonal variation in body weight among elementary school children in Tokyo. Econ Hum Biol 2006;4:253–261 [DOI] [PubMed] [Google Scholar]
- 23.von Hippel PT, Powell B, Downey DB, et al. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am J Public Health 2007;97:696–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith DT, Bartee RT, Dorozynski CM, et al. Prevalence of overweight and influence of out-of-school seasonal periods on body mass index among American Indian schoolchildren. Prev Chronic Dis 2009;6:A20. [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J, Himes JH, Hannan PJ, et al. Summer effects on body mass index (BMI) gain and growth patterns of American Indian children from kindergarten to first grade: A prospective study. BMC Public Health 2011;11:951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kato N, Sauvaget C, Kato T. Large summer weight gain in relatively overweight preschool Japanese children. Pediatr Int 2012;54:510–515 [DOI] [PubMed] [Google Scholar]
- 27.Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: Results of a 5-year longitudinal study. J Sch Health 2013;83:473–477 [DOI] [PubMed] [Google Scholar]
- 28.Xu X, Wang WP, Guo ZP, et al. Seasonality of growth in Shanghai infants (n=4128) born in 11 consecutive years. Eur J Clin Nutr 2001;55:714–725 [DOI] [PubMed] [Google Scholar]
- 29.Gillis L, McDowell M, Bar-Or O. Relationship between summer vacation weight gain and lack of success in a pediatric weight control program. Eat Behav 2005;6:137–143 [DOI] [PubMed] [Google Scholar]
- 30.Carrel AL, Clark RR, Peterson S, et al. School-based fitness changes are lost during the summer vacation. Arch Pediatr Adolesc Med 2007;161:561–564 [DOI] [PubMed] [Google Scholar]
- 31.Gutin B, Yin Z, Johnson M, et al. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: The Medical College of Georgia Fitkid Project. Int J Pediatr Obes 2008;3(Suppl. 1):3–9 [DOI] [PubMed] [Google Scholar]
- 32.Yin Z, Moore JB, Johnson MH, et al. The impact of a 3-year after-school obesity prevention program in elementary school children. Child Obes 2012;8:60–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zinkel SR, Moe M, 3rd, Stern EA, et al. Comparison of total energy expenditure between school and summer months. Pediatr Obes 2013;8:404–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCue M, Marlatt K, Sirard J, et al. Examination of changes in youth diet and physical activity over the summer vacation period. Internet J Allied Health Sci Pract 2013;11:1–6 [Google Scholar]
- 35.Carson V, Spence JC. Seasonal variation in physical activity among children and adolescents: A review. Pediatr Exerc Sci 2010;22:81–92 [DOI] [PubMed] [Google Scholar]
- 36.Rich C, Griffiths LJ, Dezateux C. Seasonal variation in accelerometer-determined sedentary behaviour and physical activity in children: A review. Int J Behav Nutr Phys Act 2012;9:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bruner MW, Chad KE, Beattie-Flath JA, et al. Examination of physical activity in adolescents over the school year. Pediatr Exerc Sci 2009;21:421–435 [DOI] [PubMed] [Google Scholar]
- 38.Pearce MS, Basterfield L, Mann KD, et al. Early predictors of objectively measured physical activity and sedentary behaviour in 8–10 year old children: The Gateshead Millennium Study. PLoS One 2012;7:e37975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wijtzes AI, Kooijman MN, Kiefte-de Jong JC, et al. Correlates of physical activity in 2-year-old toddlers: The generation R study. J Pediatr 2013;163:791–799.e2. [DOI] [PubMed] [Google Scholar]
- 40.Ergler CR, Kearns RA, Witten K. Seasonal and locational variations in children's play: Implications for wellbeing. Soc Sci Med 2013;91:178–185 [DOI] [PubMed] [Google Scholar]
- 41.Branscum P, Kaye G, Succop P, et al. An evaluation of holiday weight gain among elementary-aged children. J Clin Med Res 2010;2:167–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malina RM, Bouchard C. Growth, Maturation and Physical Activity. Human Kinetics Books: Champaign, IL, 1991 [Google Scholar]
- 43.Baranowski T, Thompson WO, DuRant RH, et al. Observations on physical activity in physical locations: Age, gender, ethnicity and month effects. Res Q Exerc Sport 1993;64:127–133 [DOI] [PubMed] [Google Scholar]
- 44.Bleich SN, Ku R, Wang YC. Relative contribution of energy intake and energy expenditure to childhood obesity: A review of the literature and directions for future research. Int J Obes (Lond) 2011;35:1–15 [DOI] [PubMed] [Google Scholar]
- 45.Cawley J, Frisvold D, Meyerhoefer C. The impact of physical education on obesity among elementary school children. J Health Econ 2013;32:743–755 [DOI] [PubMed] [Google Scholar]
- 46.Ickes MJ, Erwin H, Beighle A. Systematic review of recess interventions to increase physical activity. J Phys Act Health 2012;10:910–926 [DOI] [PubMed] [Google Scholar]
- 47.Drenowatz C, Steiner RP, Brandstetter S, et al. Organized sports, overweight, and physical fitness in primary school children in Germany. J Obes 2013;2013:935245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tovar A, Lividini K, Economos CD, et al. School's out: What are urban children doing? The Summer Activity Study of Somerville Youth (SASSY). BMC Pediatr 2010;10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilkin TJ, Mallam KM, Metcalf BS, et al. Variation in physical activity lies with the child, not his environment: Evidence for an ‘activitystat’ in young children (EarlyBird 16). Int J Obes (Lond) 2006;30:1050–1055 [DOI] [PubMed] [Google Scholar]
- 50.Long MW, Sobol AM, Cradock AL, et al. School-day and overall physical activity among youth. Am J Prev Med 2013;45:150–157 [DOI] [PubMed] [Google Scholar]
- 51.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc 2010;110:1501–1510 [DOI] [PubMed] [Google Scholar]
- 52.Yannakoulia M, Drichoutis AC, Kontogianni MD, et al. Season-related variation in dietary recalls used in a paediatric population. J Hum Nutr Diet 2010;23:489–493 [DOI] [PubMed] [Google Scholar]
- 53.Eloranta AM, Lindi V, Schwab U, et al. Dietary factors associated with overweight and body adiposity in Finnish children aged 6–8 years: The PANIC Study. Int J Obes (Lond) 2012;36:950–955 [DOI] [PubMed] [Google Scholar]
- 54.Sun M, Fernstrom JD, Jia W, et al. A wearable electronic system for objective dietary assessment. J Am Diet Assoc 2010;110:45–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gebremariam MK, Bergh IH, Andersen LF, et al. Are screen-based sedentary behaviors longitudinally associated with dietary behaviors and leisure-time physical activity in the transition into adolescence? Int J Behav Nutr Phys Act 2013;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hart CN, Jelalian E. Shortened sleep duration is associated with pediatric overweight. Behav Sleep Med 2008;6:251–267 [DOI] [PubMed] [Google Scholar]
- 57.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265–274 [DOI] [PubMed] [Google Scholar]
- 58.Nixon GM, Thompson JM, Han DY, et al. Short sleep duration in middle childhood: Risk factors and consequences. Sleep 2008;31:71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carskadon MA. Sleep in adolescents: The perfect storm. Pediatr Clin North Am 2011;58:637–647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moore M, Meltzer LJ. The sleepy adolescent: Causes and consequences of sleepiness in teens. Paediatr Respir Rev 2008;9:114–120; quiz, 20–21. [DOI] [PubMed] [Google Scholar]
- 61.Gulliford MC, Price CE, Rona RJ, et al. Sleep habits and height at ages 5 to 11. Arch Dis Child 1990;65:119–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wing YK, Li SX, Li AM, et al. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics 2009;124:e994–e1000 [DOI] [PubMed] [Google Scholar]
- 63.Hart CN, Carskadon M, Considine R, et al. Changes in children's sleep duration on food intake, weight, and leptin. Pediatrics 2013;132:e1473–e1480 [DOI] [PubMed] [Google Scholar]
- 64.Hughes SO, O'Connor TM, Power TG. Parenting and children's eating patterns: Examining control in a broader context. Int J Child Adolesc Health 2008;1:323–330 [Google Scholar]
- 65.Maitland C, Stratton G, Foster S, et al. A place for play? The influence of the home physical environment on children's physical activity and sedentary behaviour. Int J Behav Nutr Phys Act 2013;10:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jones CH, Pollard TM, Summerbell CD, et al. Could parental rules play a role in the association between short sleep and obesity in young children? J Biosoc Sci 2013June11 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 67.Bagley EJ, El-Sheikh M. Familial risk moderates the association between sleep and zBMI in children. J Pediatr Psychol 2013;38:775–784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haines J, McDonald J, O'Brien A, et al. Healthy habits, happy homes: Randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr 2013;167:1072–1079 [DOI] [PubMed] [Google Scholar]